Cephalosporins 3 and 4 generations list. IV generation cephalosporins in the treatment of severe infections in children. Pathogen resistance to antibiotic therapy
Content
Antibacterial drugs according to the mechanism of action and the active substance are divided into several groups. One of them are cephalosporins, which are classified by generations: from the first to the fifth. The third is more different high efficiency against gram-negative bacteria, including streptococci, gonococci, Pseudomonas aeruginosa, etc. This generation includes cephalosporins for both internal and parenteral use. They are chemically similar to penicillins and can replace them if you are allergic to such antibiotics.
Classification of cephalosporins
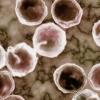
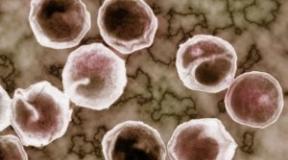
This term describes a group of semi-synthetic beta-lactam antibiotics that are derived from "cephalosporin C". It is produced by the fungus Cephalosporium Acremonium. They secrete a special substance that inhibits the growth and reproduction of various gram-negative and gram-positive bacteria. Inside the cephalosporin molecule there is a common core, consisting of bicyclic compounds in the form of dihydrothiazine and beta-lactam rings. All cephalosporins for children and adults are divided into 5 generations depending on the date of discovery and the spectrum of antimicrobial activity:
- First. The most common parenteral cephalosporin in this group is Cefazolin, oral - Cefalexin. They are used in inflammatory processes of the skin and soft tissues, more often for prevention. postoperative complications.
- Second. These include drugs Cefuroxime, Cefamandol, Cefaclor, Ceforanide. They have increased, compared with 1st generation cephalosporins, activity against gram-positive bacteria. Effective in pneumonia, combined with macrolides.
- Third. In this generation, the antibiotics Cefixime, Cefotaxime, Ceftriaxone, Ceftizoxime, Ceftibuten stand out. They are highly effective in diseases caused by gram-negative bacteria. Used for infections of the lower respiratory tract, intestines, inflammation of the biliary tract, bacterial meningitis, gonorrhea.
- Fourth. Representatives of this generation are antibiotics Cefepim, Cefpir. May affect enterobacteria that are resistant to 1st generation cephalosporins.
- Fifth. They have a spectrum of activity of cephalosporin antibiotics of the 4th generation. They act on flora resistant to penicillins and aminoglycosides. Effective in this group of antibiotics are Ceftobiprol, Zefter.
The bactericidal action of such antibiotics is due to the inhibition (inhibition) of the synthesis of peptidoglycan, which is the structural main wall of bacteria. Among the general features of cephalosporins, the following can be noted:
- good tolerance due to the minimum amount side effects compared to other antibiotics;
- high synergism with aminoglycosides (in combination with them they show a greater effect than individually);
- manifestation of cross allergic reaction with other beta-lactam drugs;
- minimal impact on the intestinal microflora (on bifidobacteria and lactobacilli).
3rd generation cephalosporins
This group of cephalosporins, unlike the previous two generations, has a wider spectrum of action. Another feature is a longer half-life, due to which the medicine can be taken only once a day. The ability of third-generation cephalosporins to overcome the blood-brain barrier can also be attributed to the advantages. Due to this, they are effective in bacterial and inflammatory lesions. nervous system. The list of indications for the use of third-generation cephalosporins includes such diseases:
- meningitis of a bacterial nature;
- intestinal infections;
- gonorrhea;
- cystitis, pyelonephritis, pyelitis;
- bronchitis, pneumonia and other infections of the lower respiratory tract;
- inflammation of the biliary tract;
- shigillosis;
- typhoid fever;
- cholera
- otitis.
Cephalosporins 3 generation tablets
Oral forms of antibiotics are convenient to use and can be used for complex therapy at home infections of bacterial etiology. Oral cephalosporins are often prescribed in a stepwise regimen of therapy. In this case, antibiotics are first administered parenterally, and then switched to forms that are taken orally. So, oral cephalosporins in tablets are represented by the following drugs:
- Cefodox;
- Pancef;
- Cedex;
- Suprax.

The active ingredient in this drug is cefixime trihydrate. The antibiotic is presented in the form of capsules with a dosage of 200 mg and 400 mg, suspensions with a dosage of 100 mg. The price of the first is 350 rubles, the second is 100-200 rubles. Cefixime is used for diseases of an infectious and inflammatory nature caused by pneumococci and streptococci pyrrolidonyl peptidase:
- acute bronchitis;
- acute intestinal infections;
- acute pneumonia;
- otitis media;
- relapses of bronchitis chronic form;
- pharyngitis, sinusitis, tonsillitis;
- infections urinary tract proceeding without complications.
Cefixime capsules are taken with meals. They are allowed for patients over 12 years of age. They are shown a dosage of 400 mg of Cefixime daily. Treatment lasts according to the infection and its severity. Children from six months to 12 years of age are prescribed Cefixime in the form of a suspension: 8 mg / kg of body weight 1 time or 4 mg / kg 2 times a day. Regardless of the form of release, Cefix is prohibited in case of allergy to antibiotics of the cephalosporin group. After taking the drug, the following adverse reactions may develop:
- diarrhea;
- flatulence;
- dyspepsia;
- nausea;
- stomach ache;
- rashes;
- urticaria;
- itching;
- headache;
- dizziness;
- leukopenia;
- thrombocytopenia.
Cefodox
The bactericidal effect of this antibiotic is due to cefpodoxime in the composition. Release form this drug- tablets and powder. Suspensions are prepared from the latter. Regardless of the form of release, Cefodox is used to treat:
- pyelonephritis, mild cystitis or moderate;
- tonsillitis, pharyngitis, laryngitis, sinusitis, otitis;
- pneumonia, bronchitis;
- urethritis, proctitis, cervicitis of gonococcal origin;
- infectious lesions of the skin, joints, bone and soft tissues.
The use of Cefodox is not practiced in people with hypersensitivity to the composition of the drug. In tablet form, the antibiotic is not prescribed for children under 12 years of age, in the form of a suspension - under the age of 5 months, with galactose intolerance, malabsorption syndrome, lactase deficiency. The dosage of Cefodox is determined as follows:
- 200-400 mg per day - for patients over 12 years old (average dose);
- 200 mg - for infectious diseases of the respiratory and genitourinary systems;
- 400 mg - with bronchitis or pneumonia.
The course of therapy continues as prescribed by the doctor. Its average duration depends on the course of the disease and is determined by a specialist. The price of the drug is about 350-400 rubles. The list of side effects of Cefodox includes the following symptoms:
- rash;
- skin itching;
- headache;
- diarrhea;
- vomiting, nausea;
- eosinophilia;
- an increase in plasma levels of creatinine and urea;
- violation of thrombopoiesis and leukocytopoiesis.
panzef
This representative of 3rd generation cephalosporins is based on cefexime. You can buy Pancef in the form of tablets and granules. They are indicated for the treatment of infectious diseases of various body systems:
- urinary. Pancef is effective in gonococcal urethritis and cervicitis.
- Respiratory. This antibiotic is indicated for acute and chronic bronchitis, tracheitis, pneumonia.
- ENT organs. Pancef is prescribed for otitis media, pharyngitis, infectious sinusitis, tonsillitis.
The contraindications of this drug include sensitivity to penicillins and cephalosporins, the elderly and the age of up to six months. The dosage is determined taking into account the following principles:
- 8 mg / kg 1 time or 4 mg / kg 2 times a day - for patients from 12 years old;
- 400 mg - the maximum drug per day;
- 400 mg for 7-10 days, 1 time per day - with gonorrhea that occurs without complications.
- 8 mg / kg 1 time or 4 mg / kg 2 times a day (6-12 ml of suspension) - for children 5-15 years old;
- 5 ml of suspension - for children 2-4 years old;
- 2.5-4 ml of suspension - for babies from 6 months to a year.
The cost of 6 tablets of Pancef 400 mg each is 350 rubles, 5 ml of suspension - 550 rubles. Side effects of the drug appear more often from the digestive tract, but there are other reactions:
- anorexia;
- dysbacteriosis;
- dizziness;
- fever;
- flatulence;
- nausea;
- dysbacteriosis;
- vomit;
- jaundice;
- dry mouth;
- hyperbilirubinemia;
- glossitis;
- stomatitis;
- nephritis;
- skin hyperemia;
- eosinophilia;
- hives.
Cephalosporin 3 generation Spectracef exists only in tablet form. Its active ingredient is cefditoren at a dosage of 200 mg or 400 mg. Microorganisms that cause such pathologies are sensitive to this substance:
- Upper respiratory diseases, including acute sinusitis and tonsillopharyngitis.
- Uncomplicated infections of the subcutaneous fat and skin, including impetigo, abscess, folliculitis, infected wounds, furunculosis.
- Infectious lesions of the lower respiratory tract, such as community-acquired pneumonia. This also includes periods of recurrence of chronic bronchitis.
Spectracef should be taken with a liquid and preferably after a meal. The recommended dose is determined by the type of infection and its severity:
- 200 mg every 12 hours for 5 days - with exacerbation of bronchitis;
- 200 mg every 12 hours for 10 days - for skin infections, sinusitis, pharyngotonsillitis;
- 200 mg every 12 hours for 4-5 days - for community-acquired pneumonia.
Compared to other cephalosporins, Spectracef has a higher cost - 1300-1500 rubles. For a list of side effects, see detailed instructions to the remedy because they are numerous. Spectracef contraindications include:
- allergy to constituent drugs and penicillins;
- children under 12;
- hypersensitivity to casein protein;
- liver failure;
- breast-feeding;
- pregnancy;
- hospital stay on hemodialysis.

Cedex
One capsule of Cedex contains 400 mg of ceftibuten dihydrate, 1 g of this preparation in the form of a powder contains 144 mg of this active component. Their price varies from 500 to 650 rubles. The list of indications for both forms of release of the drug includes such diseases:
- enteritis and gastroenteritis in children caused by Escherichia coli or strains of the genus Shigella and Salmonella;
- otitis media;
- pneumonia, bronchitis, scarlet fever, pharyngitis, acute sinusitis, tonsillitis;
- urinary tract infections.
