Method for early diagnosis of hemorrhagic fever with renal syndrome. Etiology and pathogenesis of hemorrhagic fever with renal syndrome Hemorrhagic fever with renal syndrome epidemiology
Zoonotic hantavirus infection, characterized by thrombohemorrhagic syndrome and predominant kidney damage. Clinical manifestations include acute fever, hemorrhagic rash, bleeding, interstitial nephritis, in severe cases - acute renal failure. Specific laboratory methods for diagnosing hemorrhagic fever with renal syndrome include RIF, ELISA, RIA, PCR. Treatment consists in the introduction of specific immunoglobulin, interferon preparations, detoxification and symptomatic therapy, hemodialysis.
ICD-10
A98.5

General information
Hemorrhagic fever with renal syndrome (HFRS) is a natural focal viral disease characterized by fever, intoxication, increased bleeding and kidney damage (nephrosonephritis). On the territory of our country, endemic areas are the Far East, Eastern Siberia, Transbaikalia, Kazakhstan, European territory, therefore HFRS is known under various names: Korean, Far Eastern, Ural, Yaroslavl, Tula, Transcarpathian hemorrhagic fever, etc. 20 thousand cases of diseases of hemorrhagic fever with renal syndrome. The peak incidence of HFRS occurs in June-October; the main contingent of cases (70-90%) are men aged 16-50 years.

Causes of HFRS
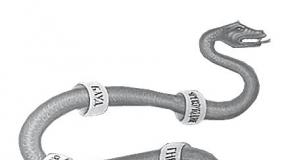
The causative agents of the disease are RNA-containing viral agents of the genus Hantavirus (hantaviruses) belonging to the Bunyaviridae family. For humans, 4 serotypes of hantaviruses are pathogenic: Hantaan, Dubrava, Puumala, Seoul. In the external environment, viruses remain stable for a relatively long time at subzero temperatures and are unstable at 37 ° C. Viruses are spherical or spiral in shape, with a diameter of 80-120 nm; contain single-stranded RNA. Hantaviruses have a tropism for monocytes, kidney, lung, liver, salivary gland cells and multiply in the cytoplasm of infected cells.
The carriers of the causative agents of hemorrhagic fever with renal syndrome are rodents: field and wood mice, voles, house rats, which become infected from each other through tick and flea bites. Rodents transmit the infection in the form of a latent carrier of viruses, releasing pathogens into the external environment with saliva, feces and urine. The ingestion of material infected with rodent secretions into the human body can occur by aspiration (by inhalation), contact (by contact with the skin) or alimentary (by eating food). Agricultural and industrial workers, tractor drivers, and drivers who are actively in contact with objects of the external environment belong to the group of increased risk for the incidence of hemorrhagic fever with renal syndrome. Human morbidity directly depends on the number of infected rodents in a given area. HFRS is recorded mainly in the form of sporadic cases; less often - in the form of local epidemic outbreaks. After the transferred infection, persistent lifelong immunity remains; cases of repeated morbidity are rare.
The pathogenetic essence of hemorrhagic fever with renal syndrome is necrotizing panvasculitis, disseminated intravascular coagulation and acute renal failure. After infection, the primary replication of the virus occurs in the vascular endothelium and epithelial cells of internal organs. The accumulation of viruses is followed by viremia and generalization of infection, which are clinically manifested by general toxic symptoms. In the pathogenesis of hemorrhagic fever with renal syndrome, a large role is played by the formed autoantibodies, autoantigens, CECs, which have a capillarotoxic effect, causing damage to the walls of blood vessels, impaired blood clotting, the development of thrombohemorrhagic syndrome with damage to the kidneys and other parenchymal organs (liver, pancreas) (liver, pancreas) , Central nervous system. Renal syndrome is characterized by massive proteinuria, oligoanuria, azotemia, impaired CBS.
HFRS symptoms
Hemorrhagic fever with renal syndrome is characterized by a cyclical course with a sequential change of several periods:
- incubation (from 2-5 days to 50 days - on average 2-3 weeks)
- prodromal (2-3 days)
- febrile (3-6 days)
- oliguric (from 3-6th to 8-14th day of HFRS)
- polyuric (from 9-13 days of HFRS)
- convalescent (early - from 3 weeks to 2 months, late - up to 2-3 years).
Depending on the severity of the symptoms, the severity of the infectious-toxic, hemorrhagic and renal syndromes, there are typical, erased and subclinical variants; mild, moderate and severe forms of hemorrhagic fever with renal syndrome.
After expiration incubation period a short prodromal period occurs, during which fatigue, malaise, headaches, myalgia, subfebrile condition are noted. The febrile period develops sharply, with an increase in body temperature to 39-41 ° C, chills and general toxic symptoms (weakness, headache, nausea, vomiting, sleep disorders, arthralgia, body aches). Characterized by pain in the eyeballs, blurred vision, flashing "flies", vision of objects in red. In the midst of a febrile period, hemorrhagic rashes appear on the mucous membranes of the oral cavity, the skin of the chest, axillary regions, and neck. An objective examination reveals hyperemia and puffiness of the face, vascular injection of the conjunctiva and sclera, bradycardia and arterial hypotension up to collapse.
In the oliguric period of hemorrhagic fever with renal syndrome, the body temperature decreases to normal or subfebrile numbers, but this does not lead to an improvement in the patient's condition. At this stage, the symptoms of intoxication intensify even more and signs of kidney damage appear: pain in the lower back increases, urine output sharply decreases, and arterial hypertension develops. In the urine, hematuria, proteinuria, cylindruria are detected. With an increase in azotemia, acute renal failure develops; in severe cases, uremic coma. Most patients have indomitable vomiting and diarrhea. Hemorrhagic syndrome can be expressed in varying degrees and include gross hematuria, bleeding from injection sites, nasal, uterine, gastrointestinal bleeding. In the oligouric period, severe complications (hemorrhages in the brain, pituitary, adrenal glands) can develop, which cause death.
The transition of hemorrhagic fever with renal syndrome to the polyuric stage is marked by subjective and objective improvements: normalization of sleep and appetite, cessation of vomiting, disappearance of lower back pain, etc. The characteristic features this period is an increase in daily urine output up to 3-5 liters and isohypostenuria. Dry mouth and thirst persist during polyuria.
The period of convalescence in hemorrhagic fever with renal syndrome can be delayed for several months or even years. In patients, post-infectious asthenia persists for a long time, characterized by general weakness, decreased performance, rapid fatigue, and emotional lability. The syndrome of autonomic dystonia is expressed by hypotension, insomnia, shortness of breath with minimal exertion, increased sweating.
Specific complications of severe clinical options HFRS can be infectious-toxic shock, hemorrhages in parenchymal organs, pulmonary and cerebral edema, bleeding, myocarditis, meningoencephalitis, uremia, etc. bacterial infection development of pneumonia, pyelonephritis, purulent otitis media, abscesses, phlegmon, sepsis is possible.
HFRS diagnostics
Clinical diagnosis of HFRS is based on the cyclical course of the infection and the characteristic change in periods. When collecting an epidemiological history, attention is drawn to the patient's stay in an endemic area, possible direct or indirect contact with rodents. When conducting a nonspecific examination, the dynamics of changes in indicators of general and biochemical analysis of urine, electrolytes, biochemical blood samples, CBS, coagulograms, etc. is taken into account.
Specific laboratory diagnostics of hemorrhagic fever with renal syndrome is carried out using serological methods (ELISA, RNIF, RIA) in dynamics. Antibodies in blood serum appear at the end of the 1st week of illness, by the end of the 2nd week they reach their maximum concentration and remain in the blood for 5–7 years. Virus RNA can be isolated using PCR assays. HFRS is differentiated from leptospirosis, acute glomerulonephritis, pyelonephritis and enterovirus infection, and other hemorrhagic fevers.
HFRS treatment
Patients with hemorrhagic fever with renal syndrome are admitted to an infectious diseases hospital. They are assigned strict bed rest and diet number 4; control of water balance, hemodynamics, indicators of the functioning of the cardiovascular system and kidneys. Etiotropic therapy of hemorrhagic fever with renal syndrome is most effective in the first 3-5 days from the onset of the disease and includes the introduction of donor specific immunoglobulin against HFRS, the appointment of interferon drugs, antiviral chemotherapy drugs (ribavirin).
In a febrile period, infusion detoxification therapy is carried out (intravenous infusions of glucose and saline solutions); prevention of disseminated intravascular coagulation (administration of antiplatelet drugs and angioprotectors); in severe cases, glucocorticosteroids are used. In the oliguric period, diuresis is stimulated (administration of shock doses of furosemide), acidosis and hyperkalemia are corrected, and bleeding is prevented. With increasing acute renal failure, the transfer of the patient to an extracorporeal infectious disease specialist, nephrologist and ophthalmologist is indicated throughout the year. A severe course is associated with a high risk of complications; mortality from HFRS ranges from 7-10%.
Prevention of hemorrhagic fever with renal syndrome consists in the destruction of murine rodents in natural foci of infection, prevention of contamination of dwellings, water sources and food with rodent secretions, and deratization of residential and industrial premises. No specific vaccination against HFRS has been developed.
In contact with
classmates
Hemorrhagic fever with renal syndrome (HFRS) is a viral zoonotic (the source of infection is an animal) disease common in certain areas, characterized by an acute onset, vascular damage, the development of hemorrhagic syndrome, hemodynamic disorders and severe kidney damage with the possible appearance of an acute renal failure.
HFRS comes out on top among other natural focal diseases. The incidence is different - on average in Russia, the incidence of HFRS varies quite strongly from year to year - from 1.9 to 14.1 per 100 thousand. population. In Russia, natural foci of HFRS are Bashkiria, Tatarstan, Udmurtia, Samara region, Ulyanovsk region. In the world, HFRS is also quite widespread - these are the Scandinavian countries (Sweden, for example), Bulgaria, Czech Republic, France, as well as China, North and South Korea.
The causative agent of HFRS, a virus, was isolated by the South Korean scientist H. W. Lee from the lungs of a rodent. The virus was named Hantaan (after the Hantaan River, which flows in the Korean Peninsula). Later, such viruses were found in many countries - in Finland, USA, Russia, China and others. The causative agent of HFRS belongs to the Bunyaviridae family and is isolated into a separate genus, which includes several serovars: the Puumala virus circulating in Europe (epidemic nephropathy), the Dubrava virus (in the Balkans) and the Seul virus (distributed on all continents). These are RNA-containing viruses up to 110 nm in size, they die at a temperature of 50 ° C within 30 minutes, and at 0-4 ° C (the temperature of a household refrigerator) they remain for 12 hours.
Hantaan virus - the causative agent of HFRS
A feature of the Hantaan virus: the tendency to infect the endothelium (inner lining) of blood vessels.
Reasons for the spread of HFRS
Red vole - carrier of HFRS
Infection routes:
Types of morbidity:
4) garden type;
Distribution features:
How does HFRS develop?
