ICD code 10 bladder disease. Bladder Cancer - An Overview of Information. How long do patients live
Oncological lesions of internal organs have recently been experiencing a tendency towards rejuvenation. They are often diagnosed at a fairly young age. Very often, patients under the age of 50 hear a terrible diagnosis - cancer. Bladder... According to the data provided by medical statistics, this dangerous oncological process affecting the genitourinary system of people has become diagnosed 4 times more often over the past decade.
In the urinary system, the development of the process of malignancy occurs much more often than in other structural elements of the body. This is due to its direct functioning. Thus, a tumor of the bladder is in 11th place among all malignant neoplasms of the human body. Experts have a simple explanation for this - caustic urine, containing a large amount of carcinogens excreted by the kidneys, passes through this organ.
Bladder cancer
The pathological mechanism of their effect on the mucous membrane of the main urinary organ is as follows:
- an aggressive liquid containing a large amount of carcinogens, after it enters the bladder, lingers in it for a fairly long time, from 20 minutes to several hours, depending on the frequency of a person's urge to urinate;
- urine, which has pronounced caustic properties, has a corrosive effect on the mucous membrane, which provokes the development of a mutation process in its cellular structures, which is expressed in their accelerated growth;
- the result of increased division of epithelial cells is the development of papilloma on the walls of the bladder, which is initially benign;
- further prolonged exposure to an aggressive liquid leads to increased cell division and the acquisition by this process of a pronounced atypia.
Malignancy of the epithelial layer of the main organ of the urinary system proceeds very quickly, and at the moment when the patient goes to the doctor, 90% of the neoplasms identified in the bladder are malignant. This tendency to rapid mutation makes the disease very dangerous, but due to the fact that it has a fairly pronounced symptomatology, the pathological process can be detected on early stages and promptly take emergency measures to stop it.
Important! A cancerous tumor that develops in the bladder has an increased tendency to invasion (germination into neighboring organs) and distant metastasis, therefore, requires timely and adequate treatment. Otherwise, the pathological process can quickly lead to death.
Classification
In mkb 10, the most recent international classification diseases of the tenth revision, there are several types of cancers of the bladder. First of all, they are differentiated by histological criteria. All types of oncological tumors, the distinguishing feature of which is the tissue structure, are detected only after examination under a microscope taken during diagnostic measures.
Based on the cellular structure, which has the main organ of the urinary system, the tumor in the bladder is divided by leading oncologists into the following histological types:
- () type of tumor structure. The most common type of malignant neoplasm affecting the human genitourinary system. Its detection occurs in 90% of cases. A feature of this type of tumor is its papillary growth, and the absence of a tendency to grow into the deep layers of muscle tissue or other internal organs.
- ... It usually occurs against the background of cystitis, which has chronic course... The process of atypia in this case affects the flat cells of the superficial epithelial layer of the main urine of the excretory organ. The tendency of malignant structures to germination and metastasis is noted.
- ... It is rare and has rather unfavorable prognosis. The tumor structure of this is localized in the muscular layer of the urinary organ, prone to rapid growth and the germination of metastases to neighboring organs at the earliest stages of development.
- ... It is formed from the connective tissue of the urinary organ due to prolonged exposure to carcinogenic substances contained in the urine. It is characterized by high malignancy, a tendency to early metastasis and frequent relapses.
- Carcinosarcoma. The rarest (0.11% among all bladder oncologies) type of malignant tumor, characterized by obvious heterogeneity, that is, the heterogeneity of the cellular structure and structure. In such a neoplasm, the sarcomatoid and urothelial components are always present simultaneously. The disease has a very high aggressiveness and an unfavorable prognosis for life.
In addition to the so-called histological subdivision of bladder cancer, leading oncologists also take into account the degree of tumor growth into the wall of the urinary organ. on this basis, it provides for its subdivision into th (the neoplasm is deployed exclusively in the upper layer of the bladder and usually has a thin stem) and (the tumor almost completely invades the wall of the bladder and begins to destroy its muscle layer).
Bladder cancer stages
In addition to revealing the histological structure of bladder cancer, the place of its localization and the degree of damage by the process of destruction of the urinary organ, specialists need to know at what stage of development the malignant process is in order to properly prescribe treatment. , as well as other organs and systems of the human body, passes through several stages in its development. Each of them has a direct relationship with the degree of tumor invasion of the walls of the bladder and the presence in the lymph nodes and nearby or distant internal organs metastases.
Leading oncologists distinguish 4 stages in the development of the disease:
- The tumor process at stage 1 affects only the upper, mucous layer of the urinary organ. The germination of abnormal structures into its wall does not occur at this stage. Also, this stage is not characterized by the earliest appearing metastases in the regional lymph nodes.
- Stage 2 bladder cancer is characterized by invasion up to the muscle layer. The favorableness of the prognosis of the disease depends on how much he was affected. In the case when the oncological process extends only to its inner layer (substage 2A), a person's chances of life increase, since the risk of abnormal cells growing into regional lymph nodes is minimal. The germination of a malignant neoplasm into the outer layers of muscle tissue is indicated by specialists with the symbol 2B, the presence of which in the patient's medical history indicates the need for more serious therapy.
- Stage 3 bladder cancer indicates tumor growth in soft tissue located in the immediate vicinity of the bladder. Also, the peritoneum, the walls of the small pelvis, and, are affected by secondary malignant foci. Cancer at this stage usually has pronounced symptoms and poses a serious threat to the patient's life.
- At stage 4 of cancer, urinary formation significantly increases in size and grows not only in the nearby organs of the small pelvis, but also in, and. This stage in the course of the pathological condition is considered the most difficult, since at this stage it is impossible to carry out a radical surgical intervention, and the life period is reduced to several months or even weeks.
To clarify the diagnosis, the following measures are used:
- General urine analysis. With its help, the specialist confirms the presence in it hidden blood and can also detect the presence of infectious agents. Such a study is prescribed first. It helps to minimize the causes of internal bleeding.
- Cytological test for bladder cancer. For this analysis, a centrifuge is used, through which urine is driven, and then the resulting residue is examined under a microscope. If a specialist histologist finds (atypical cells) in it, he most likely assumes the presence of a malignant process in the human genitourinary system.
- Ultrasound of the kidneys and bladder gives the diagnostician the opportunity to detect the presence of oncological tumor. In addition, with the help of this diagnostic study, pathological conditions of the urinary system with similar symptoms are detected.
- CT and MRI. These types of diagnostics allow you to get a clearer picture of pathological changes than ultrasound.
After the diagnostic results have confirmed the alleged diagnosis, the leading oncologist will select the appropriate one for the specific situation.
Important! Only thanks to timely and correctly conducted diagnostic tests, doctors have the opportunity to prescribe adequate therapy that helps to prolong a person's life and alleviate severe symptoms associated with the disease.
Informative video
Bladder cancer treatment
Currently, in the therapy of this type of malignant process, the same techniques are used as in general to eliminate abnormal cell structures. But they have a narrower specialization, which makes it possible to more effectively act on oncological tumors with such localization.
Treatment of bladder cancer is carried out through the combined effects of the following therapeutic measures:
- ... In this case, removal of bladder cancer can be performed as after opening abdominal cavity, and without it. In the latter case, the introduction of surgical instruments is performed by a catheter inserted into the opening of the urethra. For medical reasons, a radical operation can also be used. In bladder cancer, it is prescribed in the case when the tumor is very large and for its removal it is necessary to completely cut out the urine reservoir. But this type of surgery has a significant disadvantage - it increases the risk of kidney disease.
- ... It is used at all stages of the development of the disease to destroy abnormal cellular structures. Also, anticancer drug treatment is used as preventive measures, allowing you to avoid relapses of the disease.
- ... The best effect is obtained when this therapeutic technique is used in conjunction with chemistry. But for medical reasons, it can be prescribed separately.