Cedex is contraindicated in case of allergy to penicillins, intolerance to cephalosporins, severe form kidney failure and patients on hemodialysis. Age restrictions: suspension is allowed from 6 months, capsules - from 10 years. The dosage is determined as follows:
- 400 mg every day - with acute sinusitis and bronchitis;
- 200 mg every 12 hours for 10 days - with community-acquired pneumonia;
- 9 mg / kg suspension - for children from six months to 10 years.
Treatment on average lasts for 5-10 days. With the defeat of Streptococcus pyogenes, therapy should last for at least 10 days. List of possible adverse reactions:
- drowsiness;
- dyspepsia;
- anemia
- eosinophilia;
- gastritis;
- headache;
- dizziness;
- convulsions;
- urticaria;
- nausea, vomiting;
- thrombocytosis;
- ketonuria;
- taste changes;
- abdominal pain.
Suprax
The drug Suprax is available in the form of dispersible tablets, i.e. soluble in water. Each contains 400 mg of cefixime. The cost of 7 tablets is about 800 rubles. List of indications for the use of Suprax:
- uncomplicated gonorrhea of the urethra or cervix;
- shigellosis;
- angina agranulocytic;
- acute bronchitis;
- urinary tract infections;
- acute pharyngitis;
- otitis media, sinusitis, tonsillitis.
You can not use Suprax for colitis, kidney failure, pregnancy, colitis and in old age. You can take the drug regardless of food. The daily dose is calculated as follows:
- 400 mg for 1-2 doses - with a body weight of more than 50 kg;
- 200 mg at a time - with a weight of 25 to 50 kg.
With gonorrhea, treatment lasts 1 day, with mild infections of the genitourinary system - 3-7 days, with angina - 1-2 weeks. To prepare a suspension, one tablet must be crushed and poured with a small amount of water, then shake well. List of side effects on Suprax:
- nephritis;
- rash;
- hives;
- headache;
- constipation;
- vomit;
- skin itching;
- nausea;
- pain in the epigastric region;
- bleeding;
- kidney dysfunction.
in powder form
To prepare a solution for the purpose of injection, third-generation cephalosporins are used in the form of a powder. When administered intramuscularly, drugs have more fast action and rarely cause adverse reactions because they enter the body bypassing the digestive tract. Also, antibiotics of the cephalosporin series in the form of a powder are used for those who, due to physiological characteristics can't take pills. From this form of drugs, a suspension can be prepared that is easier to give to children.
The active ingredient of Fortum is ceftazidime at a dosage of 250, 500, 1000 or 200 mg. The drug is presented as a white powdery mass for the preparation of solutions for injection. The cost of 1 g is 450 rubles, 0.5 g - 180 rubles. The list of indications for the use of Fortum includes infections:
- respiratory tract, including lesions on the background of cystic fibrosis;
- ENT organs;
- organs of the musculoskeletal system;
- subcutaneous tissue and skin;
- urinary tract;
- infections caused by dialysis;
- in patients with suppressed immunity;
- meningitis, bacteremia, peritonitis, septicemia, infected burns.
Fortum is contraindicated in case of sensitization to ceftazidime, penicillins and antibiotics from the 3rd generation cephalosporin group. With caution, the drug is prescribed to pregnant and lactating women, with renal failure and in combination with aminoglycosides. The daily dose is selected as follows:
- the dosage per day should not be more than 6 g;
- adults are administered 1–6 g, divided into 2–3 doses;
- with reduced immunity and severe forms of infections, 2 g is administered 2-3 times or 3 g 2 times;
- with damage to the urinary tract, 0.5-1 g is administered 2 times.
Adverse reactions after the introduction of Fortum, they can manifest themselves from almost all systems and organs. More often patients note:
- nausea;
- diarrhea
- vomiting;
- candidiasis of the mucous membranes of the mouth and pharynx;
- abdominal pain;
- dizziness;
- fever
- paresthesia;
- tremor;
- convulsions;
- angioedema;
- neutropenia;
- thrombophlebitis;
- urticaria;
- itching, rash.

Tizim
This antibiotic is based on ceftazidime. One vial of Tysim contains 1 g of the indicated active ingredient. The price of the drug is 300-350 rubles. The list of diseases in which Tizim is effective includes the following pathologies:
- sepsis;
- cholangitis;
- peritonitis;
- infections of bones, skin, joints, soft tissues;
- pyelonephritis;
- infected burns and wounds;
- infections caused by hemodialysis and peritoneal dialysis.
The dosage is set for each patient individually, taking into account the localization and severity of the course of the disease. The drug is administered intramuscularly or intravenously in the following dosages:
- 0.52 g every 8-12 hours - for adults;
- 30-50 mg per 1 kg of body weight 2-3 times a day - for children from 1 month to 12 years;
- 30 mg/kg/day. With an interval of 12 hours - for children up to 1 month.
Maximum per day is allowed to enter no more than 6 g of Tizim. Contraindication to the use of this drug is high sensitivity to ceftazidime. The list of possible side effects includes:
- nausea, vomiting;
- hepatitis;
- cholestatic jaundice;
- eosinophilia;
- diarrhea
- hypoprothrombinemia;
- interstitial nephritis;
- candidiasis;
- phlebitis;
- soreness at the injection site.
drug interaction
When using 3rd generation cephalosporins against the background of alcohol consumption, there is a high risk of developing a disulfiram-like effect. This deviation is similar to the state of the body in case of poisoning. ethyl alcohol. Against this background, the patient develops an aversion to alcohol. The effect persists for several days after the abolition of cephalosporins. The danger is the possible development of hypoprothrombinemia - an increased tendency to bleed. Interactions of cephalosporins with drugs:
- simultaneous reception of antacids reduces the effectiveness of antibiotic therapy;
- combination with loop diuretics is not allowed due to the risk of nephrotoxic effect;
- combination with thrombolytics, anticoagulants and antiplatelet agents is also not recommended due to an increased likelihood of intestinal bleeding.
Video
Did you find an error in the text?
Select it, press Ctrl + Enter and we'll fix it!
4th generation cephalosporins are considered relatively new. There are no oral forms in this group. The remaining three are oral and parenteral agents. Cephalosporins have high efficiency and relatively low toxicity. Thanks to this, they occupy one of the leading positions in terms of frequency of use in clinical practice of all antibacterial agents.
Indications for use for each generation of cephalosporins depend on their pharmacokinetic properties and antibacterial activity. Medicines are structurally similar to penicillins. This predetermines a single mechanism of antimicrobial action, as well as cross-allergy in a number of patients.
Cephalosporins have a bactericidal effect. It is associated with a violation of the formation of bacterial cell walls. In the series from the first to the third generation, there is a tendency to a significant expansion of the spectrum of action and an increase in antimicrobial activity against gram-negative microbes, with a slight decrease in the effect on gram-positive microorganisms. The property common to all agents includes the absence of a significant effect on enterococci and some other microbes.
Many patients are interested in why 4th generation cephalosporins are not available in tablets? The fact is that these medicines have a special molecular structure. This does not allow the active components to penetrate into the structures of the cells of the intestinal mucosa. Therefore, 4th generation cephalosporins are not available in tablets. All medicines in this group are intended for parenteral administration. 4th generation cephalosporins are produced in ampoules with a solvent.
Preparations of this group are prescribed exclusively by specialists. This is a relatively new category of medicines. Cephalosporins 3, 4 generations have a similar spectrum of effects. The difference is in fewer side effects in the second group. Cefepime, for example, is close to third-generation medicines in a number of ways. But due to some features in the chemical structure, it has the ability to penetrate the outer wall of gram-negative microorganisms. At the same time, Cefepime is relatively resistant to hydrolysis by beta-lactamases (chromosomal) of the C-class. Therefore, in addition to the characteristics characteristic of 3rd generation cephalosporins (Ceftriaxone, Cefotaxime), the drug exhibits such features as:
- influence on microbes-hyperproducers of beta-lactamase (chromosomal) C-class;
- high activity relative to non-fermenting microorganisms;
- higher resistance to hydrolysis of extended spectrum beta-lactamases (the significance of this feature is not fully understood).
This group includes one drug "Cefoperazone / Sulbactam". In comparison with a mono-drug, the combined drug has an extended spectrum of activity. It has an effect on anaerobic microorganisms, most strains of enterobacteria capable of producing beta-lactamase.
Parenteral cephalosporins 3, 4 generations are very well absorbed when injected into the muscle. Medications for oral administration are highly absorbed in the gastrointestinal tract. Bioavailability will depend on the specific drug. It ranges from 40-50% (for Cefixime, for example) to 95% (for Cefaclor, Cefadroxil, Cefalexin). The absorption of some oral medications may be slowed down by food intake. But such a drug as "Cefuroxime asketil" undergoes hydrolysis during absorption. Food contributes to a faster release of the active ingredient.
4th generation cephalosporins are well distributed in many tissues and organs (except for the prostate), as well as secrets. IN high concentrations drugs are found in peritoneal and synovial, pericardial and pleural fluids, bones and skin, soft tissues, liver, muscles, kidneys and lungs. The ability to pass the BBB and form therapeutic concentrations in the cerebrospinal fluid is more pronounced in such third-generation drugs as Ceftazidime, Ceftriaxone, and Cefotaxime, and the representative of the fourth, Cefepime.
Most cephalosporins are not degraded. An exception is the drug "Cefotaxime". It biotransforms with the subsequent formation of an active product. The 4th generation cephalosporins, like the rest, are excreted mainly by the kidneys. When excreted in the urine, rather high concentrations are found.
Medicines "Cefoperazone" and "Ceftriaxone" are distinguished by a double route of excretion - the liver and kidneys. For most cephalosporins, the half-life is within one to two hours. A longer time is required for Ceftibuten, Cefixime (3-4 hours), and Ceftriaxone (up to 8.5 hours). This makes it possible to assign them once a day. Against the background of renal failure, the dosage of medications requires adjustment.

Antibiotics - 4th generation cephalosporins - cause a number of negative consequences, in particular:
- Allergy. Patients may present with erythema multiforme, rash, urticaria, serum sickness, and eosinophilia. Side effects in this category also include anaphylactic shock and fever, Quincke's edema, bronchospasm.
- hematological reactions. Among them, it is worth highlighting a positive Coombs test, leukopenia, eosinophilia (rarely), hemolytic anemia, neutropenia.
- Nervous disorders. When using high doses in patients with renal dysfunction, convulsions are noted.
