Insulin injections into the thigh. Important information: how to inject insulin correctly. Is it possible to put insulin and go to bed right away
Not only the quality, in fact, the patient's life itself depends on the correct behavior of a diabetic. Insulin therapy is based on teaching each patient the algorithms of actions and their application in ordinary situations. According to experts from the World Health Organization, a diabetic is his own doctor. The endocrinologist oversees the treatment, and the patient is responsible for performing the procedures. One of the important aspects in the control of chronic endocrine disease is the question of where to inject insulin.
A massive problem
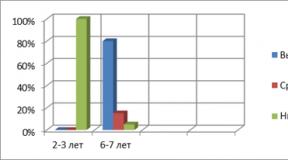
Most often young people are on insulin therapy, including very young children with type 1 diabetes. Over time, they acquire the skill of handling injection equipment and the necessary knowledge of the correct procedure, worthy of the qualifications of a nurse.
Pregnant women with weakened pancreatic function are prescribed an insulin medication for a certain period. Temporary hyperglycemia, for the treatment of which a hormone of a protein nature is required, can occur in people with other chronic endocrine diseases in a state of exposure to severe stress, acute infection.
Patients with type 2 diabetes mellitus take medications orally (by mouth). An imbalance in blood sugar indicators and a deterioration in the well-being of an adult patient (after 45 years) can occur as a result of violations of a strict diet and ignoring the doctor's recommendations. Poor blood glucose compensation can lead to insulin-dependent disease.
 Delaying the transition of the patient to insulin therapy, more often for psychological aspects, contributes to the acceleration of the onset of diabetic complications in him
Delaying the transition of the patient to insulin therapy, more often for psychological aspects, contributes to the acceleration of the onset of diabetic complications in him
The injection areas should be changed because:
- insulin absorption rate is different;
- frequent use of one place on the body can lead to local tissue lipodystrophy (the disappearance of the fatty layer in the skin);
- multiple shots can accumulate.
Insulin accumulated subcutaneously "in reserve" can appear suddenly, 2-3 days after injection. Significantly lower blood glucose levels, causing an attack of hypoglycemia. At the same time, a person develops cold sweat, a feeling of hunger, and his hands tremble. His behavior can be depressed or, conversely, agitated. Signs of hypoglycemia can appear in different people with blood glucose values in the range of 2.0-5.5 mmol / L.
In such situations, it is necessary to quickly raise blood sugar levels to prevent the onset of hypoglycemic coma. First, you should drink a sweet liquid (tea, lemonade, juice) that does not contain sweeteners (for example, aspartame, xylitol). Then eat carbohydrate foods (sandwich, milk biscuits).
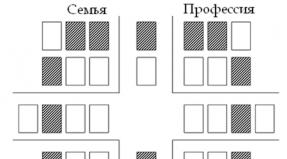
Zoning for injections on the patient's body
The effectiveness of the effect of a hormonal drug on the body directly depends on the place of its administration. Injections of a hypoglycemic agent of a different spectrum of action are not performed in the same place. So where can you inject insulin drugs?
- The first zone is the belly: along the waist, with the transition to the back, to the right and left of the navel. Up to 90% of the administered dose is absorbed from it. Characterized by a rapid unfolding of the action of the drug, after 15-30 minutes. The peak comes in about 1 hour. The injection in this area is the most sensitive. Diabetics inject short insulin into the abdomen after a meal. “To reduce the pain symptom of colitis in the subcutaneous folds, closer to the sides,” - this advice is often given by endocrinologists to their patients. After the patient can begin to eat or even take an injection while eating, immediately after the meal.
- The second zone is the arms: the outer part of the upper limb from the shoulder to the elbow. Injection in this area has advantages - it is the most painless. But it is uncomfortable for the patient to inject into the arm with the help of an insulin syringe. There are two ways out of this situation: to inject insulin with a syringe pen or to teach loved ones to give injections to a diabetic.
- The third zone is the legs: the outer thigh from the groin to the knee joint. Insulin is absorbed from areas located on the extremities of the body up to 75% of the administered dose and unfolds more slowly. The onset of action is 1.0–1.5 hours. They are used for injections with a drug of prolonged (prolonged, extended in time) action.
- The fourth zone is the shoulder blades: located on the back, under the bone of the same name. The rate of unfolding of insulin at a given site and the percentage of absorption (30%) are the lowest. The scapular region is considered an ineffective site for insulin injections.
 Four zones on the patient's body for injections of insulin preparations
Four zones on the patient's body for injections of insulin preparations
The best points with the maximum indicators are the umbilical region (at a distance of two fingers). It is impossible to inject constantly into "good" places. The distance between the last and the forthcoming injection should be at least 3 cm. It is allowed to repeat the injection at the same point in time after 2-3 days.