- (BCG vaccine, introduced for the prevention of recurrence of oncological tumors inside the damaged organ). Applied as additional method that increases human immunity. BCG for bladder cancer is included in the treatment protocol when there is a high risk of recurrence of the disease.
In the event that surgical intervention is impossible for medical reasons or the cancer patient refuses to perform the operation, the leading oncologists recommend treatment methods such as ionizing, radiation, radiation and chemistry. They can be used both isolated from each other and together.
Important! Any therapeutic technique will be effective only in cases where the pathological condition is detected on initial stages... With early access to a doctor and adequate performance of all prescribed by him treatment measures a cancer tumor localized in the urinary organ can be defeated and a long-term remission is achieved. In the case of the development of extensive metastasis or if the patient refuses radical surgery, his chances for further life become minimal.
Nutrition and alternative treatment as adjunctive therapy
In order to enhance the therapeutic effect traditional medicine, experts recommend to additionally apply phytotherapy. For him apply herbal preparations that help to destroy abnormal cellular structures and have a restorative effect. Auxiliary includes the reception of decoctions and infusions from such medicinal plants, which simultaneously have antitumor and diuretic properties (birch or lingonberry leaf, knotweed, bearberry).
Nutritional correction also plays an important role in bladder cancer. A correct diet enhances the effect of medication and promotes a speedy recovery. The diet for cancer patients with a cancer in the bladder is selected by a specialist, taking into account that in daily menu the patient included all the necessary trace elements and vitamins. The basis for this disease should be fresh vegetables and fruits containing a large amount of vegetable fiber.
Metastases and relapse in bladder cancer
Late diagnosis of bladder cancer increases the risk of tumor metastasis to other organs. Unfortunately, they are detected in about half of cancer patients with a tumor structure that has spread into the muscle layer of the bladder. Even those patients who underwent radical cystectomy are not immune from their appearance. Most often, not only regional lymph nodes, but also the liver, lungs and bone structures are exposed to the germination of abnormal cells. The presence of metastases in the human body always provokes a relapse of bladder cancer.
In addition to this, the following factors contribute to the recurrence of the disease:
- lack of therapeutic measures for the elimination of primary carcinoma;
- high degree of malignancy of the cancerous structure;
- large size of the neoplasm;
- late identification.
In the event of a relapse, the most important indicator is the time of development of the secondary tumor. The earlier the daughter neoplasm appeared, the higher the degree of aggressiveness it has. The most dangerous is the onset of a relapse of the disease in the first six months after the therapy.
Complications and consequences of treatment
If the development of this type of disease is ignored by the patient, it, as soon as possible, like any other oncology, goes into an advanced stage, which is fraught with the occurrence of some complications. Usually in the later stages, in addition to the appearance of extensive metastases in nearby and distant organs, people have pronounced problems with urination, a general deterioration in well-being due to intoxication of the body with tumor decay products, renal failure and death. Bladder cancer has such consequences in the absence of adequate treatment, but experts also note the occurrence of some complications after radical treatment.
The most common of them are:
- Macrohematuria (the presence of bloody inclusions in the urine).
- Impotence. It can occur quite often, despite the preservation of the nerve endings of the cavernous bodies during radical cystectomy.
- Renal failure and obstruction urinary tract.
These complications violate the quality of human life, but they can be effectively eliminated thanks to innovative methods of therapy, therefore, in no case, for fear of their occurrence, one should not abandon the treatment protocol proposed by a specialist. Only a timely and adequately carried out therapeutic intervention can save a person's life.
How long do patients live?
Life expectancy in bladder cancer is directly influenced by the degree of malignancy of the tumor and the stage of its development.
The smaller they are, the more favorable the outcome of the treatment:
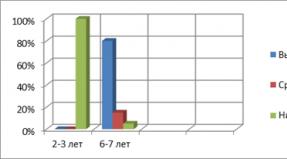
- at the initial stage of the development of the pathological condition, a five-year survival rate is observed in 90% of patients, and a ten-year or more in 80%;
- at the second stage, half of cancer patients survive up to 5 years, and 35% of patients overcome the 10-year mark;
- the third stage gives a chance to live 5 years or more for 30% of patients;
- the last stage of the disease is predicted to be practically hopeless. There are no data on ten-year survival at this stage of the disease, and only 10% of cancer patients reach 5 years.
From these statistics, it follows that bladder cancer has a more favorable prognosis only if its detection and subsequent adequate treatment were timely.
Prevention of bladder cancer
The best way to help prevent the development of bladder cancer is to prevent the aggressive effects of carcinogens on the body.
Considering all possible risk factors for the development of bladder oncology, in order to avoid the onset of the disease, it is necessary:
- treat any urological diseases in a timely manner, that is, seek medical help when the very first signs of an illness appear;
- to strengthen the drinking regime, since the liquid dilutes the carcinogens contained in the urine and promotes their rapid elimination from the body;
- regularly undergo preventive examinations, and in case of alarming symptoms, immediately consult a doctor for advice;
- start timely treatment of any pathological changes in the genitourinary system and, if possible, undergo endoscopic control;
- at the first urge to urinate, visit the toilet, and not overexpose aggressive fluid in the bladder; 6. adequately relate to the observance of safety measures when working in hazardous industries;
- give up such an addiction as smoking.
Only the right prevention of bladder cancer can prevent the development of a life-threatening disease, even in those people who are at risk. An attentive attitude to one's health helps to avoid the occurrence of not only malignant processes, but also any other pathological changes in the body.
Informative video
Malignant formation that occurs in the bladder mainly affects older people - most patients are from 40 to 60 years old. In this case, the ICD code 10 bladder cancer is considered a very common pathology. The male part of the population is more susceptible to it than the female.
International classification of diseases 10 views implies not only cancers in the bladder, but also in the kidneys and ureter, as well as in unspecified organs, due to the complication of the diagnosis. The oncological process in the bladder develops against the background of epithelial, tissue and muscle changes. On the basis of this, the types of tumors also depend. Today, medicine distinguishes the following types of malignant tumors in this organ:
- cancer itself;
- myxosarcoma;
- reticulosarcoma;
- fibrosarcoma;
- myosarcoma.
Depending on its origin, the tumor can develop very quickly, penetrating into the pelvic organs, or vice versa - slowly spreading through the tissues of the bladder, which is why it is very problematic to identify such a process in the early stages. Rapid infiltration is accompanied by damage to adjacent tissues and lymph nodes. Against this background, the patient's condition deteriorates very quickly. The spread of the malignant process to other organs occurs in the late stages of cancer development.
Metastases are mainly observed due to the entry of cancer cells into the lymph nodes and blood, due to which they are spread throughout the body.
According to our observations, they are localized in the liver, spinal cord and lungs. The circulatory system is also affected.
To avoid serious problems, given the complexity of this disease, it is strongly recommended to visit a doctor regularly and undergo appropriate diagnostic tests. It is also very important to pay attention to the symptoms that arise, since bladder cancer is quite pronounced.
The main symptoms of this ailment include:
- a constant increase in body temperature to subfebrile values or higher;
- the appearance of a persistent pain syndrome in the groin, scrotum, sacrum, which radiates to the lower back and even legs;
- signs of general intoxication of the body - increased sweating, pallor of the skin, headaches. There is also severe fatigue and weakness, which is why the patient cannot do basic things. Appetite disappears, and against this background, rapid weight loss occurs (one of the main symptoms of any type of cancer);
- problems with the function of urination - a feeling of incomplete emptying of the bladder, pain during urination, increased urge (both day and night) or vice versa -. In most cases, foreign impurities appear in the urine, mainly blood.
If you experience any of the above symptoms, you should immediately consult a doctor.
