Recurrent urinary tract infection is an interdisciplinary problem. Recurrent viral infections likely causes of frequent cystitis
Recurrent infection (ri) urinary tract (NMP) in women is one of the main and discussed problems of modern urology. This circumstance is due to the high frequency of relapses of this disease. At the same time, Ri is a complicated infection arising from anatomical, functional, hormonal and dysbiotic disorders of the organism.
Of course, an important meaning in the development of RI belongs to both different microorganisms with the dominance of the conditionally pathogenic microflora.
Proven bacterial agents of the etiological structure of RI are gram-negative microorganisms, mainly representatives of the family Enterobacteriaceae., in particular Escherichia Coli., some strains Klebsiella SPP., Serratia SPP., Enterobacter SPP. and non-enzyme gram-negative bacteria (NGOP). In recent years, work has appeared, in which it is indicated on the tendency of the displacement of the etiological structure towards the gram impassive flora, in particular, coagulas-negative staphylococci (KOS). In addition, a number of studies have been completed pointing to the involvement of non-clostrial-anaerobic bacteria to the genesis of RI's development.
However, not all types of microbes in the urinary ways are equally vigilant. Viruble bacteria strains have special mechanisms that determine their pathogenic properties, among which one of the most important in the generation of development of RI is adhesion.
Bacterial adhesion according to many authors is the main point in the colonization of the tissue surfaces of the host organism. In addition, bacterial adhesion not only contributes to the colonization of microorganisms, but conducive to the invasion of bacteria into the wall of the bladder. An important for the adhesive activity of microorganisms are: disorders of permeability or production of a mucopolysaccharide substance, blood circulation disorders of the bladder wall, the presence of ready-made receptors for interacting with microorganism receptors and reducing the protective mechanisms of the bladder wall. The larger the local and common protective mechanisms of the human body, the larger pathogenic potential may have bacterial agents.
Thus, the severity of the inflammatory process depends on the state of local and general immunity, both specific and nonspecific. Pathological changes in the immune system are one of the probable reasons leading to chronic flow and recurrence of the inflammatory process.
Standard NMP infection therapy typically includes antibacterial drugs. But none of antibiotics provide protection against ri when violating the protective mechanisms of urinary tract.
It is known that the mucous membrane of the bladder has bactericidal activity. It is proved, first of all, in relation to representatives of the family Enterobacteriaceae.disturbing the production of specific mucopolysaccharides and secretory IGA. In addition, with a long-lasting inflammatory process, the production of secretory inhibitors of bacterial adhesion, which include low molecular weight oligosaccharides, lactoferrin, and Tamm-Horsfelle protein (THP) - glycoprotein, synthesized by the cells of the tubing epithelium of the rising part of the loop of gene and convinced distal tubules and secreted in urine. The THP is both on the surface of epithelial cells and in soluble form in the urine. THP inhibits adhesion E. coli 1 type and E. coliCarrying S-Fimmpria.
The chroniization of infection is also largely given by the factors of persistence (FP) of urtopogenic strains. These include anti-interferon, anti-lib osocyne, anti-frequency activity.
In addition, multiple antibacterial therapy contributes to the formation of new clones of bacterial strains due to the transfer of genes responsible for expression of pathogenic factors.
Violate the stages of immunological protection, in addition to FP bacteria, some antibacterial drugs can be traditionally used to treat NMP infections. Therefore, sometimes there is a need to use alternative treatment approaches.
In particular, the most important link pathogenetic therapy The urine paths capable of preventing the chronosis of inflammation is recognized by immunomodulatory therapy. Its problem includes stimulation of phagocytic activity, normalization of the balance of the T-cell immunity, stimulation of interferon formation and the synthesis of non-specific protection factors. Therefore, in recent years, a number of publications appeared proving the benefits of immunomodulatory therapy. Inclusion Interferon B. comprehensive treatment The infections of the urinary system is due to the fact that the persistent bacterial infection Hard damage cells and prevents the synthesis of its own interferon. Of the three identified types of interferon man - Interferon Alpha, beta and gamma - in the treatment of latent forms of NMP infections, interferon alpha drugs are used. Among them are the most famous Viferon®, a complex preparation containing interferon alpha 2b, tocopherol acetate and ascorbic acid. It has antiviral, antibacterial and antiproliferative effect. The direct influence of the drug Viferon® on the immune system is manifested by the activation of natural killers, T-helpers, increasing the number cytotoxic T-lymphocytes and enhanced differentiation of in lymphocytes. The tocopherol and ascorbic acid in the composition of Viferon® are known to be the components of the antioxidant system and have a membrane-stabilizing effect, facilitates tissue regeneration, improve tissue breathing. These circumstances make it possible to use interferons when, with a violation of the permeability of the mucopolysaccharide substance of the bladder, antioxidant and regenerative activity is necessary to reduce inflammation processes in the bladder wall. It is shown that the rectal administration of interferon alpha 2b provides a longer circulation in the blood than with intramuscular and intravenous administration.
