Acute hepatitis ICD code 10. Chronic viral hepatitis. What is reactive hepatitis
Chronic cryptogenic hepatitis, chronic idiopathic hepatitis
Version: Directory of Diseases MedElement
Chronic hepatitis, unspecified (K73.9)
Gastroenterology
general information
Short description
Chronic hepatitis, unspecified(chronic hepatitis syndrome, cryptogenic chronic hepatitis) - a group of inflammatory liver diseases caused by various causes, characterized by varying degrees of severity of hepatocellular necrosis and inflammation with a predominance of lymphocytes in the infiltrate Infiltrate - a tissue area characterized by an accumulation of cellular elements that are usually not characteristic of it, an increased volume and increased density.
.
The concept of "chronic hepatitis" is due to the duration of the disease for more than 6 months. Other criteria for the disease are a persistent increase in liver tests by 1.5 times and, possibly, an increase in INR. International normalized ratio (INR) - a laboratory indicator determined for evaluation external path blood clotting
also 1.5 times.
The diagnosis of "chronic hepatitis, unspecified" can be set as preliminary or main, when the etiological factor is not specified or undefined.
In approximately 10-25% of cases, the etiology of chronic hepatitis cannot be unambiguously determined even when using all diagnostic tools. In this case, the term "chronic cryptogenic (idiopathic) hepatitis" is adopted - a liver disease with morphological manifestations characteristic of chronic hepatitis, with the exclusion of viral, immune and drug etiology.
With the development of diagnostic methods in the United States, the number of patients with this diagnosis has decreased to 5.4% of all patients with chronic hepatitis. About 2.8% of the US population has elevated levels ALT >1.5 norms that cannot be explained in any way.
Flow period
Minimum flow period (days): 180
Maximum flow period (days): not specified
Classification
I. Classification according to ICD-10
K73.0 Chronic persistent hepatitis, not elsewhere classified;
K73.1 Chronic lobular hepatitis, not elsewhere classified;
K73.2 Chronic active hepatitis, not elsewhere classified;
K73.8 Other chronic hepatitis, not elsewhere classified;
- K73.9 Chronic hepatitis, unspecified.
II. Principles of classification, excerpts(Los Angeles, 1994)
1. According to the degree of activity (morphological criteria):
- minimum;
- low;
- moderate;
- high.
2. According to the stage of the disease (morphological criteria):
- fibrosis is absent;
- weak;
- moderate;
- heavy;
- cirrhosis.
The activity and stage of the inflammatory process (except for cirrhosis) is determined only on the basis of a histological examination. With a preliminary diagnosis, in the absence of histology, a preliminary (evaluative) determination of the ALT level is possible.
Determination of the degree of activity by the level of ALT:
1. Low activity - an increase in ALT less than 3 norms.
2. Moderate - from 3 to 10 norms.
3. Expressed - more than 10 norms.
The degree of activity of cryptogenic hepatitis in these cases can also be described as minimal, mild and moderate, pronounced.
III. Also used to determine the degree of activity histological Knodel activity index.
Index components:
- periportal necrosis with or without bridging necrosis (0-10 points);
- intralobular degeneration and focal necrosis (0-4 points);
- portal necrosis (0-4 points);
- fibrosis (0-4 points).
The first three components reflect the degree of activity, the fourth component - the stage of the process.
The histological activity index is calculated by summing the first three components.
There are four levels of activity:
1. The minimum degree of activity - 1-3 points.
2. Low - 4-8 points.
3. Moderate - 9-12 points.
4. Expressed - 13-18 points.
IV. Chronic hepatitis is distinguished by stage (METAVIR scale):
- 0 - no fibrosis;
- 1 - mild periportal fibrosis
- 2 - moderate fibrosis with porto-portal septa;
- 3 - severe fibrosis with porto-central septa;
- 4 - cirrhosis of the liver.
Previously by morphology There are two types of chronic hepatitis:
1. Chronic persistent hepatitis - when the infiltration was only in the portal zones.
2. Chronic active (aggressive) hepatitis - when the infiltration entered the lobules.
Then these terms were replaced by the degree of activity. The same classification is used in ICD-10. Minimal activity corresponds to persistent hepatitis, moderate and high activity - active.
Note. Determination of the stage of activity and morphological features allows more accurate coding of cryptogenic hepatitis in the appropriate subcategories of K73 "Chronic hepatitis, not elsewhere classified".
Etiology and pathogenesis
Since chronic hepatitis is unspecified, the etiology of the disease is not specified or determined.
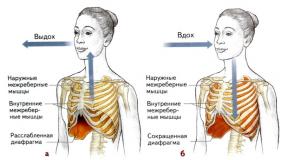
Morphological definition: chronic hepatitis is a diffuse inflammatory-dystrophic lesion of the liver, characterized by lymphoplasmacytic infiltration of portal fields, hyperplasia of Kupffer cells, moderate fibrosis in combination with dystrophy of liver cells while maintaining the normal lobular structure of the liver.
Epidemiology
Age: mostly adults
Sign of prevalence: Rare
The true prevalence is either highly variable or unknown.
With the improvement of diagnostic methods, it becomes obvious that cryptogenic chronic hepatitis is the prerogative of mainly adult patients. In children, as a rule, chronic hepatitis can be verified as viral and/or autoimmune.
One study indicates a slight predominance of men of mature age among patients with this diagnosis.
Factors and risk groups
Risk factors and risk groups for chronic hepatitis have not been identified. Certainly an important role is played by:
- genetically determined changes in the metabolic activity of hepatocytes;
- autoimmune diseases and other disorders of the immune response;
- viral infections;
- toxic damage.
Clinical picture
Clinical Criteria for Diagnosis
Weakness; abdominal discomfort; weight loss; nausea; belching; pain in the right hypochondrium; fever; jaundice; telangiectasia; bloating; hepatomegaly
Symptoms, course
The clinical picture of chronic hepatitis is diverse. The disease can have a different course - from subclinical forms with minimal laboratory changes to a symptomatic exacerbation (acute hepatitis).
Most characteristic symptoms and syndromes:
- asthenovegetative syndrome: weakness, fatigue, decreased performance, sleep disturbance, autonomic symptoms;
- weight loss (rare);
- dyspeptic syndrome: loss of appetite, nausea, belching, abdominal discomfort, bloating, bitterness in the mouth, dry mouth;
- fever or subfebrile condition in the acute stage;
- hepatomegaly, splenomegaly Splenomegaly - persistent enlargement of the spleen
(may be associated with hypersplenism) Hypersplenism is a combination of an enlarged spleen with an increase in the number of cellular elements in the bone marrow and a decrease in formed elements in the peripheral blood.
) about 20% of patients;
- cholestatic syndrome: jaundice, cholestasis Cholestasis is a violation of the flow of bile in the form of stagnation in bile ducts and/or grooves.
(rarely);
- hemorrhagic syndrome(rarely);
- moderate hepatomegaly Hepatomegaly is a significant enlargement of the liver.
.
Diagnostics
The diagnosis of chronic cryptogenic hepatitis is a diagnosis of exclusion.
Ultrasound, CT, MRI, radionuclide methods reveal hepatomegaly and diffuse changes structures of the liver. In the diagnosis of hepatitis, these studies are of little significance and are used for the differential diagnosis of complications (liver cirrhosis, hepatocellular carcinoma).
Other imaging modalities, such as ERCP ERCP - endoscopic retrograde cholangiopancreatography
, HIDA are used for differential diagnosis in severe cholestasis. It is advisable to use Fibroscan to identify the degree of fibrosis.
Puncture or safer transjugular biopsy with histological examination allows you to verify the diagnosis of chronic hepatitis, determine its activity and stage.
Laboratory diagnostics
For laboratory syndromes chronic hepatitis include syndromes of cytolysis, hepatocellular insufficiency, immunoinflammatory syndrome and cholestasis syndrome.
Cytolysis syndrome- the main indicator of the activity of the inflammatory process in the liver, the markers of which are an increase in the activity of ALT, AST, GGTP, glutamate dehydrogenase, LDH and its isoenzymes LDH4 and LDH5.
Syndrome of hepatocellular insufficiency characterized by a violation of the synthetic and neutralizing function of the liver.
Violation of the synthetic function of the liver is reflected by a decrease in the content of albumin, prothrombin, proconvertin and other blood coagulation factors, cholesterol, phospholipids, lipoproteins.
In connection with dysproteinemia, the stability of the colloidal blood system is disturbed, on the basis of which sedimentary or flocculation samples are based. Thymol and sublimate samples have become widespread in the CIS.
A sharp decrease in prothrombin and proconvertin (by 40% or more) indicates severe hepatocellular insufficiency, the threat of hepatic precoma and coma.
The assessment of the neutralizing function of the liver is carried out using loading tests: bromsulfaleic, antipyrine and other tests, as well as the determination of ammonia and phenols in the blood serum. A violation of the detoxification function of the liver is evidenced by the retention of bromsulfalein in plasma, a decrease in the clearance of antipyrine, and an increase in the concentration of ammonia and phenols.
immune inflammatory syndrome characterized primarily by changes in laboratory data:
- hypergammaglobulinemia;
- change in sediment samples;
- increase in the content of immunoglobulins;
- the appearance of antibodies to DNA, smooth muscle cells, mitochondria;
- violations of cellular immunity.
cholestasis syndrome:
- skin itching, dark urine, acholic stools;
- an increase in the concentration of bile components in the blood - cholesterol, bilirubin, phospholipids, bile acids and enzymes - markers of cholestasis (AP, 5-nucleotidase, GGTP.
If the level of alkaline phosphatase / ALT> 3 is exceeded, one should think about excluding other causes of severe cholestasis.
Clinical blood test:
- cytopenia Cytopenia - reduced compared to the norm, the content of cells of a certain type in the object of study
with the development of hypersplenism;
- possible normochromic anemia;
possible thrombocytopenia (very rare).
Urine and stool tests: with cholestasis in the urine, bilirubin can be determined in the absence of urobilin in the urine and stercobilin in the feces.
Differential Diagnosis
Differential Diagnosis chronic hepatitis, unspecified, is carried out with the following diseases:
I. Liver lesions, the etiology of which is determined:
1. Alcoholism. It matters directly toxic effect alcohol with persistent daily alcoholization, the formation of alcoholic hyaline in hepatitis, to which an immune response develops.
2. Viral infection. In 70% of cases, chronic inflammation caused by hepatitis B, C, delta viruses and their combination has been proven. If, 3 months after acute hepatitis, a hepatitis marker Australian antigen (HBs) is found in a patient, the probability of developing chronic hepatitis reaches 80%. In the case of hepatitis A, chronicity is practically not observed.
3. Toxic (including medicinal) damage:
- mushroom poisoning;
- poisoning with drugs that disrupt hepatocyte metabolism (anti-tuberculosis, psychotropic, oral contraceptives, paracetamol, antiarrhythmics, sulfonamides, antibiotics - erythromycin, tetracyclines);
- industrial intoxication with carbon trichloride, oil distillation products, heavy metals.
4. Metabolic - in metabolic diseases (Konovalov-Wilson disease, hemochromatosis, alpha-antitrypsin deficiency).
5. Cholestatic, associated with a primary violation of the outflow of bile.
6. Autoimmune, in which there is no clear connection with toxic damage and the virus, but symptoms of immune inflammation are diagnosed.
II. Specified morphologically and laboratory forms of chronic hepatitis within the rubric "Chronic hepatitis, not elsewhere classified" - K73.
1. Chronic active hepatitis, not elsewhere classified(K73.2).
Chronic active hepatitis (CAH) - long-term current inflammatory process with necrosis and degeneration of hepatocytes.
CAH is characterized by polymorphism of clinical manifestations - from meager to significant, with disability, fever and the appearance of liver signs - "asterisks" on the shoulder girdle, palmar erythema.
The liver remains painless, enlarged and protrudes from under the edge of the costal arch by 2-3 cm or more, its edge is somewhat pointed. In most patients, the spleen can be palpated.
Pathological characteristics of CAH, leading to a violation of the lobular architectonics of the liver:
Destruction of the restrictive plate of hepatocytes;
- lymphoid cell proliferation;
- portal and periportal fibrosis;
- stepwise necrosis.
Morphological examination of liver biopsy specimens is necessary to confirm clinical diagnosis CAH and differential diagnosis with other lesions, primarily with chronic persistent hepatitis and cirrhosis.
Diagnostic errors in morphological examination can occur when a biopsy of an undamaged area of the liver or when it is performed during remission.
The results of a biochemical study of the blood of patients with CAH indicate a violation of various liver functions:
- protein-synthetic - hypoalbuminemia and hyperglobulinemia;
- regulation of pigment metabolism - hyperbilirubinemia (approximately every fourth patient);
- enzymatic - 5-10-fold increase in the level of ALT and AST.
Forms of CAG according to the nature of the flow:
- with moderate activity of the process;
- with high activity of the process (aggressive hepatitis).
Clinical manifestations of process activity: fever, arthralgia, severe hepatic signs.
CAH occurs with periods of exacerbation and remission. The main causes of exacerbation can be: superinfection with hepatotropic viruses; other infectious diseases; alcoholism; taking high doses of drugs; chemical poisoning that adversely affects the liver, etc. It is believed that in approximately 40% of patients with CAH with moderate activity of the process, spontaneous remissions associated with the natural course of the disease can be registered. Currently, it is generally accepted that almost all patients with CAH progress to cirrhosis. At the same time, cases of a favorable course of CAH with stabilization of the process and its transition to chronic persistent hepatitis are described.
2. Chronic lobular hepatitis, not elsewhere classified(K73.1).
Chronic lobular hepatitis is a form of chronic hepatitis corresponding to incomplete acute hepatitis.
The main morphological feature is the predominant development of inflammatory infiltration inside the liver lobule with a prolonged increase in the level of transaminases.
Recovery is recorded in 5-30% of patients, the rest have a transition to chronic active hepatitis or chronic persistent hepatitis.
The concept of "chronic lobular hepatitis" occurs when the pathological process persists for more than 6 months. Modern classification chronic hepatitis designates it as chronic hepatitis with minimal morphological and laboratory activity of the process.
3. Chronic persistent hepatitis, not elsewhere classified(K73.0).
Chronic persistent hepatitis (CPH) is a long-term (more than 6 months) benign diffuse inflammatory process with preservation of the structure of the liver lobule.
Typically, the absence of pronounced clinical signs of the disease. Only about 30% of patients report general malaise and weakness. The liver is slightly enlarged (by 1-2 cm). Liver "signs" are absent.
Pathomorphological characteristics of CPH: mononuclear, mainly lymphocytic, infiltrates of the portal tracts with moderate dystrophic changes and mild necrosis of hepatocytes (or its absence). Mild morphological changes may persist for several years.
Biochemical study of the blood of patients with CPH (changes indicate a violation of liver function, but are less pronounced than in CAH):
- ALT and AST increased by 2-3 times;
- bilirubin is slightly elevated (about 1/4 of patients with CPH);
- a slight increase in the level of GGTP and LDH is possible;
- other biochemical parameters remain within the normal range.
The modern classification of chronic hepatitis refers to chronic hepatitis as chronic hepatitis with minimal process activity or mild.
Complications
- cirrhosis of the liver Cirrhosis of the liver is a chronic progressive disease characterized by dystrophy and necrosis of the hepatic parenchyma, accompanied by its nodular regeneration, diffuse proliferation of connective tissue and a deep restructuring of the liver architectonics.
;
- chronic liver failure;
- coagulopathy Coagulopathy - a violation of the function of the blood coagulation system
;
- hepatorenal syndrome Hepatorenal syndrome is a pathological condition that sometimes manifests itself in severe liver damage and manifests itself secondary violation kidney function up to severe kidney failure. The development of acute liver and kidney failure is manifested by a combination of jaundice, bleeding disorders, signs of hypoproteinemia and uremia
;
- hepatocellular carcinoma Hepatocellular carcinoma is the most common liver tumor. The result of malignant degeneration of hepatocytes. Main risk factors - chronic viral hepatitis, regular consumption of hepatocarcinogens, cirrhosis of the liver caused by other causes
.
Treatment abroad
Under the toxic damage to the liver understand the pathological structural changes in tissue (reversible and irreversible) under the influence of damaging chemicals. The ICD 10 code for toxic hepatitis is K71.
Etiology
The causes of chronic hepatitis are: drugs, alcohol, household, vegetable and industrial poisons.