- On the part of the liver: increased activity of transaminases.
- Digestive disorders. Among the negative consequences, diarrhea, pseudomembranous colitis, vomiting and nausea, and abdominal pain are quite common. In the event of a liquid stool with blood fragments, the drug is canceled.
- local reactions. These include infiltration and soreness at the site of intramuscular injection and phlebitis with intravenous injection.
- Other consequences are expressed in the form of candidiasis of the vagina and mouth.

4th generation cephalosporins are prescribed for severe, predominantly low-grade infections caused by multidrug-resistant microflora. These include pleural empyema, lung abscess, pneumonia, sepsis, joint and bone lesions. 4th generation cephalosporins are indicated for complicated infections in the urinary tract, against the background of neutropenia and other immunodeficiency conditions. Medications are not prescribed for individual intolerance.
When used, a cross-type allergy is noted. Patients with intolerance to penicillins have a similar reaction to first-generation cephalosporins. Cross-allergy with the use of the second or third category is less common (in 1-3% of cases). If there is a history of immediate-type reactions (for example, anaphylactic shock or urticaria), first-generation drugs are prescribed with caution. Drugs in the following categories (especially the fourth) are safer.

Cephalosporins are prescribed in the prenatal period without special restrictions. However, adequate controlled studies of the safety of drugs have not been conducted. In low concentrations, cephalosporins can pass into milk. Against the background of the use of the drug during lactation, changes in the intestinal microflora, candidiasis, skin rash, and sensitization of the child are likely.
When used in neonates, an increase in half-life is likely against the background of delayed renal excretion. In elderly patients, there is a change in renal function, and therefore a slowdown in the elimination of drugs is likely. This may require adjustment of the regimen of application and dosage.
Since the excretion of most cephalosporins occurs through the kidney system mainly in the active form, the dosage regimen should be adjusted to the characteristics of the body. When using high doses, especially in combination with loop diuretics or aminoglycosides, a nephrotoxic effect is likely to occur.
Some drugs are excreted in the bile, and therefore for patients with severe liver pathologies, the dosage should be reduced. In such patients, there is a high predisposition to bleeding and hypoprothrombinemia when using Cefoperazone. IN preventive purposes vitamin K recommended.
Cephalosporins in tablets belong to the group of antibiotic drugs. Presented drugs are mainly used to combat diseases of a bacterial nature. Let us consider in more detail the pharmacological effects, indications and features of the use of this type of medicine.
Cephalosporins are antibiotic drugs characterized by a high degree efficiency. These drugs were discovered in the middle of the 20th century. To date, there are 5 generations of cephalosporins. At the same time, antibiotics of the 3rd generation are especially popular.
 The pharmacological effect of these drugs lies in the ability of their main active ingredients to damage bacterial cell membranes, which leads to the death of pathogens.
The pharmacological effect of these drugs lies in the ability of their main active ingredients to damage bacterial cell membranes, which leads to the death of pathogens.
Cephalosporins (especially 4th generation) are extremely effective in combating infectious diseases, the emergence and development of which is associated with the pathological activity of the so-called gram-negative bacteria.
4th generation cephalosporins give positive results even in cases where antibiotic drugs belonging to the penicillin group turned out to be completely ineffective.
Cephalosporins in tablet form are prescribed to patients suffering from certain infectious diseases of a bacterial nature, as well as a means of preventing the development of infectious complications during surgical intervention. Experts distinguish the following indications for the use of the presented drugs:

- Cystitis.
- Furunculosis.
- Urethritis.
- Otitis media.
- Gonorrhea.
- Bronchitis in acute or chronic form.
- Pyelonephritis.
- Angina streptococcus.
- Sinusitis.
- Shigellosis.
- Infectious lesions of the upper respiratory tract.
It should be noted that the spectrum of action and scope of cephalosporins largely depend on the generation to which the antibiotic drug belongs. Let's consider this question in more detail:
- 1st generation cephalosporins are used to treat uncomplicated infections that affect the skin, bones, and joints.
- Indications for the use of 2nd generation cephalosporins are diseases such as tonsillitis, pneumonia, chronic bronchitis, pharyngitis, urinary tract lesions that are bacterial in nature.
- 3rd generation cephalosporins are prescribed for diseases such as bronchitis, infectious lesions of the urinary system, shigellosis, gonorrhea, impetigo, Lyme disease.
- 4th generation cephalosporins can be indicated for sepsis, joint damage, pulmonary abscesses, pneumonia, pleural empyema. It is worth emphasizing that the 4th generation cephalosporin group of drugs is not available in the form of tablets due to its specific molecular structure.
These antibiotic drugs are contraindicated only in case of individual sensitivity and allergic reactions to the main active ingredient - cephalosporin, as well as in patients under 3 years of age.
In some cases, the use of cephalosporins may develop side effects. The most common adverse reactions include the following:
- Nausea.
- Attacks of vomiting.
- Diarrhea.
- Stomach upset.
- Headaches similar in nature to migraine symptoms.
- Allergic reactions.
- Pain in the abdomen.
- Disturbances in the functioning of the kidneys.
- Liver disorders.
- Dysbacteriosis.
- Dizziness.
- Urticaria and the appearance of a rash on the skin.
- Violation of blood clotting.
- Eosinophilia.
- Leukopenia.
In most cases, the occurrence of the above side effects is associated with prolonged and uncontrolled use of cephalosporins.
The choice of the drug, the determination of the dosage and duration of the therapeutic course should be carried out exclusively by the attending physician, taking into account the diagnosis, severity of the disease, age and general condition patient's health. In addition, in order to avoid the occurrence of unwanted reactions, it is necessary to strictly follow the instructions for using the drug and take medicines that prevent the development of dysbacteriosis.
Cephalosporins in the form of tablets are in particular demand and popularity. The fact is that this form of antibiotic preparations has certain advantages. These include the following factors:
- Pronounced bacterial effect.
- Increased resistance to a specific enzyme called beta-lactamase.
- Simple and convenient application.
- The possibility of implementing the therapeutic process on an outpatient basis.
- Profitability associated with the absence of the need to purchase syringes and solutions necessary for injecting the drug.
- Absence of inflammatory reactions of local localization, characteristic of injections.
Cephalosporin preparations in tablets for adult patients are prescribed by a doctor in the appropriate dosage. The duration of the therapeutic course ranges from a week to 10 days, depending on the severity of the disease. Patients childhood the medicine is given 2-3 times a day, the dosage is calculated individually, taking into account the weight of the child.
Cephalosporins are recommended to be consumed after meals, which contributes to their better absorption by the body. In addition, according to the instructions for use, along with the drugs of the presented group, it is necessary to take antifungal medications and agents that prevent the development of dysbacteriosis.
An appropriate annotation is attached to each specific drug, which must be carefully studied before starting the course of treatment and then strictly follow the instructions provided in the instructions.
There are various tablet preparations of cephalosporins, each of which has certain characteristics and clinical properties. Let's consider them in more detail:
- Cephalexin belongs to the group of cephalosporins of the 1st generation. The presented drug is highly effective in the fight against streptococci and staphylococci. Cefalexin is prescribed for diseases of an infectious and inflammatory nature. Side effects include the possible development of allergic reactions in case of intolerance to penicillin.
- Cefixime is a 3rd generation cephalosporin. Given medicine has a pronounced antibacterial effect, inhibiting the activity of almost all known pathogens. Cefixime is characterized by the presence of pharmacokinetic properties, good penetration into tissues. The drug preparation is distinguished by an increased degree of effectiveness in the fight against Pseudomonas aeruginosa, enterobacteria.
- Ceftibuten. medicinal product belongs to the 3rd generation cephalosporins. The drug is available in the form of tablets and suspensions. Ceftibuten is characterized by a high degree of resistance to the effects of specific substances released for protective purposes by pathogens.
- Cefuroxime acetyl belongs to the group of 2nd generation cephalosporins. The presented drug is very effective in the fight against pathogens such as enterobacteria, moraxella and hemophilus. Cefuroxime acetyl is taken several times a day. The dosage is determined depending on the form and severity of the disease, the age category of the patient. With prolonged use, side effects such as diarrhea, nausea, vomiting, changes in clinical picture blood.
- Zinnat is one of the most common drugs belonging to the group of 2nd generation cephalosporins. This drug is used to treat furunculosis, pyelonephritis, pneumonia, infections of the upper and lower respiratory tract and other diseases caused by the pathological activity of pathogens that are sensitive to cefuroxime.
Cephalosporins are highly effective and effective antibiotic drugs used in the field of modern medicine to combat infectious diseases. The tablet form of drugs is especially widespread, characterized by a minimal range of contraindications and side effects.
Cephalosporins in tablets are one of the most extensive groups of antibacterial agents that are widely used for the treatment of adults and children. Medicines of this group are highly popular due to their effectiveness, low toxicity and convenient form of application.
 general characteristics Cephalosporins
general characteristics Cephalosporins
Cephalosporins have the following characteristics:
- contribute to the provision of bactericidal action;
- have a wide spectrum of therapeutic action;
- about 7-11% cause the development of cross-allergy. The risk group includes patients with intolerance to penicillin;
- drugs do not contribute to the impact against enterococci and listeria.
This group of drugs can only be taken as prescribed and under the supervision of a doctor. Antibiotics are not intended for self-medication.
The use of cephalosporin drugs may contribute to the following undesirable side reactions:
- allergic reactions;
- dyspeptic disorders;
- phlebitis;
- hematological reactions.
Classification of drugs
Antibiotics cephalosporins are usually classified by generation. List of drugs by generation and dosage forms:
The main differences between generations are the spectrum of antibacterial action and the degree of resistance to beta-lactamases (bacterial enzymes whose activity is directed against beta-lactam antibiotics).
1st generation drugs
The use of these drugs contributes to the provision of a narrow spectrum of antibacterial action.
Cefazolin is one of the most popular drugs that helps to exert an effect against streptococci, staphylococci, gonococci. After parenteral administration, it penetrates into the lesion site. A stable concentration of the active substance is achieved if the drug is administered three times within 24 hours.
Indications for the use of the drug are: the impact of streptococci, staphylococci on soft tissues, joints, bones, skin.