Materials and methods. 64 women were examined with confirmed chronic bacterial cystitis without anatomy-physiological impairment of urinary tract. The age of the surveyed patients ranged from 27 to 54 years. The survey was based on the data of clinical, laboratory, bacteriological research, consultation of the gynecologist, if necessary, the size of urethra and vagina for the polymerase chain reaction in order to exclude sexually transmitted infection. Urine crops and determination of the degree of bacteriuria were carried out according to generally accepted methods using aerobic and anaerobic cultivation techniques. The identification of selected strains of microorganisms was carried out according to morphological, tinnitorial, culture, biochemical properties. The sensitivity of the isolated microorganisms was determined to 36 antibacterial drugs.
As pathogenetic therapy 34, women (1st group) were obtained antibacterial therapy in the volume of one-time intake of phosphomycin of thrometamol (monural) in a dose of 3 g, and 30 women (2nd group) were conducted by antibiotic phosphomycin troometamol in the same dosage in combination with Interferon (Viferon®, Suppositories Rectal 1,000,000 meters). VIFERON® (recombinant interferon alpha 2b in combination with antioxidants) was assigned 1,000,000 meters per rectum 2 times a day, with an interval of 12 hours for 20 days.
Results. Randomization groups showed their comparability by age, history and clinical manifestations.
The average duration of the disease in both groups is more than 7 years.
All patients had previously repeatedly taken antibacterial drugs of various chemical groups at the next recurrence of urinary tract infection.
40.6% of women at the first symptoms of the disease independently accepted antibiotics without consulting the doctor and laboratory studies of urine.
Symptoms recorded in patients in both groups: pain, urine rapidly, imperative urge to urination, hematuria (Table 2).
The leading symptom of all examined patients was pain. To analyze the intensity and severity of pain, we used a visual analog scale (yours), offered to evaluate the patients intensity of pain on the 5-point system: 4 - very intense pain, 3 - intense, 2 - moderate, 1 - weakly pronounced, 0 - no pain ( Tab. 3).
Leukocyturia was registered in all patients. Indicator< 50х* (менее 50 лейкоцитов в поле зрения) был выявлен в 1-й группе у 9 (26,5%) пациенток и у пациенток 2-й группы 7 (23,3%) случаев, показатель ≥ 50х* (более 50 лейкоцитов в поле зрения) был диагностирован у 12 (35,3%) в 1-й группе пациенток и у 4 (13,3%) у пациенток 2-й группы. Воспалительная реакция, при которой подсчет лейкоцитов был невозможен, отмечена у 13 (38,2%) пациенток 1-й группы и у 19 (63,4%) пациенток 2-й группы. Гематурия имела место у 26,4% женщин 1-й группы и у 40% женщин во 2-й группе.
With a culture study in 94% of the urine cases, a bacterial mixture was isolated, due to both optional-anaerobic and noncommunicable-anaerobic bacteria. The average member of the urine was 10 6 CFU / ml.
Between the first and second group, statistically significant differences after treatment were observed. The overwhelming majority of women of the 1st group on the background of phosphomycin therapy was achieved a quick clinical effect. So, in 18 (53%) patients, he was characterized by the complete disappearance of the main symptoms of acute cystitis on the 3-5 day of treatment, in 5 (11.7%) patients - on the 7th day of treatment, although 7 (23.5%) The patients retained a clinical and laboratory picture of acute cystitis, which required the re-appointment of phosphomycin on the 10th day of treatment. After re-assigning the drug, clinical improvement was achieved - the disappearance of the symptoms of the disease and the lack of need for additional purpose antibacterial drugsWhat was noted in 4 (17.6%) patients. However, 3 women needed long-term antibacterial therapy with a change of antibacterial drug.
