Candidial colishes of intestines Treatment once. Modern methods for the treatment of bowel candidiasis. Factors of antifungal resistance of the body
- Infectious damage to the digestive tract caused by the patient's own fungal fluor (Candida SPP.) Against the background of a significant weakening of immunity. Clinical manifestations of the bowls of the intestines vary depending on the shape of the disease: the discharge of the chair, an increased meteorism, vague abdominal pain, ulcerative colitis and fungal sepsis. The diagnosis is made on the basis of endoscopic research, histological and cultural analysis of biopsyats, feces. Treatment includes three main directions: the purpose of antimicotics, the normalization of the intestinal microflora and the correction of the patient's immune status.

General
The bowel candidosis is a fungal lesion of the mucous membrane of the digestive tract. It is an actual problem of modernity, since the diagnosis and determination of the criteria of this disease are complexity for many clinicians. It is connected with the widespread prevalence of mushrooms of the genus Candida, including in the body healthy people (Mushroom carriages of the genus Candida in the intestine is inherent in 80% of the population). Invasive bowel candidiasis is almost never occurring in people with a normally functioning immunity, almost always this opportunistic infection associated with the body's immune imbalance.
In addition, many specialists are quite difficult to differentiate transient candidias and non-invasive candidiasis of the intestine (it is precisely the vast majority of all clinical cases of candidosis of the digestive system). Distributing two of these states is possible only in the presence of modern diagnostic equipment. To establish the correct diagnosis, it is necessary to have three diagnostic criteria: identifying one or more risk factors, endoscopic signs of bowel candidiasis, positive result of culture research. Thus, the tactics of the appointment of antimicotics in the first detection in the crops of mushrooms of the genus Candida, without further surveys, is erroneous.
Causes of the Kandidosis of the intestine
The pathogenesis of the invasive candidide of the intestine is different. Subject to the weakening of the local and general immunity, the mushrooms of the genus Candida are intimate attached to the intestinal epithelium (they have tropiness to the flat multilayer epithelium), then embedded in its thickness, transforming into a nichtail shape. In the presence of pronounced suppression of cellular immunity, Candida penetrate the bloodstream and spread through the body, causing visceral candidiasis (liver, pancreas damage). The visceral form develops against the background of pronounced neutropenia (almost complete lack of neutrophilic leukocytes) and later stages of AIDS.
To form an intestine candidosis, you must have at least one of the predisposing factors: physiological decline Immunity (newborn period or elderly age, strong stress, pregnancy); congenital immunodeficiency (syndrome di george, nezelof, etc.); oncopathology, especially in the period of polychimotherapy; autoimmune and allergic diseases (exacerbates the oppression of immunity treatment with corticosteroid hormones); reception of immunosuppressants after organ transplantation; severe endocrine diseases; somatic pathology requiring intensive therapy; long-term treatment with antibacterial drugs of the backup series; primary immunodeficiency syndrome; severe nonbalance of nutrients in the diet (especially the lack of protein and vitamins). IN clinical practice Candidiasis of the intestine is more common, due to a combination of several of the listed factors.
Symptoms of the candidias of the intestine
Candidiasis of the intestine is found in three main clinical forms: invasive diffuse, invasive focal and non-invasive. The criteria for the diagnosis of invasive diffuse bowel candidiasis are heavy condition Patient Against the background of pronounced intoxication, increasing body temperature, severe abdominal pain, diarrhea, blend of blood in a chair, systemic manifestations of mikosa (lesion of liver, pancreas, spleen, gallbladder, etc.). If this form of the bowel candidia is a random find during a survey about other diseases, first of all should be thought of the debut of AIDS or diabetes mellitus. Invasive diffuse bowel candidiasis is not characteristic of people with a normally functioning immunity system.
Invasive focal bowls of the intestine can complicate the course of duodenal ulcer disease, nonspecific ulcerative colitis. It is possible to suspect this form of the candidiasis in patients with a stubborn and protracted flow of a background disease that cannot be standard therapy. For this purpose, the Mikosa is characterized by the local invasion of the nichly shape of Candida in the places of broken epithelialization (at the bottom of the intestinal ulcers). At the same time, in the surrounding tissues, other departments of the druz mushrooms are not detected. The clinical picture corresponds to the main disease, and the pseudomycelound is randomly detected in histological examination of biopsy.
Non-invasive bowel candidiasis is the most common form of this disease. This pathology is not associated with the penetration of mushrooms into the thickness of the intestinal wall, but is associated with the massive reproduction of Candida in the opening of the intestine. This distinguishes a huge amount of toxic metabolites, which provide both local and general resorbative effect. It has been established that non-invasive candidiasis is about a third of all cases of intestinal dysbiosis. Clinically non-invasive bowls of the intestine flows against the background of a satisfactory condition of the patient, is accompanied by moderate phenomena of intoxication, discomfort in the abdomen, meteorism, an unstable stool. Often, such patients are exacerbated by various allergic diseases. This form of candidias is often confused with irritable bowel syndrome.
Diagnosis of Kandidosis of the intestine
The diagnosis of the intestine candidia is hampered by the lack of typical clinical signs, as well as sufficiently specific and sensitive methods for identifying mushrooms of the genus Candida in samples of fabrics and feces. IN general Analysis The blood with severe forms of the disease is determined by a decrease in the number of leukocytes, lymphocytes, red blood cells. The consultation of an endoscopist doctor is required to select the optimal intestinal research method. During endoscopy, nonspecific signs of the lesion of the mucous member are usually found, therefore endoscopic biopsy and morphological study of bioptats are crucial in the diagnosis. Diagnostic difficulties are that mushroom pseudomytenes can be identified not in all material samples, so false-negative results are often found quite often. Visually, with diffuse invasive bowel candidiasis, the signs of ulcerative-necrotic damage to the mucous membrane are determined, and with non-invasive - catarrhal inflammation. The diagnostic criterion of the invasive candidiasis is the presence of candidal pseudomynecia in biopsies and fingerprints of the intestinal mucosa.
All patients with fungal lesions of the intestine necessarily conducts an analysis of the feces on dysbacteriosis, bacteriological examination of Kala. Most often, these analyzes identify a mixed flora: not only mushrooms of the genus Candida, but also an intestinal wand, Klebsiella, staphylococci, etc. The identification of more than 1000 colony-forming units per grams of pathological material testifies in favor of the intestinal candidosis and eliminates the carrier of fungal flora. The main task of cultural research is to establish the type of pathogen, determining the sensitivity of the selected microflora to antimicotics.
Treatment of the Kandidosis of the intestine
Consultation of the gastroenterologist with bowel candidyosis allows you to identify the risk factors for this disease, determine the amount of research. Since the bowls of the bowel does not have specific clinical signs, to suspect this pathology is quite difficult. In the presence of laboratory testimonials of the bowl of the intestine, the choice of treatment tactics depends on clinical option, the presence of concomitant pathology, tolerance of antimicotic drugs. Commitable areas of therapeutic process with bowel candidiasis are: correction of the background disease, which led to a decrease in immunity and activation of fungal flora; appointment of target antifungal agent; Immunity modulation.
Patients with diffuse invasive form of bowel candidiasis are hospitalized in the hospital. The selection drugs for invasive mycoses are azole antimicotics (ketoconazole, fluconazole, itraconazole, etc.), which are actively absorbed from the intestines and have a systematic action. Treatment is beginning usually with the introduction of amphotericin B, then go to therapy with fluconazole.
For eradication of fungal flora with non-invasive forms of bowel candidiasis use antifungal drugs Non-heavy action - they are poorly absorbed by the intestine mucous membrane and have a strong local action. Non-massive polyenov antimitics have a number of advantages - they have practically no side effectsThey do not oppress the normal intestinal microflora, do not cause addiction. Policians include Natamicin, Nystatin. Since in the pathogenesis of the non-invasive candidiasis, the condition of dysbiosis and mixed flora are important, antimicrobial drugs, eubiotics are prescribed. Digestive enzymes, sorbents, antispasmodics and analgesics are used as symptomatic treatment.
Forecast and prophylaxis of bowel candidiasis
With the diffuse invasive form of the intestine candidiasis, the forecast is serious, as it can lead to the generalization of the process. The forecast for invasive bowel candidiasis is significantly aggravated by the presence of heavy background diseases. With other variants of the disease, the forecast is favorable at timely early treatment.
The prevention of the intestinal candidia is to eliminate the factors predisposing to this pathology; The treatment of diseases of the digestive tract leading to dysbiosis. To maintain the normal intestinal microflora, it is necessary to eat diverse, limiting the content of simple carbohydrates, to use a sufficient amount of fiber. Patients included in the risk group for the development of bowel candidiasis (HIV, severe endocrine pathology, polychimotherapy, treatment with corticosteroid hormones, etc.), require close attention and regular surveys.
Candidiasis today is the most common fungal infection, the cause of which are yeast-like mushrooms of the genus Candida (Candida). The increase in the incidence of this mycosis (from the Greek ύύκης - mushroom) in recent decades is associated with the wide use of antibiotics and the increasing number of patients with immunodeficiency. The pathogens refer to the group of conditionally pathogenic microorganisms.
The frequency of the candidia is 25% in the oral cavity and 70 - 80% in the intestine. Holds the development of the disease. Human immune system. Under normal conditions, the amount of saprophite flora is negligible. In case of failures in the work of immunich, there is an excess increase in mushrooms. They affect mucous membranes, skin cover and internal organs. The most commonly registered cases and intestines. Of the digestive organs are also affected by the same esophagus, stomach, straight intestine, biliary roads and pancreas.
Microorganisms are widespread in nature. They are found in drinking water, soil, food products. They live on the skin of animals and human mucous membranes. Of the 200 biological species of yeast-like mushrooms of the genus Candida danger to a person represent 10 species, of which about 87% fall on Candida Albicans.
Fig. 1. Mushrooms genus Candida: rounded shape (photo on the left), micellar form (photo on the right).
Factors of virulence of pathogens
The development of the bowel candidiasis, esophagus and the stomach contributes to the special properties of pathogens:
- The mushrooms of the genus Candida have the ability to attach to the cells of the mucous membrane and beyond, transforming into a filamental form (mycelium formation), are introduced into the mucous membrane (invasion), causing tissue necrosis due to the secretion of such enzymes as aspartilproteinase and phospholipase. Adhesion and education Pseudomycelium are the main factors of Candida virulence.
- The enzymes of protease and glycosidase pathogens are intensively splitting mucin (mucopolisaccharides of mucus), protecting the mucous membrane, stomach and intestines from aggressive external factors.
- Intravidaya variability contributes to the development of sustainability in the microorganisms to negative factors of the external environment, including antifungal drugs.
Factors of antifungal resistance of the body
Candid's virulence factors The human body opposes its protective forces:
- The formation of mucopolysaccharides (mucin, mucus), the production of lysozyme, complement, secretory IgA, transferin, lactoferine, acids and enzymes, the ability to regenerate the mucous membrane, maintaining normal microbiota (intestinal microflora), peristaltic activity.
- The state of cellular immunity phagocytic series - natural killers, polymorphoid leukocytes and mononuclear phagocytes, antifungal humoral response (synthesis in cells of specific immunoglobulins, inactivating enzymes and endotoxins of fungi), and complex interaction of dendritic cells with T-helpers and T-regulatory cells .
- Limiting the growth of Candida by bacteria symbiontes (bifidobacteria, lactobacilli, enterococci,).
- Normal microflora The gastrointestinal tract produces substances that impede the introduction of pathogenic microorganisms into the mucous membrane.
Factors contributing to the development of candidiasis
- Physiological immunodeficiencies (pregnancy, children and senile age, long-term stressful situations).
- Primary immunodeficiency (congenital).
- Oncological diseases and AIDS.
- Receiving glucocorticoids, cytostatics, radiation therapy.
- Reception of contraceptives containing a large number of estrogen.
- Diseases of the endocrine system (decompensated diabetes, obesity, hypothyroidism, etc.).
- Dysbiosis caused by prolonged antibiotic therapy.
- Chronic diseases depleting the patient.
- Injuries, operations, long-term stress - everything that strikes immunity.
Defects in the system of antifungal immunity - the main factor contributing to the development of the candidiasis in humans.

