Features of the use of antibacterial drugs in obstetric practice. The problem of antibiotic resistance. Antibiotic resistance and ways to overcome the problem of resistance - examples of diseases
On September 19, 2017, a report of the World Health Organization, devoted to the problem of a serious situation with antibiotics on our planet.
We will try to talk in detail about the problem that cannot be underestimated, because it is a serious threat to a person's life. This problem is called antibiotic resistance.
According to the World Health Organization, the situation on the planet is fundamentally the same in all countries. That is, antibiotic resistance develops everywhere and no matter whether the United States or Russia.
When we talk resistance to antibiotics, then you need to understand that this is a kind of jargon. Under antibiotic resistance is understood not only the resistance to antibiotics, but also to viral preparations, anti-grapple drugs and drugs against the simplest.
So where does antibiotic resistance come from?
Everything is quite simple. People live on the planet whose owners are three and a half years old are microorganisms. These organisms are fighting with each other, try to survive. And of course, in the process of evolution, they developed a colossal number of ways to protect against any type of attack.
The source of sustainable microorganisms in our everyday, is medicine and agriculture. Medicine Because, here is already 3 generations of people since 1942, antibiotics are used to treat everything possible diseases. Of course, without antibiotics, not yet do. Any operation, any treatment of infection requires the appointment of an antibacterial drug. With each taking of such a drug, a part of microorganisms dies, but the survivor remains. Here she transfers resistance to the next generation. And over time, superbacterial appears or excess infections - microorganisms that are immune almost to any antibiotic. Such superbacteries have already appeared in our everyday life and unfortunately collect a rich harvest of victims.
The second source of the problem is agriculture. From 80 to 90% of all antibiotics is not applied in medicine and not for people. Antibiotics almost feed a cattle, otherwise there is no bridge and an animal sick. There can be no other way, because we collect millions of livestock heads in a limited space, keep them in not natural conditions And feed their feeds, which nature does not provide for this type of body. Antibiotics are a kind of guarantee that Scott will not hurt and will gain weight. As a result, tens of thousands of tons of antibiotics are in nature and there, the selection of sustainable strains begins, which are returned to us with food.
Of course, not everything is so simple and it's not only in medicine and in agriculture. Here tourism and global economy playing a very large role (when food, some raw material, fertilizer is transported from one country to another). All this makes it impossible to somehow block the spread of superbacteria.
In fact, we live in one big village, so some kind of supermicrobid that arose in one country becomes a big problem in other countries.
It is worth tuping such an important reason for the development of antibiotic resistance, as the use of drugs without appointing a doctor. According to American statistics about 50% of cases in receiving antibiotics belong to viral infections. That is, any cold and man begins to apply an antibacterial drug. Not only is it not effective (antibiotics for viruses do not act !!!), it also leads to the emergence of more sustainable types of infections.
Finally, the problem that will seem amazing for many. We have no new antibiotics left. Pharmaceutical companies Just uninteresting to develop new antibacterial drugs. Development, as a rule, takes up to 10 years of heavy work, a lot of investments and in the end, even if this drug got to the market, it does not give any guarantees that resistance will not appear in a year or two to it.
In fact, in our medical arsenal, there is antibiotics developed many years ago. Of fundamentally new antibiotics in our medical use has not appeared for 30 years. What we have is modified and recycled old versions.
And so, we have a sufficiently serious situation. We arrived arrogantly to compete with a giant number of microorganisms, who have their understanding how to live, how to survive and how to respond to the most unexpected circumstances. Especially since our antibiotics, even the most chemical, not very big news for the micrometer. This is because, in its mass of antibiotics, this is the experience of the microme itself. We peep how microbes are fighting each other and making conclusions, create an antibacterial drug (for example, penicillin). But even the inventor of the antibiotic, Sir Alexander Fleming, warned: what active application Antibiotics will certainly cause the emergence of the strains of microorganisms resistant.
In connection with the foregoing, it is possible to bring simple rules for personal safety when using antibacterial drugs:
- Do not hurry to apply an antibiotic if you or someone from your loved ones quilted.
- Use only those antibiotics that a doctor prescribed you.
- Buy drugs only in pharmacies.
- If we started taking the drug, be sure to go through the entire course of treatment.
- Do not reserve antibiotics, each medicine has its own shelf life.
- Do not share antibiotics with other people. Each person is individually selected this or that drug.
Antibiotic resistance is the resistance of a certain body to connections from the class of antibiotics. Currently antibiotics - the only category drugswhose effectiveness gradually decreases. The fact of antibiotic resistance itself is simply impossible to exclude - this is due to the progress of life, evolution on different steps and forms of organisms from the simplest to complex macrosystems.
Relevance of the issue
Antibiotic resistance of microorganisms is produced completely naturally. Initially, the level is low, gradually reaches medium values, and then develops to high stability. Microscopic organisms showing the increased level of resistance to one antimicrobial preparation, with a high proportion of probability will have protection and other compounds. The process of acquiring sustainability cannot be converted, but you can slowly restore the sensitivity - the truth is only partially.
Currently antibiotic resistance is a global problem associated with insufficient infectious control. Antimicrobial compounds were widespread in agriculture, food industry. Similar antimicrobial drugs substances are actively used in everyday life. All this affects the acquisition by pathological forms of life of an increased level of resistance to those substances that were completely dangerous for them.
About nuances of phenomena
Antibiotic essence of bacteria can be natural, it is possible to purchase resistance to antibiotics.