If you follow the recommendations to prick "short" in the stomach, and "long" in the thigh or arm, then the diabetic has to do 2 injections at the same time in turn. Conservative patients prefer to use mixed insulins (Novoropid mix, Humalog mix) or independently combine two types in a syringe and make one injection in some place. Not all insulins are allowed to be mixed with each other. They can only be of short and intermediate ranges of action.
Injection technique
Diabetics are taught procedural techniques in the classroom in specialized schools organized on the basis of endocrinology departments. Patients who are too young or helpless are injected with their loved ones.
The main actions of the patient are:
- In the preparation of the skin area. The injection site must be clean. Wipe, especially rub, the skin with alcohol is not needed. Alcohol is known to destroy insulin. It is enough to wash a part of the body with warm soapy water or take a shower (bath) once a day.
- Preparation of insulin ("pen", syringe, vial). The medicine must be rolled in the hands for 30 seconds. It is best to introduce it well stirred and warm. Collect and check the accuracy of the dose.
- Making an injection. With your left hand, make a skin fold and insert the needle into its base at a 45-degree angle or into the top, holding the syringe vertically. After draining the medicine, wait 5-7 seconds. You can count up to 10.
If you quickly remove the needle from the skin, then insulin flows out of the puncture site, and part of it does not enter the body. Complications of insulin therapy can be of a general nature, in the form of allergic reactions to the type used. An endocrinologist will help replace the hypoglycemic agent with a suitable analogue. The pharmaceutical industry offers a wide range of insulin-type drugs. Local trauma to the skin occurs due to a thick needle, the injection of refrigerated medicine, and an unsuccessful choice of the injection site.
Observations and sensations during injections
Basically, what the patient experiences with the injections are considered subjective manifestations. The threshold of pain sensitivity is different for each person.
There are general observations and sensations:
- there is not the slightest pain, which means that a very sharp needle was used, and it did not hit the nerve ending;
- mild pain may occur if the nerve has been hit;
- the appearance of a drop of blood indicates damage to the capillary (small blood vessel);
- bruising is the result of using a blunt needle.
 Do not inject into the place where the bruise appears until it is completely absorbed.
Do not inject into the place where the bruise appears until it is completely absorbed.
The needle in syringe pens is thinner than in insulin syringes, it practically does not injure the skin. For some patients, the use of the latter is preferable for psychological reasons: there is an independent, clearly visible set of doses. The injected hypoglycemic agent can enter not only the blood vessel, but also under the skin and into the muscle. To prevent this from happening, it is necessary to collect the skin fold as shown in the photo.
The effect of insulin can be accelerated by the ambient temperature (warm shower), massage (light stroking) of the injection site. Before using a medicinal product, the patient must make sure of the appropriate expiration date, concentration and storage conditions of the product. Diabetic medicine should not be frozen. Its stocks are allowed to be stored in the refrigerator at a temperature of +2 to +8 degrees Celsius. The currently used vial, pen-syringe (disposable or loaded with an insulin sleeve) should be kept at room temperature.
Last updated: April 18, 2018
Timely treatment of diabetes mellitus saves a person's life. And this treatment consists of hormone replacement therapy. In the absence of glucose accumulates in the blood, and the internal organs of a person, without the supply of energy, cease to perform their functions.
How to inject insulin on your own so that a sick person can live and behave like a healthy person - we will consider in this article.
Diabetes symptoms and treatment
Before we tell you how to properly administer insulin, let's talk about diabetes. In a healthy person, the blood glucose level should be in the range from 3.5 to 6.0 mmol / l. Persistently high blood sugar is the first symptom of diabetes mellitus. The situation described is true for type 1 diabetes.
In type 2 diabetes, a person has a hormone, but the body “does not feel” it. It also occurs with elevated blood sugar. This sign of diabetes mellitus is determined by analyzing venous blood. But even before the analysis, you can suspect a disease on some grounds:
- the patient is often thirsty;
- dryness of the mucous membranes and skin is felt;
- the sick person cannot get enough of his fill - a short time after eating, he again wants to eat;
- rapid fatigue and weakness;
- phlebeurysm;
- skin diseases begin for no apparent reason;
- aching joints.
How do I take insulin? In the case of type 1 diabetes, the patient is prescribed insulin. Depending on his condition, injections should be given either 2 times a day, or before each meal. The doctor may prescribe any other treatment regimen. He will determine how to inject insulin correctly and, as well as teach the patient how to give an injection.