HFRS symptoms
prodromal period
Initial period
The main symptom of the onset of HFRS is a sharp increase in body temperature, which in the first 1-2 days reaches high numbers - 39.5-40.5 ° C. Fever can persist from 2 to 12 days, but most often it is 6 days. The peculiarity is that the maximum level is not in the evening (as is usual with ARVI), but in the daytime and even in the morning. In patients, other symptoms of intoxication immediately increase - lack of appetite, thirst appears, patients are inhibited, sleep poorly. Headaches are diffuse, intense, increased sensitivity to light stimuli, pain when moving the eyeballs. 20% of visual impairments have “fog in front of the eyes”. When examining patients, "hood syndrome" (craniocervical syndrome) appears: hyperemia of the face, neck, upper chest, puffiness of the face and neck, injection of the vessels of the sclera and conjunctiva (redness of the eyeballs is visible). The skin is dry, hot to the touch, the tongue is coated with a white coating. Already during this period, severity or dull pain in the lower back may occur. With high fever, the development of infectious-toxic encephalopathy (vomiting, severe headache, stiff neck muscles, Kernig's, Brudzinsky's symptoms, loss of consciousness), as well as infectious-toxic shock (a rapid drop in blood pressure, first an increase, and then a decrease in heart rate).
Oliguric period... It is characterized by a practical decrease in fever by 4-7 days, but the patient does not feel better. There are constant low back pain of varying severity - from aching to sharp and exhausting. If a severe form of HFRS develops, then after 2 days from the moment of painful renal pain syndrome, vomiting and abdominal pain in the stomach and intestines of a aching character join them. The second unpleasant symptom of this period is a decrease in the amount of urine excreted (oliguria). Laboratory - a decrease in the specific gravity of urine, protein, erythrocytes, casts in the urine. In the blood, the content of urea, creatinine, potassium rises, the amount of sodium, calcium, and chlorides decreases.
Hemorrhagic rash with HFRS
Scleral hemorrhage
The peculiarity of this period of HFRS is a peculiar change in the function of the cardiovascular system: a decrease in the pulse rate, a tendency to hypotension, and muffling of heart sounds. ECG - sinus bradycardia or tachycardia, extrasystoles may appear. Blood pressure during the period of oliguria with initial hypotension go into hypertension. Even during one day of illness high pressure can change to low and vice versa, which requires constant monitoring of such patients.
It is during the oliguric period that one of the fatal complications should be feared - about the structure of renal failure and acute adrenal insufficiency.
Polyuric period
Late convalescence.
Asthenia - weakness, decreased performance, dizziness, decreased appetite.
Dysfunction of the nervous and endocrine systems - sweating, thirst, itching, impotence, back pain, increased sensitivity in the lower extremities.
Renal residual effects - heaviness in the lower back, increased urine output up to 2.5-5.0 liters, the predominance of nocturnal urine output over daytime, dry mouth, thirst. Duration is about 3-6 months.
HFRS in children
Complications of HFRS
1) Azotemic uremia
3) Hemorrhagic complications
4) Bacterial complications(pneumonia, pyelonephritis).
HFRS diagnostics:
HFRS treatment
5) Symptomatic therapy:
- at temperature - antipyretic (paracetamol, nurofen, etc.);
- with pain syndrome, antispasmodics are prescribed (spazgan, took, baralgin and others),
- in case of nausea and vomiting, cerucal, ceruglan are administered;
Discharge is made with complete clinical improvement, but not earlier than 3-4 weeks of illness.
Prognosis for HFRS
1) recovery,
Prevention of HFRS
Acute viral zoonotic disease, viral etiology.
Characteristics of the causative agent of hemorrhagic fever with renal syndrome
The causative agent of HFRS is assigned to the Bunyaviridae family and is isolated into a separate genus Hantavirus, which includes several serovars: Puumala, Dobrava, Seul, Hantaan virus. These are RNA-containing viruses up to 110 nm in size, they die at a temperature of 50 ° C within 30 minutes, and at 0-4 ° C (the temperature of a household refrigerator) they remain for 12 hours. Tropene to endotheliocytes, macrophages, platelets, epithelium of the kidney tubules. Binds to cells that have specific receptors on membranes (integrins).
Infection routes: airborne dust (inhalation of the virus with dried excrement of rodents); fecal-oral (eating food contaminated with rodent excrement); contact (contact of damaged skin with objects of the external environment contaminated with rodent secretions, such as hay, brushwood, straw, feed).
A person has an absolute susceptibility to the pathogen. In most cases, autumn-winter seasonality is characteristic.
After the transferred infection, a strong immunity is formed. Repeated diseases do not occur in one person.
Symptoms of glps Cyclic disease is characteristic!
1) incubation period - 7-46 days (on average 12-18 days), 2) initial (febrile period) - 2-3 days, 3) oligoanuric period - from 3 days of illness to 9-11 days of illness, 4) period early convalescence (polyuric period - after the 11th - up to 30 days of illness), 5) late convalescence - after 30 days of illness - up to 1-3 years.
Sometimes the initial period is preceded by prodromal period: lethargy, increased fatigue, decreased performance, pain in the extremities, catarrhal phenomena. Duration no more than 2-3 days.
Initial period characterized by the appearance of headaches, chills, myalgia, arthralgia, weakness.
The main symptom of the onset of HFRS is a sharp increase in body temperature, which in the first 1-2 days reaches high numbers - 39.5-40.5 ° C. Fever can persist from 2 to 12 days, but most often it is 6 days. The peculiarity is that the maximum level is not in the evening, but in the daytime and even in the morning. In patients, other symptoms of intoxication immediately increase - lack of appetite, thirst appears, patients are inhibited, sleep poorly. Headaches are diffuse, intense, increased sensitivity to light stimuli, pain when moving the eyeballs. 20% of visual impairment - "fog in front of the eyes", flashing flies, decreased visual acuity (edema of the optic nerve, stagnation of blood in the vessels). When examining patients, "hood syndrome" (craniocervical syndrome) appears: hyperemia of the face, neck, upper chest, puffiness of the face and neck, injection of scleral vessels (there are hemorrhages in the sclera, sometimes affecting the entire sclera - a symptom of red cherry) and conjunctiva. The skin is dry, hot to the touch, the tongue is coated with a white coating. Already during this period, severity or dull pain in the lower back may occur. With high fever, the development of infectious-toxic encephalopathy (vomiting, severe headache, stiff neck muscles, Kernig's, Brudzinsky's symptoms, loss of consciousness), as well as infectious-toxic shock, is possible. Oliguric period... It is characterized by a practical decrease in fever for 4-7 days, there is no improvement in the condition .. There are constant pains in the lower back of varying severity - from aching to sharp and exhausting. In severe HFRS, after 2 days from the moment of painful renal syndrome, vomiting and abdominal pain in the stomach and intestines of a aching nature, oliguria join them. Laboratory - a decrease in the specific gravity of urine, protein, erythrocytes, casts in the urine. In the blood, the content of urea, creatinine, potassium rises, the amount of sodium, calcium, and chlorides decreases.
At the same time, hemorrhagic syndrome manifests itself. A small-point hemorrhagic rash appears on the skin of the chest, in the armpits, on the inner surface of the shoulders. The streaks of the rash can be located in certain lines, as from a "lash". Hemorrhages appear in the sclera and conjunctiva of one or both eyes - the so-called red cherry symptom. In 10% of patients, severe manifestations of hemorrhagic syndrome appear - from nosebleeds to gastrointestinal.
The peculiarity of this period of HFRS is a peculiar change in the function of the cardiovascular system: a decrease in the pulse rate, a tendency to hypotension, and muffling of heart sounds. On the ECG - sinus bradycardia or tachycardia, extrasystoles may appear. Blood pressure during the period of oliguria with initial hypotension can turn into hypertension (due to sodium retention). Even during one day of illness, high blood pressure can change to low and vice versa, which requires constant monitoring of such patients.
In 50-60% of patients in this period, nausea and vomiting are recorded even after a small sip of water. Often worried about painful abdominal pain. 10% of patients have a loose stool, often with an admixture of blood.
During this period, the symptoms of defeat occupy a noticeable place. nervous system: in patients with severe headache, deafness, delusional states, often fainting, hallucinations. The reason for such changes is hemorrhage in the brain substance.
Polyuric period (or early convalescence)... It is characterized by a gradual restoration of diuresis. The patient feels better, the symptoms of the disease regress. Patients excrete large amounts of urine (up to 10 liters per day), low specific gravity (1001-1006). After 1-2 days after the onset of polyuria, laboratory indicators of impaired renal function are restored. By the 4th week of illness, the amount of urine excreted returns to normal. For a couple of months, a slight weakness, a slight polyuria, a decrease in the specific gravity of urine remain.
Late convalescence. It can last from 1 to 3 years. Residual symptoms and their combinations are grouped into 3 groups:
Asthenia - weakness, decreased performance, dizziness, decreased appetite. Dysfunction of the nervous and endocrine systems - sweating, thirst, itching, impotence, increased sensitivity in the lower extremities. Renal residual effects - heaviness in the lower back, increased urine output up to 2.5-5.0 liters, the predominance of night urine output over daytime, dry mouth, thirst. Duration is about 3-6 months.
- zoonotic hantavirus infection, characterized by thrombohemorrhagic syndrome and predominant kidney damage. Clinical manifestations include acute fever, hemorrhagic rash, bleeding, interstitial nephritis, and in severe cases, acute renal failure. Specific laboratory methods for diagnosing hemorrhagic fever with renal syndrome include RIF, ELISA, RIA, PCR. Treatment consists in the introduction of specific immunoglobulin, interferon preparations, detoxification and symptomatic therapy, hemodialysis.
Hemorrhagic fever with renal syndrome
Hemorrhagic fever with renal syndrome (HFRS) is a natural focal viral disease characterized by fever, intoxication, increased bleeding and kidney damage (nephrosonephritis). On the territory of our country, endemic areas are the Far East, Eastern Siberia, Transbaikalia, Kazakhstan, European territory, therefore HFRS is known under various names: Korean, Far Eastern, Ural, Yaroslavl, Tula, Transcarpathian hemorrhagic fever, etc. 20 thousand cases of diseases of hemorrhagic fever with renal syndrome. The peak incidence of HFRS occurs in June-October; the main contingent of cases (70-90%) are men aged 16-50 years.
Causes of HFRS
The causative agents of the disease are RNA-containing viral agents of the genus Hantavirus (hantaviruses) belonging to the Bunyaviridae family. For humans, 4 serotypes of hantaviruses are pathogenic: Hantaan, Dubrava, Puumala, Seoul. In the external environment, viruses remain stable for a relatively long time at subzero temperatures and are unstable at 37 ° C. Viruses are spherical or spiral in shape, with a diameter of 80-120 nm; contain single-stranded RNA. Hantaviruses have a tropism for monocytes, kidney, lung, liver, salivary gland cells and multiply in the cytoplasm of infected cells.
The carriers of the causative agents of hemorrhagic fever with renal syndrome are rodents: field and wood mice, voles, house rats, which become infected from each other through tick and flea bites. Rodents transmit the infection in the form of a latent carrier of viruses, releasing pathogens into the external environment with saliva, feces and urine. The ingestion of material infected with rodent secretions into the human body can occur by aspiration (by inhalation), contact (by contact with the skin) or alimentary (by eating food). Agricultural and industrial workers, tractor drivers, and drivers who are actively in contact with objects of the external environment belong to the group of increased risk for the incidence of hemorrhagic fever with renal syndrome. Human morbidity directly depends on the number of infected rodents in a given area. HFRS is recorded mainly in the form of sporadic cases; less often - in the form of local epidemic outbreaks. After the transferred infection, persistent lifelong immunity remains; cases of repeated morbidity are rare.
