Selective IGA deficiency in children. The electoral deficiency of immunoglobulin A. Tolerance and the ability to distinguish "its" and "alien" is vital conditions for preventing reactions directed against its own cells and tissues, while maintaining times
Among the well-known immunodeficiency states, the selective deficiency of immunoglobulin A (IGA) is most often occurring in the population. In Europe, its frequency is 1/400-1 / 600 people, in the countries of Asia and Africa, the frequency of occurrence is somewhat lower.
Pathogenesis of the selective deficit of immunoglobulin A
The molecular genetic foundations of IgA-deficiency are still not known. It is assumed that the defect pathogenesis lies a functional defect in cells, which, in particular, indicates a decrease in IGA-expressing in cells in patients with this syndrome. It is shown that these patients have many LGA-positive in lymphocytes have an immature phenotype, expressing IGA and IGD simultaneously. This is probably due to the defect of factors affecting the functional aspects of the expression and IGA synthesis in cells. We will help to be defects both in the production of cytokines and violations in the response into cells on various mediators immune system. The role of such cytokines such as TGF-B1, IL-5, IL-10, as well as the CD40-CD40 ligand systems is considered.
Most cases of IGA-deficit occur sporadically, but married cases where the defect is traced in many generations. Thus, the literature describes 88 family cases of IgA-deficiency. An autosomal-recessive and autosomal dominant forms of inheritance of the defect, as well as an autosomal-dominant form with incomplete expression of the feature. In 20 families, different members have met at the same time selective IGA-deficiency and total variable failure (OVIN), which involves the generality of a molecular defect with these two immunodeficiency states, recently researchers are increasingly strengthened in the opinion that the selective IGA and Ovin deficiency are phenotypic manifestations The same, as yet revealed, genetic defect. Due to the fact that the gene suffering from IgA-deficiency is not known, is investigated by several chromosomes, the damage of which is expected to be involved in this process.
The main focus is drawn to 6 chromosome, where the genes of the main histocompatibility complex are located. 8 some of the works are indicated to the involvement of MNS III genes in the pathogenesis of IGA deficiency.
Deletions of the short shoulder 18 chromosomes are found in half cases of IgA-deficiencies, however, the accurate localization of the breakdown in most patients is not described. In other cases, studies have shown that the localization of the deletion of the shoulder 18 of the chromosome does not correlate with the phenotypic weight of the immunodeficiency.
Symptoms of selective immunoglobulin deficiency A
Despite the greatest prevalence of such immunodeficiency, as selective IGA deficiency, often people have no clinical manifestations. It is probably due to the various compensatory capabilities of the immune system, although today this question remains open. With a clinically pronounced selective deficiency IGA, the main manifestations are broncho-pulmonary, allergic, gastroenterological and autoimmune diseases.
Infectious symptoms
In some studies, it is noted that infections respiratory tract More often found in patients with IGA deficiency and reduced or missing secretory IGM. HE is excluded that only the combination of IgA deficiency and one or more IgG subclasses, which is found in 25% of cases in patients with IgA-deficiency leads to serious bronchopile diseases.
Most often, diseases associated with IGA-deficit are infections of the upper and lower respiratory tract departments, mainly the pathogens of infections in such cases are bacteria with a small pathogenicity: Moraxella Catharalis, Streptococcus Pneumonia, Hemophilus Influenzae,often causing these patients otitis, sinusites, conjunctivities, bronchitis and pneumonia. There are reports that the clinical manifestation of IGA deficiency requires a shortage of one or more IgG subclasses, which is found in 25% of IGA-deficiency cases. Such a defect leads to serious bronchopile diseases, such as frequent pneumonia, chronic obstructive lung diseases, chronic bronchitis, bronchiectase. The most unfavorable is the combined deficiency of IGA and IgG2 subclasses, which, unfortunately, is most often found.
Patients with selective deficiency IGA often suffer from various gastrointestinal diseases of both infectious and non-infectious genesis. So, among these patients, infected Gardia Lamblia(giardiasis). Non-blind and others intestinal infections. Probably, a decrease in the secretory IGA, which is part of the local immunite, leads to more frequent infection and reproduction of microorganisms in the intestinal epitheliums, as well as to frequent reinfection after adequate treatment. The consequence of chronic intestinal infection is often a lymphoid hyperplasia, accompanied by Malabsorption syndrome.
Loosity of the gastro
Lactose intolerance is also more common than in the overall population, it is found in the selective deficiency of IGA. Various diarrhea associated with IGA deficiency, the nodular lymphoid hyperplasia and Malabsorbzyl are usually poorly treatable.
The frequent combination of celiac disease and the deficiency of Iga deserves attention. Approximately 1 in 200 patients with celiac disease have this immunological defect (14.26). This association is unique, as the association of gluten-eneopathy has not yet been identified with any other immunodeficities. The combination of IGA-deficiency with autoimmune diseases gastrointestinal tract. Often there are such conditions as chronic hepatitis, billiard cirrhosis, pernicious anemia, ulcerative colitis and enteritis.
Allergic diseases
Most clinicians believe that IGA deficiency is accompanied by an increased frequency of almost the entire spectrum of allergic manifestations. it allergic rhinitis, conjunctivitis, urticaria, atopic dermatitis, bronchial asthma. Many specialists argue that the bronchial asthma in these patients has a more refractory current, which is perhaps due to the development of them infectious diseasesexacerbating asthma symptoms. However, there were no controlled studies on this topic.
Autoimmune pathology
An autoimmune pathology affects not only the gastrointestinal tract of patients with IGA deficiency. Often these patients suffer from rheumatoid arthritis, a systemic red lupus, autoimmune cytopenia.
Anti-IgA antibodies are found in patients with IgA-deficiency in more than 60% of cases. The etiology of this immune process is not fully studied. The presence of these antibodies can determine anaphylactic reactions when overflowing by these patients with IGA-containing blood products, but in practice the frequency of such reactions is sufficiently small and is about 1 per 1,000,000 blood injected drugs.
Diagnostics of the selective deficit of immunoglobulin A
In the study of humoral immunity in children, it is often quite often encountered with a reduced IGA level on the background. normal indicators Igm and IgG. Available iGA transient deficiency,in which serum IGA was shown, as a rule, are in the range of 0.05-0.3 g / l. More often such a state is observed in children under 5 years and is associated with the immaturity of the system of synthesis of immunoglobulins.
For partial deficiency IGAthe level of serum IGA although below the age oscillations (less than two sigmal deviations from the norm), but still does not fall below 0.05 g / l. Many patients with iga's partial deficit have a normal level of secretory IGA in saliva and clinically healthy.
As noted above, the selective deficiency of IgA is spoken at the level of serum IGA below 0.05 g / l. Almost always in such cases is determined by the decline and secretory IGA. The content of IGM and IgG can be normal or less common, elevated. It is often found to reduce individual IgG subclasses, especially IgG2, IgG4.
- A group of primary immunodeficiency states, which are due to a synthesis violation or accelerated destruction of the immunoglobulin molecules of this class. Symptoms of the disease are frequent bacterial infections (especially respiratory system Both ENT organs), disorders from the gastrointestinal tract, allergies and autoimmune lesions. The diagnosis of the deficit of immunoglobulin A is produced by determining its amount in serum, molecular genetic techniques are also used. The treatment is symptomatic, reduces to prevention and timely therapy bacterial infections and other violations. In some cases, replacement immunoglobulin therapy is carried out.

General
The deficiency of immunoglobulin A is the polyethological form of the primary immunodeficiency in which the lack of this class of immunoglobulins is observed when normal content other classes (G, M). The deficiency can be complete, with a sharp decline in all fractions of globulin A, and selective, with a disadvantage of only certain subclasses of these molecules. Selective deficiency of immunoglobulin A is a very common state, according to some data, its occurrence is 1: 400-600. The phenomena of immunodeficiency in the selective disadvantage of the compound is quite erased, almost two thirds of patients are not diagnosed with, because they do not seek medical help. Immunology doctors found that immunoglobulin deficiency A can manifest itself not only by infectious symptoms, patients also often observe exchange and autoimmune disorders. With this circumstance, it can be assumed that the occurrence of this state is even higher than previously expected. Modern genetics believe that the disease arises sporadically or is hereditary pathology, and as a transmission mechanism, both an autosomal dominant and autosomal-recessive path of inheritance can act as an autosomal-dominant.

Causes of Immunoglobulin's deficiency
Etiology and pathogenesis of both complete and selective immunoglobulin deficiencies and to date are not fully defined. Until only genetically molecular mechanisms for individual forms of the disease were able to establish. For example, a selective deficiency of Immunoglobulin A Type 2 is due to mutations of the NFRSF13B gene, localized on the 17th chromosome and encoder of the same name. This protein is a transmembrane receptor on the surface of B-lymphocytes, is responsible for recognizing the factor of necrosis of tumors and some other immunocompetent molecules. The compound is actively involved in the regulation of the intensity of the immune response and secretion of different classes of immunoglobulins. According to molecular studies, the genetic defect of the TNFRSF13B gene, leading to the development of an abnormal receptor, makes certain fractions of the in-lymphocytes functionally immature. Such cells instead of the production of optimal amounts of immunoglobulins A, a mixture of classes A and D, which leads to a decrease in the concentration of class A.
The TNFRSF13B gene mutations are common, but far from the only reason for the development of immunoglobulin A. During the absence of damage to this gene, and under the existing clinical manifestations of the immunodeficiency of this type, there are assumed mutations in the 6th chromosome, where the genes of the main histocompatibility complex (GKGS) are located. In addition, in a number of patients with a deficit of immunoglobulin, a short shoulder deletions of the 18th chromosome are observed, but it is not possible to unambiguously connect these two circumstances with each other. Sometimes the lack of class A molecules is combined with a deficiency of immunoglobulins of other classes and a violation of the activity of T-lymphocytes, which forms a clinical picture of the total variable immunodeficiency (OID). Some genetic doctors suggest that Immunoglobulin A and OID deficiency are provoked by very similar or identical genetic defects.