In the second group on the background of phosphomycin therapy, Trometamol + Viferon® (rectal suppositories 100 000 IU) in all cases noted the regression of clinical and laboratory indicators on the 5th day of treatment. But the complete relief of the symptoms of acute cystitis was recorded on the 6th day of treatment in 27 (90%) patients, and in 3 (10%) patients to the 15th day of treatment after the re-appointment of thromethmol phosphomycin.
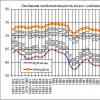
The effectiveness of the therapy was evaluated after 1, 3, 6 and 12 months.
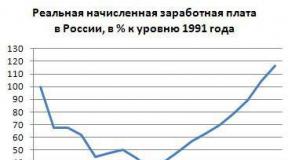
When evaluating the effectiveness of treatment for 12 months, the relapse of infection was noted after 3 months in 6% of the patients of the 1st group. After 6 months, 17.1% of women of the 1st group was prescribed again, against 6.6% of the 2nd group patients, respectively. The recurrence of the disease after 12 months was recorded in 35.3% of cases in patients of the 1st group, while in the 2nd group this indicator was 10%, which indicates a reliably higher efficiency of the combination of antibacterial drugs with interferons, in particular with the preparation of Viferon ®, in the treatment of the bottom of the urinary tract (Fig.).
.gif)
Discussion. Traditional antibiotic treatment can help with acute infection NMP, but does not provide long-term protection against ri.
Anaman data analysis revealed that all examined women on the background antibacterial therapy During the year, a recurrence of the disease was noted. The use of antibiotics of various groups did not reduce the percentage of relapse. It was also revealed that some examined women independently accepted antibacterial drugs without performing urine bacteriological analysis, and the irrational use of antibiotics led to the development of resistance and depression of the immune system.
In addition, in 94% of cases, a mix of infection was revealed, combining the association of microorganisms of various bacterial groups with multiple antibacterial sensitivity.
Therefore, the use of alternative approaches to treatment or prevention is justified, among which immunotherapy is more justified and proven today. Given the ability of interferon to increase the products of immunoglobulins, the phagocytic activity of macrophages, suppress the reproduction of bacteria, was justified by the use of Interferon in the treatment of RI NMP.
When using interferon, in combination with antibiotics in the treatment of riothe recurrence of the disease for 12 months, only 10% of the patients examined were registered.
conclusions
With the urine pathways, various immunological links of protecting the wall of the bladder are disturbed.
Therapy, combining immunomodulators and antibiotics, makes it possible to achieve a quick clinical and laboratory effect in women with RI NMP.
The data obtained require further study of the application of interferonov for the treatment of NMP.
Literature
- Zlushko E. N., Belozers E. S., Minin Yu. A.Clinical immunology. St. Petersburg: Peter, 2001.
- Laurent O. B., Petrov S. B., Pereverzev T. S., Sinyakova L. A., Vinarov A. Z., Kosova I. V. The effectiveness of the use of trimetamol phosphomycin in the treatment of patients with chronic recurrent cystitis // Effective pharmacotherapy in urology. 2008. № 4. P. 2.
- Menshikov V.V.Laboratory research methods in the clinic: directory. M.: Medicine, 1987. 383 p.
- Naja Yu. L., Kogan M. I., Gudima I. A., Ibishev, Kh. S., Kovaleva E. A.Assessment of the microbial factor in chronic cystitis / VI Russian Congress "Male Health" with international participation. Congress materials. M., 2010. P. 83-84.
- Naboka Yu. L., Gudima I. A., Ibishev H. S., Miroshnichenko E. A., Kogan M. I., Vasilyeva L. I.The etiological structure and antibiotic sensitivity of uropathogen in chronic recurrent infection of the lower urinary tract // Urology. 2011, No. 6. P. 12-15.
- Othanova T.S. Features of phytotherapy with recurrent urinary tract infection // Effective pharmacotherapy in urology. 2010. No. 1. P. 6-13.
