Symptoms of COPD - a dangerous disease masking for ordinary fatigue. Chronic obstructive pulmonary disease. COPD (J44) disease obstruction of the lungs and how to treat it
Definition.
Chronic obstructive pulmonary disease (COPD) - the disease characterized by partially irreversible, steadily progressive restriction of the air flow caused by an anomalous inflammatory response of lung tissue to the damaging factors of the external environment - smoking, inhalation of particles or gases. Under the term "COPD" imply a combination chronic bronchitis and lung emphysema.
Important provisions on COPD are set out in an international document drawn up by experts from 48 countries - "Global Purchase Initiative for Chronic Obstructive Lung Diseases - Gold, 2003". It should be noted key provisions on COPD.
COPL stopped being collective concept (chronic obstructive bronchitis, heavy forms bronchial asthma, binding bronchitis, fibrosis, etc.);
The concept of COPD does not apply only to patients with a terminal degree of respiratory failure;
The concept of "chronic obstructive bronchitis" is absorbed by the concept of "chronic obstructive pulmonary disease."
RELEVANCE.
Currently, COPD ranks fourth in the structure of the causes of mortality in the world with the predicted growth of prevalence and mortality in the coming decades. According to the study of Global Burden of Disease Study (Global Disease Damage): COPD prevalence in 1990 was 9.34 per 1000 men and 7.33 per 1,000 women (Gold, 2003). Data on prevalence, soreness and mortality from COPDs significantly underestimate the overall damage from the disease, because Usually the COPD is not recognized and is not diagnosed until it becomes clinically significant. A significant increase in widespread damage from COPD over the past 20 years reflects an increase in smoking of tobacco, as well as a change in the age structure of the population.
Risk factors COPD. Internal factors:
Genetic factors (insufficiency of alpha-1-antitripxin);
Hypersensitivity of the respiratory tract;
Height of the lungs.
External factors:
Smoking tobacco;
Professional dust and chemicals;
Home and external air pollutants;
Infections;
Socio-economic status.
Etiology and pathogenesis.
The development of the COPD can be hereditaryly determined with the congenital deficit of alpha 1 -anttripsin, but more often it is due to active or passive smoking, air pollution, long-term effects of professional factors (dust, couples, chemical stimuli), unfavorable atmosphere of dwelling (kitchen chad, household chemicals ). The pathogenetic basis of the COPD is a chronic inflammatory process of tracheosobronchial wood, pulmonary parenchyma and vessels, at which increased quantities of macrophages, T-lymphocytes and neutrophils are detected. Inflammatory cells highlight a large amount of mediators: leukotriene B4, interleukin 8, tumor necrosis factor and other capable of damaging the structure of the lungs and maintain neutrophilic inflammation. In addition, in the pathogenesis of COPDs, the imbalance of proteolytic enzymes, antiprooteinase and oxidative stress have the value.
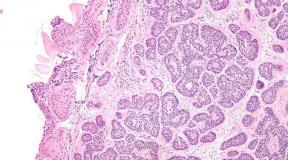
Morphologically in the tracheobronchial trees inflammatory cells infiltrate the surface epithelium. The mucous glands are expanding, and the number of glassworm cells increases, which leads to the hypersection of mucus. In small bronchops and bronchioles, the inflammatory process occurs cyclically with structural remodeling of the bronchial wall, characterized by an increase in the content of collagen and the formation of scar tissue, leading to the resistance resistance resistance.
In the development of COPD there is a consistent stage: the disease begins with a mucus hypersecretion, followed by a violation of the functions of the fiscal epithelium, develops bronchial obstruction, which leads to the formation of lung emphysema, impaired gas exchange, respiratory failure, pulmonary hypertension and development light Heart. The data for reasons, pathogenesis, morphology show that COPD is the result of chronic bronchitis, long bronchospast syndrome and / or emphysema of light and other parenchymal destruction (including congenital) associated with a decrease in the elastic properties of the lungs.
Chronic hypoxia leads to compensatory erythrocytosis - secondary polycythemia with a corresponding increase in blood viscosity and microcirculation disorders, which exacerbate ventilation and perfusion inconsistencies.
To the increasing of all signs of the disease leads an aggravation of the infectious process in the respiratory system. In terms of mukostasis, local, and sometimes systemic immunodeficiency, the colonization of microorganisms may take an uncontrollable nature and move into a qualitatively different form of relationship with macroorganism - an infectious process. Another path is possible - the usual contamination of the air-droplet by the high-voluminous flora, which is easily implemented in the conditions of impaired protective mechanisms. It should be emphasized that the bronchopulmonary infection is also frequent, but not the only reason for the development of exacerbation. Along with this, exacerbations of diseases associated with an increased action of exogenous damaging factors are possible, or in connection with inadequate exercise. In these cases, the signs of infectious damage to the respiratory system are minimal. As it progressing, COPLE gaps between exacerbations become shorter.
Classification Cobl(Gold, 2003)
0 - Risk of disease development:
Normal spirometry;
Chronic symptoms (cough, sputum products);
I - Easy current:
FEV 1 / Fire<70% от должного;
The presence or absence of chronic symptoms (cough, sputum);
II - medium-free current:
FEV 1 / Fire<70% от должного;
50% ≤ofv 1<80% от должных значений;
III - a difficult course:
FEV 1 / Fire<70% от должного;
30% ≤ofv 1<50% от должных значений;
The presence or absence of chronic symptoms;
IV - extremely difficult course:
FEV 1 / Fire<70% от должного;
OFV 1 ≤30% of the proper or FEV 1<50% от должного в сочетании с хронической дыхательной недостаточностью (PaO2≤60% мм рт. ст. и/или PaCO 2 ≥ 50 мм рт. ст.);
The presence of cough, sputum, shortness of breath, clinical signs of destroying failure.
CLINIC.
The clinical picture of the COPD is characterized by the same type of clinical manifestations - coughing and shortness of breath, despite the heterogeneity of the diseases, its components. The degree of their severity depends on the stage of the disease, the rate of progression of the disease and the predominant level of damage to the bronchial tree.
The rate of progression and severity of symptoms of COPD depends on the intensity of the impact of etiological factors and their summation. Thus, in the standards of the American Thoracic Society, it is emphasized that the emergence of the first clinical symptoms in patients with COPDs is usually preceded by smoking at least 20 cigarettes per day for 20 or more.
The first signs with which patients usually turn to the doctor are cough and shortness of breath, sometimes accompanied by whistling breathing with sputum release. These symptoms are more pronounced in the morning.
The earliest symptom that appears to 40-50 years of life is cough. By the same time, episodes of respiratory infection are beginning to occur in the cold seasons, which are not binding to one disease at first. Dyspnea, felt during exercise, occurs on average 10 years later the appearance of cough. However, in some cases, the debit of diseases with shortness of breath is possible.
The sputum is highlighted in a small (rarely\u003e 60 ml / day) quantity in the morning, has a mucosa. The exacerbations of infectious nature are manifested by the aggravation of all signs of the disease, the appearance of purulent sputum and an increase in its number.
Dyspnea can vary in very wide limits: from the sensation of lack of air with standard physical exertion to severe respiratory failure.
A number of patients with COPD is observed obstructive apnea syndrome in a dream. The combination of bronchial obstruction characteristic of COPD, with a night apnea is called cross-syndrome (Overlap Syndrom), in which the maximum expressions of gas exchange. It is believed that most patients have chronic hypercupnia formed mainly at night.