Pathogenesis
One of the functions of the liver is a barrier. It neutralizes the poisonous chemical, turning it into an inactive form.
- When a hepatotoxic substance enters the body, active metabolites are formed in the liver, which can have a direct toxic effect on the cell or an immune-mediated one (determined by the mechanism of hypersensitivity). Both of these processes cause cytolysis, necrosis of the hepatocyte. Acute or chronic hepatitis develops.
- Also, drugs and their metabolites can reduce mitochondrial oxidation in the cell and transfer the metabolism in it to the anaerobic pathway. The synthesis of low-density lipoproteins is disrupted, and triglycerides accumulate in the hepatocyte. The patient develops fatty degeneration of the liver. A large number of fatty inclusions in the cell leads to its steatonecrosis.
- The functions of enzymes and transport proteins in the cell can also be disrupted without damage to the hepatocyte itself, hyperbilirubinemia and an increase in gamma-glutamyl transferase occur. Other liver function tests do not change.
- Blockade of transport enzymes, damage to hepatocytes cause cholestasis, impaired synthesis or transport of bile. Bile is formed in the hepatocyte from bilirubin, cholesterol. Then it enters the bile duct. Intrahepatic cholestasis is intralobular and extralobular. There is also extrahepatic cholestasis, characterized by obstruction of bile flow in the extrahepatic bile ducts.
Thus, a toxic substance can cause acute liver damage with massive death of hepatocytes and chronic damage with repeated administration of small doses of a poisonous substance.
- With necrosis of hepatocytes without the occurrence of autoimmune processes and cholestasis, AST and ALT will be increased.
- If hepatocellular cholestasis joins, then there is a rise to 2 norms of alkaline phosphatase, ALT, AST, GGTP.
- With ductular cholestasis with cell necrosis, the picture is the same, but ALP increases by more than 2 norms.
- In autoimmune processes, an increase in immunoglobulins by more than 1.5 times is added.
Clinic
If liver toxicity has occurred, symptoms can develop both acutely and slowly (chronically). The patient complains of pain and heaviness in the right hypochondrium, nausea, lack of appetite, weakness. There may be itching of the skin, loose stools, bleeding. The patient is retarded. On examination, the skin and sclera are icteric. With cholestasis, the color of the urine darkens, the feces become light. There is an enlargement of the liver and spleen. Possible ascites, fever. Symptoms of toxic hepatitis and treatment depend on the activity of the inflammatory process.

Diagnostics
If toxic hepatitis is suspected, the diagnosis is made on the basis of clinical, anamnestic, laboratory, and instrumental data. A general blood and urine test, a biochemical analysis are prescribed: liver tests, protein levels, coagulation system, lipidogram are examined. An analysis for immunoglobulins, ultrasound of organs is also prescribed. abdominal cavity, endoscopy, MRI, liver biopsy.
Treatment
The main drugs used to treat liver damage include:

Assignment Algorithm
So what is toxic hepatitis? Symptoms and treatment what are it? Let's add some clarifications. According to toxic hepatitis, if GGTP, alkaline phosphatase are elevated (there is cholestasis), and AST and ALT are normal or rise no higher than two norms, then UDCA is prescribed at a dose of 15 mg per kg (750 - 1000 mg per day for two doses) for three months and longer. If more than two norms (3 - 5), then 400 - 800 mg daily is added for 10 - 15 days.
With a normal level of alkaline phosphatase (no cholestasis) and an increase in ALT and AST to 5 norms, UDCA 10 mg per kg is prescribed. Appointed for 2-3 months "Essentiale", "Berlition" depending on the causes of the disease.
If AST, ALT, bilirubin is more than 5 norms, then glucocorticoids are added. "Prednisolone" is prescribed intravenously up to 300 mg per day for up to 5 days, with subsequent transfer to tablets and a gradual decrease in dose. UDCA and "Heptral" are prescribed according to the scheme above (where alkaline phosphatase is increased). Plus vitamins B1, B12, B6, PP are needed.
GILBERT SYNDROME
ICD-10 code
E80.4. Gilbert's syndrome.
Gilbert's syndrome is a pigmentary hepatosis (simple familial cholemia, constitutional hyperbilirubinemia, idiopathic unconjugated hyperbilirubinemia, non-hemolytic familial jaundice) with an autosomal dominant type of inheritance, characterized by a moderate intermittent increase in the content of unbound (indirect) bilirubin in the blood. The syndrome was first described by French doctors A.N. Gilbert and P. Lereboullet in 1901
This is the most common form of hereditary pigmentary hepatosis, which is detected in 2-5% of the population. Among Caucasians, the prevalence of the syndrome is 2-5%, among Mongoloids - 3%, among Negroids - 36%. The disease manifests itself in adolescence and lasts almost throughout life. It occurs more often in males.
Etiology and pathogenesis
The syndrome is caused by a mutation in the gene UGT1A1, which codes for the enzyme uridine diphosphate glucuronyl transferase (UDPGT). The following links lie in the pathogenesis of the syndrome:
Violation of the capture of bilirubin by microsomes of the vascular pole of hepatocytes;
Violation of bilirubin transport with the help of glutathione-8-transferase, which delivers unconjugated bilirubin to hepatocyte microsomes;
Inferiority of the microsomal enzyme UDFGT, with the help of which conjugation of bilirubin with glucuronic and other acids is carried out.
In Gilbert's syndrome, the activity of UDPHT decreases only by 10-30% compared with the norm, the main importance is attached to the violation of the uptake of bilirubin by hepatocytes, which is associated with an anomaly in membrane permeability and a defect in the intracellular transport protein.
Bilirubin exchange consists of its transport in the blood plasma, capture by the liver, conjugation, biliary excretion (Fig. 6-1).
Approximately 250-300 mg of unconjugated bilirubin is produced daily in the human body: 70-80% of this amount is the result of the daily breakdown of erythrocyte hemoglobin; 20-30% is formed from heme proteins in the bone marrow or liver. In a healthy person, about 1% of circulating erythrocytes breaks down per day.
Bilirubin, which was formed in reticuloendothelial cells, is a toxic compound. It is called unconjugated, indirect, or free, unbound bilirubin (due to the specifics of the reaction in its determination), and is water insoluble. That is why it is present in the blood plasma in the form of a compound with albumin. The albumin-bilirubin complex prevents the entry of bilirubin through the glomerular membrane into the urine.
With the blood flow, indirect bilirubin enters the liver, where this form of bilirubin is converted into a less toxic form - direct (bound, conjugated) bilirubin. Both fractions make up total bilirubin.
In the liver, unconjugated bilirubin is separated from albumin at the level of hepato-microvilli.

Rice. 6-1. Exchange and conjugation of bilirubin
cytes, its capture by intrahepatic protein. The conjugation of bilirubin with the formation of mono- and diglucuronides (conjugated bilirubin) is provided by UDFGT.
The release of bilirubin into bile is the final stage of pigment metabolism and occurs through the cytoplasmic membranes of hepatocytes.
In bile, conjugated bilirubin forms a macromolecular complex with cholesterol, phospholipids, and bile salts. Further, with bile, it enters the duodenum and small intestine, where it is transformed into urobilinogen, part of which is absorbed through the intestinal wall, enters the portal vein and is transferred with the blood stream to the liver (enterohepatic circulation), where it is completely destroyed.
The main amount of urobilinogen from small intestine enters the large intestine, where, under the action of bacteria, it turns into stercobilinogen and is excreted in the feces. The amount of fecal stercobilinogen and stercobilin varies from 47 to 276 mg/day depending on body weight and sex.
Less than 2% of bilirubin is excreted in the urine as urobilin.
Clinical picture
Mild jaundice, including icterus of the sclera, is the main symptom of the disease. In some cases, staining of the skin occurs (Fig. 6-2, a), especially the feet, palms, nasolabial triangle, armpits.

Rice. 6-2. Gilbert's syndrome: a - the patient is a participant in a beauty contest; b - ultrasound: no changes; c - macropreparation of the liver with the accumulation of lipofuscin
Patients should be viewed in daylight. Under electric lighting, skin color is distorted and can be misinterpreted.
The yellowness of the skin and visible mucous membranes becomes clearly visible when the level of bilirubin in the blood serum reaches 43-50 µmol / l and above.
Jaundice and hyperbilirubinemia are intermittent, so these symptoms are rarely permanent. Stress (for example, during exams or with great physical exertion caused by lifting weights) contributes to the appearance of jaundice and increased scleral icterus. Exacerbates symptoms various operations, colds, improper diet, fasting, drinking alcohol and some types of medicines. Total bilirubin in Gilbert's syndrome ranges from 21 to 51 µmol/l and periodically rises to 85-140 µmol/l.
In half of the cases, dyspeptic complaints are observed: flatulence, stool disorders, nausea, belching, lack of appetite. The occurrence of jaundice may be accompanied by discomfort in the liver and weakness.
The syndrome is associated with connective tissue dysplasia (especially common in the type of Marfan and Ehlers-Danlos syndromes).
Diagnostics
Diagnosis of the disease involves testing.
Serum bilirubin test, which increases with fasting. The patient receives food for 2 days, energy value which does not exceed 400 kcal / day. The level of bilirubin in blood serum is determined on an empty stomach and after 48 hours. The test is positive if its rise is
50-100%.
Test with phenobarbital- the level of bilirubin decreases while taking phenobarbital due to the induction of conjugated liver enzymes.
Test with nicotinic acid- intravenous administration of the drug causes an increase in the level of bilirubin due to a decrease in the osmotic resistance of erythrocytes.
The result of a stool test for stercobilin is usually negative.
Liver tests, in particular the levels of AST, ALT, alkaline phosphatase, etc., are usually within the normal range or slightly elevated. There may be an increase in total protein and dysproteinemia; prothrombin time - within the normal range. Markers of hepatitis B, C, D viruses are absent.
Molecular diagnostics includes DNA analysis of the UDFGT gene.
With the help of ultrasound of the abdominal organs, the size and condition of the liver parenchyma are determined (Fig. 6-2, b); size, shape, wall thickness, possible stones in the gallbladder and bile ducts.
If there are indications to exclude chronic hepatitis (CH), liver cirrhosis, a percutaneous puncture biopsy of the liver is performed with a morphological assessment of the biopsy.
Pathomorphology
Morphological changes in the liver are characterized by fatty degeneration of hepatocytes and the accumulation of a yellowish-brown lipofuscin pigment in them, more often in the center of the lobules along the bile capillaries (Fig. 6-2, c).
Differential Diagnosis
Differential diagnosis is carried out with all types of hyperbilirubinemia (Table 6-1), hemolytic anemia, congenital cirrhosis of the liver and hepatitis, atresia of the bile ducts or small intestine, etc.
Table 6-1. Differential diagnosis of hereditary hepatosis

Treatment
Patients in special treatment, as a rule, do not need, since Gilbert's syndrome is not a disease, but an individual, genetically determined feature of the organism. The main importance is the observance of the regime of study, work, rest, nutrition.
Highly undesirable alcoholic drinks and fatty foods, physical overload (professional sports), insolation, long breaks between meals, fluid restriction are not recommended.
Components of therapy and prevention of exacerbations of Gilbert's syndrome:
Diet therapy;
Exclusion of provoking factors (infections, physical and mental stress, the use of hepatotoxic drugs and alcohol);

Sun exposure contraindication.
An episode of jaundice may resolve on its own without treatment. medicines.
If the level of bilirubin reaches 50 μmol / l and is accompanied by poor health, it is possible to take phenobarbital in a short course (1.5-2.0 mg / kg, or 30-200 mg / day in 2 doses for 2-4 weeks). Phenobarbital (luminal *) is part of drugs such as Corvalol *, Barboval *, Valocordin *, so sometimes they prefer to use these drugs (20-30-40 drops 3 times a day for 1 week),
although the effect of such treatment is observed only in a small proportion of patients. Inducers of enzymes of the monooxidase system of hepatocytes, in addition to phenobarbital, include zixorin (flumecinol *), prescribed to adolescents at a dose of 0.4-0.6 g (4-6 capsules) 1 time per week or 0.1 g 3 times a day for 2-4 weeks. Under the influence of these drugs, the level of bilirubin in the blood decreases, dyspeptic symptoms disappear, but in the course of treatment, lethargy, drowsiness, and ataxia occur. In such cases, these drugs are prescribed in minimal doses at bedtime, which allows them to be taken for a long time.
Due to the fact that a significant proportion of patients develop cholecystitis and cholelithiasis, it is recommended to take infusions choleretic herbs, periodic tubage from sorbitol (xylitol), Karlovy Vary salt, etc. Hepatoprotectors are shown: ursodeoxycholic acid preparations (ursosan *, ursofalk *), phospholipids (Essentiale *), silibinin (karsil *), milk thistle fruit extract (legalon 70 *), field artichoke leaf extract (chofitol *), liv 52 *; choleretics: cholagol *, cholenzim *, allochol *, berberine *, holosas *; vitamin therapy, especially B vitamins.