In type 2 diabetes, this hormone is also injected, but in addition, drugs are prescribed that increase sensitivity to the substance described. In addition, often simultaneously with a decrease in the amount of the hormone in a person, the content of anticoagulants decreases, which leads to ulcers, edema, gangrene in diabetes, why the doctor prescribes an anticoagulant - heparin. The drug taken cannot be used without the recommendation of a specialist, since it has a number of serious contraindications.
Hormone injections
In order for a specialist to prescribe a specific scheme for the administration of the hormone, the patient needs to check the amount of sugar in the blood during the week at different times of the day. For this, blood glucose meters are sold in pharmacies and medical equipment stores.
Based on these indicators, insulin is prescribed according to a certain scheme. For those with recent and mild diabetes mellitus, it may be enough to follow the correct diet, increase physical activity, and sugar will return to normal. In more complex cases, in addition to diet and exercise, insulin injections are indispensable for diabetes.

In type 1 diabetes, insulin is usually injected subcutaneously 2 times a day - in the morning and in the evening. A long-acting hormone is used. In type 2 diabetes, injections should be done before meals, so that under the influence of food intake there is no sharp increase in blood sugar. For this, a fast-acting hormone is used, which begins to work 5 minutes after the injection of insulin subcutaneously. How to properly give yourself an injection of insulin, we will talk about it below. In what type of diabetes to inject this or that type of hormone, how many times a day, the specialist will tell you.
Choosing an injection device
How do you administer insulin? Some people with diabetes use disposable syringes for injections. These syringes have a 10-part plastic drug container for calculating the amount of drug to be administered and a thin needle. The disadvantage of using them is that a set of insulin up to the 1 mark means 2 units of the hormone. How to use, the syringe is inaccurate? It gives an error of half a division. For sick children, this is very important, since with the introduction of an extra unit of the volume of the hormone, their sugar will drop below normal.

For the convenience of self-injections, insulin pumps have been developed. It is an automated device that can be configured to deliver a specific amount of a substance when injected. They are easy to inject with insulin. But the cost of such devices is prohibitively high - up to 200 thousand rubles. Not every patient can afford such expenses.

The most acceptable option is insulin syringes with small needles or pen syringes. They contain 1 unit of hormone volume for an adult or 0.5 unit for a child. The pen comes with a set of needles, each of which can be used 1 time. The device used for the injections affects the dosing accuracy.