It should be taken into account: earlier Cefazolin was widely used for the treatment of a large number of infectious pathologies. However, after more modern medicines of the 3rd-4th generation appeared, Cefazolin is no longer used in the treatment of intra-abdominal infections.
2nd generation drugs
Second generation drugs are characterized by increased activity against gram-negative pathogens. Cephalosporins 2 generations for parenteral administration based on cefuroxime (Kymacef, Zinacef) are active against:
- Gram-negative pathogens, Proteus, Klebsiella;
- infections caused by streptococci and staphylococci.
Cefuroxime - a substance from the second group of cephalosporins is not active against Pseudomonas aeruginosa, morganella, providence and most anaerobic microorganisms.
After parenteral administration, it penetrates into most organs and tissues, including the blood-brain barrier. This makes it possible to use the drug in the treatment of inflammatory pathologies of the lining of the brain.
Indications for the use of this group of funds are:
- exacerbation of sinusitis and otitis media;
- chronic form of bronchitis in the acute phase, development community-acquired pneumonia;
- therapy of postoperative conditions;
- infection of the skin, joints, bones.

The dosage for children and adults is selected individually, depending on the indications for use.
Internal medicines include:
- tablets and granules for the preparation of Zinnat suspension;
- Ceclor suspension - a child can take such a drug, the suspension has pleasant taste characteristics. It is not recommended to use Ceclor during the treatment of exacerbation of otitis media. The drug is also presented in the form of tablets, capsules and dry syrup.
Oral cephalosporins can be used regardless of food intake, the excretion of the active ingredient is carried out by the kidneys.
3rd generation drugs
The third type of cephalosporins was initially involved in stationary conditions in the treatment of severe infectious pathologies. To date, such drugs can also be used in the outpatient clinic due to the increased resistance of pathogens to antibiotics. 3rd generation drugs have their own application features:
- parenteral forms are used for severe infectious lesions, as well as for the detection of mixed infections. For more successful therapy, cephalosporins are combined with antibiotics from the group of 2-3 generation aminoglycosides;
- drugs for internal use are used to eliminate moderate hospital-acquired infections.
3rd generation cephalosporins intended for oral administration have the following indications for use:
- complex therapy of exacerbations of chronic bronchitis;
- development of gonorrhea, shigillosis;
- stepwise treatment, if necessary, internal administration of tablets after parenteral treatment.
Compared with 2nd generation drugs, 3rd generation cephalosporins in tablets show greater efficacy against gram-negative pathogens and enterobacteria.
At the same time, the activity of Cefuroxime (2nd generation drug) in the treatment of pneumococcal and staphylococcal infections is higher than that of Cefixime.

Indications for the use of parenteral forms of cephalosporins (Cefatoxime) are:
- development of acute and chronic forms of sinusitis;
- development of intra-abdominal and pelvic infections;
- impact intestinal infection(shigella, salmonella);
- severe conditions in which the skin, soft tissues, joints, bones are affected;
- detection of bacterial meningitis;
- complex therapy of gonorrhea;
- development of sepsis.
The drugs are characterized by a high degree of penetration into tissues and organs, including the blood-brain barrier. Cefatoxime may be the drug of choice in the treatment of newborns. With the development of meningitis in a newborn child, Cefatoxime is combined with ampicillins.
Ceftriaxone is similar to Cefatoxime in its spectrum of action. The main differences are:
- the possibility of using Ceftriaxone once a day. In the treatment of meningitis - 1-2 times in 24 hours;
- double route of elimination, therefore, for patients with renal dysfunction, dose adjustment is not required;
- additional indications for use are: complex treatment of bacterial endocarditis, Lyme disease.
Ceftriaxone should not be used during neonatal therapy.
Medicines 4 generations
4th generation cephalosporins are distinguished by an increased degree of resistance and demonstrate greater effectiveness against the following pathogens: gram-positive cocci, enterococci, enterobacteria, Pseudomonas aeruginosa (including strains that are resistant to ceftazidime). Indications for the use of parenteral forms is the treatment of:
- nosocomial pneumonia;
- intra-abdominal and pelvic infections - a combination with drugs based on metronidazole is possible;
- infections of the skin, soft tissues, joints, bones;
- sepsis;
- neutropenic fever.
When using Imipenem, which belongs to generation four, it is important to take into account that Pseudomonas aeruginosa quickly develops resistance to this substance. Before using medicines with such active substance, it is necessary to conduct a study on the sensitivity of the causative agent of the disease to imipenem. The drug is used for intravenous and intramuscular administration.
Meronem is similar in characteristics to imipenem. Instructions for use states that among the distinguishing characteristics are:
- greater activity against gram-negative pathogens;
- less activity against staphylococci and streptococcal infections;
- the drug does not contribute to the provision of anticonvulsant action, therefore, it can be used during complex treatment meningitis;
- suitable for intravenous drip and jet infusion, should refrain from intramuscular injection.
The use of an antibacterial agent of the 4th generation cephalosporin group Azactam contributes to the provision of a smaller spectrum of action. The drug has a bactericidal effect, including against Pseudomonas aeruginosa. The use of Azactam may contribute to the development of such undesirable side reactions:
- local manifestations in the form of phlebitis and thrombophlebitis;
- dyspeptic disorders;
- hepatitis, jaundice;
- neurotoxicity reactions.
The main clinically significant task of this tool is to influence the life process of aerobic gram-negative pathogens. In this case, Azaktam is an alternative to drugs from the aminoglycoside group.
Medicines of the 5th generation
Means that belong to the 5th generation contribute to the provision of a bactericidal effect, destroying the walls of pathogens. Active against microorganisms demonstrating resistance to 3rd generation cephalosporins and drugs from the aminoglycoside group.
5th generation cephalosporins are presented on the pharmaceutical market in the form of preparations based on the following substances:
- Ceftobiprol medocaril is a medicine under the trade name Zinforo. It is used in the treatment of community-acquired pneumonia, as well as complicated infections of the skin and soft tissues. Most often, the patient complained about the occurrence of adverse reactions in the form of diarrhea, headache, nausea, and itching. Adverse reactions are mild in nature, their development should be reported to the attending physician. Special care is required in the treatment of patients with a history of convulsive syndrome;
- Ceftobiprol - tradename Zefter. Available in the form of a powder for solution for infusion. Indications for use are complicated infections of the skin and appendages, as well as infection diabetic foot without associated osteomyelitis. Before use, the powder is dissolved in glucose solution, water for injection or saline. The tool should not be used in the treatment of patients under 18 years of age.
5th generation agents are active against Staphylococcus aureus, demonstrating a broader spectrum of pharmacological activity than previous generations of cephalosporins.
One of the most common classes antibacterial drugs are cephalosporins. According to their mechanism of action, they are inhibitors of cell wall synthesis and have a powerful bactericidal effect. Together with penicillins, carbapenems and monobactams form a group of beta-lactam antibiotics.
Due to a wide spectrum of action, high activity, low toxicity and good tolerance by patients, these drugs are the leaders in the frequency of prescriptions for the treatment of inpatients and account for about 85% of the total volume of antibacterial agents.
The list of drugs for convenience is presented by five groups of generations.
- Cefazolin (Kefzol, Cefazolin sodium salt, Cefamezin, Lysolin, Orizolin, Nacef, Totacef).
Oral, i.e. forms for oral use, tablets or in the form of suspensions (hereinafter trans.):
- Cefalexin (Cephalexin, Cefalexin-AKOS)
- Cefadroxil (Biodroxil, Durocef)
- Cefaclor (Ceclor, Vercef, Cefaclor Stada).
- Cefuroxime-axetil (Zinnat).
- Cefotaxime.
- Ceftriaxone (Rofecin, Ceftriaxone-AKOS, Lendacin).
- Cefoperazone (Medocef, Cefobit).
- Ceftazidime (Fortum, Vicef, Kefadim, Ceftazidime).
- Cefoperazone / sulbactam (Sulperazone, Sulperacef, Sulzoncef, Bacperazone, Sulcef).
- Cefditoren (Spectracef).
- Cefixime (Supraks, Sorcef).
- Ceftibuten (Cedex).
- Cefpodoxime (Cefpodoxime Proxetil).
- Cefepim (Maxipim, Maxicef).
- Cefpir (Cefvnorm, Isodepoi, Keiten).
- Ceftobiprol (Zefthera).
- Ceftaroline (Zinforo).
The table below shows the effectiveness of cephalosp. in relation to known bacteria from - (microbial resistance to drug action) to ++++ (maximum eff.).
| bacteria | Generations | ||||
| Gr+ | ++++ | +++ | + | ++ | ++ |
| Gr- | + | ++ | +++ | ++++ | ++++ |
| MRSA | - | - | - | - | ++++ |
| Anaerobes | - | +/- Only Cefoxitin and Cefotetan are effective* |
+ | + | + |
| Notes | Not assigned to MRSA, entero-, meningo- and gonococci, listeria, beta-lactamazo-producing strains and Pseudomonas aeruginosa. | Not effective against Pseudomonas aeruginosa, serations, most anaerobes, morganella. | Does not affect B.fragilis (anaerobes). | Effective even against penicillin-resistant strains. | |
* Antibiotics of the cephalosporin group, names (with anaerobic activity): Mefoxin, Anaerocef, Cefotetan + all representatives of the third, fourth and fifth generations.
In 1945, Italian professor Giuseppe Brotzu, while studying the ability of wastewater to self-purify, isolated a fungus strain capable of producing substances that inhibit the growth and reproduction of gram-positive and gram-negative flora. During further studies, the drug from the culture of Cephalosporium acremonium was tested on patients with severe forms of typhoid fever, which led to a rapid positive dynamics of the disease and a speedy recovery of patients.
The first cephalosporin antibiotic, cephalothin, was created in 1964 by the American pharmaceutical company Eli Lilly.
The source for the preparation was cephalosporin C, a natural producer of mold fungi and a source of 7-aminocephalosporanic acid. In medical practice, semi-synthetic antibiotics are used, obtained by acylation at the amino group of 7-ACC.
In 1971, cefazolin was synthesized, which became the main antibacterial drug for a whole decade.
The first drug and the ancestor of the second generation was cefuroxime obtained in 1977. The most commonly used antibiotic in medical practice, ceftriaxone, was created in 1982, is actively used and “does not lose ground” to this day.