Bladder cancer ICD 10 usually occurs with prolonged exposure to certain risk factors, namely:
- poisoning with carcinogenic substances - chemical and biological substances of various origins, genetically modified food, industrial carcinogens that enter the body in hazardous production, radioactive substances, tobacco, etc.;
- heredity - it is known that the risk of getting cancer is much higher if someone in the family already had problems with malignant processes;
- congenital anomalies - cancer can develop against the background of problems with organs, tissues and cells present from the moment of birth. These patients are initially at increased risk;
- uncontrolled use of hormonal drugs, which can disrupt a number of physiological processes in the body;
- chronic infections and other diseases of the genitourinary system;
- sexually transmitted diseases of the reproductive system.
A large role is also played by diseases called precancerous. In almost half of the cases, they are manipulated, that is, they are reborn into malignant formations. The most common ailments of this type are considered to be prostate adenoma, endometriosis of the uterus, leukoplakia, papilloma.
Benign lesions, such as the aforementioned papilloma or cyst, are rightly considered to be the harbingers of manglization. That is why even such tumors should be removed without fail. This is due to the fact that the process of growth of new cells is disrupted in benign neoplasms. The number of mutated cells is becoming more and more, and this is a direct path to oncology.
With the help of modern medicine, it is possible not only to quickly diagnose this problem, but also to effectively cope with it. At the moment, they resort to three main diagnostic methods that give a 100% correct research result:
- Ultrasound - ultrasound will help identify any problems present in the genitourinary system, regardless of their etymology. The tumor, like other, less noticeable pathological processes, will be examined in detail by an experienced ultrasound doctor. All further methods are aimed at assessing the degree of risk and stage of development of the disease, since this is very important for the appointment of adequate treatment.
- Cystoscopy is an invasive research method, which consists in introducing a special instrument into the urethra to study the state of the bladder. At the end of the hose inserted into the urethra there is a small chamber, so that the doctor can see with his own eyes what is happening in this organ. Cystoscopy is a very popular method, it is constantly evolving, and every year it becomes safer and, importantly, less painful and unpleasant.
- A biopsy is a method of taking tissue directly from the affected organ for further sending the sample for histological examination. A biopsy in this case is needed in order to determine the type of tumor. This applies not only to its type, but also to its etymology. It is likely that we are talking about a benign neoplasm. If this is not the case, then the biopsy is guaranteed to confirm the malignancy of this process.
Unlike benign tumors, malignant tumors can only be treated with surgery. The operation consists in the complete removal of the affected organ, as well as nearby tissues, depending on whether there are metastases. Particular attention is also paid to the age of the patient.
Nevertheless, surgery in many cases is only part of the therapy that a cancer patient will need to undergo. Before the surgeon resects the affected bladder, the patient may be given radiation or chemotherapy. This is in order to try to shrink the tumor by destroying cancer cells. Chemotherapy consists of a course of treatment with special medications.
As for radiation therapy, in this case, radioactive irradiation of the place where the tumor is located is used. Both procedures are difficult and time-consuming, in addition, they cause serious damage. the human body and hair loss is just one of the most minor side effects... But to avoid this, if, of course, the patient wants to live, it is unlikely that it will be possible.
Treatment for bladder cancer continues after surgery. It is very important to achieve complete suppression of all cancer cells that were not removed from the body along with the affected organ, because this almost always leads to a relapse. For this, the patient is assigned additional sessions of radiation therapy, as well as cytostatic drugs.
If the cancer was not detected at a later stage of its development, and also if the operation was successful, then the prognosis for most patients will be favorable. This also applies to their preservation of their ability to work.
Among the total malignant tumors bladder cancer is diagnosed in about 2-4% of cases. In men, this disease is ranked 5th in terms of the frequency of diagnosis; in women, the symptoms of this disease are almost two times less common. It can also be noted that this diagnosis of oncology is made more often to residents of civilized countries. The patients' age is more than 65-70 years.
What is bladder cancer and risk factors
 Bladder cancer (code Mkb10 - C67) is a malignant invasion of the bladder wall or mucous membrane. Often the incidence of bladder cancer is associated with smoking, and this is also confirmed by the fact that those who smoke suffer from this type of cancer 6 times more often. In addition, some biological and chemical carcinogens influence the formation of this cancer. With prolonged contact with chemicals (benzene, aniline, etc.), there is also an effect on the body, subsequently which may develop oncology of the bladder. This disease is highly susceptible to workers in the chemical industry, dry cleaners, hairdressers, etc.
Bladder cancer (code Mkb10 - C67) is a malignant invasion of the bladder wall or mucous membrane. Often the incidence of bladder cancer is associated with smoking, and this is also confirmed by the fact that those who smoke suffer from this type of cancer 6 times more often. In addition, some biological and chemical carcinogens influence the formation of this cancer. With prolonged contact with chemicals (benzene, aniline, etc.), there is also an effect on the body, subsequently which may develop oncology of the bladder. This disease is highly susceptible to workers in the chemical industry, dry cleaners, hairdressers, etc.
Another risk factor is the transfer of a radiotherapy method for treating another disease in the pelvic area (oncology of the uterus or ovaries). The risk of developing this cancer is also increased if the patient has undergone chemotherapy with cyclophosphamide.
The use of highly chlorinated drinking water can also have an impact on the onset of oncology.
The question of a hereditary predisposition to this disease has no good reason, since the presence of relatives with this type of cancer does not increase the likelihood of getting this disease.
There is no definite answer as to the causes of bladder oncology.
Leading clinics in Israel
Types of the disease and its stages
Taking into account what cells are in the malignant formation, the blastoma of the bladder can be divided into types:
- Transitional cell (Cr - carcinoma). This type belongs to the most common type of bladder tumor - it is diagnosed in 90% of cases;
- Squamous. It is less common than the previous type (in 3% of cases), its appearance is caused by the presence of cystitis (chronic inflammation).
Even more rare types of cancer of this organ are lymphoma, adenocarcinoma, papilloma, sarcoma.
 Cancers in the bladder differ in histology, the nature of growth, the degree of differentiation, and the tendency to develop metastases.
Cancers in the bladder differ in histology, the nature of growth, the degree of differentiation, and the tendency to develop metastases.
By the degree of cell anaplasia, such cancers can be classified into poorly differentiated (G3), moderately differentiated (G2) and highly differentiated (G1) types.
It has great importance the degree of involvement in the tumor process of different layers of the bladder. Depending on this, a distinction is made between low-stage superficial bladder cancer and high-stage invasive cancer.
A cancerous tumor can also be:
- Papillary;
- Flat;
- Infiltrative;
- Intraepithelial;
- Uzelkova;
- Mixed character.
Given the stages in the development of cancer, the following stages can be distinguished:
- Stage 0. At this stage, tumor cells in the bladder are detected, but they do not spread to the walls of this organ, the so-called dysplasia is a precancerous condition. Therapy at stage 0 leads to a complete cure of the disease. This stage is subdivided into two substages - 0a and 0is. Stage 0a presents as the presence of non-invasive papillary carcinoma. The growth of this tumor proceeds to the zone of the lumen of the bladder, but this tumor does not grow to the walls of the organ and does not spread to the lymph nodes. Stage 0is is called the stage of carcinoma "in situ", when the tumor does not grow into the lumen of the bladder, beyond the boundaries of its walls and into the lymph nodes;
- Stage 1 (degree) is characterized by the spread of the tumor into the deep layers of the walls of the bladder, but does not reach the muscle layer. Treatment at this stage can also lead to complete elimination of the disease;
- Stage 2. At this moment of the disease, the tumor spreads in the muscular layer of the organ, but without full germination into it. With timely treatment started, the chances of cure are 63-83%;
- Stage 3 indicates that the neoplasm has invaded the organ wall and reached the adipose tissue around the bladder. At this stage of the cancer process, it can spread to the seminal vesicles (in men) and to the uterus or vagina (in women). The tumor has not yet spread to the lymph nodes. Treatment at 3 stages of the disease gives a chance of cure of about 17-53%;
- The last, 4th stage (degree). At this stage, the disease develops very quickly and complete cure unlikely, since the tumor has already spread to the lymph nodes, metastases appear.