Injection technique
The peculiarities of insulin administration are that the needle does not need to be injected deeply. It is necessary to draw insulin into a syringe according to the rules. Step by step, the insulin injection technique looks like this:
- You need to wash your hands thoroughly. Better to wipe them with alcohol or vodka.
- Draw air into the syringe up to the mark that determines the required dose of the hormone.
- Then stick the needle through the plug of the hormone vial and squeeze the air in.
- Draw insulin into the syringe from the vial, dialing a little more than the required dose.
- Remove the syringe from the vial, tap it with your finger to release the air bubbles.
- Squeeze the excess amount of the hormone back into the vial so that the strictly required amount is drawn into the syringe.
- Lubricate the injection site with an antiseptic - alcohol, vodka, hydrogen peroxide.
- Grab the part of the skin that has been oiled with an antiseptic into a crease. If the syringe has a short insulin needle, then this is not necessary.
- Then you need to insert the needle shallowly so that the medicine gets into the subcutaneous fat. Hold the insulin needle at a 90 or 45 degree angle.
- Dispense the hormone from the syringe.
- Remove the needle, release the fold of skin after a few seconds.
- Apply an antiseptic to the pricked area.
The rules for administering insulin are simple. After a few injections, anyone will learn how to give the injections. Injection using a syringe pen differs in that with the help of a special wheel, the dose of the hormone is immediately set, which will be drawn from the vial.
How to use the special insulin pen is described in the accompanying instructions. The sites of insulin administration are determined by the experience of doctors and patients.
Where is it better to prick?
Where to inject insulin is a purely individual question. Usually, insulin injections are given to the outside of the arms or legs, to the buttocks, or to the abdomen. The effect of the hormone depends on the choice of the injection site - the speed of its assimilation, the duration of the effect on the body.
It is impossible to inject insulin into your buttock, so your arms, legs and abdomen remain. How to get an injection? You cannot inject all the time in the same place. If it is more convenient for you to inject into the abdomen, observe the distance between the points of entry of the needle at least 2 cm.Subcutaneous injection of insulin creates the risk of lipodystrophy - this is a violation of the structure of the subcutaneous fat layer with the appearance of bumps at the site of frequent injections, with the accumulation of fat in the limbs. But otherwise the medicine will not give the desired effect. Bumps can be treated with troxevasin ointment, or by drawing a grid in the area of the injections with a cotton swab dipped in iodine. The bumps do not pass quickly, but in the end they disappear. Gradually, the patient will learn to inject the hormone so that complications do not arise if insulin is injected incorrectly. The main thing is to maintain sterility. What is worth fearing is getting an infection in the wound. The methods of administration of insulin do not depend on the choice of the injection site. Insulin injection sites and hormone treatment algorithms are interconnected.

Insulin injection sites:
- Among experienced diabetics, it is customary to inject insulin into the abdomen. The hormone introduced into the subcutaneous fat of the abdomen is quickly absorbed and begins to work. Injections into this area are not too painful, and the resulting wounds tend to heal quite quickly. The abdomen is almost not subject to lipodystrophy.
- Outer arm. The medicine is not completely absorbed during injection - only up to 80%. Bumps may form. To prevent this from happening, hands need to be given physical activity during the break between injections.
- The outer part of the leg is used to inject a long-acting hormone. This part of the body slowly absorbs the injected drug. Exercise is also needed to prevent bump formation.
- Where can a child be injected with insulin? The baby is given injections in the buttocks, since he is not able to inject himself, and the injection in the buttock is less painful. The hormone is absorbed slowly but completely. The buttocks are often injected with short-acting hormones.
In any case, the technique of subcutaneous administration of insulin must be followed. Sick people should remember that the hormone is injected daily for life. But this does not negate the need for a diet containing a small amount of sweet and starchy foods, as well as physical activity. Treatment and the algorithm for insulin administration can only be prescribed by a doctor. Self-medication leads to disastrous results.
Diabetes treatment often requires insulin injections.
Most patients do not know where and how the injection is given, and most importantly, they fear such manipulation.
Using insulin in pens will allow you to inject the hormone without fear, it is simple and affordable for people of all ages.
When insulin therapy is required, the diabetic person should know how to use an insulin pen. Outwardly, this device looks like an ordinary ballpoint pen, only instead of ink it contains a compartment with insulin.

There are three types of drug administration:
- With disposable cartridge. After the end of the insulin, it is thrown away.
- With replaceable. The advantage is that after use the cartridge is replaced with a new one.
- Reusable. You can refill this insulin pen yourself. The medicine is added to the desired mark and the device is again ready for use.
The patient should remember that separate devices are provided for hormones of different effects; some manufacturers have them in a multi-colored design. One division on the device corresponds to 1 unit of medicine, on children's models there is a division of 0.5 units. It is necessary not only to know how to inject insulin with a syringe pen, but also to choose the correct thickness of the needle. Its choice depends on the age of the patient and the amount of adipose tissue.
Benefits of using:
- it is much more convenient to dose the medicine,
- use is possible outside the home,
- painful sensations are minimized,
- it is almost impossible to get into the muscle,
- easy to carry.