Two clinical forms of the disease are distinguished - emphysematous and bronchitic.
The emphysematous shape (type) of COPD is associated mainly with a panacinarian emphysema. Such patients are figuratively called "pink puffers", since to overcome the prematurely the upcoming expiratory collapse of the bronchi, the exhalation is made through the lips folded into the tube and is accompanied by peculiar puff. In the clinical picture prevails shortness of breath in peace due to a decrease in the diffusion surface of the lungs. Such patients are usually thin, the cough is more often dry or with a small amount of thick and viscous sputum. Pink color, because Sufficient blood oxygenation is maintained by the maximum possible increase in ventilation. The ventilation limit is achieved at rest, and patients are very poorly carrying physical exertion. Pulmonary hypertension is moderately expressed, because The reduction of the arterial channel caused by atrophy of the interlimoolar partitions does not reach considerable values. The pulmonary heart is compensated for a long time. Thus, the emphysematous type of COPD is characterized by the predominant development of respiratory failure.
The bronchitic form (type) is observed in centricular emphysema. Permanent hypersecretion causes an increase in resistance to inhale and exhale, which contributes to a significant violation of ventilation. In turn, a sharp decrease in ventilation leads to a significant decrease in the content of 2 in alveoli, a subsequent impaired of perfusion-diffusion ratios and blood shunting. This causes the characteristic blue shade of diffuse cyanosis in patients of this category. Such patients are fat, cough prevails in the clinical picture with abundance of sputum. Diffuser pneumosclerosis and oblusting the lumen of blood vessels lead to the rapid development of the pulmonary heart and its decompensation. This is facilitated by persistent pulmonary hypertension, significant hypoxemia, erythrocytosis and constant intoxication due to a pronounced inflammatory process in bronchi.
The allocation of two forms has prognostic value. Thus, in the emphysematous type in later stages, the pulmonary heart decompression occurs in comparison with the bronchtic version of the COPD. In the clinical conditions, patients with a mixed type of disease are more common.
COVER CLOSITION According to severity severity allocates a number of diseases of the disease. Stage 0. means an increased risk of COPD development. It is characterized by the appearance of symptoms (cough, sputum products) with normal indicators of the ventilation function of the lungs and actually corresponds to chronic bronchitis. With the easiest course of the COPD ( stage I.) and minimal clinical signs (cough, wet) are recorded obstructive violations. With a moderate course of COPD ( stage II.) The more pronounced obstructive disorders of pulmonary ventilation are recorded, and besides coughing and wet branch, shortness of breath appears, which indicates the development of respiratory failure. With severe and extremely severe COPD ( stage III-IV) There is chronic respiratory failure and signs of the pulmonary heart (destroying failure). Obstructive violations detected in the study of the ventilation function of the lungs can reach critical values.
The main features allow to suspect COPD.
Chronic cough
Intermitting or daily. It often happens throughout the day.
Chronic spending sputum
Any case of chronic wet wet can indicate COPD.
Dyspnea
Progressive, persistent. Enhanced with exercise and respiratory infections.
The impact of risk factors in history
Smoking tobacco, professional pollutants and chemicals. Smoke from kitchen and heating at home.
If there is any of the listed features, COPL should be suspected and conduct a study of the function of external respiration.
Anamnesis smoking
A prerequisite for the diagnosis of COPD, on the WHO Recommendation, is counting the index of a smoking person. The calculation of the index of a smoking person is carried out as follows: the number of cigarettes dropped on the day multiply by the number of months a year, i.e. by 12; If this value exceeds 160, then smoking in this patient represents the risk regarding the development of COPD; If the values \u200b\u200bof this index are exceeded, more than 200 patients should be attributed to the category of "malicious smokers".
Anamnesis of smoking is recommended to calculate in units of "pack / years". Anamnesis of smoking should include counting the number of cigarettes digitized per day multiplied by the number of years and, thus, the total number of packages / years of smoking is calculated. In this case, one pack contains 20 cigarettes and the number of cigarettes smoked per day for one year is equal to one pack / year.
Total number of packs / years \u003d quantity of cigarettes of cigarettes per day x number of years / 20
It is believed that if this value exceeds 25 packs / years, then the patient can be attributed to "malicious smokers." In the event that this indicator reaches 10 packs / years values, the patient is considered a "unconditional smokers." The patient is considered a "former smokers" in case of cessation of smoking for a period of 6 months or more. This must be taken into account when diagnosing COPD.
Objective study.
The results of an objective study of COPD patients depend on the severity of bronchial obstruction and emphysema.
Inspection. In the later stages of COPL, the clinical signs of the lung emphysema (increased front-base chest size, extended intercostal intervals). With a pronounced emphysema, the appearance of the patient changes, the barrel-shaped shape of the chest appears. Due to the expansion of the chest and the displacement of the top of the neck of the neck, it seems short and thickened, the permissible holes are made (filled with extended pulmonary tops). In the development of chronic respiratory failure and pulmonary hypertension, "warm" acricyanosis, swollen cervical veins are noted.
Percussion. In the presence of emphysema - a percussion box sound, expanding the lung boundaries. In cases of pronounced emphysema, absolute dullness of the heart can not be completely determined. The edges of the lungs are shifted down, their mobility is limited when breathing. As a consequence, a soft painless edge of the liver can perform from under the edge of the rib arc during its normal sizes.
Auscultation.In the lungs, scattered dry wheezes of various tides are heard. As the disease progressing, a whistling breathing is joined, the most tangible with an accelerated exhale. Sometimes auscultative phenomena in the lungs are not determined and to identify them it is necessary to offer a patient to make a forced exhalation. The aperture of the diaphragm is limited in pronounced emphysema, which leads to a change in the auscultation pattern: weakened breathing appears, the severity of wheezing decreases, exhale extends.
The sensitivity of objective methods to determine the severity of Cobl is small. Among classic signs, a whistling exhale and exhaust exhalation time can be called (more than 5 seconds), which indicate bronchial obstruction.
DIAGNOSTICS.
Diagnostic methods can be divided into a mandatory minimum used in all patients, and additional methods applied by special testimony.
Subject to mandatory methods, in addition to physical, include the definition of the function of external respiration (FVD), blood test, cytological examination of sputum, radiographic examination, blood test and ECG.
Laboratory research methods.
Survey study.
The cytological study of sputum provides information on the nature of the inflammatory process and its severity. It is a mandatory method.
The microbiological (culture) study of sputum is advisable to carry out with an uncontrolled progression of the infectious process and the selection of rational antibiotic therapy. It is an additional method of examination.
Blood research.
Clinical analysis. With a stable flow of COPL of significant changes in the content of peripheral blood leukocytes, it does not occur. In exacerbation, neutrophilic leukocytosis with a harsh shift and an increase in ESP are most often observed. However, these changes are not always observed.
With the development of hypoxemia in patients with COPDs, polycytemetic syndrome is formed, which is characterized by a change in hematocrit (hematocrit\u003e 47% in women and\u003e 52% in men), an increase in the number of erythrocytes, a high level of hemoglobin, low ESO and an increased blood viscosity.
X-ray study Chest organs is a mandatory examination method. When the lung radiography in direct and lateral projections at COPDs, an increase in the transparency of the pulmonary fabric is found, the low standing of the diaphragm dome, the limitation of its mobility, an increase in the retrosternal space, which is characteristic of emphysema.