Immunoglobulin, but differs from other related molecules in that due to the very first stage of non-specific immunological protection of the body, since it is allocated as part of the secrets of the mucous membranes. With its lack of pathogenic microorganisms it becomes easier to be introduced into weakly protected gentle tissues of the mucous respiratory tract, the gastrointestinal tract and LOR organs. The mechanisms of autoimmune, exchange and allergic disorders during the deficiency of immunoglobulin are still unknown. There is an assumption that its low concentration makes an imbalance into the entire immune system.
Symptoms of immunoglobulin deficiency
All manifestations of the deficiency of immunoglobulin A in immunology are divided into infectious, exchange (or gastrointestinal), autoimmune and allergic. Infectious symptoms Enclosed in an increased frequency of bacterial infections of the respiratory tract - in patients often arise laryngitis, trachetes, bronchitis and pneumonia, which can take a serious flow and accompanied by the development of complications. In addition, for the deficiency of immunoglobulin A characterized by a quick transition of sharp inflammatory processes in chronic formsIt is especially indicative regarding the lesions of the ENT organs - the patients are often diagnosed with otitis, sinusitis and frontitles. A sufficiently common combined deficiency of immunoglobulins A and G2 leads to severe obstructive lung lesions.
To a lesser extent, infectious damage affect the gastrointestinal tract. With a deficiency of immunoglobulin, there is some increase in giardiasis, gastritis and enteritis can be recorded. The most characteristic of this immunodeficiency symptoms of the GTS are lactose intolerance and celiac disease (immunity of cereal gluten protein), which, in the absence of nutritional correction, can lead to intestinal naval atrophy and malabsorption syndrome. Among the patients with deficiency of immunoglobulin, ulcerative colitis, biliary cirrhosis of the liver and chronic hepatitis of autoimmune genesis are also often recorded. The listed diseases are accompanied by pain in the abdomen, frequent episodes of diarrhea, weight loss and hypovitaminosis (due to disruption of the absorption of nutrients due to malabsorption).
In addition to the above-described diseases of the gastrointestinal tract, autoimmune and allergic lesions with an immunoglobulin deficiency and manifest themselves the increased frequency of the development of the systemic red lupus and rheumatoid arthritis. Thrombocytopenic purpura and autoimmune hemolytic anemia are also possible, often with a difficult course. More than half of the patients in the blood, the autoantibodies are determined against their own immunoglobulin A, which further aggravates the phenomenon of a lack of this compound. In patients with a deficit of immunoglobulin, and often reveal by urban, atopic dermatitis, bronchial asthma and other diseases of allergic origin.
Diagnosis of immunoglobulin deficiency
Diagnosis of the deficit of immunoglobulin A is made on the basis of the data of the patient's disease history ( frequent infections The respiratory tract and ENT organs, the gastrointestinal lesions), but the most accurate way to confirm the diagnosis is to determine the amount of serum immunoglobulins of different classes. In this case, an isolated decrease in this component of the humoral immunity can be detected below 0.05 g / l, which indicates its deficiency. Against this background, the level of immunoglobulins G and M remains within the normal range, the decrease in the G2 fraction is sometimes revealed. With a partial deficit of immunoglobulin, its concentration remains in the range of 0.05-0.2 g / l. When evaluating the results of the analysis, it is important to remember age features The number of globulins in the plasma of blood - for example, the concentration of fraction A 0.05-0.3 g / l in children under 5 years of age is the name of the transient deficit and can disappear later.
Sometimes the partial deficiency of immunoglobulin A is found, at which its plasma amount is reduced, but the concentration of the compound in the discharge of mucous membranes is sufficiently high. Nic clinical symptoms Diseases in patients with partial deficit are not detected. In the immunogram, attention should be paid to the number and functional activity of immunocompetent cells. With an immunoglobulin deficiency and the number of T- and B lymphocytes is usually saved on normal levelA decrease in the number of T-lymphocytes indicates the possible availability of the total variable immunodeficiency. Among other diagnostic methods, a supporting role is played by the definition in the plasma of antinuclear and other autoantibodes, automatic sequencing of the TNFRSF13B gene and allergological samples.
Treatment, forecast and prevention of immunoglobulin deficiency
No specific treatment of this immunodeficiency is absent, in some cases reactive immunoglobulin therapy. Basically use antibiotics to treat bacterial infections, sometimes prescribed antibacterial preventive courses. Correction of diet (elimination of hazardous products) is necessary in the development of food allergies and celiac disease. In the latter case, exclude dishes based on cereals. Bronchial asthma and other allergic pathologies are treated with generally accepted drugs - antihistamine and bronchodiolitical means. In pronounced autoimmune disorders, immunosuppressive drugs are prescribed - corticosteroids and cytostatics.
The forecast for the deficiency of immunoglobulin is generally favorable. In many patients, pathology proceeds absolutely asymptomatic and does not require special treatment. With increasing the frequency of bacterial infections, autoimmune lesions and absorption disorders (Malabsorption syndrome), the forecast can deteriorate accordingly with the severity of symptoms. To prevent the development of these manifestations, it is necessary to use antibiotics at the first signs of the infectious process, compliance with the rules regarding the power regime and the composition of the diet, regular monitoring of the immunologist and doctors of other specialties (depending on the accompanying violations). Care should be taken when overflowing whole blood or its components - in rare cases, patients have an anaphylactic reaction due to the presence in the blood of autoantibodies to Immunoglobulin A.
Clinical case
UDC 612.017: 615.37
Diagnosis and treatment of primary immunodeficiency state: selective immunoglobulin deficiency
The article presents the current aspects of the diagnosis of the most common primary immunodeficification state: selective immunoglobulin deficiency A. Early diagnosis and adequate therapy allow you to achieve stable general status patients with a given disease. Due to the low alertness of the primary regimens with respect to primary immunodeficiency, there is hypodiagnosis of diseases, as well as high inva-lidization caused by infectious complications.
Keywords: primary immunodeficiency state, selective deficiency of immunoglobulin A, imminent hyumoral defects.
To date, about 150 are described. clinical shapes Primary immo-modiform states. At the same time, for more than 130 of them, gene defects are defined. Of all the primary immunodeficiency states (PIDS), selective immunoglobulin deficiency and meets most often.
Graber and Williams were the first to have identified and studied Immunoglobulin A (IGA) in 1952. IgA differs from other classes of immunoglobulins in the content of carbohydrates, silic acids and the ability to create dimers, trimers and tetrame-ry. Serum IGA is always a monomer, and secretory IgA (SIGA) is combined into 2, 3 or 4 molecules by means of the J-chain and serves to protect the mucous membranes, becoming a part of tears, breast milk, secrets of digestive, respiratory and urinary tracts. The overall deficiency of IGA is associated with the anomalies of the synthesis of the monomer, which ultimately leads to a decrease in and serum and SIGA. In some cases, the defect can be implemented at the level of the J-chain and then only SIGA is missing. Siga infants appear in 3 months after birth, and the optimal concentration is set to 2-4 years. The plasma level of IGA to 6 monthly age is about 1/3 of the index of adults, and reaches a maximum of 10-12 years.
Selective IGA deficiency is equally common in men and women. Most of the cases of selective IGA deficiency are sporadic, there are also descriptions of family diseases. Inheritance in these cases occurs in an autosomal-recessive type, an autosomal-dominant, multi-factorial and polygenic with incomplete expression of inheritance types are also described.
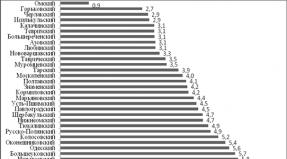
For the first time, the selective IGA deficiency was described by J. Heremans in 1960-1961. According to researchers with such immunopathology, 1 out of 142-15,000 newborns appears, depending on the ethnic group - in people of the European-like race, much more often, compared with Asian and Negroid. Prevalence
K.A. Bocharov
Belgorod State National Research University
the deficit B1 £; and in Europe varies between 1: 163 and 1: 875. This is at least 150 times more often than another primary immunodeficiency condition - common variable immune failure, which occupies a second line for the prevalence of PIDS. However, in the Russian national register of patients with PIDS, which has existed since 1989, there are information less than 1000 patients with selective deficit 1; a. So currently in Russian Federation Up to 300,000 people with undiagnosed PIDTS can live. Insufficient awareness of doctors about this pathology, the lack of a laboratory base in combination with a relatively rare prevalence and a variety of clinical forms, lead to the fact that patients do not receive a long time pathogenetic therapyAs a result, foci of chronic infection are formed and the forecast of the disease is worse.
A genetic defect that leads to the development of selective deficit 1; and still not known, but there are convincing evidence of its determination at the level of the NGL-system of human histocompatibility system, which leads to a violation of the switching of isotypes by 1; A or ripening cells producing 1; . In patients with congenital deficiency 1; and often a1, B8 and bump nyl-haplotypes are detected. But not only the genes of the main histocompatibility complex can be involved in the pathogenesis of congenital hypo-1; a. It is reported about the possible association of this pathology with G1N1 and Ciez16a.
The pathogenesis of the disease is the subject of close study, but the results obtained do not suggest a single development mechanism. During selective deficiency 1; A, the terminal differentiation of B-lymphocytes is disturbed, secretion is blocked 1; but, which may be a consequence of a decrease in expression of the SB receptor on B-lymphocytes (participates in cooperative interaction with antigen presenting cells and T-helpers when initiating synthesis 1; a) . A specific role in the pathogenesis is given by TFR-P, which is the main factor in the induction of synthesis 1; a. It is considered possible to distinguish an answer to inter-leukinam 4, 6, 7, 10. It is shown that the addition of interleukin 10, especially in combination with interleukin 4 in the culture of lymphocytes from patients with selective deficiency 1; but causes the restoration of the secretion of this immunoglobulin.
Clinical picture Selective deficiency 1; and heterogeneous. Deficiency of secretory 1; A, as factor in local immunity and protect the mucous membranes, protecting antibodies from the action of enzymes and the participating in their transportation, is clinically manifested by chronic diarrhea, frequent respiratory infections. It rarely meets a special option 1; A-deficiency - severe a-chain disease or the so-called "Mediterranean lymphoma", which is manifested by Malabsorption syndrome and severe dystrophy, due to lymphogranulomatosing intestinal lesion.