Before buying a device, you should familiarize yourself with the main models, cost, and also pay attention to:
- appearance, quality of the case,
- scale of measurement, since numbers and divisions must be clear,
- presence of an insulin sensor,
- the presence of a magnifying glass on the scale of the device is convenient for patients with poor eyesight.
The choice of the needle is also important: a person with an average degree of diabetes should have a thickness in the range of 4-6 mm. When the stage of the disease is initial, and the amount of adipose tissue is small, a needle up to 4 mm (short) will be needed. Teenagers and children are advised to select the minimum diameter.
The device is stored at room temperature, protected from heating and cooling. For safety, a protective case is used, and spare insulin cartridges are placed in the refrigerator. Before using it, you should wait until the medicine warms up slightly to room temperature, otherwise the administration may be painful.
To understand how to give an injection of insulin with a syringe-pen, you need to familiarize yourself with the rules of execution. It is necessary to get the device out of the protective case, remove the cap.
After that:
- See if there is insulin in the cartridge. Use a new one if necessary.
- Be sure to put a fresh needle: do not use old ones, due to damage and deformation.
- Shake the contents thoroughly with insulin.
- Letting out a few drops of the medicine will help prevent air from entering.
- Select the required dosage according to the scale on the insulin pen.
- The device is held at a 90 degree angle and the injection is gently injected. To do this, it is necessary to insert the needle of the syringe - the handle into the fold of the skin, while the button must be pressed all the way.
- It is advised to hold the device for at least 10 seconds after injection. This will prevent insulin from leaking from the injection site.
After carrying out, the used needle is disposed of, the injection site is remembered. The next injection should not be closer than 2 centimeters from the previous one. The choice of the injection site is individual: you can inject insulin with a pen into the abdomen, leg (thighs and buttocks). When there is enough adipose tissue, use the upper arm for convenience.

In order to make the pain from the injection minimal, it is worth:
- Avoid getting into hair follicles.
- Choose a needle with a smaller diameter.
- To make a fold of the skin carefully: you do not need to do this with all your fingers at once - the skin is lifted with two fingers. This method will protect you from the chance to get into the muscle.
- Hold the skin loose, do not pinch this place. Medicines must be freely accessible.
It will not be difficult to figure out how to inject insulin in diabetes with a pen, and in the future, all actions will come to automatism.
There is no unambiguous scheme for insulin injections. The doctor draws up an individual schedule for each patient. The hormone level is measured over a week, and the results are recorded.
The endocrinologist calculates the body's need for insulin and prescribes treatment. For example, patients who follow a low-carb diet, whose blood sugar levels are normal, can do without injections by monitoring their glucose levels. But in case of infectious, bacterial diseases, they will need to inject a hormone, because the body will need much more insulin. In such cases, injections are usually prescribed every 3-4 hours.

If the glucose level rises slightly, then 1-2 injections of extended insulin are prescribed for one day.
In a severe form of the disease, in addition to the above actions, fast insulin is used. It must be administered before every meal. With mild or moderate severity of the disease, the time of the injection is determined. The patient monitors the hours at which the sugar level rises to the maximum. Most often, this is the morning time, after breakfast - during these periods you need to help the pancreas, which is working to the limit.
The insulin pen is convenient to use because there are reusable models. They are enough for 2-3 years of operation, you just need to replace the hormone cartridges.

Pros of a reusable syringe - pens:
- The injection process is simple and painless.
- The dosage is self-adjusting, thanks to a special scale.
- Apply outside of being at home.
- It is possible to enter a more accurate dose than using a conventional syringe.
- The injection can be given through clothing.
- Convenient to carry.
- A child or an elderly person can handle the device. There are models equipped with a sound signal - they are convenient for people with visual impairments and disabilities.
An important point: it is preferable to use a pen and cartridge from the same manufacturer.
If we talk about the disadvantages of using, then they include:
- device price,
- the complexity of the repair,
- the need to select a cartridge for a specific model.
A pen syringe is not suitable for those patients who require minimal doses of the hormone. When the button is pressed, only a part of the medicine cannot be injected; in this case, it is recommended to use a regular syringe.
The unpleasant moment of the procedure is the risk of bumps or bruises. The first more often arise due to repeated use of the needle, improper procedure. There are lipodystrophic (thickening of the fat layer) and lipoatrophic (depressions in the skin) bumps.
The main thing that patients need to remember is that the medicine should not be injected into the same place. Use needles one-time, without trying to save money on it. If a lump has already arisen, then drugs are used to dissolve the infiltrate, natural medicines. Physiotherapy procedures have proven themselves well. They are used when the buds remain in place for more than a month or there are many of them.