The pathogenetic essence of hemorrhagic fever with renal syndrome is necrotizing panvasculitis, disseminated intravascular coagulation and acute renal failure. After infection, the primary replication of the virus occurs in the vascular endothelium and epithelial cells of internal organs. The accumulation of viruses is followed by viremia and generalization of infection, which are clinically manifested by general toxic symptoms. In the pathogenesis of hemorrhagic fever with renal syndrome, a large role is played by the formed autoantibodies, autoantigens, CECs, which have a capillarotoxic effect, causing damage to the walls of blood vessels, impaired blood clotting, the development of thrombohemorrhagic syndrome with damage to the kidneys and other parenchymal organs (liver, pancreas) (liver, pancreas) , Central nervous system. Renal syndrome is characterized by massive proteinuria, oligoanuria, azotemia, impaired CBS.
HFRS symptoms
Hemorrhagic fever with renal syndrome is characterized by a cyclical course with a sequential change of several periods:
- incubation (from 2-5 days to 50 days - on average 2-3 weeks)
- prodromal (2-3 days)
- febrile (3-6 days)
- oliguric (from 3-6th to 8-14th day of HFRS)
- polyuric (from 9-13 days of HFRS)
- convalescent (early - from 3 weeks to 2 months, late - up to 2-3 years).
Depending on the severity of the symptoms, the severity of the infectious-toxic, hemorrhagic and renal syndromes, there are typical, erased and subclinical variants; mild, moderate and severe forms of hemorrhagic fever with renal syndrome.
After the incubation period, a short prodromal period occurs, during which fatigue, malaise, headaches, myalgia, subfebrile condition are noted. The febrile period develops sharply, with an increase in body temperature to 39-41 ° C, chills and general toxic symptoms (weakness, headache, nausea, vomiting, sleep disorders, arthralgia, body aches). Characterized by pain in the eyeballs, blurred vision, flashing "flies", vision of objects in red. In the midst of a febrile period, hemorrhagic rashes appear on the mucous membranes of the oral cavity, the skin of the chest, axillary regions, and neck. An objective examination reveals hyperemia and puffiness of the face, vascular injection of the conjunctiva and sclera, bradycardia and arterial hypotension up to collapse.
In the oliguric period of hemorrhagic fever with renal syndrome, the body temperature decreases to normal or subfebrile numbers, but this does not lead to an improvement in the patient's condition. In this stage, the symptoms of intoxication intensify even more and signs of kidney damage appear: pain in the lower back increases, urine output sharply decreases, and arterial hypertension... In the urine, hematuria, proteinuria, cylindruria are detected. With an increase in azotemia, acute renal failure develops; in severe cases, uremic coma. Most patients have indomitable vomiting and diarrhea. Hemorrhagic syndrome can be expressed in varying degrees and include gross hematuria, bleeding from injection sites, nasal, uterine, gastrointestinal bleeding. In the oligouric period, severe complications (hemorrhages in the brain, pituitary, adrenal glands) can develop, which cause death.
The transition of hemorrhagic fever with renal syndrome to the polyuric stage is marked by subjective and objective improvements: normalization of sleep and appetite, cessation of vomiting, disappearance of lower back pain, etc. The characteristic features of this period are an increase in daily urine output up to 3-5 liters and isohypostenuria. Dry mouth and thirst persist during polyuria.
The period of convalescence in hemorrhagic fever with renal syndrome can be delayed for several months or even years. In patients, post-infectious asthenia persists for a long time, characterized by general weakness, decreased performance, rapid fatigue, and emotional lability. The syndrome of autonomic dystonia is expressed by hypotension, insomnia, shortness of breath with minimal exertion, increased sweating.
Specific complications of severe clinical variants of HFRS can be infectious-toxic shock, hemorrhages in parenchymal organs, pulmonary and cerebral edema, bleeding, myocarditis, meningoencephalitis, uremia, etc. When a bacterial infection is attached, the development of pneumonia, pyelonephritis, purulent otitis media, abscesses is possible. , sepsis.
HFRS diagnostics
Clinical diagnosis of HFRS is based on the cyclical course of the infection and the characteristic change in periods. When collecting an epidemiological history, attention is drawn to the patient's stay in an endemic area, possible direct or indirect contact with rodents. When conducting a nonspecific examination, the dynamics of changes in indicators of general and biochemical analysis of urine, electrolytes, biochemical blood samples, CBS, coagulogram, etc. is taken into account.
Specific laboratory diagnostics of hemorrhagic fever with renal syndrome is carried out using serological methods (ELISA, RNIF, RIA) in dynamics. Antibodies in blood serum appear at the end of the 1st week of illness, by the end of the 2nd week they reach their maximum concentration and remain in the blood for 5–7 years. Virus RNA can be isolated using PCR assays. HFRS is differentiated from leptospirosis, acute glomerulonephritis, pyelonephritis and enterovirus infection, and other hemorrhagic fevers.
HFRS treatment
Patients with hemorrhagic fever with renal syndrome are admitted to an infectious diseases hospital. They are assigned strict bed rest and diet number 4; control of water balance, hemodynamics, indicators of the functioning of the cardiovascular system and kidneys. Etiotropic therapy of hemorrhagic fever with renal syndrome is most effective in the first 3-5 days from the onset of the disease and includes the introduction of donor specific immunoglobulin against HFRS, the appointment of interferon drugs, antiviral chemotherapy drugs (ribavirin).
In a febrile period, infusion detoxification therapy is carried out (intravenous infusions of glucose and saline solutions); prevention of disseminated intravascular coagulation (administration of antiplatelet drugs and angioprotectors); in severe cases, glucocorticosteroids are used. In the oliguric period, diuresis is stimulated (administration of shock doses of furosemide), acidosis and hyperkalemia are corrected, and bleeding is prevented. With increasing ARF, the transfer of the patient to extracorporeal hemodialysis is indicated. In the presence of bacterial complications, antibiotic therapy is prescribed. In the polyuric stage, the main task is to carry out oral and parenteral rehydration. During the period of convalescence, restorative and metabolic therapy is carried out; full nutrition, physiotherapy (diathermy, electrophoresis), massage and exercise therapy are recommended.
Prediction and prevention of HFRS
Mild and moderate forms of hemorrhagic fever with renal syndrome in most cases result in recovery. Residual phenomena (post-infectious asthenia, back pain, cardiomyopathy, mono- and polyneuritis) are observed for a long time in half of those who have been ill. Reconvalescents need quarterly dispensary observation of an infectious disease specialist, nephrologist and ophthalmologist throughout the year. A severe course is associated with a high risk of complications; mortality from HFRS ranges from 7-10%.
Prevention of hemorrhagic fever with renal syndrome consists in the destruction of murine rodents in natural foci of infection, prevention of contamination of dwellings, water sources and food with rodent secretions, and deratization of residential and industrial premises. No specific vaccination against HFRS has been developed.
Hemorrhagic fever with renal syndrome (HFRS) is a viral zoonotic (the source of infection is an animal) disease common in certain areas, characterized by an acute onset, vascular damage, the development of hemorrhagic syndrome, hemodynamic disorders and severe kidney damage with the possible appearance of acute renal failure.
HFRS comes out on top among other natural focal diseases. The incidence is different - on average in Russia, the incidence of HFRS varies quite strongly from year to year - from 1.9 to 14.1 per 100 thousand. population. In Russia, natural foci of HFRS are Bashkiria, Tatarstan, Udmurtia, Samara region, Ulyanovsk region. In the world, HFRS is also quite widespread - these are the Scandinavian countries (Sweden, for example), Bulgaria, Czech Republic, France, as well as China, North and South Korea.
This problem should be given special attention, first of all, because of the severe course with the possibility of developing infectious-toxic shock, acute renal failure with a fatal outcome. Mortality in HFRS is on average from 1 to 8% in the country.
Characteristics of the causative agent of hemorrhagic fever with renal syndrome
The causative agent of HFRS, a virus, was isolated by the South Korean scientist H. W. Lee from the lungs of a rodent. The virus was named Hantaan (after the Hantaan River, which flows in the Korean Peninsula). Later, such viruses were found in many countries - in Finland, USA, Russia, China and others. The causative agent of HFRS belongs to the Bunyaviridae family and is isolated into a separate genus, which includes several serovars: the Puumala virus circulating in Europe (epidemic nephropathy), the Dubrava virus (in the Balkans) and the Seul virus (distributed on all continents). These are RNA-containing viruses up to 110 nm in size, they die at a temperature of 50 ° C within 30 minutes, and at 0-4 ° C (the temperature of a household refrigerator) they remain for 12 hours.
Hantaan virus - the causative agent of HFRS
A feature of the Hantaan virus: the tendency to infect the endothelium (inner lining) of blood vessels.
There are two types of HFRS virus:
Type 1 - eastern (common in the Far East), reservoir - field mouse. The virus is highly variable, capable of causing severe forms of infection with a mortality rate of up to 10-20%.
Type 2 - western (circulates in the European part of Russia), reservoir - bank vole. It causes milder forms of the disease with a mortality rate of no more than 2%.
Reasons for the spread of HFRS
The source of infection (Europe) is forest mouse-like rodents (bank and red voles), and in the Far East - the Manchurian field mouse.
Red vole - carrier of HFRS
The natural focus is the habitat of rodents (in temperate climatic formations, mountain landscapes, low-lying forest-steppe zones, foothill valleys, river valleys).
Infection routes: airborne dust (inhalation of the virus with dried excrement of rodents); fecal-oral (eating food contaminated with rodent excrement); contact (contact of damaged skin with objects of the external environment contaminated with rodent secretions, such as hay, brushwood, straw, feed).
A person has an absolute susceptibility to the pathogen. In most cases, autumn-winter seasonality is characteristic.
Types of morbidity:
1) forest type - they get sick during a short visit to the forest (picking berries, mushrooms, etc.) - the most common option;
2) household type - at home in the forest, next to the forest, more damage to children and the elderly;
3) production route (drilling, oil pipelines, work in the forest);
4) garden type;
5) camp type (rest in pioneer camps, rest homes);
6) agricultural type - autumn-winter seasonality is characteristic.
Distribution features:
Young people are more often affected (about 80%) 18-50 years old,
More often, patients with HFRS are men (up to 90% of patients),
HFRS gives a sporadic morbidity, but outbreaks can also occur: small 10-20 people, less often - 30-100 people,
After the transferred infection, a strong immunity is formed. Repeated diseases do not occur in one person.
How does HFRS develop?
The entrance gate of the infection is the mucous membrane of the respiratory tract and the digestive system, where it either dies (with good local immunity) or the virus begins to multiply (which corresponds to the incubation period). Then the virus enters the bloodstream (viremia), which is manifested by an infectious-toxic syndrome in a patient (more often this period corresponds to 4-5 days of illness). Subsequently, it settles on the inner wall of the vessels (endothelium), disrupting its function, which manifests itself in the patient as hemorrhagic syndrome. The virus is excreted in the urine, therefore, the vessels of the kidneys are also affected (inflammation and edema of the kidney tissue), the subsequent development of renal failure (difficulty in excreting urine). It is then that an unfavorable outcome can occur. This period lasts up to 9 days of illness. Then the reverse dynamics occurs - resorption of hemorrhages, reduction of renal edema, regulation of urination (up to 30 days of illness). Full recovery of health lasts up to 1-3 years.
HFRS symptoms
The cyclical nature of the disease is characteristic!
1) incubation period - 7-46 days (average 12-18 days),
2) initial (febrile period) - 2-3 days,
3) oligoanuric period - from 3 days of illness to 9-11 days of illness,
4) the period of early convalescence (polyuric period - after the 11th - up to the 30th day of illness),
5) late convalescence - after 30 days of illness - up to 1-3 years.