With a general failure of 1; A, depending on the prevailing lesion, the following flow options are distinguished:
Asymptomatic (laboratory find)
PRESENTAL BEAUTION OF THE BEYING SYSTEM
Preferential defeat of the gastrointestinal tract
Autoimmune diseases.
Oncopathology is not allocated in a separate course of the flow, since the frequency of development and pathogenesis of tumor growth in patients with selective deficiency is not established in patients with selective deficiency 1; a. Timoma, lymphoma, stomach cancer, esophagus, lungs are most often diagnosed.
In 60-70% of people, the manifestations of the selective deficit 1 are not developing throughout life; and the diagnosis is made exclusively according to the results of a re-laboratory study. The manifestic form is characterized by recurrent bacterial and viral infections of the ENT organs, the respiratory system and the gastrointestinal tract. Clinical manifestations often start
based after the cessation of breastfeeding, but they can begin at a later age.
Infectious syndrome has a number of features:
Heavy and invasive infections are not characterized (septicemia, meningitis, osteomyelitis), chronic respiratory tract infections (with an isolated selective deficiency 1; a);
A relatively light course and a favorable outcome of the disease (relative to other congenital immunodeficiency), due to compensatory activation of the synthesis 1; m, 1 £; 0 and congenital immunity;
The predominance of viral infections of the respiratory tract;
Next to diseases of the gastrointestinal tract.
Currently, it is believed that the occurrence of recurrent infections in patients with selective deficiency 1; but is due to the concomitant defects of the immune system, such as the deficiency of subclass 1; 0 (especially 1; 02), the defect of the man-nose-binding lectin, specific antibodies to polysaccharides.
For the defeat of the respiratory tract, otitis, sinusites and bronchitis, more often than viral etiology. From bacteria more often than others cause streptococci infection and hemophilic wand. The chronization of pathology and bronchiectatic disease is formed mainly with combined defects of humoral immunity - selective deficiency 1; A and the deficiency of sub-grades 1; 0.
The gastrointestinal tract is the longest lymphoid organism of the human body, so the clinical manifestations of lesions at PIDS are quite often detected. A variant of selective deficiency 1; and with the predominance of the lesion of the gastrointestinal tract is manifested by the development of herpetic agent and ulcerative stomatitis, hypertrophic gastritis, celiac disease, cholecystocholangitis, regional enteritis, ileit, hemorrhagic and nonspecific ulcerative colitis, diseases of the crown, nodular lymphoid hyperplasia, malabsorption, Muko-Vysocidoza. In this case, the histologically revealed atrophy of the bowl of the intestines. Most often, this group of patients is revealed by the Giardia of Azhai, although the clinical manifestations of the infection may not be, or symptoms do not appear brightly and are chronic.
Allergic diseases in patients with selective deficit 1; and do not have clinical features and proceed in the form of bronchial asthma, rhinitis, conjunctivitis, atopic dermatitis, urticaria and swelling swelling. Early manifestations are more often due to symptoms of food allergies. More than half of children, the intolerance to the cow's milk, induced by circulation of precipiti antibodies to the protein of cow's milk, is revealed. The antibodies to gluten appear relatively often.
With selective deficiency 1; and with a predominance of autoimmune pathology in serum, autoantibodes are found to nuclear proteins, cardiolipin, smooth muscles cells, thyroid microsomal antigens, thyroglobu-lin, basal membrane, adrenal cells, red blood cells and other circulating blood cells. Often diagnosed rheumatoid arthritis, dermatomyosit, thyroiditis, systemic red lupus, vitiligo, idiopathic thrombocytopeni-husty purple, hemolytic anemia . It is important to remember that even in asymptomatic patients with selective deficiency 1; and antibodies can appear to 1; and that when blood transfusion, plasma or administration of immunoglobulin drugs can cause post-transfusion reactions induced by the formation of immune complexes.
One of the laboratory features of the screening of patients with selective deficiency 1; but is the likelihood of a positive result of immuno-enzyme analysis into a p-chorionic gonadotropin of a person (a false positive test for pregnancy), due to the presence of heterophilic antibodies.
Selective deficiency 1; but is diagnosed after re-examining serum. Partial deficiency 1; and is exhibited at its concentration ranging from 0.05 to 0.2 g / l. Absence of 1; and newborns speak or about immaturity
munch system or the probability of selective deficiency 1; a. In early age children, more often in boys, there is a transient deficiency 1; and or its subclasses. If 1; and is not determined after the one-monthly age, then the diagnosis of selective deficiency 1; and does not cause doubt.
Thus, in children until the year, the diagnostic criterion of selective deficiency 1; and are indicators less than 0.05 g / l, the absence of 1; A1 and 1; A2, B1; and with normal content 1; m and 1; 0 (except 1; 02), the exclusion of other causes of hypogamag-lobulinemia and other PIDTS options. The content of cells of the immune system (T and B-lymphocytes, KK cells, phagocytes) in patients with selective deficiency 1; and usually within the normal range. In children over 4 years old, the diagnostic criterion is a concentration of 1; a less than 0.07 g / l.
Using a row medicinal preparations, such as b-penicillamine, sulfasalazine, captopril, carbamazepine, ibuprofen and valproic acid can lead to a reversible decrease in concentration 1; a. In addition, some diseases induce a temporary decrease of 1; A (cytomegalovirus infection, toxo plasmosis, rubella). Seasonal increase of 1; and may be celebrated during the winter months. Listed factors should be taken into account when making a diagnosis.
All patients with selective deficiency 1; and long-term monitoring of immunoglobulin concentrations, autoantibodite, 1; 0 and 1; E to food, domestic, epidermal fungal and pollen allergens are required. It is possible to gradual transformation of selective deficiency 1; and in general variable immune failure ^]. Upon exposure to adverse factors of the outer environment, the asymptomatic flow can change the infectious syndrome, autoimmune and allergic reactions, Maligination. The forecast of the disease also depends on the concomitant immunopathology.
The presence of selective deficit 1; and is not a contraindication to vaccination. However, post-specific immunity may be insufficient.
Asymptomatic course of the disease does not need therapy. Cure selective deficiency 1; and it does not seem possible. Treatment is pathogenetic and symptomatic character, aims to relieve infectious, allergic and autoimmune syndrome. Immunomodulators do not lead to meaningful and for some long-term effect. Restaurant immunotherapy is required by patients with infectious syndrome and is carried out by the drugs of immunoglobulins that do not contain 1; but, only after laboratory confirmation of the absence of anti-1; and antibodies. Commercial preparations contain trace amounts 1; A, which are sufficient to sensitize patients to 1; but, which may in turn lead the formation of anti-1; and antibodies and in rare cases induces anaphylactic reactions. Commercial immunoglobulins for intramuscular administration have almost ceased to be used after the appearance of intravenous immunoglobulins that have proven more efficient and safe. Unwanted drug reactions to intravenously injected immunoglobulins are recorded in 5-15% of cases. Immunoglobulin preparations help to stop a number of symptoms, contribute to the elimination of the pathogen, modulate the immune response and enhance phagocytosis. In addition to intravenous, in the global pharmaceutical market there are and administered subcutaneously drugs of immunoglobulins that have their advantages. First of all - this is the lack of necessity venous access and the possibility of conducting the procedure at home, which is especially important in pediatric practice, as well as a reduction in the frequency of system adverse Reactions. Smaller invasiveness of the procedure allows you to carry out more frequent transfusions (one or several times per week) smaller doses, which maintains the concentration of serum immunoglobulin at a relatively constant level. The disadvantages of such drugs include the inability to quickly introduce high doses and slow increase in level 1; 0 in the blood.
With infections of the respiratory and gastrointestinal tract with prophylactic and therapeutic goal Antibiotics apply. Routine schemes are used
appointments of antibacterial therapy, as well as other drugs used to relieve allergic and autoimmune syndromes.
Clinical case.
Anamnesis of life. Boy I., 1997 The child from the first pregnancy, which occurred with pyelonephritis in 2 trimester, urgent delivery with the cordial of the umbilical cord, weighing 3780 g, 53 cm. Physical and neuropsychic development corresponded to age. Preventive vaccinations - by calendar, without complications. IN early age - Moderate manifestations of atopic dermatitis. Up to 3 years - uncomplicated acute respiratory infections, up to eight times a year. From September 2001, he began to attend kindergarten.
Family history is not burdened.
Anamnesis of the disease. The clinical debut of the disease - since 2000 (at the age of 3 years). In February 2000 he entered the hospital, where he was on the treatment with a diagnosis: double-sided polysegenic pneumonia. Massive was carried out antibacterial therapy, transfusion of intravenous immunoglobulin (without determining the level of serum immunoglobulins). Disposable with improved state, with the absence of inflammatory infiltration by radiological data. It continued to disturb the frequent parlor cough, accompanied by an abundance of dry wheels, periodically disturbed the nasal congestion and sneezing. In July 2000, a diagnosis of bronchial asthma was made, basic therapy began in inhalation glucocorticosteroids through a nebulizer, bronchoditics with attacks. In the immunological examination in 2001, a sharp decrease in IGA was revealed (<0,05 г/л), выставлен диагноз - первичное иммунодефицитное состояние: селективный дефицит IgA. С весны 2001 года на фоне проводимой терапии приступы беспокоили несколько раз в месяц, назначен флуконазол в дозе 250 мкг в сутки, короткодействующие в2-агонисты при приступах. Приступы по несколько раз в месяц сохранялись, тяжёлые приступы в декабре 2001, январе - апреле, июне 2002 года. В июне 2002 года в связи с сохраняющейся и нарастающей заложенностью носа была проведена аденотомия, но в послеоперационном периоде заложенность носа сохранялась. С августа 2002 года к базисной терапии добавлен сальметерол 100 мкг в сутки, доза флуконазола составляла 250 мкг в сутки. На фоне терапии в декабре 2003 года тяжёлый приступ, доза флуконазола увеличена до 500 мкг в сутки, продолжен приём сальметерола, к апрелю 2004 года доза флуконазола снижена до 200 мкг в сутки. В настоящее время базисная терапия составляет: флу-коназол 500-750 мкг в сутки, сальметерол 100 мкг в сутки, сингуляр 5 мг.
