Gastroesophageal reflux disease ICD code. Gastroesophageal reflux disease (GERD) (certificate for doctors). Georny disease associated with Helicobacter Pylori
The inflammatory process covering the mucous membrane of the esophagus to form erosions and ulcers on it is called erosive esophagitis. This disease occurs equally often in men and women. By international Classification Diseases of the ICD - 10 Pathology is code to 22.1, and when the GERD is connected to 22.0.
The erosive form requires immediate treatment, since it is able to cause serious complications, up to the neoplasms of malignant type. Therefore, with the appearance of heartburn and burning out of the sternum, you need to contact the gastroenterologist to get a special treatment.
We found out what kind of erosive esophagitis code of ICD 10, follow further. Ezophagitis causes inflammation of the mucous membrane of the esophagus and develops on acute and chronic type. Acute current occurs when defeated:
- fungal infections;
- alkalis;
- acids;
- salts of heavy metals;
- hot food or couples;
- alcohol.

Also, unpleasant feelings in the form of heartburn causes overeating, physical work immediately after meals. In addition, esophagitis can be called reflux, that is, the casting content of the stomach back to the esophagus. Salonic acid contained in the gastric secretion annoys the epithelium of the esophagus tube. With damage to these factors, the mucous membrane of the esophagus is inflamed, blushes and swells. So what are characteristic symptoms? Erosive esophagitis causes a patient:
- heartburn;
- burning in the chest;
- sore throat.
This condition is treated with the use of a gentle diet, and if the disease is caused by an infectious factor, then antibiotic therapy is added.
If you do not proceed to treatment on time, then erosion appears on the mucous membrane, from here and the name erosive esophagitis. It develops in the chronic course of the disease.
Noncritical esophagitis
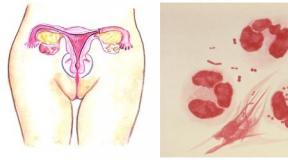
This is a form of acute course of the disease, which is found not very often and occurs in people with reduced immunity on the background infectious diseases (Scarlatina, Sepsis, Cort, Mikoz). The disease is characterized by a sharp inflammation of the mucosa of the esophagus, forming necrotic (dead) sections that are formed during rejection deep ulcers foci. During the healing of the ulcer of the epithelium of the esophagus is covered with purulent or bleeding exudate.

Against the background of symptoms corresponding to the main disease, are observed:
- pains for the sternum;
- vomiting with an admixture of necrotic tissues;
- dysphagia (violation of swallowing).
This form of the disease often causes complications in the form of bleeding, acute purulent inflammation of the mediastinum, Zaulnaya abscess.
Treatment of necrotic esophagitis takes a long time and requires patient patient and strictly fulfilling all the prescriptions of the doctor. After healing the ulcers in the esophagus, scarves are formed, which bring discomfort patients.
Chronic erosive esophagitis of the esophagus
Chronic course of the disease arises due to the following reasons:

Gastroesophagel reflux disease leads to chronic inflammation of the epithelium of the esophela. Due to the insufficient closure of the muscular sphincter ring, separating the esophagus and stomach, food can fall back into the esophageal tube, irritating the mucous membrane. Hyperemia and swelling epithelium walls of this internal organ Determined first stage Diseases. Symptoms during this period are not pronounced, mostly is a heartburn. If not to treat GERB, the shell will not only redden, and erosion is formed on it. it second stage Diseases.
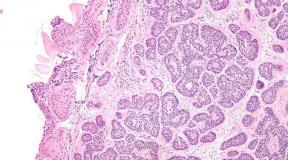
It is her who diagnose doctors when contacting them patients with complaints about heartburn and burning in the course of the esophagus. With endoscopic examination of the walls of the internal organ on the wall epithelium, the presence of single or multiple erosions, which do not merge and form defects on the mucous membrane in the area of \u200b\u200bthe same fold are noted. The walls of the esophagus are covered with a fibrous flask.
Third stage It is characterized by the rebirth of erosions in ulcers. This is already erosive ulcerative esophagitis. At this stage, not only the surface layer of the epithelium is exposed, but also undergoing fabrics. Defects further apply to one fold and may be observed in the circle of the mucosa of the esophagus. With further progression, the muscle tissue of the esophageal tube occurs. The state is worsening because the above symptoms are added to be resistant cough, vomot with blood admixture pain in the course of the esophagusarising independently of meals.

This stage is dangerous by the development of complications:
- bleeding;
- stenosis;
- barrett's esophagus.
In addition, when an infectious factor is joined against the background of erosive esophagitis, purulent inflammation of the esophagus may develop. Such states lead to deterioration general status The patient, and in the case of bleeding require emergency hospitalization. It should not be allowed to develop erosively fibrinous esophagitis.
Medical events
 The therapy of the erosive form of the disease is similar in the principles of treatment with the rest of esophagitis and GERD types. It consists of:
The therapy of the erosive form of the disease is similar in the principles of treatment with the rest of esophagitis and GERD types. It consists of:
- medical treatment;
- diet food;
- preventive measures.
Medical therapy
- Preparations that reduce the acidity of gastric juice - antacids. In the complex with them, drugs are prescribed, creating on the surface of the mucous membrane of the stomach, as well as on the food lump of a protective film that reduces harmful effects. of hydrochloric acid on the walls of the esophagus - alginats. Preparations of choice are Renny, Gevisson, Phosfalugel.
- Prokinetics - Medicines helping food faster to advance the esophagus in the stomach and to reduce the irritable effect of food on the shell of the esophagus tube ( Chirukal, Metaclopramid, Motylium).
- If erosion occurs as a result of reflux caused by insufficient cardia function, then prescribed IPP. These are medicines that increase the contractile ability of the sphincter separating the esophagus and the stomach ( Omeless).
- For better regeneration cells of the epithelium of the mucosa of the esophagus are prescribed Salcossuril, Alanton.
- In the presence of infectious inflammation Added to the above drugs add vitamins and antibiotics.