Considering the international TNM system, the following stages of bladder oncology can be distinguished:

For example, a diagnosis of T1n0m0 means the initial stage of cancer with no metastases in both adjacent lymph nodes and distant ones.
Cancer symptoms
In the early stages, manifestations of oncology of the bladder can be the release of blood clots (spots) in the urine - microhematuria or macrohematuria. This can be expressed in a slight change in the color of urine (it turns a little pink) or blood clots may be contained in the urine, and its color turns red. Against the background of hematuria, the hemoglobin level falls and anemia appears.
You may also feel pain when urinating, the process itself becomes painful and difficult. There may be pain in the groin, perineum, sacrum. In the initial stages, pain can be felt only when the bladder is full, later it becomes constant.
With the growth of the tumor, squeezing of the ureter can occur, and this leads to a violation of the outflow of urine. In this regard, hydronephrosis occurs, there may be pain like renal colic. If both mouths are compressed, then renal failure occurs, ending with uremia.
If cancer grows into the rectum or vagina, it can lead to the formation of vesico-rectal (vaginal) fistulas with corresponding symptoms. If metastases appear, then lymphatic edema may form in the area lower limbs and the scrotum.
Many of the first signs of a tumor in the bladder are not characteristic symptoms of this disease and are similar to the symptoms of other urological diseases - prostatitis, cystitis, urolithiasis, prostate adenoma, kidney disease, for example, fever, lack of appetite. This is fraught with misdiagnosis, untimely appointment correct treatment, which worsens the prognosis of the disease.
Diagnosis of the disease
To make a diagnosis, a comprehensive examination is required. Sometimes this kind of neoplasm can be palpated with gynecological examination (in women) and with rectal examination (in men).
Standard techniques that are prescribed for suspected bladder cancer are:

A blood test is also used to check for anemia, which indicates the presence of bleeding.
A transabdominal ultrasound of the bladder should be performed, which can reveal tumors larger than 0.5 cm, localized in the areas of the lateral bladder walls. Conduct MRI studies to examine the bladder and pelvic organs. To detect cancer that is located in the cervical area, transrectal scanning is used. Sometimes tranurethral endoluminal echography is used.
Mandatory research in oncology of the bladder is the cystoscopy method (to clarify the size, location and appearance tumor) and biopsy.
From radiation diagnostics, cystography and excretory urography are performed, which make it possible to judge the nature of the tumor. If there is a likelihood of involvement of the pelvic veins and lymph nodes in the tumor process, pelvic venography and lymphangioadenography are performed.
Want to get a quote for your treatment?
* Only on condition that data on the patient's illness is received, a representative of the clinic will be able to calculate an accurate estimate for the treatment.
Bladder tumor treatment
If the patient is diagnosed with superficially growing cancer, it is possible to use transurethral resection (TUR). At stages 1-2, TUR is a radical remedy, with a widespread process - at stage 3, this type of treatment is carried out with a palliative purpose. In the course of this method of treatment, the tumor is removed using a resectoscope through the urethra. Then a course of chemotherapy is prescribed.
Open cystoectomy is less common due to the high risk of recurrence and poor survival. In invasive cancer, radical cystoectomy is indicated, when the bladder in men is removed with the prostate gland and seminal vesicles, and in women with the uterus and appendages.
Instead of a removed bubble, you need to replace it; for this, the following methods are used:
- The urine is diverted to the outside (the ureters are implanted into the skin or into the part of the intestine brought out to the front wall of the peritoneum);
- The urine is diverted into the sigmoid colon;
- An intestinal reservoir is formed from the tissues of the small or large intestine.
Surgical intervention in this type of oncology is complemented by external or contact radiation therapy, and local or systemic immunotherapy.
All types of treatment are prescribed based on many factors - the stage of the disease, the patient's age, general health, etc. Chemotherapy (drug treatment) is widely used. Often use the following drugs for chemotherapy: Doxorubicin (Adriamycin), Methotrexate (Rheumatrex, Trexall), Vinblastine, Cisplatin (Platinum). This type of therapy is more often prescribed at the beginning of tumor metastasis, and radiotherapy can also be prescribed.
RCHD (Republican Center for Healthcare Development of the Ministry of Health of the Republic of Kazakhstan)
Version: Archive - Clinical Protocols of the Ministry of Health of the Republic of Kazakhstan - 2012 (Orders No. 883, No. 165)
Bladder, unspecified (C67.9)
general information
Short description
Clinical protocol"Bladder cancer"
Urinary cancer bladder- one of the most common malignant tumors of the urinary tract. It takes the 17th rank place in terms of frequency of occurrence among the population of Kazakhstan (Arzykulov Zh.A., Seitkazina G.Zh., 2010). Among all cancer patients, it accounts for 4.5% among men and 1% among women.
Protocol code: PH-S-026 "Bladder cancer"
ICD-X code: S.67 (S67.0-S67.9)
Abbreviations used in the protocol:
WHO - World Health Organization
SMP - specialized medical care
VSMP - highly specialized medical care
Ultrasound - ultrasound examination
CT - computed tomography
MRI - Magnetic Resonance Imaging
ESR - erythrocyte sedimentation rate
PET - Positron Emission Tomography
TUR - transurethral resection
RW - Wasserman reaction
HIV - Human Immunity Virus
ECG - electrocardiography
CIS - carcinoma in situ
BCG - Bacillus Calmette-Guérin, BCG
ROD - single focal dose
Gray - Gray
SOD - total focal dose
Date of protocol development: 2011 r.
Protocol users: oncologists, oncological surgeons, oncourologists, chemotherapists and radiologists of oncological dispensaries.
No Conflict of Interest Statement: the developers signed a declaration of conflict of interest on the absence of financial or other interest in the topic of this document, the absence of any relationship to the sale, production or distribution of drugs, equipment, etc. specified in this document.
Classification
International histological classification of bladder cancer:
1. Cancer in situ.
2. Transitional cell carcinoma.
3. Squamous cell carcinoma.
4. Adenocarcinoma.
5. Undifferentiated cancer.
TNM classification(International Union Against Cancer, 2009)
T - primary tumor.
To identify multiple tumors, the index m is added to the T category. To define the combination of cancer in situ with any T category, the abbreviation is is added.
TX - insufficient data to assess the primary tumor.
T0 - there are no signs of a primary tumor.
Ta is a non-invasive papillary carcinoma.
Tis - pre-invasive carcinoma: carcinoma in situ ("flat tumor").
T1 - the tumor spreads to the subepithelial connective tissue.
T2 - the tumor spreads to the muscles.
T2a - the tumor spreads to the superficial muscle (inner half).
T2b - The tumor spreads to the deep muscle (outer half).
T3 - the tumor spreads to the paravesical tissue:
T3a - microscopically.
T3b - macroscopic (extravesical tumor tissue).
T4 - the tumor has spread to one of the following structures:
T4a - The tumor has spread to the prostate, uterus, or vagina.
T4b - The tumor has spread to the pelvic wall or abdominal wall.
Note. If the histological examination does not confirm muscle invasion, then it is considered that the tumor affects the subepithelial connective tissue.
N - regional lymph nodes.
Regional for the bladder are the pelvic lymph nodes below the bifurcation of the common iliac vessels.
NX - it is not possible to determine the state of the lymph nodes.
N0 - metastases in regional nodes are not detected.
N1 - metastases in a single (iliac, obturator, external iliac, presacral) lymph node in the pelvis.