Against the background of the therapy, the episodes of the parole cough, difficulty breathing 1-2 times a week, requiring additional inhalations of short-range B2-agonists. In January 2008, against the background of ARVI, a severe exacerbation of asthma was noted, requiring the purpose of prednisolone PER OS at a dose of 1 mg / kg, short-range inhalation broutine, euphilline, antibacterial therapy was carried out within 10 days. The incidence of sharp respiratory infections throughout the entire period of observation is 1-2 times a month (including rinopharygitis, hymorites (3)). Regarding which the child receives courses of antibacterial preparations of a wide range of action up to 6 times a year. With repeated immunological surveys, the resistant reduction in IGA indicators is preserved.<0,05 г/л.
In the clinic of the disease of the patient I. attracts attention to infectious and broncho-abstructive syndromes: pneumonia, sinusitis, often recurrent Ori, worsening the course of the bronchological syndrome, poorly amenable to control the broncho-abstructive syndrome, a frequent need for antibacterial therapy. All this forces it to consider the question of the presence of a primary immunodeficiency state at the child, you can assume the presence of an IGA deficiency child. The differential diagnosis was carried out with congenital defects of the mukiciliar mechanism, cystic fibrosis, common variable immune failure.
Studies (study of the concentration of blood serum immunoglobulins, determining the number of lymphocytes) confirmed the absence of an IGA child<0,05 г/л, остальные показатели иммунограммы в пределах возрастных норм.
Patients with clinically manifested selective IGA immunodeficiency need careful observation of the immunologist, with the development of severe infections on life testimony in substitution therapy of intravenous immunoglobulin drugs and preventive anitbacterial therapy in the presence of chronic foci of infection.
From the moment of the diagnosis of the child, I. receives basic therapy of bronchial asthma according to recommendations and regular coursework preventive antibacterial therapy. Against the background of the therapy, there is a stable general condition, some regression of the broncho-prestructive syndrome.
Forecast of the disease. With early diagnosis and early adequate therapy, the prognosis of patients with selective deficiency IgA is favorable. In most cases, against the background of therapy, patients lead a normal lifestyle and live to elderly. The forecast is significantly worsening at the late diagnosis and development of chronic infection foci. In this case, the forecast is due to the volume of damage in the internal organs.
In conclusion, one should once again note the need for early diagnosis of primary immunodeficiency states, when irreversible changes in various organs and tissues affected by persistent infection have not yet been formed. Thus, in front of general practitioners is an important task of the timely direction of patients to examine in the conditions of specialized departments and further adequate dispensary observation in the event of confirming the diagnosis.
Literature
1. Kovalchuk, L.V. Clinical immunology and allergology with the basics of general immutation. / L.V. Kovalchuk, L.V. Gankovskaya, R.Ya. Meshkova // Gootar Media, 2011. 640 p.
2. Kondratenko, I.V. Primary immunodeficials / I.V. Kontdrenko, A.A. Babogov. M.: Medpraktika-M, 2005. - 233 p.
3. Shcherbina, A.Yu. Immunodeficiency States / Shcherbina A.Yu., Sodteus A.P., Rumyantsev A.G. // Difficult patient. - 2007. - T.5, №2. - P. 5-10.
4. Agarwal S., MAYER L. Pathogenesis and Treatment of Gastrointestinal Disease in Antibody Deficiency Syndromes./ S. Agarwal, L. Mayer // J Allergy Clin Immunol. 2009 Oct; 124 (4): 658-64.
5. Azar, A.E. Evaluation of the adult with suspected immunodeficiency. Am j Med. 2007; 120 (9): 764-768.
6. Ballow, M. Primary Immunodeficiency Diseases. In: Goldman L, Ausiello D, EDS. Cecil Medicine. 23rd ED. Philadelphia, PA: Saunders Elsevier; 2007: CHAP 271.
7. Low Prevalence of Iga Deficiency in North Indian Population./ S. Chandran // Indian J Med Res. 2006 May; 123 (5): 653-6.
8. DRIESSEN, G. EDUCATIONAL PAPER. Primary Antibody DeficIencies./ G. Driessen, Van der Burg M. // EUR J PediaTr. 2011 June; 170 (6): 693-702.
9. Update On The Treatment of Primary ImmunodeFicIencies. Allergol Immunopathol (MADR) ./ J.M. Garcia // 2007 SEP-Oct; 35 (5): 184-92.
10.Allele * 1 of HS1.2 Enhancer Associates with Selective Iga Deficiency and Igm Concentration./ V. Giambra // J Immunol. 2009 DEC 15; 183 (12): 8280-5.
11. Selective Deficiency Of Immunoglobulin A Among Healthy Voluntary Blood Donors in Iran. Blood TRANSFUS./ R. Houri // 2009 APRIL; 7 (2): 152-154.
12. Class Switch Recombination in Selective Iga-Deficient Subjects Clin Exp Immunol./ L. Hummelshoj // 2006 June; 144 (3): 458-466.
13. Frequent False Positive Beta Human Chorionic Gonadotropin Tests in Immunoglobulin A Deficiency./ A.K. KNIGHT // Clin Exp Immunol. 2005 August; 141 (2): 333-337.
14. McGowan, K.E. Celiac Disease and Iga Deficiency: Complications of Serological Testing Approaches Encountered in the Clinic. Clin Chem./ K.E. McGowan, M.E. Lyon, J.D. Butzner // 2008 Jul; 54 (7): 1203-9. EPUB 2008 may 16.
15. PRIMARY IMMUNODEFICIENCIES OF THE B LYMPHOCYTE./ A. MOISE // J Med Life. 2010 February 15; 3 (1): 60-63.
16. Morimoto, Y. ImmunodeFiciency Overview./ Y. Morimoto // Prim Care. 2008; 35 (1): 159-
17. Development of Cancer in Patients with Primary ImmunodeFicIencies./ K. Salavora // Anticancer Res. 2008 Mar-Apr; 28 (2b): 1263-9.
18. Stein, M. R. The New Generation of Liquid Intravenous Immunoglobulin Formulations In Patient Care: A Comparison of Intravenous Immunoglobulins./m.r. Stein // Postgrad Med. 2010 SEP; I22 (5): I76-84.
19. Stiehm, E.R. The Four Most Common Pediatric ImmunodeFicIencies./e.r. Stiehm // j im-munotoxicol. 2008 APR; 5 (2): 227-34.
20. Various Expression Patterns of Alphai and Alpha2 Genes in Iga Deficiency./ H. Suzuki // Allergol int. 2009 Mar; 58 (i): III-7. EPUB 2009 Jan 25.
21. Selective Immunoglobulin A Deficiency and Celiac Disease: Let "S Give Serology A CHANCE / E. Valletta // J Investig Allergol Clin Immunol. 20ii; 2i (3): 242-4.
22.Selective Iga Deficiency in Autoimmune Diseases./ N. Wang // MOL MED. 2011 Aug 4. DOI: I0.2II9 / Molmed.20ii.00i95.
Diagnostics and Management of Primary Immunodeficiency Disease:
The Selective Iga-Deficiency
Belgorod National Research University
e-mail: [Email Protected]
The CONTEMPORARY ASPECTS OF PRIMARY IMMUNODEFICIENCY DISEASE: Selective Iga-Deficiency Performed in Update. The Early Diagnostics and Sufficient Therapy of Primary Immunodeficiency Disease Makes It Possible to Get Stable Common Status In This Patients. But Because with Bad Information Among Pediatricians and General Practitioners About Primary Immunodeficiency Disease: Selective Iga-Deficiency, There Is A A A Lot Of Disabled Persons In Such Patients Caused by Infectious Complications.
Key Words: Primary ImmunodeFiciency Disease, Selective Iga-Deficiency, T Cells, B Cells, Innate Immunity.
- A group of primary immunodeficiency states, which are due to a synthesis violation or accelerated destruction of the immunoglobulin molecules of this class. Symptoms of the disease are frequent bacterial infections (especially respiratory system and LOR organs), disorders from the gastrointestinal tract, allergies and autoimmune lesions. The diagnosis of the deficit of immunoglobulin A is produced by determining its amount in serum, molecular genetic techniques are also used. The treatment is symptomatic, reduces to the prevention and timely therapy of bacterial infections and other violations. In some cases, replacement immunoglobulin therapy is carried out.

General
Immunoglobulin A - polyethological form of primary immunodeficiency, in which there is a lack of this class of immunoglobulins in the normal content of other classes (G, M). The deficiency can be complete, with a sharp decline in all fractions of globulin A, and selective, with a disadvantage of only certain subclasses of these molecules. Selective deficiency of immunoglobulin A is a very common state, according to some data, its occurrence is 1: 400-600. Immunodeficiency phenomena with a selective disadvantage of the compound is quite erased, almost two-thirds of patients disease is not diagnosed, as they do not seek medical help. Immunology doctors found that immunoglobulin deficiency A can manifest itself not only by infectious symptoms, patients also often observe exchange and autoimmune disorders. With this circumstance, it can be assumed that the occurrence of this state is even higher than previously expected. Modern geneticists believe that the disease arises sporadically or is a hereditary pathology, and as a mechanism of transmission can act as an autosomal dominant and autosomal-recessive path of inheritance.

Causes of Immunoglobulin's deficiency
Etiology and pathogenesis of both complete and selective immunoglobulin deficiencies and to date are not fully defined. Until only genetically molecular mechanisms for individual forms of the disease were able to establish. For example, a selective deficiency of Immunoglobulin A Type 2 is due to mutations of the NFRSF13B gene, localized on the 17th chromosome and encoder of the same name. This protein is a transmembrane receptor on the surface of B-lymphocytes, is responsible for recognizing the factor of necrosis of tumors and some other immunocompetent molecules. The compound is actively involved in the regulation of the intensity of the immune response and secretion of different classes of immunoglobulins. According to molecular studies, the genetic defect of the TNFRSF13B gene, leading to the development of an abnormal receptor, makes certain fractions of the in-lymphocytes functionally immature. Such cells instead of the production of optimal amounts of immunoglobulins A, a mixture of classes A and D, which leads to a decrease in the concentration of class A.
