Features of bacterial infections. Bacterial infection - symptoms, diagnosis and treatment. What is bacteria
Content
The problem of infectious diseases, especially bacterial ones, in modern world remains relevant. Although medicine has reached high level development, doctors have not yet succeeded in coping with bacteria. Microbes are found in public places, inhabit personal items. There are no known places on the planet that are not inhabited by these microorganisms. The pathogenicity of bacteria for the human body is caused by toxins - the products of their vital activity.
What are human bacterial diseases
The number of bacterial infections that cause disease in humans is enormous. Some diseases provoked by bacteria can not only worsen the quality of life, but also lead to death. History knows cases when the epidemic reached grandiose proportions, regions died out, and the population was rapidly declining due to just one bacterial infection. Plague, diphtheria, cholera, tuberculosis, typhoid fever were especially dangerous.
In the modern world, bacterial infectious diseases are also often exacerbated, but thanks to the development of the pharmacological industry and the qualifications of doctors, patients today get rid of the pathology faster, because the disease can be detected on early stage. Vaccination also helps protect the body from infection. List of the most common diseases caused by bacteria:
- tuberculosis;
- pneumonia;
- syphilis;
- meningitis;
- brucellosis;
- gonorrhea;
- anthrax;
- diphtheria;
- dysentery;
- salmonellosis;
- leptospirosis.
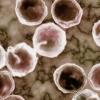
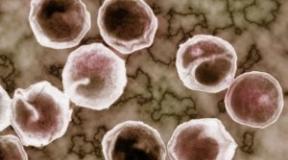
Classification of bacteria
Single-celled organisms (bacteria) are very small. You can see them only under a microscope (average size 0.5-5 microns). Because of their size, bacteria are called microbes. These microorganisms live everywhere: in water, soil, on the surface and inside plants, animals, birds, people. There are about a million varieties of microbes on earth. They do not have a formalized nuclear substance and plastids. The shape of the bacteria are spherical, rod-shaped, round, convoluted, tetrahedral, stellate, cubic O- or C-shaped.
There are different classification systems for microorganisms, but they are all conditional. In medicine and pharmacology, it is customary to divide some of the bacteria into two groups: pathogenic and conditionally pathogenic. The first type causes infectious diseases, and the second is part of the microflora of the human body. Opportunistic pathogens can also cause inflammatory processes with a decrease in immunity.
Bacteria differ in the structure of the shell and size:
- with a large cell wall - gram-positive (cocci, rods, corinemorphs);
- with a thin protective layer - gram-negative (legionella, brucella, spirochetes, pseudomonads, francisella and others).
Most dangerous to human health are gram-positive microorganisms. They cause diseases such as tetanus (botulism), mycoplasma, pharyngitis, pneumonia, sepsis, erysipelas and other diseases. Gram-negative types of bacterial infections are more resistant to antibiotics. They provoke respiratory diseases, meningitis, peptic ulcer, digestive disorders. Gram-negative microorganisms cause sexually transmitted pathologies: syphilis, gonorrhea, chlamydial infections.

Transmission routes
After getting into human body microbes take root in it. Bacteria receive all the necessary conditions for reproduction and existence. Bacterial diseases are easily transmitted to other people in a variety of ways:
- Airborne. To catch scarlet fever, whooping cough, meningitis or respiratory diphtheria, it is enough to be at a short distance from the patient. Infection can occur during a conversation or when the carrier of the infection cries, sneezes, coughs.
- Dust way. Some bacteria find shelter in layers of dust on walls and furniture. This way of transmission of infection is characteristic of tuberculosis, diphtheria, salmonellosis.
- Contact household. It involves items of everyday use: dishes, books, telephones and others. They are temporary carriers of pathogens. Using a mug or other utensils of the patient, you can instantly become infected with helminthiasis, dysentery, tetanus.
What diseases are caused by bacteria in humans?
Bacteria are divided into aerobes and anaerobes. The former, in order to live, must receive oxygen. Anaerobic bacteria do not need it or do not need it at all. Both those and other microorganisms are capable of causing bacterial diseases in humans. Aerobic microorganisms are some types of Pseudomonas, diphtheria and tuberculosis bacillus, causative agents of tularemia, Vibrio cholerae, most pathogenic microbes (gonococci, meningococci). All aerobes die at an oxygen concentration of 40–50%.
Anaerobic bacteria are more tenacious, since the presence or absence of oxygen does not affect them. They settle in dying tissues, deep wounds, where the level of body protection is minimal. Anaerobes that pose a threat to human health include peptococci, peptostreptococci, clostridia and others. Some anaerobic bacteria provide a healthy intestinal microflora, oral cavity (bacteroids, prevotella, fusobacteria). Their vital activity can lead to illness. The most common problem is suppuration and infection of wounds.