With a mild COPD, significant radiographic changes may not be found. In patients with medium and severe COPD, the low standing of the diaphragm dome, flattening and restriction of its mobility, the hypernity of pulmonary fields, bullies and an increase in retrosternal space are possible; The narrowing and extension of the heart shadow; Against the background of depleting the vascular shadows, the high density of the walls of the bronchi is determined, infiltration according to their go, i.e. A number of features that characterize the inflammatory process in the bronchial trees and the presence of emphysema are revealed.
CT scan Easy is an additional method and is carried out according to special testimony. It allows you to quantify the morphological changes in the lungs, first of all, emphysem, more clearly reveal the bulls, their localization and dimensions.
Electrocardiography Allows a number of patients to identify signs of hypertrophy of the right-hand heart departments, but its ECG criteria change dramatically due to emphysema. ECG data in most cases make it possible to exclude the cardiac genesis of respiratory symptoms.
Bronchological research (Fibrobronchoscopy) is an optional for COPD patients. It is carried out to assess the state of the mucous membrane of the bronchi and differential diagnosis with other lung diseases. In some cases, diseases that are the cause of chronic bronchial obstruction can be identified.
The study must include:
Inspection of the mucous membrane of the bronchi;
Culture study of bronchial content;
Bronchoalveolar lavage with the determination of cellular composition to clarify the nature of inflammation;
Biopsy of the mucous membrane of the bronchi.
Research Function Function (Spirography) has a leading importance in the diagnosis of COPD and an objective evaluation of the severity of the disease. The determination of the following volumetric and high-speed indicators is obligatory: the life capacity of the lungs (jerking), the forced life capacity of the lungs (freak), the volume of the forced exhalation in 1 second (FEV 1), the maximum exhalation rate at the level of 75, 50 and 25% (MCV 75- 25). The study of these indicators forms functional diagnosis of COPD.
Functional disorders for COPD are manifested not only by impaired bronchial patency, but also by changing the structure of static volumes, violation of elastic properties, the diffusion capacity of the lungs, with a decrease in physical performance. The definition of these disorders is optional.
Violation of bronchial patency.The most important for the diagnosis of COPD is the definition of chronic airflow limit, i.e. Bronchial obstruction. The main criterion that determines the chronic airflow limit, or chronic obstruction, is the drop in the indicator of FEV 1 to the level of less than 80% of the proper values. Bronchial obstruction is considered chronic if it is registered when conducting repeated spirometric studies at least 3 times within one year, despite the therapy.
To study the reversibility of obstruction, samples are used with inhalation bronchoditators, and their effect is estimated on the flow-volume curve indicators, mainly on the volume of forced exhalation in 1 second (FEV 1) during the examination of a particular patient with COPDs it must be remembered that the reversibility of obstruction - the value of the variable And the same patient can be different during periods of exacerbation and remission.
Bronnorate tests. As an armored drugs, when conducting tests in adults, it is recommended to assign:
Beta-2. - short-acting agonists (starting with a minimum dose to the maximum allowable: phenoterol - from 100 to 800 μg; salbutamol - from 200 to 800 μg, terbutal - from 250 to 1000 μg) with a measurement of the broutine response after 15 minutes;
Anticholinergic preparations - as a standard drug, it is recommended to use the ipratropium bromide, starting with minimal doses - 40 μg to the highest possible doses - 80 μg, with a measurement of the brightness response after 30-45 minutes.
It is possible to carry out bright tests by appointing higher doses of drugs that are inhaled through nebulizers.
To avoid the distortion of the results and for the correct implementation of the bronchodial test, it is necessary to cancel the therapy in accordance with the pharmacokinetic properties of the received drug (beta-2 - short action agonists - for 6 hours before the test, long-acting beta-2 - agonists - for 12 hours, prolonged theophyllins - in 24 hours).
The increase in FEV 1 by more than 15% of the initial indicators is conditionally accepted to characterize as reversible obstruction.
Monitoring 1 . An important method that allows you to confirm the diagnosis of COPD is the monitoring of FEV 1 - a perennial re-measurement of this spirometric indicator. In a mature age, the annual fall of the FEV 1 is noted within 30 ml per year. Large epidemiological studies conducted in different countries made it possible to establish that for COPD patients are characterized by an annual drop in the indicator of FEV 1 more than 50 ml per year.
Gas composition of blood. COPL is accompanied by a violation of ventilation and perfusion ratios, which can lead to arterial hypoxemia - a decrease in oxygen voltage in arterial blood (RAO2). In addition, ventilation respiratory failure leads to an increase in the voltage of carbon dioxide in arterial blood (Raso2). In patients with COPD with chronic respiratory failure, the occurring acidosis is metabolically compensated by increased hydrocarbonate products, which allows maintaining a relatively normal pH level.
Pulse oximetry It is used to measure and monitor blood saturation with oxygen (SAO2), however, it makes it possible to register only the level of oxygenation and does not allow to monitor changes to RAS2. If the SAO2 indicator is less than 94%, then the study of blood gases is shown.
In progression of COPD, it is often often observed an increase in pressure in the pulmonary artery.
The severity of pulmonary hypertension has prognostic value. Among the non-invasive methods for controlling pulmonary hypertension, the best results were obtained using dopplerhocardiography. In the usual practice of conducting patients with COPD, the use of direct methods for measuring pressure in the pulmonary artery is not recommended.
Differential diagnosis.
In the early stages of the development of COPD, chronic obstructive bronchitis (hob) and bronchial asthma (BA) should be distinguished, since at this time there are fundamentally different approaches to the treatment of each of these diseases.
The clinical examination detects the scents of symptoms with Ba is often with a combination of extrapulmonary signs of allergies (rhinitis, conjunctivitis, skin manifestations, food allergies). For patients, Kob is characterized by a constant, a little changing symptoms.
An important element of the differential diagnosis is the decrease in FEV 1 per 50 ml in patients with hob, which is not observed at ba. For hob, a reduced daily variability of picofloumometry indicators< 15%. При БА разность между утренними и вечерними показателями пикфлоуметрии повышена и превышает 20%. При БА чаще наблюдается бронхиальная гиперреактивность. Из лабораторных признаков при БА чаще встречается увеличение содержания IgЕ. При появлении у больных БА необратимого компонента бронхиальной обструкции, дифференциальный диагноз этих заболеваний теряет смысл, так как можно констатировать присоединение второй болезни – ХОБ и приближение конечной фазы заболевания – ХОБЛ.
TREATMENT.
The aim of treatment is to reduce the rate of progression of the disease leading to the increase in bronchial obstruction and respiratory failure, reducing the frequency and duration of exacerbations, improving the tolerance for physical exertion and improving the quality of life.
Training of patients - Responsible stage of individual work with patients. The patient should be well aware of the essence of the disease, the peculiarities of his current, to be an active, conscious participant in therapeutic process. Educational programs for patients necessarily include teaching the right use of drugs (individual inhalers, spacers, nebulizers). Patients should be trained by the basic rules of self-control, including using picofloumometer, should be able to objectively assess their condition and, if necessary, to take measures of urgent self-help. An important stage of patient education is their professional orientation, especially in cases where environmental aggression is related to the professional activities of the patient.
Termination of smoking - The first mandatory step. The patient should clearly realize the harmful effect of tobacco smoke on its respiratory system. A specific limitation program for smoking is compiled. In cases of nicotine addiction, the use of nicotine-substituting drugs is advisable. It is possible to attract psychotherapists, needleflexotherapists. The positive effect of non-smoking is expressed in any stage of COPD.
Bronching therapy.