The formation and distribution of the phenomenon is largely due to free sale in pharmacies of drugs from the antimicrobial class. According to the rules, the doctor must be released strictly according to the doctor's prescription, but a number of funds, many points are sold in free mode. Most often, this concerns the cases when the client is interested in the acquisition of gentamicin, ciprofloxacin.
One of the problems of modern medicine is the irrational use of antimicrobial drugs, which is also one of the antibiotic-resistant growth of mechanisms. Often the appointment of funds is unreasonable and even chaotically. Normally, antibiotics are needed before the operation, but they are often used after surgery. Appointment to the patient unjustifiably low dosages, lack of infectious control, improper organization of the treatment process - all this provokes an increase in antibiotic resistance of pathological microorganisms.
About problems and realities
Although scientists are still working on the creation of new drugs, more efficient and efficient, the use of antimicrobial means in recent years is facing two serious difficulties. This antibiotic resistance already mentioned above, as well as expanding the diversity of pathogens dosage forms. Resistance to antimicrobial means is currently relevant for all types of microscopic life forms. It is this reason that the main, due to which the drug therapy becomes less efficient. In modern medicine, special difficulties create widespread resignation antimicrobial drugs Synutaya and intestinal sticks, protea and staphylococci.
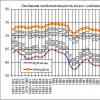
As the studies are shown, currently the problem of antibiotic resistance is becoming more relevant: half to 90% of all strains allocated resistant to different compositions.
About nuances of the problem
It has been established that the level of resistance to antimicrobial compounds is formed unevenly. Pretty slow this process proceeds relative to the preparations of penicillin rows, cycloserine, polymixin, chloramphenicol. Against the background of a slow decline in performance weakened the therapeutic effect of the course.
Regarding cephalosporins, tetracycline, aminoglycosides, as scientists have found out, microscopic forms of life antibiotic resistance is also relatively slow. Therapeutic efficiency is reduced at a prerequisite.
The problem of antibiotic resistance is most relevant in infecting strains from which Rifampicin, Linko- and Oleandomycin, Fusidin should help. These compounds resistance can be formed during the first course of treatment.

How does this happen?
Antibiotic resistance mechanisms have long attracted the attention of scientists. If it was possible to take control of these processes, the problem of persistence of pathological microorganisms would be solved. Currently, it was revealed that quite often the phenomenon is observed due to the modification of the antimicrobial composition. The form is transformed into inactive. For example, this is possible if the microorganism generates some enzyme that comes into a chemical reaction with a drug connection.
Classic example: Staphylococcus can produce beta lactamase. This substance affects the beta-lactam penicillin ring, blurring it and making the drug safe for the causative agent of diseases.
Many gram-negative forms of life show increased resistance to aminoglycosides. This is explained by their ability to generate phosphorylating, acetylating compounds that destroy the antimicrobial molecule. Also, gram-negative pathogens can produce acetyltransferase, which deactivates chloramphenicol.
About the mechanisms: continuing the topic
Studying the mechanisms of antibiotic-resistant microorganisms, scientists found that such reactions are possible, during which the target is transformed, the effect of the antibiotic on which the desired result should have been transformed. Protein structures are inactivated, a resistant complex is formed. It was revealed that at the level of chromosoma, the resistance to aminoglycosides is due to the transformation or withdrawal of the protein structure on the 30s pinnicker of the chromosome of the bacteria, the sensitivity receptor is normal. Resistance to penicillin row, cephalosporins is explained by the transformation of the penicillin-binding protein structure.
Revealing the mechanisms for the formation of antibiotic resistance, also found that in a large percentage, the cells of the microbe becomes less permeable for the active drug. For example, streptococcus inherent from nature a barrier through which aminoglycosides cannot pass. Preparations from tetracycline row accumulate only in bacteria sensitive to them. In the resistance of the lifetime, the compound in principle cannot penetrate the body of the causative agent.

Resistance development: Process Nuances
In determining antibiotic resistance, it is necessary to analyze specific microorganisms not only for the possibility of producing enzymes that depress the activity of the drug. Some bacteria can form compounds that destroy antibiotics. In particular, there are such forms of life whose cylosterin resistance is explained by the release of alanine-transferase.
Another subtle moment - antibiotic-resistance genes. It is known that microscopic forms of life are able to form new metabolism mechanisms, create a so-called metabolic shunt. It helps them avoid reactions to which the drug is affected.
In some cases, antibiotic resistance is a phenomenon associated with Effluux. The term is accepted to signify the process of actively removing the aggressive component from the microbe cell. The most vibrant representative of the diseases capable of this pathogens is a blue chopstick. Analysis and studies have shown that the resistant forms of this bacteria are able to actively extend the carbapenams from the microbial cell.
About causes and mechanisms
Currently, the problem of antibiotic resistance in Russia and in the world is becoming more larger. It is customary to allocate genetic and non-such persistence of pathological forms of life. The activity of bacterial replication largely determines the effectiveness of drugs. Inactive in terms of exchange processes, non-multiplying bacteria racks to the influence of drugs, but the offspring will still be sensitive.

It has been established that mycobacterium provoking tuberculosis, for a long time (years) exists in organic tissues of an infected person. All this period to fight it using chemotherapy is useless - the causative agent of racks to any drugs. But at the time when the immunity of the carrier weakens, and mycobacteria begins to reproduce actively, its offspring gets sensitivity to drugs.
In some cases, the loss of antibiotic resistance is explained by the loss of a specific target. Some microscopic forms of life sensitive to the penicillin row can be transformed into protoplasts when entering the antibiotic microorganism, as a result of which the cell wall is lost. In the future, the microbes can again gain sensitivity to those drugs that depress the synthesis of the cell walls: when returning to the parent form, the synthesis processes should be resumed, which leads to overcoming antibiotic resistance.