Fig. 2. Mycelium Candid on the surface of the mucous membrane forms a powerful frame - biofilm. The process is accompanied by the destruction of the mucous membarus with the formation of erosion and ulcers.
Classification of candidiasis of digestive organs
- Candidiasis Oro-Faringeal (oral and pharynx cavities): Saint, Haylit, Gingivit, Stomatitis, Faringitis, Glossite.
- Candidiasis of the esophagus (without erosion and with erosions).
- Stomach Candidiasis:
- Erosive-fibrinous (diffuse).
- Focal (secondary stomach ulcers).
- Intestine Candidiasis:
- Invasive diffuse.
- Non-invasive.
- Focal (secondary ulcers of the 12th and rosysome intestine).
- Ano-rectal candidiasis:
- Candidose proctusigmit.
- Invasive edge of the rectum.
- Candidal dermatitis of the perianal area.

Fig. 3. On the photo yeast-like mushrooms Candida Albicans under a microscope. Nights of pseudomitia, chlamyido and blastospore are clearly visible.
Diagnosis of the disease
Diagnosis of the bowel candidiasis, esophagus, stomach and other digestive organs is based on the clinical picture of the disease, identifying risk factors and data of laboratory research methods.
Anamnesis of the disease
A thorough study of the patient's complaints and the history of his disease and life will reveal the belonging of the patient to risk groups. "Random" detection of fungal infection serves as a reason for finding such background factors. Often, candidiasis is manifested first in the development of diseases accompanied by immunodeficiency.
Microscopy of native preparations
Detection of the pseudomycelination of the tensile cells of pathogens in the scraps with mucous membranes, urine sediment, feces or sputum, strokes-fingerprints from the bottom of ulcers with microscopy - "Standard" of the diagnosis of mikosa.

Fig. 4. Candida Albicans under a microscope: rounded cells and pseudomitia threads.
Methods of quick identification
The method of rapid identification of Candida Albicans is widely applied. The microorganisms of this species are capable of forming short threads of mycelium and spike tubes for 2 to 4 hours with growth on nutrient media at a temperature of + 37 ° C.
Cultural research
Cultural research is carried out in order to identify the causes of the disease, determining the quantitative assessment of pathogens, their species and sensitivity to antifungal drugs. To carry out this study, washts from the mucous membrane of the oral cavity and the esophagus, the contents of the stomach and intestines, raids, films, bile, obtained with duodenal sounding are used.
Interpretation of some research results:
- In persons with a normal immunity, the detection of single colonies Candida is not a reason for the diagnosis of Candidiasis.
- Diagnostically significant is the number of colonies more than 10 5.
- In persons S. low level Immunity is meaningful to lower diagnostically level.
- In some cases, when defeating the intestine, the discovery of candida in feces may be the only sign of the disease.

Fig. 5. In the photo on the left, the growth of the colonies of Candida Albicans on the nutrient medium. In the photo on the right view of the colony of a mushroom with nitchable cells on top.
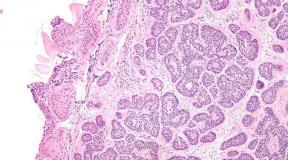
Histological examination
Histological and cytological examination of bioptats make it possible to identify tissue forms of pathogens.
Analysis of the feces on the microflora of the large intestine
In the case of non-invasive bowel candidiasis and when there is no biopsy material, the diagnostic standard is the growth of Candida mushrooms of more than 10 4 core / g. Increasing this level indicates a reduction in immune defense, long-term intake of antibiotics or food eating with large content Carbohydrates.

Fig. 6. Excessive growth of Candida Albicans in intestinal content.
Other laboratory research methods
An immununimenal analysis of fecal antigens and PCR has practical importance.
Endoscopic research methods
Endoscopic examination of the esophagus, stomach and 12 and rosewood allows you to reveal the phenomena of inflammation of the mucous membrane and the presence of cheesome-colored raids, take a piece of material for the study. Modern methods of video and colonoscopy (the study of the large intestine) allow you to explore the organ under conditions, comfortable for the patient - against the background of the "medicinal" sleep.
X-ray study
X-ray study allows you to identify defects in the contours of the mucous membranes, the size of the edible tubes and the depth of the peristalsis.
Detection of the pseudomycelia of yeast-like fungi - "Standard" of the diagnosis of the disease.

Fig. 7. Candida Albicans under a microscope.
Candidiasis of intestines: symptoms, treatment, diet
Among all types of candidiasis, the intestinal defeat occupies a leading place. The disease is due to a decrease in the protective forces of the body and the wide use of antibacterial drugs wide spectrum actions. The infection is often called "patient disease" or "disease from treatment".
How the disease is developing
Distinguish invasive and non-invasive forms of the disease. In the invasive form of the mushrooms, the mucosa layer of the intestine is germinated, with non-invasive - develop in the lumen of the intestine.
Invasive form
With invasive candidiasis, the candids stick together with the epithelial cells of the intestine, form growth (pseudomycene) of the nichlya shape, the epithelial layer gripe and penetrate the limits of the baseal membrane. Next, the causative agents fall into the lymphatic system and with blood is spread throughout the body. So develops systemic candidiasis with the damage to the internal organs.
The disease is developing in the digestion organs, the inner wall of which is lined with a multi-layer flat (more often) and cylindrical (less often) epithelium. More often, the disease occurs in the oral cavity and the esophagus, less often - the stomach and intestines. Erosive-ulceous intestinal wall defects have different shape and sizes. Cracks, membrane impositions and polypovoid formations appear.

Fig. 8. In the active phase of the candida form pseudomytelas, germinating through the intestinal mucosa.
Non-invasive form
With the non-invasive form of candidiasis, mushroom cells do not form pseudomytenesses and the mucosal layer of the intestine does not gem. They reproduce hard in the enlightenment of the organ, breaking the honest and ridicule digestion. Microbial components and metabolites depress the normal microflora, penetrating into the blood, they lead to the development of systemic immuno-inflammatory reactions and allergic rebuilding of the body.
The bulk of the yeast-like mushrooms of the genus Candida is localized in the intestine of a person. The extraordinary localization of Mikosa (oral cavity, genitals and internal organs) is a manifestation of a systemic candidiasis, the beginning of which in most cases is the defeat of the intestine.
Signs and symptoms of bowel candidiasis
Symptoms of bowel candidiasis depend on the form of the disease, level and degree of damage.
- Abdominal discomfort is a symptom of the bowel candidiasis. The patient is disturbed by pain spastic nature, bowelism (flatulence), blood and mucus can be present in feces.
- The frequency and consistency of the chair changes. In the feces are detected in a large amount of yeast-like mushrooms of the genus Candida.
- The permanent symptom of the intestinal candidia is flagged - the release of digestive gases with the sound of varying degrees of volume and the fettered odor.
- Inxication for the disease moderate.
- The body sensitization is characterized by signs of allergies of different localization and degree of severity.
Signs and symptoms of bowel candidiasis (diffuse invasive form)
The diffuse invasive form of the intestinal candidation takes place by the type of enterocolitis. Patients are disturbed by spastic pain, the intestine swelling, blood and mucus can be present in feces, often appear signs of the Candidosis of the mucous membranes of the oral cavity and genital organs. Moderate fever. Changes in the intestines with fibrinous-ulcer endoscopy. Sometimes the disease proceeds by the type of non-specific ulcerative colitis or ulcerative disease of the 12th and rosis. In some cases, the perianal dermatitis develops. Treatment with antifungal drugs gives a positive result.
Signs and symptoms of bowel candidiasis (non-invasive form)
The non-invasive form of the intestinal candidation proceeds with pain in the abdomen and oxidation of the intestine, the gases are stencil, stand out with sound, the chair is not decorated. Treatment with antifungal drugs gives a positive result.