If complications or drug therapy have arisen, it turned out to be ineffective, then surgery is carried out. It can be a traditional technique (incision on chest or abdomen) or a method of larposcopy, which is less traumatic.
Diet
Dietary food plays a big role. Diet in erosive esophagite is aimed at reducing the irritating effect of food on the mucous membrane of the esophagus. Meals exclude dishes from the diet:

As well as products:
- fresh vegetables;
- fruits of acid varieties;
- legumes;
- black bread;
- mushrooms.
Alcohol and smoking are strictly prohibited.
Patients should eat small portions at least 5-6 times a day, so as not to overload the stomach and do not cause reflux. After eating, you can not go to rest, and you need to resemble a little, but do not fulfill physical work, especially requiring tilt torso. After the last meal and before sleep, it should go at least 3 hours.
 Patients can be used pieces cooked for a couple, baked or boiled. You can also not take a very hot or cold food. During the meal, you need to chew food well, do not use a coarse food so as not to injury the mucous membrane.
Patients can be used pieces cooked for a couple, baked or boiled. You can also not take a very hot or cold food. During the meal, you need to chew food well, do not use a coarse food so as not to injury the mucous membrane.
When the GERB is diagnosed with erosive esophagitisThe diet must be fulfied.
Useful video
Some more useful information How to treat and eat and eat, can be found in this video.
Prevention
After treatment, patients need to be monitored not only for food, but also change their way of life. Such people can not be playing sports connected with the strain of the abdominal press. Also need to reduce physical and emotional loads. If the work is associated with the position - the slope of the body forward, then such a kind of activity should be changed. You can not wear shy clothes, tight belts and corsets.
A good result is given hiking before bedtime, as well as tease taking ( mint, melisa, calendula, chamomile), having a sedative and anti-inflammatory action.

It must be remembered that when the first signs of the disease, you need to consult a doctor, since self-treatment or application folk methods It will not be able to fully cure the disease, and in some cases leads to the appearance of exacerbations. Once a year, such patients need to visit the gastroenterologist with the mandatory conduct of endoscopic research. If the patient's condition deteriorated, then the consultation is needed immediately.
In the therapy, much depends on the course of the course of the disease. Such information affects the duration of treatment and select some medicinal substances. In the case of GERD, primarily matters how deeply the mucous membrane of the esophagus is affected.In medicine, the classification of gastroesophageal reflux disease is more often used, which is detected by this method of research as FGDS (fibrogastroduodenoscopy).
What symptoms will be disturbed by a person on each of the stages of the disease? Today is to answer not only on this question. There are several variants of the GERB classification, consider the most common of them.
GERB classification on μb-10
 The simplest classification is spelled out in one of the classical medical books called the ICD-10 (this is an international classification of the disease of the tenth revision). Here clinical option GERD divisions next.
The simplest classification is spelled out in one of the classical medical books called the ICD-10 (this is an international classification of the disease of the tenth revision). Here clinical option GERD divisions next.
- GERB with esophagitis (inflammation of the mucous membrane of the esophagus) is the code on the ICD-10: K-21.0.
- GERB without phenomena of esophagitis - Code on the ICD-10: K-21.9.
Endoscopic classification GERB
Endoscopic classification was proposed in the late 80s of Savari and Miller, and is quite widely used in our time.
It has long been known that the GERD development mechanism is a violation of the function of the lower-flow sphincter (the muscle on the border between the esophagus and the stomach, which limits the opposite movement of food). When this muscle is weakened, the gastric content is cast, including hydrochloric acid, in the esophagus. And over time, almost all of its shells are subject to change. So they served as the basis for this classification.

defeasure of the esophagus
It can be submitted in detail as follows.
- The first stage. At the last departure of the esophagus, the one is closer to the stomach, there are sections with erythema (redness of the mucous membrane due to the expansion of capillaries), single erosion (places of the mucous membrane with fabric defects) are possible. In some not far-improving cases of the disease, such changes may not be, and the diagnosis is based either only on symptoms or in their absence on other research methods.
- In the second stage of the endoscopic classification of GERD erosion, about 20% of the circumference of the esophagus are already occupied. With such lesions, the heart rate comes out of the first place among the manifestations of the disease.
- The third stage of the painful process is characterized by the damage not only the mucous membrane of the esophagus and the lower esophageal sphincter in the form of erosion. Here already appear ulcerative defects that affect the muscular layer of the organ. Such changes occupy more than half of the circumference of the esophagus. The man is disturbed by burning, painful pain, laughing night manifestations.
- In the presence of the fourth stage of the development of the disease, thanks to FGDS, it can be seen that the entire mucous membrane is damaged, defects occupy almost 100% of the circumference of the esophagus. Clinically, at this stage of the defeat, a person can feel all the symptoms characteristic of this disease.
- The last fifth and most unfavorable is the stage of development of complications. The narrowings and shortening of the esophagus are revealed, deep bleeding ulcers, the Barrett's esophagus (parts for replacing the mucous membrane of this department in intestinal epithelium).
In its practice, gastroenterologically doctors use this endoscopic classification more often to determine the stages of the development of GERD. It is more often resorted to the therapists, considering it simpler for understanding and exhaustive. But this is not the only division of GERD.
Los Angeles Classification GERB
At the end of the 20th century, on the European Gastroenterological Week, they proposed to use the degree of prevalence of lesions. So the Los Angeles classification of GERD appeared. That's what she includes.

- Severity A - There is one or several lesions of the mucosa of the esophagus (erosion or ulcers), each of which is not more than 5 mm, within the limits of only one fold of the mucous membrane.
- Degree B - Changes also concern only one fold, but one of the lesions can go beyond 5 mm.
- The degree C - the process has spread already on 2 folds or more, sections with changes over 5 mm. At this stage, the defeat of the esophagus reaches 75%.
- Degree d - Most of the esophagus is amazed. During the circumference of the lesion, they constitute at least 75%.
According to the Los Angeles classification of complications in the form of ulcers and escirations may be present at any of the above stages.
Divisions at the disease stage of the disease were created to simplify the work of the doctors. Thanks to classifications it becomes easier to understand the manifestations of the process and it is better to select the methods of its treatment. At what stage of the development of the disease is every person suffering GERB, only a doctor can. Therefore, at the first signs of the disease, to speed up recovery, refer to the specialists.
Diseases of the digestive system organs are widely distributed both among adults and among children. Such pathology as a duodenogastral reflux causes a lot of unpleasant sensations and contributes to the development of serious complications from the stomach and esophagus.
Timely appeal to the doctor will make it possible to recognize the disease in the early stages and prevent its progression.
What is this duodenogastral reflux (DGR): With the help of this term, the pathological grounds of bile, gastric and pancreatic juices in the stomach and the lumen of the esophagus due to the weakness of locking sphincters are denoted.
Normally, digested and crushed food (chimus) enters the lumen thin gut Through the stomach pyloric department, which is represented by a powerful circular muscle - a pyloric romance. Its reduction prevents the inverse current of intestinal content.

