Principles of innervation of internal organs. Internal organs innervation principles innervates internal organs
2.
3.
4.
5.
6.
Complete vegetative reflex arc
Vegetative fibers approach methods to innervored
Structures.
Morphofunctional differences between the somatic part of the NA
Vegetative.
Types of innervation.
Essence of afferent and efferent innervations.
Innervation of vessels and internal organs of the head, neck,
Breast, abdominal cavities and pelvis.
1
In the innervation of internal organs participates as
somatic nervous system and vegetative
Somatic nervous system provides
Afferent (sensitive) innervation and;
Efferent (motor) somatic
Innervation (maintenance of tone and reduced
cross-striped muscles)
2
The principle of innervation of internal organs
Vegetative nervous system provides:Afferent innervation without the participation of CNS
According to the principle of axon reflex;
and efferent vegetative
(sympathetic and parasympathetic)
a) motor (maintenance of tone and
Reducing smooth muscles and heart muscles)
b) secretory (change in secretory
Roleberry cells)
3The essence of afferent innervation is:
In the perception of receptor energies
irritants from the external and internal environment;
transforming it into the nervous impulse
(excitation);
transfer it to the instance of the CNS, on the basis of which
A response of the body is formed
(Adaptation is carried out).
The essence of efferent innervation is
Transfer of a nervous pulse formed
based on afferent innervation, to workers
organs (effectors) that are muscles
and iron fabric, resulting in
regulation of tone and degree of muscle contraction or
Regulation of the allocation of quantity and quality
Secret.
4 Almost all internal organs have
Three types of innervation:
afferent
Efferent somatic
and vegetative (sympathetic and
parasympathetic).
5
Ways of the approach of afferent nerve fibers:
INComposition
Structures
(branches)
Spinal nerves
As part of the structures (branches) of the cranial
nerves
IN
Composition
Structures
(branches)
Vegetative
trunks
plexus
nerves.
(For example, to
Sympathetic
Nervam.
Sensitive fibers are suitable
Through white connecting branches) 6
Ways of the approach of efferent somatic motor) nerve fibers:
TOScalp and Neck (muscles
language, soft sky, pharynx, larynx,
upper third of the esophagus, eye
apple, middle ear) - as part
branches of relevant skulls
nerves (III, IV, V, VI, VII, IX, X, XI, XII couples
Chernoy
nerves)
to
Outdoor
Sphintera of the rectum and urethra - in
7
Fine nerve composition.
Ways of the approach of efferent vegetative (motor and secretory) nerve fibers:
Parasympathetic nerve fibers:As part of the branches of the cranial nerves (from
Parasympathetic nuclei of III, VII, IX, X pairs)
As part of the branches of the in-government nerves (from
Sleep segments spinal cord)
Sympathetic nerve fibers:
As part of the branches of the spinal nerves
(on white connecting branches)
As part of the branches of perivasal plexuses
8
VII, IX, X pairs of cranial nerves.
910.
1011.
EfferentSympathetic
Innervation
Internal organs are obtained from sympathetic
Ganglia
–
Paveltebral
and
Properebral
through
Sympathetic
plexus.
Efferent parasympathetic innervation
Internal heads of heads get from
parasympathetic nuclei 3, 7, 9 pairs of cranial
nerves; Neck, chest and abdominal organs
cavities sigmid gut - iz
parasympathetic core 10 pairs of cranial
nerves; Sigmid intestine and all the organs of small
pelvis - from lateral intermediate
sacral segments Sii-IV.
11
12. Innervation of vessels
Innervation.
Afferent
Innervation
Vessels
Head
carried out by sensitive fibers in the composition
Branches of cranial nerves (V, IX, X).
Afferent innervation of neck vessels, torso,
limbs and internal organs are carried out
sensitive fibers in the composition of the branches
Spinal nerves.
12
13.
1314. Innervation of vessels
EfferentInnervation
vessels.
The overwhelming number of vessels have only
Sympathetic effectant innervation.
from
All
Sympathetic
nodes
(Paraia.
Properebral)
Connecting branches.
14
15. What innervates the VNS?
All smooth musclesa) in the wall of the internal organs
b) in the wall of the vessels
c) in sense organs (in the skin - M.ERRECTOR PILI,
Mm.Ciliares, Sphincter et dilatator pupilae)
Cardiac muscle
Breeding cells
VNS function - adaptation-trophic
15
16. Localization of neurons in a three-meric vegetative reflex arc.
The body of the first afferent (sensitive)neuron (it is common for somatic and
Vegetative reflex arcs) is located
In the ganglia of the spinal and cranial nerves.
The body of the second inserted neuron is in
Side pillars of the spinal cord C8-L2, S2-S4
segments and in parasympathetic nuclei III, VII,
IX, X pairs of cranial nerves.
The body of the third efferent (motor or
secretory) neuron is localized in all
Vegetative ganglia.
16
17. The method of approach vegetative fibers to the innervored authorities.
Vegetative fibers reachinnervated organs in the composition:
1) somatic CMN and CN and their
branches
2) vegetative nerves,
3) vegetative plexuses and their
branches.
17
18.
12
3
18
19. Morphofunctional differences between the somatic part of the nervous system from the vegetative (see the previous lecture)
SomaticView of the difference
nervous system
1. Like nerve relative
Fibers (nerves) segmentality
From the central nervous system.
Fiber output
(nerves)
2. Availability
Melinovye
Melinova
nerve fibers
Shell
3. Objects
Exhausted
Efferent
Crossinnevation
striped
(skeletal)
muscle.
Vegetative
nervous system
Foci of exit
Fibers (nerves)
Mostly
Bezhelinic
nerve fibers
- Momes.
the cloth,
-Ischarge
Cardual
muscle,
- Irony
19
Cells
20.
View of the difference4. Structure
Efferent level
reflex arc
Somatic nervous
system
Single-stage (axon
Motor Neuron
Without a break reaches
effector)
Vegetative nervous
system
Double-line, B.
which is distinguished by post-genonar
Nervous fibers.
5. Localization places
Reflux neurons
Arcs:
a) afferent
neuron;
b) insert neuron;
c) efferent neuron
-In somatic ganglia - in somatic
CMN and H).
Ganglia SMN and CN.
-Ont back horns
spinal cord I.
Sensitive nuclei
CN.
-In side horns
spinal cord and in
Vegetative
(parasympathetic)
nuclei CN.
- in the front horns
spinal cord I.
Motor nuclei CN
- Vegetative
(sympathetic I.
parasympathetic)
20
ganglia.
21. Types of innervation
I. Afferent (sensitive)II. Efferent:
1. somatic (motor) only
The attitude of skeletal muscles
2. Vegetative (sympathetic and
parasympathetic)
a) Motor (with respect to smooth
muscles and muscles of the heart)
b) secretory (in relation
ferbo cells)
21
22. The essence of afferent innervation is:
in perception receptor formationsEnergy of irritants from the external and internal
environments;
2. Transformation of this energy into a nervous impulse
(excitation);
3. Transfer nerve impulses In the instance of the CNS, on
basis of which is formed a response
organism (providing its adaptation to
constantly changing conditions).
Part of nerve impulses by conductive
The paths of analyzers reach their cortical nuclei,
in which based on top analysis and synthesis
Human pulse data occurs
sensations, ideas, concepts, generalizations
22
about the world (cognitive function)
1.
23. The essence of efferent innervation is:
in the transfer of the nervous impulse formed onbasis of afferent innervation, from nuclear formations
CNS, to the working bodies (effectors), which are
Muscles and glandular cells. Distinguish
noted above, the efferent somatic and
Vegetative innervation.
Efferent somatic (motor) innervation
lies in the regulation of the tone of skeletal muscles and
implementation of the effect of their reduction;
Efferent vegetative (motor) sympathetic and
Tonus of cardiac and smooth muscles and effect implementation
their abbreviations;
Efferent vegetative (secretory) sympathetic and
couple sympathetic innervation lies in regulation
Allocations of quantity and quality by themes by iron. 23.
24.
Almost all human body organshave
Sensitive
innervation
which is carried out mainly
somatic part of the NA.
Organs in the structure of which are there although
would one type of muscle tissue or
ferbo cells, for example, internal
Organs
have
and
Efferent
innervation that is carried out as
somatic and vegetative
ns departments.
24
25.
Thus, the overwhelming majorityinternal organs have three types
Innervations:
1.Apphetable.
2. Effective vegetative innervation
(sympathetic and parasympathetic).
3. And the organs, which are available
Cross-striped muscles, have
yet
and
Efferent
somatic
Innervations.
Afferent and efferent somatic
Innervation
Domestic
organs
25
It is carried out somatic CMN and CN.