N2 - metastases in several (iliac, obturator, external iliac, presacral) lymph nodes in the pelvis.
N3 - metastases of one or more common iliac lymph nodes.
M - distant metastases.
MX - it is not possible to determine the presence of distant metastases.
M0 - there are no signs of distant metastases.
M1 - there are distant metastases.
Histological classification of bladder cancer without muscle invasion
1973 WHO classification
G - histopathological grading.
GX - The degree of differentiation cannot be established.
1. G1 - high degree of differentiation.
2.G2 - medium degree differentiation.
3. G3-4 - poorly differentiated / undifferentiated tumors.
2004 WHO classification
1. Papillary tumor of the urothelium with low malignant potential.
2. Papillary urothelial carcinoma of low grade.
3. High-grade papillary urothelial cancer.
According to the 2004 WHO classification, bladder tumors are divided into papilloma, papillary urothelial tumor with low malignant potential, urothelial cancer of low and high degree malignancy.
Grouping by stage
|
Stage 0a Stage 0is |
Tis |
N0 | M0 |
| Stage I | T1 | N0 | M0 |
| Stage II |
T2a T2b |
N0 | M0 |
| Stage III |
T3a-b T4a |
N0 N0 |
M0 M0 |
| Bladder | |
|
That Tis T1 T2 T2a T2b T3 T3a T3b T4 T4a T4b |
Non-invasive papillary Carcinoma in situ: flat tumor Extension to subepithelial connective tissue Muscle layer Inner half Outer half Outside the muscle layer Microscopically Peri-vesicular tissue Spread to other surrounding organs Prostate, uterus, vagina Pelvic walls, abdominal wall One lymph node ≤ 2 cm One lymph node> 2< 5 см, множественные ≤ 5 см Metastases to regional l / y> 5 cm in greatest dimension |
Diagnostics
Diagnostic criteria
Clinical manifestations depending on the stage and localization: hematuria, macro- or microhematuria, more often painless hematuria; dysuric phenomena such as difficulty urinating, painful urination, urgent urge, pain in the suprapubic region, weakness, sweating at night, low-grade fever, weight loss.
Physical examination... On examination, there may be local soreness above the bosom. A bimanual examination is mandatory to determine the state of the rectum, prostate gland (in men), determine ingrowth, mobility of these structures; in women, a vaginal examination.
Lab tests: norm or decrease in red blood counts; there may be minor, non-pathogenic changes (such as increased ESR, anemia, leukocytosis, hypoproteinemia, hyperglycemia, a tendency to hypercoagulability, etc.).
Instrumental methods research:
1. Cystoscopy in order to identify the source of hematuria, the location of the tumor process in the bladder. Taking a biopsy from the formation and / or from suspicious areas.
2. Cytological and / or histological confirmation of the diagnosis of malignant neoplasm.
3. Ultrasound of the pelvic organs to confirm the localization of the formation and the prevalence of the process.
4. X-ray research methods - if necessary, to clarify the diagnosis (survey and excretory urography, cystography, CT, MRI).
Indications for specialist consultation:
1. Urologist, the goal is consultations for the exclusion of non-neoplastic diseases (tuberculosis, chronic cystitis, hemorrhagic cystitis, ulcers and leukoplakia of the bladder).
2. Cardiologist - to identify and correct the treatment of concomitant cardiac pathology.
3. Radiologist - performing X-ray examinations, description of X-ray examinations.
Differential diagnosis bladder cancer: sharp or chr. cystitis, cystolithiasis, bladder tuberculosis, prostate adenoma, wasps. or hr. prostatitis, bladder diverticulum; conditions such as prostate cancer, rectal cancer, cervical cancer with invasion into the bladder.
Basic and additional diagnostic measures
Obligatory scope of examination before planned hospitalization:
Anamnesis;
Physical examination;
Bimanual examination, digital rectal examination, vaginal examination;
Laboratory tests: general urine analysis (if necessary, cytological examination of urine sediment), general blood test, biochemical analysis blood (protein, urea, creatinine, bilirubin, glucose), RW, blood for HIV, blood for Australian antigen, blood group, Rh factor;
Coagulogram;
Cystoscopy with biopsy of the tumor and from suspicious areas of the bladder mucosa;
Cytological or histological confirmation of the diagnosis of a malignant neoplasm;
Ultrasound of the pelvic organs (in men - the bladder, prostate gland, seminal vesicles, pelvic lymph nodes; in women - the bladder, uterus with appendages, pelvic lymph nodes);
Ultrasound of the abdominal and retroperitoneal organs;
X-ray of organs chest.
List of additional diagnostic measures:
Transurethral, transrectal and / or transvaginal ultrasound;
CT / MRI of the pelvic organs to determine the extent of the process;
CT scan of the abdominal and retroperitoneal organs;
Laboratory analyzes: ions K, Na, Ca, Cl; and etc.;
Excretory urography with descending cystography;
Fibrogastroscopy and colonoscopy before radical cystectomy - if indicated;
Diagnostic laparoscopy;
Radioisotone renography;
Osteoscintigraphy;
Consultations of related specialists and other examinations - if necessary.
Transurethral resection (TUR) of the bladder (category A) should be performed in all patients with a mass in the bladder for therapeutic and diagnostic purposes (except if there are clear signs of an invasive process in the case of a verified diagnosis). In case of superficial tumors during TUR, the exophytic part of the tumor is resected, then the base with a portion of the muscle layer, 1-1.5 cm of the mucous membrane around it, and altered areas of the bladder mucosa.
In invasive tumors, the bulk or part of the tumor with a portion of muscle tissue is resected. In the case of planning a radical cystectomy, a biopsy of the prostatic urethra should be performed. The stage of the disease is established after histological examination based on data on the depth of invasion of the bladder wall (invasion of the basement membrane and muscle layer).
Treatment abroad
Undergo treatment in Korea, Israel, Germany, USA
Get advice on medical tourism
Treatment
Bladder cancer treatment goals: elimination of the tumor process.
Treatment tactics
Non-drug methods: mode 1 (general), diet - table number 7.
Bladder cancer treatment tactics depending on the stage of the disease
|
Stage diseases |
Treatment methods |
| Stage I (T1N0M0, TisN0M0, Ta N0M0) |
1. Radical operation, TUR * (category A) Intravesical BCG immunotherapy (category A) or intravesical chemotherapy 2. Resection of the bladder 3. Radical cystectomy ** - with multifocal growth and ineffectiveness of previous treatment (category A) |
|
Stage II (T2аN0M0, T2bN0M0) |
1. Radical cystectomy (TUR * at T2a; resection of the bladder with lymphadenectomy ***) |
|
Stage III (T3aN0M0, T3bN0M0, T4a N0M0) |
1. Radical cystectomy 2. Chemo-radiation therapy - as a component of multimodal treatment or in case of contraindications to radical cystectomy |
|
Stage IV (T any N any M1) |
1. Chemoradiation therapy for palliative purposes 3. Palliative surgery |
* In the absence of a TUR device, a resection of the bladder can be performed. If this operation was performed in urology department of the general medical network, it is necessary to obtain histological materials confirming the depth of invasion of the bladder tumor.
** Radical cystectomy should be performed in a specialized (urological oncology) department. This operation can be performed in dispensaries if there is specialized department or beds, as well as in the presence of trained professionals.
*** Resection of the bladder is not a radical operation and should be performed only if there are contraindications to radical cystectomy.
Recommendations
1. There is evidence that radiotherapy alone is less effective than radical treatment (recommendation grade B).
L Treatment of superficial bladder tumors
(stages Tis, Ta and T1)
Organ-preserving tactics (TUR is mainly used - transurethral resection). As an adjuvant effect within 24 hours (preferably within the first 6 hours), a single intravesical instillation with chemotherapy is carried out for 1-2 hours.