Sometimes the initial period is preceded by prodromal period: lethargy, increased fatigue, decreased performance, pain in the limbs, sore throat. Duration no more than 2-3 days.
Initial period characterized by the appearance of headaches, chills, aches in the body and limbs, joints, weakness.
The main symptom of the onset of HFRS is a sharp increase in body temperature, which in the first 1-2 days reaches high numbers - 39.5-40.5 ° C. Fever can persist from 2 to 12 days, but most often it is 6 days. The peculiarity is that the maximum level is not in the evening (as is usual with ARVI), but in the daytime and even in the morning. In patients, other symptoms of intoxication immediately increase - lack of appetite, thirst appears, patients are inhibited, sleep poorly. Headaches are diffuse, intense, increased sensitivity to light stimuli, pain when moving the eyeballs. 20% of visual impairments have “fog in front of the eyes”. When examining patients, "hood syndrome" (craniocervical syndrome) appears: hyperemia of the face, neck, upper chest, puffiness of the face and neck, vascular injection of the sclera and conjunctiva (redness of the eyeballs is visible). The skin is dry, hot to the touch, the tongue is coated with a white coating. Already during this period, severity or dull pain in the lower back may occur. With a high fever, the development of infectious-toxic encephalopathy (vomiting, severe headache, stiffness of the occiput muscles, Kernig's, Brudzinsky's symptoms, loss of consciousness), as well as infectious-toxic shock (a rapid drop in blood pressure, first an increase in the frequency, and then a decrease in heart rate ).
Oliguric period... It is characterized by a practical decrease in fever by 4-7 days, but the patient does not feel better. There are constant low back pain of varying severity - from aching to sharp and exhausting. If a severe form of HFRS develops, then after 2 days from the moment of painful renal pain syndrome, vomiting and abdominal pain in the stomach and intestines of a aching character join them. The second unpleasant symptom of this period is a decrease in the amount of urine excreted (oliguria). Laboratory - a decrease in the specific gravity of urine, protein, erythrocytes, casts in the urine. In the blood, the content of urea, creatinine, potassium rises, the amount of sodium, calcium, and chlorides decreases.
At the same time, hemorrhagic syndrome manifests itself. A small-point hemorrhagic rash appears on the skin of the chest, in the armpits, on the inner surface of the shoulders. The streaks of the rash can be located in certain lines, as from a "lash". Hemorrhages appear in the sclera and conjunctiva of one or both eyes - the so-called red cherry symptom. In 10% of patients, severe manifestations of hemorrhagic syndrome appear - from nosebleeds to gastrointestinal.
Hemorrhagic rash with HFRS
Scleral hemorrhage
The peculiarity of this period of HFRS is a peculiar change in the function of the cardiovascular system: a decrease in the pulse rate, a tendency to hypotension, and muffling of heart sounds. On the ECG - sinus bradycardia or tachycardia, extrasystoles may appear. Blood pressure during the period of oliguria with initial hypotension go into hypertension. Even during one day of illness, high blood pressure can change to low and vice versa, which requires constant monitoring of such patients.
In 50-60% of patients in this period, nausea and vomiting are recorded even after a small sip of water. Often worried about painful abdominal pain. 10% of patients have a loose stool, often with an admixture of blood.
During this period, symptoms of damage to the nervous system occupy a noticeable place: patients have severe headache, deafness, delusional states, often fainting, hallucinations. The reason for such changes is hemorrhage in the brain substance.
It is during the oliguric period that one of the fatal complications should be feared - acute renal failure and acute adrenal insufficiency.
Polyuric period... It is characterized by a gradual restoration of diuresis. The patient becomes better, the symptoms of the disease weaken and regress. Patients excrete large amounts of urine (up to 10 liters per day), low specific gravity (1001-1006). After 1-2 days after the onset of polyuria, laboratory indicators of impaired renal function are restored.
By the 4th week of illness, the amount of urine excreted returns to normal. For a couple of months, a slight weakness, a slight polyuria, a decrease in the specific gravity of urine remain.
Late convalescence. It can last from 1 to 3 years. Residual symptoms and their combinations are grouped into 3 groups:
Asthenia - weakness, decreased performance, dizziness, decreased appetite.
Dysfunction of the nervous and endocrine systems - sweating, thirst, itching, impotence, back pain, increased sensitivity in the lower extremities.
Renal residual effects - heaviness in the lower back, increased urine output up to 2.5-5.0 liters, the predominance of night urine output over daytime, dry mouth, thirst. Duration is about 3-6 months.
HFRS in children
Children of all ages, including infants, can be ill. Characterized by the absence of precursors of the disease, the most acute onset. The duration of the temperature is 6-7 days, children complain of constant headache, drowsiness, weakness, they lie more in bed. Pain in the lumbar region appears already in the initial period.
When should you see a doctor?
High fever and severe symptoms of intoxication (headache and muscle pain), severe weakness, the appearance of "hood syndrome", hemorrhagic skin rash, as well as the appearance of pain in the lower back. If the patient is still at home, and he has a decrease in the amount of urine excreted, hemorrhages in the sclera, lethargy - an urgent call for an ambulance and hospitalization!
Complications of HFRS
1) Azotemic uremia... It develops in severe HFRS. The reason - "slagging" of the body due to a serious dysfunction of the kidneys (one of the excretory organs). The patient develops constant nausea, repeated vomiting that does not bring relief, hiccups. The patient practically does not urinate (anuria), becomes inhibited and gradually develops coma (loss of consciousness). It is difficult to remove a patient from an azotemic coma, often the outcome is death.
2) Acute cardiovascular failure... Either symptoms of infectious-toxic shock in the initial period of the disease against the background of high fever, or on the 5-7th day of the disease against the background of normal temperature due to hemorrhage in the adrenal glands. The skin becomes pale with a bluish tinge, cold to the touch, the patient becomes restless. Heart rate rises (up to 160 beats per minute), falls rapidly blood pressure(up to 80/50 mm Hg, sometimes it is not determined).
3) Hemorrhagic complications: 1) Tearing of the renal capsule with the formation of hemorrhage in the perineal tissue (with improper transportation of a patient with severe back pain). The pain becomes intense and persistent. 2) Rupture of the kidney capsule, which can result in severe hemorrhage in the retroperitoneal space. The pains appear suddenly on the side of the rupture, accompanied by nausea, weakness, sticky sweat. 3) Hemorrhage in the adenohypophysis (pituitary coma). Manifested by drowsiness and loss of consciousness.
4) Bacterial complications(pneumonia, pyelonephritis).
HFRS diagnostics:
1) If HFRS is suspected, such moments as the stay of the sick in natural foci of infection, the incidence rate of the population, the autumn-winter seasonality and characteristic symptoms disease.
2) Instrumental examination of the kidneys (ultrasound) - diffuse changes parenchyma, pronounced parenchymal edema, venous congestion cortical and medulla.
3) The final diagnosis is made after laboratory detection of IgM and G antibodies using enzyme-linked immunosorbent assay (ELISA) (with an increase in antibody titer 4 times or more) - paired sera at the onset of the disease and after 10-14 days.
HFRS treatment
1) Organizational and regime activities
Hospitalization of all patients in a hospital, patients are not contagious to others, so they can be treated in infectious, therapeutic, surgical hospitals.
Transport excluding any shock.
Creation of a sparing conservatory regime:
1) bed rest - mild form - 1.5-2 weeks, wed-heavy - 2-3 weeks, severe - 3-4 weeks.
2) adherence to a diet - table number 4 without restriction of protein and salt, non-hot, non-coarse food, eating in small portions often. There are enough liquids - mineral water, Borjomi, Essentuki No. 4, mousses. Fruit drinks, fruit juices with water.
3) daily sanitation of the oral cavity - with solution of furacillin (prevention of complications), daily bowel movement, daily measurement of daily urine output (every 3 hours the amount of fluid drunk and excreted).
2) Prevention of complications: antibacterial drugs in usual doses (usually penicillin)
3) Infusion therapy: the goal is to detoxify the body and prevent complications. Stock solutions and drugs: concentrated glucose solutions (20-40%) with insulin to provide energy and eliminate excess extracellular K, prednisolone, ascorbic acid, calcium gluconate, lasix according to indications. In the absence of the "soaking" effect (that is, an increase in diuresis), dopamine is prescribed in a certain dosage, as well as for the normalization of microcirculation - curantil, trental, euphyllin.
4) Hemodialysis in severe disease, according to certain indications.
5) Symptomatic therapy:
- at temperature - antipyretic (paracetamol, nurofen, etc.);
- with pain syndrome, antispasmodics are prescribed (spazgan, took, baralgin and others),
- in case of nausea and vomiting, cerucal, ceruglan are administered;
7) Specific therapy (antiviral and immunomodulating effect): virazole, specific immunoglobulin, amixin, iodantipyrine - all drugs are prescribed in the first 3-5 days of illness.
Discharge is made with complete clinical improvement, but not earlier than 3-4 weeks of illness.
Prognosis for HFRS
1) recovery,
2) lethal (on average 1-8%),
3) interstitial nephrosclerosis (overgrowth of connective tissue in places of hemorrhage),
4) arterial hypertension (30% of patients),
5) chronic pelonephritis (15-20%).
Dispensary observation of those who have recovered:
Upon discharge, a sick leave is issued for 10 days.
Follow-up for 1 year - 1 time in 3 months - consultation of a nephrologist, blood pressure control, examination of the fundus, OAM, according to Zemnitsky.
6 months exemption from physical activity doing sports.
Children for a year - medical withdrawal from vaccinations.
Prevention of HFRS
1. Specific prophylaxis (vaccine) has not been developed. For the purpose of prevention, iodantipyrine is prescribed according to the scheme.
2. Non-specific prophylaxis includes deratization (rodent control), as well as the protection of environmental objects, grain stores, hay from the invasion of rodents and pollution by their secretions.
Infectious disease doctor N.I. Bykova
HFRS, in other words, is an acute viral natural focal disease (popularly, mouse fever). The disease is characterized by fever and intoxication, can affect the kidneys and develop thrombohemorrhagic syndrome.
The HFRS virus was first discovered in 1944. A.A. Smorodintsev, but it was isolated by a scientist from South Korea N. W. Lee a little later, in 1976. Later, this virus was used for diagnostic examination of hemorrhagic fever. There were 116 patients who received a severe form of fever, and 113 of them were noted with a diagnostic increase in the titers of immunofluorescent antibodies in the blood serum.
After a while, a similar virus was isolated in the following countries: USA, Finland; Russia, China and others. Today it is a separate genus of the virus.
The so-called Hantaan virus and Puumala virus are RNA viruses. Their diameter is 85 - 110 nm. The virus can die at a temperature of 50 ° C, while it must be kept for at least half an hour. The virus can function for up to 12 hours at temperatures between 0 and 4 ° C. Today there are two main HFRS viruses:
Hantaan is able to circulate in natural foci in the Far East, Russia, South Korea, North Korea, Japan and China. It can be carried by a field mouse; The European type of the virus - Puumala - is found in Finland, Sweden, Russia, France and Belgium. The carrier is the bank vole.
It is possible that there is a third species, it is suspicious that it is in the Balkans.