26.
EfferentMotor
and
Secretoric
Vegetative sympathetic and parasympathetic
Innervations
implemented
Vegetative
Fibers and nerves.
Efferent vegetative innervation.
a) Efferterent sympathetic innervation of organs
It is carried out from a single sympathetic nucleus, n.
Intermediolateralis (C8 - L2) of the spinal cord. Nervous
Impulses from neurons of this kernel are followed by their axes
(Preggglyonar
fibers)
Reach
paravertebral or excellent ganglia.
In these ganglia, the nervous switch occurs
Impulses on the neurons of ganglia. According to the axes of these
neurons (postganglyonary fibers) that
form sympathetic perivzal plexuses,
Nervous impulses are suitable for innervored
26
structures of organs.
27.
b) Efferent parasympathetic innervationorgans are carried out from nuclear structures
Head and pelvic parts parasympathetic
Systems are parasympathetic kernels III, VII, IX, X
Caps of cranial nerves and parasympathetic kernel, n.
Intermediolateralis S2-4 spinal cord.
Nerve impulses from neurons parasympathetic
kernels go on their axons (preggangonary
fibers)
Reach
Porgranny
and
Ostrganian ganglia. In these ganglia occurs
Switching nerve pulses on neurons
ganglia.
By
axon
These
Neurons
(postganglionary fibers) nerve impulses
Suitable for innervated organ structures.
27
28.
Often at a certain length, asPreggalionary and postgangling
Sympathetic and parasympathetic fibers
form vegetative (sympathetic and
parasympathetic) nerves. Therefore, when
Hearing
Innervations
organs
Often
Figure vegetative nerves having
Own name.
28
29. Innervation of vessels
Vessels have afferent and efferentInnervation.
Afferent
Innervation
Vessels
Head
is carried out by sensitive fibers in
composition of branches V, IX, X pairs of cranial nerves, and
neck vessels, torso, limbs and internal
organs - sensitive fibers in the composition
Branches of CMN and N. Vagus (x).
To the internal organs sensitive fibers
Suitable in the composition sympathetic nervesin which
they go through white connecting branches, and
Also as part of the branches of the vagus nerve.
All sensitive fibers are dendrites.
afferent
pseudoNIPolar
Neurons
somatic ganglia SMN and CN
29
30.
3031.
Efferent innervation of vessels. Vesselshave only sympathetic efferent
Innervation.
1) to the smooth muscles of the vessels of internal
Pastgangle fibers are suitable in
composition of sympathetic perivasal plexuses
from
All
Sympathetic
nodes
(Paraia.
Properebral)
2) To the smooth muscles of transverse muscles postgangling fibers
suitable as part of the branches of the spinal
nerves in which they come through gray
Connecting branches.
31
32. Innervation of internal organs
InnervoiledBodies I.
Structures
Afferent
somicich.
Innervation
Head
1.
Mucous
oral cavity
nose, sky,
pharynx
GORTANY I.
conjunctiva
Nizhnye
century
Branches
and
n. Trigeminus.
(v)
Efferent innervation VNS
Sympathetic
Parasimpatic
Columna.
Intermediolateralis,
Radix Ventralis.
NN.Spinales, RR.
Communicantes Albi *,
Ganglion Cervicale
Superius TR.SYMPATHICI,
N.CAROTICUS INTERNUS,
Plexus Caroticus.
INTERNUS, N. Petrosus.
PROFUNDUS.
N. Salivatorius sup.
(Vii), n.interMedius,
N.Petrosus Major,
G.Pterigopalatinum:
1.Rr.Nasales.
Posteriores Mediales,
Laterales et Inferiores.
2.Nn.Palatinus Major et.
Palatini minores.
3.r.pharyngeus
Efferent
somicich.
Innervation
not
32
33.
Innervored authorities I.Structures
2.
Language
Afferent somatic.
Innervation
General
Sensitivity: n.
Lingualis (V).
Flavor
sensitivity:
Front nipples 2/3
mucous membrane
Taste fibers
Chorda Tympani (VII), and
nipples rear 1/3.
mucous membrane
RR flavor fibers.
Linguales (IX).
In area
Nastestrian - R.
Laryngeus Superior (X)
Effer. Sympathetic.
Inn-Ya
Efferent parasympathetic Inn-I
Efferent somatic.
Inn-Ya
n.Salivatori- muscles
US SUP. (VII), Language -
–«–
n. intermedius;
Chorda.
Tympani.
(Vii).
n.
Hypogloss.
US (XII)
33
34.
3.Branches
Soft 1) n.
sky
Palatinus.
Major, NN.
–«–
Palatini.
Minores (V)
2) NN. Palatini et n. Nasopalatinus.
(IX)
4.
Plexus.
*, Ganglion.
PHARINGEUS, CERVICALE
Educated superius
IX and X CH TR.SYMPATHIC
I, RR.
ET TR.
Sympathicus Laryngopharyngei.
n.Salivatori 1) M.Tensor Veli
-US.
Palatini - n.
sup. (VII),
MandiBularis (V)
n. intermedius;
N.Petrosu.
s major.
2) m. Levator Veli.
Palatini, m. Palato.
Glossus, m.
Palatopharyngeus, m.
Uvulae - RR. Palatini (X)
1) M.Stylopharyngeus -
n. Glossopharyngeus.
(IX)
2) mm. Constric-Tor
PHARYNGIS SUPERIOR,
PHARYNGE MEDIUS, INFERIOR; m.
Salpingopharyngeus34i (x).
RR. PHARYNGEI (x)
n.Salivatori.
-us inf.
(IX),
n.dorsalis
Nervi Vagi.
(X), RR.
35.
InnerviruMy bodies
and structures
Afferent
somicich.
Innervation
5. Employed. LINMECHLUST- Gualis
Naya I.
(v)
Subject
glands
6.
Okolous
gland
n.
Auriculotemporeles.
(v)
Efferent innervation VNS
Sympathetic
*, Ganglion Cervicale
Superius TR.SYMPATHICI,
NN.CAROTICI EXTERNI, PLEXUS
Caroticus externus
- \\ -
Parasimpatic
N.Salivatorius sup.
(N.interMedius), Chorda
Tympani (VII),
G.SUBMANDIBULARE ET.
G.Sublinguale.
N.Salivatorius Inferior,
N.Tympanicus.
N.Petrosus Minor (IX)
g.oticum
N.Aoriculotemporaalis (V)
35
36.
3637.
3738.
4. mm.SphIncter.
Pupilae et.
ciliaris.
vascular
Shell
Eye
Apple
n.
Ophthal.
Micus
NN.
Ciliares.
Longi et.
Breves.
m.dilatator.
Pupilae.
vascular
Shell
Eye
Apple
- \\ -
not
N.oculomotorius.
Accessorius (III),
Radix.
ParasyMpaticus,
G.Ciliare,
NN.CILIARES BREVES.
(V)
*
n.caroticus.
Internus.
Pl.caroticus.
Internus.
Pl.ophthalmicus.
not
38
39.
NeckIX and X CHN ET
larynx,
tr.
trachea,
Sympathicus.
Shield I.
Parasitovoid
glands
*, Ganglii.
Cervicales Superius,
medium
Cervicothoracicum
(Stellatum)
TR.SYMPATHICI.
NN. Carotici Externi,
Plexus Caroticus.
externus.
1. nucl.dorsalis
N.Vagi, Chine
branches (x)
39
40.
Chestcavity
Esophagus
Lung
A heart
Sensses
Elno
branches
N.Vagus I.
Sympathetic
nerves
Ganglii Thoracici (C2-5)
TR.SYMPATHICI,
Aortic
plexus
*,
1) N.Cardiacus
Cervicalis Superior (from
Top Shane. node)
2) - \\\\ - Medius (from
Middle Shane. node)
3) - \\\\ - Inferior (from
Nizhny Shane. node)
4) nn.cardiaci
Thoracici (from the upper
chest. nodes
TR.SYMPATHICI.)
Nucl.dorsalis N.Vagi.
(X), breast branches
N.Vagi.
Rami Cardiaci N.Vagi:
a) Rami Cardiaci
Superiores (from
N.LARYNGEUS Superior)
b) Rami Cardiaci
Inferiores (from
N.LARYNGEUS Reccures I.
Breedless N.Vagi)
40
Plexus Cardiacus Superficialis et Profundus
41.
PericardiumNucl.dorsalis
Breast
*
Top N.Vagi (X),
branches n.
Breast
(Breasts
Vagus (x),
Truncus branch nodes) (x)
branches n.
Sympathicus.
phrenicus:
RR.PERICARDI.
Acophrenic
US.
41
42.
4243.