Fig. 9. In the photo of the bowl of the bowel. The arrows are "Curled" type of imposition.
Complications of the candidias of the intestine
- With long-term flow of candidation, an allergic rearrangement of the body occurs, which is characterized by the appearance of urticaria, itching the skin, allergic vasculitis or fungal eczema.
- In severe forms, invasive bowls of the intestine is complicated by the spinning of ulcers and bleeding.
- In case of causative agents, candidal sepsis occurs in the vascular bed. From parenchymal organs are amazed gall-bubble and liver, pancreas, which is often observed in patients with AIDS.
- The systemic nature of Mikosa says simultaneous defeat of the oral cavity and / or genital organs.
Mortality in invasive bowel candidia reaches 25 - 55%. In patients after transplantation and sharp leukemia, invasive forms of mikoz are the main causes of death.

Fig. 10. In some cases, the bowel candid mind proceeds along the type of fibrinous-ulcerative colitis.
Treatment of the Kandidosis of the intestine
The treatment of intestinal candidation is directed to the effective destruction of pathogens and all the links of the pathological process. It is necessary to identify and eliminate factors contributing to the development of Mikosa. In the process of treatment, patients must comply with a strict diet and abandon bad habits.
Treatment of intestinal candidiasis by antifungal drugs
In the treatment of candidation, antifungal drugs are used, non-surveying from the intestinal lumen, since the healing effect is not observed without suppressing growth, or it turns out to be unstable and short-term. Fluucanazole, ketoconazole, intracocole and amphotericin are completely absorbed in the upper gastrointestinal tract and do not reach the level of the ileum, where the main population of mushrooms of the genus Candida focuses.
The group of antifungal drugs that are not absorbed from the intestinal lumen includes Nystatin, Lev Room and Natamicin (Pimafucin). Nystatin and Lev Room Possess a large number of side effects: dyspepsia, toxic hepatitis, allergies, etc.
Pimafucin It is an antifungal preparation of a wide range of a group of polyenov antibiotics. Under its effect, the integrity and function of cell membranes are disturbed, which leads to the death of pathogens. At the beginning of treatment, patients appear nausea and diarrhea, which independently pass without cancellation of the drug. Pregnancy and breastfeeding are not contraindicated. Data influence on the fruit is not received.
The main criteria for the effectiveness of treatment are:
- Disappearance clinical manifestations Diseases.
- Normalization of the number of colonies Candid under the condition of adequate analysis of the analysis.
In some cases to obtain necessary effect Resort to re-courses of treatment.

Fig. 11. Under the influence of antifungal drugs, the mushroom envelope becomes porous, "holes". The contents of the cell flows to the surface of mycelium.
Pathogenetic treatment of candidias
Comprehensive treatment of methods should be directed to the correction of the patient's immune status, a decrease in the body sensitization and the restoration of intestinal biocenosis, which will significantly increase the effectiveness of treatment.
- In order to reduce the body sensitization, the patients are recommended to receive antiallergic means of a new generation.
- In order to replace the loss of vitamins and trace elements (including iron), reception Ferroglobolina B12,which includes group vitamins in (B1, B2, B3, B6 and B12), folic and pantothenic acid, vitamin C, iron ammonium citrate, calcium gliderophosphate, zinc, copper, manganese, iodine, lysine, licorice root extract and honey.
- Restoration of intestinal microbiocenosis.
The restoration of intestinal microbiocenosis should be held in two directions:
- Fighting a conditioned pathogenic flora (reception of antibiotics, intestoopan, meks form, eating products with bactericidal action).
- For the normalization of intestinal flora, it is recommended to receive preparations containing live lacto, bifido- and other types of bacteria: Linex, Acipol, Hilak Forte, Bifti-Form, Biofibumba Katerina, Bakusubtil, Lactobacterina, Acilact, Lactomeola, Profitor, Bicyca.
Bad to food Bacytatin It is an indispensable multicomponent drug in the treatment of candidiasis:
- Metabolites Bacillus subtilis Inhibit the conditionally pathogenic and pathogenic intestinal microflora, contribute to full digestion, increase the protective forces of the body by stimulating the synthesis of interferon.
- Zeolite is a natural sorbent. Selectively sorbitis and removes allergens and toxins, thereby contributes to a decrease in different species toxicosis. With its effect, the intestinal peristalsis is normalized, bloating and spastic phenomena decrease.
- Hydrolyzate of soy flour It is a prebiotic component. It contributes to the growth and.
- Preparations, overwhelming fermentation processes ( Carbollen.- activated carbon) and normalizing digestion ( Pepsidide, gastric juice, acidine-pepsin, magnesium sulfate, enzyme preparations).
- With a low hemoglobin content in the blood, iron preparations are used: Ferroplex, iron lactate, iron gliderophosphate, hemostimulin.
- In order to combat hypoproteinemia to normalize nitrogenous exchange, anabolic steroids are prescribed: Inosine, Nandrolon, ORTISTIC Acid, Methyluracil and etc.
- With proven functional and quantitative insufficiency of T- and B-cellular immunity, immunomodulators are assigned: Nucleicate Sodium, Splenin, Tabuti, Arbidol, Levamizol, Splenin, Methyluracyland etc.
- In order to correct humoral immunity, immunoglobulin of a person, Gamma-Globulin, etc. applies.
Diet with bowel candidiasis
- Yeast-like mushrooms of the genus Candida prefer to dwell in the tissues rich in the inner sugar - glycogen. In order to reduce the processes of fermentation and the control of the dyskinesia of the gastrointestinal tract, it is recommended to limit the use of the daily rate of sugar and products containing a large amount of carbohydrates. Not recommended for sweetness, pastry, pastries, white bread, Pasta, sweet drinks, beer and kvass, potatoes, beets and corn, grapes, bananas and other sweet fruits.
- Allowed to use: low-fat varieties of meat in stewed, boiled or baked form, chicken boiled eggs and omelet, vegetable oils, dairy products, from vegetables - cucumbers and tomatoes, from croup - buckwheat and rice, from berries - currants, lingonberries and cranberries in the form of horses, from drinks - herbal champs, pomegranate or carrot juice, rugg of rosehip, green tea, drink with lemon without sugar.
Highly efficient antifungal drug, anti-inflammatory, connotatory and immunomodulatory products, correction of related diseases - the basis of the treatment of candidiasis of the digestive tract.

Fig. 12. Candida albicans yeast-like mushrooms under a microscope: the rounded cells of pathogens and fragments of the pseudomitelines are visible.
Food Candidiasis: Symptoms and Treatment
Candidiasis of the esophagus is rare (in 1.3% - 2.8% of patients), mainly in persons with reduced immunity, in 4% of patients after transplantation, in 3-6.7% of patients with disseminated carcinomatysis, each third AIDS patient It is often observed in patients with dysfunction of adrenal glands and parachitoid glands, in 5 - 10% of patients with diabetes. The main risk factors for the development of the candidias of the esophagus are burns, polyposis and diverticulosis.
Classification
Candidial esophagitis can flow without erosion and erosions. Morphologically distinguish between 3 severity of Mikosa:
- With the 1st degree of gravity on the mucosa of the esophagus there are separate raids of gray-white coloring. Pseudomycelions of mushrooms sprout the epithelial layer.
- With a 2nd degree of severity, the flavored raids, the places merge, forming extensive areas. The threads of mycelium sprout the mucous and submucosal layer.
- With a 3rd degree of gravity, pseudommable impositions are extensive. The threads of mycelium germinate into the muscular layer.
How does esophagus candidation develop
Sticking with the cells of the mucous membrane of the esophagus and not receiving proper essay by immune system, Candids begin to form pseudomiters and germinate through the mucous layer. Under the effects of enzymes of causative agents, the cells of the mucosa are destroyed. Sewage epithelium and fungal bodies form on the surface of the raids having a gray-white color. Initially, these are small whitic chambers, which over time merge and form dense raids - films. In some cases of film species raids, so much that they completely overlap the clearance of the esophagus. In patients with immunodeficiency, ulcers appear, it often occurs perforation (run) walls and bleeding. Phlegmosic inflammation of the esophagus and the mediastinum becomes the cause of the death of patients. At microscopy, pseudomytelines and ticking cells of pathogens are detected.

Fig. 13. The formation of mycelium on the surface of the mucous membrane. On the photo on the right, the pseudomycelium is visible and the chlamydospore rounded shape is the bodies of blessing reproduction. The process is accompanied by the destruction of the mucous membrane, followed by erosion and ulcers formations.
Symptoms of candidiasis of the esophagus
On the basis of the endoscopic pattern, 4 types of disease flow are isolated - from light to severe, complicated. Candidiasis of the esophagus during latent flow can proceed asymptomatic.
The main symptoms of the candidiasis of the esophagus are dysphagia (unpleasant sensations when swallowing), pain (identifiagia), in some cases of salivation (hypersession). Pain when swallowing a different intensity, sometimes the inability to swallow food. In vomiting, the formation of a film species is distinguished. Dysphagia occurs in 70% of cases, the defeat of the oral cavity is 45%, nausea and vomiting - 15%, weight loss - 8%, diarrhea - 2%, there are no third patients with the symptoms of the candidosis of the esophagus. Heartburn and liquid chair rarely occur.
Complications of the candidiasis of the esophagus:
- Inability to swallow liquid food leads to dehydration of the body.
- Split wall (perforation).
- Bleeding with the subsequent development of anemia.
- Development of stricture (narrowing) of the esophagus.
- The dissemination of fungal lesion with the damage to the internal organs.
- Candidal sepsis.
- Phlegmosic inflammation of the esophagus and the mediastinum becomes the cause of the death of patients.