The TNFRSF13B gene mutations are common, but far from the only reason for the development of immunoglobulin A. During the absence of damage to this gene, and under the existing clinical manifestations of the immunodeficiency of this type, there are assumed mutations in the 6th chromosome, where the genes of the main histocompatibility complex (GKGS) are located. In addition, in a number of patients with a deficit of immunoglobulin, a short shoulder deletions of the 18th chromosome are observed, but it is not possible to unambiguously connect these two circumstances with each other. Sometimes the lack of class A molecules is combined with a deficiency of immunoglobulins of other classes and a violation of the activity of T-lymphocytes, which forms a clinical picture of the total variable immunodeficiency (OID). Some genetic doctors suggest that Immunoglobulin A and OID deficiency are provoked by very similar or identical genetic defects.
Immunoglobulin, but differs from other related molecules in that due to the very first stage of non-specific immunological protection of the body, since it is allocated as part of the secrets of the mucous membranes. With its lack of pathogenic microorganisms it becomes easier to be introduced into weakly protected gentle tissues of the mucous respiratory tract, the gastrointestinal tract and LOR organs. The mechanisms of autoimmune, exchange and allergic disorders during the deficiency of immunoglobulin are still unknown. There is an assumption that its low concentration makes an imbalance into the entire immune system.
Symptoms of immunoglobulin deficiency
All manifestations of the deficiency of immunoglobulin A in immunology are divided into infectious, exchange (or gastrointestinal), autoimmune and allergic. Infectious symptoms are in the increased frequency of bacterial respiratory tract infections - in patients often arise laryngitis, tracheites, bronchitis and pneumonia, which can take a serious flow and accompanied by the development of complications. In addition, for the deficiency of immunoglobulin, but a rapid transition of acute inflammatory processes in chronic forms is characterized, which is especially indicative about the lesions of the ENT-organs - the patients are often diagnosed by otitis, sinters and frontitis. A sufficiently common combined deficiency of immunoglobulins A and G2 leads to severe obstructive lung lesions.
To a lesser extent, infectious damage affect the gastrointestinal tract. With a deficiency of immunoglobulin, there is some increase in giardiasis, gastritis and enteritis can be recorded. The most characteristic of this immunodeficiency symptoms of the GTS are lactose intolerance and celiac disease (immunity of cereal gluten protein), which, in the absence of nutritional correction, can lead to intestinal naval atrophy and malabsorption syndrome. Among the patients with deficiency of immunoglobulin, ulcerative colitis, biliary cirrhosis of the liver and chronic hepatitis of autoimmune genesis are also often recorded. The listed diseases are accompanied by pain in the abdomen, frequent episodes of diarrhea, weight loss and hypovitaminosis (due to disruption of the absorption of nutrients due to malabsorption).
In addition to the above-described diseases of the gastrointestinal tract, autoimmune and allergic lesions with an immunoglobulin deficiency and manifest themselves the increased frequency of the development of the systemic red lupus and rheumatoid arthritis. Thrombocytopenic purpura and autoimmune hemolytic anemia are also possible, often with a difficult course. More than half of the patients in the blood, the autoantibodies are determined against their own immunoglobulin A, which further aggravates the phenomenon of a lack of this compound. In patients with a deficit of immunoglobulin, and often reveal by urban, atopic dermatitis, bronchial asthma and other diseases of allergic origin.
Diagnosis of immunoglobulin deficiency
The diagnosis of immunoglobulin deficiency A is made on the basis of these patient's disease history (frequent respiratory tract infections and LOR organs, gastrointestinal lesions), but the most accurate way to confirm the diagnosis is to determine the amount of serum immunoglobulins of different classes. In this case, an isolated decrease in this component of the humoral immunity can be detected below 0.05 g / l, which indicates its deficiency. Against this background, the level of immunoglobulins G and M remains within the normal range, the decrease in the G2 fraction is sometimes revealed. With a partial deficit of immunoglobulin, its concentration remains in the range of 0.05-0.2 g / l. When evaluating the results of the analysis, it is important to remember about the age features of the number of globulins in the blood plasma - for example, the concentration of fraction A 0.05-0.3 g / l in children under 5 years of age is the name of the transient deficit and can be disappeared later.
Sometimes the partial deficiency of immunoglobulin A is found, at which its plasma amount is reduced, but the concentration of the compound in the discharge of mucous membranes is sufficiently high. No clinical symptoms of the disease in patients with partial deficit are not detected. In the immunogram, attention should be paid to the number and functional activity of immunocompetent cells. With a deficiency of immunoglobulin, a number of T-and B lymphocytes is usually stored at a normal level, a decrease in the amount of T-lymphocytes indicates the possible availability of total variable immunodeficiency. Among other diagnostic methods, a supporting role is played by the definition in the plasma of antinuclear and other autoantibodes, automatic sequencing of the TNFRSF13B gene and allergological samples.
Treatment, forecast and prevention of immunoglobulin deficiency
No specific treatment of this immunodeficiency is absent, in some cases reactive immunoglobulin therapy. Basically use antibiotics to treat bacterial infections, sometimes prescribed antibacterial preventive courses. Correction of diet (elimination of hazardous products) is necessary in the development of food allergies and celiac disease. In the latter case, exclude dishes based on cereals. Bronchial asthma and other allergic pathologies are treated with generally accepted drugs - antihistamine and bronchodiolitical means. In pronounced autoimmune disorders, immunosuppressive drugs are prescribed - corticosteroids and cytostatics.
The forecast for the deficiency of immunoglobulin is generally favorable. In many patients, pathology proceeds absolutely asymptomatic and does not require special treatment. With increasing the frequency of bacterial infections, autoimmune lesions and absorption disorders (Malabsorption syndrome), the forecast can deteriorate accordingly with the severity of symptoms. To prevent the development of these manifestations, it is necessary to use antibiotics at the first signs of the infectious process, compliance with the rules regarding the power regime and the composition of the diet, regular monitoring of the immunologist and doctors of other specialties (depending on the accompanying violations). Care should be taken when overflowing whole blood or its components - in rare cases, patients have an anaphylactic reaction due to the presence in the blood of autoantibodies to Immunoglobulin A.
Send your good work in the knowledge base is simple. Use the form below
Students, graduate students, young scientists who use the knowledge base in their studies and work will be very grateful to you.
Posted by http://www.allbest.ru/
Volgograd State Medical University
Department of Immunology and Allergology
"Selective IGA deficiency"
Prepared:
student 28 groups 3 courses
therapeutic faculty
Jandarova Milan Khasanovna
Volgograd 2015.
Content
- 1. Introduction
- 2. Determination of selective immunoglobulin deficiencyA. (IGA)
- 4. Pathogenesis of the selective deficit of immunoglobulinA.
- 5. Clinic
- 6. Treatment
- 7. Conclusion
1. Introduction
Humoral and cellular immunity in relation to all immunologists has a number of fundamental properties:
- specificity. The immune response is specific to various structural components of proteins, polysaccharides and other antigens. Such specificity is due to the fact that each B - and T-lymphocyte, which responds to a foreign antigen, is able to distinguish the slightest differences between the antigens.
- Diversity. It has been established that the immune system of mammals can recognize 109 antigens. The total number of lemphocyte receptors in separate individuals are enormous.
Memory. The immune system is capable of responding to the re-introduction of a foreign antigen (secondary immune response). The secondary immune response is usually developing faster, stronger and qualitatively different from the first. This property of specific immunity is called immunological memory and is due to the characteristics of lymphocytes responsible for it. Memory cells (in-lymphocytes that implemented the primary immune response) are prepared for the rapid response to the re-administration of the antigen.
- End of the immune response. Normal immune response fuses after some time after antigenic stimulation. Activated lymphocytes perform their function for a short period of time after antigenic stimulation, and then, after 2-3 divisions, go into resting memory cells.
- The ability to distinguish "their" from "someone else's". One of the main properties of the immune system is the ability to recognize and respond to alien antigens and do not interact with antigens of its own body.
Immunological inability to such an answer is called tolerance. Disorders in the induction of tolerance lead to an immune response to their antigens and the emergence of pathological processes that are called autoimmune diseases. The listed abilities of specific immunity are necessary to perform their protective functions by the immune system. Fighting infection is due to the presence of specificity and memory. The variety of lymphocyte receptors is needed by the immune system to protect against many potential antigens. The end of the immune response returns the immune system to the state of rest after the destruction of the alien antigen, thus, the possibility is subsequently optimally responding to other antigens.
Tolerance and the ability to distinguish "their" and "alien" is vital conditions for preventing reactions directed against their own cells and tissues, while maintaining the diversity of antigenic receptors of lymphocytes specific for alien antigens.
Almost forty years ago, the WHO Expert Commission described immunoglobulins (LG), as "animal proteins that have antibody activity, as well as proteins similar to them in a chemical structure, and, consequently, on immunochemical specificity." The activity of antibodies (AT) is manifested in their ability to highly specific interaction with an antigen (AG) with the formation of multimolecular complexes of AG-AT.
But, along with this, antibodies (immunoglobulins) have secondary immunobiological properties that are manifested in their ability to be recorded on cells, interact with the proteins of the complement system, enhance the phagocytic activity of the phagocytic system cells, cytotoxic. The activity of NK cells, regulate the function of lymphocytes and have some other immunobiological effects. As effector mechanisms of immunity, antibodies are able to interact and form complexes with molecular and corpuscular antigens. Complexes antigen antibody are actively displayed from circulation, captured and destroyed by endothelial cells of vessels, circulating and resident macrophages, in particular, liver and spleen. Interacting, as with antigens, with toxins and enzymes of antibodies, their active centers block their active centers, neutralize toxicity and oppress the enzymatic activity of these molecules.