With diffuse unresectable superficial bladder cancer and recurrent T1G3 tumors, poorly differentiated tumors with concomitant CIS, in case of ineffectiveness of the treatment, an organ-carrying operation (radical cystectomy) should be performed.
Radiation therapy shown: T1G3, multicentric growth (if radical cystectomy is abandoned).
Surgical treatment of superficial bladder tumors
Conservation surgeries can be performed using high-frequency currents (TUR) and a surgical scalpel (bladder resection).
Transurethral resection (TUR) is the main method of surgical treatment of superficial bladder tumors and tumors invading the superficial muscle. At the same time, TUR is also a diagnostic procedure, as it allows you to establish the histological form and stage of the disease.
TUR involves the removal of the tumor within healthy tissues with morphological control of the edges of the resection, including the bottom of the resection wound. The histological report should indicate the degree of differentiation, the depth of invasion of the tumor, and whether the lamina propria and muscle tissue are present in the material (recommendation level C).
In the case when the primary TURP was incomplete, for example, with multiple or large tumors, in doubt about a radically performed previous TUR operation, or in the absence of a muscular membrane, as well as in case of a G3 tumor, it is recommended to carry out a second TUR in 2-6 weeks (“second look ”- therapy). Repeated TURP has been shown to increase relapse-free survival (LE: 2a).
5-year survival rate primary treatment RMP in the Ta-T1 stage by means of TUR alone is 60-80%. TUR completely cures about 30% of patients. Within 5 years, 70% develop relapses, and 85% of them - within 1 year.
Bladder resection is a surgical method of organ-preserving treatment, it is used in the absence of a TUR device, or the impossibility of performing TUR for one reason or another. Requirements for resection are the same as for TUR - the presence of a muscular membrane is required in the materials (wedge resection should be performed).
Adjuvant treatment methods:
A single direct postoperative intravesical administration of chemotherapy drugs (mitomycin C, epirubicin and doxorubicin). A single direct postoperative administration of chemotherapy drugs should be performed in all patients with suspected bladder cancer without muscle invasion after TUR. Instillation time is significant. In all studies, administration was performed within 24 hours. Intravesical administration should be avoided in cases with obvious or suspected intra- or extraperitoneal perforation, which is very likely to develop with extended TURP.
Intravesical administration of chemotherapy drugs.
Intravesical chemotherapy and immunotherapy.
The choice between further chemotherapy or immunotherapy largely depends on the type of risk that needs to be reduced: the risk of relapse or the risk of progression. Chemotherapy prevents the development of relapse, but not the progression of the disease. If chemotherapy is being carried out, it is recommended to use drugs with an optimal pH and maintain their concentration during instillation by reducing fluid intake. The optimal regimen and duration of chemotherapy remains unclear, but it should probably be given for 6-12 months.
Intravesical chemotherapy and immunotherapy can be used in combination with surgical treatment to prevent recurrence and progression after surgery. The best effect is observed with immediate (within 1-2 hours) intravesical chemotherapy in order to prevent the "dispersion" and "implantation" of tumor cells after TUR, and therefore to reduce recurrence (category B).
Currently, the following chemotherapy drugs are used for intravesical administration: doxorubicin, mitomycin C, cisplatin, and other chemotherapy drugs.
Intravesical chemotherapy regimens:
1. Epirubicin at a dose of 50 mg, diluted in 50 ml of saline, once a week, for 6 weeks, the first injection immediately after the TUR.
2. Doxorubicin 50 mg in 50 ml of saline, intravesical, for 1 hour daily for 10 days, then 50 mg once a month.
3. Doxorubicin 50 mg in 50 ml of saline, intravesical, for 1 hour weekly, for 8 weeks.
4. Mitomycin C 20 mg in 50 ml of isotonic sodium chloride solution, intravesical, 2 times a week, for 3 weeks.
5. Thiophosphamide 60 mg in 50 ml or 30 mg in 30 ml of a 0.5% solution of novocaine, intravesical, for 1 hour, 1-2 times a week, up to a total dose of 240-300 mg.
6. Cisplatin 60 mg in 50-100 ml of isotonic sodium chloride solution, intravesical, 1 time per month.
7. Methotrexate 50 mg, once a week, No. 3-5
When using intravesical chemotherapy in order to prevent relapse after TUR in superficial bladder cancer, the same drugs are used in similar doses, but they are usually administered once a month for 1-2 years.
Intravesical BCG immunotherapy
Intravesical BCG administration is indicated in the presence of unfavorable risk factors: tumors with a high degree of malignancy (T1G3), recurrent tumors, multiple tumors (4 or more), non-radical surgery (tumor growth foci in the cutting edges), the presence of carcinoma in situ, aggressive course of precancerous changes urothelium, positive cytology of urinary sediment after TUR.
BCG (strain RIVM, 2 x 108 - 3 x 109 viable units in one bottle).
BCG - immunotherapy regimen:
3. Intravesical administration of BCG is carried out according to the following technique: the contents of the vial (2 x 108 - 3 x 109 viable units of BCG in one bottle) are diluted in 50 ml of isotonic sodium chloride solution and injected into the bladder for 2 hours. To facilitate contact of the drug with the entire surface of the bladder, the patient is advised to change the position of the body at regular intervals.
Unlike chemotherapeutic agents, BCG cannot be administered immediately after bladder resection due to the potential for severe systemic infection. BCG treatment usually begins 2-3 weeks after TUR. Excessive use of lubricants to lubricate the catheter during instillation can lead to a clinically significant decrease in the number of viable mycobacteria injected and worsening of BCG contact with the bladder mucosa. Therefore, a small amount of lubricant should be used to catheterize the urethra. Lubrication-free catheters are preferred.
When carrying out intravesical BCG immunotherapy, both local and general reactions can be noted, the most common of which is fever. Any patient with a fever greater than 39.5 ° C should be hospitalized and treated as for BCG sepsis. If treatment is not started quickly, sepsis can lead to death of the patient. Modern guidelines for the treatment of BCG sepsis: prescribe a combination of three anti-tuberculosis drugs (isoniazid, rifampicin, and ethambutol) in combination with high doses of corticosteroids short acting.
Patients with a history of BCG sepsis should no longer receive BCG immunotherapy.
Contraindications to intravesical administration of BCG:
Previously transferred tuberculosis;
Sharply positive skin reaction to the Mantoux test;
Diseases of an allergic nature;
Primary immunodeficiency, HIV infection;
Bladder capacity less than 150ml;
Vesicoureteral reflux;
Severe concomitant diseases in the stage of decompensation;
Severe cystitis or gross hematuria (until symptoms disappear);
Traumatic catheterization or the appearance of blood after catheterization of the bladder are contraindications for instillation of BCG on a given day.
In contrast to chemotherapy, BCG immunotherapy, in addition to reducing the frequency of relapses, leads to a decrease in the frequency of tumor progression and increases the survival rate of patients with superficial transitional cell carcinoma. BCG immunotherapy is indicated for patients with a high risk of recurrence and progression of superficial bladder cancer (cancer in situ, stage T1, poorly differentiated tumors), as well as ineffectiveness of intravesical chemotherapy in highly and moderately differentiated Ta tumors.
L treatment of invasive bladder cancer
At the initial treatment, an invasive tumor is detected in 20-30% of patients with bladder cancer, and 20-70% of them (depending on the stage and grade of malignancy) already have regional, and 10-15% have distant metastases.
The gold standard treatment for invasive bladder cancer is radical cystectomy (category A). The following are the various surgical options.
Surgery
In invasive bladder cancer, organ-preserving (TUR with T2a and resection of the bladder) and organ-carrying (radical cystectomy) operations are used. TUR can also be used as a palliative method for stopping bleeding in advanced bladder cancer.
Bladder resection. Bladder resection is not a radical operation and should be performed only if there are contraindications to radical cystectomy or if the patient refuses to do it.