A breakthrough in the treatment of Pseudomonas aeruginosa can be called the receipt in 1983 of Ceftazidime.
Despite the similarity in structure with penicillins, which determines a similar mechanism of antibacterial action and the presence of cross-allergies, cephalosporins have an extended spectrum of influence on pathogenic flora, high resistance to the action of beta-lactamases (enzymes of bacterial origin that destroy the structure of an antimicrobial agent with a beta-lactam cycle) .
The synthesis of these enzymes causes the natural resistance of microorganisms to penicillins and cephalosporins.
All medicines in this class are different:
- bactericidal effect on pathogens;
- easy tolerability and relatively low number of adverse reactions in comparison with other antimicrobial agents;
- the presence of cross-allergic reactions with other beta-lactams;
- high synergy with aminoglycosides;
- minimal disruption of the intestinal microflora.
The advantage of cephalosporins can also be attributed to good bioavailability. Antibiotics of the cephalosporin series in tablets have a high degree of digestibility in the digestive tract. The absorption of funds increases when used during or immediately after a meal (the exception is Cefaclor). Parenteral cephalosporins are effective for both IV and IM routes of administration. Possess high index distribution in tissues and internal organs. The maximum concentrations of drugs are created in the structures of the lungs, kidneys and liver.
Ceftriaxone and cefoperazone provide high levels of the drug in bile. The presence of a dual route of elimination (liver and kidneys) allows them to be effectively used in patients with acute or chronic renal failure.
Cefotaxime, cefepime, ceftazidime and ceftriaxone are able to cross the blood-brain barrier, creating a clinically significant levels in cerebrospinal fluid and are prescribed for inflammation of the meninges of the brain.
Drugs with a bactericidal mechanism of action are most active against organisms in the growth and reproduction phases. Since the wall of the microbial organism is formed by high-polymer peptidoglycan, they act at the level of synthesis of its monomers and disrupt the synthesis of transverse polypeptide bridges. However, due to the biological specificity of the pathogen, between different types and classes, the appearance of various, new structures and ways of functioning is possible.
Mycoplasma and protozoa do not contain a membrane, and some types of fungi contain a chitinous wall. Due to this specific structure, the listed groups of pathogens are not sensitive to the action of beta-lactams.
The natural resistance of true viruses to antimicrobial agents is due to the absence of a molecular target (wall, membrane) for their action.
In addition to the natural, due to the specific morphophysiological characteristics of the species, resistance can be acquired.
The most significant reason for the formation of tolerance is irrational antibiotic therapy.
Chaotic, unreasonable self-prescribing of medications, frequent cancellation with a switch to another drug, the use of one drug for short periods of time, violation and underestimation of dosages prescribed in the instructions, as well as premature cancellation of the antibiotic - lead to the appearance of mutations and the emergence of resistant strains that do not respond to classical schemes treatment.
Clinical studies have shown that long time intervals between the appointment of an antibiotic completely restore the sensitivity of bacteria to its effects.
Mutation-selection
- Rapid resistance, streptomycin type. It develops into macrolides, rifampicin, nalidixic acid.
- Slow, penicillin type. Specific for cephalosporins, penicillins, tetracyclines, sulfonamides, aminoglycosides.
transmission mechanism
Bacteria produce enzymes that inactivate chemotherapy drugs. The synthesis of beta-lactamase by microorganisms destroys the structure of the drug, causing resistance to penicillins (more often) and cephalosporins (less often).
Most often, resistance is characteristic of:
- staphylo- and enterococci;
- coli;
- klebsiella;
- mycobacterium tuberculosis;
- shigella;
- pseudomonads.
- strepto- and pneumococci;
- meningococcal infection;
- salmonella.
First generation
Currently used in surgical practice for the prevention of surgical and postoperative complications. Applicable for inflammatory processes skin and soft tissues.
Not effective for urinary and upper respiratory tract infections. Used in the treatment of streptococcal tonsillopharyngitis. They have good bioavailability, but do not create high, clinically significant concentrations in the blood and internal organs.
Effective in patients with community-acquired penneumonia, well combined with macrolides. They are a good alternative to inhibitor-protected penicillins.
- Recommended for the treatment of otitis media and acute sinusitis.
- Not used for damage to the nervous system and meninges.
- It is used for preoperative antibiotic prophylaxis and drug cover for surgical intervention.
- It is prescribed for non-severe inflammatory diseases of the skin and soft tissues.
- Included in the complex treatment of urinary tract infections.
Stepwise therapy is often used, with the appointment of parenteral cefuroxime sodium, followed by the transition to oral administration of cefuroxime axetil.
It is not prescribed for acute otitis media, due to low concentrations in fluid media. ear. Effective for the treatment of infectious and inflammatory processes of bones and joints.
They are used for meningitis of a bacterial nature, gonorrhea, infectious diseases of the lower respiratory tract, intestinal infections and inflammation of the biliary tract.
Well overcome the blood-brain barrier, can be used for inflammatory, bacterial lesions of the nervous system.
They are the drugs of choice for the treatment of patients with renal insufficiency. Excreted through the kidneys and liver. Changing and adjusting the dose is necessary only for combined renal and hepatic insufficiency.
Cefoperazone practically does not overcome the blood-brain barrier, therefore it is not used for meningitis.
It is the only inhibitor-protected cephalosporin.
It consists of a combination of cefoperazone with the beta-lactamase inhibitor sulbactam.
Effective in anaerobic processes, can be prescribed as a one-component therapy for inflammatory diseases of the small pelvis and abdominal cavity. Also, it is actively used for severe hospital infections, regardless of localization.
Cephalosporin antibiotics combine well with metronidazole for the treatment of intra-abdominal and pelvic infections. They are the drugs of choice for severe, complicated inf. urinary tract. They are used for sepsis, infectious lesions of bone tissue, skin and subcutaneous fat.
They are prescribed for neutropenic fever.
They cover the entire spectrum of activity of the 4th and act on penicillin-resistant flora and MRSA.
Not appointed:
- up to 18 years;
- patients with a history of seizures, epilepsy and renal failure.
Ceftobiprol (Zefthera) is the most effective tool for the treatment of diabetic foot infections.
Parenteral application
Used in / in and / m introduction.
| Name | Calculation for adults | Dosages of cephalosporin antibiotics for children (in the column are indicated from the calculation mg/kg per day ) |
| Cefazolin | It is prescribed at the rate of 2.0-6.0 g / day for three injections. For prophylactic purposes, appoint 1-2 g an hour before the start of surgery. |
50-100, dividing by 2-3 times. |
| Cefuroxime | 2.25-4.5 g per day, in 3 applications. | 50-100 for 2 rubles. |
| Cefotaxime | 3.0-8.0 g for 3 times. With meningitis, up to 16 g in six injections. For gonorrhea, 0.5 g is prescribed intramuscularly, once. |
From 40 to 100 in two injections. Meningitis - 100 for 2 rubles. No more than 4.0 g per day. |
| Ceftriaxone | 1 g every 12 hours. Meningitis - 2 g every twelve hours. Gonorrhea - 0.25 g once. |
For the treatment of acute otitis media, a dose of 50 is used, in three injections. not exceeding 1 g at a time. |
| Ceftazidime | 3.0-6.0 g in 2 injections | 30-100 for two times. With meningitis 0.2 g for two injections. |
| Cefoperazone | From 4 to 12 g for 2-4 injections. | 50-100 for three times. |
| cefepime | 2.0-4.0 g for 2 times. | At the age of over two months, 50 are used, divided into three injections. |
| Cefoperazone/sulbactam | 4.0-8.0 g for 2 injections. | 40-80 for three applications. |
| Ceftobiprol | 500 mg every eight hours as a 120-minute IV infusion. | - |
Undesirable effects and drug combinations
- The appointment of antacids significantly reduces the effectiveness of antibiotic therapy.
- Cephalosporins are not recommended to be combined with anticoagulants and antiplatelet agents, thrombolytics - this increases the risk of intestinal bleeding.
- Do not combine with loop diuretics due to the risk of nephrotoxicity.
- Cefoperazone has a high risk of a disulfiram-like effect with alcohol. Remains up to several days after the complete discontinuation of the drug. May cause hypoprothrombinemia.
As a rule, they are well tolerated by patients, however, the high frequency of cross-allergic reactions with penicillins should be taken into account.
The most common dyspeptic disorders, rarely - pseudomembranous colitis.
Possible: intestinal dysbacteriosis, oral and vaginal candidiasis, transient increase in liver transaminases, hematological reactions (hypoprothrombinemia, eosinophilia, leukemia and neutropenia).
With the introduction of Zeftera, the development of phlebitis, taste perversion, the occurrence of allergic reactions are possible: Quincke's edema, anaphylactic shock, bronchospastic reactions, the development of serum sickness, the appearance of erythema multiforme.
Rarely, hemolytic anemia may occur.
Ceftriaxone is not prescribed to newborns, due to the high risk of developing kernicterus (due to the displacement of bilirubin from its association with blood plasma albumins), it is not prescribed to patients with biliary tract infections.
N.V. Beloborodova
Office of Rational Antibiotic Therapy of the Moscow Health Committee, Department of Pediatric Surgery, Russian State Medical University
URL
IN last years cephalosporin antibiotics occupy a leading position in clinical practice, especially in the treatment of severe infections of various localization (pneumonia, meningitis, peritonitis, sepsis), including pediatrics and neonatology.
Why are IV generation cephalosporins needed?
The unjustifiably widespread and uncontrolled use of III generation cephalosporins eventually led to the emergence of resistant hospital strains, which became the only, but very serious, limitation in the use of this group of antibiotics. The development of resilience is associated with plasmid production by bacteria b extended spectrum lactamase, as well as overproduction of chromosomal b -lactamase capable of inactivating third-generation cephalosporins. The emergence and accumulation of such strains is most likely in departments where, according to the severity of the condition, more than 70-80% of patients receive antibiotics, for example, intensive care and resuscitation departments, children's onco-hematological departments and departments of purulent surgery. In addition to "ordinary" enterobacteria and Pseudomonas aeruginosa, microbiological monitoring in such departments reveals strainsEnterobacter cloacae, Enterobacter aerogenes, Serratia marcescens, Klebsiella pneumoniaeand others with multiple antibacterial resistance, hyperproducers b -lactamase. Against the background of treatment with III generation cephalosporins, with the elimination of sensitive microorganisms, not only the selection of these strains on the mucous membranes occurs, but also their involvement in the infectious process (local or generalized). In case of development of bacteremia, pneumonia or meningitis caused by these enterobacteria, traditional treatment regimens based on third-generation cephalosporins (cefotaxime, ceftriaxone, ceftazidime), even in combination with aminoglycosides (gentamicin, amikacin) or fluoroquinolones (ciprofloxacin), will be ineffective. In such situations, the timely use of fourth-generation cephalosporins is not only indicated, but may be life-saving.