Fig. 14. Hypersalevation (photo on the left), swelling, hyperemia of the mucous membrane and "curly" raids are the main symptoms of the candidiasis of the esophagus.
Diagnosis of candidiasis of the esophagus
The survey on the candidation of the esophagus should be carried out by all patients with risk factors in their occurrence of unpleasant sensations and pain when swallowing. Confirms the diagnosis of candidal stomatitis in patients, but in the absence of the esophageal damage is also not excluded.
Microscopy of native malas
The discovery of the pseudomycelia is a "standard" diagnosis of candidiasis of mucous membranes. Mushroom cells are detected both in case of disease and under candidia.
Detection of pathogens is carried out by cytological (study of native smears) and histological (study of biopsy material) methods. Analysis of scrapets is the most reliable.
Cultural method
Sowing biomaterial allows you to identify the cause of the disease, give a quantitative assessment of pathogens, determine the species affiliation of mushrooms and sensitivity to antifungal drugs, monitor the effectiveness of treatment. The disadvantages of the culture method is the inability to differentiate candidiasis from the candidia.
Seric and skin tests
Serological studies (ELISA, definition of specific IgE, etc.) and skin tests in practice are rarely applied due to the lack of required accuracy.
Fast diagnosis of esophagus candidiasis
Fast diagnosis of esophageal diseases are carried out using a cytological brush and balloon catheter. Tools for the fence of the material are introduced through the nose or mouth. The material obtained is investigated cytologically and culturely. The sensitivity of the method is significantly higher than histological examination of biopsies obtained during endoscopy, since mushrooms can be washed from the surface of the mucous layer during the processing of the material obtained.

Fig. 15. Candidiasis of the esophagus. Microscopy of the contents of esophageal ulcers. Pseudomycelical threads are clearly visible and candidy cells.
Endoscopic examination of the esophagus
This type of esophageal study allows you to visually assess the picture of inflammation and make a fence of the material to the study. The disadvantages are the preparation of a miniature fragment of the tissue using biopsy forceps, which significantly reduces the likelihood of detection necessary for the diagnosis of information, so one-time biopsy is not enough to confirm the diagnosis.
The main endoscopic signs of the candidation of the esophagus are hyperemia of the mucous membrane, an increased vanity upon contact, fibrinic plates of different localization, sizes and configurations.
- With catarrial candidium esophagitis, diffuse hyperemia of varying degrees of severity, the edema of the mucous membrane is moderate. In contact, there is an increased bleeding.
- With fibrinous candidium esophagitis against the background of elaborate and hyperemic mucous membrane, gray-white or yellowish color loose rounded shape 1 - 5 mm in diameter are marked. In contact, there is an increased bleeding.
- With fibrin-erosive candidium esophagite, the rains of dirty gray, "fringe", tanning, are located on the ridges of longitudinal folds. The mucous membrane is echoing and hyperemic. In contact, there is an increased bleeding.

Fig. 16. Endoscopic pattern of the candidiasis of the esophagus.
Histological examination
Only histological examination biological material Allows you to identify pseudomitis, penetrated into the depth of the wall of the esophagus.
X-ray method
The X-ray method of the esophagus study is inffective, but it can be identified with the complications of the disease - stricture, ulcers, perforation.
Treatment of candidias of esophageal
The treatment of candidiasis of the esophagus complex. The first search, identification and correction of background diseases is carried out. Medical therapy implies the use of antifungal drugs, immunocorrects, pathogenetic and symptomatic means.
Antimiotics are prescribed mainly in tablet form. Intravenous administration is used in the case of the stability of the candidiasis to traditional treatment and inability to swallow. Local therapy is not held.
In the candidation of the esophagus apply:
- Triazoles (azole compounds) (Flukonazole, Iratenazole.). Medicines containing Fluconazole.are "gold standard" in the treatment of patients with candidiasis. They penetrate well into the bloodstream.
- Derivatives of imidazole (Miconazole Ketoconazole, isokonazole, omoconazole, clotrimazole, econazole, bifonazole, oxyconazole, butoconazole, sectomaconazole (imidazole + benzothiophene).
- Group of polyenov antibiotics (Nystatin, Lev Room, Natamycin, Amphotericin and Pimafucin). Not absorbed from the intestinal lumen.
- Echinocandines (Kaspofungn, Anidulafungin, Mikafungin).
Preparations of the first line include Fluconazole., Ketokonazole. and Inrambonezole..
Medicines containing Fluconazole.are "gold standard" in the treatment of candidiasis of the esophagus. They penetrate well in the bloodstream, exceeding efficiency Ketokonazole. and Inrambonezole..
The second line drugs include: Ketoconazole, intrambonezole, amphotericin, capsofungin, voriconazole, plinazole.
With the development of resistance to antifungal drugs, the treatment diagram changes:
- In the treatment of azoles ( Flukonazol) It is necessary to increase the dose of the drug. If ineffectiveness go to the reception of another drug of this group - Inraconazolewhich is appointed in a higher dosage.
- With the ineffectiveness of high dose Flukonazola. (400 mg daily) go to intravenous administration Amphotericin B.. Resistance to this drug is rarely observed.
The treatment of the candidosis of the esophagus is carried out only for its intended purpose and under the supervision of the doctor.
Stomach Candidiasis
The fungal infection of the stomach in the absence of damage to the wall of the organ is rarely evolving. Among all types of specific lesions of the gastrointestinal tract, candidiasis of the stomach is 5.2%. In chronic gastritis and in biopsies, the ulcer of the stomach and the 12th and rosary of the gut, yeast-like mushrooms are found at 17 - 30% of cases.
The stomach candidosis is erosive-fibrinous (diffuse) or focal (secondary stomach ulcers). Candidation is often common in patients with ulcerative and gastroesophaginal reflux diseases. The pathogens are intensively multiplied against the background of a decrease or absence of hydrochloric acid in the gastric juice (ahlorohydria), especially in the zones of the mystery and damage (erosion) of the mucous membrane. As a result, ulcers and erosion do not survive for a long time, and the germination of mushrooms in the submucoscent layer causes pain and bleeding.
Endoscopic study of the stomach and 12 and rosysome intestine allows you to reveal the phenomena of inflammation of the mucous membrane, the presence of cheesome colors raids, take a piece of material for the study. Reliable confirmation of the diagnosis is based on the identification of pseudomitia Candid in cytological and / or histological preparations.
In recent years, mushrooms of the genus Candida in the Association with Helicobacter pylori.. It has been established that anti-sized therapy contributes to an increase in the frequency of the candidiasis, and in the presence of mushrooms of the disease of the stomach occur.
Treatment in such cases should be carried out with antibacterial together with antifungal drugs.
Diffuse stomach candidiasis
The diffuse loss of the stomach develops against the background of hypochlorohydria, after surgery and burns. When endoscopy, signs of fibrin-ulcery gastritis are detected, pseudomitia threads are revealed in print strokes. In the treatment, fluconazole 200 mg per day for 10 to 14 days or the drug amphotericin V.
Focal candidiasis stomach
Focal (limited) lesion of the stomach (cantidosis of ulcers) develops against the background of the ulcerative disease of the stomach or 12 and rosis. Ulcers, as a rule, are of large sizes, prone to bleeding, tolerant to traditional treatment. Inhibitory and strokes, invasive pseudomytelines are found in biopsyty. Fluconazole is a drug selection, applied at a dose of 200 mg per day for 10 to 14 days.

Fig. 17. The ulcer of the stomach (photo from the left) and the 12th and rosary (photo on the right, indicated by arrows).
Candidosis of the pancreas
It has been proven that the mushrooms of the genus Candida affect the pancreas to the same extent as other organs. The disease causes development sugar diabetesIt has been proven to obtain positive dynamics when appointing antifungal drugs.
Candidiasis of the biliary system
Candida genus mushrooms are able to hit the gallbladder and biliary ducts. This contributes to the dyskinesia of biliary tract, cholestasis, giardiasis, pancreas disease, gallbladder hypotension and other types of pathology. At the same time, conditions are conducive to the development of pathogens. Stones B. bile durses become "reservoirs" of mushrooms. A number of authors call them "candidoid stones."
Lab diagnostics is based on a microbiological study of bile portions obtained with duodenal multi-scale sensing.
In the treatment of antifungal drugs are prescribed Nystatin, Mikogeptin, Lev Room, choleretic and antimicrobial preparations. Supplement treatment physiotherapy procedures. In the diet should include products rich in proteins, bread from coarse grinding flour, fermented milk products, lemonade and fruit juices. It should limit products with a large amount of carbohydrates. Food fractional, small portions 5 - 6 times a day.

Fig. 18. Anorectal candidiasis.
Ano-rectal candidiasis
The defeat of the ano-rectal area of \u200b\u200bthe mushrooms of the genus Candida occurs due to the introduction into the intestinal wall of the pseudomitsis of pathogens. The micaosis develops against the background of a decrease in the work of the immune system, is a consequence of the bowel candy. Often, the skin covers of the perianal area are involved in the pathological process.
Candidosis of the rectum
Candidiasis of the rectum is often developing in patients with AIDS, homosexuals and as a mixture infection during herpes lesion, processes the type of proctitis. Pain in the field of rectum, false calls for the act of defecation, blood impurities and mucus in feces are the main symptoms of the disease. With rectoroscopy on the background of edema and hyperemia of the mucous membrane, red nipples and granulation are visible, increased bleeding. In severe flow, ulcers appear, the process extends to the crotch area and external genitals. Often, bipolar lesions are observed - thrush in the mouth and rectum. Anorectal candidiasis flows for a long time, heavily treatable.
The diagnosis is established on the basis of the detection in the brine-fingerprints of the pseudomitsis of mushrooms. When treating is applied Fluconazole. 200 mg per day for 14 - 20 days, from the preparations of the second row - Inrambonezole. and Ketoconazole.Additionally, local treatment is carried out using candles with Nistato and Levier, microclism with water gloss Lev Room0.02% of methylene blue solution.
Perianal candidal dermatitis
The damage to the skin of the perianal area proceeds with complaints to itching and burning. The act of defecation becomes painful, cracks and bleeding appear. In viewing there is hyperemia, numerous erosion and folliculites.
The diagnosis is established on the basis of the discovery of the pseudomycelia Candad in the scales of the skin. In the treatment, antifungal drugs are used in the form of cream and ointment for outdoor use with Clotrimazole. Outflows and creams apply from the preparations of the second row Lowords or Exoderil. With a strong itching, antimiotics with hormones are used.