About genetics
Genetic antibiotic resistance is a phenomenon formed as a result of genetic transformations occurring in a microscopic organism. In some cases, resistance is explained by the specificity of metabolism. This form of resistance is divided into two groups: chromosomal and not one.
Chromosomal resistance
This phenomenon may be formed as a result of a random mutation in the chromosome of the bacterium responsible for the receptivity of drugs. Antibiotics affect some specific mechanisms, while resistance is gradually formed. Mutants have absolute protection, under the influence of external factor, receptor structures are not rebuilt.
As a rule, a certain narrow chromosomal section has genes in which receptors for antimicrobial compounds are encoded. For streptomycin, for example, it is the protein structure of P12 on the 30s pod. For gene mutations, under which the features of reactions with P12 are changing, resistance to streptomycin appears. Gene mutations may cause an exception from the structure of the receptor microorganism. It was revealed that some microorganisms became resistant to penicillin-row preparations, since no longer contains receptors in their structure capable of perceiving penicillin.

Extra- and extrachromosomal resistance
The development of such features is explained by the genetic elements outside the chromosome. It can be round DNA molecules, plasmids, which account for up to 3% of the total weight of the chromosome. They have unique genes, the genes of other plasmids. Free plasmids are in bacterial cytoplasm or embedded in chromosome. During their account, the pest usually gets resistance to penicillin row, cephalosporins, since the genes of beta-lactamase formation is laid in genes. They explain enzyme compounds that provide acetylation, phosphorylation of aminoglycosides. According to such logic, the development of resistance to tetracycline row due to the impermeability of the microbial cell for the substance is possible.
To transfer genetic information, plasmids resort to the processes of change, transduction, conjugation, transposition.
Cross resistance is possible. This is said when the microscopic form of life receives resistance to different means, the mechanisms of the influence of which are similar to the microbes. This is more characteristic of drugs having such a chemical structure. In some cases, the cross phenomenon is characteristic and for substances whose chemical structures differ quite strongly. Characteristic example: erythromycin and lincomycin.
What to do?
Since the problem of antibiotic resistance is becoming increasingly relevant, the scientific community makes efforts to form new principles and treatments to overcome complexity. As a rule, use the possibilities of combined therapy, but it is inherent in certain disadvantages, and in the first place - an increased frequency side Effects. A positive effect in some cases is observed when applying fundamentally new drugs showing a good result with strain resistance to previously used drugs.
For the resistance of microorganisms to be overcome, and the effectiveness of the therapeutic course is increased, it is reasonable to resort to proven combinations of funds. If the infection of life forms producing beta-lactamase is revealed, such drugs should be used, as part of which there are components that suppress the activity of the enzyme. For example, a similar feature was revealed from Clavulana, a pelvictam. These substances have a rather weak antibacterial effect, but the inhibitory process is irrelevant, which allows to protect the main antibiotic from the enzyme. Most often, clavulanic acid is prescribed in combination with amoxicillin or ticarcillin. In pharmacies, such drugs are presented under trade names "Augmentin" and "Timentyp". Another reliable drug "Unzin" is based on ampicillin, which was protected through Sulbacts.

Treatment price
Often, when choosing therapy makes a decision on the simultaneous reception of several types of drugs with different mechanisms of influence on the pathological forms of life. It is customary to say that the most effective antibiotic - the one that in the minimum volume gives a sufficient effect, without provoking negative phenomena in macroorganism. Currently, the fundamentally appropriate to this description is simply not, together with the desired result, there is always a negative impact.
In some cases, side effects are strong enough, and this completely eliminates the use of an antimicrobial preparation according to its purpose. As can be seen from statistical data, up to 40% of all cases of antibiotics lead to complications, of which the preferential part (8 cases out of 10) are allergic reactions, another 7% of poisoning. The classification of side effects on allergic, and also explained by the effect of the drug on macroorganism and influence on immunity, positive microflora.
What will help?
Since resistance to K. different forms drugs in microorganisms are becoming more wider, before appointing the therapeutic course it is necessary to resort to modern methods Definitions of antibiotic resistance, in order to have a selected program showed the desired effect and delivered a patient from the causative agent. To verify the intended effectiveness, it is necessary to allocate the culture of the pathological form of life and study it for the susceptibility of a particular preparation. Given that in the laboratory and in practical use, the results may be different. There are several explanations to this phenomenon, including the acidity of the body environment, the conditions of cultivation and the magnitude of the colonies.

The main method for determining antibiotic resistance is to carry out laboratory tests. Recently, express tests have appeared for individual forms of pathogens.
Antibacterial drugs are important and often by the main component. complex therapy Infectious pathology in obstetric practice, their rational and reasonable use in most cases determines the effectiveness of the treatment, favorable obstetric and neonatal outcomes.
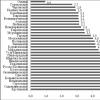
In Russia, 30 different groups of antibiotics are currently used, and the number of drugs (excluding non-original) is approaching 200. In the US, it is shown that antibiotics are one of the most frequently appointed pregnant drugs: 3 of the 5 drugs used during pregnancy are antibacterial agents. Despite the fact that a small amount of research revealed the possible negative effects of antibacterial therapy during pregnancy, the frequency of using antimicrobial drugs during gestation remains largely unknown.