Table 1. Comparative in vitro activity of some antibiotics against three types of gram-negative bacteria in children's intensive care units in Moscow
| K.pneumoniae (n=28) | Enterobacter spp. (n=20) | P.aeruginosa (n=16) | |||||||
|
H, % |
P, % |
R,% |
H, % |
P, % |
R,% |
H, % |
P, % |
R,% |
|
| Cefotaxime |
64,3 |
10,7 |
43,8 |
50,2 |
|||||
| Ceftazidime |
78,6 |
17,8 |
81,3 |
12,5 |
|||||
| Cefpir |
89,3 |
31,3 |
18,7 |
||||||
| cefepime |
92,8 |
3,6 |
3,6 |
95 |
5 |
0 |
87,5 |
12,5 |
0 |
| Imipenem |
62,5 |
31,3 |
|||||||
| Meropenem |
62,5 |
31,3 |
|||||||
| Ciprofloxacin |
96,4 |
43,8 |
|||||||
| Note. H - sensitive, P - intermediate, R - resistant | |||||||||
Features of the antibacterial spectrum of cefepime
Two IV generation cephalosporins, cefepime and cefpirome, are known in clinical practice. A detailed description of these antibiotics is presented in the reviews by S.V. Yakovlev. In 1999, cefepime was approved in Russia for use in pediatric practice, therefore, the focus of this article will be on this drug. Features of the structure of the cephem nucleus of cefepime cause a more pronounced effect on gram-negative bacteria and give resistance to action. b- lactamase of any type.
Table 2. Main publications on the efficacy of cefepime in pediatrics
|
Indications |
Number of children |
Age |
Year |
|
| Meningitis |
2 months - 15 years (average 1 year) |
1995 |
X. Saez-Llorens et al. |
|
| Bacterial infections in the hospital |
2 months - 16 years (up to 2 years - 57%) |
1997 |
M.D. Reed et al. |
|
| Febrile neutropenia |
under 19 |
1997 |
M.M. Mustafa |
|
| Pyelonephritis |
1 month - 12 years (up to 2 years - 53%) |
1998 |
U.B. Shaad et al. |
The spectrum of activity of cefepime is a combination of spectra of cephalosporins of I and II generations in relation to gram-positive bacteria and cephalosporins of the third generation in relation to gram-negative bacteria. It covers familiesEnterobacteriaceae, Neisseriaceae, Haemophilus influenzae, Moraxella catarrhalis, Pseudomonas spp, Acinetobacter spp.,methicillin-sensitive staphylococci, streptococci, pneumococci and some anaerobes.
After the widespread introduction of antipseudomonal drugs into the clinic b- lactams, modern aminoglycosides, fluoroquinolones and carbapenems the problem of hospital infections caused byPseudomonas aeruginosaseemed to recede somewhat. But in hospitals, new difficulties have arisen that need to be overcome: this is the resistance of other gram-negative bacteria, as well as superinfections caused by multi-resistant staphylococci and enterococci.
Table 3. Recommended combinations of cefepime with other antimicrobials for empiric treatment of sepsis, septic shock and multiple organ failure in children
| Leading microflora | Combinations of antibiotics | |
| Sepsis (after previous therapy, for example: cephalosporin + gentamicin) |
|
|
| Sepsis, shock, multiple organ failure |
|
cefepime+ ciprofloxacin ± metronidazole |
Today, among the problematic microorganisms, some enterobacteria with "harmless" names are increasingly indicated (Enterobacter spp., Serratia spp.etc.) or non-fermenting bacteria (Acinetobacter spp.), characterized by multiple resistance to antibiotics due to the presence of plasmid b extended spectrum lactamase and chromosomal hyperproduction b -lactamase. Such microorganisms-hyperproducers easily destroy almost all b- lactam antibiotics. Only IV generation cephalosporins and carbapenems can resist them. A microbiological study conducted by us in 1998 included 100 successively isolated strains of Gram-negative bacteria in children's intensive care units in Moscow. At comparative study antibiotic sensitivity in vitro IV generation cephalosporins, especially cefepime, showed undoubted advantages over third generation cephalosporins - cefotaxime and ceftazidime. Moreover, it turned out that in relation to P.aeruginosa, cefepime is more active in vitro than many reserve drugs, such as carbapenems and fluoroquinolones (Table 1). times more active than ceftazidime.
Cefepime showed high activity against all enterobacteria. With regard to non-fermenting gram-negative bacteria - in relation to acinetobacter cefepime was second only to imipenem, and for Pseudomonas aeruginosa showed comparable activity with aztreonam, ciprofloxacin and aminoglycosides. Thus, theoretically, the replacement of traditional b- lactams (semi-synthetic penicillins, ureidopenicillins and cephalosporins of I, II, III generations) to IV generation cephalosporins would help to cope with the problem of selection and accumulation of dangerous enterobacteria.
This thesis was confirmed in practice in a detailed study conducted by colleagues from Belgium in the Hematology Center for 4 years. In the empirical treatment of fever in patients with neutronia on the background of the routine use of ceftazidime in combination with vancomycin in this Center, the level of resistance of enterobacteria to ceftazidime reached 75%, which entailed the need to use various reserve drugs in increasing quantities. In order to break the vicious circle of selection of inducible strains-hyperproducers b- lactamase in this Center, it was decided to rotate in antibacterial policy: abandon third-generation cephalosporins, replacing them with cefepime, which, if indicated, should be used in combination with amikacin. Based on the results of 3-4-year monitoring, a significant improvement in the epidemiological situation in the Center was shown: the level of resistance significantly decreased, not only to ceftazidime, but also to other antibiotics (amikacin, co-trimoxazole, ciprfloxacin, etc.), and the consumption of expensive glycopeptides decreased. The authors made an important conclusion about the possibility of managing bacterial resistance by reasonably modifying antibiotic therapy regimens in high-risk units.
The in vitro activity of cefepime against common staphylococci is quite high (more than 98% of sensitive strains), and against methicillin-resistant (MP) staphylococci, it varies significantly depending on the bacterial species. So, MP sensitivity coagulase-negative staphylococci (eg.S.epidermidis) to cefepime can reach 75%, while MP strains of S. aureus are more than 90% resistant to IV generation cephalosporins. In view of the above, the risk of developing staphylococcal superinfections in the treatment with cefepime is significantly lower than in the treatment with third-generation cephalosporins, which is a definite advantage of the drug. However, it is generally accepted that in infections caused by methicillin-resistant staphylococcus aureus, cefepime is not sufficiently effective, therefore, in departments with high level staphylococcal superinfections, cefepime should be combined with anti-staphylococcal reserve drugs (parenteral glycopeptides: vancomycin or teicoplanin, as well as oral preparations fusidin, rifampicin, co-trimoxazole).
The activity of cefepime against Enterococcus faecalis is insufficient to consider it as a therapeutic drug, however, it is higher than that of III generation cephalosporins, which reduces the risk of enterococcal superinfection, which is characteristic of all other cephalosporins, and this is very important, especially if long-term course of antibiotic therapy. For example, in patients with febrile neutropenia, when comparing several antibacterial regimens, it was shown that the need for the addition of glycopeptides occurred less often in patients receiving cefepime monotherapy compared with combined regimens (ceftazidime + amikacin or piperacillin + gentamicin).
Summarizing what has been said about the spectrum of antibacterial activity of cefepime, it is necessary to emphasize the most important points:
* Thanks to resistance to b- lactamase, including extended spectrum, it retains activity against strains resistant to III generation cephalosporins, which has been repeatedly confirmed by the results of clinical studies.
* With regard to gram-negative bacteria, the activity of cefepime is comparable to that of fluoroquinolones and carbapenems, which makes it effective in gram-negative infections, especially in intensive care units.
* In the treatment of anaerobic infections of the abdominal cavity and non-clostridial anaerobic infections of wounds, in which Bacteroides fragilis is the leader among anaerobes, cefepime should be combined with metronidazole.
* When using cefepime, a reduced risk of enterococcal and staphylococcal superinfections can be expected.
Features of pharmacokinetics and dosing in children
Since the beginning of the 90s, many works have been published on the study of the effectiveness of cefepime in children of all ages. The indications for use were severe bacterial infections different localization. The most serious studies are devoted to a detailed analysis of the pharmacokinetics of cefepime in children with infections of the central nervous system (CNS), urinary tract, sepsis, as a rule, after previous antibiotic therapy. More than half of the patients described in these studies belong to the younger age group - these are children under the age of 2 years (Table 2).
Pediatric experience allows us to comment on the general pharmacokinetic characteristics of cefepime: in children, the half-life of the drug is slightly shorter than in adults (1.7 versus 2.2 hours); the volume of distribution is greater (0.35 l/kg versus 0.21 l/kg in adults) and the clearance is accelerated (3.1 ml/min/kg versus 1.5 ml/min/kg in adults). However, it has been shown that in children, regardless of age, maintaining doses of cefepime at concentrations above the MIC for the most important pathogens requires the same frequency of administration of the drug as in adults, i.e. twice a day. Data on the stability of the concentration of cefepime for more than 12 hours after administration in children aged 2 years and older justify the sufficiency of a dose of 50 mg / kg twice a day with an interval of 12 hours (daily dose of 100 mg / kg) for microorganisms with an MIC not exceeding 8 mg/l. which applies to most clinically relevant pathogens.