Many scientists are inclined to the fact that bile, or biliary, reflux is not an independent disease, and the syndrome that arises against the background of existing pathologies gastrointestinal tract. In some cases, it is classified as a gastroesophageal reflux disease, in which the concentration of bile in the stomach is common enough.
The relevance of the problem is not only high prevalence, but also that the presence of duodenogastral reflux bile contributes to the development of related pathologies, worsening the quality of life. When untimely diagnostics, DGR acquires chronic flow With frequent relapses, which ultimately entails an increase in the duration and cost of treatment.
Code of the ICD-10
According to the tenth revision of the board on the international classification of diseases, the biliary reflux does not have its code on the ICD, which once again confirms the secondaryness of its occurrence. The syndrome may be part of such diagnoses:
- Gastroesophageal reflux disease (K.21).
- Duodenitis (K.29).
- Gastritis (K.29.3).
- Gastroduodenit unclear etiology (K.29.9).

Causes of disease and risk factors
The independent course of gastroduodenal reflux occurs in 25% of cases of all violations of the valve apparatus of the digestive organs. Otherwise, pathology is due to the presence of other diseases of the gastrointestinal tract in the patient.
These include:
- chronic gastroduodenitis, gastritis;
- chronic pancreatitis and cholecystitis;
- functional dyspepsia and irritable syndrome;
- ulcerative disease duodenal gut, stomach;
- giardiasis, melting invasion;
- congenital anomalies of the gastroduodenal zone.
To the main reasons for bile (alkaline) reflux also include:

Among provoking factors worth noting elderly age, irregular rude nutrition, overeating, alcohol abuse, tobacocco, long-term and uncontrolled reception NSAID (nonsteroidal anti-inflammatory drugs). An important role in the genesis of reflux plays the high acidity of the gastric juice, transferred operations on the stomach, intestines.
Mechanism for the development of duodenogastral reflux
The work of the digestive organs is a complex and multi-step mechanism, which is implemented through the nervous regulation, the effects of hormones and neuropeptides. Sphinte nerve sprigs affect the operation of the pyloric sphincter, the vegetative nervous and endocrine systems.
 The stomach in turn produces hormone-gastrin, which regulates the peristaltics of the organ and has a direct impact on the tone of the pyloric sphincter. Normalizes the motorcy of gastric glycagon, cholecystokinin, secretine, histamine. The operation of the muscular apparatus of the digestive tube depends on their concentration.
The stomach in turn produces hormone-gastrin, which regulates the peristaltics of the organ and has a direct impact on the tone of the pyloric sphincter. Normalizes the motorcy of gastric glycagon, cholecystokinin, secretine, histamine. The operation of the muscular apparatus of the digestive tube depends on their concentration.
Hormonal imbalance, impaired nervous regulation - all this contributes to the occurrence of pathological casting of duodenal content in the cavity of the stomach, often in the lumen of the esophagus.
Pregnancy is another common pathology factor. Increased in the sizes of the uterus leads to an increase in intra-abdominal pressure in abdominal cavity and squeezing a 12-rosewind, contributing to the regurgitation of bile, digestive enzymes up and the appearance of symptoms.
Useful video
What is the danger: possible complications of the disease
The most frequent complication of duodenogastral reflux is erosive gastritis. This is a chronic inflammation of the gastric mucosa with the appearance of small shallow defects on it - erosions. This consequence is due to the effects of aggressive bile acids with hydrochloric acid.
In the photo - Barreta esophagus
Hundreds of suppliers are carrying medications from hepatitis with from India to Russia, but only M-Pharma will help you buy Sofosbuvir and Daclatasvir and at the same time professional consultants will answer any of your questions throughout the therapy.
Gastroduodenit Code on the ICD-10

When it comes to inflammation of the duodenal mucosa and the stomach pyloric department, the diagnosis of gastroduodenitis is made. Its species are classified on an endoscopic picture. Until recently, this pathology did not stand out in a separate group. In the international classification of diseases (ICD-10) is a diagnosis of "Gastritis" (K29.3) and the diagnosis of Duodenitis (K29). Now and gastroduodenitis has a code on the ICD-10. A possible combination of gastritis and duodenitis is released in the ICD-10 clause K29.9 and is denoted by the phrase "gastroduodenitis uncomfortable", which is, we will tell in the article.
In the ICD-10, unspecified gastroduodenitis was allocated quite recently. Doctors still lead disputes about whether the combination of two pathologies (inflammation of the gastric mucosa and duodenum is justified). Those who vote "for" pay attention to general pathogenetic mechanisms:
Domestic medicine, given that pathological processes in the stomach are determined and maintained pathological processes in the duodenum, considers the disease as a whole. Such a disease, as gastroduodenitis classified, taking into account various factors, therefore it makes sense to list them all.
Detailed classification of gastroduodenitis:

For example , Surface gastroduodenitis is diagnosed if the inflammation only affects the walls of the gastric mucosa, with the walls of the intestine simply thicken, its vessels are overwhelmed with blood, swelling appears. In this case, the pastel mode and therapeutic diet will be effective.
Erosive type is accompanied by the appearance of painful scars, erosions and ulcers throughout the gastrointestinal tract. They can form for various reasons: due to insufficient release of mucus, the presence of reflux, the penetration of infections. Treatment should help eliminate the root cause of illness. It is this stage that allocates ICD 10, gastroduodenitis in this case is able to provoke the development of ulcerative disease.
Catarial gastroduodenitis is diagnosed in the process of exacerbation, when inflammatory process Touching the walls of the stomach and the initial duodenal department. It can be caused by improper nutrition or excessive use of drug drugs. And here the healing diet becomes the right saving circle.
The erythematous variety is diagnosed when inflammation of the gastrointestinal tract is the character of focal education. In this case, a large amount of mucus is formed, it causes swelling of the walls. Such a clinical picture signals that the ailment turns into a chronic stage. Treatment in this case will be integrated.
Source: http://zhkt.guru/gastroduodenit-2/mkb-10-vidy
Duodenogastral reflux (DGR)
Physiological duodenogastral
Duodenogastral reflux (DGR) - Throw the contents of the duodenal in the stomach. Permissible Writing Option: duoden-gastric reflux. Incorrect names: duodeno Gastric Reflux, Duodenal Reflux, Gastric Reflux, Gastroduodenal Reflux.
Duodenogastral reflux occurs in 15% healthy people. At the same time, duodenogastral reflux is often the syndrome accompanying many diseases of the upper departments of the gastrointestinal tract: chronic gastritis. Ulcerative ulcer of the stomach and duodenalist, gastroesophageal reflux disease.