According to modern ideas about the essence of COPD, bronchial obstruction is the main and universal source of all pathological events developing in constant progression of the disease and leading to respiratory failure.
The use of armored drugs - basic therapy, mandatory in the treatment of COPD patients. All other means and methods should be applied only in combination with the means of basic therapy.
Preference is given to the use of inhalation forms of broncholists. The inhalation route of administration of drugs contributes to a more rapid penetration of the drug into the affected organ, consequently more efficient drug influence. At the same time, the potential risk of developing side system effects is significantly reduced. The use of the spacer allows: to facilitate the implementation of inhalation, increase its efficiency, further reduce the potential risk of systemic and local side effects.
The optimal to date is the use of powder inhalers or bronchodilics in solutions for nebulizer therapy.
From the existing bronchusshiring agents in the treatment of COPDs use M-cholinolites, beta-2-agonists and methylxantins; The sequence of application and the combination of these means depends on the severity of the disease, the individual characteristics of its progression.
Traditionally, basic armor-taiters for the treatment of COPD are considered m-cholinolitiki. They are represented by bromide ypratropy (duration of 6-8 h) and a combined broth-tutorial - Berodual (bromide + phenoterol and ipratopia). Currently there is a new cholinolitic prolonged action, Tiotropia Bromide (Spiriva), which is used 1 time per day.
Are used selective sympathomimetics (beta-2-agonists) Short (4-6 h) Actions: Fenoterol, Salbutamol, Terbutalin. The action of sympathomimetics occurs quickly, but they are characterized by a number of systemic side effects due to the impact on the cardiovascular system. With age, the sensitivity of receptors to sympathomimetics is reduced. In recent years, the new drug from the Beta-2-agonist group has become widely used to relieve the Bapton obstruction and basic therapy, the active substance of which is formoterol, which possesses not only the rapid start of action (after 1-3 minutes), but also lasting Effect (for 12 hours or more).
Theophyllins Prolonged action (Teotard, Teopek) is effective in the treatment of COPD and are currently used quite widely as in the form of monotherapy and in addition to sympathomimetics. But due to their narrow facet between therapeutic and toxic doses, preference is given to inhalation broutine.
In the I stage of the COPD, bright action briefs are used. In stage II-IV, a systematic use of one bright or long-term effect with a quickly upcoming effect is appointed (or a combination of drugs). Inhalation corticosteroids are used if clinical and ventilation indicators are significantly improved when applied.
Magaze regulatory products. Improving mukiciliary clearance is largely achieved with a focused impact on the bronchial secret with the use of muggy regulatory drugs.
The use of proteolytic enzymes as the musolithic means is unacceptable due to the high risk of developing serious side effects - hemoptia, allergies, bronchokonstriction. Ambroxol (Ambrosan, Lazolyvan) stimulates the formation of tracheobronchial secretions of low viscosity due to the depolymerization of acid mucopolisaccharides of the bronchial mucus and the production of neutral mucopolysaccharides by glass-like cells.
A distinctive feature of the drug is its ability to increase the synthesis, the secretion of the surfactant and block the decay of the latter under the influence of adverse factors.
When combined with antibiotics, ambroxol enhances their penetration into the bronchial secret and mucous membrane of the bronchi, increasing the effectiveness of antibacterial therapy and reducing its duration. The drug is used inside and in inhalations.
Acetylcistein Free from damaging proteolytic enzymes. Sulfhydryl groups of its molecules tear the disulfide bonds of sputum mucopolysaccharides. Stimulation of amusing cells also leads to springs. Acetylcysteine \u200b\u200bwill increase the synthesis of glutathione participating in the detoxification processes. It is used inside and in inhalations.
Carbocystein Normalizes the quantitative ratio of the acidic and neutral sialomycins of the bronchial secret. Under the influence of the drug, the regeneration of the mucous membrane occurs, a decrease in the number of glazing cells, especially in terminal bronchops, i.e. The drug has flourishing and musually effects. This restores the secretion of IGA and the number of sulfhydryl groups. It is used inside.
Glucocorticosteroid therapy. The testimony for the use of GKS at COPD is the ineffectiveness of maximum doses of funds of basic therapy - bronchoids. GCS, so effective in the treatment of bronchial asthma, used in COPL therapy only with a proven clinical or spirometric effect. The reversibility test is formulated, which makes it possible to predict the feasibility of the appointment of corticosteroids: after the initial definition of FEV 1, corticosteroids are prescribed orally (for 1-2 weeks) or inhalation (for a period of 6-12 weeks). An increase in FEV 1 by 15% (or 200 ml) after the test use of steroids is considered as a positive result and gives the basis for long-term therapy in inhalation corticosteroids. This test can also be carried out with picofloometer (the increase in the power of the exhalation by 20% is considered positive).
The use of GKS in tablets for more than 2 weeks is undesirable. Optimally use inhalation GCS or solutions (suspensions) for nebulizers (for example, pulmikart suspension). With severe and extremely severe COPD ( stage III-IV) As a basic therapy, it is recommended to use a combined drug symbicant, which includes GKS Budfestonide and the Beta-2-agonist of long-acting formoterol.
In the treatment of exacerbations of COPD of Middle and severe, the use of nebulizer therapy is necessary. The nebulizer makes it possible to inhalation administration of bronchology and glucocorticosteroid hormones in high doses.
Correction of respiratory failure It is achieved by using oxygen therapy, respiratory muscles. It should be emphasized that the intensity, the volume and nature of drug treatment depends on the severity of the state and the ratio of the reversible and irreversible components of the bronchial obstruction. When the reversible component is depleted, the nature of the therapy is changing. Methods aimed at correction of respiratory failure are first place. In this case, the volume and intensity of basic therapy persist.
Indication K. systematic oxygenotherapy is to reduce the partial tension of oxygen in the blood - PAO2 to 60 mm Hg. Art., Reducing oxygen saturation - SAO2< 85% при стандартной пробе с 6-минутной ходьбой и < 88% в покое. Предпочтение отдается длительной (18 часов в сутки) малопоточной (2-5 л в мин) кислородотерапии как в стационарных условиях, так и на дому. При тяжелой дыхательной недостаточности применяются гелиево-кислородные смеси. Для домашней оксигенотерапии используются концентраторы кислорода, а также приборы для проведения неинвазивной вентиляции с отрицательным и положительным давлением на вдохе и выдохе.
Training of respiratory muscles It is achieved with the help of individually selected respiratory gymnastics. It is possible to use percutaneous electrostimulation of the diaphragm.
With pronounced polycytemic syndrome (HB\u003e 155 g / l), it is recommended to conduct erythrocytaffeza With the removal of 500-600 ml of the deplaced erythrocytic mass. In the event that the erythrocytophoresis is technically impossible, it is possible to carry out blooding In the volume of 800 ml of blood with adequate substitution with an isotonic solution of sodium chloride or gurudotherapy (Treatment with leeches).
Antibacterial therapy. During the period of a stable flow of COPD, antibacterial therapy is not carried out.
In the cold season, in patients with COPDs often arise exacerbations of infectious origin. Most often their reason are Streptococcus Pneumonia, Naemophilus Influenzae, Moraxella Catarralis and viruses. Antibiotics are prescribed in the presence of clinical signs of intoxication, increasing the number of sputum and the appearance of purulent elements in it. Typically, treatment is prescribed empirically from drugs inside and lasts 7-14 days, with severe exacerbation, parenteral administration is used.