Abdominalcavity
1. Stomach,
Thin I.
Thick
Kiska Bes
Sigmoid
Hepar,
Pancreas, Ren,
Lien
gl.suprarenalis
(Cortex)
Abdominal
branches
1) N.Vagus.
2) N.Splanch
Nici Major.
3) - \\\\ - minor
4)
n.phrenicus.
sinister
5) NN.
splanchnici.
Lumbales.
N.dorsalis
Nervi Vagi.
1) Lower
(X),
Breast gangll. tr. (abdominal
Sympathici,
branches)
N.Splanchnicus.
Major.
2) - \\\\ - minor
3) Ganglia
coeliaca,
Aortorenalia,
PL. Mesenttericum.
SUP. ET INF.
(pl.caeliacus)
*
43
44.
4445.
2.1.N. SplanSigmid-chnici.
Naya I.
Pelvini.
straight
guts;
3. Matter,
Muffal
pipes
Seed
bubbles
prostate,
ovary,
testicle
Ganglia Sacralia.
Trunci Sympathici.
a) PL.
Intermesentericus,
MeSentericus.
Inferior
Hypogastricus.
Superior.
b) nn.
Hypogastrici.
DEXTER ET SINISTER
c) Plexus.
Hypogastrici.
Inferiores.
Nuclei.
ParasyMpathetici S2-4,
N.N.
splanchnici.
Pelvini.
The innervation of the internal organs is the reflex activity of the nervous system. The sensitive link for the head organs is represented by the sensitive apparatus V, VII, IX and X cranial nerve-cranial sensitive afferent innervation. But the wandering nerve, justifying its name, reaches its fibers of the descending colon, these fibers contain, including a sensitive portion. The face of the crane sensitive afferent innervation of the internal organs of the neck, chest, abdomen. These organs have both spinal sensitive innervations, so - There is a double nature of the sensitive innervation of the organs of the neck, chest and abdomen. The descending colon, the sigmoid guts and the small pelvis organs receive only spinal sensitive innervation, since the branches of the vagus nerve do not reach them (the area of \u200b\u200bits innervation corresponds to the basin of the upper mesenteric artery). In addition to sensitive innervation, internal organs should receive vegetative innervation, and in some cases they need a motor. The question of the nature of the innervation of internal organs is quite interesting. To answer it, it is necessary to clearly represent the structure of the organ, various fabrics require of various types Innervation, its localization and place of its embryo bookmark. The innervation path of the organ, as well as the blood supply passes in the shortest straight line. Motor innervation will be absent in organs devoid of cross-striped muscles.
Innervation GL. Lacrimalis
Innervation of muscle, narrowing pupil and ciliary muscles, m. Sphincter pupilae et m. Ciliaris.
Muscle innervation, expanding pupil, m. Dilatator Pupilae.
Innervation Tunicae Mucosae Nasi Et Palati
| Names of central kernels | ||||
| SNS. | N. Caroticus Internus è Plexus Caroticus Internus, èn. PETROSUS PROFUNDUS, è N. Canalis Pterygoidei è further follows with parasympathetic fibers | |||
| PSNS. | N. FACIALIS, èN. Petrosus Major, è N. Canalis Pterygoidei. | Cutting knot, gangl. Pterygopalatinum | N. Trigeminus èn. Maxillaris, branches of a chamber knot: RR. Nasales Posteriores Superiores, Laterales et Mediales, N. Nasopalatinus, n. Palatinus Major, NN. Palatini Minores, NN. Nasales Posteriores Inferiores. |
INNERVATION GLANDULAE SUBMANDIBULARIS ET SUBLINGUALIS
| Names of central kernels | Travel of predaranny nerve fibers | The names of peripheral vegetative ganglia | Postganglionic nerve fibers | |
| SNS. | Substantia Intermedia Lateralis, (th i - th iv) spinal cord segments | Front recesses of spinal nervesè White connecting branches | Upper cervical gangli, gangl. Cervicale Superius. | N. CAROTICUS EXTERNUS и PLEXUS CAROTICUS EXTERNUS, и PLEXUS PERIARIALIS A. lingualis |
| PSNS. | Upper salivaeotivative nucleus, NUCL. Salivatorius Superior (N. Intermedius, Pons) | N. Facialis è Chorda Tympani è n. Lingualis, nodal branches, RR. ganglionares. | Lummy gear, Gangl. SubmandiBulare, Podium Node, Gangl. Sublinguale | Ferrous branches, RR. Glandulares. |
Innervation Glandula Parotis
| Names of central kernels | Travel of predaranny nerve fibers | The names of peripheral vegetative ganglia | Postganglionic nerve fibers | |
| SNS. | Substantia Intermedia Lateralis, (th i - th iv) spinal cord segments | Front recesses of spinal nervesè White connecting branches | Upper cervical gangli, gangl. Cervicale Superius. | N. CAROTICUS EXTERNUS и PLEXUS CAROTICUS EXTERNUS, и Plexusion around the surface temporal artery and its branches to the parotidei salivary gland (RR. Parotidei) |
| PSNS. | Bottom salivaeotivative nucleus, NUCL. Salivatorius Inferior (N. Glossopharyngeus, Medulla Oblongata) | N. Glossopharyngeus è N. TYMPANICUS и PLEXUS TYMPANICUS, è N. Petrosus Minor | Own node, Gangl. Oticum. | Connecting branches with urinous nerve, RR. Communicantes Cum n. Auriculotemporalis, èn. Auriculotemporalis. |
Heart innervation
| Names of central kernels | Travel of predaranny nerve fibers | The names of peripheral vegetative ganglia | Postganglionic nerve fibers | |
| SNS. | Substantia Intermedia Lateralis, (th i - th iv) spinal cord segments | Front recesses of spinal nervesè White connecting branches | Gangl. CERVICALE SUPERIUS, MEDIUM, GANGL. Cervicothoracicum (Stellatum), Gangl. THORACICA II-V | N. Cardiacus Cervicalis Superior, Medius, Inferior, Breast Heart Branches II-V Breasts, RR. Cardiaci Thoracici. |
| PSNS. | N. Vagus è RR. Cardiaci Cervicales Superiores Et Inferiores, Breast Cardiac Branches, RR. Cardiaci Thoracici. | Installations of parasympathetic visceral plexuses, Gangl. ParasyMpathica Plexus Visceralis (node \u200b\u200bfields of six plexigcardial heartbands) | Cardiac plexus, Plexus Cardiacus |
Innervation of trachea, bronchi, lungs, and esophagus
| Names of central kernels | Travel of predaranny nerve fibers | The names of peripheral vegetative ganglia | Postganglionic nerve fibers | |
| SNS. | Substantia Intermedia Lateralis, (th i - th iv) spinal cord segments | Front recesses of spinal nervesè White connecting branches | Gangl. Cervicothoracicum (Stellatum), Gangl. THORACICA II-V | RR. Oesophagei Breast nodes of the sympathetic barrel è Plexus Oesophagalis, RR. Pulmonales of nodes of the sympathetic barrel è Plexus Pulmonalis |
| PSNS. | The rear core of the wandering nerve, NUCL. dorsalis n. Vagi (MEDULLA OBLONGATA) | N. Vagus è Plexus esophagalis, bronchial branches, RR. Bronchiales, | Esophagalia Plexus Osophagalia, Light Weight, Plexus Pulmonalis |
Innervation of the stomach, intestines, liver,
pancreas, kidneys, spleen, adrenal cortex
| Names of central kernels | Travel of predaranny nerve fibers | The names of peripheral vegetative ganglia | Postganglionic nerve fibers | |
| SNS. | The front roots of the spinal nervesè White connecting branches. Splanchnicus Major, N. Splanchnicus Minor, NN. Splanchnici Lumbales, èlexus Suprarenalis | Gangl. Coeliaca, Gangl. Aortorenalis, Gangl. Mesenttericum Superius, Gangl. Mesenttericum Inferius. | Plexus Coeliacus, Plexus Intermesenttericus, Plexus Hepaticus, Plexus Lienalis, Plexus Pancreaticus, Plexus Renalis, Plexus Suprarenalis, Plexus Mesenttericus Superior, Plexus Mesenttericus Inferior | |
| PSNS. | The rear core of the wandering nerve, NUCL. dorsalis n. Vagi (MEDULLA OBLONGATA) | N. Vagus è Plexus esophagalis è truncus vagalis anterior; Truncus Vagalis Posterior; èrr. Hepatici, RR. coeliaci, | Parasympatic nodes, Gangl. Parasympathica, visceral plexuses, Plexus Visceralis, innervated organs | Plexus Hepaticus, Plexus Lienalis, Plexus Pancreaticus, Plexus Gastricus, Plexus Entericus, Plexus Subserosus, Plexus Myentericus, Plexus Submucosus, Plexus Renalis |
Innervation of adrenal brainstant
(Analogue of finite sympathetic ganglia)
| Names of central kernels | Travel of predaranny nerve fibers | The names of peripheral vegetative ganglia | Postganglionic nerve fibers | |
| SNS. | Substantia Intermedia Lateralis, (TH IV - TH XII) spinal cord segments | The front roots of the spinal nervesè White connecting branches. Splanchnicus Major, N. SPLANCHNICUS MINOR èPLEXUS SUPRARENALIS | AKSOeepithelial synaps of the end of the first neuron sympathetic chain with brainstant cells of adrenal glands | Postganglionary fibers are missing. Human nature control signals - brainstant hormones of adrenal glands stand out into the bloodstream and transferred blood flow to control objects |
| PSNS. | The rear core of the wandering nerve, NUCL. dorsalis n. Vagi (MEDULLA OBLONGATA) | N. Vagus è Plexus esophagalis è Truncus Vagalis Posterior; è RR. Renales. | Parasympatic nodes, Gangl. Parasympathica, visceral plexuses, Plexus Visceralis, innervated organs | Renal, plexus, Plexus Renalis, adrenal plexus, Plexus Suprarenalis. |