If the contents of the duodenum is thrown not only in the stomach, but also in the esophagus, then such a reflux is called duodenogrostorezophageal.
The duodenogastral reflux existing for a long time leads to the emergence of reflux gastritis. Gastric ulcers and gastroesophageal reflux disease.
In a clinical picture, with pronounced duodenogastral refluxs, there is a high frequency and severity of pain and dyspeptic syndromes, the chores of the tongue with a yellow rode, diffuse abdominal pain during palpation. Duodenogastral refluxs are very often combined with pathological gastroesophageal refluxs (Pakhomovskaya N.L., etc.).
pH-gram of the body of the patient's stomach, duodenogastral refluxes in the night and morning clock (Sadovova O.A. Trukhmanov A.S.)
Acidness indicator and the number of duoden-gastric refluxs in healthy people
The table shows the average quantitative assessments of acidity and duodenogastral refluxs from "Healthy" (not having complaints about gastroenterological problems and having no subjective sensations) of people (Kolesnikova I.Yu. 2009):
Source: http://www.gastroscan.ru/handbook/117/361
Clinical picture of Duoden-Gastric Reflux
Such signs are both gastritis and duodenitis. Remove gastroduodenitis refluxers only fibrogastroduodenoscopy helps. If the described phenomena proceeds independently, it is reduced to comply with a strict gentle diet. It is based on several rules, which are worth talking separately.
Treatment of reflux gastroduodenitis

On the menu at DGR and GERD will have to include only easily dishes. The bulk of food should be divided into three parts, it is important to organize snacks between them. They will allow you to prevent starvation - the main provocateur. For snacks, it is better to choose products that contribute to the removal of bile. These are crackers, rye crackers, bran and oatmeal.
What can be used in reflux gastroduoden?
So, for example, both there, and here you can only have low-fat varieties of meat and fish, prepare them are necessary for a couple. Forbidden dairy products, as well as acidic juices. Milk products are allowed: milk, degreased cottage cheese and spring. You can form the menu by studying the diet "Table No. 1" and "Table No. 2", and all incomprehensible moments agree with the gastroenterologist.
It is important to understand that the diet will not be able to help if the causes of the disease were not eliminated. Almost all the symptoms will return immediately after its end. Therefore, it is so important not to engage in self-medication. It should always be remembered that the first light stages of pathology, such as superficial reflux-gastroduodenitis, are easily applied. If you do not take any steps to recovery, the surface form of the disease quickly develops into chronic, which is characterized by a protracted flow.
It will be more complicated to cope with them. Medical therapy will have to help. It is integrated. The doctor will advise to take prokinetics, antacids, histamine receptor blockers. Physiotherapy helps well folk Medicine. But they must necessarily go paired with medicines.
Code of ICD 10 Functional Dyspepsia
Functional dyspepsia is a symptomatic complex of disorders in the digestive process, which has a f-unique character. Dyspsic functional syndrome is manifested by discomfort, severity in the epigastric abdominal region and other symptoms. Nausea, bouts of vomiting, heartburn, belching, excessive gas formation, bloating. Dyspepsia of this type is considered one of the most common pathologies of the gastrointestinal tract. Provice the development of functional dyspepsia can disorder a motor function digestive organ.
The main causes of the disease
According to the international classification of diseases of the ICD 10, the functional dyspepsia has code K30.

Dyspepsia on the ICD implies a comprehensive type of disorder of the gastrointestinal tract. Disps syndrome is a kind of indigestion, a general disorder of the digestive system. Pathology has a similar clinical picture with many other diseases of the gastrointestinal tract.
Of particular importance in the formation of functional dyspeption is the harmful habits, as well as a set of an alimentary error. Often this smoking, abuse of alcoholic beverages and drugs.
A similar disorder of the gastrointestinal tract flows against the background of a lack of digestive enzymes, as a result of which a violation of the absorption process of nutrients, minerals and vitamins in the bowel cavity is observed. In some cases, it provokes a banal indigestion of the digestive system. Failures can be caused by abuse of greasy and heavy products, as well as overeating. One of the main reasons for the development of pathology is incorrect or unbalanced nutrition.
Functional dyspepsia is often found in newborns. In this case, the provocateur is the inconsistency of food the possibilities of the gastrointestinal tract. The reason may be in early babies or overcharging.
Several types of non-disconnecting functional formality differ. The fermentation type is developing in case of purple abuse, which provoke bouts of strong fermentation. Such products include cabbage, fruits, sweets, yeast dough, as well as legumes. Pinged dispersic syndrome is manifested against the background of consumption of a large amount of protein (red meat). This type of food products is digested hard, which allows bacteria to actively multiply in the intestine. The reason for the occurrence of fatty dyspepsia is the use of labor-based fats.
The disorder of the gastrointestinal tract, which is directly related to the deficiency of food enzymes, can be a consequence of intestinal pathologies, gallbladder, liver, stomach.
Clinical picture of functional dyspepsia
Disps syndrome is based on a variety of disorders and faults in gastroduodenal motility, manifested as follows:

The clinical picture of dyspeptic functional syndrome depends on violations that provoked it. The general features of the disorder of the gastrointestinal tract include nausea, vomiting, belching, pain syndrome and sensation of gravity in the stomach.
The cause of heartburn may be the penetration of the edible lump from the cavity of the stomach back to the esophagus. From the side of the intestine there are the following signs:
Diarrhea is a characteristic symptom of any kind of dyspeptic syndrome. Also observed abdominal pain, excessive formation of intestinal gases, a taste in the oral cavity, no appetite, nausea. In some cases, the intolerance to fried and fatty food products occurs.
Features of diagnosis and treatment
Before proceeding with therapy, it is important to complete the full diagnosis. It is necessary to conduct blood test on biochemistry to determine inflammation and failures in the functioning of the kidneys, liver, stomach, as well as pancreas. Based on the analysis of key masses, it is possible to detect diseases manifested by dyspepsia.
With the help of the Corpoogram, you can find untapped food in roast masses, as well as food fibers and fats. To determine the pathological syndrome of functional dyspepsia will help the measurement of acidity. Ezophagogastroduodenoscopy allows you to assess the condition of the mucousa. Endoscope is used for this, and fabric fence (biopsy) is performed.
A pH-metry has a particular importance that helps determine the level of acidity of the gastric secret. An important indicator of the diagnosis is to check on the chelicobacter pylori, a peculiar microorganism, which provokes the development of gastritis, ulcerative duel of duodenum and stomach. Thanks to ultrasound examination there is a chance to detect malignant tumor In the gastrointestinal tract flowing on the background of functional dyspeption.
If listed is detected clinical picture It is necessary to urgently turn to the gastroenterologist. Medical treatment therapy is selected on the basis of the cause of the disease. Basically, doctors prescribe drugs that increase the motorcycle of the digestive tract.
In the treatment of functional type dyspepsia, it is important to adhere to a strict diet. Showing fractional and frequent meals, not less than five times a day. Strictly forbidden to overeat, starve, as well as eat before bedtime. It is forbidden to drink alcohol and gas production, as well as smoking cigarettes. If the cause of pathology is the lack of enzymes, then special preparations are prescribed, capable of filling out the lack of these substances in the human body.