Disease history
HFRS is related to natural foci zones. HFRS is a hemorrhagic fever with renal syndrome. The carrier and causative agent of this kind of disease are mice and rodents of the mouse species. In the European half of our country, the infection is carried by the bank vole. In epidemic foci, their infection can reach 40, or even up to 60%.
The Far East is much more rich in sources of infection. Here, the infection is spread by: field mice, red-gray field mice and Asian bats. In urban-type settlements, pathogens can be house rats. The causative agent of HFRS is excreted in the urine or feces.
Mice vectors of HFRS
Rodents transmit infection to each other by airborne droplets. Infection is carried out by inhaling the odor from the feces of an infected individual. You can also become infected by contact with an infected rodent, as well as an infected object (for example, hay or brushwood, which an infected mouse walked on). A person can get infected by eating foods that rodents have come into contact with, including through cabbage, carrots, cereals, etc.
An infected person cannot infect any other person. The HFRS virus is most commonly transmitted to men aged 16 to 50. The percentage of men infected can be up to 90%. So during the cold winter, the number of rodents decreases, the activity of the virus in January-May also drops significantly. But with the end of the spring season (at the end of May), the virus begins to grow. The peak incidence occurs in June – December.
In 1960, diseases with the HFRS virus were observed in 29 regions of our country. If we consider the present, then the disease, first of all, can progress between the Volga and the Urals. This includes the following republics and regions: the republics of Bashkiria and Tatarstan, the republic of Udmurtia, the Ulyanovsk and Samara regions.
People of any country are prone to get sick with hemorrhagic fever. HFRS was observed in the following countries: Sweden, Finland, Norway, Yugoslavia, Bulgaria, Belgium, Czechoslovakia, France, China, South Korea and North Korea. A special serological survey carried out in central African countries, in Southeast Asia, Hawaii, as well as in Argentina, Brazil, Colombia, Canada and the United States showed that the population of these countries has a number of specific antibodies against the HFRS virus.
To summarize, we can say that the history of HFRS disease began thanks to murine rodents. They are carriers of many more diseases.
The doors for infection are opened by the mucous membrane of the respiratory tract, in some cases it can be the skin or the mucous membrane of the digestive organs. The first signs of HFRS are intoxication and viremia. The disease causes great damage to the vascular walls. Vascular damage plays an important role in the genesis of renal syndrome. Studies have shown that complications reduce glomerular filtration.
Presumably, the cause of the development of renal failure in most cases is an immunopathological factor. Thrombohemorrhagic syndrome may occur, which depends on the severity of the disease. People who have had HFRS disease have good immunity. Recurrent diseases have not yet been identified.
Symptoms of GPLS
With this disease, the incubation period lasts 7-46 days, generally it takes 3-4 weeks to recover. There are several stages of the disease:
Initial stage; Oligouric period (at this moment renal and hemorrhagic manifestations are monitored); Polyuric period; Convalescence period.
Symptoms of HFRS disease in children are no different from those of an adult.
The initial stage of the disease lasts up to 3 days. As a rule, it has pronounced and acute symptoms(chills, high fever, which can rise to 40 ° C). In addition, there may be such ailments as severe headache, feeling of weakness, dryness in the mouth. When examining a patient, doctors may notice flushing of the skin on the face, neck, in the upper part of the chest. During the disease, hyperemia of the pharyngeal mucosa and injection of the vascular sclera occur.
In some cases, a hemorrhagic rash appears. Some patients begin to get sick with HFRS gradually. A few days before the disease, weakness, malaise, catarrhal phenomena may occur upper paths breathing. Changes occurring in the internal organs of the body are quite difficult to identify on initial stage disease, they will manifest themselves a little later. At the initial stage of the disease, symptoms such as dull pain in the lumbar region, moderate manifestation of bradycardia may occur. In severe diseases, meningism may appear.
The next oliguric period lasts anywhere from 2 or 4 days to 8 or 11 days. The patient's body temperature remains at the same level: 38 - 40 ° C. She can hold out at this level for up to 7 days of illness. But, as it turned out, a decrease in the temperature level does not affect the patient's well-being in any way, it does not get any easier for him. In most cases, with a drop in temperature, the patient feels much worse.
The second period of the disease is often manifested by pain in the lumbar region, the degree of pain can be any. If, within 5 days, lower back pain does not appear, you can think about the correctness of the diagnosis and the disease of HFRS. In many patients, 1 or 2 days after the cessation of pain in the lumbar region, vomiting may appear. Vomiting may occur at least 8 times a day. Vomiting is independent of food intake and drugs... Abdominal pain or bloating is also possible.
On examination, doctors can reveal dry skin, hyperemia of the face and neck, hyperemia of the mucous membrane of the pharynx and conjunctiva. Puffiness is possible upper eyelid... Manifestation of hemorrhagic symptoms.
Thrombohemorrhagic syndrome of any severity is manifested only in some patients who have an advanced form of the disease. At this stage of the disease, a high fragility of blood vessels is manifested. In about 10 or 15% of patients, petechiae appears, 7 -8% of patients are marked by the formation of gross hematuria. Approximately another 5% of patients suffer from intestinal bleeding. You can also notice bruising at the site where the injection was carried out, there are nosebleeds, hemorrhages in the sclera, in even more rare cases, bleeding may be accompanied by vomiting or sputum production. The disease is not accompanied by bleeding from the gums or uterus.
The frequency of manifestation of symptoms and ailments is accompanied only by the degree of complexity of the disease. In about 50-70% of cases, they manifested themselves in a severe form of the disease, 30-40% less often in cases of moderate illness and in 20-25% of cases in a mild form of the disease. With an epidemic manifestation of the disease, the symptoms of the disease appear much more often and stronger.
In any case, the symptoms that appear require an urgent visit to the hospital and proper treatment.
The most common manifestation of HFRS disease is kidney damage. As a rule, kidney disease is accompanied by swelling of the face, pasty eyelids, and positive Pasternatsky symptoms.
Oliguria in a severe form of the disease can develop into enuresis. When taking tests, special attention is paid to the protein content in the urine, it usually increases greatly and can reach the figure of 60 g / l. At the beginning of the period, microhematuria may appear, there is a likelihood of detecting hyaline and granular cylinders in the urine sediment, and in some cases even long Dunaevsky cylinders. The level of residual nitrogen rises. More pronounced symptoms of azotemia may appear by the end of the week of the disease or by its 10th day. Restoring nitrogen norms is possible in two or three weeks.
The polyuric period of the disease begins approximately from the 9th or 13th day of the onset of the disease. Vomiting gradually stops, pains in the lumbar region and abdomen disappear, sleep and appetite gradually return to normal. The daily rate of urination increases (up to 3-5 liters per day). Dryness of the oral cavity remains a little, and from the 20th - 25th day of the illness, the patient's recovery period begins.
HFRS treatment
For any form of this disease, it is advisable to carry out treatment in a hospital. The main treatment is antibiotics.
Complications
Any advanced disease develops into a severe form of the disease and causes all sorts of complications. Complications of HFRS disease include:
Azotemic uremia; Ruptured kidney; Eclampsia; Acute vascular insufficiency; Puffiness of the lungs; Focal pneumonia.
In some cases, the disease progresses with pronounced brain symptoms.
Prevention of HFRS
In order to recognize the disease in time, prevention of HFRS is necessary. Timely detection of the disease will help to avoid numerous complications and consequences of the disease.
HFRS in children
The disease in children under 7 years of age is very rare. They have little contact with nature, so the likelihood of the disease is significantly low.
Possible complications of HFRS
Diet for HFRS and after recovery
Features in children
Features in pregnant women
Incubation period ranges from 7 to 46 days, most often 2-3 weeks. Clinical syndromes in HFRS are characterized by a certain periodical, which is important not only for diagnosis, but also for the correct therapy. During the course of the disease, the following periods are distinguished: prodromal, febrile (initial or pre-hemorrhagic), oliguric with hemorrhagic syndrome, polyuric and convalescence.
In a significant part of patients, the appearance of pronounced signs of the disease is preceded by a prodrome: malaise, fatigue, headache, a slight sore throat. The duration of this period does not exceed 1-3 days.
Feverish period develops after the prodrome or without it: chills, chills, headache, weakness, aches in muscles and joints appear. An important sign of the disease is a rapid increase in body temperature, which in the next 1-2 days reaches a maximum level of 39.5-40.5 ° C. The duration of fever varies from 1-2 to 12 days or more, but more often 5-6 days. The temperature curve is irregular and can be of a remitting, constant, or irregular type. The fever is reduced by a short lysis or a delayed crisis. From the first days of the disease, appetite disappears, thirst, insomnia, lethargy appear. The headache is intense, can be combined with dizziness, photophobia, pain when turning the eyeballs. Approximately 20% of patients have a "mesh" or "fog" in front of their eyes, they see objects poorly, especially at close range. Sleep disorder is manifested by insomnia. In some patients, lethargy is expressed, short-term loss of consciousness is possible, in severe cases - complete prostration. The development of meningoencephalitic syndrome is relatively rare: vomiting, severe headache, stiff neck muscles, Kernig's, Brudzinsky's symptoms, pyramidal signs. With a spinal puncture, the cerebrospinal fluid flows out in frequent drops, transparent, without pathological changes. When examining patients, attention is drawn to hyperemia and some puffiness of the face, edema of the eyelids, injection of the vessels of the sclera and conjunctiva. Hyperemia extends to the neck and upper chest, as well as the mucous membrane of the oropharynx. The skin is dry, hot, the tongue is coated with a whitish coating. Along with a decrease in appetite, patients are worried about severe dry mouth and thirst. In some cases, already in this period, there is a feeling of heaviness or dull pain in the lower back, a weakly positive symptom of Pasternatsky.
Oliguric period. A decrease in body temperature to normal or subfebrile numbers on days 4-7 (from 3-4 to 8-11 days) does not bring relief to the patient, since the manifestations of renal and hemorrhagic syndromes are increasing. The most constant symptom of this period is lower back pain of varying severity: from unpleasant to sharp, painful, requiring the use of analgesics. In severe HFRS, vomiting is noted, not associated with food intake, 1-2 days after the onset of pain. At the same time, a significant proportion of patients experience abdominal pain of varying intensity, more often they are localized in the epigastric or iliac regions. Against the background of pain syndrome, the amount of urine released progressively decreases. Oliguria is combined with a decrease in specific gravity, proteinuria, hematuria, cylindruria. In the blood, the content of nitrogenous toxins, potassium rises, and the concentration of alkaline acids, the concentration of sodium, calcium, and chlorides decreases.
The face remains puffy, hyperemic, although less bright than in the febrile period. In parallel with acute renal failure, hemorrhagic syndrome is growing. One of the most frequent manifestations it is a small-point hemorrhagic rash on the skin of the chest, in the area of the anterior and middle axillary lines, pectoralis major muscles, on the inner surface of the shoulders. Often it has a linear arrangement in the form of stripes - "abrasions from a lash." Another manifestation of hemorrhagic syndrome may be hemorrhages on the oral mucosa and conjunctiva. A common site of hemorrhage is the sclera of one or both eyes. They are usually localized in the outer corner of the eye, in severe patients they can occupy the entire eyeball - "red cherry". There may be hemorrhages at the sites of former injections. In 10-15% of patients, cavity bleeding is observed, to-rye can take on a threatening character, cause severe posthemorrhagic anemias and even deaths. The most common are nosebleeds, less often stomach and intestinal. In some patients, gross hematuria occurs. Clinical manifestations of hemorrhagic syndrome are more often recorded and more intensely expressed in severe HFRS.