Fig. 19. In the photo, the perianal candidal dermatitis.
Articles section "Candidoz (thrush)"Most popularNowadays, in addition to the many pathogens of serious infections, previously not known and intensity of increasing the impact on the human body of external factors (terrifying ecology, chemistry present in cosmetic products, emulsifiers, dyes, stabilizers in food), all this undermines our immune system The body and causes immunosuppressive states. The effects of mushrooms of the genus Candida causes human pathological conditions in humans, which relate to the category of micoses of opportunistic.
Characteristics of the causative agent of Kandidose
Candida - yeast mushrooms that are a relative ascomycetes. The genus candidates a variety of views. The main value as a causative agent of candidiasis, present: Candidaalbicans, Candidatropicalis, Candidaparapsilosis, Candidaglabrata, Candidadybliniensis, CandidalySitaniae, Candidakrysei. Microflora component represents Candidaspp. In a small part of the population that does not have clinical signs of fungal defeat, sometimes Candidaspp. We are found in the oral cavity and half of the population in the content of the intestine, and in the detritus of gastroduodenal ulcers - in 17% of patients.
Under normal conditions, Candidaspp. Inhabit the intestines, and the population of them is negligible. Growing colonies Candidaspp. In the human body is regulated by immunity, as well as intestinal bacteria. Healthy intestinal microflora produces antibacterial activity substances that prevent the reproduction and introduction of pathogenic organisms. Intestinal wands (bifidobacteria, lactobacillia and enterococci) have antogonistic properties.
Candidiasis implies a pathological process where the excessive growth of Candida is based on the basis: at the beginning in gastrointestinaland then in other areas. Candida has adhesion to epithelial cells. Attaching the mucous membrane, the conditions for the further invasion of the microorganism in the tissue are created. The protective barrier in this situation is Muzin glycoprotein of the cell wall of the epithelium cells.
Factors of Development of Candidoza
Factors preceding the development of candidiasis of digestive organs:
- Immunodeficiency physiological (pregnancy, stressful states, early children's period).
- Immunodeficiency congenital (syndrome of Neetheof, Sediakhahigashi, Di. Georgie, etc.).
- Human immunodeficiency (infection with a virus in the terminal stage) is a syndrome acquired immunodeficiency.
- Oncological diseases, at the same time (chemotherapy malignant tumors; Development of candidiasis against the background of antitumor therapy). It is believed that when carrying out chemotherapy, the percentage of fungal microorganisms increases.
- Allergic I. autoimmune diseases (Purpose of glucocorticosteroids).
- Organ transplantation (after transplantation The use of immunosuppressants).
- Endocrinopathy (decompensated diabetes mellitus).
- Diseases (anemia, cirrhosis of the liver, hepatitis, chronic infections, shock states, etc.). Disruption of digestibility of food and suction leads to an increase in microorganisms in the lumen of the intestine.
- Antibiotics therapy. It leads to a violation of the equilibrium of the microbial biocenosis of the intestine, which is why the excessive development of the candidomic population is possible. Almost a third of cases, idiopathic antibiotic-associated diarrhea, due to candidiasis of the intestine.
- Unbalanced nutrition (lack of vitamins and proteins).
Types of Kishini Candida
Two different mechanism of the pathogenesis of the edge of digestive organs are isolated: invasive and non-invasive.
Invasive candidiasis. This species is due to the introduction of Candida in fabric. The first stage is infectious (serves adhesion to epithelialocytes), and after invasion in the epithelial layer and beyond the basement membrane. These manifestations are characterized by the formation of erosions, cracks, membrane overlays, polypovoid and circular. With progressive invasion, systemic candidiasis can develop with damage to the mucous membranes and other organs. In the artistic forms of the candidiasis in the ducts lymph nodes We detect huge multi-core cells that contain mushrooms. Candidiasis invasive often detect in the oral cavity, esophagus and less often in the stomach and intestines.
Non-invasive candidiasis. This species does not turn the fungus into a nichtail shape. Excessive growth of colonies is observed in the lumen of the intestinal body. It is believed that this is the result of the reaction of inflammation of the immune system. Candidiasis of mucous localities outside the intestines, serves as a manifestation of translocation of fungi from the intestine, where their main mass is located. Extra case candidiasis (oral or genital) is a manifestation of a systemic candidiasis that originates from the intestine.
Classification of candidiasis of digestive organs
- Orofaring towed candidiasis (Gingivitis, Glossite, Haleit, Farriage and Stomatitis).
- Candidiasis of the esophaw (Stricks and complications for bleeding).
- Stomach Candidiasis:
- diffuse (erosisinochibrinic gastritis);
- focal (secondary in the ulcer of the stomach).
- :
- invasive (diffuse);
- focal (secondary for ulcers of the 12-rosewoman and with ulcerative colitis (nonspecific));
- non-invasive (a huge growth of the intestines).
- Candidiasis anorectal:
- candidosis of the rectum (invasive);
- candidal dermatitis (perianal).
Clinical picture
Features of the course of the bowl of the intestines are not well understood. Clinical manifestations of the bowel candidiasis are different and depend on the level of lesion.
Diffuse invasive candidiasis. In this case, enterocolite is manifested: pain in the abdomen, flatulence, the presence of mucus and blood in the chair. There are also signs of system candidiasis (lesion of genital and mucous membranes of the oral cavity).
Invasive focal candidiasis. Reminds the course of ulcerative disease of the 12-pans, or nonspecific ulcerative colitis.
With non-invasive bowel candidiasis such complaints:
- unformed chair;
- discomfort in the stomach;
- meteorism (treated with antimicotic drugs).
With invasive Candidiasis of the rectum such complaints:
- symptoms of proctitis (pain, pathological impurities in feces;
- sometimes there is a phenomenon of perianal candididermit.
Complications of disease
The complication of this disease is the development of intestinal perforation, penetration of ulcers into organs that surround it, bleeding and even the development of fungal sepsis. The defeat of parenchymal organs (gallbladder, liver, pancreas) accompanies neurophenia and visible in the terminal phase of AIDS.
Mortality in invasive type candidiasis reaches 25-55%.
Diagnostics

Diagnosis with bowel candidiasis is very important. It is important to distinguish the candidyosis and an infectious process caused by Candida. To increase the sensitivity of morphological and culture methods of diagnostics, it is recommended to explore several bioptats of the mucous membrane.
Biopcated fabric is collected in two sterile Petri dishes. One is investigated for histological studies, and the other is for microscopic. The material should be delivered no later than an hour after taking during storage (room temperature) for no more than three hours. An examination under the microscope must be carried out in painted native drugs. In the diagnosis of any form of candidiasis digestive organsIt is important to take into account the predisposing risk factors. It is necessary to know that candidiasis may be manifestation of diseases general viewwhich are accompanied by the development of immunodeficiency.
In case of endoscopic examination, erosive-pseudo-membrane colitis detect. When candidium colitis, specific damage to the skin, lungs, esophagus and oral cavity are detected. In the morphological study of the mucous membranes, the nice forms of Candidaspp are found. Note that invasive bowel candidiasis is unlikely in immunocompetent patients.
The course of ulcerative colitis and ulcerative disease duodenal gut May be complicated by candidiasis. In this case, the invasion of the Candidaspp pseudomitia. It happens in the intestinal areas.
In medical practice, intestinal dysbiosis is often found with a significant growth of Candidaspp. This is based on the action of mushroom metabolites, which are resolved in the intestine in their massive growth. In candidium intestinal dysbacteriosis, patients, as a rule, feel satisfactory.
The diagnoses of "intestinal dysbiosis" should not be confused with high proliferation of Candida mushrooms and "irritable colon syndrome". Common for these diseases is the absence of morphological changes in the intestine, but the treatment and pathogenesis differ significantly. Apparently, a significant portion of patients with irritable colon syndrome are sick by intestinal dysbiosis, and the treatment of the latter improves their state of health.

It should be noted that the detection of Candida mushrooms in a bacteriological analysis of detergents cannot be indicated for the treatment of patient with antimicotic drugs. It is necessary to treatment with drugs that are not inadessurbed from the intestinal lumen. The choice of the method of treatment of candidiasis of digestive organs must pursue 3 main objectives:
- correction of background diseases;
- appointment with antimicotic drugs should be rational;
- therapy should be immunocorrecting.
When choosing treatment in each case, the doctor must take into account clinical shape Candidose, character that accompanied this pathology and the risk of side effects.
There are many antimicotic effects. These are amphotericin in, itraconazole, fluconazole, ketoconazole, etc., which have a systemic effect. These drugs can be applied locally, intravenously and perfectly.
Inadessorbing antimicotic drugs is nastatin and Lev Room. (Side phenomena: toxic hepatitis and allergies).
PIMAFUCIN - a wide spectrum antibiotic. It has a higher efficiency in comparison with Nistatan. Pimafucin is valid only in the lumen of the intestine and is almost not absorbed from the gastrointestinal tract.
It must be remembered that only the doctor can assign a qualified and effective treatment In each case.
A significant criterion for the effectiveness of therapy is not to obtain a negative result when sowing mushrooms, but the disappearance of the manifestations of the disease and the amount given to the norm. To achieve the desired effect, sometimes you have to resort to a re-course of treatment.
Folk Treatments of Candidosis of the intestine
- As much as possible, eat forest berries (blueberries, blueberries, honeysuckle, Irga, strawberries). Eat cabbage, salads, leafy vegetables, dill and parsley greens.
- Clean in the morning the language from white Nalea And wechit the cavity of the mouth with a decoction of Sage, Celebre, calendula. After that, eat garlic or salad tooth, with the addition of garlic.
- Drink the infusion of dairy mushroom before bedtime - eliminates the symptoms of the candidiasis.
- Eat grated root roots.
- Oat flakes Must enter the daily diet in the form of viscous porridge or bravery.
In the intestine of each person there is a huge number of different microorganisms. Many of them belong to the category of conditionally pathogenic, representing the danger only in the presence of certain factors. Representatives of conditionally pathogenic microflora include the fungi of the clan clan, which are the causative agent of such an unpleasant disease as the bowls of the intestine. This microorganisms are quite common, they are present in the body about 80% of the population. However, not always, their presence leads to the development of pathology. This requires various predisposing factors.
Opinion expert
Sevastyanov Roman
Symptoms of the disease depends on the form of its flow and stage of development of the pathological process. Diagnostics includes the use of laboratory research methods and evaluating existing clinical manifestations. Treatment is carried out in 3 directions: elimination of reasons antibacterial therapy, Normalization of intestinal microflora.
Characteristics of pathology
Against the background of a long disturbance of the work of the immune system or in the presence of other predisposing factors, there is a rapid increase in the number of fungal bacteria of the genus Candidas, which are in the intestine of a person. These bacteria, or rather, their products of their livelihoods, adversely act on the walls of the organ, lead to the development of the inflammatory process. At the same time, useful bacteria involved in the process of cleavage of food die. The intestinal microflora is disturbed, which leads to the appearance characteristic symptoms pathological process.