Removal of conjugated bilirubin is possible with the help of increased diuresis, the use of activated carbon that adsorbs bilirubin in the intestine.
Thermal physiotherapy on the liver area is contraindicated.
Through phototherapy, the destruction of bilirubin fixed in tissues is achieved, thereby releasing peripheral receptors that can bind new portions of bilirubin, preventing its penetration through the blood-brain barrier.
Prevention
Prevention includes compliance with the regime of work, nutrition, rest. Significant physical exertion, fluid restriction, fasting and hyperinsolation should be avoided. The use of alcoholic beverages, hepatotoxic drugs is unacceptable.
Gilbert's syndrome is not a reason to refuse vaccinations.
Sanitation of chronic foci of infection and treatment of the existing pathology of the biliary tract are mandatory.
Forecast
The prognosis is favorable. Hyperbilirubinemia persists for life, but is not accompanied by progressive changes in the liver and increased mortality. When insuring life, such people are referred to the group of ordinary risk. During treatment with phenobarbital, the level of bilirubin decreases to normal values. Perhaps the development of inflammation in the biliary tract, cholelithiasis, psychosomatic disorders.
Parents of children with this syndrome should consult a geneticist before planning another pregnancy.
The same should be done if relatives of a couple planning to have children are diagnosed with this syndrome.
FATTY LIVER
ICD-10 code
K76.0. Fatty degeneration of the liver.
Hepatosis (liver steatosis, non-alcoholic steatohepatitis) is a group of liver diseases, which are based on metabolic disorders in hepatocytes and the development of dystrophic changes in liver cells, while inflammation is absent or mild.
IN last years observed a significant increase in the incidence of fatty liver, mainly associated with an increase in the prevalence of obesity. Among patients who underwent liver biopsy, approximately 7-9% of cases of hepatosis in Western countries and 1-2% in Japan are detected.
Etiology and pathogenesis
The cause of the disease is obesity, diabetes, dyslipidemia, fast weight loss, lack of protein in the diet, congenital defects in β-oxidation of fatty acids, deficiency of α-1-antitrypsin, exposure to toxic substances for the liver, including alcohol, etc. Hepatosis can be both an independent disease and a manifestation of other diseases.
Excess accumulation of fat in the liver tissue (in hepatocytes and Ito cells) may result from first impact(Fig. 6-3, a, d) - saturated with lipids, simple carbohydrates and high calorie content of food:
Increasing the flow of free fatty acids to the liver;
Decrease in the rate of β-oxidation of free fatty acids in liver mitochondria;
Increasing the synthesis of fatty acids in the mitochondria of the liver;
Decrease in the synthesis or secretion of very low density lipoproteins and the export of triglycerides in their composition.
The result of a violation of the diet are insulin resistance and fatty liver.
Second impact(see Fig. 6-3, d) implies a violation of the excretion of lipids from the liver, which occurs with a decrease in the amount of substances involved in their processing (protein, lipotropic factors). The formation of phospholipids, β-lipoproteins, lecithin from fats is disrupted. Tumor necrosis factor-α, endotoxin, and immune factors are important in pathogenesis. It is assumed that, regardless of the causes of steatosis, inflammatory-necrotic changes in the liver are based on universal mechanisms. Being highly reactive compounds, free fatty acids serve as a substrate for lipid peroxidation. The formed free radicals cause the destruction of lipid, protein components of membranes, liver receptors, etc., causing further changes in the liver.
Classification
Distinguish between pigment and fatty hepatosis. Most often, the term "hepatosis" means fatty hepatosis (steatosis), since pigmentary hepatoses are much less common and are considered separately (see "Rare syndromes"), with the exception of Gilbert's syndrome.
Clinical picture and diagnosis
In the early stages, symptoms are minimal. As a rule, the course of the disease is latent, only an increase in the activity of hepatic transaminases and hepatomegaly are noted. In many patients, liver dysfunction is detected incidentally during examination for other diseases. There is a minimal or moderately pronounced activity of inflammation in the liver, detected by biochemical studies of blood serum. However, without treatment, a transition to cirrhosis of the liver can be observed, the phenomena of liver failure gradually increase.
Fatty hepatosis is often concluded by ultrasound diagnostic doctors based on characteristic features: a uniform increase in the liver, a diffuse increase in its echogenicity (sometimes pronounced) while maintaining its homogeneity, although with the progression of the process, a characteristic granularity of the parenchyma appears, indicating the onset of the development of steatohepatitis and hepatitis (Fig. 6-3, b).
Pathomorphology
According to morphological studies, steatohepatitis is an excessive accumulation of triglycerides in the liver, which is accompanied by damage to cell membranes and other hepatocyte organelles, an inflammatory process, fibrosis up to liver cirrhosis (Fig. 6-3, c).

Rice. 6-3. Functions and diseases of the liver: a - participation of the liver in lipid metabolism; b - ultrasound: hepatomegaly and increased echogenicity of the liver; c - macropreparation: liver steatosis; d - staging of liver pathology formation
Treatment
Diet therapy is permanent and safe method treatment of fatty liver disease.

In order to normalize the oxidation of fatty acids in mitochondria, improve the transport of triglycerides from the liver, reduce the processes of lipid peroxidation, drugs that improve lipid metabolism are prescribed - hepatoprotectors, vitamin B 12, folic acid, thioctic acid ( lipoic acid*) etc.
Prevention
The basis of primary prevention is a healthy lifestyle and healthy eating(Fig. 6-4). Sufficient physical activity is recommended.

Rice. 6-4. Nutrition pyramid for fatty liver
Dispensary observation is described below (see "Prevention of chronic hepatitis").
Forecast
With the exclusion of causative factors and timely treatment recovery is possible, however, hepatosis can be transformed into chronic hepatitis and cirrhosis (see Fig. 6-3, d).
CHRONIC HEPATITIS
ICD-10 code
K73. chronic hepatitis.
Chronic hepatitis is a group of diseases accompanied by the development of a diffuse inflammatory process in the liver that lasts more than 6 months, confirmed by biochemical parameters, the results of a morphological study of the liver, as well as specific markers in the blood serum.
The prevalence of CG has not been accurately established due to the large number of erased and asymptomatic forms, and the lack of population studies. Most often, chronic viral hepatitis (CVH), caused by the persistence of hepatitis B (29.2%), C (33.3%), chronic hepatitis B + C (16.7%), less often B + D (4.1%), D + G (no more than 2%) is detected. In 16.7% of cases, hepatitis of unknown etiology is detected.
Classification
The modern classification of hepatitis is presented in Table. 6-2. Taking into account the etiology, the following types of hepatitis are distinguished.
. Specific viral hepatitis. The main forms of such hepatitis are hepatitis A, B and C. Hepatitis D is less common in the world. Hepatitis E remains a major problem in developing countries. Other hepatitis viruses (G, TTV, etc.) have also been described, but their clinical significance is low.
. Nonspecific viral hepatitis are caused by a group of viruses that can affect both the liver and other organs. For example, a virus infectious mononucleosis(Epstein-Barr virus) selectively affects the cells of the reticuloendothelial system (clinically manifests itself in the form of tonsillitis, hypersplenism, hepatitis, etc.). Adenovirus causes pharyngoconjunctival fever, acute pneumonia, hepatitis. Herpes simplex virus is an AIDS-defining infection.
Hepatitis - manifestation of an etiologically independent disease(with leptospirosis, pseudotuberculosis).
Hepatitis associated with the use of drugs - toxic-allergic And medicinal hepatitis. Alcoholic hepatitis is a combined lesion with acetaldehyde and some other factor.
. Nonspecific reactive hepatitis- the reaction of liver cells to the pathology of neighboring organs: pancreas, gallbladder, duodenum. Reactive hepatitis develops in patients with chronic pancreatitis, duodenal ulcer.
Among autoimmune forms of chronic hepatitis 3 types of diseases have been identified (see Table 6-2).
Row rare liver disease may have clinical and histological features of chronic persistent hepatitis:
Primary biliary cirrhosis;
Wilson-Konovalov disease;
Primary sclerosing cholangitis;
Deficiency of α-1-antitrypsin.
The stage of fibrosis is established on the basis of a pathomorphological study of liver biopsy specimens (Table 6-3), approximately according to ultrasound data (Table 6-4).
Table 6-2. Classification of Chronic Hepatitis (International Expert Group, Los Angeles, 1994)

* It is determined based on the results of a histological examination of the liver tissue and approximately - according to the degree of ALT and AST activity (1.5-2 norms - minimal, 2-5 norms - low, 5-10 norms - moderate, above 10 norms - pronounced). ** Established on the basis of a morphological study of the liver and approximately - according to ultrasound.
Table 6-3. Hepatitis histological activity index in points (Knodell R.. J. et al., 1994)

Note: 1-3 points - the minimum degree of activity of chronic hepatitis; 4-8 - chronic hepatitis of moderate severity; 9-12 points - moderate chronic hepatitis; 13-18 points - severe chronic hepatitis.
Table 6-4. Ultrasound criteria for the stages of liver fibrosis in chronic hepatitis in children

Mixed hepatitis is established as the main diagnosis in the presence of simultaneous replication of 2 types of virus or more. With the replication of one and the integration of the other, the main hepatitis and concomitant hepatitis are established.
Chronic viral hepatitis
ICD-10 codes
B18. Chronic viral hepatitis.
818.0. Viral hepatitis B chronic with D-agent.
818.1. Viral hepatitis B chronic without D-agent.
818.2. Viral hepatitis C is chronic.
818.8. Viral hepatitis chronic others.
818.9. Viral hepatitis, chronic, unspecified. More than 70% of cases of CG are caused by hepatotropic viruses B, C and D. Worldwide, there are 350-400 million people infected with the hepatitis B virus, and about 1 million people die every year from hepatitis B virus (HBV) infection-related diseases. The prevalence of HBV infection in different countries ranges from 0.1 to 20%. The risk of transition from acute HBV infection to chronic decreases with age: with perinatal infection, it reaches 90%, with infection at the age of 1-5 years - 25-35%, and with adult infection - less than 10%.
Etiology and pathogenesis
The mechanism of formation, diagnosis of hepatitis B and C are shown in fig. 6-5. Viral hepatitis B (8 main genotypes - A-H) is found in blood and other biological fluids (semen, saliva, nasopharyngeal mucus), transmitted in four main ways:
sexual;
Perinatal (from mother to child in the prenatal period and in childbirth);
Parenteral (through the blood);
Horizontal (with close household contact or through infected common items; mainly observed in early childhood).
In children, the main route of transmission of viral hepatitis B is perinatal. If a pregnant woman is a carrier of viral hepatitis B (and, in addition, HBeAg-positive), the probability of infection of a newborn with the development of a carriage of the virus is 90%. As adults, 25% of these children die of chronic liver failure or liver cancer. Although HBsAg, HBeAg, and HBV DNA are found in breast milk, type of feeding on the risk of transmission of viral hepatitis B does not affect. Other risk factors for hepatitis B infection include:
Transfusion of blood and/or its components;
Injection drugs, tattoos, piercings and other invasive skin procedures;
Unprotected penetrative sex, especially anal and vaginal intercourse;
Organ transplantation;
Work in medical institutions;
Hemodialysis.
In regions with low endemicity of HBV infection, the highest incidence occurs in adolescents and young people. The most common routes of transmission of viral hepatitis B in these groups are sexual and parenteral (with unsafe drug injections, in particular, the reuse of disposable syringes).
It is believed that chronic hepatitis B(CHB) - initially chronic or arising after an erased or subclinical form acute infection disease.
Phases of CHB:
Initial, or immune tolerance;
Immune response (replicative), occurring with pronounced clinical and laboratory activity;
Integrative;
Carriage of HBsAg.
Hepatitis B DNA virus (HBV DNA) itself does not cause cytolysis. Damage to hepatocytes is associated with immune responses that occur in response to circulating viral and hepatic antigens. In the 2nd phase of virus replication, virus antigens are expressed: HBsAg (surface), HBcAg (nuclear), HBeAg (Fig. 6-5, a), the immune response is more pronounced, which causes massive necrosis of the liver parenchyma and further virus mutation.
Replication of the hepatitis B virus is also possible outside the liver - in cells bone marrow, mononuclear cells, thyroid and salivary glands, which causes extrahepatic manifestations of the disease.
Transmission routes chronic hepatitis C(CHC) are similar to those in CHB. Unlike viral hepatitis B, hepatitis C RNA virus has a direct hepatotoxic effect. As a result, viral replication and persistence in the body are associated with hepatitis activity and progression. Interestingly, viral hepatitis C is able to block apoptosis (programmed death) of cells affected by it in order to stay in the human body for a long time. Apoptosis is a normal process that rids the body of "worn out" or diseased cells. The protein encoded in the genome of viral hepatitis C, known as NS5A, blocks the opening of potassium channels in liver cells, protecting their “shelters” from natural death and thus lingering in the human body for a long time. The life cycle of viral hepatitis C is shown in Fig. 6-5, b.

Rice. 6-5. Chronic hepatitis C and B: a - diagnosis of hepatitis C and B and dynamics of serological markers of hepatitis B; b - life cycle hepatitis C virus
Pathogen chronic hepatitis D(HGO) - an RNA-containing particle, the outer shell of which is represented by HBsAg. In the center of the particle is the antigen of the hepatitis D virus. The delta virus is able to multiply in the liver cells only in the presence of viral hepatitis B, since its proteins are used to exit the cell of the delta virus particle. The disease proceeds simultaneously with viral hepatitis B by the type of co-or superinfection.
Clinical picture
The clinical picture of chronic hepatitis is mild and nonspecific. Asymptomatic course is observed in 25% of patients. The formation of chronic hepatitis occurs more often in the outcome of acute hepatitis, which occurs in the form of atypical (erased, anicteric, subclinical) forms and extremely rarely in manifest (icteric) forms of acute hepatitis. The acute phase of hepatitis and the appearance clinical symptoms the chronic form of the disease is separated by 5 years or more.
Clinical manifestations of CG depend on the age of the child at the time of infection, the severity of morphological
changes in the liver, phases of the infectious process (replication, integration), premorbid background. Children, unlike adults, cholestatic variant CG is rare; in the presence of cholestasis, it is necessary to exclude congenital pathology of intrahepatic or extrahepatic passages, deficiency of α-1-antitrypsin, cystic fibrosis. The main syndromes of the disease are given in table. 6-5.
Table 6-5. The main syndromes of chronic viral hepatitis

extrahepatic manifestations, associated with extrahepatic replication of the virus, are more characteristic of CHC, can manifest as recurrent dermatitis, hemorrhagic vasculitis, glomerulonephritis, arthropathy, thyroiditis, Sjögren's syndrome, pancreatopathies. Extrahepatic manifestations often develop at puberty, girls are characterized by the development of endocrine disorders, boys develop glomerulonephritis and other diseases.
Extrahepatic manifestations include vascular changes (Table 6-6; Fig. 6-6). In children, they are much less common, their presence requires an extended study of liver function.
Table 6-6. Vascular extrahepatic manifestations in chronic hepatitis


Rice. 6-6. Vascular extrahepatic manifestations in chronic hepatitis: a - telangiectasia; b - capillaritis; c - palmar erythema
Diagnostics
specific methods. Using enzyme-linked immunosorbent assay (ELISA), the main markers of CG are detected, using polymerase chain reaction(PCR) - DNA or RNA virus (Table 6-7; Fig. 6-5, a).
Table 6-7. Marker diagnosis of chronic hepatitis B and C

Serological markers viral hepatitis B is used to establish the diagnosis and stage of the disease.
Antigens were presented above (see Fig. 6-5, a). Antibodies to the surface antigen of the virus (anti-HBsAg) appear in the blood after 3-6 months and persist for many years or possibly a lifetime. Their detection indicates either a previous infection or a previous vaccination.
The nuclear antigen (HBcAg) usually does not circulate in the blood, but antibodies to it appear on early stages diseases, their titer quickly reaches a maximum, and then gradually decreases (but does not completely disappear). First, antibodies of the IgM class (anti-HBcAg IgM) appear, then IgG appear. Antigen E (HBeAg) appears in the blood for a short time at the onset of the disease, which is accompanied by the production of antibodies to it (anti-HBe).