Human immunoglobulins are combined by heterogeneous in the physico-chemical properties of blood protein, which, on the basis of the results of the study of their molecular structure and the organization, are divided into five different groups, or classes (isotypes) of immunoglobulins, additionally denoted by capital Latin letters: IGG, IGM, LGA, IGD, and IgE. Immunoglobulins of different classes and subclasses differ in molecular weight, primary structure, the content of carbohydrates, electrophoretic mobility, life expectancy and speed of updating in the body, the ability to transplacent transfer, immunobiological active.
The dominant immunoglobulin secrets of the body (saliva, digestive juice, discharge of the nasal mucosa and the breast) is IGA. In serum, it contains slightly and is only 10-15% of the total number of immunoglobulins. The IGA monomer form is built by classic type.
The heavy chain includes a V-region with a domain of the C-region and a hinge section. In person, he has two immunoglobulin subclass: Igal and IgA2. The corresponding designation of heavy chains: A1 and A2. Excluding a hinge section The degree of homology between A1 and A2 is very high about 95%. In addition, the IGA2 subclass has two allele variants - A2T allotypes (1) and A2T (2). With the exception of the hinge section, the differences between the IGAL and IGA2 subclasses relate to 14 provisions of amino acid residues in the areas of heavy chains. At the same time, the differences between allotype A MSH A2T (1) and A2T (2) are absent in these provisions, but they are pressed in other areas of heavy chains, near the hinge section. It is these provisions that define serological differences between allotypes. The hinge regions of the chain of the A2 chains differ significantly from each other. Chain A1 in this place on 13 amino acid residues than chains A2. In this case, the sequence 224 - 239 Al-chains arose as a result of tandem duplication in the part of the genome, which controls only eight amino acid residues. Duplication of such a small segment of DNA - the phenomenon is extremely rare, but the feature of this hinge plot in Gom. In the saliva and the contents of man's thick intestine, proteolytic enzymes are presented, capable of splitting IgA in the duplicate part of the chain.
2. Determination of selective deficiency of immunoglobulin A (IGA)
Congenital and acquired violations of the function T - and B lymphocytes are associated with their quantitative insufficiency or functional failure. The causes of these deviations may be associated with genetic or metabolic disorders, as well as with the impact on the body of various infectious agents and damaging factors. Gainennye immunodeficiency There may be a consequence of various noncommunicable diseases (tumors) and medical influences (splenectomy, plasmapheresis, cytotoxic therapy, etc.).
Vsshutions B-Systems Immunity is detected in the blood test in-lymphocyte, total immunoglobulins and immunoglobulins IGM, IgG, IgA and IgE classes. The presence of blood in the examined isomagglyutinins and antibodies to previously administered vaccine drugs indirectly also indicate the state of the in-cellular immunity.
Clinically B-cell deficits Most often, recurrent bacterial infections are manifested, especially often caused staphylococci, streptococci, hemophilic stick and other pathogens, so-called, pyrogen infections, as well as conditionally pathogenic microbes - causative agents of opportunistic infections. The failure of B cells is often accompanied by the development of autoimmune processes. From congenital immunodeficses, selective IGA deficiency is the most common. According to different authors, the frequency of this type of immunodeficiency varies in the range of 1: 400-1: 800. The reason for this disease is unknown. With selective IGA, blood deficiency in patients have in-lymphocytes carrying MLGM, however, in B cells, the ability to differentiate into LGA-secreting plasma cells is broken. Clinically, IgA-deficiency can no longer manifest itself, however, allergic (bronchial asthma) and autoimmune diseases are more common among individuals with such a deficit, and autoimmune diseases, etc.), as well as timoma and tumors of the esophagus and lungs. The deficit is often detected during examination of patients suffering from infections of appendages of nasal sinuses and lungs. For individuals with IGA-deficit, the danger is a possible development of post-transfusion immunopathological reactions, including in the intravenous administration of immunoglobulins containing IG A. These reactions are required to accumulate IgG antibodies against LGA immunoglobulins in such patients. Instead of the secreted IgA, SLGM is defined in patients with LGA-deficiency in secrets.
Among the well-known immunodeficiency states, the selective deficiency of immunoglobulin A (IGA) is most often occurring in the population. In Europe, its frequency is 1/400-1 / 600 people, in the countries of Asia and Africa, the frequency of occurrence is somewhat lower. Selective deficit It is considered to be a condition in which the level of serum IGA is less than 0.05 g / l with normal quantitative indicators of other immunity units.
Selective deficit IGA. Surprisingly, the fact that when screening of normal serums with a certain frequency (0.03-0.97%), IGA deficiency may be detected (0.03-0.97%).<50 мг/л) у клинически здоровых лиц. Очевидно, этот дефект может быть компенсирован при иммунном ответе как за счет локального синтеза Ig другого класса, так и посредством транссудации секреторного IgA через слизистые оболочки. Детальные исследования показали отсутствие IgG2 и увеличение мономерного IgM. Частота инфекционных осложнений составляет примерно 15%. У части больных обнаруживают энтеропатию. Сторонники одной теории предполагают ассоциацию данного дефекта с нарушением защитных свойств слизистой оболочки, согласно другой - определенную роль играет процесс беспрепятственного всасывания ряда антигенов, к примеру лекарственных препаратов, что приводит к интрамуральным реакциям иммунных комплексов, в частности при толерантности к глутенину. При биопсии слизистой оболочки кишечника на фоне нормальных морфологических данных было обнаружено значительное количество IgM-продуцирующих плазматических клеток при ограниченном числе плазматических клеток, секретирующих IgA. Были описаны сопутствующие заболевания, такие как ревматоидный артрит, системная красная волчанка и гемосидероз легких, однако без указания на возможные причины этих нарушений. При анализе 150 клинических случаев селективного дефицита IgA было установлено, что в 18% случаев встречался ревматоидный артрит, в 7 - СКВ, в 6 - тиреоидит, в 4 - пернициозная анемия, в 3 - хронически прогрессирующая форма гепатита. Половине обследованных больных был поставлен диагноз аутоиммунного заболевания. Довольно часто выявляют преципитирующие антитела к белкам, содержащимся в сыворотке и молоке жвачных животных. С помощью специфической козьей сыворотки к IgA человека можно распознать замаскированный IgA или убедиться в его отсутствии. Примерно у 40% больных были обнаружены циркулирующие антитела анти-IgA, что можно объяснить анафилактической реакцией больного на переливание крови или плазмы. По этой причине необходимо использовать для гемотрансфузии многократно отмытые эритроциты. Большинство авторов отводят анти-IgA значительную роль в патогенезе (угнетение продукции IgA). Приблизительно в 35% случаев выявляют анти-IgG, в отдельных случаях - анти-IgM. Содержание mIgA-несущих клеток в периферической крови в целом незначительно отличается от нормы; очевидно, нарушается процесс преобразования В-клетки в IgA-продуцирующую клетку, что может ассоциировать с активацией "классоспецифичных" клеток-супрессоров. Поскольку В-клетки обнаруживаются в периферической крови больных с дефицитом IgA, то можно предположить, что признаком нарушения зрелых В-клеток служит одновременное присутствие на них а-цепей, что несовместимо с нормальной характеристикой зрелой В-клетки. Известны данные о присутствии в цитоплазме а-цепей. В некоторых случаях с помощью стимуляции лимфоидных клеток митогеном лаконоса in vitro удается вызвать продукцию и секрецию IgA. Данные о наследовании дефицита IgA противоречивы. В большинстве сообщений отсутствуют указания на возможность генетически обусловленного дефекта, частота его в семьях свидетельствует как об аутосомно-доминантном, так и рецессивном типах наследования. Наиболее часто обнаруживают аномалии хромосомы 18, в частности делецию ее длинного плеча и другие нарушения. Частота соответствия дефекта у детей и родителей свидетельствует о возможной патогенетической роли трансплацентарного переноса антител класса IgA. Дефицит секреторного IgA может быть обусловлен нарушением синтеза секреторного компонента, к тому же получены данные о нарушении процесса миграции IgA-секретирующих В-клеток в слизистой оболочке. В этих случаях концентрация сывороточного IgA поддерживается на нормальном уровне.
Selective deficit immunoglobulinov for immunodeficiency Along with hypogammaglobulinemia, which can manifest itself in the form of immunodeficiency of the three basic IG classes, states associated with a selective deficit of one of the IG classes or with a combined deficit. As observations showed, the variable deficiency Ig can be detected in 0.5% of the patients being examined in the clinic. Very often this condition is indicated as disbammaglobulinemiaHowever, this term is used and when describing other forms of IG deficiency.
In accordance with the existing idea of \u200b\u200bnormal ontogenesis, the following situations are possible:
a) the complete absence of typical B cells, or the loss or "disguise" in the cell marker (about 25% of all cases);
b) B cells are present, but are not converted to Ig-producing cells of the explicit deficit of T cells (polyclonal activators are ineffective - endogenous defect);
c) B cells can even produce IG, but not secreted them (glycosylation defect). There is no EBV receptor on the cells;
d) disruption of differentiation of in vivo cells; In vitro is effective polyclonal activators. In some cases, circulating inhibitors are found;
e) pumoral ID, mediated by violation of T-suppressor activity (about 20%). Transition forms to violations designated in paragraph "G".
The experimental model showed that massive suppressor activity can lead to a cell deficit as a secondary effect. In all likelihood, we are talking about hypogammaglobulinemia as a secondary phenomenon. An attempt was made to use high doses of prednisolone (over 100 mg per day) for the treatment of patients with hypogammaglobulinemia with high-activity suppressor cells. In some cases, a clinical effect was obtained. The suppressor activity of T cells can manifest itself at different stages of B-cell ripening (differentiation of pre-B cells through the Fc phase in a MLG-positive B cell, the differentiation of B-cells in the plasma cell) and, probably, when exposed to the plasma cell.
Experimental research and clinical observations when selective deficiency IGA It suggests that the suppressor cells may differ in the ability to cause a deficit of a certain class IG (specific T-suppressors). Improving our knowledge will allow in the future to develop a pathogenetic classification of these states.