If bruises appear after the injection, it means that a blood vessel was injured during the procedure. This is not as scary as the appearance of bumps, bruises will dissolve on their own.
Sometimes there are cases when the pen does not work. Patients complain of a jammed button, sometimes insulin flows out. To avoid such situations, it is worth:
- carefully choose the manufacturer of the device,
- carefully store the syringe pen, keep it clean,
- select needles suitable for the device,
- do not administer large doses with one injection.
- do not use the device beyond the expiration date.
Before the first use, be sure to study the instructions for the syringe - pen. The cartridge should not be used for more than 28 days; if there is excess solution left, discard it. Careful attention to the device and its components will ensure the correct administration of insulin without consequences.
For reading 8 min. Views 1.6k. Posted on 28.12.2018
Diabetes mellitus is a disease that cannot be cured. With an insulin-independent form of pathology, to maintain the patient's condition, it is necessary to regularly take pills that lower blood sugar levels. With type 1 diabetes, injections are needed. Each patient should clearly understand how to administer insulin.
Preparation
Most diabetics self-administer insulin injections. The algorithm is simple, but it is vital to learn it. You need to know where to put insulin injections, how to prepare the skin and determine the dosage.
In most cases, the insulin bottle is designed for multiple uses. Therefore, it should be refrigerated between injections. Immediately before the injection, the composition must be lightly rubbed in the hands in order to warm the substance before contact with the body.
It should be borne in mind that the hormone is of different types. It is necessary to enter only the type recommended by the doctor. It is important to strictly adhere to the dosage and timing of the injection.
Insulin injections should only be done with clean hands. Before the procedure, they should be washed with soap and dried thoroughly.

This simple procedure will protect the human body from the possibility of infection and infection of the injection site.
A set of the drug in a syringe
An injection with insulin is delivered according to a regulated algorithm. It is important to be careful to get it right.

The following instruction will help.
- Check the doctor's prescription with the drug to be used.
- Make sure that the hormone used is not expired and is not stored for more than a month from the moment the bottle was first opened.
- Warm the bottle in your hands and mix its contents thoroughly without shaking so that bubbles do not form.
- Wipe the upper part of the bottle with a napkin soaked in alcohol.
- Draw as much air into an empty syringe as needed for a single injection.
The insulin injection syringe has divisions, each indicating the number of doses. It is necessary to gain a volume of air equal to the required volume of the drug for administration. After this preparatory stage, you can proceed to the very process of introduction.
Do I need to wipe my skin with alcohol
Cleansing the skin is always required, but the procedure can be carried out in different ways. If, shortly before the injection of insulin, the patient took a bath or shower, additional disinfection is not necessary, alcohol treatment is not required, the skin is clean enough for the procedure. It is important to consider that ethanol destroys the structure of the hormone.

In other cases, before making an injection of insulin, the skin should be wiped with a napkin soaked in an alcohol solution. You can start the procedure only after the skin is completely dry.
Installing the needle
After the required amount of air has been drawn into the syringe plunger, the needle should carefully pierce the rubber stopper on the vial with the drug. The collected air must be introduced into the bottle. This will make it easier to take the correct dose of medication.
The bottle should be turned upside down and the required amount of medicine should be drawn into the syringe. In the process, hold the bottle so that the needle does not bend.

After that, the needle and syringe can be removed from the vial. It is important to make sure that no air droplets get into the container together with the active substance. Although it is not dangerous to life and health, the retention of oxygen inside leads to the fact that the amount of active substance that has entered the body is reduced.
Where to inject insulin
Insulin injection sites can be used in different ways. They differ in the rate of absorption of the substance and the method of administration. Experienced doctors recommend changing the location every time.

Insulin injections can be injected into the following areas:
- in the buttock;
- in leg;
- in the thigh;
- in the hand;
- in the stomach.
It should also be borne in mind that the types of insulin used in type 2 diabetes are different.
Long-acting insulin has the following features:
- entered once a day;
- enters the bloodstream within half an hour after administration;
- evenly distributed and acts;
- remains in the blood for a day at a constant concentration.