Innervation of the rectum, urinary organs, genital organs
| Names of central kernels | Travel of predaranny nerve fibers | The names of peripheral vegetative ganglia | Postganglionic nerve fibers | |
| SNS. | SUBSTANTIA INTERMEDIA LATERALIS, (THI IV - L II) spinal cord segments | Front recesses of the spinal nerves. White connecting branchesèEZhUZNE branches. Nn. Splanchnici Sacrales, Plexus Hypogastricus Superior, Plexus Hypogastricus Inferior | Sampling, Gangl. Sacralia Trunci Sympathies. | Plexus Rectales Medii Et Inferiores, Plexus Prostaticus, Plexus Deferentialis, Plexus Uterovaginalis, Plexus Vesicales. |
| PSNS. | Nucll. ParasyMpathici Sacrales (S II - S IV) spinal cord segments | Front spores of the spinal nerve of the branch branches of the spinal nervesèradices Ventrales NN. Spinales, è Plexus Sacralis, ènn. Splanchnici Pelvini. | Pelvic nodes, Gangl. Pelvina, Visceral Ganglia, Ganglia Visceralia, Lower Straightened Plexus, Plexus Rectalis Inferioris | Plexus Recales Inferiores, Plexus Prostaticus, Plexus Deferentialis, Plexus Uterovaginalis, Plexus Visceralis. |
Innervation blood vessels
A brief overview of the vegetative innervation of internal organs (anatomy)
Stories and Comments (Start)
In the "human anatomy", edited by the Honored Worker of Science of the RSFSR, Professor M.G. The bridges are a chapter where a brief overview of the vegetative innervation of organs and, in particular, innervation of the eye, glands of tears and salivary, hearts, lungs and bronchi, gastrointestinal tract, sigmoid and rectum and bladderas well as blood vessels. All this is necessary to build a logical circuit of evidence, but to solve everything in the form of a quotation, too cumbersome - it is enough to bring one quote regarding only innervation of lungs and bronchi, and in the future only adhere to the main semantic content (with the preservation of the material presentation) already covered in anatomy, vegetative innervation of organs.
Describing that actually occurring cases and comments on them, I will not adhere to the classical sequence practiced by presenting the pathology of the internal organs, because this work is not a textbook. Equally, how to comply with the exact chronology of these cases either will not. In my opinion, such a form of information feeding, despite a certain, seemingly mad, most convenient for perception.
And now it's time to turn to a brief review of the vegetative innervation of internal organs and lead the fundamental quotation on which the whole evidence base is based on this? Concept?.
Innervation of lungs and bronchi
The afferent paths from visceral pleura are the pulmonary branches of the thoracic premium of the sympathetic barrel, from the parietal pleura - nn. INTERCOSTALS N. Phrenicus, from bronchi - n. Vagus.
Efferent parasympathetic innervation
Protected fibers begin in the dorsal vegetative core of the wandering nerve and go in the latter and its pulmonary branches to Plexus Pulmonalis, as well as nodes located along the trachea, bronchi and inside the lungs. Postgangngling fibers are sent from these nodes to muscles and iron bronchial wood.
Function: The narrowing of the lumen of the bronchi and bronchiol and the separation of mucus; Expansion of vessels.
Efferent sympathetic innervation
Pregganionic fibers come out of the side horns of the spinal cord of the upper chest segments (TH2-TH6) and pass through the corresponding Rami CommunicaNTES ALBI and the border trunk to the star and the upper chest nodes. From the latter, postganglyonary fibers begins, which pass in the composition of pulmonary plexus to bronchial muscles and blood vessels.
Function: Expansion of the Bronchi Light. Narrowing and sometimes extension of vessels "(50).
And now, in order to understand why a spear breaks, it is necessary to submit the following situation.
Suppose that there was a violation in the thoracic spine, at the level of TH2-TH6 (breast segments of the spinal column): there was a physiological unit or, in other words, a banal vertebral displacement occurred (for example, due to injury), which led to squeezing soft tissues, and, In particular, the spinal ganglia or nerve. And as we remember, the consequence of this will be a violation of bio electric current, in this case, to bronchoms; Moreover, it will be excluded (or decrease) the effect of pretty vegetative innervation, which expands the lumen of the bronchi. It means that the predominant will be the effect of the parasympathetic part of the autonomic nervous system, and its function is the narrowing of the lumen of the bronchi. That is, the lack of influence of efferent sympathetic innervation, expanding the bronchial muscles, will lead to the prevailing effect of the parasympathetic vegetative innervation of bronchi, the consequence of which there will be their narrowing. That is, the spasm of bronchi will arise.
If the electric current is violated to bronchms, electric (ie, electromagnetic) will arise there, which means energy, imbalance. Or, in other words, asymmetry, in the tensions of sympathetic and parasympathetic innervation, or, in other words, a value other than zero.
After the discharge of the motor segment of the spine, the bioelectric current is restored to the bronchi from the side of the sympathetic nervous system, and this will mean that bronchi will start expanding. And the balance of sympathetic and parasympathetic vegetative innervation, in particular, bronchi will be restored.
Violation of the energy balance, I think you can simulate on the computer or measure the experienced way.
During the practice, as a manual therapist, I had no one case when I managed to stop the bouts of bronchial asthma and suppress the cough reflex in patients, breathing the thoracic department of their spine. Moreover, always quickly and all.
Once I had to work with a patient (a woman of 40 years old), which at the 10th age fell into the hole. Saved her native father, but since then she had a constant shaking, and she consisted of dispensary taking into account chronic bronchitis. However, she turned to me quite differently - in connection with the arterial hypertension. And I, as usual, worked with the spine. But what was the surprise of this woman (and mine, of course), when she noted the lack of passing and, the fact that it became easier for her to breathe ("silent with complete breasts"). Blocking in the motor segment of the spinal column was preserved thirty years, and left for the week.
Four the following quotes are not better illustrated by the possibilities and nervous system, in particular, the body, in general, and, most importantly, manual therapy.
1. The purpose of manipulative treatment is the restoration of the joint function in those places where it is inhibited (blocked). "
2. "After successful manipulation of the mobility of the segment, as a rule, is restored immediately."
3. "Manipulations cause muscle hypotension and connective tissueAt the same time, patients experience a sense of relief and at the same time a feeling of heat. All this happens instantly. "
4. And, "that the power of relaxed muscles after manipulation can increase instantly" (51).
Although the authors of the above-mentioned sayings attributed them only to the engine segment, and, it should be thought, no way to what it was said in this work, I, nevertheless, I take the courage to argue what I say. On the direct connection of displacements or sublifting in the motor segment of the spinal column and the occurrence of diseases of the internal organs. The consequence of displacements is the appearance of functional blocks in the compromised areas of the spine, which leads, in turn, to multi-level combinations of displacements throughout the spine, on which the pathogenesis of all human diseases, and animals, too. And the quotes given only confirm the effectiveness this method Treatment and, indirectly, all my conclusions. From his experience of treating internal pathology with the help of manipulations from the arsenal of manual therapy, I can accurately confirm the direct connection of changes in the internal organs with blocks in the spinal column, and the speed of the effect when the spine segments is released. The spasm of smooth muscles of bronchi and vessels is replaced by a dialing (expansion or stretching) almost instantly. For example, asthmatic status stops for 3 - 5 minutes, as well as reduced arterial pressure (If it was high), also occurs in about the same time limits (and some patients are faster).