Indications for resection of the bladder: a single invasive tumor within the muscular wall of the bladder, low tumor grade, primary (non-recurrent) tumor, the distance from the tumor to the bladder neck is at least 2 cm, no dysplasia and cancer in situ with a biopsy free of tumors of the bladder mucosa. During the operation, it is necessary to retreat from the visible edge of the tumor at least 2 cm with complete isolation of the affected wall.
Resection of the bladder should be performed to the full depth, including removal of the adjacent part of the perivesical fat, with histological examination of the edges of the resection wound. The operation is combined with mandatory pelvic lymph node dissection. The latter includes the removal of the external and internal iliac and obturator lymph nodes from the bifurcation of the common iliac artery to the obturator foramen. With metastatic lesions of the lymph nodes, the volume of lymph node dissection can be expanded.
If the histological examination reveals tumor cells (R1) at the edges of the resection wound, a radical cystectomy is performed.
When the ureteral orifice is involved in the process, after resection of the bladder and removal of the tumor, ureteroneocystoanastomosis (in various modifications) is performed.
The optimal surgery for invasive bladder cancer is radical cystectomy. The operation includes deletion in a single block along with bladder and perivesical tissue: in men - the prostate gland and seminal vesicles with adjacent adipose tissue, proximal parts of the vas deferens and 1-2 cm of the proximal urethra; in women - the uterus with appendages and the urethra with the anterior wall of the vagina. In all cases, a pelvic lymph node dissection is performed (see above).
With the development of renal failure due to impaired outflow of urine from the upper urinary tract, as the first stage in removing the bladder for temporary urine diversion, as well as in inoperable patients, palliative surgery is performed - percutaneous nephrostomy.
All the huge number of methods for urine diversion after cystectomy can be roughly summarized in three groups:
1. Diverting urine without creating artificial reservoirs:
On the skin;
Into the intestines.
2. Diversion of urine with the creation of a reservoir and its removal to the skin.
3. Various methods bladder modeling with urination recovery (artificial bladder).
The simplest method of diverting urine after removal of the bladder is to the skin (ureterocutaneostomy). This method is used in debilitated patients with a high risk of surgery.
Today, the most convenient method of urine derivation (diversion) is the creation of an ileum conduit according to Bricker. With this method, the ureters are anastomosed into an isolated segment small intestine, one end of which in the form of a stoma is brought to the skin (Bricker operation). In this case, the ureters are anastomosed with the segment of the intestine, and the intestine itself is a kind of conductor for urine (Ileum Conduit). With this method of diversion, urine is constantly excreted on the skin, therefore it is necessary to use special adhesive urine bags. If you cannot use the small intestine as a conduit for urine diversion, you can use the large intestine (usually transversely to the colon).
Drainage of urine into the continuous intestine was considered a convenient method for patients, since there are no open stomas. The most commonly used various techniques of ureterosigmoanastomosis. The main disadvantage of the method is cicatricial deformities of the anastomotic sites with hydronephrotic transformation of the kidneys, as well as the possibility of developing intestinal-ureteral reflux and ascending pyelonephritis. Frequent bowel movements and acute incontinence are additional side effects of this type of surgery. Patients, as a rule, die from chronic renal failure more often than from the progression of the tumor process. Therefore, this technique has recently been used less and less.
The optimal variant of the operation is the creation of an artificial bladder from the small intestine, large intestine and stomach with the restoration of the normal act of urination.
The indications for cystectomy are:
Possibility of performing radical cystectomy;
Normal kidney function (creatinine< 150 ммоль/л);
Lack of metastases (N0M0);
Negative prostatic urethral biopsy.
Of the methods of operation, the most widespread are the methods of U. Studer, E. Hautmann.
Palliative surgery in patients with bladder cancer
The indications for them are:
Life-threatening bleeding from a bladder tumor;
Violation of the outflow of urine from the upper urinary tract and the development of renal failure, acute obstructive pyelonephritis;
Concomitant diseases (diseases of cardio-vascular system, endocrine disorders, etc.).
For the purpose of stopping bleeding, the following are used: TUR of a tumor with stopping bleeding; ligation or embolization of the internal iliac artery; stopping bleeding in an open bladder; palliative cystectomy.
In case of violation of the outflow of urine from the upper urinary tract, the following is used: percutaneous puncture nephrostomy; open nephrostomy; ureterocutaneostomy; supravesical urine diversion into an isolated segment of the small intestine (Bricker operation, etc.).
Radiation therapy for invasive bladder cancer
Confirmation of the diagnosis is required for radiation therapy. In the treatment of bladder cancer, radiation therapy can be used as an independent method and as an integral part of the combined and complex treatment before surgery or after surgery.
Radiation therapy according to the radical program is indicated only in case of contraindications to radical surgery or if the patient is planned to undergo organ-preserving treatment and if the patient refuses surgical treatment.
Radiation therapy according to the radical program is carried out using the inhibitory radiation of a linear accelerator or gamma therapy in the traditional dose fractionation mode (single focal dose (RAD) 2 Gy, total focal dose (SOD) 60-64 Gy for 6-6.5 weeks ( irradiation rhythm - 5 times a week) with a continuous or split course.In this case, first the entire pelvis is irradiated up to SD 40-45 Gy, then in the same mode only the bladder zone up to SD 64 Gy. conservative treatment bladder cancer is achieved with the use of chemoradiation therapy or with the use of radiomodifiers (electron-acceptor compounds, based on the oxygen effect, etc.).
External beam therapy is carried out in the traditional mode: ROD 1.8-2 Gy to SOD 40 Gy. The effect of the treatment is assessed after 3 weeks. When complete or significant resorption of the tumor is achieved, chemoradiation therapy is continued up to SOD 60-64 Gy. In case of incomplete resorption or continued tumor growth, cystectomy can be performed (with the consent of the patient to the operation and functional tolerance of the surgery).
The indication for palliative radiation therapy is stage T3-4. Usually, lower doses of radiation (30-40 Gy) are used with a single dose of 2-4 Gy. Bad general state(Karnofsky index below 50%) and a significant decrease in bladder capacity are contraindications to palliative radiation therapy. Such treatment, in general, has a symptomatic effect, which is mainly limited to a decrease in the severity of gross hematuria. No effect on life expectancy is observed. After 3 weeks, cystoscopy and ultrasound are performed. If the effect is obtained, it is possible to continue radiation therapy up to SOD 60-64 Gy.
At the same time, in some patients, the process becomes resectable and it becomes possible to perform a radical operation.
Symptomatic radiation therapy for bladder cancer is used as a type of palliative therapy to relieve certain manifestations of the disease and alleviate the patient's condition (as a rule, this is radiation of tumor metastases to reduce the severity of pain syndrome).
The use of radiation therapy after surgery is indicated for non-radical surgery (R1-R2). A total focal dose of 60-64 Gy is used in the usual dose fractionation mode (2 Gy) with a five-day irradiation rhythm.
Contraindications to radiation therapy (except for palliative therapy): shrunken bladder (volume less than 100 ml), previous irradiation of the pelvis, presence of residual urine over 70 ml, bladder stones, exacerbation of cystitis and pyelonephritis.
Pre-radiation preparation using an ultrasound machine or with the help of an X-ray stimulator provides:
The position of the patient on the back;
Empty bladder
Obligatory accounting of information obtained during CT, MRI;
Catheterization of the urinary bladder with a Foley catheter with the introduction of 25-30 ml of contrast agent into the bladder and 15 ml into the balloon;
When planning irradiation from the lateral fields, contrasting of the rectum is mandatory.
Irradiation technique
The radiation therapist is free to choose technical solutions (quality of radiation, localization and size of fields), provided that the volume of radiation is included in the 90% isodose.