Intestinal
Over 400 species of bacteria live in the human intestine. They support microflora and immunity in order, play an important role in digestion. When the balance is disturbed, when pathogenic microorganisms displace beneficial bacteria, diseases develop. The main causative agents of infectious diseases of the intestine are:
|
Type of pathogen |
Source of infection |
Transmission method |
Symptoms |
Possible Complications |
|
|
Salmonella |
Fish, meat, dairy products. |
Alimentary |
From 6 to 72 hours. |
High fever, abdominal pain, vomiting, nausea. |
Colitis, gastritis, reactive arthritis, acute heart failure. |
|
Bacteroids |
From person to person. |
Sexual, contact-household. |
From 2 to 12 days. |
Violation of intestinal motility: constipation, diarrhea, bloating, flatulence, loss of appetite. |
Peritonitis, abscess, sepsis, colitis, phlebitis, inflammation of the inner membranes of the heart. |
Respiratory tract
Acute infectious diseases develop due to infection in the respiratory tract. Accompanied by inflammatory reactions, characteristic clinical manifestations:
|
Type of pathogen |
Source of infection |
Transmission method |
The duration of the incubation period |
Symptoms |
Possible Complications |
|
pneumococci |
From person to person. |
Airborne |
1 to 3 days. |
High fever, weakness, chills, palpitations, wet cough with purulent sputum. |
Cerebral edema, acute respiratory / heart failure, cardiac arrest. |
|
whooping cough |
From person to person. |
Airborne |
From 3 days to 2 weeks. |
Moderate fever, dry paroxysmal cough, sore throat, chest pressure. |
Bronchitis, pneumonia, pleurisy, stroke, hemorrhoids, purulent otitis media, tonsillitis. |
Genitourinary system
infections urinary tract caused by a huge number of pathogenic and opportunistic microorganisms. The most common bacteria that cause disease are:
|
Type of pathogen |
Source of infection |
Transmission method |
The duration of the incubation period |
Symptoms |
Possible Complications |
|
Gonococcus |
For men - 2-5 days, for women - 5-10 days. |
Hyperemia, swelling of the urethra, burning, itching in the vagina, cutting pain during urination. |
Total urethritis, prostatitis, inflammation of the pelvic peritoneum, uterine mucosa. |
||
|
Chlamydia |
The carrier of the pathogen is a person. |
Sexual, transplacental. |
1 to 2 weeks. |
Mucopurulent discharge from the urethra and vagina, swelling, redness of the urethra, itching, burning, abdominal pain. |
Ascending urinary tract infections, joint damage, vascular disease, heart disease, impotence. |
circulatory
Bacterial infections affecting circulatory system a person can enter the body after an insect bite, from mother to fetus, through sexual contact. The most common sources of blood diseases:
|
Type of pathogen |
Source of infection |
Transmission method |
The duration of the incubation period |
Symptoms |
Possible Complications |
|
Malarial Plasmodium |
The bite of a female Anopheles mosquito. |
Transmissible |
from 7 to 16 days. |
Head and muscle pains, general malaise, pallor and dryness of the skin, cold extremities. |
Malarial coma, cerebral edema, mental disorders, rupture of the spleen. |
|
Tick-borne encephalitis |
ixodid tick |
Transmissible, fecal-oral. |
From 7 to 14 days. |
An increase in body temperature up to 38 ° C, insomnia, headaches, prolapse upper eyelid, lack of eye movements. |
Atrophic paralysis, death. |
Skin
About a third of all skin diseases make up pyoderma - pustular diseases caused by pyogenic bacteria. The main causative agents of this pathology are gram-positive cocci:
|
Type of pathogen |
Source of infection |
Transmission method |
The duration of the incubation period |
Symptoms |
Possible Complications |
|
Staphylococcus aureus |
People are permanent and temporary carriers, food. |
Contact-household, airborne, dust, oral-fecal, alimentary. |
From several hours to several days. |
Headache, skin lesions at the mouth of the hair, folliculitis, furuncle, carbuncle. |
Meningitis, brain abscess. |
|
Streptococcus |
From person to person. |
2 to 5 days. |
The skin is inflamed to the level of subcutaneous tissue, large sticky scales, abscesses are formed. |
Purulent otitis media, chronic lymphadenitis, rheumatoid arthritis, sepsis, acute rheumatic fever. |
Diagnostics
The main method for diagnosing bacterial infections is bacteriological examination (bakposev). Biomaterial (urine, blood, sputum, secretions, skin) containing bacteria is taken from the patient and inoculated on special nutrient media for 48 hours. After the growth of pathogen colonies, symptomatic treatment is identified and prescribed. The advantage of diagnostics is the ability to study the sensitivity of the isolated microorganism to antibiotics. Also used:
- General blood analysis. Effective diagnostics the presence of an infection in the body.
- Serological study. Shows the presence in the blood of antibodies to certain bacteria. An increase in their titer indicates the presence of a bacterial infection.
- Examination of material under a microscope. Helps to quickly make an approximate diagnosis.
Treatment of bacterial diseases
When diagnosing a bacterial infection, treatment with antibacterial drugs is prescribed. To destroy the pathogen, several groups of antibiotics are used - with a bacteriostatic effect (suppress the reproduction and growth of bacterial cells) and bactericidal (kill bacteria). Appointed antibacterial drugs groups of monobactams, cephalosporins, quinolones and penicillins exclusively by a doctor on an individual basis.
To slow down the growth of pathogenic flora, Chloramphenicol, Tetracycline tablets are used (orally). To destroy the pathogen, prescribe Rifampicin, Penicillin in capsules and ampoules (intramuscularly). Symptomatic therapy is prescribed in the complex:
- non-steroidal anti-inflammatory drugs - Ibuprofen, Indomethacin are used for analgesic effect for pains of different localization;
- saline solution Regidron - prescribed for acute intoxication organism;
- antiseptics - Septifril, Stopangin, Strepsils, Ingalipt will help with throat infections;
- physiotherapy is used to cleanse the nose: inhalation using a nebulizer with Aqualor, Dolphin solutions;
- antibacterial suppositories / ointments - Metronidazole, Diflucan are used topically to treat bacterial infections in gynecology / urology;
- antihistamines - Allegra, Tigofast are prescribed for bacterial allergies;
- Polysorb sorbent - used for gastric lavage in case of intestinal infections;
- Tannin powder - used to treat dermatological infections;
- sorbents and probiotics Laktofiltrum, Linex - to restore the intestines.