The insulin syringe mimics the function of the pancreas of a healthy person. It is recommended to give such injections to patients at the same time. So you can ensure the stable state and storage properties of the drug.
Short and ultrashort insulin
This type of insulin is injected into your usual injection sites. Its peculiarity is that it should be used 30 minutes before meals. It is especially effective only for the next 2-4 hours. Remains active in the blood for the next 8 hours.

The introduction is carried out using a syringe pen or a standard insulin syringe. It is used to maintain normal glucose levels in pathology of the second or first type.
How much time should elapse between long and short insulin injection?
If you need to use a short insulin and a long one at the same time, it is better to discuss the order of their correct combination with your doctor.
The combination of the two types of hormone is done like this:
- every day, once a day, long-acting insulin is injected to maintain a stable blood sugar level for 24 hours;
- shortly before a meal, a short-acting drug is administered to prevent a spike in glucose after a meal.
The exact amount of time can only be determined by a doctor.
When injections are given at the same time every day, the body gets used to it and responds well to using two types of insulin at the same time.
How to inject insulin
In order to properly give an injection of insulin, it is worthwhile to understand a few simple rules.
What, in your opinion, are the most important factors when choosing a medical institution?
Poll Options are limited because JavaScript is disabled in your browser.
Not only the quality, in fact, the patient's life itself depends on the correct behavior of a diabetic. Insulin therapy is based on teaching each patient the algorithms of actions and their application in ordinary situations. According to experts from the World Health Organization, a diabetic is his own doctor. The endocrinologist oversees the treatment, and the patient is responsible for performing the procedures. One of the important aspects in the control of chronic endocrine disease is the question of where to inject insulin.
A massive problem
Most often young people are on insulin therapy, including very young children with type 1 diabetes. Over time, they acquire the skill of handling injection equipment and the necessary knowledge of the correct procedure, worthy of the qualifications of a nurse.
Pregnant women with weakened pancreatic function are prescribed an insulin medication for a certain period. Temporary hyperglycemia, for the treatment of which a hormone of a protein nature is required, can occur in people with other chronic endocrine diseases in a state of exposure to severe stress, acute infection.
Patients with type 2 diabetes mellitus take medications orally (by mouth). An imbalance in blood sugar indicators and a deterioration in the well-being of an adult patient (after 45 years) can occur as a result of violations of a strict diet and ignoring the doctor's recommendations. Poor blood glucose compensation can lead to insulin-dependent disease.
 Delaying the transition of the patient to insulin therapy, more often for psychological aspects, contributes to the acceleration of the onset of diabetic complications in him
Delaying the transition of the patient to insulin therapy, more often for psychological aspects, contributes to the acceleration of the onset of diabetic complications in him
The injection areas should be changed because:
- insulin absorption rate is different;
- frequent use of one place on the body can lead to local tissue lipodystrophy (the disappearance of the fatty layer in the skin);
- multiple shots can accumulate.
Insulin accumulated subcutaneously "in reserve" can appear suddenly, 2-3 days after injection. Significantly lower blood glucose levels, causing an attack of hypoglycemia. At the same time, a person develops cold sweat, a feeling of hunger, and his hands tremble. His behavior can be depressed or, conversely, agitated. Signs of hypoglycemia can appear in different people with blood glucose values in the range of 2.0-5.5 mmol / L.
In such situations, it is necessary to quickly raise blood sugar levels to prevent the onset of hypoglycemic coma. First, you should drink a sweet liquid (tea, lemonade, juice) that does not contain sweeteners (for example, aspartame, xylitol). Then eat carbohydrate foods (sandwich, milk biscuits).
Zoning for injections on the patient's body
The effectiveness of the effect of a hormonal drug on the body directly depends on the place of its administration. Injections of a hypoglycemic agent of a different spectrum of action are not performed in the same place. So where can you inject insulin drugs?
- The first zone is the belly: along the waist, with the transition to the back, to the right and left of the navel. Up to 90% of the administered dose is absorbed from it. Characterized by a rapid unfolding of the action of the drug, after 15-30 minutes. The peak comes in about 1 hour. The injection in this area is the most sensitive. Diabetics inject short insulin into the abdomen after a meal. “To reduce the pain symptom of colitis in the subcutaneous folds, closer to the sides,” - this advice is often given by endocrinologists to their patients. After the patient can begin to eat or even take an injection while eating, immediately after the meal.