If the disease is detected in a child, against the background of diarrhea, strong dehydration of the body can begin. It is urgent to consult a doctor. As a rule, various medicines are prescribed, eliminating the cause of the development of dyspepsia, as well as warning dehydration. You can give a child a recider, rice decoction or sweet tea. Vitamins V. in the case of pathogenic microflora are well suited to enhance motility and peristaltics. In the case of pathogenic microflora.
Dyspex functional syndrome is a set of pathogenic manifestations by the gastrointestinal tract. It is important to turn to the doctor in time and not engage in self-medication.
Source: http://vashzhkt.com/Bolezni/Dispepsiya-KOD-PO-MKB-10.html
Duoded Gastric Reflux
Duodenogastral reflux is functional disorder gastrointestinal tract. It occurs when the contents of the duodenum along with the groil salts instead of moving into small intestine, returns to the stomach. This content is mixed with digestive acids and has a toxic effect on the stomach.
Causes of illness
The reasons for duoden-gastric reflux are not entirely understood. This disease can be caused by the disorder of nerve signals entering the duodenum and bile ducts (consequently, the reflux occurs in patients after removal of the gallbladder). In addition, it meets with excessive relaxation of the gatekeeper, changes in its motor skills or the strength of the peristaltic.
Duodenogastral reflux can cause a gastric or stagnation hyperplasia. In addition, the composition of the bile penetrating the stomach affects the secretion of prostaglandins, which are responsible for the activity of the protective mechanisms of the stomach mucosa, which further aggravates the problem and makes it difficult to treat.
Symptoms
Duodenogastral reflux calls:
It should be noted that these symptoms do not appear immediately, but as the disease develops.
Treatment at home
This ailment can be easily treated independently, observing a diet and using folk remedies. Duodenogastral reflux is not a complex disease - it is rather a violation of the work of the gastrointestinal tract, which in the future can lead to diseases. So far, it did not happen, take responsibility for your hands.
Diet
An important step in treatment is to change the habits of food. A reasonable diet minimizes the symptoms of duodenogastral reflux and helps to establish the work of the digestive system.
- You should exclude from the diet of margarine, fat, sled, - it is better to replace them with olive oil. Creamy oil can be eaten in limited quantities (it is very important not to fry on it).
- Exclude smoked and fried dishes.
- You can eat low-fat poultry meat, but oily meat and products from it should be avoided (for example, duck meat, goose, pork, offal, pies).
- From fish Choose low-fat varieties: cod, trout, mixtail. Fish canned food from the diet.
- Diet limits the melted cheeses.
- From drinks eliminate strong coffee, cocoa, strong tea.
- From carbohydrates for you will be useful wheat-rye bread or bread made of coarse grinding flour, solid variety pasta, brown rice.
- You must minimize the use of chocolate, cakes, cakes with greasy creams.
- Cucumbers, all kinds of cabbage, green beans and citrus are contraindicated from vegetables. Acute spices (curry, red pepper) can be used in limited quantities.
- The diet completely prohibits carbonated drinks. Alcohol in small doses is not contraindicated.
Phytotherapy
Treatment of healing herbs, roots, honey and other folk remedies gives a stunning effect, which largely exceeds the effect of medical procedures. After all, to establish the work of the body is best natural ways - this will help exclude side effects.
Yarrow, Chamomile and St.
These three herbs are three "whales", which builds the health of our digestive system. They can be treated by many diseases - gastritis, heartburn, indigestion, nausea, dysbacteriosis and, of course, duodenogastral reflux. Mix the thousandths, chamomile and a trunk in any proportions (that is, take the ingredients "to the eye"), pour boiling water, and make delicious tea with honey. You need to drink such a drink every morning and evening.
Grass with bark vita
If the disease aggravated so much that it began not only pain, but also vomiting with bile, spend the treatment of grass in smoke. From it you need to make info (2 tablespoons of plants on the floor of the liter of boiling water, hold under the lid of 1 hour). Take 50 ml of infusion every 2 hours until vomiting and sick subsides. Then go to the treatment of chamomile, yarrow and a beast (as described in the previous recipe).
No less effective and the root of the forefront. From it you need to do cold infusions - that is, fill the plant cold water At the rate of 2 tablespoons of crushed roots on the floor of the liter of water. The mixture should be 5-6 hours. Take it in small portions for the day until the bile vomiting stop.
Flax seed
Treatment with flaxseed seed effectively when heartburn, gastritis and all types of reflux (including duodenogastral reflux). It envelops the gastric mucosa, protecting it from the negative effects of bile salts. Pour a tablespoon of seeds with cool water (approximately 100 ml) and wait for them to swell, and the slime will be separated from the seed. This mixture should be drunk on an empty stomach before meals. Additionally, conduct treatment with other plants that would support the peristalsis of the duodenum.
Plants in Peristaltics
Mix these herbs:
From this mixture you need to make warm infusions - 1 tsp. The grass flood the glass of boiling water, cover with a lid, after 20 minutes they fill and drink. For taste, you can add honey to drink. Drink medicine 3 times a day in an hour after eating.
Also, the stimulating effect on the peristalsis of the duodenum is the root. It can be brewing instead of tea. But the easiest way is simply chewing 1-2 leaflet plants every time after eating.
Standards of diagnosis and treatment of acid-dependent and associated with Helicobacter Pylori diseases (Fourth Moscow Agreement)
List of abbreviations
GERB - Gastroesophageal reflux disease. IPP - proton pump inhibitor. HP. - Helicobacter pylori.. Npvp - nonteroidal anti-inflammatory drugs. EGDS - Ezophagogastroduodenoscopy.
Gastroesophageal reflux disease
Cipher on μb-10:
To 21. (Gastroesophageal Reflux - GER), GER with Ezophagitis - By 21.0., GER without esophagitis - By 21.9.
Definition