Prevention of bacterial diseases
To prevent infectious pathologies, it is recommended to monitor the cleanliness of the room, regularly ventilate it, 2-3 times a week carry out wet cleaning with products containing antibacterial substances. In addition, other preventive measures must be observed:
- observe personal hygiene;
- periodically disinfect (wash) household items in hot water;
- after visiting public places - wash your hands with soap;
- avoid contact with sick people;
- wash vegetables and fruits several times;
- meat and fish require washing and heat treatment;
- when cut, wounds must immediately be disinfected and protected from external influences (bandaged);
- take vitamins and minerals to boost immunity (especially during seasonal epidemics);
- apply bacterial vaccines (after consulting a doctor), especially when planning a trip abroad.
Video
Did you find an error in the text?
Select it, press Ctrl + Enter and we'll fix it!
Today, thousands of bacteria are known - some are beneficial, while others are pathogenic and cause diseases. Many terrible diseases - plague, anthrax, leprosy, cholera and tuberculosis - are bacterial infections. Well, the most common are meningitis and pneumonia. It is important not to confuse bacterial infections with viral ones, to know the symptoms and treatment options.
What infections are called bacterial?
Bacterial infections are a huge group of diseases. One reason unites them - bacteria. They are the most ancient and numerous microorganisms.- Airways;
- intestines;
- blood;
- skin covering.
Bacterial infections of the respiratory tract often develop after a cold, as a complication. The immune system becomes weaker, and pathogenic bacteria that did not manifest themselves before begin to multiply. Respiratory bacterial infections can be caused by the following pathogens:
- staphylococci;
- pneumococci;
- streptococci;
- whooping cough;
- meningococci;
- mycobacteria;
- mycoplasmas.
To bacterial infectious diseases of the lower respiratory tract include bacterial bronchitis and.
Bacterial infections of the intestine often occur due to unwashed hands, the use of products with poor heat treatment, improper storage or expired. In most cases, the problem is caused by:
- shigella;
- staphylococci;
- cholera vibrios;
- typhoid bacillus;
- salmonellosis.
Intestinal bacterial infections more often manifested by the following diseases:
- salmonellosis;
- typhoid fever;
- dysentery.
In children most often there are viral infections, which are complicated by bacterial ones due to the weakening of the body during the period of illness. In most cases in childhood the following viral diseases are observed:
- measles;
- rubella;
- piggy;
- chickenpox.

Children who have been ill with such infections receive strong immunity and are no longer exposed to these diseases. But if during the period of illness the child had contact with harmful bacteria, then it is quite possible to develop complications in the form of bacterial pneumonia, otitis media, etc.
How to distinguish a viral infection from a bacterial one
Bacterial and viral infections are often confused. They may have the same symptoms and even similar results in diagnostic tests.It is imperative to differentiate these infections, since drugs for their treatment are completely different.
There are several signs by which you can determine whether a bacterial or viral infection is present in the body:
- duration. Symptoms viral infection usually subside quickly (in about 7-10 days), and a bacterial disease can last for more than a month.
- Slime color. If the disease is accompanied by sputum or nasal mucus, then you should pay attention to their color. The virus is usually accompanied by secretions of a transparent color and liquid consistency. For bacterial infections, the discharge is more characteristic of a dark greenish or yellow-green color. You should not completely rely on this sign.
- Temperature. Both types of infections are usually accompanied by elevated temperature, but in bacterial diseases it is higher and is characterized by a gradual increase. With a virus, this indicator behaves the other way around - it gradually decreases.
- Ways of infection. Among bacterial infections, only some diseases are transmitted by contact, and for the virus this is the main route of spread.
- Development and localization. Bacterial infections tend to develop slowly, and the virus immediately manifests itself brightly. In the first case, the lesion is isolated, that is, the disease is localized in a certain area. A viral disease affects the entire body.
- Test results. One of the main indicators is the level of leukocytes and lymphocytes. Leukocytes increase with infection of any etiology, but neutrophils are elevated during bacterial infection(this is a special type of leukocytes). With a viral infection, leukocytes can be increased, but most often they are lowered (including neutrophils) (for example, with influenza, viral hepatitis, measles, rubella, mumps, typhoid fever, leukocytes are necessarily below normal), but here with a viral infection, an increase in the number of lymphocytes is necessarily traced, and an increase in monocytes may also be observed (at, for example), therefore, the result is evaluated general analysis blood complex. Another analysis is a bacteriological examination of a biological fluid (detachable eye, ear, sinuses, wounds or sputum, for example). This analysis will identify the causative agent of a bacterial infection.
Symptoms of bacterial infections
There are many possible bacterial infections. Each has its own characteristics, so the set of symptoms is different.Incubation period in bacterial infections has a wide range. Some pathogens actively multiply in a few hours, while others take several days.