Functional blocks in the motor segments of the human spinal column (and vertebrate animals, by the way, also), leading to degenerative changes in intervertebral discs due to chronic compression of the spinal ganglia and nerves, may not affect the conduct of bioelectric impulses from the CNS to the periphery to the authorities and back . And, it means that it is necessary to violate the work of the internal organs, which (violations) and will be a mirror reflection of the energy imbalance in the vegetative nervous system.
Pleurite exudative (post-trap)
In 1996, in the evening, the brother of my former classmate called me - I called the hospital. The buddy fell into a car accident, as a result of which he was covered between the steering wheel and the seat. And rib cage It was siled so that after it was extracted from the baked car, he could not breathe fully.
But the doctors did not immediately appeal, considering that the problem would leave on their own. However, it did not make it easier to breathe - moreover, the condition has deteriorated that it was still forced to turn to doctors.
He was hospitalized in the therapeutic department, where he was detected exudative pleurisy.
IN pleural cavity Exudate (serous fluid effusion) was accumulated, which was necessary to remove (pump out) in order to facilitate the work and directly light and hearts. To climb on foot without stopping on the third floor, he could no longer.
And it was for tomorrow that the so-called pleural puncture was planned.
In the same evening, when he called, I invited him to come home to me to decide and in his condition, and what he could help. And he came - barely barely, but came! And in the same evening I worked on his spine. After the first set of manipulations, Anatoly became easier to breathe, and the next day, as he then spoke, on the third floor of the hospital he was already raised quite easily, i.e. Without stops. And according to my recommendation, the next day, he refused to be pleural puncture, which was perplexed by doctors. And I worked with my back (spine) of the buddy after that, just twice. And more Anatoly in this regard did not have any problems.
Two cases of inflammation of lungs
One day a woman came to me on reception, from which I, while listening to her lungs, diagnosed pneumonia (inflammation of the lungs). In accordance with the requirements, she proposed hospitalization from which the patient refused; She refused and from those proposed for the treatment of antibiotics, motivating this by the fact that she had an allergy. The diagnosis of pneumonia was confirmed by radiographic pictures and laboratory studies.
Then I just started thinking about the impact of changes in the spinal column on the occurrence and course of internal pathology, and that, removing the blocks in the modified spine, can be influenced by the course of the disease, and its outcome. And to restore the problem vertebral pole at that time it was possible only with the help of manual therapy.
That is me and was offered to the patient - for which I received consent. At that time, I just started practicing as a manual therapist, I had to work with the patient five times within 10 days (later I worked no more than three times with each patient), with x-ray control after a half weeks - pneumonia was resolved. Without medicine! It was 1996.
Four years later, I had the opportunity to heal pneumonia, by correction of the spine. This time, a very young woman. And there is also no antibiotics, and again with x-ray control after the expiration of 10 days. Although, as you know - the doctor treats, but the nature is heal!
And only three complexes (sessions) of manipulations took everything about everything. In fairness, it is necessary to say that drugs that contribute to the elimination of the bronchi spasm, I still prescribed. But, nevertheless - 10 days against three weeks! It is for such a period (21 days) pneumonia is cured, in accordance with the classical foundations of therapy. Think away! The body cut to the fascia to the skin restores to the formation of the scar for 21 days. And the skin is a rather rude substance, unlike the epithelium of the bronchi.
So what can you explain all three cases? But what. I will start on the first time, and then in order.
Displaced vertebral injury violated bioelectric impulses not only to bronchoms, but also to interrochemical muscles. The latter circumstance and was the main start-up mechanism in the occurrence of traffic in the pleural cavity. Our chest functions like a blacksmithing fur - when inhaling, inside the thoracic cavity, it occurs, so to speak, blood and air, and air, and when exhaled, interrochel muscles, shrinking, squeeze out of light and air, and blood . In case of violation of excursions, Ryoeber on some one party arises, this is what situation. Blood to light is injected in full, but is expelled in a smaller one from the half (lungs), where the work of the interrochemical muscles will be broken. That is, where excursions (movement) Ryoebers will not be full (that is, not in full), there are conditions for the formation of the transfer of serous fluid, or in the pleural cavity, or in the parenchyma of the lungs. A classic school challenge with incinerating and pouring water into the pool through pipes with different diameters, and a question - after what time will the pool be filled with?
And as soon as the electrical pulses are restored to the interrochemical muscles, the chest begins to work as a pump (the old name of the pump), which makes it pretty quickly to drive out all the extra liquid from the pleural cavity, as in the case of anatoly, or from the parenchyma of the lungs, as the case spontaneously The ceased edema of the lungs, described by me in the second part, this concept.
P.S. Serous (serum, from lat. Serum - serum) or similar blood serum or liquid generated from it.
As for pneumonia, there is a fairly simple explanation.
The inner wall of the bronchi is wounded by the so-called fiscal epithelium, each cell of which has constantly cutting vehicles. In the first phase, it, shrinking, is almost parallel to the outer membrane of the cell, and in the second - returned to its original position, and thus progress the mucus (produced by glass-like cells located under the flicker epithelium) from the bronchus. (The movement of the Village reminds the wheat perforating in the wind). We, reflexively, this mucus, along with foreign particles (dust, expressing the bronchi epithelium) swallow. In the nasal cavity almost as well, with the only difference that the mucus is promoted in the nose in the nose, the mucus from the nostrils into the oral cavity from top to bottom. Here, by the way, why the situation occurs when the mucus arises when the mucus is produced too much (there is more liquid in it and it is less viscous than normal) and the villi do not cope with the increased volume of the qualitatively changed mucus, and it runs from the nose, as if water .
So what about pneumonia or the same bronchitis?
In the case of vertebrae offplaces in the chest department (TH2 - TH6), there is a violation of bioelectric impulses in the sympathetic part of the autonomic nervous system, which expands the lumen of the bronchi, which will be the prevalence of parasympathetic innervation. And this is the narrowing of the lumen of the bronchi and the excretion of the mucus, which cannot move up from the spasm.
And almost the ideal conditions are created for the vital activity of microorganisms (staphylococci, streptococcal, pneumococci, viruses). Many mucus (mixture of glycoproteins - complex proteins containing carbohydrate components), moisture, heat and no movement. That is why leukocytes and macrophages immediately rush here, which, destroying the rapidly growing colonies of microbes, are dying themselves, turning into a pus. But there is no way out - no - spasm is saved! And the inflammatory focus arises. And we, doctors, "we treat - treat, treat, we treat" ... Powerful antibiotics, millions of units (units) daily, and even for three weeks. And it is not always successful, alas.
And you know what the difference between pneumonia and bronchitis?
It depends only only on the level of lesion (spasm) bronchi. If the spasm occurred a little higher than the end bronchiol, then we will get - pneumonia. After the final bronchiol, only respiratory bronchiols are already on the walls of which there are alveoli through which gas exchange occurs. If the violation of the conduction of the bronchial tree occurs above, for example, in the bronchi of the eighth (lolly bronchi) of the order - we are banal bronchitis. It we treat only two weeks. And why? But because on these overlying levels, the resistant narrowing of the bronchi is allowed and easier and faster. If the defeat is even higher - please, here you are bronchial asthma! Of course, I exaggerate somewhat, but in general terms everything is exactly what happens.
Of course, in the treatment of doctors, drugs are used, the action of which is directed to the chemical blocking of the muscles of the bronchi, which eliminates the effect of parasympathetic innervation leading to the resistant narrowing of the lumen of the bronchi (with all the ensuing consequences). But since the shift in the spinal column is not eliminated, then when canceling medications - everything returns to the circles. That is, we are actually tritely waiting for the displacement in the thoracic spine (even without thinking about it!), And after it, and the predominant influence of the parasympathetic component of the autonomic nervous system leading to a spa in bronchi. Only and everything!
In the same way, you can approach the consideration of violations of the vegetative innervation of other bodies, which, in principle, should be done. And let's start, or rather, we continue, with the tasteless control of the hearts.
Afferent innervation. Interoceptive analyzer
The study of sources of sensitive innervation of internal organs and conducting interior trajectures has not only theoretical interest, but also of great practical importance. There are two interrelated targets that the sources of sensitive innervation of organs are being studied. The first of them is the knowledge of the structure of reflex mechanisms regulating the activities of each body. The second goal is the knowledge of conducting pain irritations, which is necessary to create scientifically based surgical methods of anesthesia. On the one hand, the pain is a signal about the disease of the organ. On the other hand, it can grow into a grave suffering and cause serious changes in the body's activities.