Chronic CHB infection is characterized by the presence of HBsAg and anti-HBcAg IgG in the blood.
With CHC, in addition to viremia (HCV RNA), antibodies of the IgM and IgG classes are detected. Outside of an exacerbation, CHC RNA and anti-HCV IgM are not detected, but IgG class antibodies remain (see Tables 6-7).
TO non-specific methods include biochemical, immunological tests and instrumental studies.
Biochemical tests do not carry information about the etiology of the disease, but reflect the nature of liver damage and the state of its function. These include:
An increase in the level of liver enzymes: with chronic hepatitis, an increase in ALT is more pronounced than AST, which is associated with different localization of enzymes (ALT - in the cytoplasm, AST - in mitochondria), in cirrhosis, on the contrary, AST activity predominates over that of ALT; also characterized by an increase in such enzymes as lactate dehydrogenase, γ-glutamyl transpeptidase,
AP;
Violation of fat and pigment metabolism: an increase in the direct fraction of bilirubin, total cholesterol, β-lipoproteins, alkaline phosphatase activity, 5-nucleotidase;
Violation of the protein-synthetic function of the liver: a decrease in total protein, an increase in thymol test, a decrease in sublimate test, a decrease in the level of prothrombin, persistent dysproteinemia due to an increase in globulin fractions, especially γ-globulins, and a decrease in albumin.
Biochemical syndromes reflecting liver dysfunction are presented in Chapter 1 (see Tables 1-8, changes in protein fractions - Fig. 1-16, b).
immunological tests. Characterized by a decrease in the levels of T-suppressors, an increase in the levels of serum immunoglobulins.
Instrumental methods. Ultrasound of the liver is a mandatory research method for chronic hepatitis, since it allows you to visualize the liver, determine its size, identify liver cirrhosis and portal hypertension. Even with asymptomatic course of the disease with the help of this method it is possible to reveal an increase in the liver, a change in the echogenicity of the parenchyma. Rheohepatography, puncture liver biopsy can be used.
To date liver biopsy is the gold standard for diagnosing liver diseases (Fig. 6-7, a). During a biopsy, a piece of the liver with a diameter of about 1 mm is obtained using a special needle. The procedure is carried out under local or general anesthesia and under ultrasound control, since it is necessary to control the course of the needle, which makes the manipulation safe.
The degree of CG activity is most often assessed using a semi-quantitative histological activity index, also known as the Knodell system, defined in points (see Tables 6-3). Histology of the biopsy (tissue sample) of the liver allows you to decide on the need and tactics of antiviral therapy.
Pathomorphology
Morphological examination of liver biopsy specimens already in the first months of life of a child with primary CG reveals signs of inflammation that persist for many years, as well as progressive fibrosis with the formation of liver cirrhosis.

Rice. 6-7. Diagnosis of chronic hepatitis: a - biopsy technique; histological picture: b - CHB (staining with hematoxylineosin; χ 400); c - CHC (x 400).
CHB is characterized by necrosis (Fig. 6-7, b); a pathognomonic sign in CHC is vacuolization of the nuclei of hepatocytes, the so-called opaque vitreous hepatocytes, as well as their stepwise necrosis (Fig. 6-7, c).
Differential Diagnosis
Treatment
IN replication phase (exacerbation) showing hospitalization in specialized department, bed rest, strict diet therapy.

Basic therapy includes appointment antiviral drugs. Indications for its appointment:
The presence of markers of active hepatitis replication;
The level of ALT is more than 2-3 times higher than normal;
Absence of cholestasis and signs of liver cirrhosis with decompensation;
Absence of severe concomitant diseases in the stage of decompensation;
Absence of autoimmune diseases, immunodeficiency, mixed hepatitis.
Interferon inducers characterized by low toxicity and the absence of side effects, unlike interferon preparations, thanks to their use, it is possible to significantly increase life expectancy in children and adults (Fig. 6-8).

Rice. 6-8. Chronic hepatitis (course and treatment): a - antiviral treatment of children and adults with chronic viral hepatitis B and C and years of life gained; b - natural course of hepatitis B
Interferon preparations contraindicated in psychosis, epidemic syndrome, severe neutro- and thrombocytopenia, autoimmune diseases (AIH, thyroiditis, etc.), decompensated liver cirrhosis and kidney disease, heart pathology in the decompensation stage.
Interferon-a-2b (reaferon*, roferon*, neuroferon*) - a lyophilisate for oral suspension - is prescribed 30 minutes before a meal, 1-2 ml of chilled water is added to the contents of the vial before use. boiled water. The drug is administered in injections for CHB at a dose of 5 million IU / m 2, for CHC - 3 million IU / m 2 of body surface area three times a week (1 time with an interval of 72 hours) s / c or / m. The calculated dose of interferon is initially administered for 3 months. After this period, a control study is carried out (RNA or DNA of the virus, activity). If there is no clear positive dynamics of these indicators (the disappearance of RNA, virus DNA from the blood, a decrease in ALT), it is better to stop treatment according to this scheme or switch to combination therapy. But if there is a decrease in ALT activity, a drop in the concentration of RNA, DNA of the virus in the blood, treatment according to the selected scheme is continued for another 3 months, followed by a control
laboratory research. With positive dynamics in CHC, treatment is still continued for 3 months to consolidate the results of treatment. Thus, the course of treatment for CHB is 6 months, for CHC - 9-12 months.
In pediatric practice, viferon is used (a combination of α-interferon with membrane stabilizers), which is available in rectal suppositories. Doses for children: up to 3 years - 1 million IU, over 3 years - 2 million IU 2 times a day with an interval of 12 hours 3 times a week. In patients treated according to the protocol program using viferon, the effectiveness of treatment is assessed according to the above principles. If there is no positive effect in this category of patients during a control study 3 months after the start of therapy, then viferon can be replaced with reaferon*, roferon*.
The α-interferon inducer meglumine acridone acetate (cycloferon*) is administered for chronic hepatitis at 6-10 mg/kg per day, 10 injections daily, then 3 times a week for 3 months as a complex therapy.
The antiviral drug tilorone (amiksin) is prescribed to children over 7 years old in tablets of 0.125 orally after meals, the first 2 days daily, then 125 mg every other day - 20 tablets, then 125 mg once a week for 10-20 weeks. The course of treatment for CHA is 2-3 weeks, for CHB - 3-4 weeks.
In CHB against the background of virus replication, the antiviral chemotherapy drug lamivudine (Zeffix, Epivir*) is recommended in oral solution and tablets. It is dosed at 3 mg / kg per day for children from 3 months, but not more than 100 mg orally 1 time per day for a course of 9-12 months. Tablets of 100 mg 1 time per day are prescribed to adolescents (16 years and older) orally, regardless of food intake.
In general, interferon therapy is effective in 40% of patients with CHB and in 35% of patients with CHC, but in 10-30% of patients after the end of treatment, relapses of the disease are possible.


In severe form of CG, prescribe glucocorticoids: prednisolone or methylprednisolone in tablets of 0.001; 0.0025 and 0.005 mg, 1-2 mg / kg per day in 2 divided doses, without taking into account the daily rhythm. After achieving remission, the dose is reduced by 5-10 mg to a maintenance dose of 0.3-0.6 mg/kg per day: 10-15 mg/day of prednisolone or 8-12 mg/day of methylprednisolone.
Criteria for the effectiveness of treatment:
. biochemical - the most informative is the determination of the level of ALT, and during treatment, ALT activity should be determined throughout the course and for another 6 months after withdrawal, and then every 3-6 months for 3 years;
Virological - determination of RNA, DNA of the virus using PCR;
Histological ones are the most informative for evaluating the effectiveness of treatment, but in practice they are not always realizable, especially in pediatrics.
Biochemical remission at the end of treatment involves the normalization of enzyme levels immediately after the end of the course of therapy; complete remission- normalization of AST and ALT levels and the disappearance of RNA, virus DNA immediately after treatment; stable biochemical remission- preservation normal value transaminases 6 months or more after discontinuation of therapy; stable complete remission- maintaining normal levels of AST and ALT and the absence of RNA, DNA of the virus 6 months after treatment.
If a stable complete remission is achieved, it is recommended to continue monitoring the patient for at least 2 years with a frequency of 1 every six months. In the remission phase (integration phase of CVH), antiviral therapy is usually not carried out, the treatment consists of organizing a diet, regimen, connecting probiotics, enzymes, herbal remedies, laxatives according to indications to prevent gastrointestinal dysfunction and intestinal autointoxication.
Accompanying therapy is symptomatic and pathogenetic treatment.
In order to stop cholestasis, ursodeoxycholic acid preparations (ursosan *, urdox *, ursofalk *) are used as monotherapy in the non-replicative phase of hepatitis, in the replicative phase - in combination with interferons up to 6-12 months, 10 mg / kg once a day before bedtime.
Hepatoprotectors that have the ability to protect hepatocytes are prescribed in courses of up to 1.5-2 months. Repeated course - in 3-6 months according to indications.
Artichoke leaf extract (chophytol *) is a herbal remedy that has hepatoprotective and choleretic effects. Hofitol * is prescribed for children over 6 years old, 1-2 tablets or 1/4 tsp. oral solution 3 times a day before meals, adolescents - 2-3 tablets or 0.5-1 tsp. solution 3 times a day, course - 10-20 days. Solution for intramuscular or intravenous slow administration - 100 mg (1 ampoule) for 8-15 days; average doses can be significantly increased, especially in hospital treatment.
Hepatoprotector "Liv 52 *" is a complex of biologically active substances of plant origin; it is prescribed for children over 6 years old, 1-2 tablets 2-3 times a day, for adolescents - 2-3 tablets 2-3 times a day.
Ademetionine (Heptral *) is a hepatoprotector that has choleretic and cholekinetic, as well as some antidepressant effects. Children are prescribed with caution inside, in / m, in / in. In intensive care in
the first 2-3 weeks of treatment - 400-800 mg / day in / in slowly or / m; the powder is dissolved only in the special supplied solvent (L-lysine solution). For maintenance therapy - 800-1600 mg / day inside between meals, without chewing, preferably in the morning.

Prevention
The main preventive measures should be aimed at preventing infection with hepatitis viruses, therefore, early detection of patients with erased forms diseases and their appropriate treatment. Carriers of HBsAg require regular (at least once every 6 months) monitoring of biochemical and virological parameters in order to prevent activation and replication of the virus.
For vaccination against hepatitis B, recombinant vaccines are used: Biovac B *, Engerix B *, Euvax B *, Shanvak-B *, etc. RD for newborns and children under 10 years old - 10 mcg (0.5 ml of suspension), for children over 10 years old - 20 mcg (1 ml of suspension).
For newborns born to mothers who are carriers of hepatitis B, it is recommended to administer hepatitis B immunoglobulin simultaneously with the vaccine, and the drugs should be administered at different sites. In accordance with the rules existing in the Russian Federation, vaccination of this category of children is carried out four times according to the scheme: 0 (on the day of birth) -1 - 2-12 months of life. Against hepatitis B, adolescents aged 11-13 years old must be vaccinated according to the same scheme.
Widely vaccinate medical workers and persons at risk for hepatitis B infection. Vaccination leads to a gradual decrease in the level of infection of the population of the Russian Federation with the hepatitis B virus.
A vaccine against hepatitis C has not yet been developed, and therefore the prevention of hepatitis C is built on the suppression of all possibilities of parenteral (including transfusion) infection.
Clinical supervision is described below.
Forecast
The chance of a complete recovery is low. With chronic hepatitis B, a long-term persistence of the causative virus occurs, possibly a combination with an active pathological process. On average, after 30 years, 30% of patients with chronic active hepatitis B develop cirrhosis of the liver. Within 5 years, approximately one in four patients with hepatitis B cirrhosis will develop liver decompensation, and another 5-10% of patients will develop liver cancer (see Fig. 6-8). Without treatment, approximately 15% of patients with cirrhosis die within 5 years. In 1-1.5% of cases, cirrhosis is formed, and in the remaining 89%, a long-term remission occurs with HBsAg carriage. With ΧΓD, the prognosis is unfavorable: in 20-25% of cases, the process flows into cirrhosis of the liver; release from the pathogen does not occur. CHC flows slowly, gently, without cessation of viremia for many years, with a periodic increase in transaminase activity and with a pronounced tendency to fibrosis. As the process progresses, cirrhosis of the liver and hepatocellular carcinoma develop.
AUTOIMMUNE HEPATITIS
ICD-10 code
K75.4. autoimmune hepatitis.
AIH is a progressive hepatocellular inflammation of the liver of unknown etiology, characterized by the presence of periportal hepatitis, frequent association with other autoimmune diseases, an increase in the concentration of immunoglobulins (hypergammaglobulinemia) and the presence of autoantibodies in the blood.
Like other autoimmune diseases, AIH is more common in females, with an overall incidence of approximately 15-20 cases per 100,000 population. In childhood, the proportion of AIH among chronic hepatitis ranges from 1.2 to 8.6%, observed at the age of 6-10 years. The ratio of girls and boys is 3-7:1.
Etiology and pathogenesis
The pathogenetic mechanism of the development of AIH is based on a congenital defect in HLA membrane receptors. Patients have a defect in the function of T-suppressors linked by the HLA haplotype, resulting in uncontrolled synthesis of IgG class antibodies by B-lymphocytes that destroy the membranes of normal hepatocytes, and pathological immune reactions against their own hepatocytes develop. Often, not only the liver is involved in the process, but also large glands of external and internal secretion, including the pancreas, thyroid, and salivary glands. As the main factor in the pathogenesis of AIH, genetic predisposition (immunoreactivity to self-antigens) is considered, which, however, is not sufficient in itself. It is believed that triggering agents (triggers) are necessary for the implementation of the process, among which viruses (Epstein-Barr, measles, hepatitis A and C) and some drugs (for example, interferon drugs) and adverse environmental factors are considered.