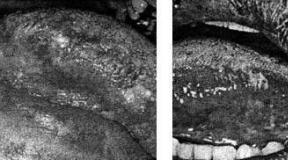
When comparing intravenous and intramuscular administration of cefepime, it was shown that in children the pharmacokinetic parameters leveled off already after the first 30 minutes from the moment of injection. Studies provide a solid foundation for optimal dosing of cefepime 50 mg/kg at 12 hour intervals (100 mg/kg per day) in the treatment of all pediatric infectious diseases except CNS disease. For meningitis in children aged 2 months to 15 years, after detailed pharmacokinetic studies, the optimal dose of cefepime is 50 mg/kg three times a day, with an interval of 8 hours, i.e. daily dose of 150 mg/kg divided into 3 injections. Cefepime well penetrates the blood-brain barrier and, with this dosing regimen, provides concentrations in the cerebrospinal fluid sufficient to suppress the growth of gram-positive(S.pneumonia, S.agalactia, S.aureus)and gram negative(H.influenzae, E.coli, K.pneumoniae, P.aeruginosa)bacteria - potential causative agents of meningitis. It is important to recall that, as with other antibacterial regimens for the treatment of meningitis, the administration of an antibiotic should be preceded by an injection of dexamethasone at a dose of 0.15 mg per 1 kg of the child's body weight.
Safety of cefepime in pediatrics
The high safety of cefepime, which is characteristic of all cephalosporins, is evidenced by the results of targeted studies conducted by foreign colleagues, including studies of the drug in children of different ages.
Comparative studies of the safety of cefepime and ceftazidime conducted in high-risk patients with an unfavorable background, comorbidities and other aggravating factors showed that side effects were recorded in 13.8% of patients in the cefepime group and 15.6% in the ceftazidime group. The most common side effect of cefepime was headache (2.4%), followed by nausea (1.8%), rash (1.8%) and diarrhea (1.7%). At high doses of cefepime clinical signs hemolysis was not observed even in patients with a positive Coombs test. The simultaneous use of analgesics, diuretics and anticoagulants did not increase the incidence of side effects. Organotoxic and other dangerous side effects (anaphylaxis) were neither in children nor in adults, nor in persons over 65 years of age. Thus, the safety profile of cefepime has been found to be virtually flawless.
In our country, cefepime is officially approved for use in children from the age of 2 months. The decision was made quite recently, in the summer of 1999, so there are no domestic publications on the experience of using cefepime in pediatrics. The lack of recommendations for the use of cefepime in neonates and premature infants is not associated with toxicity or side effects of the drug, but is due only to insufficient experience with the use of cefepime in neonatology. Usually, as clinical data are accumulated confirming the safety of the drug, the decision is reviewed and recommendations for use also apply to newborns and premature babies.
Cefepime - rational use in children's hospitals
1. When children are hospitalized for infections that have developed outside the hospital
Cefepime is certainly highly effective in children as a starting empirical therapy for infections of almost any localization - from pyelonephritis to meningitis and sepsis. However, a doctor with a sufficient outlook, who is well acquainted with the literature on antibiotic therapy and has his own clinical experience, perfectly understands how important it is to observe the principle of minimum sufficiency, i.e. do not prescribe new and reserve antibiotics where traditional drugs work well. This is important both in the treatment of a particular patient and in planning an antibiotic therapy policy in the scope of the entire department or hospital. It should be considered short-sighted to prescribe a IV generation cephalosporin in cases where, for example, penicillins or cephalosporins of the I, II and III generations are effective: this situation is identical in meaning to the proverb: "Shoot sparrows from a cannon." The principle of minimum sufficiency makes it possible to extend the terms of effective use of a new antibiotic in the clinic.
Respecting the principle minimal sufficiency, it should be considered inappropriate to use IV generation cephalosporins for the treatment of infections of moderate severity and for infections that have developed outside the hospital, since in these cases ordinary "home" microorganisms are involved in the infectious process.
As an example, we present data obtained in pediatric urological practice. A European randomized controlled trial in 13 countries across 39 clinical centers compared cefepime with ceftazidime in the treatment of pyelonephritis in 299 children (300 cases) under 12 years of age. The average age of patients was 1.7-1.8 years, the main pathogens were Escherichia coli (88% of cases), Proteus (5%), Pseudomonas aeruginosa (2%), Klebsiella (2%). Bacteriological sanitation achieved in 96% of cases in the cefepime group and 94% of cases in the ceftazidime group. At the end of the study, urine sterility was maintained in 86% of patients in the cefipime group and in 83% of patients in the ceftazidime group for 4-6 weeks. Satisfactory clinical the effect was achieved in 98 and 96%, respectively. Side effects were registered in 14 (9%) patients from the cefepime group and 10 (7%) from the ceftazidime group. The investigators concluded that cefipime and ceftazidime are equally effective and safe for the treatment of pediatric pyelonephritis.
Another comparative study of the efficacy of cefepime in the treatment of bacterial meningitis in pediatric practice was conducted in 1991-1993. joint efforts of the pediatric clinics of the University of Texas (Dallas, USA) and Panama. The reference drug was the third generation cephalosporin cefotaxime. The study included 90 children with meningitis, 43 were treated with cefepime, 47 with cefotaxime. Of the 90 patients, 43 were randomized to the cefepime group and 47 to the cefotaxime group. Both groups of children were comparable in age, etiology, duration of the disease, history, and severity of the course. Clinical response, terms of CSF sterilization, complications, severity of toxic reactions and duration of inpatient treatment were identical. The concentration of cefepime in the cerebrospinal fluid exceeded the MIC for most isolated pathogens of meningitis by 55-95 times. Pathogens isolated from the cerebrospinal fluid in 84% of patients: 61% -H. influenzae, 18% - N. meningitidis, 13% - S. pneumoniae, 8% - other bacteria. In the cefepime group, neurological and audiological complications were observed in 16% of patients, in the cefotaxime group - in 15% (patients were examined 2 and 6 months after the end of the therapeutic course). side effects - diarrhea, rash - observed in 18% of patients in the cefepime group and 23% in the cefotaxime group. Superinfection (candidiasis) developed in 1 (3%) patient from the cefepime group and in 3 (7%) patients from the cefotaxime group; eosinophilia - in 8 and 2% of patients, respectively. The overall mortality in this study was 6.7%. According to the results of the study, the safety and efficacy of cefepime are comparable to those of cefotaxime. A study involving 16,000 patients is needed to elucidate the fact of a decrease in mortality in meningitis during treatment with cefepime.
Thus, both studies conducted in children with infections that developed outside the hospital (uroinfections, bacterial meningitis) did not reveal significant advantages of cefepime compared to third-generation cephalosporins, but allowed us to demonstrate good tolerability and safety of the new antibiotic cefepime, comparable to traditional ceftazidime and cefotaxime.
The appointment of IV generation cephalosporins, in particular, cefepime, for infections that developed outside the hospital is most justified in cases where the patient, due to the severity of the condition, immediately enters the intensive care unit. With the use of IV generation cephalosporins in the intensive care unit, it can be expected to reduce the risk of selection of multidrug-resistant gram-negative bacteria with overproduction b- lactamase and reducing the risk of enterococcal superinfections in patients. These two factors that contribute to improving the epidemiological situation are extremely important for any pediatric intensive care unit where the highest-risk patients are treated.
2. With nosocomial infections
In the treatment of children with infectious diseases and complications that developed in a hospital against the background of the underlying disease, cefepime certainly has advantages over II and III generation cephalosporins. These advantages are greater, the more "rich" antibacterial history the patient has, since against the background of previous antibacterial therapy, the probability of infection of the patient with multidrug-resistant hospital gram-negative bacteria increases. In nosocomial infections, cefepime, even in monotherapy, may be more effective than standard combinations of other drugs. b- lactam antibiotics with aminoglycosides.
3. In severe sepsis, including multiple organ failure
In a generalized septic process, we often deal with an association of microorganisms: in conditions of gross violations of the protective systems, a variety of opportunistic bacteria in the child's body get the opportunity to multiply excessively not only on the mucous membranes, but also in the blood and tissues, which manifests itself (or not manifested) by the formation of various purulent-inflammatory foci. Often in the blood and organs it is possible to fix associations of gram-positive cocci with gram-negative bacteria, aerobes with anaerobes. Against the background of antibiotic therapy, the elimination of some bacteria leads to the rapid selection of others - the clinician is forced to document the change of the pathogen. As a rule, sepsis therapy is successful if, for a certain period, rational selection of antibiotics allows not only to eliminate a certain type of microorganisms, but to minimize the number of all potential pathogens, "unloading" the immune system, which creates conditions for restoring an adequate response. That's why in sepsis, combined regimens of antibiotic therapy are not just popular, but vital.
In the vast majority of cases, sepsis does not occur on its own and at lightning speed, but develops against the background of some other disease as a result of inadequate therapy. In recent years, more and more often we have to deal with cases when sepsis develops after previous therapy with penicillins or cephalosporins of I, II, III generations in combination with aminoglycosides. What role can IV generation cephalosporins play in such cases? Extremely important - both in the case of the dominance of multiresistant gram-negative flora, and in the case of sepsis with a leading gram-positive microflora.
In the first situation - with the so-called gram-negative sepsis - cefepime is most rationally used in combination with aminoglycosides - netilmicin or amikacin. In children with staphylococcal or enterococcal sepsis, the main drug, a glycopeptide (vancomycin or teicoplanin), should be combined with cefepime to protect against concomitant multidrug-resistant gram-negative flora.
In multiple organ failure, when the risk of nephrotoxic side effects of aminoglycosides may exceed their expected efficacy, a combination of cefepime with fluoroquinolones is recommended, which may be life-saving, including in children. In children with surgical pathology, it is important to timely assess the participation of anaerobic bacteria in the septic process and add metronidazole to the treatment regimen. Empirically, metronidazole is included in therapy in all cases of abdominal sepsis (peritonitis, abdominal abscesses, intestinal fistulas), with deep suppurative processes chest(mediastinitis, esophageal perforation, pleural empyema), with ruptures internal organs, hematomas, brain abscesses, etc. In the table. 3 presents recommendations for the combined use of IV generation cephalosporins.