Interoceptive conductive pathways carry afferent impulses from receptors (inter -ceptors) of internally, vessels, smooth muscles, gland glands, etc. Pain in the internal organs may occur under the influence of various factors (stretching, compression, lack of oxygen, etc.)
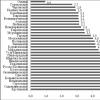
The inter -ceptive analyzer, like other analyzers, consists of three departments: peripheral, conductive and cortical (Fig.18).
The peripheral portion is represented by a variety of interoceptors (mechanical, baro-, thermo-, osmo-, chemoreceptors) - the nerve endings of dendrites of sensitive cells of cranial nerve nodes (V, IX, X), spinal and vegetative nodes.
Nervous cells of sensitive ganglia of cranial nerves are the first source of afferent innervation of internal organs. Peripheral processes (dendrites) of pseudo-monopolar cells are followed in the composition of the nerve trunks and branches of the triangistic, tongue-silica and wandering nerves to the internal organs of the head, neck, chest and abdominal cavity (stomach, duodenum gut, liver).
The second source of afferent innervation of internal organs is the spinal nodes containing the same sensitive pseudo-monopolar cells, as well as the cranial nerve nodes. It should be noted that the cerebrospinal nodes contain neurons both innervating skeletal muscles and skin and innervating insides and vessels. Consequently, in this sense, the spinal assemblies are somatic-vegetative formations.
Peripheral processes (dendrites) of neurons of cerebrospinal nodes from the spinal nerve barrel are moving in the composition of white connecting branches in a sympathetic barrel and pass transit through its nodes. The afferent fibers are followed by the branches of the sympathetic barrel, the hearty nerves, pulmonary, esophageal, gentle-in-law and other branches. To the internal organs of the abdominal cavity and the pelvis, the bulk of the afferent fibers takes place in the atrief nerves and further, passing the "transit" through the ganglia of vegetative plexuses, and in secondary plexuses reaches internal organs.
To the blood vessels of the limbs and walls of the body, afferent vascular fibers - peripheral processes of sensitive cells of the spinal assemblies - are held as part of the spinal nerves.
Thus, the afferent fibers for internal organs do not form independent trunks, but are held as part of vegetative nerves.
The heads of the head and vessels of the head are obtained by afferent innervation, mainly of the trigeminal and tongue nerve. In the innervation of the pharynx and the neck vessels takes part in its afferent fibers of the Language nerve. Internal organs of the neck, thoracic cavity and upper "floor" abdominal cavity have both vagus and spinal affreading innervation. Most of the internal organs of the abdomen and all the pelvis organs have only spinal sensitive innervation, i.e. Their receptors are formed by dendrites of the cells of the spinal nodes.
The central processes (axons) of pseudo-monopolar cells enter the composition of sensitive roots in the head and spinal cord.
The third source of the afferent innervation of some internal organs is the vegetative cells of the second type of doogle, located in intraigan and huggy plexuses. The dendrites of these cells form receptors in the internal organs, some of them achieve the dorsal and even brain (I.A. Buligin, A.G. Corotkov, N.Gorikov), following or in the composition of a wandering nerve or through sympathetic trunks in Rear roots of cerebrospinal nerves.
In the brain of the body of the second neurons are located in sensitive cortic nerve kernels (NUCl. Spinalis N. Trigemini, NUCl. Solitarius IX, X nerves).
In the spinal cord, interoceptive information is transmitted over several channels: according to the front and lateral spinal thalias, along the spinal cerebelling paths and on rear channels - thin and wedge-shaped beams. The participation of the cerebellum in the adaptation and trophic functions of the nervous system explains the existence of wide interoceptive paths following the cerebellum. Thus, the bodies of the second neurons are located in the spinal cord - in the cores of the rear horns and the intermediate zone, as well as in the thin and wedge-shaped cores of the oblong brain.
The axons of the second neurons are sent to the opposite direction and in the composition of the medial loop reach the Talamus nuclei, as well as the cores of the reticular formation and hypothalamus. Consequently, in the brain barrel, firstly, a concentrated beam of interoceptive conductors followed in the medial loop to the thalamus kernels (III NEON), and secondly, the divergentization of vegetative paths, heading for many reticular formation nuclei and to the hypothalamus occurs. These links ensure the coordination of the activities of numerous centers involved in the regulation of various vegetative functions.
Third neurons proceeds through the rear leg of the inner capsule and end on the cells of the cerebral cortex, where the disease is discussed. Usually these sensations are spilled in nature, do not have accurate localization. I.P. Pavlov explained this by the fact that the cortical representation of the inter -ceptor has a small life practice. So, patients with repeated attacks of pain associated with diseases of internal organs determine their localization and much more accurate than at the beginning of the disease.
In the core, vegetative functions are presented in motor, premotor zones. Information about the work of the hypothalamus enters the boring of the frontal share. The afferent signals from the respiratory and blood circulation organs - in the Coru is an island, from the abdominal organs - in post-central ulivan. The bark of the central part of the medial surface of the hemispheres of the brain (limbic fraction) is also part of the visceral analyzer, participating in the regulation of respiratory, digestive, urogenital systems, metabolic processes.
The afferent innervation of internal organs is not segmental. Internal organs and vessels are distinguished by the plurality of sensitive innervation paths, among them the majority are fibers originating from the nearest spinal cord segments. These are the main ways of innervation. The fibers of the same (neighboring) ways of innervation of internal organs pass from remote spinal cord segments.
A significant part of the pulses from the internal organs reaches the vegetative centers of the head and spinal cord through the afferent fibers of the somatic nervous system due to numerous bonds between the structures of the somatic and vegetative departments of a single nervous system. The afferent impulses from the internal organs and the movement apparatus can come to the same neuron, which, depending on the current situation, ensures that vegetative or animal functions are performed. The presence of bonds between the nerve elements of somatic and vegetative reflex arcs causes the appearance of reflected pain, which must be considered in the formulation of diagnosis and treatment. Thus, with cholecystitis there are dental pains and marked by a fracenik-symptom, with an aburiety of one kidney there is a delay in the separation of urine by another kidney. In case of diseases of the internal organs, skin zones have increased sensitivity - hyperesthesia (Zakharin-Ging zones). For example, during angina, the reflected pains are localized in the left hand, with a stomach ulcer - between the blades, with the damage to the pancreas - the stuffing pain on the left at the level of the lower ribs up to the spine, etc. Knowing the features of the structure of segmental reflex arcs, you can affect internal organs, inflicting irritations in the field of the corresponding skin segment. This is based on the needlerapy and the use of local physiotherapy.
Efferent innervation
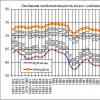
The efferent innervation of various internal organs is ambiguous. The organs that include smooth involuntary muscles, as well as organs possessing a secretory function, as a rule, obtain effectant innervation from both parts of the autonomic nervous system: sympathetic and parasympathetic, which have the opposite effect on the organ function.
The excitation of the sympathetic department of the vegetative nervous system causes the increase and enhancement of heartbreaks, an increase in blood pressure and blood glucose levels, an increase in the emission of the brain layer of the adrenal glands, the expansion of the pupils and the lumen of the bronchi, the decrease in the secretion of the glands (except sweat), the oppression of the intestinal peristaltics causes sphincter .
The excitation of the parasympathetic unit of the vegetative nervous system reduces blood pressure and blood glucose level (increases the secretion of insulin), replete and weakens the reduction of the heart, narrows pupils and lumen of the bronchi, increases the secretion of glands, enhances the peristaltics and reduces the muscles of the bladder, relaxes the sphincters.
Depending on the morphofunctional features of a particular organ in its efferent innervation, a sympathetic or parasympathetic component of the vegetative nervous system may prevail. Morphologically, this is manifested in the amount of relevant conductors in the structure and severity of the intrahane nervous apparatus. In particular, in the innervation of the bladder and the vagina, the decisive role belongs to the parasympathetic department, in the innervation of the liver - sympathetic.
Some bodies receive only sympathetic innervation, for example, pupil dlyatator, sweat and sebaceous glands Skin, hair muscles, spleen, and pupil sphincter and ciliac muscle -pasimpatic innervation. Only sympathetic innervation has the overwhelming majority of blood vessels. At the same time, an increase in the tone of the sympathetic nervous system, as a rule, causes a vasoconstrictor effect. However, there are organs (heart) in which the increase in the tone of the sympathetic nervous system is accompanied by a vasodilatory effect.
Domestic organs containing cross-striped muscles (language, pharynx, esophagus, larynx, straight intestine, urethra) get an efferent somatic innervation from motor core or spinal nerves.
Important for determining the sources of nervous supply of internal organs is knowledge of its origin, its displacements in the process of evolution and ontogenesis. Only from these positions will be understood innervation, for example, hearts from the cervical sympathetic nodes, and the sex glands from the aortic plexus.