It must be said that the microbiological feature of purulent-inflammatory diseases in obstetrics, gynecology and neonatology is the polyimicrobial etiology of these diseases. Among the pathogens of the purulent-inflammatory diseases of the urogenital tract in pregnant women and the maternity hospitals are dominated by conditionally pathogenic enterobacteria ( E. coli, klebsiellasPP. ., Proteus.sPP.), Often in association with bonde anaerobes of the Bacteroids family - PrevotellasPP. and anaerobic coccobs. In recent years, the role of enterococci in the etiology of purulent-inflammatory diseases in obstetrics and neoatology has increased, which, apparently, is associated with the stability of these bacteria to cephalosporins, widely used in obstetric practice. The common patterns of the dynamics of the etiological structure of purulent-inflammatory diseases make it possible to say that in each hospital there are a certain epidemiological situation, the biological features of pathogens and their sensitivity to antibiotics, and therefore local monitoring of the species composition and antibiotic resistance of the allocated microorganisms, which determines the choice of drugs for preventive and the treatment of the disease.
The use of antibacterial drugs in obstetric practice has a number of features that should be considered for effective treatment infectious inflammatory diseases in pregnant women and herds. Antibacterial therapy of purulent-inflammatory diseases in obstetrics and gynecology can only be effective taking into account their clinic, etiology, pathogenesis and a number of features arising in the body of pregnant women and determining right choice and adequate use of antibacterial drugs.
During pregnancy, antibacterial therapy should be aimed at eliminating infection, prevention of infection of the fetus and a newborn, as well as the development of postpartum purulent inflammatory diseases. Rational I. effective application Antibiotics during pregnancy implies the following conditions:
- it is necessary to use drugs only with prescribed use of use during pregnancy, with the well-known metabolic pathways (criteria for sanitary control of food quality of food and US drugs (Food and Drug Administration, FDA));
- when prescribing drugs, the term of pregnancy should be taken into account, it is necessary to take particularly carefully to the appointment of antimicrobial drugs in the first trimester of gestation;
- in the process of treatment, careful control over the state of the mother and the fetus is necessary.
Antibacterial drugs for use in obstetric practice should not have neither teratogenic nor embryotoxic properties; As far as possible, at maximum efficiency, it is low toxic, with a minimum frequency of unwanted drug reactions. Row modern antibiotics Fully satisfies these requirements, in particular, inhibitors of penicillins, cephalosporins and macrolides. Modern antibiotic therapy of individual nosological forms begins with empirical treatmentWhen antibiotics are introduced immediately after diagnosing the disease, taking into account possible pathogens and their sensitivity to drugs. When choosing a drug for starting therapy, known literary data on its spectrum of action on microorganisms, pharmacokinetic features, the etiological structure of this inflammatory process, antibiotic resistance structure. Before starting therapy, it is necessary to obtain material from the patient for the microbiological research.
From the first days of the disease, it is advisable to prescribe an antibiotic or a combination of antibiotics that are maximally overlapping the range of possible causative agents of the disease. To do this, it is necessary to use a combination of synergistic active antibiotics with complementary spectrum of action or one drug with wide spectrum actions. With the positive dynamics of the disease on the basis of the results of the microbiological research, it is possible to switch to drugs of a narrower spectrum of action. After the excitation of the pathogen and determining its sensitivity to antimicrobial drugs, in the absence of a clinical effect on the initial empirical therapy, it is advisable to continue treatment with the drug, which, according to the analysis, the causative agent of the disease is sensitive. Purposeful monotherapy is often more effective, it is more profitable and economically. The combination of antibacterial drugs is shown in the treatment of diseases of polyminomicrobial etiology in order to reduce the possibility of developing the antibiotic resistance of certain types of bacteria, to use the advantages of the joint action of antibiotics, including reduced dose of drugs used and their side effect. However, it should be borne in mind that combination therapy is usually less beneficial economically than monotherapy.
Antibacterial therapy of purulent-inflammatory diseases in obstetrics and gynecology should be systemic, not local. With systemic treatment, it is possible to create the necessary concentration of antibiotics in the blood and a focus of the lesion, maintaining its required time. The local use of antibacterial drugs does not allow to achieve the indicated effect, which in turn can lead to the selection of resistant strains of bacteria and the insufficient efficiency of the local antibiotic therapy.
Antibiotic resistance of microorganisms is one of the most acute problems of modern medicine. Sustainability of microorganisms distinguish between two types: primary (species) due to the lack of a target for medicinal substance, impermeability of the cell membrane, the enzymatic activity of the pathogen; and secondary, acquired, - when using erroneous doses of the drug, etc.
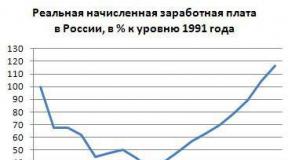
"If modern medicine ... The root will not revise the attitude towards the use of antibiotics, sooner or later the post-libeotic era will come in which many common infectious diseases There will be nothing to be treated, and they will again carry a lot of human lives. The surgery, transplantology and many other industries will become impossible ... "These bitter words of the general director of the World Health Organization (WHO), Dr. Margaret Chen, pronounced on World Health Day 2011, today sound even more relevant. Drugstore bacteria are rapidly distributed on the planet. More and more fundamental medicines cease to act on bacteria. Arsenal of therapeutic agents is rapidly reduced. Nowadays, in the countries of the European Union, Norway and Iceland annually about 25 thousand people die of infections caused by resistant bacteria, and most of such cases are observed in hospitals. The domestic problem of drug sustainability of microorganisms is also regarded as a threat to national security, which confirms the World Economic Forum, which included Russia into the list of countries with global risk, since 83.6% of Russian families uncontrollably take antimicrobial drugs. According to the Ministry of Health of the Russian Federation, about 16% of Russians today have antibiotic resistance. At the same time, 46% of the population of Russia are convinced that antibiotics kill viruses as well as bacteria, and therefore antibiotics are prescribed at the first symptoms of ARVI and influenza. Currently, 60-80% of doctors in the Russian Federation for reinsurance are prescribed antibiotics, without checking whether it will act on this strain of bacteria in this particular patient. We our own hands grow monsters - superbacteria. Along with this, over the past 30 years, no new class of antibiotics was opened, but during the same time the resistance of some pathogens to individual antibiotics completely eliminated the possibility of their application at present.