- Pushkar D. Yu., Zaitsev A. V.Modern view of the use of Cephixim in the treatment of infection urinary tract // Russian Medical Journal. 2010. № 29.
- Pushkar D. Yu., Zaitsev A. V.Modern possibilities of immunoprophylaxis of uncomplicated urinary tract infection.
- Streltsova O. S., Tararova E. A., Kiselev E. B. Application of the drug Laveomax with chronic cystitis // Urology. 2008, No. 4.
H. S. Ibishev,doctor of Medical Sciences, Professor
GBOU VPO ROSGMU MINDRESSOVITIVITY OF RUSSIA,Rostov-on-Don
Why small children so often sick and what preventive measures Assist to strengthen their immunity.
How often do children have recurrent infections?
Children are born with an immature immune system, so infectious diseases often have infectious diseases, as a rule, once in one or two months. Soon after birth the immune system The child begins to develop, and over time the frequency of infectious diseases is reduced. As a rule, school-age children suffer from recurrent infections them are no more often than adults.
Why do the doctor can alarm the recurrences of infections in a child?
Most doctors beat alarm if ordinary viral infections Children are complicated by bacterial, such as sepsis or pneumonia. Frequent or unusual infections are also a reason for concern.
Why do some children have infectious diseases more often than usual?
Sometimes the reasons lie on the surface. For example, the whole thing may be that the child goes to a kindergarten, where children touch shared toys and touch each other, spreading the infection. Adults are much less in contact with other people's microbes, therefore they are not infected so often.
Another reason for a runny nose and sneezing in young children is passive smoking. Since more and more women of childbearing are smoking, passive smoking more often becomes respiratory infections in children. Now has its connection with infections and asthma in childhood.
Can be the cause of recurrent infections anatomical features?
The common cause of recurrent infections in children is the features of the structure of the nasal sinuses and Eustachius pipes (channels connecting the middle ear with a throat). Such infections can be inherited. In some children, the anatomical features make it difficult to the outflow of separated from Eustachius pipes and the nasal sinuses, which is why bacteria begin to multiply. Therefore, such children are more susceptible to infections. In most cases, as the child grows, the drainage improves. Children younger ageAlways suffering from ear infections, you may need treatment with antibiotics or the introduction of special tubes to drain the middle ear.
Allergy and asthma can lead to a recurrent sinusitis (nasal congestion or the appearance of discharge from it). Allergies sometimes cause long-term irritation in the nose. Because of him, the ducts of the nose and the nasal sinuses through which the outflow of the discharge occurs, they scatter, their lumen is closed. Bacteria multiply, leading to infection. In such cases, drugs need to eliminate the cause of the disease, that is, allergies.
Cough accompanying a viral infection may be a sign of asthma. So children need medicines from asthma in addition to other medicines they take from infection.
Why do children have severe recurrent infections?
Sometimes it is just a matter of chance. Even healthy children can change 2-3 severe infections without a visible reason. In such cases, the doctor may appoint additional surveys to make sure that the child has no immunodeficiency. Immunodeficiency states - the main reason for repeating heavy infections.
Other possible reasons There may be diseases such as fibergation and AIDS. Mukobovidosis is very rare, and the AIDS child in the overwhelming majority of cases receives from the mother.
How to protect the child from recurrent infections?
- Smoking parents need, first of all, quit smoking. If it is not yet possible, you should stop smoking at home and in the car. To protect the child from passive smoking, not smoking only in the children's room is not enough: tobacco smoke spreads everywhere. Air filters also do not protect children from passive smoking.
- The most "cold" season is winter. If someone from relatives can take care of the child, it is better to pick it up from a kindergarten for the winter, where children are often cold. Another good option is small home groups (up to 5 children). Less children are fewer infections that can be picked up.
- If the family has a hereditary predisposition to allergies or asthma, it is worth checking if these diseases do not have these diseases.
- Caution: Ear candles. American Food quality supervision and medicines Does not recommend using ear candles. They can lead to serious injury, and their effectiveness is not confirmed by scientific research.
Everything will be fine?
Most children suffering from recurrent infections are not serious health problems, and they will grow healthy people. Already closer to school age They will hurt much less often. It is only necessary to take care that the children have more sleep and eat right. Sleep and healthy food are as important to combat infections, like medications.