A distinctive feature of the nervous apparatus of internal organs is the multi-segment of sources of its formation, the plurality of paths connecting the body with the central nervous system and the presence of local innervation centers. This can explain the impossibility of complete denervation of any internal organ surgically.
Efferent vegetative conducting ways to internal organs and double-line vessels. The bodies of the first neurons are located in the nuclei of the head and spinal cord. The bodies of the second - in vegetative nodes, where the pulse switching from the pregganionic fibers occurs.
Sources of the efferent vegetative innervation of internal organs
Head and Neck
Parasympathetic innervation. The first neurons: 1) the added and median kernel III pairs of cranial nerves; 2) upper salivary core VII pairs; 3) the lower salivatory core of the IX pair; 4) Dorsal core x pairs of cranial nerves.
Second neurons: rolling heads of head (eyelashes, stubble, lifterless, ear), intraganic nodes x pairs of nerves.
Sympathetic innervation. The first neurons are the intermediate bold spinal cord kernels (from 8, th 1-4).
The second neurons are the cervical nodes of the sympathetic barrel.
Breastfish organs
Parasympathetic innervation. The first neurons are a dorsal core of a wandering nerve (x pair).
Sympathetic innervation. The first neurons are the intermediate borders of the spinal cord (TH 1-6).
The second neurons are the lower cervical and 5-6 top nodes of the sympathetic barrel. Second neurons for the heart are located in all cervical and upper chest nodes.
Abdominal organs
Parasympathetic innervation. The first neurons are the dorsal core of the wandering nerve.
The second neurons are robust and intraongoral nodes. The exception is a sigmoid intestine that is innervated as the pelvis organs.
Sympathetic innervation. The first neurons are the intermediate bloc cores of the spinal cord (TH 6-12).
The second neurons are the nodes of the curly, aortic and lower mesenteric plexuses (II of the order). Chromofink brainstorm cells of adrenal glands are innervized by pregganionic fibers.
Oral bodies
Parasympathetic innervation. The first neurons are the intermediate cores of the sacred spinal cord (S 2-4).
The second neurons are robust and intraongoral nodes.
Sympathetic innervation. The first neurons are the intermediate bold spinal cords (L 1-3).
The second neurons are the lower mesenter node and the nodes of the upper and lower gradual plexuses (II of the order).
Innervation of blood vessels
The nervous apparatus of blood vessels is represented by interoceptors and perivascular plexuses that propagate along the vessel in its adventitiation or along the boundaries of the outer and middle shells.
Afferent (sensitive) innervation is carried out at the expense of nerve cells of the spinal assemblies and cranial nerve nodes.
The efferent innervation of blood vessels is carried out due to sympathetic fibers, and the arteries and arterioles are experiencing a vasoconstrictor effect continuously.
To the vessels of the limbs and the body, the sympathetic fibers go in the composition of the cerebrospinal nerves.
The bulk of the efferent sympathetic fibers to the vessels of the abdominal cavity and the pelvis takes place in the composition of the crank nerves. The irritation of the curled nerves causes the narrowing of blood vessels, the cut - a sharp extension of the vessels.
A number of researchers discovered veasaceous fibers that are part of some somatic and vegetative nerves. It is possible only the fibers of some of them (Chorda Tympani, NN. Splanchnici Pelvini) have a parasympathetic origin. The nature of most vasodinating fibers remains unclear.
T.A.grigoryeva (1954) substantiated the assumption that the vasodilator effect is achieved as a result of the reduction of non-annular, but longitudinally or space-oriented muscle fibers of the vascular wall. Thus, the same impulses, brought by sympathetic nerve fibers, cause a different effect - a vasoconstrictor or vasodilator, depending on the orientation of the smooth muscle cells themselves relative to the longitudinal axis of the vessel.
Another vasodilization mechanism is allowed: the relaxation of the smooth muscles of the vascular wall as a result of the occurrence of braking in vegetative neurons, innervating vessels.
Finally, it is impossible to exclude the expansion of the lumen of the vessels as a result of humoral influences, since humoral factors can organically enter the reflex arc, in particular, as its effector link.
Innervation of the eye. In response to certain visual irritations, which comes from the retina, the convergence and accommodation of the visual apparatus are carried out.
Eye convergence - the reduction of the visual axes of both eyes on the subject matter - occurs a reflexively combined abbreviation of cross-striated muscles
eye apple. This reflex required for binocular visionis associated with accommodation of the eye. Accommodation - the ability of the eye clearly see objects from him
at various distances, depends on the contraction of the muscles of the eye - M.Ciliaris and M.Sphincter Pupillae. Since the activity of musculature eyes is carried out in conjunction with
reduction of its cross-striped muscles, the vegetative innervation of the eye will be considered together with the animal innervation of its engine apparatus.
Afferent pathway from the muscles of the eyeball (proprioceptive sensitivity) are, according to some authors, the animal nerves themselves, innervating data
muscles (III, IV, VI cranial nerves), according to other data - N.ophthalamicus (N.Trigemini).
The innervation centers of the enemy apple muscles are kernel III, IV, and VI pairs. Efferent path - III, IV and VI cranial nerves. The convergence of the eye is carried out as indicated,
combined abbreviation of muscles of both eyes.
It should be borne in mind that there are no isolated movements of one eyeball at all. In any arbitrary and reflex movements, both of them are always involved.
eyes. This possibility of combined movement of eyeballs (gaze) is provided by a special system of fibers that connects the nuclei of III, IV and VI nerves and wearing
the name of the medial longitudinal beam.
The medial longitudinal beam begins on the kernel in the legs of the brain, connects to the nuclei of III, IV, VI nerves with the help of collaterals and heads through the brain barrel
down in the spinal cord, where it ends, apparently, in the cells of the front horns of the upper cervical segments. Thanks to this, the movement of the eye is combined with the movements of the head and
Innervation of smooth eye muscles - M.Sphincter Pupillae and M.Ciliaris occurs at the expense of the parasympathetic system, innervation M.Dilatator Pupillae - due to sympathetic.
The afferent paths of the vegetative system are N.oculomotorius and N.ophthalmicus.
Efferent parasympathetic innervation. Preggangional fibers come from the addition core of the eye nerve (Mesiencephalotic department
the parasympathetic nervous system) as part of N.oculomotorius and on its RADIX Oculomotoria reaches Ganglion Ciliare, where and ends. In the ciliary node begin
postgangngling fibers, which, through NN.Ciliares Breves, reach the ciliary muscles and sphincter pupil. Function: The narrowing of the pupil and accommodation of the eye to the long-distance and
close vision.
Efferent sympathetic innervation. Preggangional fibers go from the cells of substantia intermediolateralis lateral horns of the last cervical and two top
breast segments (CVIII - Thii Centrum Ciliospinal), over two top breast Rami CommunicaNTES ALBI, pass as part of the cervical sympathetic barrel and
complete in the upper cerval. Postganglionic fibers go in N.Caroticus Internus to the skull cavity and enter Plexus Caroticus Internus and Plexus Ophtalmicus
After that, part of the fibers penetrates the Ramus Communicans connecting with N.Nasociliaris, and Nervi Ciliares Longi, and the part is sent to the ciliary node through which
it passes without interrupting, in Nervi Ciliares Breves. Both those and other sympathetic fibers passing through long and short rash nerves are sent to the dilatator.
pupil. Function: Pushing the pupil, as well as the narrowing of the vascular eye.
Innervation of glands - tear and salivary. The afferent path for the lacrimal gland is N.Lacrimalis (branch N.ophthalmicus from N.Trigemini), for subband and
subject - N.Lingualis (N.MandiBularis branch from N.Trigemini) and Chorda Tympani (branch N.interMedius), for near-noise - N.Auriculotemporalis and N.Glossopharyngeus. Efferent
parasympathetic gear innervation. The center lies in the top department of the oblong brain and linked to the nucleus of the intermediate nerve (Nucleus Salivatorius Superior).
Preggangionary fibers are coming as part of N.interMedius Next N.petrosus Major to Ganglion Pterygopalatinum. Hence the postganglionary fibers, which are as part of
Efferent parasympathetic innervation of the lifting gland and sub-surround glands. Preggangionary fibers go from Nucleus Salivatorius Superior in the composition
Efferent parasympathetic innervation of the parish gland. Preggangionary fibers go from Nucleus Salivatorius Inferior in N.Glossopharyngeus, further
n.TYMPANICUS, N.PETROSUS MINOR TO GANGLION OTICUM. From here, postganglyonic fibers starting to the gland in N.Auriculotemporalis begin. Function: Strengthening Secretion
tear and mentioned salivary glands; Expansion of blood vessels.