Candidiasis of the intestine is a disease in which the balance of useful and conditionally pathogenic microflora is disturbed. The number of pathogenic bacteria is constantly growing, while the process of digestion and suction of nutrients in the intestines is disturbed. The patient develops a pathological condition with all the manifestations inherent in it.
Signs
The main sign of the development of the intestinal candidosis is the violation of the digestive process. The patient feels discomfort after meals, may occur painful sensations, and the localization of pain is quite difficult to determine. The appetite is broken, the patient feels saturation even after the use of a minor number of food. In addition, there is a persistent violation of the chair. Changes the consistency and color of the feces, in the wheel masses it is often possible to notice extraneous inclusions.
Disorders of the intestine negatively affect the state of the entire digestive tract, and this leads to a deterioration of well-being, the emergence of weakness, unpleasant sensations in humans.
The main symptoms include:
- which occurs not only after eating food, but also at any other time;
- Severity in the field of epigastria;
- Painful, arising after meals;
- The discharge of the chair, a change in the consistency of Cala;
- A slight increase in body temperature;
- Decline in appetite;
- Blood and purulent elements in the wheel masses;
- Silent allocations of cotton consistency in the area of \u200b\u200bthe rear pass;
- Violation of the defecation process ( frequent urges, sometimes false, feeling of incomplete intestinal emptying after visiting the toilet);
- Characteristic rash on the skin.
Types and forms
The bowls of the bowel can be divided into invasive and non-invasive. Invasive candidiasis is characterized by a more severe flow. With this form of the pathology of bacteria, the causative agent penetrates the body of the body, damaging them. This leads to severe inflammation. Invasive candidiasis can be diffuse (when bacteria damage the healthy walls of the organ on the entire length) and focal (the pathogen is introduced into the organ wall in strictly defined places, for example, in areas of ulcers and other physiological damage).
Non-invasive candidiasis is considered a more common and less dangerous variety in which the pathogenic microflora actively multiplies in the area of \u200b\u200bthe gastrointestinal tract, but does not penetrate it into its wall. Of course, the products of life fungus also negatively act on the intestinal walls, however, in this case inflammatory process It has less pronounced.
Symptoms and signs
| Signs of invasive candidiasis | Symptoms of non-invasive candidias |
Pathology is characterized by a more severe flow and manifests itself in the form of the following symptoms:
|
With the non-invasive form of candidiasis, the following manifestations occur:
|
Candidiasis of the intestine is a disease that is prone to rapid development and progression. In the absence of therapy, the pathogenic microflora quickly applies to neighboring sites. The organs of the urogenital system are most often affected. For this situation, their symptoms are also characteristic. In particular, a patient has abundant discharges that have a curly consistency, a sharp unpleasant smell.
During urination or sexual intercourse (in women), pain and discomfort arises, also for this disease, a strong tooth in the field of penis or vagina is characterized. The color of urine is changing, it acquires a whitish shade, loses its transparency.
Stages of the disease
Allocate 3 stages of the development of the pathological process.
| Stage of carrier | The candidate fungus penetrates the human body, but, with the normal operation of the immune system, its rapid reproduction does not occur. There are no symptoms of the disease, treatment is not required. |
| Stage of breeding | When exposed to certain negative factors, an active increase in the number of fungal infection is observed. Bacteria allocate more livelihood products that negatively affect the human body, in particular, on the performance of the digestive tract. At this stage, the first symptoms appear, such as discomfort and severity in the intestines, diarrhea, decline in appetite. |
| Candidose colitis | The patient's intestine contains a large amount of fungal infection, as a result of which the work of the affected organ is violated to a large extent. There are such manifestations like blood and mucus in feces, significant deterioration of well-being. The pathogenic microflora continues to multiply, the bacteria are affected by other human bodies, violating their work. As a result clinical picture It becomes more pronounced, symptoms of toxic lesion and severe pain of uncertain localization appear. |
Etiology
The main reason for the appearance of the candidiasis in the intestine - long disturbance of the immune system functions. At the same time, there are a number of secondary adverse factors contributing to the development of this situation. It:
- Belonging to certain age categories (it is known that children younger age, as well as representatives of the older generation, immunity fails are observed significantly more often);
- Frequent stresses, chronic physical or emotional fatigue;
- Pregnancy, period of childbirth and breastfeeding;
- Congenital or acquired autoimmune diseases;
- The presence or application of potent chemicals to remove them;
- Tendency to allergies;
- Pathology in the chronic form of flow, striking various sections of the human body;
- Uncontrolled and long-term use of antimicrobial means (antibiotics are destructively acting not only on pathogenic, but also for useful bacteria, leading to their mass death);
- Improper nutrition, in particular, insufficient use of vitamins, protein products;
- Harmful habits, such as long-term drug use, addiction to alcohol.
Diagnosis of Kandidosis of the intestine
To identify the presence of candidiasis, the doctor first conducts a patient's survey and an assessment of his complaints. After that appoint additional diagnostic eventsincluding instrumental and laboratory methods Research, such as:
- Endoscopy to determine the state of the mucous membranes of the intestinal walls (with candidiasis on these tissues, you can see the dense white flare);
- X-ray to detect possible damage to the organ;
- Microscopic examination of carts and selections. They detect bacteria - pathogens;
- Bacteriological sowing to identify the number of pathogenic microorganisms and determine their sensitivity to the action of one or another antimicrobial preparation;
- Histological examination to detect a bacterial agent in bowel tissues.
Methods of treatment
The treatment of bowel candidiasis is carried out in three different directions:
- Destruction of bacteria - pathogen;
- Normalization of healthy intestinal microflora and restoration of organ functions;
- Immunity strengthening (treatment of pathological conditions, which led to its decrease).
Antibacterial therapy
To suppress the growth in the number of bacteria Candida, special antifungal drugs are used. Most often assign funds local actionproduced in shape rectal candles. Such drugs have faster and effective action, because they penetrate directly into the defeat area.
Opinion expert
Sevastyanov Roman
Therapist, hepatologist, a gastroenterologist, highly qualified category. Expert Site.
With a severe course of the disease, antibacterial treatment It is complemented by using systemic antimicrobial agents in the form of pills for oral use.
Normalization of microflora
For successful treatment The candidia is not only enough to destroy the causative agent of the disease, it is necessary and stimulating the increase in the number of useful microorganisms. For this use various drugs Based on pre- and probiotics. The effect of these tools contributes to an increase in the number of beneficial bacteria in the intestine, as a result of which the normal functionality of the organ is restored.

Strengthening immunity
Since the main cause of the development of candidia is reduced immunity, comprehensive therapy Includes measures to restore the functionality of the immune system. For this, the patient is prescribed various drugs - immunostimulants, vitamin complexesAnd also develop a special diet, which includes a large number of products rich in vitamins.