The key cause of resistance development is the improper use of antimicrobial drugs, such as:
- the use of drugs without necessity or against the disease that this drug does not treat;
- reception of drugs without appointment by a medical specialist;
- non-compliance with the prescribed mode of intake of antibiotics (insufficient or excessive use of drugs);
- excessive purpose of antibiotics by doctors;
- antibiotics transmission to other persons or the use of remnants of prescribed drugs.
Stability threatens to achieve modern medicine. Return to Daentibiotic ERU can lead to the fact that many infectious diseases in the future will become incurable and uncontrollable. In many countries, government programs to combat antibiotic-resistant are already available.
The term "superbacterium" (Superbug) in recent years has become increasingly appearing not only in professional literatureBut in the media for the non-Medicine audience. We are talking about microorganisms with stability to all known antibiotics. As a rule, superbacteries are available non-hospital strains. The appearance of antibiotic resistance is a natural biological phenomenon reflecting in the action of evolutionary laws of variability and natural selection of Charles Darwin with the only difference that human activity acts as a factor of "selection", namely, the irrational use of antibiotics. The stability of bacteria to antibiotics develops due to mutations or as a result of the acquisition of genes of resistance from other bacteria already having stability. It turned out that the superbacteria distinguishes from the rest of the presence of the enzyme metal-B-lactamase-1 New Delhi (NDM1; for the first time it was found in New Delhi). Enzym provides resistance to one of the most effective classes of antibiotics - carbapenes. At a minimum, each tenth bacteria strain carrying the NDM1 enzyme gene has an additional, while not a deciphered set of genes providing polesistance - no antibiotic is able to affect this microorganism neither bactericidal or even bacteriostatically. The probability of transmitting the NDM1 gene from the bacteria to the bacterium is large, as it is detected in plasmids - additional non-chromasome carriers of genetic information. These forms of life transmit to each other genetic material horizontally, without division: they are connected in pairwise with cytoplasmic bridges, according to which ring RNA (plasmids) are transported to another. The varieties of bacteria included in the "superprocess" is becoming more and more. This is primarily the pathogens of anaerobic and aerobic wound infection - Klostridia, golden staphylococcus (in some countries are more resistant to one or many antibiotics are more than 25% of the strains of this infection), Klebsiella, asinobacter, pseudomonades. As well as the most frequent pathogen with inflammatory diseases of the urinary tract - intestinal wand.
It is very important in combating the problem of resistance. Compliance with the rules for the appointment of antimicotics and antibiotics. Against the background of the upcoming superbacterial, optimistic messages began to appear that ways of dealing with an invincible enemy were found. Some are relieved on bacteriophages, others - on coatings with nanopours that attract any bacteria due to the difference of charges, the third persistently look for new antibiotics.
The medical facilities for overcoming antibiotic resistance include the use of alternative methods for the treatment of infectious processes. In the US, Europe and Russia, the Renaissance of targeted therapy of infections with bacteriophages occurs. The advantages of phageotherapy is its high specificity, no suppression of a normal flora, a bactericidal effect, including in biofilms, self-evaporation of bacteriophages in the lesion focus, that is, "automatic dosing", the absence of toxic and teratogenic effects, safety during pregnancy, good Portability and very low chemotherapeutic index. The purpose of bacteriophages can be called highly specific antibacterial therapy without exaggeration. Historically, the only drugs overwhelming the growth of bacteria were antibacterial viruses - bacteriophages. Bacteriophage preparations have good prospects as an alternative to chemotherapeutic antibacterial therapy. Unlike antibiotics, they have strict selectivity of action, do not suppress normal microflora, stimulate factors of specific and non-specific immunity, which is especially significant in the treatment of chronic inflammatory diseases or bacterias.
Therapeutic and prophylactic bacteriophages contain polyclonal virulent bacteriophages of a wide range of action, active in t. And with respect to antibiotic-resistant bacteria. Fagotherapy can be successfully combined with the appointment of antibiotics.
Thus, in the context of the formation of antimicrobial resistance, the formation of sustainable bacterial films The need for new alternative medical technologies and antimicrobial preparations is becoming increasingly important. Prospects for the use of bacteriophages concern not only antimicrobial therapy, but also of high-precision diagnostics, as well as oncology.
But all this should not calm down. Bacteria is still smarter, faster and more experienced us! The most faithful way is the total change in the use of antibiotics, tightening control, a sharp limitation of the availability of drugs without a prescription, a ban on the non-chosen use of antibiotics in agriculture. In the United States adopted the program "GetSmart" ("Crave!"), Focused on the reasonable use of antibiotics. Canadian program "Do Bugs Need Drugs?" ("Are the drug microbes need?") Reduced by almost 20% the use of antibiotics in respiratory tract infections. In Russia, the problem of the broad and uncontrolled use of antibiotics is discussed little and does not meet the active counteraction of the medical community and state structures regulating the treatment of medicines.