Signs of a bacterial infection depend on which part of the body it has affected. Intestinal diseases in this case are manifested by the following symptoms:
- high temperature and fever;
- pain in the abdomen;
- vomiting;
- diarrhea.
Children's bacterial infections are characterized by a wider range of symptoms. The thing is that almost always a bacterial infection is a continuation of a viral one. For example, a child gets sick, but under certain conditions he develops a bacterial infection as a complication of the original disease, so the clinical picture is erased.
But still, the diseases are expressed by the following symptoms:
- high temperature (more than 39°C);
- nausea and vomiting;
- plaque on the tongue and tonsils;
- severe intoxication.
If, after improving well-being, there is a deterioration in the patient's condition, then most often this indicates the development of complications of a bacterial nature after a viral illness.
bacterial infections in the upper respiratory tract also often appear after the transferred virus, when immunity is reduced. Infection is expressed in the following symptoms:
- deterioration of well-being;
- pronounced lesion;
- purulent secretions;
- white coating in the throat.

A bacterial lesion in women affecting the genitourinary system has the following symptoms:
- vaginal discharge - the color and consistency depends on the causative agent of the infection;
- itching and burning;
- bad smell;
- painful urination;
- pain during intercourse.
- pathological discharge from the urethra;
- unpleasant odor of discharge;
- painful urination, itching, burning;
- discomfort during intercourse.
Diagnostics
For bacterial infections, specific investigations are needed. They are used to differentiate a bacterial lesion from a viral one, as well as to determine the pathogen. The course of treatment depends on the results of the tests.
Bacterial infections are diagnosed mainly through laboratory tests. The following methods are usually used:
- Blood test with leukocyte formula. With a bacterial infection, an increased number of neutrophils is observed. When the number of stab neutrophils is increased, they speak of an acute infectious disease. But if metamyelocytes, myelocytes are found, then the patient's condition is characterized as dangerous, and requires emergency care physicians. With the help of such diagnostics, it is possible to identify the nature and stage of the disease.
- Analysis of urine. Shows whether the urinary system is affected by bacteria, and is also necessary to determine the severity of intoxication.
- Bacteriological examination with antibiogram. With the help of this analysis, it determines the type of the causative agent of the infection, and by what means it can be killed (the so-called sensitivity of the pathogen to antibiotics is determined). These factors are important for prescribing the correct therapy.
- Serological study. Based on the detection of antibodies and antigens that interact in a specific way. For such studies, venous blood. This method is effective when the pathogen cannot be isolated.
Laboratory research is the main direction in the diagnosis of bacterial infections. In some cases, additional examinations are required:
- X-ray. Performed to differentiate specific processes in individual organs.
- Instrumental diagnostics. Ultrasound or laparoscopy is more commonly used. These methods are needed to study internal organs for specific lesions.
The appointment of the correct treatment, its effectiveness and the risk of complications directly depend on the timeliness of diagnosis. You should consult a doctor at the first alarming symptoms - at the reception, the patient is always prescribed tests.
General approach to the treatment of bacterial infections
The treatment of bacterial infections is guided by general principles. This implies a certain therapy algorithm:- Eliminate the cause of the disease.
- Cleanse the body of toxins.
- Heal the organs affected by the infection.
- Reduce the severity of symptoms and alleviate the condition.
As far as taking medications, broad action include antibiotics penicillin group and 3rd generation cephalosporins. Read more about antibiotics prescribed for genitourinary infections - read), for intestinal -, but basically the treatment is carried out with the same drugs, just the dosage, duration and frequency of taking the medicine can be different.
There are a lot of antibiotics, each group of such drugs has its own mechanism of action and purpose. Self-medication, at best, will not bring an effect, and at worst, it will lead to neglect of the disease and a number of complications, so the doctor should prescribe treatment depending on the nature of the disease. The patient is only obliged to follow all the doctor's instructions and not to arbitrarily reduce the course of taking antibiotics and the prescribed dosage.
Let's summarize what has been said. There are a lot of bacterial infections, and the effectiveness of their treatment directly depends on the identification of the causative agent of the disease. Most people are carriers of certain bacteria, but only certain factors provoke the development of infection. This can be avoided with preventive measures.
Next article.
Bacterial infections are a huge group of diseases caused by microorganisms - bacteria. These are small unicellular microorganisms with a strong cell wall to protect against the effects of aggressive environmental factors. Bacteria are isolated in a separate kingdom - prokaryotes, since they do not have a nucleus, their genetic material is located in the cytoplasm of cells. These microorganisms are the most numerous and ancient of all living beings, they live almost everywhere (water, air, soil, other organisms).
A few historical facts
For the first time to see a microcosm full of living beings in the 17th century. succeeded by the Dutch manufacturer Anthony van Leeuwenhoek, who, being fond of grinding glass, was the first in the world to build a microscope. Looking at the water from the puddle, he saw that it was full of microorganisms, and gave them the name "microscopy". The relationship of microorganisms with diseases that are transmitted from one person to another was discovered by the French scientist Louis Pasteur in the 19th century. Prior to this, there was an idea that a patient with an infectious disease has a certain contagious beginning - "miasma". Further, with the improvement of microscopic technology at the end of the 19th century. early 20th century Scientists managed to discover the causative agents of many infectious diseases (tuberculosis, typhoid fever, dysentery, cholera, plague). And although the pathogens were known, humanity was able to effectively fight bacteria only from the moment the English bacteriologist Alexander Fleming discovered the antibiotic penicillin.
Classification of bacteria
Given that bacteria are a very large group of microorganisms, they are divided into several groups according to certain criteria.
The most important in the development of diseases caused by a bacterial infection is the release of toxins (poisons) by bacteria, which have an inflammatory effect, cause intoxication of the body and damage internal organs:
- endotoxins - are released after the death of the bacterium and the destruction of its cells (intestinal infections). The most dangerous is meningococcal endotoxin in meningococcal infections. In the event of the death of a significant number of bacteria, the released endotoxin can lead to the development of infectious-toxic shock and lead to death.
- exotoxins - poisons secreted by living bacteria in the course of their life activity (diphtheria).
Principles for diagnosing bacterial infections
The main method in the diagnosis of bacterial infections is bacteriological examination. At the same time, material containing bacteria is taken from the patient and inoculated on special nutrient media. After growth of colonies on nutrient media (about 48 hours), the bacteria are identified. A huge plus this method It is possible to conduct a study of the sensitivity of the isolated bacterium to antibiotics, for the appointment of rational treatment. Also used:
- microscopic examination of the material - allows you to make an approximate diagnosis when detecting bacteria using a microscope.
- serological examination - the presence of antibodies in the blood to certain bacteria is determined, an increase in antibody titer indicates the presence of bacteria in the body.
Principles of treatment of bacterial infections
Treatment of bacterial infections, like any other disease, is complex and includes:
- etiotropic therapy - treatment aimed at destroying the cause of the disease - bacteria. For this, an arsenal of antibiotics is used. At the moment, there are several groups of antibiotics, but the most important is their division into bactericidal antibiotics (kill bacteria) and bacteriostatic (suppress the growth and reproduction of bacterial cells). This is very important to know, especially in the case of meningococcal infection, the appointment of bactericidal antibiotics will lead to the mass death of meningococci and the release of endotoxins into the blood.
- pathogenetic therapy- is aimed at removing bacterial toxins from the body that accumulate in the process infectious disease(detoxification). Also, treatment is carried out aimed at restoring damaged organs.
- symptomatic therapy - is necessary to alleviate the condition of a person with a bacterial infection and reduce the severity of symptoms.
At the present time, thanks to antibiotics, it is possible to cure most bacterial infections, but it is worth remembering that improper use of antibiotics can lead to the development of resistance (insensitivity) in bacteria and even dependence on antibiotics.
Diseases caused by bacteria are currently considered the most common of all that can appear in humans. Today, there are many pathologies and microorganisms that provoke them. Next, we will consider in detail the diseases caused by bacteria. The table that will be given at the end of the article will contain basic information about pathologies and pathogens.
General information
Pathogenic (disease-causing) microorganisms have a cell wall and a unique set of defense and aggression factors. Many people know such pathologies as scarlet fever, acute respiratory infections, pyelonephritis, plague, salmonellosis, syphilis, gonorrhea, tetanus, tuberculosis. The cause of their development are pathogenic bacteria. Diseases can proceed in different ways, have several stages, degrees of severity. Treatment of a particular pathology is carried out on the basis of the results of the tests.
Characterization of bacteria
What is a pathogen? It is a microscopic organism that, unlike prions and viruses, has the following types of bacteria:
- Non-pathogenic.
- Conditionally pathogenic.
- Pathogenic.
Consider the features of bacteria that provoke pathologies. The negative effect of microorganisms is due to the presence of special aggressive devices in them. Among them, the following factors should be highlighted:

These "devices" are fully equipped with pathogenic bacteria. Examples of such microorganisms: salmonella, pale treponema, gonococcus, bacillus Luffner. Conditionally pathogenic bacteria can be in a person without causing pathologies in the norm. However, under certain conditions, they turn into harmful bacteria. Examples of such microorganisms: staphylococcus, streptococcus, proteus and some others. Conditionally pathogenic elements are necessary for the body. Thanks to their presence, balance is maintained. Some intestinal bacteria are considered opportunistic pathogens. The last category of microorganisms does not cause any negative conditions under any conditions. At the end of the article there is a table "Human Diseases Caused by Bacteria". It contains provoking various infectious pathologies.
In what cases does the development of pathology occur?

Incubation period
It exists in every infection. During it, bacteria get used to a new place, multiply, develop. The incubation period can last from several hours (for example, with food poisoning) to several years (with tick-borne borreliosis, leprosy). From the moment the first symptoms began to appear, we can say that the pathology is fully developing. The incubation period is over, groups of bacteria have settled throughout the body. With some pathologies, the immune system is able to cope on its own. But in some cases, he needs outside help.
How are diseases caused by bacteria diagnosed?
Identification of pathologies is carried out in several ways:

Therapeutic activities
Diseases caused by bacteria are treated with various antibiotics. The use of drugs is the main therapeutic method for infectious pathologies. There are a lot of antibiotics on the market today. The action of some may be directed against any particular group of bacteria. Other drugs have wide range activity. The use of antibiotics must be treated with great care. It should be remembered that illiterate treatment (as a rule, independent, without consulting a doctor) can lead to serious consequences.
Antibiotic resistance
It occurs in microorganisms due to their ability to mutate. Sooner or later, bacteria develop resistance to a particular drug. Medicines cease to act - to neutralize harmful microorganisms. In such cases, experts prescribe stronger drugs - the means of the next, new generation. Medicine is considered indirectly responsible for the occurrence of infections that arose as a result of therapeutic assistance. Previously, such pathologies were called nosocomial (hospital). From common diseases they differ precisely in that simple (traditional) medicines do not have the necessary effect, and one has to resort to more strong drugs. Relatively recently began to appear, for example, multidrug-resistant tuberculosis strains. Today, there are not many medicines for this disease. Basically what was developed in the USSR is used. These medicines do not work on a new type of infection. Such patients become not only incurable, but also extremely dangerous for others, as they are carriers of pathogenic bacteria.