Recurrent urinary infection
Recurrent urinary infection (RMI) is pretty frequent disease. Massage, pathogenesis and treatment of RMI depend on the floor and age of the patient. Treatment of urinary tract infection (IMP) is best to discuss separately, especially highlighting a group of patients with special risk - women before menopause.
Women in front of menopause
At least 1/3 of women there is an uncomplicated sharp IMT, and most of them have the beginning of the disease at the beginning of the maturity period after the completion of the puberty period. Now it is known that bacteria, causing infection Urinary tract in such women develops from fecal microflora. Sexual activity is the main risk factor of clinically significant implies, while the degree of risk depends on sexual practice, as well as on the frequency and regularity of the sexual acts. The period of 48 hours after the vaginal intercourse is the period of the greatest risk. The use of oral contraceptives, urination before the sexual act, the frequency of the arms, the direction of movement of the toilet paper after the act of defecation, the use of tampons - all this does not affect the risk of developing Imp. Urination after sexual intercourse seems to reduce the risk of imp. The use of a vaginal diaphragm increases the risk of developing bacterurium, but not clinically significant imp.
Approximately 20% of women with one episode imposed in the findings are noted relapses of infection. The mixture is mainly determined by the pathologically large number of fecal bacteria on the mucous membrane of the vagina and urethra.
When recurrences, impregnating, incomplete therapy of infection, the preserving bacteriuria is not the main problem. The reason for the unsuccessfulness of medication therapy in most cases is the resistance of bacteria.
If bacteriuria is continuously preserved and impacted, the reason for this is the infection or reinfection in the patient's body. Preservation of infection is repeated appearance UTI from the hearth within the urinary tract, in women, the preservation of infection can be caused by stones, fistulas, a diverticulous, and other relatively rare abnormalities of the urogenital system development. Reinfection, in turn, arises from a focus that is not associated with the urinary system. Among the factors causing the emergence of RMI in women, reinfection occurs more often than the preservation of infection. This is not surprising if we take into account the length of the urethra in women and the proximity of the outer opening of the urethra to the infected mucous membrane of the vagina.
Collect information and diagnostics
Approximately 20-40% of women with a clinically significant determin number of bacteria in the urine is less than 105 / ml. In patients with dysuria, a more suitable threshold for determining significant bacteriuria is considered to be 102 / ml of the famous pathogen in the urine sample obtained by the catheter. With rim such, E. coli is most often most often. With urine screening analysis, severe pyuria is almost always revealed, which allows doctors to start preliminary therapy. Urine tests also help retperiate the RMI from other unsepar factors causing symptoms of dizuri in women.
The testimony for visualizing urological studies and cystoscopy in women in front of menopausosis is not defined and depend on what glances to the treatment of this pathological condition adheres to the attending physician, as well as information about a particular patient. A typical relapse due to reinfection is most often due to sexual act and is etiologically connected with E. coli. Atypical circumstances are considered to be infected with causative agents, decomposing urea, obstructive symptoms associated with urination, and such a sign of involvement in the process of the upper urinary tract, as pain on the side surface of the body. Suspicion of preservation of infection, and not to reinfection, occurs if the Imp repeats 2 weeks after the end of therapy. These circumstances should cause a physician on the presence of the sick anatomical or structural change. Such patients with RMI must be sent to an urologist for in-depth examination and treatment.
As already noted, some women have a biological predisposition to RMI resulting from the colonization of the vagina and whether the periurethral tissues of the fecal microflora. Understanding this process led to clinical trials killed by heat of vaginal stamps of oliform bacteria as means of immunization of patients against RMI.
Prevention with antibiotics is the most significant practical measure for most women. Since 85% of women with RMi appearance of the symptoms of the disease is observed in the 1st day after sexual intercourse, then the preventive purpose of antibiotics after sexual intercourse should be tested before the "normal" course of antibacterial therapy is tested. Randomized, double-blind, controlled tests of various drugs proved the effectiveness of this approach.
For prevention after sexual intercouction, co-trimoxazole, furadonin, quinolone, cephalosporins and sulfisoxazole were tested. The first three of these funds gave a partial effect, from which it follows that the decision to conduct a longer course should be taken with the ineffectiveness of prevention after sexual intercourse.