In the second quarter of 2014, the World Health Organization published a report on antibiotic resistance in the world. This is one of the first detailed reports over the past 30 years regarding such a relevant global problem. It analyzes data from 114 countries, including Russia, on the basis of which it was concluded that antibiotic resistance today is celebrated in all countries of the world, regardless of their level of welfare and economic development. the Russian Federation In 2014, for its part, it became the initiator of the signing of the document, which enshrines that the assessment of the situation with antibiotic-resistant country in the country is a national priority. The current situation has a lot of socio-economic importance and is considered as a threat to national security. To overcome this problem in 2014, a number of summits of antibacterial therapy specialists in Samara, Yekaterinburg, St. Petersburg and Novosibirsk were successfully held. The Expert Council for Health at the Committee on Social Policy of the Council of the Federation is actively engaged in the development of strategic directions on this issue. Conducting summits of such a format will make it possible to arrange and consolidate the opinion of leading specialists in all regions of the Russian Federation and convey our ideas to the Ministry of Health and the Government of the Russian Federation. The World Health Organization recommends real measures to prevent infections at the most initial stage - by improving hygiene and access to clean water, the fight against infections in medical institutions and vaccinations, and also draws attention to the need to develop new drugs and diagnostic tests of microbial resistance, as well as the development of national recommendations on the rational use of antibiotics and national regulations for monitoring their observance. An example of the effectiveness of these measures is national companies in Europe. For example, the program "Antibiotics: A Reasonable Approach", adopted in Thailand, is aimed at tightening the control over the appointment and release of antibacterial drugs and is addressed to both doctors and patients. Initially, changes in the principles of antibiotics were developed and implemented, which led to a decrease in their consumption by 18-46%. Further, decentralized networks, united local and central partners, for further expansion of the program are created. In Australia, a comprehensive package of measures aimed at improving the culture of antibiotics consumption was adopted. A key role in containing antimicrobial resistance, taking into account the long-term period of struggle with it, is currently given by governments and politicians, as well as training for health workers. Many countries implement continuous training programs for the rational use of antibiotics.
Analysis of literary sources, reports on the implementation of the tasks of the Global Strategy and Antibiotic Resistance Resolutions showed a small number of information about Russia's participation in this global process, which is evidence of a lack of research conducted in this area. In this regard, the domestic health care is tasked with creating a reliable supervision system for the use of antibiotics, the organization of network monitoring of antibiotic-resistant, systematic data collection of antibioticograms and the spread of the clinical consequences of this phenomenon. To overcome the stability of bacteria to antibiotics, a systemic interdepartmental approach and active actions are needed at the national level.
The study was carried out at the expense of the grant of the Russian Scientific Foundation (project No. 15-15-00109).
Literature
- Balushkin A. A., Tyutyunnik V. L. The basic principles of antibacterial therapy in obstetric practice // Russian Medical Journal. Obstetrics and gynecology. 2014, No. 19. P. 1425-1427.
- Gurtova B. L., Kulakov V. I., Voropheyeva S. D. The use of antibiotics in obstetrics and gynecology. M.: Triada, 2004. 176 c.
- Clinical recommendations. Obstetrics and gynecology. 4? E ed., Pererab. and add. / Ed. V. N. Serov, T. Tryym. M.: Gootar Media, 2014. 1024 p.
- Kozlov R. S., Blya A. V. Strategy for using antimicrobial drugs as an attempt by Renaissance antibiotics // Wedge. Microbiol. and antimicrob. Chemother. 2011. № 13 (4). P. 322-334.
- Kuzmin V.N. Modern approaches To the treatment of inflammatory diseases of the small pelvic organs // Consilium Medicinum. 2009. No. 6, vol. 11, p. 21-23.
- Medicinal products In obstetrics and gynecology / ed. Acad. Ramne V. N. Serov, Acad. RAMS G. T. dry. 3rd ed., Act. and add. M.: Gootar-Media, 2010, 320 p.
- Practical guidance on anti-infectious chemotherapy / ed. L. S. Stachunsky, Yu. B. Belousova, S. N. Kozlova. Publishing house NIIA SGMA, 2007. 384 p.
- The increasing threat to the development of antimicrobial resistance. Possible measures. World Health Organization, 2013. 130 p.
- ADRIAENSSENS N., COENEN S., VERSPORTEN A.et al. European Surveillance of AntimiCrobial Consumption (ESAC): Outpatient AntiBiotic Use in Europe (1997-2009) // J. Antimicrob. Chemother. 2011. Vol. 66 (6). P. 3-12.
- Broe A., PottegRD A., Lamont R. F.et al. Increasing Use of Antibiotics in Pregnancy During The Period 2000-2010: Prevalence, Timing, Category, and demographics // BJOG. 2014. Vol. 121 (8). P. 988-996.
- Lapinsky S. E.ObStetric Infections // Crit. Care Clin. 2013. Vol. 29 (3). P. 509-520.
- Antimicrobial Resistance Global Report on Surveillance 2014/226 AP2.2 Guiding WHO Documents for Surveillance of AMR General and Comprehensive Recommendations. Available AT: http://www.who.int/drugresistance/who_global_ strategy. HTM / EN / WHO GLOBAL STRATEGY FOR CONTAINMENT OF ANTIMICROBIAL RESISTANCE.
- Reporting Protocol: The European Antibiotic Resistance Surveillance Network (Ears-Net). Version 3, 2013. 43 s.