Causes of drug resistance development
Antibiotic resistance is considered a fairly natural process. This is due to the ability of a microorganism, like all living things, to adapt to constantly changing environmental conditions. However, the rate of development of antibiotic resistance has been significantly affected by the inept use of drugs. Relatively recently, antibiotics were sold in pharmacies without a prescription. In this regard, many people went and purchased medicines without consulting a doctor. As a rule, self-treatment ends after 1-3 days, when the symptoms disappear. This leads to incomplete destruction of pathogenic bacteria. Some of them are eliminated, and the rest mutate, turning into another L-form. They are distributed throughout the body and take a wait-and-see attitude. When favorable conditions arise for them, they are activated. To prevent such consequences, antibiotics are prescribed in courses of 5 to 14 days. Microorganisms must be completely destroyed, and not adapted to medicines.
The main problem of antibiotic therapy
Along with pathogenic bacteria, the use of medicines destroys beneficial microorganisms that inhabit the gastrointestinal tract, for example. An imbalance can lead to the fact that opportunistic elements can turn into harmful ones. One of the most common diseases is dysbacteriosis. Elimination of pathology is carried out by stimulating the growth of beneficial microflora.
Clinical picture with infection
Fever is considered the first symptom. It is caused by the fact that when the cell wall of the microorganism is destroyed, the LPS complex penetrates into the bloodstream and reaches the hypothalamus, and then the thermoregulatory center in it. As a result, the set point shifts, and the body begins to "think" that it is cold. Therefore, heat production increases and heat transfer decreases. Fever acts as defensive reaction. Temperature up to 39 degrees. stimulates the activity of the immune system. If this indicator is exceeded, it is necessary to take antipyretics. As such a drug, the medicine "Paracetamol" can act. The temperature can be indirectly lowered with antibiotics. With its decrease during the first 24-28 hours from the start of administration, it can be concluded that the drug is correctly selected. Another manifestation of the infectious process is intoxication syndrome. It is manifested by a significant deterioration in the condition, a decrease in mood, apathy, muscle and joint pain. Probably nausea, vomiting. Relief of the condition will help the reception of a large volume of liquid (at least two liters). Excess water will dilute the toxins, reduce their concentration and excrete some of them in the urine. These two symptoms described above are considered universal and appear in almost all infections. All other signs are determined by the characteristics of a particular pathogen, exotoxins and other aggressive factors.

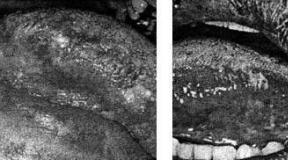
Specific infections
These include, for example, tuberculosis, syphilis. These pathologies are somewhat different from others. It must be said that these infections have existed for a long time in humans and the body is somewhat "used" to them. As a rule, these pathologies are not accompanied by bright clinical picture. However, against the background of infections, specific inflammations develop, which can be seen through a microscope. These pathologies are very difficult to treat. In this case, treatment is aimed only at eliminating clinical manifestations infections. Completely rid the body of specific diseases is not possible today.
Immune activity
The body's defense system includes two branches: cellular and humoral. The latter is necessary to create specific antibodies to the antigens of harmful bacteria. When a pathogenic microorganism penetrates, it is met by immune cells - macrophages. They destroy bacteria, studying their structure in the process. Then they transfer the received information to the central organs of the defense system. They, in turn, give a signal for the production of proteins (antibodies) that will have the ability to attach to bacteria and destroy them. The antibodies created are released into the bloodstream. Cellular defense of the body is built according to a different scheme. White blood cells attack foreign bacteria using proteolytic enzymes. Outwardly, they are pus. Due to the presence of these enzymes, pus has the ability to dissolve surrounding tissues and break out, taking foreign compounds with it.
The state of the body after therapy
Recovery of the body can be of three types: complete, laboratory or clinical. In the latter case, we are talking about the absence of any symptoms that relate to pathology. Laboratory recovery is established when there are no laboratory signs. Complete cure a condition is considered in which no harmful microbes that provoked pathology are found in the human body. Of course, not all diseases end in recovery. In practice, a lot of cases and deaths have been registered. Also, the course of pathology can go from acute to chronic.