In this period, changes in the function of the CVS are important. The boundaries of the heart in the overwhelming majority of cases are within normal limits. Heart tones are muffled. 60-70% have relative bradycardia, less often pulse compliance and relative tachycardia. On the ECG - sinus bradycardia or tachycardia, extrasystole and MA are possible. After normalization of the temperature, a decrease in the voltage of all teeth, an offset of int. ST below the isoline, inversion T. In some cases, serous-hemorrhagic myocarditis develops with scant physical data. Blood pressure in the initial period is reduced, in some individuals, collapse may be observed on days 2-6. From the moment of development of PN, blood pressure may increase. Systolic pressure rises more often, diastolic pressure is less common. During this period, hypertension is observed in 40-50% of patients. Pressure lability is more pronounced in patients with severe and moderate forms of HFRS. It should be borne in mind that even within a day, hypertension can suddenly be replaced by hypotension.
Quite often in this period, there is an abdominal syndrome. It is manifested by nausea, vomiting, to-rye can be persistent, sometimes painful in nature, occur spontaneously or after a small sip of water. Often there are abdominal pains, while the abdominal wall remains soft, but some patients may have tension in the abdominal muscles and the appearance of signs of irritation of the peritoneum. 10-12% of b's have loose stools, in which there may be an admixture of blood. Enlargement of the liver is possible.
The defeat of NS and ES in the clinic of this period takes a noticeable place. On autopsy, hemorrhages and necrosis of the pituitary gland are found, which is assessed as a typical manifestation in HFRS, in 33% - necrosis and hemorrhages in the adrenal glands. With the defeat of the NA, general cerebral symptoms prevail, characterized by signs of encephalitis and meningism. Hemorrhages can be observed in various parts of the GM with the development of focal symptoms. Bs note an intense, growing headache, edges combined with lethargy or stunnedness; possibly deep confusion, delirium, hallucinations. Among the symptoms of meningism, the appearance of symptoms of Kernig and Brudzinsky is possible. Sometimes pathological symptoms of Oppenheim, Gordon, Babinsky, uneven tendon reflexes are found.
Polyuric period. From 9-13 days of illness, diuresis is gradually restored, then polyuria and polydipsia appear. Following an improvement in diuresis, the symptoms of the disease soften and reverse development. B-ies in this phase excrete a large amount of urine (7-10 liters per day), low specific gravity (1001-1006). 1-2 days after the onset of polyuria, the concentration of nitrogenous toxins in the blood begins to decrease and the level of electrolytes is restored. The content of potassium ions in the plasma decreases with the subsequent development of hypokalemia, the hyperemia and swelling of the face, characteristic of HFRS, disappears.
At 3-4 weeks of the disease, polyuria begins to decrease, the condition of the patients improves. Symptoms of asthenization, a tendency to polyuria, a decrease in beats. urine weights can persist for several weeks or even months.
The period of convalescence and outcomes. HFRS is not characterized by a subacute and even more chronic course. However, residual phenomena can persist in convalescence for up to 1 year. Residual symptoms and their combinations are grouped into 3 groups:
· post-infectious asthenia- weakness, decreased performance, headaches, decreased appetite, palpitations with a slight physical. load.
· NS lesions and endocrine disorders- sweating, thirst, pruritus, alopecia, impotence. There may be back pain, paresthesia in the lower extremities, positive symptoms of tension (Lasegue, Wasserman).
· renal manifestations- due to tubular insufficiency. Severity or moderate back pain, increased urine output up to 2.5-5.0 liters, nocturia, isohypostenuria, dry mouth, thirst. The duration of this syndrome does not exceed 3-6 months.
HFRS refers to diseases that contribute to the formation of chronic tubulo-interstitial nephropathy (diagnosed on the basis of persistent - more than 6 months - tubular insufficiency).
Mortality in different geographic zones is not the same and ranges from 1.05 to 8.0%. The cause of the fatal outcome is: ITSH with the development of DIC syndrome, hemorrhages in vital organs, azotemic uremia, kidney rupture.
Clinical options. Severe forms of HFRS occur with a tendency to hyperthermia, pronounced intoxication and hemorrhagic syndromes, PN with oliguria (less than 300 ml per day) or anuria (less than 50 ml per day), high levels of residual nitrogen, urea, creatinine, deselectrolithemia, prolonged proteinuria, and slow convalescence. Complications are common.
With a moderate course, intoxication, oliguria, azotemia, and electrolyte metabolism disorders are less pronounced. Hemorrhagic syndrome is moderately expressed, complications are rare.
In milder forms of HFRS, the febrile period is shortened, body temperature is moderately elevated, urine output is slightly reduced, proteinuria and polyuria are moderate and short-lived. Residual nitrogen and urea are within normal limits.
Hemorrhagic fever with renal syndrome (HFRS) or mouse fever should be familiar to every resident of Russia.
The disease is dangerous with the likelihood of severe complications. The number of deaths among patients in Russia reaches 8%.
Is there a problem? Enter in the form "Symptom" or "Name of the disease" press Enter and you will find out all the treatment for this problem or disease.
The site provides background information. Adequate diagnosis and treatment of the disease is possible under the supervision of a conscientious doctor. Any drugs have contraindications. A specialist consultation is required, as well as a detailed study of the instructions! ...
What are the reasons for HFRS?
This is a viral disease that affects the blood vessels and kidneys. The causative agent of the disease is the Hantaan virus, which belongs to the Bunyavirus family.
The virus is spread between animals by flea or tick bites. Rodents are latent carriers of the virus and will excrete it into the environment with feces, urine and saliva.
The virus is characterized by resistance to negative temperatures and dies within half an hour at temperatures from 50 degrees. The peculiarity of the virus is that it infects the inner lining of blood vessels (endothelium).
There are 2 types of virus:
- Eastern type. The type predominates in the Far East; the Manchurian field mice are carriers of the infection.
- The western type is common in the European part of Russia. The carrier is the red and red vole.
It is noted that the first type is more dangerous and causes from 10 to 20% of deaths, the second - up to 2%. There are several ways of getting this disease.
Infection occurs when a person comes into contact with the secretions of infected rodents by inhalation, eating, or when they come into contact with damaged skin. The disease is seasonal in autumn and winter.
Symptoms of this disease
The course of HFRS is divided into several periods.
Depending on the stage of the disease, the patient shows symptoms of the disease.
- Incubation period. This stage lasts about 20 days. At this stage, the disease does not manifest itself. The patient may not be aware of the infection.
- The initial (febrile) period lasts 3 days.
- Oligoanuric lasts about a week.
- Polyuric (early convalescence) - 2 to 3 weeks.
- Late convalescence begins approximately from the second month of the course of the disease and lasts up to 3 years.
The initial stage of the disease is characterized by a significant jump in body temperature from morning to day. The patient is accompanied by insomnia, body aches, fatigue, lack of appetite.
There is a headache, painful reaction to light stimuli, conjunctivitis. The language is formed white bloom... There is redness in the upper body.
In the third stage of the disease, the temperature decreases slightly, but other pronounced symptoms appear.
Typical for this period are pain in the lower back, which in a severe form of the disease may be accompanied by nausea, vomiting, aching pains in the abdominal part.
The volume of excreted urine is reduced. Due to this, the level of potassium and urea in the blood increases, and the level of calcium and chloride decreases.
A small rash appears on the patient's skin (hemorrhagic syndrome). The area of the chest, armpits and shoulders is more often affected. This is accompanied by nose and gastrointestinal bleeding.
The patient's cardiovascular system malfunctions: the pulse becomes less frequent, blood pressure in a short period grows from low to high and vice versa. 
A characteristic symptom of hemorrhagic fever with renal syndrome is damage to the nervous system. Hemorrhages in the patient's brain can provoke hallucinations, deafness, fainting. At the stage of oliguria, the patient has complications - acute renal and adrenal insufficiency.
At the stage of early convalescence, the patient feels relief. At first, there is an abundant flow of urine (up to 10 liters per day), then diuresis gradually returns to normal.
Late convalescence is characterized by residual symptoms. The patient feels a general malaise - dizziness, weakness, increased sensitivity in the legs, need for fluid, increased sweating.
Features of the development of HFRS
The development of HFRS begins in the patient from the incubation period in the first 2-3 weeks from the moment of infection. The infection enters the body through the lining of the respiratory tract or digestive system, less commonly through open wounds on the skin.
If a person has strong immunity, the virus dies. It starts to multiply.
Then the infection enters the bloodstream and the patient begins to manifest infectious-toxic syndrome. Once in the blood, the virus settles on the endothelium.
The vessels of the kidneys are more affected. The infection leaves the patient's body with urine.
At this time, the patient may experience acute renal failure. Regression sets in, and body functions are restored. The recovery process is complex and slow, this period can last up to 3 years.
Diagnosis of pathology
The first symptoms of the disease are similar to ARVI, so the patient often hesitates to seek help in medical institution... Consider the peculiarities of the symptoms of HFRS on early stages development of the disease.
Firstly, with ARVI, the patient's temperature rises in the evening, while with HFRS it occurs mainly in the morning. Another feature of the disease is redness of the skin of the upper body of a person, the eyeballs.
In the later stages of the development of the disease, more distinct symptoms appear. This is a hemorrhagic rash, a decrease in the volume of excreted urine, pain in the lumbar region.
At the first suspicion of the development of hemorrhagic fever, you should consult a doctor. When making a diagnosis, the seasonal factor, the likelihood of the patient staying in endemic foci and other epidemiological characteristics are taken into account.
To make an accurate diagnosis, apply differential and laboratory diagnostics... During differential research methods, specialists exclude other diseases, acute respiratory viral infections, influenza, tonsillitis, pyelonephritis.
The patient is constantly monitored to identify new symptoms of the disease.
Laboratory diagnostic methods include urine analysis, general and biochemical analysis of the patient's blood. With HFRS, fresh erythrocytes are found in the patient's urine, the protein level is significantly reduced.
In the blood, the level of urea and creatine rises, and the level of hemoglobin and red blood cells decreases. The concentration of fats in the blood serum increases and the level of albumin decreases.
Confirm the diagnosis of HFRS by detecting IgM and G antibodies in the body. For this, enzyme-linked immunosorbent assay is used.
An important feature of the diagnosis of this disease is not the very fact of the studies being carried out, but their frequency.
The patient should be under constant supervision, and the diagnosis is made on the basis of changes that are observed in the results of studies throughout the course of the disease.
Instrumental diagnostic methods (X-ray, computed tomography and others) are carried out to identify the degree of damage to internal organs.
Video
Effective treatment of the disease
When a disease is detected, hospitalization is strictly indicated to the patient as soon as possible. Due to the fact that the disease is not transmitted from person to person, the treatment of hemorrhagic fever with renal syndrome is carried out in infectious diseases hospitals, in surgical, therapeutic.
Transportation of the patient in the later stages of development is carried out with extreme caution, fearing hemorrhage and rupture of the kidneys.
The patient needs adherence to bed rest, diet. During the patient's stay in the hospital, preventive measures are taken to prevent complications.
Drug treatment of the disease includes taking antibacterial drugs... For energy conservation, glucose solutions with insulin are prescribed.
Curantil and aminophylline normalizes microcirculation. To relieve the symptoms of the disease, antipyretic and analgesic drugs are used.
Features of a therapeutic diet
Recovery will require a strict diet. For patients with HFRS, diet No. 4 of 15 systems of therapeutic nutrition is recommended, developed by the Soviet doctor M.I. Pevzner.