Despite the fact that the results of the use of antibiotics were successful, from the choice as a therapeutic agent in this case is not unambiguous. Comparative tests of KO-Trimoxazole and Furadonin gave approximately the same results, despite the assertion that co-trimoxazole is capable of provoking the selection of sustainable stamps of intestinal and vaginal microflora. Furadonin, although it does not affect the intestinal microflora, with long-term treatment it is capable of causeing irreversible fibrosis of the lungs in some patients, and therefore some doctors do not recommend it. Hinolone seems to have a slightly greater efficiency, although they are more expensive. These drugs are not only sterilized by urine, but also contribute to the elimination of urinary microflora, inhabiting urethra and zones in the natural holes of the body.
In the absence of the effect of the prevention of infection after sexual intercourse, women conduct coursework with a duration of 6-12 months.
Women after menopause
The estrogens circulating with blood stimulates the colonization of the vagina with lactobacteriums. These bacteria produce glycogen milk acid, which maintains low pH values \u200b\u200binto the vagina, and this factor inhibits the growth of many bacteria. In the absence of sexual activity, this mechanism is effective to preserve urine sterility.
According to some reports, 10-15% of women over the age of 60 are often observed imp. After the occurrence of menopause changes in the vaginal microflora due to the lack of circulating with the blood of estrogen play, as is commonly considered, a key role in the occurrence of this significant dependence. Due to the disappearance of lactobacterium, Enterobacteriaceae is colonized, first of all E. coli.
Treatment of women in the period after menopause
Treatment of RMI in women of this age group should be essential to the replacement therapy with estrogens. The results of several studies using Estor PER OS confirmed the effectiveness of this method of preventing RMI. However, one large-scale test study, nevertheless showed that the use of Estrogen PER OS corresponded to a two-time increase in the risk of the first episode of the IMP.
Other conclusions regarding the effectiveness of the systemic administration of estrogen patients of the age group also turned out to be unpassed. Therefore, a randomized, double-blind control study of the local application of a cream containing estriol was carried out. This technique made it possible to significantly reduce the pH into the vagina, to increase its colonization with lactobacteriums and reduce the colonizing number of Enterobacteriaceae without manifestation of systemic effects of estrogen. It is especially important that the number of PM data has significantly decreased compared to the group where Placedo was used.
The local use of estrogen preparations (introduction into the vagina) seems to be a methodology for selecting initial therapy for many patients after menopause, although the course prevention of antibiotic doses is still necessary for many patients. Studies conducted for several years have shown the long-term effectiveness of therapy with many drugs, while there is little data about increasing the resistance of bacteria or an increase in the toxicity of therapy.
PREGNANT WOMEN
The dominance of RMI among pregnant women is similar to the picture marked among sexually active non-embled, as well as women under the age of menopause. RMi during pregnancy, however, can develop to the degree of acute pyelonephritis, which is happening about 1/3 of cases. This frequency may be associated with the dilatation of the upper urinary tract and, ultimately, with stained, noted often at the end of pregnancy.
An obvious increase in the number of imparts in the upper sections of the urinary tract with a fever occurring during pregnancy, convinced the need to apply more energetic measures to prevent the emergence of the infection of the lower unit of the urinary tract of pregnant women. Comparative data on the frequency of impresses in pregnant women and non-remote women show that 43% of women (who have been developed during pregnancy) imp to pregnancy, and it seems to indicate the overall mechanism for the development of infection in all women to stop menstruation, independently From the factor of pregnancy.
Treatment of pregnant women
Many schemes of antibacterial therapy RMI during pregnancy were proposed. Without a doubt, with asymptomatic bacteruria, the patient of the high risk group therapy is shown. Many believe that prevention should be carried out after therapy of the first impression during pregnancy, especially if the patient has an anamnesis has already been imp. The optimal course of therapy, including the choice of drugs and the duration of the course, is still discussed. Nevertheless, most obstetres recommend using furadonin or benzylpenicillin.