Finally
Pathology | Pathogen | Localization center | Distribution method |
Diphtheria | Corynebacterium diphtheriae (gram-positive, rod-shaped bacterium) | Upper respiratory tract (pharynx, usually) | Airborne |
Tuberculosis | Mycobacterium tuberculosis (rod-shaped microbe, belongs to the genus Actinomycete) | Predominantly light | Airborne, through the milk of infected animals |
Bordetella pertussis (gram-negative, rod-shaped bacterium) | Upper respiratory tract | Airborne |
|
Neisseria gonorrhoeae (gram-negative coccus) | Genital organs (mainly mucous membranes of the urinary tract) | During sexual contact |
|
Treponema pallidum (spirochete) | Genitals, eyes, bones, CNS, joints, skin, heart | During sexual contact |
|
Inner walls of blood vessels (clots), skin (rash) | Epidemic form - carrier of louse, endemic - rat fleas |
Above is a table. Human diseases caused by bacteria are briefly highlighted in the presented scheme.
Reading time: 7 minA small unicellular microorganism is equally adapted to living in the aquatic environment, soil and air space. Bacteria cannot be observed under normal conditions. Exclusively under a microscope. Although there are a huge number of them in the environment, which is in the millions.
Man and bacteria coexist peacefully. Even with absolutely healthy person there are plenty of them in the body. The microflora that is present inside human body becomes an excellent habitat for many types of microorganisms. And they are harmless as long as human immunity is strengthened.
But under the influence of damaging microbes, the body's defense functions are weakened. That's when bacteria can cause disease, cause irreparable, sometimes, harm to health.
All known types of microorganisms were combined into appropriate groups according to their distinctive features.
Since their diversity is too numerous, all bacteria have an individual shape:
- spherical cocci;
- bacillus or bacillus;
- spirally twisted spirochetes.
Not all microorganisms are sensitive to the effects of oxygen compounds.
This is also their distinguishing feature:
- aerobic. Need oxygen;
- anaerobic. Capable of obtaining sufficient energy without the participation of oxygen microorganisms.
In addition to the external and internal composition, they are also distinguished by the way they affect the human body:
- pathogenic. With their participation, the process of bacterial infection occurs. Either by contact, or from the external environment;
- conditionally pathogenic. They are constantly in the body. They cause diseases only under the influence of certain conditions, such as a decrease in immunity, the penetration of microbes;
- non-pathogenic. Adapted to the normal healthy microflora of the body. They are not sources of disease, exclude interaction with other microbes and viruses.
These are the microorganisms that actually exist: useful and dangerous.
They are not all the same, so do not confuse them.
The process of bacterial infection

The decline in immunity caused by infections will certainly lead to activation. But not all of them are only in our body.
Many of them enter the human body from the outside:
- traditional for viruses and infections - airborne method of infection of the body. Occurs through the ambient air by aerobic representatives, as well as through dust in poorly ventilated areas; through public goods. Hygiene products, towels, toys, dishes;
- water environment. Naturally, water bodies are polluted with waste and the consequences of improper human activity. This also applies to poorly boiled drinking water, wells;
- soil interaction. These are suburban areas, suburban areas, flower beds. Putrefactive bacteria live here;
- products. wild yeast, mold, salmonella;
- defeat of the fetus of the unborn child in the womb;
- sexually.
In order for the process of bacteria to enter, certain conditions are necessary.
Provoke infection:
- decline in immunity;
- warm or hot season. Bacteria are temperature sensitive. An indicator from +4 ° C is considered ideal;
- a large number of individuals.
To avoid the consequences of the penetration of pathogenic bacteria, vaccination can be carried out, which will prevent their development in the body and produce antibodies.
Intestinal bacteria in the human body

Microorganisms live in the normal healthy microflora of the gastrointestinal tract. They peacefully coexist with the human body.
What is a healthy intestine and its natural microflora:
- bacteroids. Can provoke the appearance of toxic infections, abscesses, pneumonia;
- bifidobacteria. They prevent the entry of toxins from the external environment. Protect and prevent the growth and spread of pathogenic and opportunistic microorganisms, enhance the synthesis of protein, nicotinic, folic, pantothenic acid, riboflavin, thiamine or B vitamins. Activate the ability of the intestinal mucosa to absorb vitamin D, iron and calcium;
- enterococci. Causative agents of heart problems spread through the blood;
- clostridia. The source of the strongest poison is botulinum toxin. Poisoning results in serious illnesses like tetanus and gas gangrene;
- pathogens, enterobacteria. Prominent representatives of this group are plague, E. coli, salmonella and others. Disrupt the work of all body systems, destroy tissues;
streptococci. Contribute to the appearance pneumococcal infections, toxic damage to internal organs; - staphylococci. Can cause purulent inflammatory infections, sepsis, conjunctivitis. Leads to diseases of the genitourinary system;
- lactobacilli. Represent lactic acid bacteria. Normalize stable intestinal microflora.
All of the above microorganisms constantly live in the human gastrointestinal tract. In a healthy person, they do not appear, since bifidobacteria and lactobacilli inhibit them and activate protection.
What bacteria cause bowel disease

Not all microorganisms are equally useful and harmless. Some of them are in the external environment, but when they enter the body, they lead to infectious inflammatory processes. They can also enter other organs.
Then they become dangerous:
- Escherichiosis. Become the cause of diarrhea, inflammation of the mucous membrane of the colon. Provoke colitis, acute intestinal infections. Can be transferred to other organs and cause sepsis, pneumonia;
- Coli infection. The main sources of manifestations of enteritis, gastroenteritis, dysentery. Complications occur in the form of cystitis, meningitis, vomiting, strong pain in the abdomen.
Pronounced indicators of the presence of bacteria in the human body are possible diseases they call:
- Peretonitis. The entry of pathogenic bacteria and intestinal microflora into abdominal cavity from the gastrointestinal tract;
- Colpitis. The source of the appearance can be bacteria, such as streptococci, staphylococci, Haemophilus influenzae, chlamydia, Trichomonas. It proceeds as an inflammation of the vaginal mucosa. Penetrates into female organs reproductive system through infection by sexual intercourse. The consequences can be infertility, erosion of the cervix;
- Prostatitis. The infectious route of infection involves the penetration of Escherichia and Pseudomonas aeruginosa, as well as bacteria, such as enterococci, Klebsiella, into the pelvic organs;
- Dysbacteriosis. It is observed when the microflora is inhibited by potent antibiotics.
To get rid of them, qualified medical assistance is needed.
All microbes, viruses and infections are eliminated only with the help of antibiotics and complex restorative therapy, which is prescribed by the appropriate specialist.
What bacteria live in the mouth