Medicia treatment
To eliminate the causes and symptoms of the pathological process, various groups use medicinal preparations. These are antifungal agents of local or systemic, means against dysbacteriosis, vitamin preparations and immunostimulants.
| Name | Description | Features of reception | Price |
| The preparation of a wide range of action, negatively affecting the activity of fungal microflora. Available in various forms (candles, creams, tablets), which allows you to choose the most convenient and effective method use. | Tablets take 100 mg per day. This quantity should be divided by 4 times. Candles are used 1-3 times a day, depending on the severity of the problem. Candidiasis cream is prescribed quite rarely, only in cases where the infection has spread to the field of genital organs. It is also necessary to apply it 1-3 times a day. The course of treatment is determined individually. |
Citation:Shulpekova Yu.O. Candidiasis of intestines // RMG. 2002. №1. P. 25.
In recent decades, opportunistic infections caused by conditionally pathogenic fungi occupy a special place in the practice of clinicians of various specialties.
No matter how paradoxically, this is partly due to the successes that modern medicine has reached in the treatment of cancer and in the fight against the pathogens of serious infections. In addition, it is obvious that in recent decades, an increase in the intensity of the impact on the human body of external factors causing the development of immunosuppressive states is observed. In addition, the end of the 20th century was marked by a significant spread of fatal disease - HIV infection.
Pathological conditions caused by the influence of mushrooms of the genus Candida on the human body also belong to the category of opportunistic mycoses.
Characteristic pathogen
Representatives of the genus Candida are yeast mushrooms related ascomycetes.
The genus Candida includes a variety of types (Candida SPP.), Among which are the main importance as the causative agents of the candida, have: Candida Albicans, Candida Tropicalis, Candida Parapsilosis, Candida Glabrata, Candida Dubliniensis, Candida Lusitaniae, Candida Krusei.
Candida SPP. They are a component of microflora, symbiotic for a person. In 10-25% of the population that do not have clinical signs of fungal lesion, Candida SPP. It is not permanently detected in the oral cavity, 65-80% in the bowel content. Candida SPP. Detected in the Detooter of Gastroduodenal Yazv about 17% of cases.
According to modern ideas, under normal conditions, the main "habitat" Candida SPP. In the human body is the intestine. In the microbial population of the intestine, the proportion of these mushrooms is negligible. Growing colonies Candida SPP. In the body of a person, he is partly regulated by the work of the unit of immunity. The main place in this process is occupied by non-specific immunity units - mononuclear phagocytes (monocytes / macrophages) and polymorphic leukocytes.
A very important role in restricting the growth of the Candida population belongs to the bacteria - intestinal symbilations. Normal microflora, inhabiting the clearance of the gastrointestinal tract, produces substances with antibacterial activity (in particular, bacterio blocks and short-chain fatty acid), which prevent the introduction of pathogenic microorganisms and redundant growth, the development of a conditioned pathogenic flora. Intestinal sticks, enterococci, bifidobacteria and lactobacillies have the most pronounced antagonistic properties.
The term "candidiasis" implies the pathological process, the basis of which is an excessive growth of Candida primary in the gastrointestinal tract and the secondary - in other areas (on the mucous membrane of genitals, bronchi, in parenchymal organs).
Candida virulence factors
Mushrooms of the genus Candida have adhesiveness to epithelial cells. The attachment to the mucous membrane is one of the conditions for the further invasion of the microorganism to the subjectable tissue. The ability to adhesion among representatives of various types of Candida varies significantly; The most high this ability in C.albicans, c.tropicalis, c.dubliniensis; The smallest is Candida Glabrata, Candida Krusei. As a protective barrier that prevents the attachment of the microbe to the mucous membrane, Muzin - glycoprotein of the cell wall of epithelial cells plays an important role.
The factors of the aggression of these microorganisms include proteases and glycosidases that can intensively split mucin.
As a virulence factor also consider the ability to rapidly form pseudomitia threads; This feature is most pronounced in C.Albicans.
The virulence of microorganisms is subject to intraspecific variability, depending on the genotype.
Kandidose Risk Risk Factors
As common factors that predict to the development of candida of digestion organs and subsequent lymph-hematogenous dissemination of fungi, as in cases of other opportunistic infections, states in which the insufficiency of immune protection of the body is observed. They include:
1) physiological immunodeficiency (newborn period and early children's period, senile immunodeficiency, pregnancy, stressful states).
2) Congenital immunodeficiency (Di-Georgi Syndrome, Unteof, Sediak-Higashi, etc.).
3) an infection of a human immunodeficiency virus in the terminal stage (acquired immunodeficiency syndrome). Mycoses make up 70% in the structure of clinical manifestations of HIV infection.
4) oncological diseases (including hemoblastosis); Chemotherapy of malignant tumors accompanied by severe granulocyteneenia (<1х109 гранулоцитов в л). Развитие кандидоза на фоне противоопухолевой терапии обычно связывают с подавлением функций иммунной системы, наблюдающимся как нежелательный эффект лечения. В то же время существуют предположения, что цитостатики и лучевая терапия угнетают защитные функции эпителиального покрова кишечника и способствуют транслокации Candida в другие органы. При проведении химиотерапии возрастает процент грибковых микроорганизмов, адгезированных к энтероцитам.
5) autoimmune and allergic diseases, especially when prescribing glucocorticosteroids.
6) organ transplantation (application of immunosuppressants in post-transplantation period). More than half of the patients who are planned to carry out bone marrow transplantation, even before transplantation have a picture of a system of system candidiasis.
7) endocrinopathy (decompensated diabetes, autoimmune polyglandular syndrome).
8) Other diseases and conditions (shock conditions, anemia, hepatitis, liver cirrhosis, chronic infections, malabsorption syndrome, etc.). In pathological conditions, accompanied by a decrease in the intestinal blood supply, the translocation of mushrooms into other fabrics increases. Disruption of digestion and suction is accompanied by excessive growth of microorganisms in the intestinal lumen.
9) antibiotic therapy (usually - long-term use of the preparations of a wide range of action). The introduction of antibacterial drugs can lead to an equilibrium imbalance in the microbial bowelosis of the intestine, as a result of which the excessive development of the candidomic population in the intestine is possible. Purpose of tuberculostatic preparations for 3-4 months. accompanied by the development of bowel candidiasis in 58-62% of cases. The risk of developing idiopathic antibiotic-associated diarrhea depends on the dose of the introduced antibiotic; This disease usually proceeds without increasing the body temperature and leukocytosis in the blood and in the absence of laboratory signs of Clostridium Difficile infection. It is believed that about a third of cases, the development of idiopathic antibiotic-associated diarrhea is due to the bowls of the intestine.
10) Unbalanced nutrition (deficiency in the diet of proteins, vitamins). In animal experiment, it was shown that the insufficient admission of protein into the body is accompanied by a decrease in the phagocytic and bactericidal activity of the macrophagum, incomplete phagocytosis and an increase in the permeability of the intestinal barrier for Candida Albicans.
According to autopsy, candidiasis of 12-rings, thin and colon is detected by about 3% of dead patients (only macroscopic changes were taken into account). At the same time, half of the cases fall into the share of patients receiving chemotherapy for malignant neoplasms.
Pathogenesis of development
Candidosis of the intestine
Studies of recent years to a large extent clarified the patterns of the interaction of Candida fungi with the host body. According to modern ideas, two fundamentally different mechanism of pathogenesis of the edge of digestive organs can be distinguished: invasive and non-invasive candidiasis.
Invasive candidiasis is due to the introduction of the nice shape of the Candida mushroom in tissue. The first stage of the candidosis, as an infectious process, is the adhesion to epithelialocytes, then invasion in the epithelial layer, penetration beyond the basement membrane. This manifestations of microbial aggression macroscopically correspond to erosive-ulcerative defects of the intestine wall of various sizes and shapes, cracks, membrane overlays (similar to those with pseudo-memory colitis), polypovoid or segmental circular formations.
With progressive invasion, the development of lymph-hematogenous dissemination of mushrooms is possible (systemic candidiasis with damage to the mucous membranes of other organs; generalized candidiasis with the defeat of visceral organs). In an experimental model on animals orally infected with C.albicans under immunosuppression, the initial emergence of erosion and the ulcers of the mucous membrane in the ileum, the colonization of the lymphoid formations of the intestine, their necrosis and further dissemination are shown. The absence of macroscopic changes, apparently, should not be considered as evidence against the invasive candidiasis.
With the disseminated formats of the candidiasis in lymph nodes and ducts, multi-core giant cells containing mushrooms are found, which probably reflects the phenomenon of unfinished phagocytosis.
Invasive candidiasis is more often observed in organs lined with multilayer flat epithelium (oral cavity, esophagus), and less often with cylindrical epithelium (stomach, intestines), which is probably due to the peculiarities of local immune defense.
Non-invasive candidiasis is not accompanied by the transformation of the fungus in a nichtail shape; There is an excess growth of his colonies in the lumen of a hollow-intestine. It is assumed that important pathogenetic significance has a violation of a strip and clutch digestion, penetration into systemic blood flow of microbial components and metabolites, development in one degree or another of a pronounced systemic immuno-inflammatory reaction.
Based on all the above, it should be emphasized once again that candidiasis of the mucous membranes of extrainsecable localization or generalized candidiasis with the defeat of parenchymal organs serves as a manifestation of translocation of fungi from the intestinal lumen, where the bulk of these saprophytic fungi is presented. Candidiasis of extra-walled localization (for example, oral cavity or genitals) serves as a manifestation of a systemic candidiasis, "originating" from the intestine.
Below is the classification of the edidation of the digestive organs:
1. Oro-Faringean Candidiasis (Haleitis, Gingivitis, Saint, Glossite, Stomatitis, Farriage).
2. Candidiasis of the esophagus (complications - bleeding, stricture).
3. Candidiasis of the stomach:
- diffuse (specific erosive fibrinous gastritis);
- Focal (secondary for stomach ulcers).
4. Candidiasis of the intestine:
- Invasive diffuse;
- focal (secondary for ulcers of the 12-rosewoman, with non-specific ulcerative colitis);
- non-invasive (excessive growth of Candida in the intestinal lumen).
5. Ano-rectal candidiasis:
- Invasive Candidosis of the rectum,
- Perianal Candidia dermatitis.
The following are the main manifestations of candidalist bowel damage, which, as mentioned above, is the basis for the development of systemic manifestations.
Clinical picture
Candidosis of the intestine
The peculiarities of the course of the intestinal candidiasis are not clearly outlined enough, they are not well understood and few familiar to the most part practicing doctors. It is characteristic that those who died from different causes of patients, in which, with autopsy, macroscopic intestinal changes were discovered, corresponding to invasive candidiasis, during life, as a rule, there was very poor symptoms from the gastrointestinal tract, and the endoscopic diagnosis was often erroneous. Often, when detecting single ulcerations of the intestinal wall, the doctor is hampered in their interpretation, and according to the results of the morphological research, it is concluded about non-specific inflammatory changes in the edges of ulcerative defects, while targeted micrical research is not carried out.
Clinical manifestations of bowel candidiasis may be different depending on the level of lesion.
In the diffuse invasive candidiasis of the intestine, there are manifestations of enterocolitis: complaints of pain in the abdomen of a spastic nature, meteorism, the presence of pathological impurities in a chair (blood and mucus), there are usually signs of a systemic candidiasis (damage to the mucous membranes of the oral cavity, genitals). With endoscopic examination, changes are detected by the type of fibrinous-ulcerative colitis.