Of course, the treatment of such children should be carried out under microbiological control at least 2 times a week; timely targeted correction of antibiotic therapy regimens, depending on the monitoring data, significantly increases the chances of saving the patient. Conclusion
The arsenal of antibacterial drugs approved for use in children has been replenished with a new antibiotic, the fourth-generation cephalosporin cefepime. The drug is extremely important for the treatment of children with severe infections, especially in the case of isolation of gram-negative multi-resistant microorganisms with sensitivity to cefepime. Use of cefepime for empiric therapy indicated in children with failure of previous treatment with other b- lactam antibiotics, since cefepime is active against hospital strains-hyperproducers b- extended spectrum lactamase. cefepime it is advisable to include in the formulary of antibiotics for children's intensive care units, since at present, in terms of efficiency and safety, it can be considered as a highly effective antibiotic in children with the most severe manifestations of sepsis, including septic shock and multiple organ failure.Literature:
1. Yakovlev S.V. Cefepime is a 4th generation cephalosporin antibiotic; Antibiotics and Chemotherapy, 1999; 44(7): 32-7.
2. Vostricova T.Yu, Beloborodova N.V., Kurchavov V.A. In vitro activity of Cefepime and othe
r antimicrobials against gram-negative bacteria. J Chemother April 1999; 11(suppl.2): 107.
3. Quadri SM., Cunha BA., Ueno Y., Abumustafa E., et al: Activity of cefepime against nosocomical blood culture isolates; J Antimicrob Chemother 1995 Sep; 36(3): 531-6.
4. Sofianou D., Tsoufla S., Kontodmou L., Polydorou F., Malaka E.: Comparative in vitro activity of cefepime against nosocomical isolates. J. Chemother, Oct 1997; 9(5): 341-6.
5. Mebis J., Goossens H., Bruyneel P. et al. Decreasing antibiotic resistance of Enterobacteriaceae by introducing a new antibiotic combination therapy for neutropenic fever patients. Leukemia, 1998; 12:1627-9.
6. Hancock RE, Bellido F. Antibacterial in vitro activicy of fourth generation cephalosporins. J Chemoherapy 1996; 8(Suppl.2): 31-6.
7. Ramphal R., Gulcap R., Rotstain C. et al. Clinical experience with single agent and combination regimens in the management of infection in the febrile neutropenic patient. Am. J. Med., 1996; 100:83-9.
8. Saez-Llorens X., Castano E., Garcia R., Baez C., Perez M., Tejeira F., McCracken GH Jr.: Prospective Randomized comparison of cefepime and cefotaxime for treatment of bacterial meningitis in infants and children; Antimicrob Agents Chemother Apr. 1995; 39(4): 937-40.
9. Reed MD., Yamashita TS., Knupp CK., Veazey JM. Jr, Blumer JL: Pharmacokinetics of intravenously and intramascularly administered cefepime in infants and children; Antimicrob Agents Chemother Aug 1997; 41(8): 1783-7.
10. Schaad UB., Eskola J., Kafetzis D, Fishbach M., Ashkenazi S., Syriopoulou V., Boulesteix J., De Pril V., Gres JJ, Rollin C.: Cefepime vs. Ceftazidime treatment of pyelonephritis: a European, randomized, controlle study of 300 pediatric cases. European Society for Pediatric Infectious Disease (ESPID) Pyelonephritis Study Group; Paediatr Infect Dis J Jul 1998; 17(7): 639-44.
11. Mustafa M.M. Cefepime versus Ceftazidime in the Empiric Treatment of Febrile Neutropenic Children with Malignancy. In: Febrile Neutropenia /J.A.Klastersky (ed.), 1997; 75-6.
12. Neu HC.: Safety of cefepime: a new extended-spectrum parenteral cephalosporin; Am J Med Jun 1996; 24; 100(6A): 68S-75S.
4th generation cephalosporins act on pathogenic microorganisms due to 7-aminocephalosporanic acid, the abbreviation for the substance is 7-ACA. Wide spectrum The action of drugs of the fourth generation is due to their effectiveness against all gram-negative bacteria, anaerobic microorganisms and bacterioids. Scope of 7-ACC:
- damage to the bacterial cell membrane;
- stopping the growth and spread of the colony;
- inhibition of all associated microorganisms from the list of pathogens that are involved in the formation of the inflammatory process.
4th generation drugs include drugs that have repeatedly confirmed their benefits for the recovery of patients:
- Cefepime;
- Cefpir.
You can not independently treat such potent drugs. Cephalosporins are prescribed only by a doctor when the nature of the infection is established. For Gram-positive microorganisms, fourth-generation drugs are less effective than first-generation drugs, so if a patient starts self-treatment, it may not get the desired result. The doctor evaluates the risks of side effects, selects the best treatment strategy for each clinical picture.
Pathogenic agents synthesize beta-lactamase, an enzyme that protects the membrane lining of their cells. The main task of the antibiotic is to destroy the cell, and the membrane shell prevents this. 7-ACA destroys both types of beta-lactamase:
- chromosomal;
- plasmid.

When beta-lactamase is destroyed, cells cannot exist, the contents are released into the environment, captured by phagocytes and excreted from the body in the same way as any decay products.
All four generations of cephalosporins inhibit the synthesis of beta-lactamase, but only 4th generation drugs are aimed at the chromosomal type of the enzyme. The instructions for Cefepim and Cefpirom contain information that treatment during pregnancy should be carried out only if the probable benefit to the mother is greater than the potential threat to the development of the fetus. This means that only the attending physician can assess whether it is necessary to prescribe 4th generation cephalosporins or less powerful drugs can be dispensed with. If treatment is required during lactation, there are 3 options:
- stop feeding;
- curtail feeding and transfer the child to artificial feeding;
- choose another drug.
The patient should not take antibiotics on her own, because, getting into the child's body with breast milk, they cause intestinal dysbacteriosis.
When is the medicine given?
 The scope of influence of drugs of the 4th generation includes all infectious diseases, in the formation of which take part:
The scope of influence of drugs of the 4th generation includes all infectious diseases, in the formation of which take part:
- enterococci and enterobacteria;
- staphylococci and streptococci;
- meningococci and gonococci;
- proteobacteria, including salmonella;
- helicobacteria.
These microorganisms cause more than 80% of cases of all infectious inflammatory processes.
A distinctive feature of gram-negative bacteria is the presence of additional protection on the cell wall.
During the breakdown of lipopolysaccharides, which are part of the membrane, toxic substances are released - endotoxins. If a large number of pathogenic agents are simultaneously destroyed, endotoxins, entering the circulatory and lymphatic systems, cause the patient:

- headache, heaviness in the head;
- weakness, muscle pain, joint pain;
- nausea and vomiting;
- lack of appetite;
- temperature rise to 38°C or more;
- lowering blood pressure;
- in severe cases - delirium, confusion, shortness of breath, fainting;
- without medical attention, death from toxic shock is possible.
When the immune system destroys gram-negative microorganisms, intoxication occurs with the decay products of their cellular structures, including endotoxins.
If treatment is started as soon as the diagnosis is established, then intoxication has minimal consequences for the body. In advanced cases, intoxication takes life-threatening forms. 4th generation cephalosporins can be used in combination with drugs that cleanse circulatory system, with sorbents and diuretics.
The main indications for the appointment
If a laboratory analysis of a smear, scraping or blood reveals one or more gram-negative microorganisms, the attending physician prescribes antibiotics. Most often, cephalosporins are prescribed: 
- In diseases of the genitourinary system: cystitis, urethritis, prostatitis, gonorrhea, epididymitis, salpingo-oophoritis, pyelonephritis and others.
- In diseases of the respiratory system: lung abscess, tracheitis and bronchitis, pneumonia, pleural empyema.
- With abscesses, carbuncles and boils of the skin, with wounds complicated by a purulent inflammatory process.
Cephalosporins are sometimes prescribed to patients with a reduced immune status, but in making such a decision, the doctor takes into account the potential benefit and potential harm to the patient.
Contraindications
To reduce the harmful effects of cephalosporins on gastrointestinal tract and increase the bioavailability of drugs, 4th generation drugs have been created that are administered parenterally:
- intramuscularly;
- intravenously.
 Previous generations included oral cephalosporins, which increased the chance of side effects and reduced the bioavailability of 7-ACA. 4th generation cephalosporins also have contraindications, but they are much less than 1-2 generation tablets. There are restrictions on reception, you can not use:
Previous generations included oral cephalosporins, which increased the chance of side effects and reduced the bioavailability of 7-ACA. 4th generation cephalosporins also have contraindications, but they are much less than 1-2 generation tablets. There are restrictions on reception, you can not use:
- during pregnancy and during breastfeeding;
- newborn children up to 2 months of life;
- with chronic uncompensated kidney disease;
- with an individual allergic reaction.
The frequency of allergy to 7-ACC and other components of the drug, according to clinical trials, does not exceed 1%. Patients with hypersensitivity are more likely to be allergic to:
- to 1-3 generation cephalosporins, since 4th generation cephalosporins have a similar chemical composition;
- to all antibiotics that also act on beta-lactamase and cause the release of endotoxin.
 Studies have been conducted on the study of allergies to various groups of antibiotics. The data obtained indicate that 10% of all patients allergic to penicillin were also allergic to cephalosporins. In addition to an allergic reaction, an increased number of complications and side effects was noted. The use of Cefepim and Cefpirome most often occurs in a hospital, therefore, even if there are any complaints about side effects, doctors can immediately take steps to improve the patient's well-being. In some cases, for example, with complications from the kidneys, you need to change the course of treatment and choose another drug. The most likely (with a frequency of up to 1%) side effects:
Studies have been conducted on the study of allergies to various groups of antibiotics. The data obtained indicate that 10% of all patients allergic to penicillin were also allergic to cephalosporins. In addition to an allergic reaction, an increased number of complications and side effects was noted. The use of Cefepim and Cefpirome most often occurs in a hospital, therefore, even if there are any complaints about side effects, doctors can immediately take steps to improve the patient's well-being. In some cases, for example, with complications from the kidneys, you need to change the course of treatment and choose another drug. The most likely (with a frequency of up to 1%) side effects:
- From the digestive system: jaundice, hepatitis, vomiting and nausea, constipation or loose stools, epigastric pain, belching, heartburn, flatulence, colic.
- For allergies: skin rash, hives, fever, sweating, shortness of breath.
- From the side of cardio-vascular system: angina pectoris, increased or slowed down heart rate, increase or decrease in the tone of blood vessels.
- From the nervous system and psyche: psychomotor agitation, headache, insomnia, convulsions and spasms of smooth muscles.
- From the respiratory system: shortness of breath, cough.
Intravenous administration of 4th generation cephalosporins should be carried out in accordance with professional nursing standards. Otherwise, post-injection phlebitis occurs.