Gastroesophageal reflux disease (GERB) - a chronic recurrent disease characterized by casts (reflux) into the esophagus of gastric or duodenal content arising from disorders of the motor-evacuator function of the esophagastrodenal zone, which manifests the symptoms that are disturbed by the patient and / or the development of complications. The most characteristic symptoms of GERD are heartburn and regurgitation, and the most common complication is reflux-esophagitis.
GERB classification
|
Esophageal syndromes |
Explicited syndromes |
||
|
Syndromes that are manifested exclusively symptoms (in the absence of structural damage to the esophagus) |
Syndromes with damage to the esophagus (complications of GERD) |
Syndromes whose relationship with GERD is installed |
Syndromes whose relationship with GERD is assumed |
|
1. Classic reflux syndrome 2. Chest pain syndrome |
1. Reflux Ezophagitis 2. Strictures of the esophagus 3. Food Barrett 4. Adenokarcinoma |
1. Cough of Reflux Nature 2. Larygitis of reflux nature 3. Bronchial asthma reflux nature 4. Erosion of dental enamel of reflux nature |
1. Faringit 2. Sinusitis 3. idiopathic fibrosis of the lungs 4. Recurnting average otitis |
According to the International Scientific Radiation Agreement (Montreal, 2005).
Methods of diagnostics GERB
Clinical. The most common classic reflux syndrome (endoscopically negative form of GERD), manifested exclusively symptoms (the presence of heartburn and / or regurgitation, disturbing the patient). The diagnosis is clinically based on verification and evaluation of patient complaints, therefore the same interpretation of symptoms by a doctor and sick is important. Heartburn - a feeling of burning in the sternum and / or "under the spoon", which spreads upwards, individually arising in the sitting position, standing, lying, or when the tricks of the body, sometimes accompanied by a feeling of acid and / or bitterness in the throat and in the mouth, often associated with A sense of overflow in the epigastric that causes an empty stomach or after the use of any kind of solid or liquid food products, alcoholic or non-alcoholic beverages or a tobacco-acting act (the national definition of heartburn, approved by the VII Congress of the Nogr, 2007). Under regurgitation, it is necessary to understand the ingress of the contents of the stomach due to reflux to the mouth or the lower part of the pharynx (Montreal definition, 2005).
Therapeutic test with one of proton pump inhibitors In standard dosages for 5-10 days.
Endoscopic research allows you to identify and evaluate changes to distal Department esophagus, primarily reflux-esophagitis. If the metaplacia of the esophagus is suspected (Barrett's esophagus) and malignant defeat, multiple biopsy and morphological examination are carried out.
Daily reflux monitoring of the esophagus (pH monitoring, combined multichannel impedance-pH monitoring ) To identify and quantify the pathological gastroesophageal reflux, the determination of its connection with the symptoms of the disease, as well as to assess the effectiveness of therapy. Daily pH monitoring allows you to identify a pathological sour reflux ( pH < 4,0). Импеданс-рН-мониторинг наряду с кислыми дает возможность выявлять слабокислые, щелочные и газовые рефлюксы.
Pressure gauge - To assess the motility of the esophagus (peristalistic of the body, the pressure of rest and relaxation of the lower and upper esophages of sphincters), differential diagnosis with primary (ahalasia) and secondary (sclerodermia) of the esophagus lesions. Manometry helps to properly arrange the probe with the pH monitoring of the esophagus (5 cm above the proximal edge of the lower esophageal sphincter).
According to the indications, a x-ray study is carried out by the upper gastrointestinal tract: for the diagnosis and differential diagnosis of peptic ulcers and / or peptic stricture of the esophagus.
According to the testimony - estimate of the disorders of the asseacitor function of the stomach ( electrheasterography and other methods).
When identifying off-glass syndromes and in determining the indications for surgical treatment of GERD - consultation of specialists (cardiologist, pulmonologist, ENT, dentist, psychiatrist, etc.).
Medical therapy GERB
To control the symptoms and treatment of complications of GERD (reflux-esophagitis, Barrett's esophagus), proton pump inhibitors are most effective ( omeprazole 20 mg, lansoprazole 30 mg, pantoprazole 40 mg, rabeprazole 20 mg or ezomeprazole 20 mg) appointed 1-2 times a day 20-30 minutes before meals. The duration of the main course of therapy is at least 6-8 weeks. In the elderly patients with erosive reflux-esophagitis, as well as in the presence of off-line syndromes, its duration increases to 12 weeks. The effectiveness of all IPSs with long-term treatment of GERD is similar. Metabolism features in the system cytochromes P450 Provide the smallest profile of Pantoprazole drug interactions, which makes it most safe if necessary for the treatment of preparations for the treatment of synchronously occurring diseases (clopidogrel, digoxin, nifedipine, phenytoin, theophylline, R-warfarin, etc.).
For IET, a long latent period is characterized, which does not allow them to be used to quickly relieve symptoms. To quickly relieve heartburn should be used antacids and alginic acid preparations (alginates). At the beginning of the course of the GERD therapy, a combination of IPP with alginates or antacids is recommended until resistant control of symptoms (heartburn and regurgitation).
With the classical reflux syndrome (endoscopically negative GERD), as well as in the ineffectiveness of the IPP, monotherapy with alginates lasting at least 6 weeks.
When identifying disorders of the evacuation function of the stomach and a pronounced duodenogrostorezophageal reflux shows the purpose prokinatikov (metoclopramid, domperidon, iather hydrochloride).
According to the indications (intolerance, insufficient efficiency, refractoriness to the IPP) is possible histamine H2-receptors antagonists (famotidin).
Criteria for the effectiveness of therapy is the achievement of clinical and endoscopic remission (no symptoms and / or signs of reflux-esophagitis in EGDS).
It should be noted that the flow of GERD, as a rule, continuously recurrent and in most patients with the abolition of antisecretory therapy, symptoms and / or reflux-esophagitis are quickly returned.
Options for maintaining patients with GERD after persistent elimination of symptoms and reflux-esophagitis:
With a recurrent erosive-ulcerative reflux-esophagitis, Barrett's esophagus - continuous supporting IPP therapy (omeprazole 20 mg, Lansoprazole 30 mg, Pantoprazole 40 mg, Rabeprazole 20 mg or Ezomeprazole 20 mg) 1-2 times a day;