Taking into account the specified spectrum of microorganisms, apply:
aminopenicillins inside (amoxicillin),
cephalosporins II-III of generations (cefuroxime inside, ceftriaxone - tripled),
new macrolides inward (spiramycin, clarithromycin, azithromycin, Midekamycin),
respiratory (pneumatic) fluoroquinolones III-IV generations (Levofloxacin).
Selection of an antibiotic for sensitivity in vitro is carried out only with the ineffectiveness of empirical antibiotic therapy.
Antibiotics in inhalations should not be prescribed.
Vaccinationanti influenza (Vaxigrip, Grippol, Inflivak, Begdivak, etc.), against pneumococcus (pneumo 23) reduces the number of exacerbations of the disease and the severity of their flow, thereby reducing the number of disability days and improve the indicators of bronchial patency. Annual prophylactic vaccination against influenza patients with COPDs with light and middle degrees of gravity of the disease at infectious recurrence frequency is more than 2 times a year. A single vaccination pneumo 23 is effective for 5 years, then revaccination is carried out every 5 years.
Rehabilitation therapy.
Rehabilitation therapy is prescribed when COPD of any severity. The doctor defines an individual rehabilitation program for each patient. Depending on the severity, the phase of the disease and the degree of compensation of respiratory and cardiovascular systems, the program includes regime, exercise, physiotherapy procedures, sanatorium-resort treatment.
The obstruction of the lungs is the progressive disease of the broncho-pulmonary system, in which the air in the respiratory tract runs incorrectly. This is due to abnormal inflammation of the pulmonary fabric in response to external stimuli.
This is an non-infectious disease, it is not associated with the vital activity of pneumococci. The disease is common, according to WHO, 600 million people suffer in the world of lung obstruction. Mortality statistics suggests that 3 million people die from illness every year. With the development of megacities, this figure is constantly growing. Scientists believe that after 15-20 years, mortality will double.
The problem of prevalence and incurability of the disease is the absence of early diagnosis. A person does not attach importance to the first signs of obstruction - cough in the morning and shortness of breath, which appears faster than in peer when performing the same physical activity. Therefore, patients are asked for medical care at the stage when it is impossible to stop the pathological destroyer.
Risk factors and disease development mechanism
Who faces obstruction in the lungs and what are the risk factors? In the first place is smoking. Nicotine is several times increases the likelihood of lung obstruction.
Professional risk factors play a major role in the development of the disease. Professions under which a person is constantly in contact with production dust (ore, cement, chemicals):
- miners;
- builders;
- employees of the pulp processing industry;
- railway workers;
- metallurgists;
- grain processing workers, cotton.
Atmospheric particles that can serve as a launcher in the development of the disease - exhaust gases, production emissions, industrial waste.
Also in the occurrence of the obstruction of the lungs plays the role of hereditary predisposition. The internal risk factors refers to the hypersensitivity of the tissues of the respiratory tract, the growth of the lungs.
Special enzymes are widely produced - protease and antiprotease. They regulate the physiological equilibrium of metabolic processes, support the tone of respiratory organs. When the systematic and long-term exposure of air pollutants (harmful air particles) is underway, this equilibrium is broken.
As a result, the skeleton function of the lungs is disturbed. This means that alveoli (lung cells) fall, lose their anatomical structure. The lungs are formed numerous bulls (formations in the form of bubbles). So gradually decreases the amount of alveoli and the rate of gas exchange in the organ falls. People begin to feel pronounced shortness of breath.
The inflammatory process in the lungs is the reaction to pathogenic aerosol particles and the progressive airflow limit.
Lung obstruction stages:
- inflammation of tissues;
- pathology of small bronchi;
- destruction of parenchyma (lung tissues);
- restriction of air flow rate.
Symptoms of lung obstruction
 Obstructive respiratory diseases are characterized by three main symptoms: shortness of breath, cough, sputum isolation.
Obstructive respiratory diseases are characterized by three main symptoms: shortness of breath, cough, sputum isolation.
The first symptoms of the disease are associated with breaking disorders. Man is experiencing a shortage of air. It is difficult for him to rise several floors. A hike to the store takes more time, a person constantly stops to catch his breath. It becomes problematic to get out of the house.
The development system of progressive shortness of breath:
- initial signs of shortness of breath;
- difficult breathing with medium physical activity;
- gradual load limit;
- significant reduction in physical activity;
- shortness of breath with slow walking;
- refusal of physical exertion;
- permanent shortness of breath.
Patients with lung obstruction develops chronic cough. It is associated with partial impassability of bronchi. Cough is permanent, daily, or intermitting, with recession and lifts. As a rule, the symptom is enhanced in the morning and can manifest itself during the day. At night, cough is not worried about man.
A shortness of breath bears a progressive and persistent (daily) character and over time only worsens. It is also enhanced with physical activity and respiratory diseases.
When obstruction of the lungs in patients, sputum is recorded. Depending on the stage and launching of the disease, the mucus may be scarce, transparent or abundant, purulent.
The disease leads to chronic breathing failure - the inability of the pulmonary system to provide high-quality gas exchange. Saturation (saturation of arterial blood oxygen) does not exceed 88%, at a rate of 95-100%. This is a threatening condition for a person's life. At the last stages of the disease in a person at night, apnea can occur - choking, stopping the pulmonary ventilation by more than 10 seconds, on average it lasts half a minute. In extremely severe cases, the respiratory stop lasts 2-3 minutes.
In the daytime, a person feels strong fatigue, drowsiness, the instability of the heart.
The obstruction of the lungs leads to early loss of disability and reduce life expectancy, a person acquires the status of disability.
Obstructive changes in the lungs in children
The obstruction of the lungs in children is developing due to respiratory diseases, malformations of the pulmonary system, chronic pathologies of respiratory organs. An exemplary value has an hereditary factor. The risk of development of pathology increases in the family, where parents are constantly smoking.
The obstruction in children is fundamentally different from the obstruction in adults. The blockage and destruction of the respiratory tract are a consequence of one of the nosological forms (some independent illness):
- Chronical bronchitis. The child has a wet cough, single-caliber wheezes, exacerbations up to 3 times a year. The disease is a consequence of the inflammatory process in the lungs. Initial obstruction occurs due to excess mucus and sputum.
- Bronchial asthma. Despite the fact that the bronchial asthma and chronic obstruction of the lungs are different diseases, they are interrelated in children. Asthmatics fall into the risk risk of obstruction.
- Bronchildren dysplasia. These are chronic pathology in the kids of the first two years of life. The risk group includes premature and low-handed children who have suffered an ARVI immediately after birth. In such babies, bronchiols and alveoli are affected, the functionality of the lungs is disturbed. Respiratory failure and oxygen dependence is gradually. Rough changes of the fabric (fibrosis, cysts) are occurring, bronchi deform.
- Interstitial lung diseases. These are chronic hypersensitivity of the tissues of the lungs to allergenic agents. Developed by inhalation of organic dust. It is expressed by a diffuse defeat of Parenhim and Alveol. Symptoms - cough, wheezing, shortness of breath, ventilation disorder.
- Reputing bronchiolitis. This is a disease of small bronchi, which is characterized by a narrowing or complete blockage of bronchiole. Such obstruction in the child is mainly manifested in the first year of life.. Cause - ORVI, adenoviral infection. Signs - unproductive, heavy, recurrent coughing, shortness of breath, weak breathing.