As before Menopause, when imposed after sexual intercourse, pregnant women were investigated by the effectiveness of post-cellular antibacterial prevention as "starting" therapy. This technique was ultimately, as effective as the daily, single therapy. In a newly conducted examination of 39 women who, during previous pregnancies, a total of 130 Imps were noted, during the observation period, only one pregnant woman was noted after the start of therapy. In this case, a one-time dose of cephalexin or furadonin was used. The advantage of postcoital prophylaxis in comparison with the daily is to apply the minimum amount of drugs. It seems that the use in this case co-trimoxazole or furadonin can be effective, but it should be emphasized that only benzylpenicillin and cephalosporins are known as means of safe for use at all stages of pregnancy.
Infectious and inflammatory processes in the bladder preserve today in urology, the status of a global problem due to the greatest risk of transition to a chronic clinic of the current frequent manifestation recurrences of the disease and inconsistency traditional treatment. According to statistics (for the last five-year period), the recurrent cystitis was diagnosed with 50% of young girls and women of childbearing age, more than 70% of patients were accompanied by various dysfunctions in the urinary system.
Despite the fact that the non-complicated acute clinic of cystitis is pretty easy, it often recurrences. Half patients recurrences are noted several times a year, and the elderly patients (in 55 years) cystitis can return every month. In medicine, it is customary to share pathology on recurrent infection and reinfection.
Recurrent, the disease is called in the presence of manifestations of three and more episodes for the year. At the same time, the same infectious pathogen preserves with which they fought in the treatment of primary pathology. Reinfection is called cystitis caused by a different microbial pathogen, intestinal, or "coming" from the perianal zone.
A deep study of this problem with scientists showed that the recurrence of cystitis in 90% of patients examined, this is a new pathology, and not a relapse of the previous one.
Probable reasons for frequent cystitis
Scientists voiced several versions of the etiology of the development of recurrence of the disease - these are individual physiological, vegetative and psycho-emotional violations, which are largely contradictory and are still under discussion. But one thing, what did the physicians come to and what there is no disagreement, this is the immune component, which is the most important link in pathogenesis inflammatory processesdetermining the individual clinic of the course of the disease and its outcome.

Today, the reasons for frequent cystitis in women are accepted to explain by classical generally accepted physiological impairment with many concomitant factors, and psychosomatic disorders.
Physiological reasons are due to:
- Anomaly anomaly arrangement of urethral outer outlet - dystopia (the outer opening of the urethra is located on the front vaginal wall).
- Defect in the development of MP (ectopia) - the front wall of the organ is missing, and the back will act in the zone of the underdeveloped Lonnoy articulation.
- Congenital hypermobility of urethra.
- The presence of urethro-hymenile weights (adhesions) that contribute to the cast of the vaginal secret to the urethral channel, thereby making the introduction of infection in the urinary system.
- The presence of urethral strictures (narrowing of the canal) that prevent the free outflow of urin.
- The weakening of the muscular-ligament apparatus of the pelvic bottom, which contributes to the accumulation of residual urin in the urinary reservoir cavity, initiates an increase in the pathogen population and the development of infectious-inflammatory reactions in MP.
Causes of psychological character
More Ancient Healers Since the Time of Hippocratic, the connection of all the "reel" of a person with nerves. Research in this direction by modern scientists confirmed this hypothesis. For example, parasympathetic department is answered for emptying MP nervous system, And urination delay processes regulates its sympathetic department. Any imbalance in the vegetation system (VNS) is able to lead to functional violations MP and development in its structural tissues of inflammatory processes.

Frequent manifestation of cystitis in women psychologists and neurologists associate with problems of metaphysical and psychological nature.
Metaphysical genesis is due to:
- feeling of fear and awareness of complete insecurity;
- anxiety and anxiety on the background psychological influence, without the possibility of throwing out the negative;
- disappointments, resentment and irresistible desire to revenge the guilty;
- problems in sexual relationships.
The psychological factor is often associated with difficult circumstances in life:
- with manifestation of resentment and anger;
- uncertainty in itself and fear;
- alarms and jealousy;
- experiences and loneliness.
The recurrence catalyst can be and long contained positive emotions that cannot be splashing openly. Prolonged emotion suppression provokes internal stress and the development of a number of internal pathologies.

Among the concomitant factors explaining why cystitis returns again and again, note:
- premature interruption of the course of treatment;
- individual susceptibility to re-reinfection;
- increased loads and injuries of the lower back zone;
- the influence of venereal infections;
- insufficient compliance with hygiene (after intimate acts and defecation).