Rice. 6-9. AIH pathogenesis
The pathogenesis of AIH is shown in Fig. 6-9. The effector mechanism of hepatocyte injury seems to be more related to autoantibody response to liver-specific hepatocyte antigens than to direct T-cell cytotoxicity.
Classification
There are currently 3 types of AIH:
- type 1- the classic version, it accounts for 90% of all cases of the disease. Detect antibodies to smooth muscle cells (Smooth Muscle Antibody- SMA) and nuclear antigens (liver-specific
squirrel - Antinuclear Antibodies- ANA) in a titer of more than 1:80 in adolescents and more than 1:20 in children;
-type 2- accounts for about 3-4% of all cases of AIH, most of the patients are children from 2 to 14 years old. Detect antibodies to liver and kidney microsomes (Liver Kidney Microsomes- LKM-1);
-type 3- characterized by the presence of antibodies to soluble liver antigen (Soluble Liver Antigen- SLA) and hepato-pancreatic antigen (LP).
Some features of AIG, taking into account the types, are presented in Table. 6-8.
Table 6-8.Classification and features of types of AIH

Clinical picture
The disease in 50-65% of cases is characterized by the sudden onset of symptoms similar to those of viral hepatitis. In some cases, it begins gradually and is manifested by increased fatigue, anorexia and jaundice. Other symptoms include fever, arthralgia, vitiligo (pigmentation disorder characterized by loss of melanin pigment in patches of skin) and nosebleeds. The liver protrudes from under the edge of the costal arch by 3-5 cm and thickens, there is splenomegaly, the abdomen is enlarged in size (Fig. 6-10, a). As a rule, extrahepatic signs of chronic liver pathology are detected: spider veins, telangiectasias, palmar erythema. Some patients have a Cushingoid appearance: acne, hirsutism and pink striae on the thighs and abdomen; 67% are diagnosed with other autoimmune diseases: Hashimoto's thyroiditis, rheumatoid arthritis and etc.
Diagnostics
Diagnosis is based on the detection of syndromes of cytolysis, cholestasis, hypergammaglobulinemia, an increase in the concentration of IgG, hypoproteinemia, a sharp increase in ESR, and is confirmed by the detection of autoantibodies against hepatocytes.
characteristic hypersplenism syndrome, its signs:
Splenomegaly;
Pancytopenia (decrease in the number of all blood cells): anemia, leukopenia, neutropenia, lymphopenia, thrombocytopenia (with a sharp degree of severity, a bleeding syndrome appears);
Compensatory hyperplasia of the bone marrow.
In diagnostics, instrumental research methods (scanning, liver biopsy, etc.) are of unconditional importance.
Pathomorphology
Morphological changes in the liver in AIH are characteristic but nonspecific. CG, as a rule, turns into multilobular cirrhosis of the liver (Fig. 6-10, b); characteristic high degree activities: periportal
necrosis, porto-portal or centroportal bridging necrosis, less often - portal or lobular hepatitis, predominantly lymphocytic infiltration with a large number of plasma cells, the formation of rosettes (Fig. 6-10, c).

Rice. 6-10. AIH: a - a child with an outcome in liver cirrhosis; b - macropreparation: macronodular cirrhosis; c - micropreparation: histological picture (staining with hematoxylin-eosin; χ 400)
Differential Diagnosis
Differential diagnosis is carried out with CHB, cholecystitis, Wilson-Konovalov disease, drug-induced hepatitis, α-1-antitrypsin deficiency, etc.
Distinguish between definite and probable AIH. The first variant is characterized by the presence of the above indicators, including an increase in autoantibody titers. In addition, there are no viral markers in the blood serum, bile duct damage, copper deposition in the liver tissue, no indications for blood transfusions and the use of hepatotoxic drugs.
The probable variant of AIH is justified when the present symptoms suggest AIH, but are not sufficient to make a diagnosis.
Treatment
The basis is immunosuppressive therapy. Assign prednisolone, azathioprine, or combinations thereof, which allow to achieve clinical, biochemical and histological remission in 65% of patients within 3 years. Treatment is continued for at least 2 years until remission is achieved for all criteria.
Prednisolone is prescribed at a dose of 2 mg/kg ( maximum dose- 60 mg / day) with a gradual decrease by 5-10 mg every 2 weeks under weekly monitoring of biochemical parameters. In the absence of normalization of transaminase levels, azithioprine is additionally prescribed at an initial dose of 0.5 mg/kg (maximum dose is 2 mg/kg).
A year after the onset of remission, it is desirable to cancel immunosuppressive therapy, but only after a control puncture liver biopsy. Morphological examination should indicate the absence or minimal activity of inflammatory changes.
With the ineffectiveness of glucocorticoid therapy, cyclosporine (sandimum neoral *) is used for oral administration from the first year of life, which is released in a solution of 100 mg in 50 ml in a vial, capsules of 10, 25, 50 and 100 mg,
prescribe the drug at a dose of 2-6 mg / kg per day (no more than 15 mg / m 2 per week). Cyclophosphamide (cyclophosphamide *) is prescribed intravenously at a dose of 10-12 mg / kg 1 time in 2 weeks, then in tablets of 0.05 g, 15 mg / kg 1 time in 3-4 weeks, the course dose is not more than 200 mg / kg.

In 5-14% of patients, primary resistance to treatment is observed. They are primarily subject to consultation at liver transplant centers.

Prevention
Primary prevention has not been developed, the secondary consists in early diagnosis, dispensary observation patients (described below) and long-term immunosuppressive therapy.
Forecast
The disease without treatment continuously progresses and does not have spontaneous remission - cirrhosis of the liver is formed. In AIH type 1, glucocorticoids are more often effective and the prognosis is relatively favorable: in many cases, prolonged clinical remission can be achieved. In AIH type 2, the disease usually progresses rapidly to cirrhosis. Type 3 is clinically poorly defined and its course has not been studied.
With the ineffectiveness of immunosuppressive therapy, patients are shown liver transplantation, after which the 5-year survival rate is more than 90%.
drug-induced hepatitis
ICD-10 code
K71. drug-induced hepatitis.
Drug-induced hepatitis is a toxic liver injury, including idiosyncratic (unpredictable) and toxic (predictable) drug-induced liver disease, associated with the intake of hepatotoxic drugs and toxic substances.
Etiology and pathogenesis
The liver plays an important role in the metabolism of xenobiotics (foreign substances). The group of enzymes located in the endoplasmic reticulum of the liver, known as cytochrome P450, is the most important family of enzymes in liver metabolism. Cytochrome P450 absorbs about 90% of toxic and medicinal products.
Often the liver becomes a target for their damaging effects. There are direct and indirect types of liver damage.
Direct type of liver injury depends on the dose of the drug and is due to the action of the drug itself on liver cells and its organelles. The drugs with obligate dose-dependent hepatotoxic effects include paracetamol and antimetabolites, leading to necrosis of hepatocytes. Direct liver damage can also be caused by tetracycline, mercaptopurine, azathioprine, androgens, estrogens, etc.
Indirect type of liver damage, not dependent on the dose of drugs, observed when taking nitrofurans, rifampicin, diazepam, meprobamate, etc. This type reflects the individual reaction of the child's body as a manifestation of hypersensitivity to drugs.
The liver is involved in the metabolism of various xenobiotics through biotransformation processes, which are divided into two phases.
. First phase- oxidative reactions taking place with the participation of cytochromes P450. During this phase, active metabolites may be formed, some of which have hepatotoxic properties.
. Second phase during which the conjugation of previously formed metabolites with glutathione, sulfate or glucuronide occurs, resulting in the formation of non-toxic hydrophilic compounds that are excreted from the liver into the blood or bile.
A special place among toxic liver damage is occupied by medicinal, or drug-induced, hepatitis. Their formation occurs more often as a result of uncontrolled use of drugs (Fig. 6-11, a). Almost any drug can cause liver damage and the development of hepatitis of varying severity.
Toxins can be conditionally divided into household and industrial. Organic production poisons are isolated (carbon tetrachloride, chlorinated naphthalene, trinitrotoluene, trichlorethylene, etc.), metals and metalloids (copper, beryllium, arsenic, phosphorus), insecticides (dichlorodiphenyltrichloroethane - DDT, karbofos, etc.).

Rice. 6-11. Drug-induced hepatitis: a - the formation of drug-induced hepatitis with necrosis of hepatocytes; b - histological picture of drug-induced hepatitis after treatment of acute leukemia (hematoxylin-eosin stain; χ 400)
Particularly severe forms of hepatocyte damage develop when poisoned with substances such as paracetamol, pale toadstool poison, white phosphorus, carbon tetrachloride, and all industrial poisons.
Clinical picture
Typical forms of liver damage with hepatotoxic effects of drugs are presented in Table.
6-9.
Table 6-9. The most common hepatotoxic drug effects

Drug reactions can be transient, hCG are observed infrequently. Liver function tests may return to normal within a few weeks (up to 2 months) after discontinuation of drugs, but in cholestatic hepatitis this period may increase up to 6 months. Jaundice always indicates more severe liver damage, possibly the development of acute liver failure.
Diagnostics
The basis of the diagnosis of drug-induced liver damage is a carefully collected anamnesis of the drugs used, prescribed or used as self-medication. Usually the time interval between taking the drug and the onset of the disease is from 4 days to 8 weeks.
A biopsy may be indicated if pre-existing liver disease is suspected or if there is no normalization of blood chemistry (liver function tests) after discontinuation of the drug.
Pathomorphology
Discomplexation of hepatic beams, severe protein (granular and balloon) dystrophy of hepatocytes, polymorphism of hepatocyte nuclei, dystrophic and necrobiotic changes in the nuclei of hepatocytes are observed (Fig. 6-11, b).
Differential Diagnosis
The possibility of toxic effects of drugs should be taken into account in the differential diagnosis of liver failure, jaundice. It is necessary to exclude other causes: viral hepatitis, diseases of the bile ducts, etc. In rare cases it is necessary to differential diagnosis with congenital metabolic diseases that can cause liver damage, type I glycogenosis (Girke's disease),
Type III (Cori's disease), Type IV (Andersen's disease), Type VI (Hers disease). These diseases occur due to excessive accumulation of glycogen in the liver cells. Chronic liver damage of drug genesis should also be differentiated from lipidosis: Gaucher's disease (based on the accumulation of nitrogen-containing cerebrosides in reticulohistiocytic cells) and Niemann-Pick disease (resulting from the accumulation of phospholipids, mainly sphingomyelin, in the cells of the reticuloendothelial system). It is also necessary to exclude galacto- and fructosemia.
Treatment
An obligatory and main condition for treatment is the complete rejection of the use of a hepatotoxic drug.
High-calorie (90-100 kcal/kg per day) diet rich in proteins (2 g/kg per day) and carbohydrates promotes recovery functional state liver. WITH medicinal purposes recommend essential phospholipids with membrane-stabilizing and hepatoprotective effects, as well as inhibitors of lipid peroxidation processes. Thioctic acid is also prescribed
lota (lipoic acid *, lipamide *), which reduces the toxic effects of drugs due to its antioxidant effect; children over 12 years of age - flavonoid silibinin (karsil *) 5 mg / kg in 3 divided doses (do not chew pills, take after meals with plenty of water).
Forecast
The prognosis depends on how quickly the drug that caused liver damage is stopped. Usually clinical manifestations and changes in biochemical parameters normalize within a few days, rarely weeks.
The prognosis is always serious when a picture of chronic liver damage with hepatocellular insufficiency is formed.
Prevention of chronic hepatitis
Primary prevention has not been developed, the secondary one consists in early recognition and adequate treatment of children with acute viral hepatitis.
The widespread introduction of vaccination against hepatitis A and B will solve the problem of not only acute, but also chronic hepatitis.

CIRRHOSIS OF THE LIVER
ICD-10 codes
K71.7. Toxic liver damage with fibrosis and cirrhosis of the liver.
K74. Fibrosis and cirrhosis of the liver cryptogenic. K74.3. Primary biliary cirrhosis. K74.4. Secondary cirrhosis of the liver. K74.5. Biliary cirrhosis, unspecified. K74.6. Other and unspecified cirrhosis of the liver. P78.3. Cirrhosis is congenital.
Cirrhosis of the liver is a chronic progressive disease characterized by dystrophy and necrosis of the hepatic parenchyma, accompanied by its nodular regeneration, diffuse proliferation of connective tissue. Is a late stage various diseases liver and other organs, in which the structure of the liver is disturbed, and the functions of the liver are not fully performed, resulting in liver failure.
Liver cirrhosis should be distinguished from its fibrosis. Fibrosis - focal proliferation of connective tissue in various liver lesions: abscesses, infiltrates, granulomas, etc.
In economically developed countries, cirrhosis of the liver occurs in 1% of the population, is one of the 6 main causes of death in patients aged 35 to 60 years. Every year, 40 million people die in the world from viral cirrhosis of the liver and hepatocellular carcinoma, which develops against the background of carriage of the hepatitis B virus. It is more often observed in males, the ratio with the female sex is 3:1.
Biliary atresia is one of the common causes biliary cirrhosis in infants, the incidence is 1 in 10,000-30,000 newborns.
Etiology and pathogenesis
Many diseases of the liver and other organs, long-term use of drugs (see Fig. 6-11, a, 6-12, a), etc. lead to cirrhosis of the liver. In addition, other diseases are important in the formation of cirrhosis:
Primary biliary cirrhosis;
Hereditary metabolic disorders (hemochromatosis, hepatolenticular degeneration, galactosemia, α-1-antitrypsin deficiency, etc.);
Violation of the venous outflow from the liver (Budd-Chiari syndrome, veno-occlusive disease, severe right ventricular heart failure), etc.
Atresia of the biliary tract refers to developmental anomalies, which in most cases are associated with intrauterine hepatitis, often caused by one of the reoviruses. In some children, the occurrence of this malformation is due to adverse factors that acted on the 4-8th week of intrauterine life. Usually these children have malformations of other organs (often kidneys, heart, spine). Some children have an association with trisomy on the 13th and 18th pairs of chromosomes. Atresia is characterized by complete closure of intra-, extrahepatic bile ducts in various variants. More often (in 70-80% of cases) intrahepatic form of atresia occurs.
One of the main signs and complications of liver cirrhosis is portal hypertension syndrome which occurs due to an increase in pressure in the portal vein (a vein that brings blood from the abdominal organs to the liver) of more than 5 mm Hg. As a result of increased pressure in the portal vein, blood cannot flow from the abdominal organs and blood stagnation occurs in these organs (Fig. 6-12, b).
Approximate cellular composition of the liver: 70-80% - hepatocytes, 15% - endothelial cells, 20-30% - Kupffer cells (macrophages), 5-8% - Ito cells (Fig. 6-13, a). Ito cells(synonyms: liver stellate cells, fat-storing cells, lipocytes), located in the perisinusoidal space of Disse, play a key role in the pathogenesis of liver cirrhosis. Being the main cells of the connective tissue in the liver, they form the extracellular matrix, accumulating lipids normally. When the liver is damaged, Ito cells begin to produce type I collagen and cytokines, acquiring fibroblast-like properties (Fig. 6-13b). This process occurs with the participation of hepatocytes and Kupffer cells.