You need to eat often and in small portions. The food should be of medium temperature. Fermentation products (cabbage, plums, sour cream, cheese) should be completely excluded from the diet.
Diet # 4 aims to limit the amount of fat and carbohydrates. Difficult to digest foods that increase gastric secretion are also excluded from it. 
These include:
- Fatty fish and meat;
- Smoked products;
- Pickles;
- Sausages;
- Sauces;
- Canned food;
- Bakery;
- Dried fruits;
- Carbonated drinks;
- Sweets.
Dishes should not be spicy or spicy.
Low-fat boiled meat and fish, low-fat cottage cheese, wheat rusks are acceptable. From cereals you need oats, rice, buckwheat, semolina, jelly decoctions from these cereals are useful.
Raw fruits and vegetables are not permitted. Compotes, jelly, jelly are prepared from fruits, vegetables are used in the form of mashed potatoes.
Help of folk remedies
Effective treatment of the disease is impossible without medical help.
Self-medication of this disease leads to serious consequences and death. Before taking this or that folk remedy, you should consult with your doctor.
Doctors advise taking different decoctions aimed at normalizing kidney function. In herbal medicine, many medicinal plants are known, the use of which has a diuretic and anti-inflammatory effect.
The most common decoctions used for HFRS:
- Bring 1 teaspoon of flax seeds and 200 ml of water to a boil. You need to drink a decoction of 100 ml every 2 hours.
- 50 g of young birch leaves should be infused for 5 hours in 200 ml of warm water, take 100 ml 2 times a day.
- Add 2 tablespoons of lingonberry leaves to 200 ml of hot water. Insist the broth in a water bath for half an hour, you need to take 100 ml 2 times a day.
- Add 3 g of dry orthosiphon leaves (kidney tea) to a glass of boiling water and boil for another 5 minutes. The broth is infused for 4 hours and 100 ml is drunk before meals.
The most effective are fees from medicinal herbs, they are already available in ready-made proportions in pharmacies.
Most of these collections use bearberry leaves, they can be brewed separately as tea.
Compositions of fees with bearberry:
- Bearberry leaves, licorice root, cornflower inflorescences in proportions 3: 1: 1;
- Bearberry leaves, licorice root, juniper fruits in proportions 2: 1: 2;
- Bearberry leaves, orthosiphon leaves, lingonberry leaves in proportions 5: 3: 2.
A tablespoon of the collection is brewed in a glass of water. You need to take the broth for half a glass 3 times a day. To normalize the work of the cardiovascular system, currant juice and a decoction of fragrant geranium roots are used.
Currant juice is taken in 100 ml 3 times a day. Geranium roots (about 4 pieces) are poured into 1 liter of water and boiled for 20 minutes. You need to drink this broth warm every 20 minutes.
The use of folk remedies is also possible to relieve the symptoms of the disease. To lower body temperature, they take baths with cool water (about 30 degrees) and drink decoctions of raspberries, honeysuckle and strawberries.
Possible complications of the disease
It has been proven that the most dangerous in terms of complications is the oligoanuric stage of the disease. The period runs from 6 to 14 days of the disease.
The complications that hemorrhagic fever can cause are specific and nonspecific.
Various complications include:
- Infectious toxic shock;
- DIC syndrome (disseminated vascular coagulation);
- Swelling of the brain and lungs;
- Acute cardiovascular failure;
- Various hemorrhages (in the brain, adrenal glands and others) and bleeding;
- Kidney rupture.
Infectious toxic shock is characterized by acute circulatory failure. The patient's blood pressure drops, and internal organ failure develops.
This disease complication is the most common cause of death in HFRS.
With DIC syndrome, the normal blood circulation in the patient's body is disrupted. This leads to the development of serious dystrophic changes.
Hypocoagulation develops - the patient's blood clotting ability decreases, thrombocytopenia - the level of platelets in the blood decreases. The patient has bleeding. 
Among non-specific complications, diseases are distinguished - pyelonephritis, purulent otitis media, abscesses, pneumonia. Complications with HFRS are dangerous and can often lead to death.
Patients who have had this disease develop strong immunity to the virus. This statement is justified by the fact that there were no cases of re-infection in patients who underwent HFRS.
Timely diagnosis of the disease is important, which will provide effective and qualified treatment.
Disease prevention
In order to prevent hemorrhagic fever with renal syndrome, personal hygiene rules must be observed.
It is necessary to thoroughly wash your hands and consumed fruits and vegetables, do not leave food in the reach of rodents.
Use a gauze bandage to protect the respiratory tract from dust that can carry infection.
The main measures for the general prevention of the disease is the destruction of the population of murine rodents in the foci of HFRS.
It is necessary to ensure the improvement of the territories adjacent to residential buildings, crowded places, grocery warehouses, and the like. Weeds and thickets should not be allowed to spread.
5 / 5 ( 6 votes)
Hemorrhagic fever with renal syndrome (HFRS) is a viral infection that has a certain territorial attachment and is manifested by thrombohemorrhagic syndrome and specific kidney damage.
What is hemorrhagic fever with renal syndrome?
The pathology is caused by a virus that, penetrating into the body, accumulates in the endothelium (inner layer) of blood vessels and in the epithelium of internal organs (kidneys, myocardium, pancreas, liver). Then the virus spreads with the blood throughout the body, provoking the onset of the disease, which is manifested by symptoms of general intoxication. The virus damages the vascular walls, disrupts the blood clotting ability, causing the development of hemorrhagic syndrome. Blood clots form in different organs; in severe cases, extensive hemorrhages occur. The kidneys are most damaged by the toxins of the virus.
On the territory of Russia, residents of Siberia, the Far East, Kazakhstan, Transbaikalia are susceptible, therefore the name of this viral infection is tied to the area - Far East, Omsk, Korean, Ural, Tula hemorrhagic fever, etc. residents of Scandinavian countries (Norway, Finland), Europe (France, Czech Republic, Bulgaria), China, North and South Korea. Synonyms for the name of the pathology - hemorrhagic or epidemic nephrosonephritis, Churilov's disease, mouse fever.
Every year in our country, from 5 to 20 thousand cases of the disease are recorded. Mostly men of active age are ill - from 16 to 50 years (70-90%). Hemorrhagic nephrosonephritis is mostly sporadic, that is, isolated cases are recorded, but there are also small outbreaks - 10–20, less often up to 100 people.
The highest incidence is observed in the summer and until mid-autumn; in winter, pathology is rarely diagnosed. This is because the carriers of the virus are rodents - the field mouse and the bank vole, which are active in the warm season. In urban conditions, house rats can be carriers of infection.
Up to the age of three, hemorrhagic fever with renal syndrome is practically not recorded, until the age of seven, children are extremely rarely ill. This is due to the fact that babies have little contact with wildlife, do not take part in agricultural work. Children can only get sick if their parents violate hygiene standards (for example, they fed the child with unwashed vegetables contaminated with the feces of a carrier mouse). Among children, small outbreaks of the disease are possible in pioneer camps, sanatoriums, kindergartens if the institutions are located near a forest or field.
In young children, especially newborns and infants, the disease is very difficult, since the virus infects the vessels, and in children they are characterized by increased permeability. Babies, as a rule, develop multiple bleeding into internal organs with disruption of the work of entire systems.
Hemorrhagic nephrosonephritis is always acute, chronic course does not exist. After the illness, lifelong immunity remains.
Doctor in detail about the infection - video
Causes, development factors and transmission routes
The causative agents of the disease are RNA-containing viruses belonging to the Bunyavirus family, of which four serotypes are pathogenic for the human body: Hantaan, Puumala, Dubrava and Seoul. Each of these viruses is distributed in a specific area. Hantaviruses have the shape of a sphere or a spiral, reach sizes from 80 to 120 nm, are stable in the external environment, lose their stability at a temperature of 37 ° C, at 0-4 ° C they remain viable for up to 12 hours, at 50 ° C they die within half an hour. The person is absolutely susceptible to these viruses.
Creep into human body infectious agents can in different ways:
- aspiration (through the air) - when inhaling the smallest particles of dried rodent feces;
- contact - penetration through damaged human skin when interacting with contaminated objects (agricultural feed, cereals, straw, hay, brushwood);
- alimentary (fecal-oral) - through foods contaminated with rodents.
The risk group for morbidity includes agricultural workers (farmers, tractor drivers), workers of enterprises producing feed and other food products, drivers, that is, everyone who is actively in contact with the environment. The possibility of human infection is directly related to the number of rodents in a particular area. The patient is not dangerous to the environment - the virus is not transmitted from person to person.
HFRS symptoms
Depending on the severity of manifestations, the severity of intoxication, renal and thrombohemorrhagic syndromes, mild, moderate and severe forms of pathology are distinguished. The course of hemorrhagic nephrosonephritis can be typical, blurred and subclinical.
The disease is characterized by a cyclical course, during which several periods change:
- incubation (can last from a week to 50 days, most often 3 weeks);
- prodromal (short, only lasts a couple of days);
- febrile (lasts from 3 days to a week);
- oliguric (only 5–8 days);
- polyuric (begins on the 10-14th day of illness);
- convalescent (from 20 days to 2 months - early period and up to 2-3 years - late).
After incubation, a short prodrome period begins, which may be absent. At this time, the patient feels weakness, malaise, he is worried about muscle, joint, headaches, the temperature may rise slightly (up to 37C o).
The febrile stage begins violently: the temperature rises to 39–41C o, signs of intoxication appear: nausea, vomiting, body aches, severe headache, lethargy, pain in the eyes, muscles, joints. The patient's vision is blurred, "flies" flash before his eyes, color perception is disturbed (everything around is seen in crimson). This period is characterized by the appearance of a petechial (small hemorrhagic) rash on the neck, chest, armpit skin, and oral mucosa. The patient's face and neck are hyperemic, the sclera are red, the heartbeat is slow (bradycardia), the pressure is low (it can go down to collapse - critically low numbers with the development of acute heart failure, loss of consciousness and the threat of death).
The next period, oliguric, is characterized by a decrease in temperature to low or normal numbers, but this does not improve the patient's well-being. The signs of general intoxication intensify even more, symptoms from the kidneys join: severe pain in the lower back, the amount of urine decreases, the pressure rises sharply. In the excreted urine, blood, protein appears, the number of cylinders increases (protein imprints of the renal tubules - one of the structural elements of nephrons). Azotemia is increasing (a high level of nitrogenous metabolic products in the blood, which are normally excreted by the kidneys), a severe impairment of the functional abilities of the kidneys (acute renal failure) is possible, and a threat of uremic coma arises. Most patients in this stage suffer from diarrhea and excruciating vomiting.
Hemorrhagic syndrome manifests itself as gross hematuria (blood clots in the urine that are visible to the naked eye), intense bleeding - nasal, from injection sites, as well as from internal organs. Hemorrhagic syndrome is dangerous with severe complications: stroke, extensive hemorrhages in vital organs - the pituitary gland, adrenal glands.
The onset of the polyuric stage is characterized by an improvement general condition the patient. Sleep and appetite gradually normalize, nausea and back pain go away. The volume of urine increases significantly: up to 3-5 liters can be excreted per day. Polyuria is a specific feature of this stage. The patient complains of thirst and dryness of the mucous membranes.