- Expert Consultation on AntimiCrobial Resistance / Report On a Meeting Edited by: Dr Bernardus Ganter, Dr John Steeling. World Health Organization, 2011. Available at: http://www.euro.who.int/pubrequest.
- The Bacterial Challenge: Time to React / European Center for Disease Prevention and Control, Stockholm, 2009. Available at: http://www.ecdc.europa.eu.
- European Strategic Action Plan on Antibiotic Resistance 2011-2016 / Dr Guenael Rodier, Director, Division of Communicable Diseases, Health Security and Environment - European WHO Regional Committee, 61 Session, 12-15.09.2011.
- Zsuzsanna Jakab. Prevention of Health-Care-Associated Infections (AMR) And Antimicrobial Resistance (AMR) in Europe WHO / V International Conference on Patient Safety, Healthcare Associated Infection and Antimicrobial Resistance, Madrid, Spain, 2010.
- Antibiotic Use in Eastern Europe: A Cross-National Database Study In Coordination For Europe // Lancet Infectious Diseases. 2014. Available at: http://dx.doi.org/10.1016/s1473-3099 (14) 70071-4.
- CENTERS FOR DISEASE CONTROL AND PREVENTION. Sexually transmitted deseasses // Treatment Guidelines. 2006. MMWR 2006; 55 (No. RR-11).
- Bonnin R. A., Poirel L., Carattoli A.et al. CHARACTERIZATION OF AN INCFIIPLASMID ENCODING NDM-1 FROM ESCHERICHIA COLI ST131 // PLOS ONE. 2012. № 7 (4). E34752. Epub 2012. Apr 12.
- LESKI T., VORA G. J., TAITT C. R. Multidrug Resistance DeterminantsFrom NDM-1? PRODUCING KLEBSIELLAPNEUMONIAE IN THE USA // INT. J. Antimicrob. Agents. 2012. No. 17. Epub Ahead of Print.
- Tateda K. Antibiotic-Resistant Bacteria and New directions of AntimiCrobial Chemotherapy //Rinshobyori. 2012. No. 60 (5). P. 443-448.
- Bolan G. A., Sparling P. F., Wasserheit J. N.The Emerging Threat of Untreatable Gonococcal Infection // N. engl. J. Med. 2012. No. 9; 366 (6). P. 485-487.
- Preventing Hospital-Aquired Infection // Clinical Guidelines. 2000. R. 42.
- Royal College of ObStetricians and Gynaecologists Bacterial Sepsis in Pregnancy // Green-Top Guideline. 2012. № 64 a.
- Rivers E. P., Katranji M., Jaehne K. A.et al. Early Interventions in Severe Septic Schock: A Review of the Evidence One Decade Later // Minerva Anestesiol. 2012. No. 78 (6). P. 712-724.
- SOGC Clinical Practice Guideline Antibiotic Prophylaxis // Obstetric Procedures. 2010. № 247.
L. V. Adamyan,doctor of Medical Sciences, Professor, Academician of the Russian Academy of Sciences
V. N. Kuzmin 1, doctor of Medical Sciences, Professor
K. N. Arsalanan, candidate of Medical Sciences
E. I. Kharchenko, candidate of Medical Sciences
O. N. Loginova,
candidate of Medical Sciences
GBU HPE MGMS. A. I. Evdokimova of the Ministry of Health of the Russian Federation, Moscow
The solution to the problem of antibiotic-resistant in the hospital requires the development of a strategy to prevent and deterrence, which would include several directions. Key of them are: Activities aimed at limiting the use of antibiotics, conducting targeted epidemiological supervision, compliance with the principles of isolation in infections, education of medical personnel and the implementation of administrative control programs.
Famous facts:
- The resistance of microorganisms to antimicrobial preparations is a global problem.
- Implementation of effective control over the rational use of antibiotics requires the solution of numerous problems.
- Strategies that rigorly control the use of antibiotics in the hospital make it possible to reduce the frequency of their irrational use and limit the appearance and distribution of resistant strains of microorganisms.
- Insulation of sources of infection and the elimination of potential reservoirs of pathogens in the hospital are essential events. Such sources are colonized by pathogenic microorganisms or infected patients, as well as colonized / infected medical personnel and contaminated medical equipment and consumables. Patients' long-staying in the hospital are a permanent source of infection, especially if they suffer from chronic diseases flowing with various pathological discharges, or have fixed fixed catheters.
- The basis of the epidemiological supervision is to conduct a permanent monitoring in order to identify, confirm and register infections, their characteristics, trends in the frequency of development and the determination of sensitivity to antimicrobial drugs of their causative agents. Especially important to solve the problem of antibiotic resistance is a targeted supervision aimed at monitoring and collecting information on the appointment of antibiotics in the hospital. One of the most important objects for such a focused supervision is the Orit. The information obtained as a result of its holding can serve as a basis for developing policies to apply antibiotics in the hospital with the support of the administration.
- The microbiological diagnosis of infection and the rapid provision of its results (the dedicated pathogen and its sensitivity to antibiotics) are the main factors that determine the rational choice and the appointment of adequate antimicrobial therapy.
Controversial issues:
- Many believe that the resistance of microorganisms is extremely the result of the irrational use of antibiotics. However, antimicrobial resistance will develop even with their proper use. Due to the fact that in modern medicine, antibiotics are an indispensable class of drugs and their use is necessary, the emergence of resistant microorganisms will be inevitable undesirable phenomenon when applying them. Currently, there has been an extreme need to revise many regimens of antibacterial therapy, which probably have a direct impact on the emergence of poly-resistant strains of microorganisms in a hospital.