Statistics of the results of the study of this problem shows that infectious-inflammatory ascending defeat of MP, a local weakening of the mechanisms of protection of the urine-bubble body and the system of urinary in general, anatomical anomalies of the urethral channel, disruption of urodynamic functions of MP and background gynecological problemsare the main factor that supports, and sometimes provoking the development of inflammation reactions in tissues of the tank bubble cavity, and the main cause of oppression of immunity (immunosuppression).

The main orientation of therapy is the restoration of the protective mechanisms of the urinary system and its sanitation. The principle of therapeutic treatment of the recurrent clinic of cystitis in women is due to the definition and timely relief of the factor supporting the persistent clinic of the disease. Therapeutic course includes:
- The use of local and overall anti-inflammatory and antibacterial therapy. Since recurrences cystitis, it is almost always a new pathology, identifying the pathogen necessarily. Since it may be a completely different pathogen and the appointment of standard antibiotics will not give results. Today, accurate analysis gives tank-sowing from bubble bioptate tissues. Recommendations for antibiotic therapy with a course for at least a week include - the purpose of the drugs according to the detected pathogen, for example - norfloxacin (0.4 g 2 times / day), -Klavulanta (0.375 g 3 times / day), the cefuroxime Axietyl (0.25 g 2 times / day).
- Elimination of urodynamic disorders (techniques of operational interventions, laser rejuvenation, etc.).
- Correction of hygienic and sexual factors (timely emptying of MP, personal hygiene, permanent partner, and protected sexual contact).
As practice has shown, the standard classical therapy of cystitis, with a recurrent form, does not give effective results, which leads to frequent recurrent processes. The stability and effectiveness of the results showed only immunostimulating methods - the appointment of a ten-day course of intravenous and intravenous ozone therapy (bubble - 1000 μg / l, intravenous - 500 μg / l).

It is noted that good protective immunological indicators are achieved in a combination of immunomodulators - geniferon with ciploofloxacin and cilloofloxacin in combination with ozone therapy, which improves the therapeutic effect and allows you to achieve an excellent result in the treatment in a short period of time. Alternatively, the oral administration of the Uro-Wax may be prescribed.
- ban on the use of spermicides (female contraception);
- timely complete liberation of the urine-bubble tank;
- compliance with peace regime during the exacerbation period;
- providing abundant drinking regime;
- strict adherence to the dosage and course appointed by a doctor of prophylactic antibacterial therapy is a single reception before bedtime low doses of ciprofloxacin (100 mg), offloxacin (100 mg.). Course individual;
- related to sexual contacts - individual dosage preparations should be taken immediately after intimate proximity;
- antibiotic pylaxis in front of each procedure of urological invasive manipulations;
- using intravaginal and periurethral hormonal masses (For example, Ovrestin) women of old age (in postmenopausal).
Important component of prevention - power and abundant use of liquid.
- With frequent cystitis, salted products should not be present in the diet, as they contribute to the accumulation in the tissues of excess fluid and the formation of swelling.
- It is necessary to refuse from oily food, as it is capable of negatively affects metabolism processes in the body (metabolic processes).
- Refrain from spices, carbonated, coffee and alcoholic beveragesTo protect the mucous tissues from strong irritation.
- The diet should be saturated with protein food. It is the basis for the formation of the necessary antibodies for phagocytic protection.
- It is necessary in the menu dishes from vegetables and fruits, as they effectively remove toxins and free radicals from the body.
- Equally important is the abundant use of juices, mineral water, horses, compotes and green tea. Drinking a day of up to 2 liters of fluid can be prevented by stagnation of urins in the urine-bubble tank, which will deprive the pathogens of the reproduction environment.
From all this, it should be concluded - if the exacerbation of cystitis over the past six months, at least twice, it is necessary to undergo diagnosis, to identify the cause and on time to eliminate it. Otherwise, recurrences of the disease will chase a woman with "enviable constancy", pretty spoiling life.
Read also ...
- The work of "Alice in Wonderland" in a brief retelling
- That transformation. "Transformation. Attitude towards the hero from the sister
- Tragedy Shakespeare "King Lear": the plot and the history of the creation
- Gargantua and Pantagruel (Gargantua et Pantagruel) Francois Rabl Gargantua and Pantagruel Brief