With often recurring endoscopically negative GERB, GERB with reflux-esophagitis, GERB in elderly patients - continuous supporting IPE therapy in a minimum, but effective dose (selected individually);
With a classic reflux syndrome (endoscopically negative form of GERD) - alginate therapy, comprehensive means with antacid properties or IPP "on demand", under the control of symptoms.
GERB and Helicobacter Pylori:
Prevalence NR Patients with GERD are lower than in the population, but the nature of this negative relationship is unclear.
Currently adopted point of viewthat HP infection is not the cause of GERD, the eradication of HP does not worsen the current of the GERD.
Against the background of a significant and long-term suppression of acid products, HP is distributed from the anthral duty to the body of the stomach (NR translocation). In this case, the processes of the loss of specialized glands of the stomach, leading to the development of atrophic gastritis and, possibly, the gastric cancer can be accelerated. Therefore, the HARB patients who need long-term antisecretory therapy must be diagnosed with Helicobacter Pylori, when identifying - to make an eradication (see the section "Medical therapy of the ulcer of the stomach and duodenum associated with N. pylori").
Surgical treatment of GERB
The differentiated selection of HARB patients for surgical treatment is recommended to carry out surgical treatment - laparoscopic fondoplikation. Accurate readings for surgical treatment GERB remain controversial, and remote results do not guarantee complete abandonment of IPS.
Preoperative examination should include EGDS (if the Barrett esophagus is suspected - with multiple biopsy and morphological examination), radiographic study of the esophagus, stomach and duodenum, manometry of the esophagus and 24-hour pH monitoring . The optimal decision on the operation of a consulium, including a gastroenterologist, a surgeon, if necessary, cardiologist, pulmonic, ENT, psychiatrist and other specialists.
Indications for surgical intervention:
Saving or constantly emerging symptoms, despite the optimal therapy.
Negative impact on the quality of life due to the dependence on the reception of medicines or in connection with their side effects.
The presence of complications of GERD (Barrett's esophagus, reflux-esophagitis III or IV degree, stricture, esophageal ulcer).
Restrictions on the quality of life or the presence of complications associated with the hernias of the teaching hole of the diaphragm.
Georny disease associated with Helicobacter Pylori
Cipher on μb-10: Stomach ulcer - To 25., Duodenal ulcer - By 27.
Definition
A peptic disease is a chronic recurrent disease, the main morphological manifestation of which is a gastric ulcer or duodenal ulcer, as a rule, developing against the background of chronic gastritis associated with HP.
Methods for the diagnosis of peptic disease:
Clinical.
Endoscopic, with an ulcer of the stomach, necessarily to eliminate malignancy - aiming biopsy (5-7 fragments) of the bottom and edges of ulcers.
X-ray to identify complications (penetration, malignancy). Determination of the acid-forming function of the stomach ( pH-METERY ).
Helicobacter Pylori diagnostic methods
1. Biochemical methods:
1.1. Quick urease test;
1.2. Ureazy respiratory test with 13c-urea;
1.3. ammonium respiratory test;
2. Morphological methods:
2.1. Histological method - detection of HP in the biopsyats of the mucous membrane of the anthral department and the bodies of the stomach;
2.2. The cytological method is the detection of HP in the layer of the tranquil mucus of the stomach.
3. Bacteriological method with the release of pure culture and the determination of sensitivity to antibiotics.
4. Immunological methods:
4.1. Identification of antigen N. pylori in feces (saliva, dental, urine);
4.2. Detection of antibodies to N. pylori in blood using an enzyme immunoassay analysis.
5. Molecular genetic methods:
5.1. Polymerase chain reaction (PCR) to explore the biopsy of the gastric mucosa. PCR is carried out not so much to identify N. pylori, as for the verification of N. pylori strains (genotyping), including molecular genetic features that determine the degree of their virulence and sensitivity to clarithromycin.
Drug therapy of ulcer of the stomach and duodenum associated with N. pylori
The choice of treatment option depends on the presence of individual intolerance to patients of those or other drugs, as well as the sensitivity of Helicobacter pylori strains to drugs. Application clarithromycina In eradication schemes, it is possible only in regions, where there is less resistance to it less than 15 - 20%. In regions with resistance above 20%, its use is advisable only after determining the sensitivity of HP to clarithromycin by the bacteriological method or PCR method.
Antacids Can be used in comprehensive therapy as a symptomatic agent and in monotherapy - before the pH metry and the diagnosis of HP.
The first line of antihelicobacter therapy
First option. One of proton pump inhibitors In the standard dosage (omeprazole 20 mg, Lansoprazole 30 mg, pantoprazole 40 mg, Ezomeprazole 20 mg, Rabeprazole 20 mg 2 times a day) and amoxicillin (500 mg 4 times a day or 1000 mg 2 times a day) in combination with clarithromycin ( 500 mg 2 times a day), or josamicin (1000 mg 2 times a day), or nifuratera (400 mg 2 times a day) within 10 - 14 days.
The second option (four-component therapy). Preparations used at first variant (one of the IPPs in the standard dosage, amoxicillin in combination with clarithromycin, or josamicin, or a nifuratener) with the addition of the fourth component - bismuth Trikalia Ditrateta 120 mg 4 times a day or 240 mg 2 times a day duration of 10-14 days.
Third option (in the presence of atrophy of the mucous membrane of the stomach with ahlorohydria, confirmed at pH-metry ). Amoxicillin (500 mg 4 times a day or 1000 mg 2 times a day) in combination with clarithromycin (500 mg 2 times a day) or Josamamicin (1000 mg 2 times a day), or a nifuratener (400 mg 2 times a day), and bismuth tricia dicyrate (120 mg 4 times a day or 240 mg 2 times a day) duration 10-14 days.
Note. When maintaining a ulcerative defect on the results of the control EGDS for the 10-14th day of the beginning of treatment, it is recommended to continue cytoprotective bismuth therapy tricia dicyrate (120 mg 4 times a day or 240 mg 2 times a day) and / or gearbox in a half dose for 2 -3 weeks. The prolonged therapy of bismuth tricia Dicitrate is also shown in order to improve the quality of the post-point scar and the speedy reduction of inflammatory infiltrate