- It is known that in most cases heavy infections (Bacteremia, pneumonia) caused by antibiotic-resistant strains of bacteria, accompanied by a higher frequency of lethal outcomes than the same infections, but caused by sensitive strains of microorganisms. Despite this requires further study, the result of which is a higher mortality rate.
- Currently in many countries, especially in developing, there is no adequate microbiological diagnosis of infections and bilateral interaction between microbiologists and clinicians. It pretty much prevents rational choice antimicrobial drugs and the implementation of infection control measures in the hospital.
- The use of antibiotics and the development of resistance to them in microorganisms are interrelated phenomena. Many believe that national Recommendations And various strategies aimed at limiting the use of this group of drugs, not justified themselves. Despite this, currently there is an inevitable need to evaluate, review and implement recommendations on the rational choice and the use of antibiotics, which must be adapted depending on the existing practices and conditions in each particular hospital.
- Develop and enforce administrative control activities:
- the policy of using antibiotics and hospital formulars;
- protocols, compliance with which will allow you to quickly identify, isolate and carry out treatment of patients colonized or infected with antibiotics strains of bacteria, which in turn will contribute to the prevention of the spread of infections in the hospital.
- Develop a system that allows you to monitor the use of antibiotics (selecting the drug, dose, route of administration, multiplicity, the number of courses), evaluate its results and based on their relevant recommendations, as well as concentrate resources for these purposes.
- Develop educational programs and conduct training aimed at improving the level of knowledge of the relevant medical personnel relating to: the results of the irrational use of antibiotics, the values \u200b\u200bof strict implementation of infectious control measures in cases of infections caused by poly-resistant bacteria strains and compliance general principles infectious control.
- Use an interdisciplinary approach to a strategic solution to the problem of antibiotic resistance.
According to the materials of the Infection Control Guide. Per. from English / Ed. R. Wentsell, T. Brevers, J.-P. Bootzler - Smolensk: McMa, 2003 - 272 p.
Reducing the effectiveness of antibiotic therapy for purulent infection is due to drug resistance of microorganisms. Antibiotic resistance of microorganisms is due to: 1) the duration of the course of antibiotic therapy; 2) irrational, without due testimony, the use of antibiotics; 3) the use of the drug in small doses; 4) short-term course of antibiotic therapy. Considerable importance in increasing the stability of microorganisms to antibiotics is uncontrolled by the use of antibiotics of patients, especially tableted drugs.
Simultaneously with the growth of antibiotic resistance, a microbial landscape change occurs. The main causative agent of the purulent surgical infection has become staphylococci, intestinal wand, protein. Often began to meet microbial associations. In the treatment of purulent processes caused by associations of microorganisms, the use of antibiotics is now a difficult task, as if one of the strains of the association is resistant to the antibiotics used, then in the treatment of microorganisms that are sensitive to them, and sustainable strains will actively multiply.
It has been established that the development rate and the degree of severity of antibiotic resistance depend on both the type of antibiotic and microorganisms. Therefore, before conducting antibiotic therapy, it is necessary to determine the sensitivity of microorganisms to antibiotics.
Currently, the most common method of determining the sensitivity of the microbial flora to antibiotics is the method paper disks. This method, as the most simple, uses most practical laboratories. Assessing the degree of sensitivity of the microbial flora to antibiotics is carried out in the zones of growth delay in accordance with the instructions for determining the sensitivity of microbes to antibiotics approved by antibiotic committees in 1955.
but this method It has a very serious disadvantage - usually takes 2-3 days, and even more days before the sensitivity of the microorganism to the antibiotic becomes known. This means that time to start using antibiotic therapy will be missed. That is why in clinical practice persistently seek ways to early determine the sensitivity of microorganisms to antibiotics. However, so far this method has not yet been developed. True, A.B. Chernomyrdik (1980) proposed an indicative method for the rapid purpose of antibiotics based on bacterioscopy separated from purulent wounds. At the same time, strokes painted in grams are viewed under the microscope. According to a specially developed table, the antibacterial drug is chosen according to the preparation in the preparation of the microorganism.
The fight against the adaptive ability of microorganisms to antibiotics, as well as with the antibiotic resistance of the strains of microorganisms, is rather difficult and carried out in three directions: 1) the use of large doses of antibiotics; 2) the identification of new antibacterial drugs, including antibiotics; 3) a combination of antibacterial drugs and antibiotics with different mechanism of action on a microbial cell, as well as a combination of antibiotics with others medicinal preparationshaving a specific impact on antibiotic resistance.
The use of large doses of antibiotics is not always possible due to the toxicity of some of them. In addition, the use of large doses of antibiotics is permissible only under the condition of the sensitivity of the microorganism to this antibiotic. In elevated doses, but not more than 2-3 times greater than therapeutic, drugs can be applied with minimal toxicity to the patient's body. At the same time, as evidenced by the data of American scientists, the use of high doses of antibiotics does not prevent the formation of antibiotic-systemic forms of microorganisms.
In our country, the struggle against the resistance of microorganisms to antibiotics is aimed at creating new antibacterial drugs, including antibiotics. In addition, more rational ways of administering antibiotics are being developed to create high concentrations in the patient's body.
Antibiotic-resistant microorganisms can be overcome by combined antibiotics purposes. In this case, it is necessary to take into account the nature of their interaction - it is unacceptable to use the combination of antibiotics, which mutually destroy each other's activity (antogonism of antibiotics). Knowing the possibility of interaction of antibiotics makes it possible to increase the effectiveness of antibacterial therapy, avoid complications and reduce the manifestation of the adaptive properties of microorganisms.