Diagnosis of lung obstruction
 When handling a person, history (subjective data) is collected to the doctor. Differential symptoms and lung obstruction markers:
When handling a person, history (subjective data) is collected to the doctor. Differential symptoms and lung obstruction markers:
- chronic weakness, reduced quality of life;
- unstable breathing during sleep, loud snoring;
- body weight increase;
- an increase in the circle of the collar zone (neck);
- blood pressure above the norm;
- pulmonary hypertension (increase in pulmonary vascular resistance).
The compulsory examination includes a general blood test for the exclusion of tumor, purulent bronchitis, pneumonia, anemia.
The overall urine analysis helps to exclude purulent bronchitis, in which the amyloidosis is detected - disruption of the exchange of proteins.
A common sputum analysis is rare, as it is non-informative.
Patients are carried out picoflorometer - the functional method of diagnosis, with which the rate of exhalation is estimated. So determine the degree of obstruction of the respiratory tract.
All patients make spirometry - a functional study of external breathing. Evaluate the speed and volume of breathing. Diagnostics are carried out on a special device - spirometer.
In the process of examination, it is important to exclude bronchial asthma, tuberculosis, binding bronchiolitis, bronchiectatic disease.
Treatment of the disease
 Targets for the treatment of lung obstruction multifaceted and include such steps:
Targets for the treatment of lung obstruction multifaceted and include such steps:
- improving the respiratory function of the lungs;
- constant monitoring of symptoms;
- improving physical stability;
- warning and treatment of exacerbations and complications;
- stop progression of the disease;
- minimization of side effects of therapy;
- improving the quality of life;
The only way to suspend the rapid destruction of the lungs is to completely abandon smoking.
In medical practice, special programs to combat nicotine addiction in smokers have been developed. If a person smokes more than 10 cigarettes a day, then he is shown a medical course of therapy - short up to 3 months, long - up to the year.
Nicotine-specific treatment is contraindicated with such internal pathologies:
- heavy arrhythmia, angina, myocardial infarction;
- blood impairment in the brain, stroke;
- ulcers and erosion of the gastrointestinal organs.
Patients are assigned to browillating therapy. Basic treatment includes bronchopholics to expand the respiratory tract. Preparations are prescribed both intravenously and inhalation. When inhalation, the medicine instantly penetrates the affected light, provides a quick effect, reduces the risk of developing negative consequences and side effects.
During inhalation you need to breathe calmly, the duration of the procedure is on average 20 minutes. With deep breaths there is a risk of developing a strong cough and choking.
 Effective bronchoids:
Effective bronchoids:
- methylxantins - Teophilin, caffeine;
- cholinolitics - Atrovant, Berodal, Spiriva;
- b2-agonists - phenoterol, salbutamol, formoterol.
In order to increase survival, patients with respiratory failure are prescribed oxygen therapy (minimum 15 hours a day).
To dilute the mucus, enhancing its deposition from the walls of the respiratory tract and the expansion of the bronchi is prescribed a complex of drugs:
- Givephenesin;
- Bromgexine;
- Salbutamol.
To consolidate treatment, obstructive pneumonia needs rehabilitation activities. Daily patient must conduct physical training, increase strength and endurance. Recommended sports - walking from 10 to 45 minutes daily, exercise bike, lift of dumbbells. The nutrition plays an important role. It must be rational, high-calorie, contain a lot of protein. An integral part of the rehabilitation of patients is psychotherapy.
Modern methods of diagnosis and treatment of COPDModern methods of COPD treatment
Chronic obstructive pulmonary disease
COPD is characterized by the progressive increase in irreversible obstruction as a result of chronic inflammation induced by pollutants, which are based on coarse morphological changes of all lung fabric structures with the involvement of the cardiovascular system and respiratory muscles.
COPD leads to the restriction of physical performance, disabled patients and in some cases to death.
The term "COPD", taking into account all stages of the disease, includes chronic obstructive bronchitis, chronic purulent obstructive bronchitis, lung emphiza, pneumosclerosis, pulmonary hypertension, chronic pulmonary heart.
Each of the terms is chronic bronchitis, lung emphysema, pneumosclerosis, pulmonary hypertension, pulmonary heart - reflects only the peculiarity of morphological and functional changes that occur when COPD.
The appearance in the clinical practice of the term "COPD" is a reflection of the basic law of formal logic - "one phenomenon has one name."
According to the international classification of diseases and the causes of the death of the 10th revision of the COPD encrypted in the coda of the main disease, which led to the development of COPD, - chronic obstructive bronchitis and sometimes bronchial asthma.
Epidemiology. It has been established that the prevalence of COPD and the world among men and women in all age groups is 9.3 and 7.3 per 1000 population, respectively.
For the period from 1990 to 1999 The incidence of COPD among women increased more than men - by 69% compared with 25%.
This information reflects the situation among men and women in the prevalence of the most important risk factor COPD - tobacco-law, as well as the increased role of influence on women's domestic pollutants when cooking and combustion of fuel.
COPD is the only one of the most common diseases in which mortality continues to increase.
According to the National Institute of US health, mortality rates from COPD are small among people under 45 years old, but in older age groups it takes 4-5th place, i.e., it is among the main reasons in the US mortality structure.
Etiology.COPD is determined by the disease that caused it.
At the heart of COPD - a genetic predisposition, which is implemented due to the long exposure to the mucous membranes of the bronchi factors that have a damaging (toxic) action.
In addition, several loci of mutated genes are opened in the human genome, with which the development of COPD is connected.
First of all, this is the deficiency of AranthitripSin - the foundations of the antiprotea activity of the organism and the main inhibitor of elastase neutrophils. In addition to the congenital deficit of A1-antitripsein, the hereditary defects of A1-antichymotrixin, A2-macroglobulin, vitamin-D-binding protein and cytochrome P4501A1 are taken in the development and progression of COPL.
Pathogenesis. If we talk about chronic obstructive bronchitis, then the main consequence of the impact of etiological factors is the development of chronic inflammation. Localization of inflammation and features of trigger factors determine the specifics of the pathological process when hob. Biomarkers inflammation at hob are neutrophils.
They are mostly involved in the formation of a local deficit of antiproteases, the development of "oxidative stress", play a key role in the circuit of the processes characteristic of inflammation, the lead end up with irreversible morphological changes.
An important role in the pathogenesis of the disease plays a violation of mukiciliary clearance. The effectiveness of mukiciliary transport, the most important component of the normal functioning of the airways, depends on the coordination of the action of the clarifier apparatus of the fiscal epithelium, as well as the qualitative and quantitative characteristics of the bronchial secret.
Under the influence of risk factors, the fishing movement is disturbed up to a complete stop, the epithelium metaplasia is developing with the loss of cereal epithelium cells and an increase in the number of glassworm cells. The composition of the bronchial secret is changing, which violates the movement of significant ciliates.
This contributes to the occurrence of a mucostasis that causes the blockade of small air pathways. The change in the viscoelastic properties of the bronchial secret is accompanied by substantial qualitative changes in the composition of the latter: the content in the secret of non-specific components of local immunity, which have antiviral and antimicrobial activity - interferon, lactoferin and lysozyme is reduced. Along with this decreases the content of secretory IGA.
Disorders of mukiciliary clearance and phenomenon of local immunodeficiency create optimal conditions for colonization of microorganisms.
The thick and viscous bronchial mucus with reduced bactericidal potential is a good nutrient medium for various microorganisms (viruses, bacteria, mushrooms).
The entire complex of listed pathogenetic mechanisms leads to the formation of two main processes characteristic of KOB: impaired bronchial patency and the development of centralobular emphysema.