Efferent sympathetic innervation of all named glands. Pregganionic fibers begin in the side horns of the upper breast spinal cord segments and
end in the upper cervical node of the sympathetic barrel. Postgangle's fibers begin in the node called and reach the lacrimal gland as part of Plexus Caroticus
iNTERNUS, to the parotone - as part of Plexus Caroticus Externus and to the subband and sub-surround glands - through Plexus Caroticus Externus and then through Plexus Facialis.
Function: delayed saliva separation (dry mouth); Toothing (not sharp effect).
Heart innervation. The afferent paths from the heart are coming as part of N.Vagus, as well as on average and lower cervical and chest heartless nurses. At the same time
sympathetic nerves are a feeling of pain, and on parasympathetic - all other afferent impulses.
Efferent parasympathetic innervation. Preggangionary fibers begin in the dorsal vegetative kernel of a wandering nerve and go in the latter, his
heart branches (Rami Cardiaci N.Vagi) and heart plexuses to the internal nodes of the heart, as well as the nodes of the necroserous hollow. Postgangle fibers come from these
knots to the muscle of the heart. Function: braking and oppression of heart activities; The narrowing of the coronary arteries.
Efferent sympathetic innervation. Preggangonary fibers begin from the side rogs of the spinal cord 4-5 of the upper chest segments, exit the composition
referred Rami Communicantes Albi and pass through the sympathetic barrel to five top chest and three cervical nodes. In these nodes begin postganglyonary
fibers that are as part of heart nerves, NN.Cardiaci Cervicales Superior, Medius et Inferior and NN.Cardiaci Thoracici, reach the heart muscle. Break is carried out
only in Ganglion Stellatum. Cardiac nerves contain in its composition preggling fibers, which are switched to postganglyonary in cardiac cells
plexus. Function: Strengthening the work of the heart (it was installed by I.P. Pavlov in 1888, calling the sympathetic nerve reinforcing) and the acceleration of the rhythm (for the first time I installed I.F.
1866 r.), Expansion of coronary vessels.
Innervation of lungs and bronchi. The afferent paths from the visceral pleura are the pulmonary branches of the thoracic presence of a sympathetic barrel, from parietal pleura -
nN. INTERCOSTALES AND N.PHRENICUS, from bronchi - N.Vagus.
Efferent parasympathetic innervation. Preggangionary fibers begin in the dorsal vegetative core of the wandering nerve and go in the latter and
its pulmonary branches to the Plexus Pulmonalis nodes, as well as nodes located along the trachea, bronchi and inside the lungs. Postgangle fibers are sent from these nodes
to the muscles and glands of the bronchial tree. Function: The narrowing of the lumen of the bronchi and bronchiol to the excretion of the mucus.
Efferent sympathetic innervation. Pregganionic fibers come out of the side horns of the spinal cord of the upper chest segments (THII - THVI) and pass through
relevant Rami Communicantes Albi and a sympathetic barrel to star and upper chest nodes. From the latter, postganglyonary fibers begin, which
pass in the composition of pulmonary plexus to bronchial muscles and blood vessels Function: expansion of the lumen of the bronchi; narrowing.
Innervation of the gastrointestinal tract (to the sigmoid intestine), pancreas, liver. The afferent paths from these bodies are coming as part of N.Vagus,
n.Splanchnicus Major et minor, Plexus Hepaticus, Plexus coeliacus, breast and lumbar spinal nerves and in N. phrenicus.
In sympathetic nerves, the feeling of pain from these organs is transmitted, according to N.Vagus - other afferent impulses, and from the stomach - a feeling of nausea and hunger.
Efferent parasympathetic innervation. Pregganionic fibers from the dorsal vegetative nucleus of a wandering nerve pass in the latter
terminal nodes in the thickness of these organs. In the intestine these are cells of intestinal plexuses (Plexus Myentericus, Submucosus). Postgangylionic fibers go
from these knots to smooth muscles and glands. Function: Strengthening the peristals of the stomach, relaxation of the sphincter of the gatekeeper, enhancing the peristaltics of the intestine and gallbladder,
expansion of vessels. In the composition of the wandering nerve there are fibers that excite and braking secretion.
Efferent sympathetic innervation. Preggangionary fibers come out of the side horns of the spinal cord V - XII breast segments, go through the relevant RAMI
communicantes Albi into a sympathetic barrel and further without a break in the NN.Splanchnici Majores (VI-IX) to intermediate nodes involved in the formation of the curl, top
and lower mesenter plexuses (Ganglia Coeliaca and Ganglion Mesenttericum Superius Et Inferius). From here there are postganglyonic fibers, coming as part of Plexus Coeliacus
and Plexus Mesenttericus Superior to the liver, Pancreas, to thin intestine and to the thick until the middle of Colon Transversum; Left half of Colon Transversum and Colon Descendens
innews from Plexus Mesenttericus Inferior. These plexuses supply muscles and glands of these organs.
Function: slowdown in the peristalsis of the stomach, intestine and gallbladder, the narrowing of the lumen of blood vessels and the oppression of the secretion of the glands.
To this, it should be noted that the delay in the movements of the stomach and intestines is also achieved by the fact that the sympathetic nerves cause active reduction in sphincters:
sphIncter pylori, intestinal sphincters, etc.
Innervation of the sigmoid and rectum and bladder. The afferent paths are coming as part of Plexus Mesenttericus Inferior, Plexus Hypogastricus Superior Et Inferior and in
composition NN.Splanchnici Pelvini.
Efferent parasympathetic innervation. Preggling fibers begin in the side horns of the spinal cord of II-IV sacral segments and extend in the composition
the corresponding front roots of the spinal nerves. Next, they go in the form of Nn. Splanchnici Pelvini to intraganic nodes of these colon departments and
narrow bladder nodes. In these nodes, postganglionary fibers begin, which reach the smooth muscles of these organs.
Function: excitation of the peristalsis of the sigmoid and rectum, relaxation M.Sphincter Ani Internus, reduction of M.Detrusor Vesicae and relaxation M.Sphincter
Efferent sympathetic innervation. Preggangional fibers go from side horns lumbar Department spinal cord through the appropriate front roots in
rami Communicantes Albi, pass without interrupting, through a sympathetic barrel and reach Ganglion Mesenttericum Inferius. Here begin postgangle fibers, going
as part of NN.Hypogastrici to the smooth muscles of these organs. Function: delay in the peristaltics of the sigmoid and rectum and the reduction of the internal sphincter
rectum.
In the bladder, sympathetic nerves cause m.detrusor vesicae relaxation and reducing the bladder sphincter. Innervation of genital organs sympathetic
and parasympathetic.
Innervation of blood vessels. The degree of innervation of arteries, capillaries and veins of Nativeinakov. Arteries who have more developed muscular elements in Tunica Media,
get more abundant innervation, veins are less abundant; V.Cava Inferior and v.Portae occupy an intermediate position.
Large vessels located inside the cavities of the body receive innervation from the branches of the sympathetic barrel, the immediate weaving of the vegetative nervous system and
adjacent spinal nerves; The peripheral vessels of the walls of the cavities and the vessels of the limbs receive innervation from the nerves passing nearby. Nerves,
suitable to vessels, go segmentally and form perivascular plexuses, from which fibers penetrate into the wall and distributing in Adventilation (Tunica
externa) and between the last and Tunica Media. The fibers innervate the muscular formation of the wall, having a different end form. Currently proved availability
receptors in all blood and lymphatic vessels.
The first neuron of the afferent path of the vascular system lies in the cerebrospinal nodes or nodes of vegetative nerves (NN.Splanchnici, N.Vagus); Next he goes in the composition
conductor interoceptive analyzer. Vasomotor center lies in oblong brain. The relationship of blood circulation is related to Globus Pallidus, Talamus, and
also gray hill. The highest centers of blood circulation, like all the vegetative functions, are elected in the cortex of the brain motor zone (frontal share), as well as ahead and rear
her. Cork end of the analyzer vascular functions It seems to be in all bark departments. Downlink brain bonds with stem and spinal
the centers are carried out, apparently, pyramid and extrapyramidal paths.
The closure of the reflex arc can occur at all levels of the central nervous system, as well as in nodes of vegetative plexuses (own vegetative
reflex arc).
The efferent path causes a vasomotor effect - expansion or narrowing of vessels. Vaconishing fibers are held in the composition of sympathetic nerves,
the vessels of the fibers go in all parasympathetic nerves of the cranial department of the vegetative nervous system (III, VII, IX, X), as part of the front roots
the spinal nerves (not recognized by all) and the parasympathetic nerves of the sacred department (NN.Splanchnici Pelvini).