The recovery stage can be significantly delayed - from several months to several years. Those who have had hemorrhagic fever experience post-infectious asthenia for a long time: weakness, increased fatigue, emotional instability. The convalescent has symptoms of VSD (vegetative-vascular dystonia): decreased blood pressure, increased sweating, shortness of breath even with a slight load, sleep disturbances.
Diagnostics
When collecting an epidemiological anamnesis, it is necessary to take into account the stay of the sick person in the area where there were cases of hemorrhagic nephrosonephritis, possible contact with rodents or objects contaminated with the waste products of these animals. Clinical diagnosis is based on the cyclical course of the disease, the characteristic change in symptoms in successive periods, as well as laboratory data.
General and biochemical blood and urine tests, coagulogram (blood clotting test) are performed. Analyzes are carried out in dynamics, since the disease is characterized by a constant change in indicators.
In the blood at the initial stage of the disease, leukopenia (a decrease in the level of leukocytes) is noted, and then a sharp leukocytosis (an increase in leukocytes), thrombocytopenia (a decrease in the number of platelets), a high ESR (up to 40-60 mm per hour). In the oliguric stage, the amount of residual nitrogen, magnesium and potassium in the blood significantly increases, the level of chlorides, calcium and sodium decreases. Hemoglobin and erythrocytes increase due to blood thickening due to the leakage of plasma through the walls of the vessels damaged by the virus. A coagulogram shows a decrease in the blood clotting ability.
Blood biochemistry determines the change in the main indicators, which indicates a deep violation of metabolic processes in the patient's body.
In the analysis of urine, erythrocytes, protein, cylinders are determined. Albuminuria (high protein in the urine) appears a few days after the onset of the disease and reaches a maximum high performance by about 10 days, and then sharply declines. Such a sharp change in protein indicators (even within a few hours) is characteristic of mouse fever and does not happen with any other disease.
Hypoisostenuria (low specific gravity of urine) is observed from the very beginning of the disease, significantly increases at the oliguric stage and does not recover for a long time. This symptom, along with albuminuria, has valuable diagnostic value.
Specific diagnostics consists in detecting antibodies to the pathogen in the blood serum by means of serological methods - ELISA (enzyme-linked immunosorbent assay) or RNIF (indirect immunofluorescence reaction). Blood for research is taken at the earliest possible period of the disease and again after 5-7 days. In the repeated analysis, an increase in antibody titers is found not less than 4 times. Antibodies remain in the blood of those who have been ill for many years (5–7).
To assess the severity of kidney damage, ultrasound procedure, the patient undergoes ECG, chest x-ray, fibrogastroscopy according to indications.
Differential diagnosis
The disease should be distinguished from pathologies with similar symptoms: other types of hemorrhagic fevers, leptospirosis, enterovirus infection, typhus, sepsis, renal diseases - acute pyelonephritis, glomerulonephritis, nephrosis.
Treatment
The patient is treated only in a hospital. Early hospitalization with an adapted medical transport, with the observance of precautions due to the danger of rupture of the kidney capsule, significantly reduces the percentage of complications and deaths.
Therapy is aimed at combating intoxication, maintaining the functionality of the kidneys, and preventing complications. Strict bed rest is prescribed, up to the first days of the polyuric stage. The patient is shown diet table No 4, with restriction of protein (meat products) and potassium (due to the development of hyperkalemia), salt is not limited, it is recommended to drink plenty of water, mainly mineral waters without gas - Essentuki No 4, Borjomi.
Doctors conduct constant monitoring of the patient's condition - control of water balance, hemodynamics, functional indicators of the kidneys and cardiovascular system. The patient needs careful hygienic care.
Etiotropic therapy in the form antiviral drugs effective in the first few days of the disease (up to 5 days). The patient is injected with donor immunoglobulin, interferon preparations, chemical antiviral agents- Ribavirin (Ribamidil, Virazol) or Amiksin, Cycloferon.
At the febrile stage, detoxification measures are carried out: intravenous infusion of saline with ascorbic acid, 5% glucose solution, in case of heart failure - Gemodez, Reopolyglyukin. Prevention of disseminated intravascular coagulation (dessimented intravascular coagulation or thrombohemorrhagic syndrome - the formation of blood clots in small vessels) consists in prescribing:
- angioprotectors:
- Calcium gluconate, Rutin, Prodectin;
- disaggregants:
- Pentoxifylline (Trental), Complamin, Curantil;
- drugs to improve microcirculation:
- Heparin, Fraxiparina, Kleksana.
In the oliguric period, infusion of saline solutions is canceled, the daily amount of parenteral (intravenous) solutions is calculated based on the amount of urine excreted per day. Diuresis is stimulated with diuretics - Eufillin intravenously, Furosemide in shock doses.
The fight against acidosis is carried out by injecting the patient with a 4% sodium bicarbonate solution. Prevention of bleeding is carried out by the introduction of Dicinon, Aminocaproic acid, with severe bleeding, blood substitutes are prescribed. In case of acute impairment of renal functions, the patient is transferred to hemodialysis (contraindicated in case of kidney rupture, massive bleeding, hemorrhagic stroke).
With an increase in renal failure, a patient with mouse fever is transferred to hemodialysis - a method of blood purification using an "artificial kidney" apparatus
In case of severe course and complications, the following is prescribed:
- hormonal drugs:
- Prednisolone, Hydrocortisone, Doxu;
- protease inhibitors:
- Contrikal, Trasilol, Gordox;
- transfusion of fresh plasma;
- oxygen therapy.
Severe pain is relieved with analgesics (Spazmalgon, Baralgin, Trigan) together with antihistamines (Suprastin, Tavegil, Diphenhydramine), if they are ineffective - drugs, for example, Promedol, Fentanyl, Tromadol. For nausea and vomiting, Raglan, Cerucal, Perinorm are used, with indomitable vomiting, Aminazine, Droperidol, Atropine are indicated. The development of cardiovascular failure requires the use of cardiac glycosides and cardiotonics to normalize the work of the heart - Strofantin, Korglikon, Cordiamin.
With anuria (absence of urine), uremic intoxication is treated by washing the stomach and intestines with 2% sodium bicarbonate solution.
After diuresis has recovered, to prevent secondary infection urinary tract appoint:
- nitrofurans:
- Furogin, Furodonin;
- sulfonamides:
- Groseptol, Biseptol.
Bacterial complications are treated with antibiotics, mainly of the cephalosporin and penicillin series. In the polyuric period, therapy is aimed at optimal rehydration (restoration of water balance): infusion saline solutions are administered - Acesol, Quintasol, Laktosol, the patient must take alkaline mineral waters, Regidron, Cytroglucosolan. The patient is prescribed fortifying drugs: multivitamins, Riboxin, ATP, Cocarboxylase.
The convalescent is discharged after the normalization of urine output, laboratory parameters of urine and blood:
- at easy form- not earlier than 17-19 days of illness;
- for severe - no earlier than 25-28 days.
The sick leave after discharge is continued by the doctor of the polyclinic for at least 2 weeks. Reconvalescent is observed by a therapist (children - pediatrician) and an infectious disease specialist. The sick person is released from heavy physical labor, sports activities (children - from physical education lessons) for 6-12 months. Children cannot be routinely vaccinated throughout the year.
During the recovery period, a full, fortified food and drink is recommended: an infusion of rose hips, herbs with a diuretic effect, taking multivitamin preparations is recommended. Exercise therapy, massage, physiotherapy (electrophoresis, diathermy) are important measures for the early recovery of the patient.
The diet involves the exclusion of fatty, fried, salty, spicy, spicy foods. It is necessary to remove smoked meats, marinades, canned food, spices, all products that can irritate the kidneys from the diet of the patient. The food should be complete, fortified, balanced in the content of proteins, fats and carbohydrates.
- dried fruits:
- raisins, dried apricots;
- berries:
- blackberries, strawberries;
- beverages:
- rosehip broth;
- cranberry, lingonberry juice;
- natural juices;
- fruits and vegetables:
- bananas, pears, pumpkin, cabbage;
- dairy products;
- jelly, fruit and milk jellies;
- cereal porridge;
- lean meats and fish.
For drinking, it is best to choose mineral waters without gas with an antispastic and diuretic effect - Borjomi, Essentuki, Kurgazak, Krasnousolskaya. Herbs are recommended in the form of teas and infusions to normalize urine output: bearberry (bear's ear), lingonberry leaves, cornflower flowers, strawberry leaves, dill seeds with a string, meadow clover. Anyone who has suffered from the disease is categorically contraindicated in alcohol in any form.
Photo gallery - products recommended for convalescents of hemorrhagic nephrosonephritis
 Those who have had hemorrhagic fever with renal syndrome are especially useful fresh vegetables and fruit
Those who have had hemorrhagic fever with renal syndrome are especially useful fresh vegetables and fruit  During the recovery period, you need to include low-fat varieties of meat and fish in the diet.
During the recovery period, you need to include low-fat varieties of meat and fish in the diet.  Cranberry juice is recommended for all kidney diseases
Cranberry juice is recommended for all kidney diseases  Decoctions of raisins and dried apricots are very rich in potassium
Decoctions of raisins and dried apricots are very rich in potassium  Porridge is useful for its high content of trace elements
Porridge is useful for its high content of trace elements  Dairy and fermented milk products are necessary for recovery from illness
Dairy and fermented milk products are necessary for recovery from illness  Blackberries, strawberries, strawberries contain many vitamins, trace elements and have a diuretic effect
Blackberries, strawberries, strawberries contain many vitamins, trace elements and have a diuretic effect  Bearberry leaf is useful for kidney disease, as it has a diuretic effect
Bearberry leaf is useful for kidney disease, as it has a diuretic effect
Treatment prognosis and complications
Mild and moderate forms of the disease usually result in recovery. Residual effects, signs of vascular dystonia, weakness, lumbar pain, cardiopathy, polyneuropathy (decreased muscle strength and tendon reflexes) persist for a long time in half of those who have undergone pathology. Dispensary observation indicated for 12 months by an infectious disease specialist and a nephrologist.
A severe course of the disease can cause complications:
- infectious toxic shock - the development of a uremic coma is possible;
- DIC syndrome leading to multiple organ failure;
- pulmonary edema (acute respiratory failure);
- stroke, hemorrhage in the heart muscle, pituitary gland, adrenal glands with the formation of areas of necrosis (one of the main causes of death);
- acute heart failure;
- damage (rupture) of the renal capsule;
- the imposition of a bacterial infection threatening sepsis, peritonitis, severe pneumonia, otitis media, pyelonephritis.
Mortality from hemorrhagic nephrosonephritis is 7-10%.
Video - How to protect yourself from the virus?
Preventive measures
Specific prophylaxis does not exist today. To prevent infection, the following measures must be taken:
- destruction of rodents, especially in endemic areas;
- storage of food, grain, feed in warehouses and barns, reliably protected from the penetration of rats and mice;
- work at agricultural facilities in overalls and respirators;
- observance of sanitary and hygienic standards when arranging the territory of summer camps, sanatoriums, open health centers, home farms (cutting down and destruction of thickets of weeds, wild bushes, removal of garbage and latrine pits at considerable distances from residential buildings, protection of food storage facilities);
- regular deratization of residential and industrial premises;
- observance of the rules of personal hygiene (washing hands, using disinfecting disposable wipes) in rural areas, in the country, during outdoor recreation.
Hemorrhagic fever with renal syndrome is a disease that threatens with severe complications and death. At timely diagnosis and full therapy of these consequences can be avoided. Do not forget about prevention, which can protect you from infection and keep you healthy.