The bronchial obstruction when the hob is made of irreversible and reversible components.
The irreversible component is determined by the destruction of the elastic collagen base of lungs and fibrosis, a change in the shape and obliteration of bronchiol. The reversible component is formed due to inflammation, reducing the smooth muscles of bronchi and mucus hypersecretion. Ventilation disorders at hob mainly obstructive, which is manifested by expiratory breath and decrease in the FEV, indicator reflecting the severity of bronchial obstruction. The progression of the disease, as a mandatory sign of KOB, is manifested by an annual decrease in FEV1 by 50 ml and more.
Classification. Experts of the International Program "Global Initiative for Chronic Obstructive Lung Disease" (GOLD - Global Strategy for Chronic Obstructive Lung Disease) Mix the following stages of COPD:
■ Stage I - Easy Cobl flow. At this stage, the patient may not be noticed that the function of the lungs is broken. Obstructive disorders - the OFV1 ratio to the forced life capacity of the lungs less than 70%, OPV1 more than 80% of due values. Usually, but not always, chronic cough and sputum products.
■ Stage II - COPD of medium-step flow. This is a stage in which patients seek medical care due to shortness of breath and exacerbation of the disease. It is characterized by an increase in obstructive disorders (OPV1 greater than 50%, but less than 80% of due values, the OFV1 ratio to the forced life capacity of the lungs less than 70%). There is a strengthening of symptoms with a breath appearing during exercise.
■ Stage III is a difficult COPD. It is characterized by a further increase in the air flow limit (the OPV1 ratio to the forced life capacity of the lungs less than 70%, OPV1 is greater than 30%, but less than 50% of due values), increasing shortness of breath, frequent exacerbations.
■ Stage IV is an extremely difficult COPD. At this stage, the quality of life is worsens noticeably, and exacerbations may be threatening for life. The disease acquires disabled flow. It is characterized by extremely heavy bronchial obstruction (the OPV1 ratio to the forced vitality capacity of the lungs less than 70%, OPV1 is less than 30% of due vality or OPV1 less than 50% of the proper values \u200b\u200bin the presence of respiratory failure). Respiratory failure: Rao2 less than 8.0 kPa (60 mm Hg) or saturation oxygen less than 88% in combination (or without) RAS2More 6.0 kPa (45 mm Hg). At this stage, the development of a light heart is possible.
The course of the disease. In assessing the nature of the course of the disease, it is important not only a change in the clinical picture, but also determining the dynamics of the fall of bronchial patency. At the same time, the definition of the OTV1 parameter - the volume of forced exhalation in the first second is of particular importance. Normally, with the age of non-smoking, the FEV1 is dropped by 30 ml per year. Smoking reducing this parameter reaches 45 ml per year. A prognostically unfavorable feature is an annual decrease in OFV1 by 50 ml, which indicates the progressive course of the disease.
Clinic. The main complaint on relatively early stories of chronic obstructive bronchitis is a productive cough, mainly in the morning. With the progression of the disease and the accession of obstructive syndrome, more or less permanent shortness of breath appears, the cough becomes less productive, bred, adsadd.
With auscultation, a wide variety of phenomena is revealed: weakened or rigid breathing, dry whistling and solubular wet wet, if there are pleural battles, the resistant pleural "crackle" is listened. In patients with severe illness, clinical symptoms of emphysema are usually present; Dry wheezing, especially on the forced exhalation; In the later stages of the disease, weight loss is possible; cyanosis (in its absence it is possible for a small hypoxemia); There are peripheral edema; The swelling of the cervical veins, an increase in the right heads of the heart.
In auscultation, the splitting of the I tone on the pulmonary artery is determined. The appearance of noise in the projection zone of the tricuspid valve indicates pulmonary hypertension, although auscultative symptoms can be masked expressed emphysens.
Signs of exacerbation of the disease: the appearance of purulent sputum; increase the number of sputum; strengthening shortness of breath; Strengthening wheezing in the lungs; The appearance of gravity in the chest; Liquid delay.
Treaty reactions are expressed weakly. Erythrocytosis may develop and the associated decrease in ESP.
In the wet detected pathogens of the exacerbation of Khob.
At the radiographs of the chest can be revealed and deformation of the broncho-vascular pattern and signs of lung emphysema. The external respiratory function is violated by obstructive type or mixed with the predominance of obstructive.
Diagnostics.The diagnosis of COPD should be assumed by each person who has cough, excess sputum and / or shortness of breath. It is necessary to take into account each patient the risk factors for the development of the disease.
If there are any of these symptoms, it is necessary to study the function of external respiration.
These features are not diagnostically significant separately, but the presence of several of them increases the likelihood of the disease.
Chronic cough and excess sputum products are often long preceded by ventilation disorders leading to the development of shortness of breath.
It is necessary to talk about chronic obstructive bronchitis in the exclusion of other reasons for the development of broncho-construction syndrome.
Diagnosis criteria - risk factors + productive cough + bronchial obstruction.
The establishment of a formal diagnosis of hob entails the next step - clarifying the degree of obstruction, its reversibility, as well as the severity of respiratory failure.
The hob should be suspected of chronic productive cough or stress shortness, the origin of which is unclear, as well as the LRI detection of signs of slowing the forced exhalation.
The basis for the final diagnosis is:
- detection of functional signs of the obstruction of the respiratory tract, which remains despite intensive treatment using all possible funds;
- Exclusion of specific pathology (for example, silicose, tuberculosis or tumor of the upper respiratory tract) as the causes of these functional disorders.
So, key symptoms for the diagnosis of COPD.
Chronic cough worries the patient constantly or periodically; More often there is a wage of the day, less often at night.
Cough is one of the leading symptoms of the disease, its disappearance of LRI COPD may indicate a decrease in the cough reflex, which should be considered as an unfavorable sign.
Chronic sputum products: At the beginning of the disease, the amount of sputum is small. The sputum has a mucous nature and stands out mainly in the morning clock.
However, with the exacerbation of the disease, its number may increase, it becomes more viscous, the color of sputum changes. Dyspnea: progressive (enhanced with time), persistent (daily). Strengthens when loading and during respiratory infectious diseases.
Action of risk factors in history; smoking and tobacco smoke; industrial dust and chemicals; Smoke home heating devices and fell from cooking.
In a clinical examination, the elongated phase of exhalation in the respiratory cycle is determined, over the lungs - with percussion, pulmonary sound with a boxed tint, with auscultation of the lungs - weakened vesicular breathing, scattered dry wheels. The diagnosis confirms the study of the function of external respiration.
Definition of the forced lung life capacity (freak), the volume of forced exhalation in the first second (FEV1) and the calculation of the FEV / FELE index. Spirometry shows a characteristic decrease in the expiratory respiratory flow with a slowdown of the forced exhalation (decrease in the FEV1). The slowdown of the forced exhalation is also clearly traced by the flow curve - the volume. The jerks and the fritter are slightly reduced in patients with severe hob, but closer to normal than the parameters of the exhalation.
OFV1 is much lower than the norm; The ratio of the FEV1 / ZAN with a clinically pronounced COPD is usually below 70%.
The diagnosis can be considered confirmed only while maintaining these violations, despite the long, maximum intensive treatment. An increase in FEV1 by more than 12% after the inhalation of the bronchoditics indicates a significant reversibility of the respiratory tract. It is often noted in patients with hob, but not pathogeneous for the latter. The absence of such reversibility, if it is judged according to one-time testing data, does not always indicate a fixed obstruction.