With invasive focal candidiasis of the intestinal intestinal manifestation of the disease can resemble a resistant, resistant to traditional therapy, the course of ulcerative disease of a 12-rosewind or nonspecific ulcerative colitis.
With non-invasive bowls of the intestine, patients make complaints to an unformed chair, flatulence, abdominal discomfort, with positive clinical and laboratory dynamics in antimicotic drugs.
With the invasive edge of the rectum, the symptoms of the proctitis (pain, teensals, pathological impurities in feces can be marked. In some cases, the phenomena of Perianal Candidio dermatitis are accompanied.
The bowel candidosis is often accompanied by a subfebrile fever.
Complications
As complications of the intestine candidiasis, the development of intestinal perforations, penetration of ulcers in the surrounding organs, bleeding, generalization with the defeat of parenchymal organs, the development of fungal sepsis is possible.
The defeat of parenchymal organs (liver, gallbladder, pancreas, etc.) is very often accompanied by deep neutropenia (less than 500 neutrophils in mm3) and is observed in the terminal phase of AIDS.
Mortality in invasive candidiasis reaches 25-55%. For some categories of patients (transplant recipients, acute leukemia patients) Invasive mycoses are the main cause of death.
Diagnostics
The question of the diagnosis of the bowel candida and determining the indications for antifungal therapy is extremely important.
In recognition of the candidiasis of mucous membranes, it is necessary to distinguish between the physiological "candidiasis" and the infectious process caused by this fungus.
To diagnose the candida is absolutely informative of the detection of Candida in sterile liquids (spinal cerebral, lavary, peritoneal, etc.) or mushroom detection in tissues (changes are often detected by the type of granuloma with necrosis).
To increase the sensitivity of the culture and morphological methods of diagnosis of candidiasis, it is recommended to explore several bioptats of the mucous membrane.
Biopcated tissue is collected in 2 sterile Petri dishes or sterile jars with a screw lid; One sample is poured with a 10% solution of formaldehyde and directed for histological examination, the second is used for micrical research. The material is transported to the microbiological laboratory, protecting against direct sunlight. It is necessary that the material be delivered to a micrological study no later than 1 hour after taking when stored under room temperature or no more than 3 hours during storage at + 4 ° C.
Microscopic examination must be carried out in native and painted drugs.
Chic reaction (chromic acid treatment) or its modification - painting according to gridli - allow you to reveal the pathogen in tissue or smear due to the coloring of the polysaccharide components of the cell wall; To suppress the color of the surrounding tissues, "counter-processing" is used by light green, methanyl yellow, and the like. In this case, only invasive mushroom cells are detected, at the same time it is impossible to judge the response from the surrounding tissues. Therefore, it is also necessary to evaluate drugs, "addicted" hematoxylin and eosin.
Candida pseudomycelions can also be revealed in a smear-fingerprint of the mucous membrane or a brush-imprint from the bottom of the ulcer (painting on Romanovsky-Gymzea).
On the surface of the dense nutrient medium in a cup of Petri make a print with a test piece of fabric, then produce sinking loop. The same piece of fabric is placed in 50 ml of liquid nutrient medium (Saburo medium, wort) and incubated at + 37 ° C for 5 days.
The long-end methods of C.Albicans are widely used. This type of Candida is capable of forming sprout tubes and short pseudomynevia threads for 2-4 hours at + 37 ° C on serum, egg protein, etc. such environments. For the type C.albicans, this phenomenon is characterized in 90% of cases.
For effective treatment, it is necessary to strive to determine the species affiliation of Candida fungi and determine the individual sensitivity of the strain to antimicotic drugs; Some Candida Lusitanlae strains are resistant to amphotericin, Candida Krusei and Candida Glabrata - to Fluconazole.
The discovery of Candida in the blood allows to diagnose the generalized candidiasis only in combination with the appropriate clinical symptoms (especially informatively re-detecting Candida in the blood). It should be remembered that 70-80% of patients who are actually suffering from generalized candidiasis, to identify mushrooms when cropping blood fails.
The value of serological methods is mainly in identifying patients with probable invasive methods. False-positive results of serological samples are possible in conjunction and in healthy people sensitized by antigens of mushrooms; False negative samples can be observed in immunodeficiency.
Original antigen detection procedures and antibodies of certain metabolites of mushroom cells are proposed; Created special diagnostic sets. As an example, Pastorex Candida can be cited - to determine in the reaction "latex agglutination" of repeating oligomannospic epitopes of antigenic structures expressed on the large number of macromolecules of the mushroom. The Platelia Candida set can be used to determine the Candida antigen mannana, for example, in a patient's serum with a microorganism circulation. Using the first set, the threshold for determining antigenic structures is 2.5 ng / ml, using a second-in-binding system with a method of determination - 0.5 ng / ml.
In the diagnosis of non-invasive intestinal candidiasis, in which there is no tissue biopsy material for a micrical research, the following criteria are proposed as a diagnostic standard: an increase over 1000 CODA / g Candida SPP. When sowing the intestinal contents taken under sterile conditions, in combination with the phenomena of intestinal dyspepsia and positive clinical and laboratory dynamics in the treatment of antimicotic drugs. Unfortunately, the correct fence of intestinal content for culture research is technically complicated; The method of sowing feces on dysbacteriosis cannot be widespread in our country cannot serve as a support in assessing the real composition of the intestinal microflora.
In the diagnosis of any form of candidiasis of digestive organs, it is important to take into account the presence of a patient with predisposing risk factors. "Random" identification of candidiasis should serve as an incentive to find such a background factor. It is important to remember that candidiasis can act as an early manifestation of common diseases accompanied by the development of immunodeficiency.
Considering the foregoing, it would probably be not entirely correctly formulated a diagnosis briefly as "candidiasis", without pointing out the background state.
Differential diagnosis of invasive intestinal candidiasis (when macroscopic intestinal changes is detected) It is necessary to carry out with chronic inflammatory bowel diseases, antibiotic-associated diarrhea, due to C. difficile infection, malignant lesion, ischemic colitis. The non-invasive form of the candidiasis should be differentiated with a wide range of enteritis and colitis of other etiology. Indirect certificate in favor of the presence of the Candida of the Cyeschik can be the extraordinary systemic manifestations of the candidiasis.
Treatment
It should be emphasized once again that only the detection of mushrooms of the genus Candida in a bacteriological analysis of the feces (according to the adopted methodology in Russia), regardless of the presence or absence of symptoms of intestinal dyspepsia, can not be an indication for prescribing an antimicotic drug to the patient.
For the treatment of an intestine candidiasis, it is necessary to appoint drugs that are not inadessing from the intestinal lumen.
Today there are a variety of antimicotic agents. Preparations such as amphotericin in, itraconazole, ketoconazole, fluconazole, have a systemic effect, can be used locally, orally and intravenously. When appropriate, these drugs are almost completely adsorbed from the upper departments of the gastrointestinal tract and do not reach the level of the ileum, where the main population of mushrooms is concentrated. In addition, the use of "systemic" antifungal drugs is often accompanied by side effects, in particular, the development of toxic hepatitis.
Almost non-unadighted antimicotic drugs include Lev Room, nystatin and natamycin (pimafucine). The purpose of Lev Room and Nistatin with a sufficiently high frequency is accompanied by the development of side effects (dyspeptic phenomena, allergies, toxic hepatitis).
Pimafucine (natamycin) is an antifungal polyenic antibiotic wide spectrum. It has a fungicidal potential. Pimafucin binds cell membrane solsters, violating their integrity and function, which leads to the death of microorganisms. The most pathogenic yeast mushrooms are sensitive to Natamicin, to the greatest extent - Candida Albicans. Pimafucine has a higher efficiency compared to Nistatan. Cases of resistance to natamycin in clinical practice did not meet; With repeated use of this drug, the minimum overwhelming concentration of it in relation to C.albicans does not change. Pimafucin in tablets is valid only in the lumen of the intestine, almost not absorbed from the gastrointestinal tract.
When applying tablets in the first days of treatment, dyspeptic phenomena are possible - nausea and diarrhea, which do not require the abolition of the drug and are independently resolved during treatment. The only contraindication to the purpose of pimafucine is increased sensitivity to the components of the drug. Pimafucin can be prescribed during pregnancy and lactation periods, as well as newborn children.
For the treatment of intestinal candidiasis, it is necessary to conduct a course of treatment with non-gas antifungal drugs within 7-10 days. Nystatin is appointed at 250000 cells 6-8 times a day (daily dose - up to 3 million units) within 14 days. It is prescribed 100 mg (1 tablet) 2-4 times a day for 7-10 days.
Based on the above provisions and clinical experience, it is necessary to recognize that the tactics of the treatment of candidoses of the mucous membranes of the extraordinary localization only by local antifungal agents or the preparations of systemic, the absorbing gastrointestinal tract, in essence it is erroneous. Since the source of lymph-hematogenous spread of the Candida's virulent strains causing the system candidiasis is the intestine, - without suppressing the growth of mushrooms in its lumen, antifungal therapy is ineffective or only a short-term unstable effect is observed. With systemic candidiasis, the dose of nihistan can be increased to 4-6 million units / day, at the same time a local acting antifungal agent is prescribed. In system candidiasis, pimafucine is used in the same dose while simultaneously assigning a local acting antifungal agent. In severe cases, preparations with systemic action are added to complex therapy.
Especially important timely recognition and therapy of intestinal candidiasis, as the prevention of systemic and generalized candidiasis in patients with risk groups, to which are primarily the patients receiving antitumor radiation and / or chemotrepium, anti-tuberculosis drugs, patients preparing for planned operations on the abdominal organs. In these situations, most preferably the purpose of the non-supersonic antifungal drugs is most preferable, since their long-term and reuse does not significantly affect the pharmacodynamics of other drugs.
The main criterion for the effects of therapy is not to obtain a negative result of sowing on mushrooms, and above all the disappearance of the main manifestations of the disease, the normalization of the amount of mushrooms according to the micrological research data (with the possibility of adequate sowing of intestinal contents). To achieve the effect, it is often necessary to resort to re-courses of treatment.
This article was set to expand the representations of practical doctors about the flexibility of the human body interaction with a symbiotic microflora, about the pathogenic potential that the harmless intestinal commemmose belongs to Candida. In front of the internotists and specialists in medical micrology, there are current tasks of a distinct determination of the prevalence and clinical value of fungal infections in clinical practice, developing an algorithm for diagnostics and testimony to the treatment of bowel candidiasis.
Literature
1. Zlatkin A.R., Isakov V.A., Ivnikov I.O. Candidiasis of the intestine as a new problem of gastroenterology. // Russian Journal of Gastroenterology, hepatology, coloproctology. - 2001. - №6. - p.33-38.
2. Danna P.L., Urban C., Bellin E., Rahal J.j. Role of Candida in Pathogenesis of Antibiotic-Associated Diarrhoea in Elderly Patients.//lancet/1991.-VOL.337.-P.511-514.
3. Prescott R.J., Harris M., Banerjee S.S. FUNGAL INFECTIONS OF SMALL AND LARGE INTESTINE.//J.Clin.path .-1992.-VOL.45.-P.806-811.
4. Redmond H.P., Shou J., Kelly C.J. et al. Protein-Calorie Malnutrition Impairs Host Defense Against Candida Albicans.//j.surg.res.-1991.-VOL.50.-P.552-559.
5. THE MERCK MANUAL. Sixtenth Edition. Copyright (C) 1992 by Merck & Co., Inc.