- The second zone is the arms: the outer part of the upper limb from the shoulder to the elbow. Injection in this area has advantages - it is the most painless. But it is uncomfortable for the patient to inject into the arm with the help of an insulin syringe. There are two ways out of this situation: to inject insulin with a syringe pen or to teach loved ones to give injections to a diabetic.
- The third zone is the legs: the outer thigh from the groin to the knee joint. Insulin is absorbed from areas located on the extremities of the body up to 75% of the administered dose and unfolds more slowly. The onset of action is 1.0–1.5 hours. They are used for injections with a drug of prolonged (prolonged, extended in time) action.
- The fourth zone is the shoulder blades: located on the back, under the bone of the same name. The rate of unfolding of insulin at a given site and the percentage of absorption (30%) are the lowest. The scapular region is considered an ineffective site for insulin injections.
 Four zones on the patient's body for injections of insulin preparations
Four zones on the patient's body for injections of insulin preparations
The best points with the maximum indicators are the umbilical region (at a distance of two fingers). It is impossible to inject constantly into "good" places. The distance between the last and the forthcoming injection should be at least 3 cm. It is allowed to repeat the injection at the same point in time after 2-3 days.
If you follow the recommendations to prick "short" in the stomach, and "long" in the thigh or arm, then the diabetic has to do 2 injections at the same time in turn. Conservative patients prefer to use mixed insulins (Novoropid mix, Humalog mix) or independently combine two types in a syringe and make one injection in some place. Not all insulins are allowed to be mixed with each other. They can only be of short and intermediate ranges of action.
Injection technique
Diabetics are taught procedural techniques in the classroom in specialized schools organized on the basis of endocrinology departments. Patients who are too young or helpless are injected with their loved ones.
The main actions of the patient are:
- In the preparation of the skin area. The injection site must be clean. Wipe, especially rub, the skin with alcohol is not needed. Alcohol is known to destroy insulin. It is enough to wash a part of the body with warm soapy water or take a shower (bath) once a day.
- Preparation of insulin ("pen", syringe, vial). The medicine must be rolled in the hands for 30 seconds. It is best to introduce it well stirred and warm. Collect and check the accuracy of the dose.
- Making an injection. With your left hand, make a skin fold and insert the needle into its base at a 45-degree angle or into the top, holding the syringe vertically. After draining the medicine, wait 5-7 seconds. You can count up to 10.
If you quickly remove the needle from the skin, then insulin flows out of the puncture site, and part of it does not enter the body. Complications of insulin therapy can be of a general nature, in the form of allergic reactions to the type used. An endocrinologist will help replace the hypoglycemic agent with a suitable analogue. The pharmaceutical industry offers a wide range of insulin-type drugs. Local trauma to the skin occurs due to a thick needle, the injection of refrigerated medicine, and an unsuccessful choice of the injection site.
Observations and sensations during injections
Basically, what the patient experiences with the injections are considered subjective manifestations. The threshold of pain sensitivity is different for each person.
There are general observations and sensations:
- there is not the slightest pain, which means that a very sharp needle was used, and it did not hit the nerve ending;
- mild pain may occur if the nerve has been hit;
- the appearance of a drop of blood indicates damage to the capillary (small blood vessel);
- bruising is the result of using a blunt needle.
 Do not inject into the place where the bruise appears until it is completely absorbed.
Do not inject into the place where the bruise appears until it is completely absorbed.
The needle in syringe pens is thinner than in insulin syringes, it practically does not injure the skin. For some patients, the use of the latter is preferable for psychological reasons: there is an independent, clearly visible set of doses. The injected hypoglycemic agent can enter not only the blood vessel, but also under the skin and into the muscle. To prevent this from happening, it is necessary to collect the skin fold as shown in the photo.
The effect of insulin can be accelerated by the ambient temperature (warm shower), massage (light stroking) of the injection site. Before using a medicinal product, the patient must make sure of the appropriate expiration date, concentration and storage conditions of the product. Diabetic medicine should not be frozen. Its stocks are allowed to be stored in the refrigerator at a temperature of +2 to +8 degrees Celsius. The currently used vial, pen-syringe (disposable or loaded with an insulin sleeve) should be kept at room temperature.
Last updated: April 18, 2018