Rice. 6-12. Cirrhosis of the liver: a - etiological factors; b - the portal system of the liver and the mechanism of formation of portal hypertension
The pathogenesis of liver cirrhosis is shown in Fig. 6-13, b, but in approximately 10-35% of patients, the etiology and pathogenesis of liver cirrhosis remain unknown.

1 Rice. 6-13. a - part of the hepatic lobule and its cellular composition; b - pathogenesis of liver cirrhosis
Liver changes in cirrhosis are usually diffuse, only in biliary cirrhosis they can be focal. The death of hepatocytes associated with inflammation and fibrosis leads to disruption of the normal architectonics of the liver: the loss of the normal hepatic vasculature with the development of porto-caval shunts and the formation of regeneration nodes of preserved hepatocytes (Fig. 6-14, a), rather than normal hepatic lobules detected in autopsy material or in vivo using MRI (Fig. 6-14, b ).

Rice. 6-14. Changes in the liver in cirrhosis: a - macropreparation of micronodular cirrhosis of the liver; b - MRI of the liver: the arrow indicates the node of regeneration
Classification
Allocate atresia of the extrahepatic biliary tract (without or in combination with atresia of the gallbladder), atresia of the intrahepatic bile ducts (without or in combination with atresia of the extrahepatic biliary tract), total atresia. The classification of liver cirrhosis is presented in Table. 6-10.
Table 6-10. Classification of liver cirrhosis

Clinical picture
In primary biliary cirrhosis, which is manifested by inflammation of the bile ducts of the liver with a violation of the outflow of bile, jaundice, pruritus, fever and other symptoms are observed. Biliary cirrhosis, associated with congenital atresia of the biliary tract, is formed quickly, leading to death in the absence of surgical intervention for health reasons.
Alcoholic cirrhosis of the liver develops in people who consume alcoholic beverages in excessively large doses for a long time, in hepatology childhood it is not considered.
Cirrhosis of the liver in older children develops slowly and may be asymptomatic at first. The signs indicated in the table. 6-11, as a rule, develop gradually and are invisible to a child who has been suffering from a chronic disease of the liver or other organs for a long time, and to his parents.

Hepatomegaly is observed at the onset of the disease. Gradual destruction of hepatocytes, fibrosis as the underlying disease progresses lead to reduction in the size of the liver. Especially characteristic is a decrease in the size of the liver in cirrhosis caused by viral and autoimmune hepatitis.
Table 6-11. Signs of cirrhosis of the liver


Complications of liver cirrhosis are portal hypertension syndrome (Table 6-12), varicose veins lower extremities, bleeding from dilated veins of the esophagus, hepatic coma.
Table 6-12. Diagnosis of Portal Hypertension Syndrome

Varicose veins- a complication of cirrhosis of the liver, manifested by pain in the limbs, visible and significant enlargement of the veins. Bleeding from dilated veins of the esophagus manifested by the release of blood from the mouth and / or blackening of the stool. hepatic coma- brain damage that develops as a result of the accumulation of a large amount of toxic substances in the blood, as a rule, develops with decompensated cirrhosis; the main signs of the syndrome of hepatocellular insufficiency are presented in table. 6-13.
Table 6-13. Signs of hepatocellular insufficiency syndrome

Diagnostics
IN biochemical analysis identify initially syndromes of cytolysis, cholestasis, inflammation, later - hepatodepressive syndrome (see Tables 1-8).
Ultrasound describes micronodular (Fig. 6-15, a) or macronodular (Fig. 6-15, b) types of liver cirrhosis. Histological synonyms for these names:
Small-nodular cirrhosis - the formation of small nodules (about 1 mm in diameter) is characteristic;
Large-nodular cirrhosis - in areas of previous destruction of the hepatic architectonics, large fibrous scars are detected.
Pathomorphology
A classic liver macropreparation, clearly representing biliary cirrhosis of the liver, is shown in Fig. 6-15, c.
During the life of a child, only a biopsy can accurately indicate cirrhosis of the liver, in which severe dystrophic changes in hepatocytes, cholestasis, foci of growth of connective tissue (fibrous nodes), between which islets are located normal liver cells (Fig. 6-15, d).
Differential Diagnosis
Treatment
The main principles of treatment of cirrhosis of the liver are as follows.
Elimination of the causes that led to cirrhosis (etiotropic treatment): antiviral therapy (viral hepatitis), withdrawal (alcoholic cirrhosis), drug withdrawal (medicated hepatitis).

Rice. 6-15. Cirrhosis of the liver according to ultrasound: a - micronodular; b - macronodular: congenital atresia of the bile ducts with the formation of cirrhosis: c - macropreparation; d - micropreparation (staining with hematoxylin-eosin; χ 400)
Diet therapy.
Therapy of developed complications of liver cirrhosis: symptomatic treatment of hepatic encephalopathy, portal hypertension syndrome, etc.
Pathogenetic: removal of excess iron and copper (hemochromatosis, Wilson-Konovalov disease), immunosuppressive therapy (AIH), treatment of cholestasis (primary biliary cirrhosis).

With established diagnosis biliary atresia surgical treatment: choledochojejunostomy or protoenterostomy (Kasai operation - the creation of a direct anastomosis between the decapsulated opened surface of the liver in
gate area and intestines), transplantation of a part of the liver. Before surgery, treatment is supportive. Glucocorticoids are ineffective, as are other drugs. At the same time, vitamin K should be administered parenterally once a week, periodically taking courses of hepatoprotectors, vitamins E, D.
Treatment of complications of liver cirrhosis
Strict bed rest;
Hyponatrium diet: with minimal and moderate ascites - restriction of salt intake to 1.0-1.5 g / day; with intense ascites - up to 0.5-1.0 g / day;
Restriction of fluid intake to 0.8-1.0 liters per day;
Diuretic therapy: aldosterone antagonists and natriuretics;
Therapeutic paracentesis (3-6 l) with intravenous administration of albumin solution (at the rate of 6-8 g per 1 l of removed ascitic fluid);
Ultrafiltration with a peritoneal-venous shunt, transjugular intrahepatic portosystemic shunt;
Liver transplant.
Diuretics. Hydrochlorothiazide (hypothiazid *) in tablets and capsules is prescribed orally for children from 3 to 12 years old, 1-2 mg / kg per day in 1 dose. Hypokalemia can be avoided by the use of drugs containing potassium, or by eating foods rich in potassium (fruits, vegetables).
Spironolactone (veroshpiron*, aldactone*, veropilactone*) tablets, capsules, initial daily dose- 1.33 mg / kg, maximum - 3 mg / kg in 2 doses, or 30-90 mg / m 2, course - 2 weeks. Contraindicated in infancy.
Furosemide (lasix *) in tablets of 40 mg and granules for suspension, ampoules 1% - 2 ml. Newborns are prescribed 1-4 mg/kg per day 1-2 times, 1-2 mg/kg intravenously or intramuscularly 1-2 times a day, children - 1-3 mg/kg per day, adolescents - 20-40 mg / day.
Diuretic drugs are prescribed in the morning. It is necessary to control the level of potassium in the blood serum, ECG.

The criterion for the effectiveness of the therapy is a positive water balance, which is 200-400 ml/day with a small amount of ascites and 500-800 ml/day with edematous ascitic syndrome in older children. Paracentesis perform according to strict indications (with a large amount of liquid) with the simultaneous administration of albumin in the amount of 4-5 g / in. If drug therapy fails, it is possible surgical treatment(shunting).
Hemostatic therapy (ε-aminocaproic acid, vikasol*, calcium gluconate, dicynone*, erythrocyte mass).
Restoration of the volume of circulating blood (albumin solution, plasma).
Pharmacological reduction of portal pressure (vasopressin, somatostatin, octreotide).
Mechanical tamponade of the esophagus (Sengstaken-Blackmore probe).
Endoscopic methods of stopping bleeding (sclerotherapy with ethanolamine, polidocanol, ligation of vein trunks).
Transjugular intrahepatic portosystemic shunt.
Prevention of stress ulcers of the gastrointestinal tract (blockers of H2-histamine receptors, PPIs).
Prevention of hepatic encephalopathy (lactulose, siphon enemas).
Prevention of spontaneous bacterial peritonitis (antibiotics).
Main pharmacological agents with hemorrhagic syndrome
ε-Aminocaproic acid for intravenous administration and in granules for the preparation of a suspension for oral administration, the daily dose for children under 1 year is 3 g; 2-6 years - 3-6 g, 7-10 years - 6-9 g.
Menadione sodium bisulfate (Vikasol *) 1% solution is prescribed for children under 1 year - 2-5 mg / day, 1-2 years - 6 mg / day, 3-4 years - 8 mg / day, 5-9 years - 10 mg / day, 10-14 years - 15 mg / day. The duration of treatment is 3-4 days, after a 4-day break, the course is repeated.
Etamsylate (dicynone *) is produced in tablets of 250 mg and as a 12.5% solution in ampoules of 2 mg (250 mg per ampoule) for intramuscular and intravenous administration. When bleeding, children under 3 years of age are administered 0.5 ml, 4-7 years - 0.75 ml, 8-12 years - 1-1.5 ml and 13-15 years - 2 ml. The indicated dose is repeated every 4-6 hours for 3-5 days. In the future, treatment with dicynone * can be continued in tablets (daily dose - 10-15 mg / kg): children under 3 years old - 1/4 tablet, 4-7 years old - 1/2 tablet, 8-12 years old - 1 tablet and 13-15 years old - 1.5-2 tablets 3-4 times a day.
Means for strengthening the vascular wall - flavonoid troxerutin, ascorbic acid + rutoside (ascorutin *).
To reduce portal pressure, desmopressin (minirin *) is used - an analogue of the natural hormone arginine-vasopressin, 100-200 mg at night.

Treatment malignant neoplasm of the liver carried out by specialists cancer center. Indications for splenectomy
Segmental extrahepatic portal hypertension.
Severe hypersplenism with hemorrhagic syndrome.
Lag in the physical and sexual development of children with cirrhosis of the liver.
Giant splenomegaly with marked pain syndrome(heart attacks, perisplenitis).
Treatment spontaneous bacterial peritonitis carry out cephalosporins III-IV generation.
A radical treatment for cirrhosis of the liver is liver transplantation.
Prevention
basis secondary prevention is a timely etiotropic and pathogenetic treatment of acute and chronic hepatitis.
Prevention of cirrhosis in essence tertiary And quaternary, since they carry out treatment aimed at stabilizing the pathological process in the liver, preventing exacerbations, reducing the risk of development and progression of complications. Children should be under dynamic supervision in specialized clinics and centers, and on an outpatient basis - under the supervision of a pediatrician and a gastroenterologist. Immunoprophylaxis is carried out strictly individually.
Prevention of complications, for example, the first bleeding from varicose veins of the esophagus, is possible due to endoscopic examination at least 1 time in 2-3 years in order to dynamically monitor their likely development. The condition of patients with initial stage varicose veins esophageal veins are monitored endoscopically once every 1-2 years. Preventive treatment carried out with moderate and severe.
Forecast
The prognosis of liver cirrhosis is unfavorable and, as a rule, uncertain and unpredictable, as it depends on the cause of cirrhosis, the age of the patient, the stage of the disease, and the possibility of unforeseen fatal complications. By itself, cirrhosis of the liver is incurable (except in cases where a liver transplant was performed), but the correct treatment of cirrhosis allows for a long time (20 years or more) to compensate for the disease. Compliance with the diet, traditional and alternative methods of treatment (Fig. 6-16), the rejection of bad habits significantly increase the patient's chances of compensating for the disease.

Rice. 6-16. Treatment options for patients with cirrhosis
Without surgical treatment children with atresia of the biliary tract die in the 2-3rd year of life. The earlier the operation is performed, the better the prognosis. About 25-50% of early operated children survive 5 years or more when they receive a liver transplant. The outcome depends on the presence or absence of an inflammatory and sclerotic process in the liver.
LIVER FAILURE
ICD-10 codes
K72. Liver failure. K72.0. Acute and subacute liver failure. K72.1. Chronic liver failure. K72.9. Liver failure, unspecified.
Liver failure is a complex of symptoms characterized by a violation of one or more functions of the liver, resulting from damage to its parenchyma (hepatocellular or hepatocellular insufficiency syndrome). Portosystemic or hepatic encephalopathy is a symptom complex of CNS disorders that occurs with liver failure with a profound impairment of numerous vital liver functions.
Mortality from liver failure is 50-80%. In acute liver failure, hepatic encephalopathy may develop, which is rare in acute liver diseases, but mortality can reach 80-90%.
Etiology and pathogenesis
Acute liver failure occurs in severe forms of viral hepatitis A, B, C, D, E, G, poisoning with hepatotropic poisons (alcohol, some drugs, industrial toxins, mycotoxins and aflatoxins, carbon dioxide and etc.). Its causes may be herpes viruses, cytomegalovirus, infectious mononucleosis virus, simple and herpes zoster, Coxsackie virus, the causative agent of measles; septicemia in liver abscesses. Acute liver failure is described in toxic hepatoses (Reye's syndrome, a condition after the small intestine is turned off), Wilson-Konovalov's disease, Budd-Chiari syndrome.
Budd-Chiari Syndrome(ICD-10 code - I82.0) develops due to progressive narrowing or closure of the hepatic veins. On the basis of thrombophlebitis of the umbilical vein and the Arantzian duct, which flows into the mouth of the left hepatic vein, Budd-Chiari syndrome can begin in early childhood. As a result, stagnation develops in the liver with compression of the liver cells.
Reye's syndrome(ICD-10 code - G93.7) - acute encephalopathy with cerebral edema and fatty liver infiltration that occurs in previously healthy newborns, children and adolescents (usually at the age of 4-12 years), associated with a previous viral infection (for example, chicken pox or influenza type A) and taking drugs containing acetylsalicylic acid.
Chronic liver failure is a consequence of the progression of chronic liver diseases (hepatitis, cirrhosis, malignant tumors liver, etc.). The main etiological factors are shown in fig. 6-17, a.
At the basis of pathogenesis liver failure there are two processes. Firstly, severe dystrophy and widespread necrobiosis of hepatocytes lead to a significant decrease in liver function. Secondly, due to the numerous collaterals between the portal and vena cava, a significant part of the absorbed toxic products enters the big circle circulation around the liver. Poisoning is caused by non-neutralized protein breakdown products, end products of metabolism (ammonia, phenols).
emergence hepatic encephalopathy in liver failure is associated with impaired homeostasis, acid-base status and electrolyte composition blood (respiratory and metabolic alkalosis, hypokalemia, metabolic acidosis, hyponatremia, hypochloremia, azotemia). Cerebrotoxic substances enter the systemic circulation from the gastrointestinal tract and liver: amino acids and their decay products (ammonia, phenols, mercaptans); products of hydrolysis and oxidation of carbohydrates (lactic, pyruvic acid, acetone); products of impaired fat metabolism; false neurotransmitters (asparagine, glutamine), which have toxic effects on the central nervous system. The mechanism of damage to brain tissue is associated with impaired function of astrocytes, which make up approximately 30% of brain cells. Astrocytes play a key role in regulating the permeability of the blood-brain barrier, in ensuring the transport of neurotransmitters to brain neurons, and in the destruction toxic substances(in particular, ammonia) (Fig. 6-17, b).