Selective IgG deficiency is relatively rare. It manifests itself in the form of a lack of one or more subclasses IgG. Currently known defects correspond to certain genetic disorders, in particular, may be the result of gene repairs. In this case, the genes controlling the synthesis of IG subclasses are localized on chromosome 14. The deficiency of IgG2 + IgG4 is most often determined (partly in combination with IGA). The deficiency in the form of IgGi, 2.4 + IgA1 was also described. With selective IgG4 deficits, recurrent infections of the upper respiratory tract are noted, however, as with selective deficiency IgG3, IgG1 and IgG2, clinical symptoms may not appear. The deficiency of IgG2 was observed in patients in combination with attaxia - teleangectasia and sickle cell anemia. These defects are usually missed in diagnostics, since the concentration of the total IgG corresponds to the norm.
The primary IgG deficiencies are often due to the insufficient degree of heterogeneity of IgG molecules (disbammaglobulinemia).
IgG deficiency at a high level of IGM. Part of patients with IgG deficiency detect a significant rise in IGM level, in some cases up to 10 g / l. In this case, the IGA concentration can be reduced or match the norm. All patients reduced resistance to infectious diseases, in particular, it is manifested in the form of recurrent bronchitis and pneumonia. The defect can be both congenital (enclosed with a gender immunodeficiency with hyper-IgM) and acquired. This state is described mainly in boys. Family anamnesis It showed that the decline in IG products may be inherited. In addition, in some cases deficit IgG. It may be the result of the fetus fetus virus virus.
Histological study Demonstrates a rather heterogeneous picture. Along with normal morphological data, part of patients found a decrease in the number of plasma cells and a number of other violations. Plasma cells were chic-positive, which is explained by the high content of carbohydrate component against the background of a significant amount of IGM molecules. The germinal centers in some cases are detected, but may not be taken especially in congenital forms. In some patients, the infiltration of plasma cells of the intestinal wall, gallbladder, liver and other organs is placed. Sometimes hyperplasia of lymphoid elements is the most pronounced feature. More often than with other humoral forms of IDs, autoimmune disorders appear. Analyzing the data obtained, some authors indicate the defect of the central organs, others on a partial violation of the synthesis of IG molecules. Discussing the issue of combining IgG deficiency with a high level of IGM, most researchers believe that in this case the feedback mechanism between IGM and IgG synthesis is violated. Globulin replacement therapy in some cases led to normalization of IGM levels. An experimental model of this state was reproduced on chickens, bursectomed after hatching. Such chickens often developed the IGG deficiency with IGM excessive products. The combination of IgG and IGA deficiency with a high level of IGM was described as inherited, recessive syndrome. Often, the IG synthesis defect is accompanied by hemolytic or aplastic anemia, thromboenia and leukopenia. Indication to the defect of the hematopoietic stem cell. Lymph nodes demonstrate a violation of the structure of the B-cell, thymus-dependent zone. EBV-stimulated cell lines express only MLGM and MLGD. In some cases, the IGM monomer is secreted. Part of the patients found a limited defect in the T-dependent zone.
Selective IGA deficiency. Surprisingly, the fact that when screening of normal serums with a certain frequency (0.03-0.97%), IGA deficiency may be detected (0.03-0.97%).<50 мг/л) у клинически здоровых лиц. Очевидно, этот дефект может быть компенсирован при иммунном ответе как за счет локального синтеза Ig другого класса, так и посредством транссудации секреторного IgA через слизистые оболочки. Детальные исследования показали отсутствие IgG2 и увеличение мономерного IgM. Частота инфекционных осложнений составляет примерно 15%. У части больных обнаруживают энтеропатию. Сторонники одной теории предполагают ассоциацию данного дефекта с нарушением защитных свойств слизистой оболочки, согласно другой - определенную роль играет процесс беспрепятственного всасывания ряда антигенов, к примеру лекарственных препаратов, что приводит к интрамуральным реакциям иммунных комплексов, в частности при толерантности к глутенину. При биопсии слизистой оболочки кишечника на фоне нормальных морфологических данных было обнаружено значительное количество IgM-продуцирующих плазматических клеток при ограниченном числе плазматических клеток, секретирующих IgA. Были описаны сопутствующие заболевания, такие как ревматоидный артрит, системная красная волчанка и гемосидероз легких, однако без указания на возможные причины этих нарушений. При анализе 150 клинических случаев селективного дефицита IgA было установлено, что в 18% случаев встречался ревматоидный артрит, в 7 - СКВ, в 6 - тиреоидит, в 4 - пернициозная анемия, в 3 - хронически прогрессирующая форма гепатита. Половине обследованных больных был поставлен диагноз аутоиммунного заболевания. Довольно часто выявляют преципитирующие антитела к белкам, содержащимся в сыворотке и молоке жвачных животных. С помощью специфической козьей сыворотки к IgA человека можно распознать замаскированный IgA или убедиться в его отсутствии. Примерно у 40% больных были обнаружены циркулирующие антитела анти-IgA, что можно объяснить анафилактической реакцией больного на переливание крови или плазмы. По этой причине необходимо использовать для гемотрансфузии многократно отмытые эритроциты. Большинство авторов отводят анти-IgA значительную роль в патогенезе (угнетение продукции IgA). Приблизительно в 35% случаев выявляют анти-IgG, в отдельных случаях - анти-IgM. Содержание mIgA-несущих клеток в периферической крови в целом незначительно отличается от нормы; очевидно, нарушается процесс преобразования В-клетки в IgA-продуцирующую клетку, что может ассоциировать с активацией "классоспецифичных" клеток-супрессоров. Поскольку В-клетки обнаруживаются в периферической крови больных с дефицитом IgA, то можно предположить, что признаком нарушения зрелых В-клеток служит одновременное присутствие на них а-цепей, что несовместимо с нормальной характеристикой зрелой В-клетки. Известны данные о присутствии в цитоплазме а-цепей. В некоторых случаях с помощью стимуляции лимфоидных клеток митогеном лаконоса in vitro удается вызвать продукцию и секрецию IgA.
Data on the inheritance of IGA deficiency is contradictory. Most messages lack indications for the possibility of a genetically determined defect, its frequency in families indicates both an autosomal-dominant and recessive type of inheritance. The abnormalities of chromosome 18 are most often found, in particular the deletion of its long shoulder and other disorders. The frequency of conformity of the defect in children and parents testifies to the possible pathogenetic role of transplantary transfer of IGA antibodies.
The deficit of secretory IgA may be due to a violation of the synthesis of the secretory component, besides, data on the violation of the IGA-secreted B-cell migration process in the mucous membrane was obtained. In these cases, the concentration of serum IGA is maintained at a normal level.
3. Etiology of the selective deficit of immunoglobulin A
As a rule, the selective deficiency of immunoglobulin A is combined with a deficit of immunoglobulin A secretory. Selective immunoglobulin deficiency A-Most common immunological failure: one case for 500 people. The hereditary nature of the deficit was established, autosomal-dominant and recessive types of inheritance, communication with the defect of the 18th chromosome are described. Selective immunoglobulin deficiency A can be secondary in nature: with intrauterine korea rubella, toxoplasmosis, Lichen Planus, cytomegalovirus infections, chronic lymphocose colors, lymphomas. A decrease in the level of immunoglobulin A is described with the introduction of diphenin, penicillamin, gold preparations. Sometimes selective immunoglobulin deficiency and accidentally discovered in healthy people.
4. Pathogenesis of the selective deficit of immunoglobulin A
The molecular genetic foundations of IgA-deficiency are still not known. It is assumed that the defect pathogenesis lies a functional defect in cells, which, in particular, indicates a decrease in IGA-expressing in cells in patients with this syndrome. It is shown that these patients have many LGA-positive in lymphocytes have an immature phenotype, expressing IGA and IGD simultaneously. This is probably due to the defect of factors affecting the functional aspects of the expression and IGA synthesis in cells. Defects will help both in the production of cytokines and violations in response into cells to various mediators of the immune system. The role of such cytokines such as TGF-B1, IL-5, IL-10, as well as the CD40-CD40 ligand systems is considered.
Most cases of IGA-deficit occur sporadically, but married cases where the defect is traced in many generations. Thus, the literature describes 88 family cases of IgA-deficiency. An autosomal-recessive and autosomal dominant forms of inheritance of the defect, as well as an autosomal-dominant form with incomplete expression of the feature. In 20 families, different members have met at the same time selective IGA-deficiency and total variable failure (OVIN), which involves the generality of a molecular defect with these two immunodeficiency states, recently researchers are increasingly strengthened in the opinion that the selective IGA and Ovin deficiency are phenotypic manifestations The same, as yet revealed, genetic defect. Due to the fact that the gene suffering from IgA-deficiency is not known, is investigated by several chromosomes, the damage of which is expected to be involved in this process.
The main focus is drawn to 6 chromosome, where the genes of the main histocompatibility complex are located. In 8 some works, it is indicated to involve MNS III genes in the pathogenesis of IGA deficiency.
Deletions of the short shoulder 18 chromosomes are found in half cases of IgA-deficiencies, however, the accurate localization of the breakdown in most patients is not described. In other cases, studies have shown that the localization of the deletion of the shoulder 18 of the chromosome does not correlate with the phenotypic weight of the immunodeficiency.
5. Clinic
The manifestations of the selective deficiency of immunoglobulin A are associated with a violation of the function of immunological barriers, which include immunoglobulin A. The patients include chronic recurrent infections of the upper and lower respiratory tract, in severe cases - the formation of bronchiectasis, the hemosiderosis of the pulmonary idiopathic. Often the pathology of the gastrointestinal tract is often found: gluten's disease, ileyt regional, ulcerative colitis, hyperslasia of mesenteric lymph nodes. With a selective deficiency of immunoglobulin, the likelihood of autoimmune diseases, collagen diseases, collagen diseases: red systemic, rheumatoid arthritis, pernicious anemia with antibodies against caste factor, hemolytic anemia, sigere syndrome, chronic active hepatitis. In persons with a deficit of immunoglobulin A, including practically healthy, there is an increased antibody in response to expo and endo allergens (cow's milk, immunoglobulins), anti-nuclear, anti-rampant, etc. are found.
antibodies. The combination of juvenile diabetes with selective deficiency of immunoglobulin A and HLA-B8, HLA-DW3 histoins, as well as a combination of a selective deficiency of immunoglobulin A with juvenile arthritis (still disease) and ulcerative colitis were noted. In patients, there are a high frequency of allergic responses of the respiratory tract and the gastrointestinal tract, allergic to food allergens, especially for cow's milk, increased the level of general immunoglobulin E in serum, eosinophilia is often revealed. Due to the presence of patients with antibodies against immunoglobulin, allergic reactions of instant type on repeated transfusion of the plasma are possible, the introduction of U-globulin.