I. Standard irradiation of the entire pelvis is carried out from 4 fields (anterior, posterior and two lateral).
Front and back margins:
Upper limit - upper limit S2;
The lower border is 1 cm below the lower edge of the obturator hole;
Lateral borders - 1-1.5 cm lateral to the outer edge of the pelvis (in the largest dimension).
The femoral heads, anal canal and rectum are maximally protected by blocks.
Side margins:
The anterior border is 1.5 cm anterior to the anterior surface of the contrasted bladder;
The posterior border is 2.5 cm behind the posterior wall of the bladder.
II. Targeted irradiation (boost) involves the use of two (opposite) or three (straight front and two side) fields.
The entire bladder + 2 cm outside of it is included in the irradiation zone (if the tumor is not clearly defined). In the case of good visualization of the tumor during pre-radiation preparation, the irradiation field includes the tumor + 2 cm beyond its borders.
The standard of the planned radiation volume: 90% isodose includes the bladder and 1.5-2 cm outside of it.
Systemic chemotherapy
Chemotherapy can be used:
In the form of neoadjuvant chemotherapy before surgery or radiation treatment;
Adjuvant chemotherapy after radical surgery or radiation therapy performed according to a radical program;
Independently for unresectable and metastatic bladder cancer as a palliative method.
The greatest percentage of regressions is given by the polychemotherapy regimens containing a combination of cisplatin and gemcitabine, as well as the M-VAC regimen. With almost the same indicators of the objective effect, overall survival. The scheme gemcitabine + cisplatin has an undoubted advantage in terms of the frequency and severity of side effects, improving the quality of life, and reducing the cost of concomitant therapy.
Scheme: gemcitabine 1000 mg / m 2, on days 1, 8, 15, cisplatin 70 mg / m 2, on days 1, 8, 15.
Other polychemotherapy regimens can be used:
1. PG: cisplatin 50-60 mg / m 2, intravenous drip, on the 1st day; gemcitabine 800-1000 mg / m 2, intravenous drip, on the 1st and 8th day. The cycle is repeated after 28 days.
2. GO: gemcitabine 1000 mg / m 2, IV, on the 1st day; oxaliplatin 100 mg / m 2, 2-hour infusion on day 2. Repetition of cycles every 2 weeks.
Epidemiology. The tumor is one of the most common malignant neoplasms (about 3% of all tumors and 30-50% of tumors of the genitourinary organs). Bladder cancer in men is noted 3-4 times more often. Most often they are registered at the age of 40-60. Incidence: 8.4 per 100,000 population in 2001
Code for the international classification of diseases ICD-10:
Causes
Etiology. The occurrence of bladder cancer is associated with tobacco smoking, as well as with the action of several chemical and biological carcinogens. Industrial carcinogens used in rubber, paint and varnish, paper and chemical industries are implicated in bladder cancer. Bilharziasis of the bladder often leads to squamous cell carcinoma. Other etiologic agents include cyclophosphamide, phenacetin, kidney stones, and chronic infection.
Morphology ( bladder tumors are most often of transitional cell origin). papillary. transitional cell. squamous. adenocarcinoma.
Classification... TNM .. Primary focus: Ta - non-invasive papilloma, Tis - cancer in situ, T1 - with invasion into the submucosal connective tissue, T2 - with invasion into the muscular membrane: T2a - inner layer, T2b - outer layer, T3 - Tumor invades peri-vesicular tissues : T3a - determined only microscopically; T3b - determined macroscopically; T4 - with germination of adjacent organs: T4a - prostate, urethra, vagina, T4b - pelvic and abdominal walls .. The lymph nodes: N1 - single up to 2 cm, N2 - single from 2 to 5 cm or more than 5 nodes, N3 - more than 5 cm. Distant metastases: M1 - presence of distant metastases.
Grouping by stage... Stage 0a: TaN0M0. Stage 0is: TisN0M0. Stage I: T1N0M0. Stage II: T2N0M0. Stage III: T3-4aN0M0. Stage IV .. T0-4bN0M0 .. T0-4N1-3M0 .. T0-4N0-3M1.
Clinical picture
... Hematuria. Dysuria (pollakiuria, imperative urge). When the infection joins, pyuria occurs. Pain syndrome does not always occur.
Diagnostics... Physical examination with mandatory digital rectal examination and bimanual examination of the pelvic organs. OAM. Excretory urography: filling defects with large tumors, signs of damage to the upper urinary tract. Urethrocystoscopy - the leading research method for suspected cancer, is absolutely necessary to assess the condition of the mucous membrane of the urethra and bladder. To determine the extent of the lesion and the histological type, an endoscopic biopsy of the tumor is performed. Examine the mucous membrane. In the presence of carcinoma in situ, the mucous membrane is outwardly unchanged, or diffusely hyperemic, or resembles a cobblestone pavement (bullous change in the mucous membrane). Cytological examination urine is informative both in severe tumor lesions and in carcinoma in situ. Ultrasound: intravesical formations and the condition of the upper urinary tract. CT and MRI are the most informative for determining the prevalence of the process. X-rays of the chest and skeletal bones are performed to detect metastases. Bone lesions in high-grade forms of cancer, they can be the first signs of the disease.
Treatment
Treatment depends from the stage of the disease, unambiguous standards for the treatment of bladder cancer have not been developed.
... In case of carcinoma in situ, malignant transformation of mucosal cells occurs .. Local chemotherapy is possible .. In case of widespread lesions (urethra, prostate ducts) and progression of symptoms, early cystectomy with simultaneous plastic surgery of the bladder or transplantation of the ureters into the intestine is indicated.
... Transurethral resection: used for superficial tumor growth without affecting the muscular membrane of the organ. At the same time, relapses are quite frequent. Intravesical chemotherapy reduces the frequency of relapses of superficial bladder tumors. Doxorubicin, epirubicin and mitomycin C are effective. The drug is diluted in 50 ml of physiological solution and injected into the bladder for 1-2 hours. With the degree of differentiation G1, a single instillation immediately after transurethral resection is sufficient. In stage G1-G2 tumors, a 4-8 week course of instillations is carried out .. Local immunotherapy with BCG reduces the frequency of relapses .. External radiation therapy does not give long-term remission (relapses within 5 years in 50% of cases). Interstitial radiation therapy is rarely used. Cystectomy is used to treat patients with diffuse superficial lesions if transurethral resection and intravesical chemotherapy fail.
... Invasive bladder cancer .. Intensive local treatment with cytostatics is prescribed to patients to eliminate rapidly progressing tumor without metastasis .. Radiation therapy. In some tumors, irradiation in a total dose of 60-70 Gy to the bladder area proved to be effective. Radical cystectomy is the method of choice in the treatment of deeply infiltrating tumors. Includes removal of the bladder and prostate in men; removal of the bladder, urethra, anterior wall of the vagina and uterus in women. After radical cystectomy, urine is diverted in one of the following ways: the iliac reservoir, intestinal stoma for self-catheterization, bladder reconstruction or ureterosigmostomy. In villous tumors, localized tumors "in situ", treatment is often started with transurethral resection, adjuvant immunotherapy (BCG), and intravesical chemotherapy. In case of recurrence of such tumors, it is necessary to resolve the issue of performing a cystectomy.
Postoperative follow-up... After transurethral resection, the first control cystoscopy after 3 months, then, depending on the degree of differentiation of the tumor, but not less than 1 r / year for 5 years with the degree of TaG1 and within 10 years in other cases. After reconstructive operations - ultrasound of the kidneys and urinary reservoir, biochemical blood test: the first year every 3 months, the second or third year every 6 months, from 4 years - every year.
The forecast depends on the stage of the process and the nature of the treatment carried out. After radical surgery, the 5-year survival rate reaches 50%
ICD-10. C67 Malignant neoplasm of the bladder. D09 Preinvasive bladder cancer