Rice. 6-17. Chronic liver failure and hepatic encephalopathy: a - etiology of liver failure; b - the mechanism of formation of hepatic encephalopathy
ammonia exchange. At healthy people In the liver, ammonia is converted to uric acid in the Krebs cycle. It is required in the conversion of glutamate to glutamine, which is mediated by the enzyme glutamate synthetase. In chronic liver damage, the number of functioning hepatocytes decreases, creating prerequisites for hyperammonemia. When portosystemic shunting occurs, ammonia, bypassing the liver, enters the systemic circulation - hyperammonemia occurs. Ammonia, acting
in the brain, leads to disruption of the functioning of astrocytes, causing morphological changes in them. As a result, with liver failure, cerebral edema occurs, and intracranial pressure increases.
Under conditions of liver cirrhosis and portosystemic shunting, the activity of skeletal muscle glutamate synthetase increases, where the process of ammonia destruction begins to occur. This explains the decrease in muscle mass in patients with cirrhosis of the liver, which, in turn, also contributes to hyperammonemia. The processes of metabolism and excretion of ammonia also occur in the kidneys.
Clinical picture
The clinical picture is manifested by disorders of consciousness and cognitive functions, drowsiness, monotonous speech, tremor, and discoordination of movements. Especially important signs are a rapid decrease in the size of the liver, its softening and pain on palpation. In table. 6-14 briefly summarized the clinical manifestations of the stages of liver failure and encephalopathy, the differences between acute and chronic liver failure - in table. 6-15.
Table 6-14. Classification of stages of liver failure and encephalopathy

Table 6-15. Differential diagnosis of acute and chronic liver failure

Hepatic coma is preceded by general excitation, which turns into oppression of consciousness: stupor and stupor, then its complete loss occurs. Appear meningeal phenomena, pathological reflexes (grasping, sucking), restlessness, convulsions. Breathing becomes arrhythmic, like Kussmaul or Cheyne-Stokes. Pulse small, irregular. From the mouth and from
the skin emits a liver smell (feetor hepatica), due to the release of methyl mercaptan; jaundice and hemorrhagic syndrome increase, ascites, hypoproteinemic edema increase (Fig. 6-18, a). Clinical manifestations of the decompensated and terminal stages are clearly shown in Fig. 6-18, Gd. The term "malignant form" (the most severe form) refers to a qualitatively new clinical condition that occurs in patients with viral hepatitis B if they develop massive or submassive liver necrosis.

Rice. 6-18. Liver failure: a - clinical manifestations; a and b - decompensated stage; c - terminal stage ("floating eyeball»); d - hepatic coma

Over the next 2-3 days, a deep hepatic coma develops. Sometimes a coma occurs, bypassing the stage of excitement.
Diagnostics
Conduct laboratory and instrumental studies.
IN general analysis blood revealed anemia, leukocytosis, thrombocytopenia, increased ESR.
In a biochemical study, bilirubinemia, azotemia, hypoalbuminemia, hypocholesterolemia are diagnosed, the levels of ALT, AST, alkaline phosphatase increase, the levels of fibrinogen, potassium, sodium, prothrombin index decrease, metabolic acidosis is noted.
Ultrasound, CT scan of the liver reveals a change in the size and structure of the liver parenchyma.
Pathomorphology
Morphological changes in the liver affect all of its tissue components: parenchyma, reticuloendothelium, connective tissue stroma, and to a lesser extent - biliary tract.
Distinguish three options acute form diseases:
Acute cyclic form;
Cholestatic (pericholangiolytic) hepatitis;
Massive necrosis of the liver.
The severity of morphological changes depends on the severity and etiology of the disease (Fig. 6-19, a, b). At the height of the disease, alternative, exudative processes predominate; during the recovery period, the processes of proliferation and regeneration prevail.

Rice. 6-19. Liver necrosis, macro- and micropreparations: a - etiology is unknown; b - adenovirus etiology; c - χ 250; d - χ 400 (hematoxylin-eosin staining)
In cholestatic (pericholangiolytic) hepatitis, morphological changes mainly concern the intrahepatic bile ducts (cholangiolitis and pericholangiolitis).
Liver necrosis is an extreme degree of changes in the liver, which can be massive, when almost the entire hepatic epithelium dies or an insignificant border of cells is preserved along the periphery of the lobules, or submassive, in which most hepatocytes undergo necrobiosis, mainly in the center of the lobules (Fig. 6-19, c, d).
Differential Diagnosis
For the purposes of differential diagnosis, it is necessary to exclude extrahepatic causes of symptoms from the CNS. The level of ammonia in the blood is determined upon admission to the hospital of a patient with cirrhosis of the liver and signs of CNS damage. It is necessary to establish the presence in the patient's history of such pathological conditions as metabolic disorders, gastrointestinal bleeding, infections, and constipation.
If symptoms of hepatic encephalopathy occur, a differential diagnosis is made with diseases that include the following.
Intracranial pathological conditions: subdural hematoma, intracranial bleeding,
stroke, brain tumor, brain abscess.
Infections: meningitis, encephalitis.
Metabolic encephalopathy, which developed against the background of hypoglycemia, electrolyte disturbances, uremia.
Hyperammonemia caused by congenital anomalies of the urinary tract.
Alcohol-induced toxic encephalopathy acute intoxication, Wernicke's encephalopathy.
Toxic encephalopathy that arose while taking medications: sedatives and antipsychotics, antidepressants, salicylates.
Postconvulsive encephalopathy.
Treatment
Treatment consists in limiting the amount of protein in the diet, the appointment of lactulose. Patients with hepatic encephalopathy are candidates for liver transplantation.

In complex medical measures liver failure, there are stages (Fig. 6-20), as well as basic (standard) therapy and a number of more radical means aimed at cleansing the body of toxic products of metabolic disorders, as well as replacing (temporary or permanent) the functions of the affected liver.
Basic therapy acute liver failure is aimed at correcting the electrolyte, energy balance, acid-base state, vitamins and cofactors, disorders of the blood coagulation system, hemocirculation, elimination of hypoxia, prevention of complications, prevention of absorption of putrefactive decay products from the intestine. Basic therapy also includes the use of glucocorticoids.
General principles of managing a patient with acute liver failure
Individual post of a nurse.
Monitor urinary output, blood glucose and vital signs every hour.

Rice. 6-20. Stages of treatment of hepatic encephalopathy
Control of potassium in the blood serum 2 times a day.
Blood test, determination of the content of creatinine, albumin, assessment of the coagulogram daily.
Prevention of bedsores.
General principles of managing a patient with chronic liver failure
Active monitoring of the patient's condition, taking into account the severity of symptoms of encephalopathy.
Daily weighing of the patient.
Daily assessment of the balance of fluids drunk and excreted per day.
Daily determination of blood tests, electrolytes, creatinine.
Determination 2 times a week of the content of bilirubin, albumin, activity of AST, ALT, alkaline phosphatase.
Coagulogram, prothrombin content.
Evaluation of the need and possibility of liver transplantation in the final stage of liver cirrhosis.
Treatment of hepatic encephalopathy
Elimination of provoking factors.
Stop gastrointestinal bleeding.
Suppression of the growth of proteolytic microflora in the colon and treatment of infectious diseases.
Normalization of electrolyte disorders.
Reducing the degree of hyperammonemia:
a) reduction of ammoniacogenic substrate:
Cleansing the gastrointestinal tract (siphon enemas, laxatives);
Decreased protein intake;
b) the binding of ammonia in the blood:
Ornithine (hepa-merz*);
c) suppression of ammonia formation:
Antibiotics a wide range actions;
Acidification of intestinal contents with lactulose. Enemas are recommended to reduce ammonia levels.
or the use of laxatives for bowel movements at least 2 times a day. For this purpose, lactulose (Normaze *, dufalac *) is prescribed in syrup, 20-50 ml orally every hour until diarrhea appears, then 15-30 ml 3-4 times a day. For use in an enema, up to 300 ml of the drug is diluted in 500-700 ml of water.
Before the patient is discharged from the hospital, the dose of lactulose should be reduced to 20-30 ml at night, with a possible subsequent cancellation at the outpatient stage.

TO radical treatment methods include the following measures to massively remove toxic products from the patient's blood.
controlled hemodilution.
Plasmapheresis.

Exchange transfusion.
Temporary (or permanent) replacement of the patient's liver by extracorporeal connection of xeno-liver (pork), cross-circulation.
Hetero- and orthotopic liver transplantation.
Prevention
The best way to prevent liver failure is to prevent the risk of developing cirrhosis or hepatitis. This requires specific immunization, compliance is important healthy lifestyle life, rules of personal hygiene, diet therapy.
The introduction of a specific immunoglobulin in case of an accidental transfusion of infected blood and at the birth of a child in a mother - a carrier of HBsAg or a patient with hepatitis B will allow passive immunization. Active immunization - vaccination of a child on the first day after birth, unvaccinated children of any age, as well as persons from risk groups: professional (doctors, emergency workers, military, etc.), persons on program hemodialysis, etc. (revaccination every 7 years). Vaccination against viral hepatitis B protects against infection with hepatitis D.
Forecast
When the cause of liver failure is eliminated, the manifestations of hepatic encephalopathy can be reduced. Chronic hepatic coma is fatal, however, with acute hepatocellular insufficiency, recovery is sometimes possible. With the development of hepatic encephalopathy, mortality can reach 80-90%.
You can ask a DOCTOR a question and get a FREE ANSWER by filling out a special form on OUR SITE, using this link >>>
ICD code: B19
Viral hepatitis, unspecified
Viral hepatitis, unspecified
- Search by ClassInform
Search in all classifiers and directories on the KlassInform website
Search by TIN
- OKPO by TIN
Search for OKPO code by TIN
Search for OKTMO code by TIN
Search OKATO code by TIN
Search for OKOPF code by TIN
Search for OKOGU code by TIN
Search for OKFS code by TIN
Search PSRN by TIN
Search for TIN of an organization by name, TIN of IP by full name
Counterparty check
- Counterparty check
Information about counterparties from the database of the Federal Tax Service
Converters
- OKOF to OKOF2
Translation of the OKOF classifier code into the OKOF2 code
Translation of the OKDP classifier code into the OKPD2 code
Translation of the OKP classifier code into the OKPD2 code
Translation of the OKPD classifier code (OK 034-2007 (KPES 2002)) into the OKPD2 code (OK 034-2014 (KPE 2008))
Translation of the OKUN classifier code into the OKPD2 code
Translation of the OKVED2007 classifier code into the OKVED2 code
Translation of the OKVED2001 classifier code into OKVED2 code
Translation of the OKATO classifier code into the OKTMO code
Translation of the TN VED code into the OKPD2 classifier code
Translation of the OKPD2 classifier code into the TN VED code
Translation of the OKZ-93 classifier code into the OKZ-2014 code
Classifier changes
- Changes 2018
Feed of classifier changes that have taken effect
All-Russian classifiers
- ESKD classifier
All-Russian classifier of products and design documents OK 012-93
All-Russian classifier of objects of administrative-territorial division OK 019-95
All-Russian classifier of currencies OK (MK (ISO 4217) 003-97) 014-2000
All-Russian classifier of types of cargo, packaging and packaging materials OK 031-2002
All-Russian classifier of economic activities OK 029-2007 (NACE Rev. 1.1)
All-Russian Classification of Economic Activities OK 029-2014 (NACE REV. 2)
All-Russian classifier of hydropower resources OK 030-2002
All-Russian classifier of units of measure OK 015-94 (MK 002-97)
All-Russian classifier of occupations OK 010-2014 (MSKZ-08)
All-Russian classifier of information about the population OK 018-2014
All-Russian classifier of information on social protection population. OK 003-99 (valid until 12/01/2017)
All-Russian classifier of information on social protection of the population. OK 003-2017 (valid from 01.12.2017)
All-Russian classifier of elementary vocational education OK 023-95 (valid until 07/01/2017)
All-Russian classifier of government bodies OK 006 - 2011
All-Russian classifier of information about all-Russian classifiers. OK 026-2002
All-Russian classifier of organizational and legal forms OK 028-2012
All-Russian classifier of fixed assets OK 013-94 (valid until 01/01/2017)
All-Russian classifier of fixed assets OK 013-2014 (SNA 2008) (effective from 01/01/2017)
All-Russian classifier of products OK 005-93 (valid until 01/01/2017)
All-Russian classifier of products by type of economic activity OK 034-2014 (KPES 2008)
All-Russian classifier of occupations of workers, positions of employees and wage categories OK 016-94
All-Russian classifier of minerals and groundwater. OK 032-2002
All-Russian classifier of enterprises and organizations. OK 007–93
All-Russian classifier of standards OK (MK (ISO / infko MKS) 001-96) 001-2000
All-Russian classifier of specialties of higher scientific qualification OK 017-2013
All-Russian classifier of countries of the world OK (MK (ISO 3166) 004-97) 025-2001
All-Russian classifier of specialties in education OK 009-2003 (valid until 07/01/2017)
All-Russian classifier of specialties in education OK 009-2016 (valid from 07/01/2017)
All-Russian classifier of transformational events OK 035-2015
All-Russian classifier of territories municipalities OK 033-2013
All-Russian classifier of management documentation OK 011-93
All-Russian classifier of forms of ownership OK 027-99
All-Russian classifier of economic regions. OK 024-95
All-Russian classifier of public services. OK 002-93
Commodity nomenclature of foreign economic activity (TN VED EAEU)
Classifier of types of permitted use of land plots
General government transactions classifier
Federal classification catalog of waste (valid until 06/24/2017)
Federal classification catalog of waste (valid from 06/24/2017)
Classifiers international
Universal Decimal Classifier
International Classification of Diseases
Anatomical Therapeutic Chemical Classification of Drugs (ATC)
International Classification of Goods and Services 11th edition
International Industrial Design Classification (10th edition) (LOC)
Reference books
Unified Tariff and Qualification Directory of Works and Professions of Workers
Unified qualification directory of positions of managers, specialists and employees
2017 Occupational Standards Handbook
Samples of job descriptions taking into account professional standards 2016-2017
Federal state educational standards 2017-2018
All-Russian database of vacancies Work in Russia
State cadastre of civil and service weapons and cartridges for them
Production calendar for 2017
Production calendar for 2018
ICD code 10 hepatitis
Sofosbuvir + Daclatasvir
Delivery to the regions of the Russian Federation and Belarus - 3 days without prepayment
viral hepatitis C code 10
Welcome. There is only one answer to your question The key to getting rid of hepatitis C quickly and completely is an approved and certified generic latest generation Lesovir-C developed by Beximco Pharmaceuticals LTD in Bangladesh. The 1st (the most common in Russia), 2nd and 6th genotypes, as well as the 3rd - according to unofficial data, can be treated. The chance of cure is 98%, which is confirmed by research results. All other "Indian generics" that are "sold" today are not yet released, but only announced, and this is easy to verify. Now the drug is produced only in Bangladesh. Advantages of Lesovir-S: 1. Already exists; 2. Low price(tens of times cheaper than European analogues); 3. Most high performance cure (all drugs sold in Russia give only a 50% chance, and this is at best); 4. Does not require combinations with other drugs; 5. Low toxicity; 6. Virtually no side effects; 7. Short "course" - no need to take medicine for years; 8. The product is approved and certified; 9. Any information about him is easy to find in open sources. Check it out, check it out, and come back. viral hepatitis C code 10 Lesovir-S is an obvious solution. Our experience in the pharmaceutical industry market of the best certified generics is more than 8 years. Our company will help with sending the drug to anywhere in the world. The company's office is located in Dhaka (Bangladesh), close to the manufacturing plant, which allows you to keep dumping prices. If you find a cheaper Lesovir-S from a reliable supplier, just let us know - our price will always be lower. We work with a guarantee - money after you receive the goods: this, in our opinion, is how reliability is determined. We always solve all problems with delivery in favor of the client. Our company gives one hundred percent chance. If you have any questions - call us at the specified phone number or use the feedback form, we will contact you immediately. And to your question viral hepatitis C code 10. there is only one answer, and that answer you have already found. You are safe.
Life expectancy in chronic hepatitis C
In the twenty-first century, medicine has reached a new level - many adverse conditions can be defeated at the very beginning of development thanks to the invention of various drugs and methods. However, this, unfortunately, does not apply to liver diseases - they still occupy one of the first places in the list of the most common pathologies in the human population. According to the statistics of the World Health Organization (WHO), today more than two billion people are sick or carriers of chronic viral hepatitis on the planet. These are truly frightening numbers, given the inexorably increasing speed with which the pathogen is spreading. Infectious damage to the liver does not only affect a specific patient, it is a large-scale problem for the health sector and the economy of many countries - especially those where programs are being developed for the social support of patients. In this article, you will learn what chronic hepatitis C is, why it is considered so dangerous - and what ways to overcome the disease are recognized as the most effective.