In some studies, it is noted that respiratory infections are more common in patients with IGA deficiency and reduced or missing Secretorial IGM. HE is excluded that only the combination of IgA deficiency and one or more IgG subclasses, which is found in 25% of cases in patients with IgA-deficiency leads to serious bronchopile diseases.
Most often, diseases associated with IGA-deficit are infections of the upper and lower respiratory tract departments, mainly the pathogens of infections in such cases are bacteria with a small pathogenicity: Moraxella Catharalis, Streptococcus Pneumonia, Hemophilus Influenzae, often causing these patients with otitis, sinusitis , conjunctivities, bronchitis and pneumonia. There are reports that the clinical manifestation of IGA deficiency requires a shortage of one or more IgG subclasses, which is found in 25% of IGA-deficiency cases. Such a defect leads to serious bronchopile diseases, such as frequent pneumonia, chronic obstructive lung diseases, chronic bronchitis, bronchiectases. The most unfavorable is the combined deficiency of IGA and IgG2 subclasses, which, unfortunately, is most often found.
Patients with selective deficiency IGA often suffer from various gastrointestinal diseases of both infectious and non-infectious genesis. So, among these patients, the infection of Gardia Lamblia (giardiasis) is common. Frames and other intestinal infections. Probably, a decrease in the secretory IGA, which is part of the local immunite, leads to more frequent infection and reproduction of microorganisms in the intestinal epitheliums, as well as to frequent reinfection after adequate treatment. The consequence of chronic intestinal infection is often a lymphoid hyperplasia, accompanied by Malabsorption syndrome.
6. Treatment
With a selective immunoglobulin deficiency, a hypoallergenic diet, the treatment of infectious and allergic complications is recommended. Persons with the presence or absence of antibodies against immunoglobulin and to solve the question of the possibility of treating blood drugs are: plasma, U-globulin, including concentrated immunoglobulin A. The prevention of respiratory infections is necessary. With a favorable course in childhood, the selective deficiency of immunoglobulin A can be compensated with age.
7. Conclusion
The immune system is a combination of organs, tissues and cells providing cells - genetic constancy of the body. Principles antigenic (genetic) purity Based on the recognition of "their own - someone else's" and largely due to the system of genes and glycoproteins (their products expression) - the main thing complex histocompatibility (MHC.), the person has a commonly called HLA system (Human Leucocyte Antigens). The human leukocytes are clearly expressed by MNS proteins, with the help of leukocyte research, MNC antigens typing.
Organs immune systems.
Central (bone marrow - blood-forming organ, fork iron or thymus, lymphoid bowel cloth) and peripheral (spleen, lymph nodes, lymphoid tissue, in its own layer of intestinal type mucous membranes) Immunity organs.
Cells - the precursors of immunocompetent cells are produced by the bone marrow. Some descendants of stem cells become lymphocytes. The lymphocytes are divided into two classes - T and B. The predecessors of T - lymphocytes migrate to the thymus, where they ripen in cells capable of participating in an immune response. In humans, the lymphocytes ripen in the bone marrow. In the birds immature in - cells migrate to the bag (Bursa) of Fabrichs, where they reach maturity. Mature V - and T - lymphocytes are populated by peripheral lymph nodes. Thus, the central organs of the immune system are based on the formation and maturation of immunocompetent cells, the peripheral organs provide an adequate immune response to the antigenic stimulation - "processing" of antigen, its recognition and clonal proliferation of lymphocytes - antigen-dependent differentiation.
selective deficit immunoglobulin immunity
Disbammaglobulinemia (Greek DYS + Gamma Globulins + Greek Haima Blood) - congenital or acquired immunological failure characterized by a shortage of one or more classes of blood immunoglobulins with a normal or compensatory elevated level of the rest. The overall level of gamma globulin can be normal or slightly reduced. Disbammaglobulinemia is reliably detected only in determining all classes of immunoglobulins (IgG, IgM, IGA, IGD, IGE). The term "disbammaglogulinemia" is used only to assess the nature of the changes in the content of IG in the blood.
The first classifications are immunological failure, which was based on a change in the content and ratio of individual IG classes, isolated disbammaglobulinemia as a special form of immuno l. Insufficiency. Rosen and Janeway (F. S. Rosen, S.A. Janeway, 1966) allocated three three, and then four types of disbammaglobulinemia; Hobbs (J. R. Hobbs, 1968) supplemented this classification by offering seven types of disbammaglobulinemia. However, further studies have shown that not all cases of violations in the content of IG may be included in the existing classification. In addition, changes in the ratio of Ig levels are not always stable and may vary with the progression of the disease. Survey of relatives of patients with disbammaglobulinemia detected various, unstable deviations in the content of Ig; In most cases, disbammaglobulinemia was hereditaryly determined. Former classifications of immuno l. Insufficiency is recognized as incorrect and replaced by a more modern classification proposed by WHO Expert Group in 1971, which is complemented as new data accumulates.
According to Janeway (1966), one of the manifestations of disbammaglobulinemia is hypergammaglobulinemia - elevated synthesis of one or more IG classes. Hypergammaglobulinemia are diffuse, or polyclonal (polyclonal gammapathy), characterized simultaneous, more often than an uneven increase in all classes Ig, and discrete, or monoclonal, under which the increase in one of the IG classes (more often Igm) or IG fragments are lightweight and heavy chains, FC- Fragment (see the full arch of the knowledge of immunoglobulins).
Diffuse hypergammaglobulinemia are observed in chronic infectious and inflammatory diseases, autoimmune processes (see the full arch of knowledge of immunopathology), liver diseases, collagen diseases (see the full arch of knowledge). Monoclonal hypergammaglobulinemia is more often a consequence of malignant reproduction of any clone of B-lymphacitis, accompanied by the products of homogeneous monoclonal protein and paraproteinemia. This protein was called the M-component (gradient). Monoclonal hypergammaglobulinemia accompanies a multiple face (see the full vault of knowledge myeloma), Macroglobulinemia Valdenstrema (see the full vault of Valdenstrem's knowledge), severe chain disease (Franklin), leukemia. Monoclonal hypergammaglobulinemia without clinical, manifestations (monoclonal gammapaty) is more common in adults.
List of used literature
1) Agadzhanyan N.A. Basics of human physiology. - M: Medicine, 2002, pp 123-156
2) Allergology and Immunology / Under Red R.M. Khaitova, N.I. Ilyina M: Gootar - Media, 2009, pp 149-154
3) Immunology / under Red R.M. Khaitova - M: Gootar Media, 2009, pp 112-123
4) Immunological accuracy. / near Ed Mikhailov.z.m. - M: Medicine, 2002, pp 123-156
5) Clinical Allergology and Immunology / Edged Goryachkaya L.A. M: Miklash, 2011, page 73-85
Posted on Allbest.ru.
Similar documents
The main purpose of lymphocytes. The role of mediators of cell and humoral immunity in the pathogenesis of bronchial asthma, obstructive diseases of the lungs, an ideopotic fibrosising alveolitis. Study of clinical data of patients with tuberculosis.
article, added 01/28/2015
Etiology, pathology and clinical manifestations of deficiencies of a specific link - deficit of antibodies and T-cellular immune response. Features of the manifestation of chronic granulomatosis and Chadiak-Higashi syndrome as manifestations of phagocytosis deficiency.
abstract, added 07/17/2013
Megaloblastic anemia is the result of a DNA synthesis violation. The causes of megaloblastic anemia are a deficiency of folic acid and vitamin B12. Causes of vitamin B12 deficiency. Causes of folic acid deficiency. Folic acid metabolism. Hemolytic anemia.
abstract, added 04.01.2009
Causes of attention deficit syndrome with hyperactivity. Pathogenesis of the disease, clinical triad syndrome, concomitant states. Assessment of the prevalence of attention deficit syndrome with hyperactivity in preschool children.
examination, added 12.02.2012
Obbiological importance of immunity. Central and peripheral organs of the immune system. Nonspecific factors for protecting the body. The structure of the antigen molecule. Anaphylaxis, anaphylactic shock and pollinosis. The main functions and types of immunoglobulin.
presentation, added 12/17/2014
The general concept of HIV infection and the acquired immune deficit syndrome. Investigation of the HIV action mechanism on the immune system. Defining the paths of infection and identification of clinical manifestations of HIV / AIDS. Medical and social consequences of the disease.
presentation, added 01.12.2012
Primary immunodeficiency properties: blood-forming stem cell, systems T- and B-lymphocytes, complement systems, selective, combined forms of immunoglobulin deficiency. The concept and properties of secondary immunodeficiency, their distinctive features from the primary.
abstract, added 03/17/2011
Mechanisms of cellular and humoral immunity. Resistance to the body to infections. Autoimmune pathological reactions and development of reactions of rejection during organs of organs and tissues. Immunostimulants and immunosuppressors, the mechanism of their action.
abstract, added 08/21/2011
The concept and types of immunoprophylaxis as medical measures contributing to the suppression of causative agents of infectious diseases with the help of factors of humoral and cellular immunity or oppressing it. Nonspecific factors for protecting the body.
presentation, added 12.10.2014
Cytokines and their cell receptors. Phagocytosis as an important component of antimicrobial protection. The choice of effector mechanisms of cellular immunity. Network interactions of cytokines. Reactions aimed at eliminating viruses of organism cells infected with viruses.