A) One of the IPSs in the standard dosage in combination with amoxicillin (500 mg 4 times a day or 1000 mg 2 times a day) and bismuth tricia dicyrate (120 mg 4 times a day or 240 mg 2 times a day) within 14 days .
B) bismuth tricia dicyrate 120 mg 4 times a day for 28 days. In the presence of pain syndrome - a short rate of IPP.
Fifth option (with polyvalent allergies to antibiotics or patient failure from antibacterial therapy). One of the proton pump inhibitors in the standard dosage in combination with 30% aqueous solution propolis (100 ml twice a day on an empty stomach) within 14 days.
Second line of antihelicobacter therapy
It is conducted in the absence of eradication of Helicobacter Pylori after the treatment of patients with one of the options for therapy of the first line.
First option (classic quadrotherapy). One of the IPPs in the standard dosage, bismuth tricia dicyrate 120 mg 4 times a day, metronidazole. 500 mg 3 times a day, tetracycline 500 mg 4 times a day for 10-14 days.
Second option. One of the IPPs in the standard dosage, amoxicillin (500 mg 4 times a day or 1000 mg 2 times a day) in combination with a nitrofuran drug: nifuratera (400 mg 2 times a day) or furazolidone (100 mg 4 times a day) and bismuth tricia dicyrate (120 mg 4 times a day or 240 mg 2 times a day) duration 10-14 days.
Third option. One of the IPPs in the standard dosage, amoxicillin (500 mg 4 times a day or 1000 mg 2 times a day), rifaximin (400 mg 2 times a day), bismuth tricia dicyrate (120 mg 4 times a day) within 14 days.
Third line of antihelicobacter therapy
In the absence of eradication of Helicobacter pylori, after treatment with the preparations of the second line, selection of therapy is recommended only after determining the sensitivity of Helicobacter pylori to antibiotics.
Drug therapy of the ulcer of the stomach and duodenum, not associated with N. pylori
Antisecretory preparations: one of proton pump inhibitors (omeprazole 20 mg 2 times a day, lansoprazole 30 mg 1-2 times a day, pantoprazole 40 mg 1-2 times a day, ezomeprazole 20-40 mg 1-2 times a day, rabeprazole 20 mg 1-2 times a day) or h2 receptor blockers (famotidin 20 mg twice a day) within 2-3 weeks.
Gastroprotectors: bismuth tricia dicyrate (120 mg 4 times a day), sukralfat 0.5-1.0 g 4 times a day 14-28 days.
Antacids can be used in complex therapy as a symptomatic agent and monotherapy - prior to pH metry and HP diagnostics.
Chronic gastritis
CIFRM on the ICD-10: chronic gastritis by 29.6 Definition
Chronic gastritis is a group of chronic diseases that are morphologically characterized by the presence of inflammatory and dystrophic processes in the gastric mucosa, progressive atrophy, functional and structural adjustment with a variety of clinical signs.
The most common cause of chronic gastritis is HP, which is associated with the high prevalence of this infection.
Diagnostic methods:
Clinical;
Endoscopic with morphological assessment of biopsyats;
Diagnosis of HP (see above)
Determination of the acid-forming function of the stomach ( pH-METERY );
X-ray.
The principles of treatment of chronic gastritis
Therapy of chronic gastritis is differentiated, depending on the clinic, the etiopathogenetic and morphological form of the disease.
Chronic antral gastritis, HP-associated (type B)
The main principle of treatment of this type of chronic gastritis is the eradication of HP (see the section "Drug therapy of the ulcer of the stomach and duodenum associated with N. pylori").
Chronic chemical (reactive) gastritis (reflux gastritis, type C)
The cause of gastritis C is cast (reflux) of duodenal content in the stomach. For duodenogastral reflux The damaging effect on the mucous membrane of the stomach is provided bile acids and lizolecithin. The damaging properties of bile acids depend on the pH of the stomach: at pH< 4 наибольшее воздействие на слизистую оболочку желудка оказывают тауриновые конъюгаты, а при рН > 4 - non-conjugated bile acids, have a significantly large damaging effect.
In the treatment of reflux gastritis uses:
bismuth Trikalia Dititrats (120 mg 4 times or 240 mg 2 times a day);
Sukralfat (500-1000 mg 4 times a day) most effectively connects the conjugated bile acids at pH \u003d 2, with increasing pH, this effect decreases, so its simultaneous purpose with antisecretory preparations is impractical;
Preparations ursodeoxycholic acid (250 mg 1 time per day for 2-3 weeks to 6 months);
To normalize the motor function - prokinetics (metoclopramide, domperidon, yid hydrochloride) and motility regulators (trime, mebavserin).
NPVP gastropathy
Definition
NPVP gastropathy - the pathology of the upper sections of the digestive tract arising in chronological connection with the reception of nonsteroidal anti-inflammatory drugs (NSAIDs) and characterized by damage to the mucous membrane (the development of erosions, ulcers and their complications - bleeding, perforations).
Diagnostic methods:
Clinical (complaints study, collection of the abstractness of the disease, identifying the fact and duration of the reception of the NSAID, aspirin, the assessment of the risk factors for the development of the NSP-Gastropathy);
Common blood test (hemoglobin concentration, erythrocyte number, hematocrit), biochemical analysis blood (iron metabolism), feces analysis on hidden blood for bleeding;
Endoscopic and / or x-ray.
Drug treatment of NSAID-Gastropathy
For drug treatment of damage to the stomach and duodenal intersection associated with the reception of the NSAID, it is advisable to cancel the reception of the NSAID and use H2-blocator (Famotidine) or IPPs in standard dosages, a combination of IPP and bismuth of the tricia of dicyrate duration of 4 weeks is also possible.
If the reception of the NSAVP cannot be canceled, it is advisable to appoint the concomitant IPE therapy for the entire period of receiving NSAIDs.
If a patient with NSAID gastropathy shows the continuation of the reception of the NSAID, it is advisable to appoint selective inhibitors COF-2. However, such treatment does not exclude the development of the complications of the NSAID-Gastropathy and does not cancel the need to receive antisecretory drugs or gastroprotectors according to the indications.
As an alternative NSAID as anti-inflammatory therapy in patients with osteoarthritis, it is possible to prescribe a drug based on a ginger extract 1 capsule 2 times a day for a duration of 30 days.
Mandatory is the diagnosis of HP, in identifying which an eradication therapy should be carried out using the schemes presented in the section "Drug therapy of the ulcer of the stomach and duodenum associated with N. pylori"