Viral lesions of the liver, like any other infectious diseases, have an important feature - they always have a pathogen, the presence of which can be checked using laboratory methods. This allows not only to establish an accurate diagnosis, but also to select a specific, so-called etiotropic treatment. Chronic hepatitis C (C, HCV) develops after a person is infected with a virus containing RNA (ribonucleic acid) in the genome. In the International Classification of Diseases (ICD-10), it is coded B18.2.
The infection does not manifest itself immediately - the patient may feel the first symptoms months and years after the penetration of a dangerous agent into the body. In many people, it is already detected at the stage of cirrhosis - for this reason, hepatitis C is called the “gentle killer”, because at the stage of late changes it is no longer possible to cure a person. At the same time, liver disease is caused not only by the presence of viral particles in its cells (hepatocytes). In addition to their direct impact, an aggressive reaction from the immune system is also observed, which leads to the constant destruction of the functional units of the organ and an active inflammatory process.
Symptoms of chronic hepatitis C
The disease is characterized by a long latent period, during which the infected person does not complain about anything; sometimes he is disturbed by general signs - fatigue, weakness. They are transient and stop on their own. People with chronic hepatitis C live months, years, and even decades unaware of the infection.
Typical manifestations
This is a group of signs, the occurrence of which clearly indicates the presence of liver damage:
- Nausea, vomiting, lack of appetite.
- Enlargement of the liver, feeling of heaviness in the abdomen.
- Darkening of urine, gray color of feces.
- Icteric coloration of the skin of varying degrees of intensity, itching
- Pain in the joints, muscles, and also in the right upper quadrant of the abdomen.
These symptoms develop gradually.
The formation of cirrhosis (dense fibrous nodes in the liver) takes a different time, but then exhaustion joins the symptoms of chronic hepatitis C -  the patient loses weight, suffers from constant nausea, heaviness in the abdomen.
the patient loses weight, suffers from constant nausea, heaviness in the abdomen.
Portal hypertension caused by high blood pressure in the portal vein, - brings such a manifestation as a dilated (expanded) venous network on the abdomen. It is easily seen by visual inspection. In addition, the diameter of the lumen of the veins of the esophagus and stomach increases, but confirmation requires fibroesophagogastroduodenoscopy (FGDS), during which these departments are examined using a flexible optical tube-endoscope. In the abdominal cavity, a serous effusion (ascites) is determined.
Atypical manifestations
They can also be called general, non-specific - they complement the objective picture described in the previous section, but at the same time cannot be attributed only to the symptoms associated with liver damage. Chronic viral hepatitis C is characterized by such signs as:
- fatigue even with little physical exertion;
- constant weakness, irritability, nervousness, depressed mood;
- prolonged persistent increase in body temperature without objective reasons.
Fatigue can be perceived as a consequence of daily workload and often goes unnoticed - it is beginning to be assessed as a symptom of pathology only after the development of a typical complex of manifestations. Fever is usually subfebrile (within 37.1–37.9 ° C). Depressive disorders are often recorded in the medical history.
How is chronic hepatitis C transmitted?
 The disease belongs to the group of transfusion pathologies of the liver. A few decades ago, the pathogen that provokes it was not even suspected. Blood prepared for transfusion was not tested, and many people in need of this procedure were infected. However, this is not the only way of distribution; The main mechanisms of infection include several groups:
The disease belongs to the group of transfusion pathologies of the liver. A few decades ago, the pathogen that provokes it was not even suspected. Blood prepared for transfusion was not tested, and many people in need of this procedure were infected. However, this is not the only way of distribution; The main mechanisms of infection include several groups:
- parenteral (contact of damaged skin or mucous membranes with the patient's blood during hemotransfusion, contact with its remains on instruments for medical procedures, cosmetic manipulations, injections);
- sexual (sexual contact not protected by a condom);
- vertical (infection of a child in utero or during passage through the birth canal of a sick woman).
How is chronic viral hepatitis C transmitted by contact? Spread in a family or close team is possible if people share the same toothbrush, cutlery with the patient in the presence of wounds in the oral cavity.
A kiss is dangerous if the oral mucosa of both partners has at least minimal damage.
How long do people live with chronic hepatitis C?
This is largely determined by the presence of additional liver diseases, which can accelerate the development of complications, as well as the individual characteristics of the patient's body. With modern medications started (up to the stage of cirrhosis formation), the prognosis is relatively favorable - a person is able to live for several more decades, up to a very old age.
Viral hepatitis NOS
In Russia International Classification of Diseases 10th revision ( ICD-10) is adopted as a single regulatory document for accounting for morbidity, reasons for the population to apply to medical institutions of all departments, and causes of death.
ICD-10 introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997. №170
The publication of a new revision of the ICD is planned by WHO in 2017-2018.
Amendments and additions to ICD-10 introduced by WHO to date.
Code micb acute hepatitis unspecified micb 10
For the treatment of the liver, our readers successfully use Leviron Duo. Seeing the popularity of this tool, we decided to bring it to your attention.
Read more here…
The ICD is a classification system for various diseases and pathologies.
Since its adoption by the world community at the beginning of the 20th century, it has gone through 10 revisions, so the current version is called ICD 10. For the convenience of automating the processing of diseases, they are encrypted with codes, knowing the principle of formation of which, it is easy to find any disease. So, all diseases of the digestive system begin with the letter "K". The next two digits identify a specific organ or group of them. For example, liver disease begins with K70–K77 combinations. Further, depending on the cause, cirrhosis may have a code starting with K70 (alcoholic liver disease) and K74 (fibrosis and cirrhosis of the liver).
With the introduction of ICD 10 into the system medical institutions, the design of sick leave began to be carried out according to the new rules, when instead of the name of the disease, the corresponding code is written. This simplifies statistical accounting and makes it possible to use computer technology to process data arrays both in general and for various types of diseases. Such statistics are necessary for the analysis of morbidity on the scale of regions and states, in the development of new drugs, determining the volume of their production, etc. To understand what a person is sick with, it is enough to compare the entry on the sick leave with the latest edition of the classifier.
Classification of cirrhosis
Cirrhosis is a chronic liver disease characterized by its insufficiency due to tissue degeneration. This disease tends to progress and differs from other liver diseases by irreversibility. The most common causes of cirrhosis are alcohol (35–41%) and hepatitis C (19–25%). According to ICD 10, cirrhosis is divided into:
- K70.3 - alcoholic;
- K74.3 - primary biliary;
- K74.4 - secondary biliary;
- K74.5 - biliary, unspecified;
- K74.6 - different and unspecified.
Alcoholic cirrhosis
Cirrhosis of the liver caused by alcohol in ICD 10 has the code K70.3. It was specially identified in a group of separate diseases, the main cause of which is ethanol, the damaging effect of which does not depend on the type of drinks and is determined only by its amount in them. Therefore, a large amount of beer will do the same harm as a smaller amount of vodka. The disease is characterized by the death of liver tissue, which is transformed into cicatricial, in the form of small nodes, while its correct structure is disturbed and the lobules are destroyed. The disease leads to the fact that the body ceases to function normally and the body is poisoned by decay products.
Primary biliary cirrhosis
Primary biliary cirrhosis is an immune-related liver disease. According to ICD 10, it has the code K74.3. Causes autoimmune disease not installed. When it occurs the immune system starts fighting with own cells bile ducts of the liver, damaging them. Bile begins to stagnate, which leads to further destruction of the tissues of the organ. Most often, this disease affects women, mostly 40-60 years. The disease manifests itself skin itching, which at times intensifies, leading to bleeding scratches. This cirrhosis, like most other types of disease, reduces performance and causes depressed mood and lack of appetite.
Secondary biliary cirrhosis
Secondary biliary cirrhosis occurs due to the action of bile, which, having accumulated in the organ, cannot leave it. According to ICD 10, it has the code K74.4. The cause of obstruction of the bile ducts may be stones or the consequences of surgery. Such a disease requires surgical intervention to eliminate the causes of obstruction. Delay will lead to the continuation of the destructive effect of bile enzymes on the liver tissue and the development of the disease. Men suffer from this type of disease twice as often, usually between the ages of 25-50, although it also occurs in children. The development of the disease most often takes from 3 months to 5 years, depending on the degree of obstruction.
Biliary cirrhosis, unspecified
The word "biliary" comes from the Latin "bilis", which means bile. Therefore, cirrhosis associated with inflammatory processes in the bile ducts, stagnation of bile in them and its effect on liver tissues is called biliary. If, however, he does not have hallmarks primary or secondary, then it is classified according to ICD 10 as biliary unspecified cirrhosis. The cause of these types of disease can be various infections and microorganisms that cause inflammation of the intrahepatic biliary tract. In the 10th edition of the classifier, such a disease has the code K74.5.
Other and unspecified cirrhosis
Diseases that, by etiology and clinical signs, do not coincide with those previously listed, are assigned the general code K74.6 according to ICD 10. Adding new numbers to it allows their further classification. So unspecified cirrhosis in the 10th edition of the classifier was assigned the code K74.60, and the other - K74.69. The latter, in turn, can be:
Chronic viral hepatitis (B18)
Hepatitis B (viral) NOS
In practice, allocate the following varieties non-viral disease
At the moment, the etiology of each of these pathogens is being studied in detail. In each variety of the disease, genotypes were found - subspecies of viruses. Their distinctive features always has each of them.
Viruses A and E are the least dangerous. Such infectious agents are transmitted through contaminated drink and food, dirty hands. A month or one and a half is the period of cure for these varieties of jaundice. The most dangerous are viruses B and C. These insidious pathogens of jaundice are transmitted sexually, but more often through the blood.This leads to the development of severe chronic hepatitis B (ICD-10 code B18.1). Viral C jaundice (CVHC) is often asymptomatic until the age of 15 years. The destructive process gradually occurs in the body of a patient with chronic hepatitis C (ICD code B18.2). Hepatitis, unspecified, lasts for at least six months.
If a pathological inflammatory process develops for more than 6 months, it is diagnosed chronic form diseases. Wherein clinical picture not always pronounced. Chronic viral hepatitis proceeds gradually. This form often leads to the development of cirrhosis of the liver if not properly treated. The described organ of the patient increases, the appearance of its soreness is observed.
The mechanism and symptoms of the development of the disease
The main multifunctional liver cells are hepatocytes, which play a major role in the functioning of this exocrine gland. It is they who become the target of hepatitis viruses and are affected by pathogens of the disease. Functional and anatomical damage to the liver develops. This leads to severe disorders in the patient's body.A rapidly developing pathological process is an acute hepatitis, which is in international classification diseases of the tenth revision under the following codes:
- acute form A - B15;
- acute form B - B16;
- acute form C - B17.1;
- acute form E - B17.2.
The blood test is characterized by high numbers of liver enzymes, bilirubin. In short periods of time, jaundice appears, the patient develops signs of intoxication of the body. The disease ends with recovery or chronicity of the process.
Clinical manifestations of the acute form of the disease:
The danger of viral jaundice
Of all the pathologies of the hepatobiliary system, the viral type of the disease most often leads to the development of liver cancer or cirrhosis.
Due to the risk of the formation of the latter, hepatitis is of particular danger. Treatment of these pathologies is extremely difficult. Death in the case of viral hepatitis is often observed.