Microflora oral cavity, of course, can not do without its inhabitants. They can be expressed by diseases and emit an unpleasant odor, as well as just being and doing nothing.
Do not forget that only in the absence of proper immunity, diseases caused by certain bacteria progress:
- half of the microflora is made up of streptococci. They populate almost the entire body: respiratory organs, gastrointestinal tract, reproductive system and skin. But in a healthy person, they do not appear. With a decrease in the body's defenses, bacteria lead to tonsillitis, pneumonia, peritonitis, boils, scarlet fever, rheumatism and toxic shock. This list is quite large. Until defeat of cardio-vascular system and kidneys. They cause the main harm to tooth enamel, lead to caries;
- Pneumococcus. Children's institutions become the most favorable environment for its launch. It is the child who manifests pneumonia, peritonitis, middle ear disease. In severe advanced forms, many diseases that cause certain bacteria begin to actively progress. The result is meningitis, arthritis;
- gingivalis. They do not act until a certain point, although they are constantly in the mouth. They provoke only inflammation of the tissues around the tooth, periodontitis;
- treponema denticolum. The gums became their habitat. Become the cause of periodontal disease under certain conditions.
These bacteria, unfortunately, cause most of the diseases that occur in the oral cavity associated with teeth and gums.
Bacteria can live on the skin

The skin has become the most favorable place for microorganisms. This and hair follicles, and keratinized areas, and numerous folds.
The bacterial layer located on the surface of the epidermis is quite dense.
- streptococci. Bacteria common in almost all systems. But there are many of them on the upper layer of the epidermis. Lead to toxic poisoning of the skin. Able to provoke purulent formations. Accompanying symptoms are always headaches, vomiting, nausea and a sharp increase in temperature. Worse the condition in diseases like tonsillitis;
- skin staphylococci, disease-causing like cellulitis, mastitis, abscesses, styes. During exacerbations spread sepsis, toxic shock. Also often provoke a bacterial type of arthritis, diseases of the urinary system, joints, muscle tissue;
You cannot completely get rid of them. They live on a person all his life from the moment of birth and do no harm until favorable conditions for this occur.
Diseases can be caused by fungi on the skin

Mold is also related to bacteria. Molds are often referred to by their characteristics as bacteria. Skin diseases equally can be called by these two representatives.
Fungi are located mainly in the same places where other microorganisms of the epidermis live: on the folds, at the base of the hair, in the area of dead skin:
- trichophyton. They affect unprotected parts of the body, live in hay, straw. Lead to dermatological diseases in the knees, buttocks, gradually spread throughout the body;
- yeast provoke lichen, seborrhea. Observed in areas of the head, beard, eyebrows, in the anus;
- known representative of the genus Candida. It becomes the cause of candidiasis, which harms not only the skin, but also the mucous membranes of external and internal organs. Often leads to mycoses. In children provokes diabetes, goes into somatic pathology;
- genus Trichophyton rubrum. Causes diseases affecting the surfaces of the feet, areas between the fingers, nails, gradually covers the entire body;
- Pityrosporum orbiculare. These fungi spread to areas where sebum accumulates. Violate the full-fledged work of the sebaceous gland;
- dermatophytes. Fungal and dermatological problems are characteristic of the large distribution of these representatives on the skin;
- microsporum. The carrier of this genus of fungi are stray dogs and cats. Children are more susceptible to infection by these representatives. The lesion occurs in the area of vellus hair.
Bacteria that cause diseases

Infectious diseases caused by microbes are quite common. When interacting and favorable conditions affect important systems in the human body.
They can be conditionally divided according to distribution in the body:
- respiratory diseases;
- intestinal infections;
- diseases of the circulatory system;
- skin infections;
- sexual inflammatory processes and others.
Consider the most dangerous and those that doctors most often have to deal with. These major infectious diseases are caused by bacteria.
Whooping cough. The cause is the Borde-Jangu bacterium. Appears in strong persistent cough. Seen in younger and older children school age. Transmitted through the air. Duration - up to 14 days.
Tuberculosis. The disease is caused by Koch's wand. Affects the lungs, less often the digestive tract. The patient has cough, sweating, fever. It flows in open and closed forms. Infection is possible by airborne droplets.
Gonorrhea. Infectious lesions of the genital and urinary organs, less often - the rectum and oropharynx. The disease is caused by gonococcus. Refers to venereal diseases. Transmission occurs in the process of intimate contact.
Syphilis. Treponema pallidum is the carrier of this venereal infection. It leads to a violation of the mucous membranes of the genital, urinary organs, bones, nervous system.
Tetanus. It can be caused by microorganisms and acquires sharp shape infectious lesions of the skeleton, muscles, nervous system. Immunity to tetanus does not develop. After recovery, I recommend getting vaccinated to prevent re-infection.
Cholera. The causative agent is Escherichia coli Vebrio cholerae. The fecal-oral route of entry into the body is characteristic. Provokes watery diarrhea, dehydration, death.
Common food poisoning caused by bacteria. The main reason is salmonella. gets into digestive system and leads to intoxication of the body and the gastrointestinal tract.
Dysentery. call can intestinal infection Shigella, Shigella. Poisons the body, affects the intestines and stomach, leads to a decrease blood pressure, the appearance of mucus in feces, bleeding and fever.