Often, the reversibility of obstruction is detected only after a long, maximum intensive drug treatment. Establishing a reversible component of bronchial obstruction and its more detailed characteristic is carried out when carrying out inhalation samples with bronchodylators (cholinolics and B2-agonists).
The sample with berodal allows you to objectively evaluate both adrenergic and the cholinergic components of reversibility of bronchial obstruction. In most patients, an increase in the FFV1 after the inhalation of anticholinergic drugs or sympathomimetics occurs.
Bronchial obstruction is considered reversible with an increase in FEV1 by 12% or more after the inhalation of pharmaceuticals.
It is recommended to carry out a pharmacological sample before the appointment of bright therapy. At home to monitor the function of the lungs, the definition of the peak feed rate (PSV) is recommended using picofloumetres.
The steady progression of the disease is the most important sign of COPD. The severity of clinical signs in patients with COPD is constantly increasing. To determine the progression of the disease, the repeated definition of the FEV1 is used. Reducing FEV1 by more than 50 ml per year indicate the progression of the disease.
When the hob arises and violations in the distribution of ventilation and perfusion occur in the distribution of ventilation and perfusion. Excessive ventilation of the physiological dead space indicates the presence of in light areas, where it is very high in comparison with the bloodstream, i.e. it goes "in good". Physiological shunting, on the contrary, indicates the presence of poorly ventilated, but well perfused alveoli.
In this case, part of the blood coming from the arteries of a small circle into the left heart is not completely oxygenated, which leads to hypoxemia.
In the later stages, general alveolar hypoventilation arises with hypercapnia, exacerbating hypoxemia caused by physiological shunting.
Chronic hypercupnia is usually well compensated and blood pH is close to normal, with the exception of periods of sharp aggravation of the disease. Radiography of chest organs.
The patient's examination should be started with the production of images in two mutually perpendicular projections, better on the film with dimensions of 35x43 cm with an x-ray amplifier.
Polyprosection radiography allows you to judge the localization and length of the inflammatory process in the lungs, the state of the lungs in general, the roots of the lungs, pleura, mediastinum and the diaphragm. The snapshot only in direct projection is allowed for patients in very serious condition. CT scan.
Structural changes in the pulmonary tissue are significantly ahead of the irreversible obstruction of the respiratory tract, detected in the study of the function of external respiration and is less than 80% of due vality as measured by the average indicators.
In the zero stage of COPD using CT, coarse changes are detected in the pulmonary fabric. This raises the question of the beginning of the treatment of the disease at the highest possible stages. In addition, CT makes it possible to eliminate the presence of tumor diseases of the lungs, the likelihood of which in chronically smokers are significantly higher than in healthy. CT allows you to identify widespread congenital malformations in adults: a cystic light, lung hypoplasia, congenital share emphysee, bronchogenic cysts, bronchiectasia, and structural changes in pulmonary tissue associated with other permanent lung diseases that can significantly affect the COPD.
When COP CT allows you to investigate the anatomical characteristics of affected bronchi, establish the length of these lesions in the proximal or distal part of the bronchi; With the help of these methods, bronchoestases are better diagnosed, their localization is clearly established.
With the help of electrocardiography, the state of myocardium is evaluated and the presence of signs of hypertrophy and overload of the right ventricle and atrium.
With laboratory studies, the counting of red blood cells can identify erythrocytosis in patients with chronic hypoxemia.
When determining the leukocyte formula, it is sometimes detected by eosinophilia, which, as a rule, indicates a hob of the type of asthmatic.
Survey study is useful for determining the cell composition of the bronchial secret, although the value of this method is relative. Bacteriological examination of sputum is necessary to identify the pathogen in the signs of the purulent process in the bronchial tree, as well as its sensitivity to antibiotics. Evaluation of symptoms.
The rate of progression and severity of symptoms of COPD depends on the intensity of the impact of etiological factors and their cumulative action. In typical cases, the disease makes itself felt over the age of 40 years. Cough is the earliest symptom that appears to 40-50 years of life. By the same time, episodes of respiratory infection are beginning to occur in the cold seasons, which are not binding to one disease at first.
Subsequently, the cough takes everyday character, rarely intensifying at night. Cough is usually low-product; It can wear an attacking nature and provoked by inhalation of tobacco smoke, a change of weather, inhalation of dry cold air and a number of other environmental factors.
The sputum is highlighted in a small amount, more often in the morning, and has a mucosa. The exacerbations of infectious nature are manifested by the aggravation of all signs of the disease, the appearance of purulent sputum and an increase in its number, and sometimes the delay of its allocation. The sputum has a viscous consistency, which often discovered the "lumps" of the secret.
When aggravating the disease of the sputum becomes greenish color, an unpleasant smell may appear.
The diagnostic significance of an objective survey at COPL is insignificant. Fisical changes depend on the degree of obstruction of the respiratory tract, the severity of the lung emphysema.
Classic signs of hob - whistling wheels with a single breath or with a forced exhalation, indicating the narrowing of the respiratory tract. However, these signs do not reflect the severity of the disease, and their absence does not exclude the presence of a hob in a patient.
Other signs, such as the weakening of breathing, restriction of the chest excursion, the participation of additional muscles in the act of breathing, central cyanosis, also do not show the degree of obstruction of the respiratory tract.
Bronchildren infection - although frequent, but not the only reason for exacerbation.
Along with this, the development of exacerbation of the disease is possible due to an increased action of exogenous damaging factors or with inadequate physical activity. In these cases, the signs of the respiratory system are less pronounced.
As the disease progresses, the gaps between exacerbations become shorter.
Dyspnea as the disease progressing can vary from the sensation of a shortage of air at the usual physical exertion to pronounced manifestations alone.
Dyspnea, felt during exercise, occurs on average 10 years later the appearance of cough.
It is a reason to appeal to the doctor most of the patients and the main cause of disability and anxiety associated with the disease.
As the lung function decreases, the shortness of breath is becoming increasingly pronounced. With emphysema, it is possible to debut disease.
This is happening in those situations where a person contacts production with fine (less than 5 microns) pollutants, as well as in the hereditary deficiency of A1-antitripsein, leading to the early development of the panlobular emphysema.
To quantify the severity of shortness of breath, the MEDICAL RESERCH COUNCIL DYSPNEA SCALE (MRC) is used.
In the wording of the diagnosis of COPD, the severity of the disease flows is indicated: the lightest flow (I stage), the medium-free flow (stage II), the difficult course (III stage) and the extremely difficult course (IV stage), exacerbation or remission of the disease, the exacerbation of purulent bronchitis (if any) ; The presence of complications (pulmonary heart, respiratory failure, blood circulation failure), indicate risk factors, smoking person index.
COPL treatment With a stable condition.
1. Broncholitic drugs occupy a leading place in the complex COPL therapy. To reduce bronchial obstruction in patients, COPDs are used anticholinergic preparations of short and long-term action, B2-agonists of short and long-term action, methylxantins and combinations thereof.
Broncholitics are assigned "on demand" or on a regular basis to prevent or reduce the severity of symptoms of COPD.
To prevent the pace of progression of bronchial obstruction, priority is long and regular treatment. M-cholinolithic preparations are considered to be the preparations of the first row in the treatment of COPD and their appointment is necessary for all degrees of the severity of the disease.
Regular treatment of long-acting bromide (Tiotropia Bromide - Spiriva, Salmetterol, Formoterol) is recommended with a moderate, severe and extremely heavy COPD.
Inhalation M-cholinolics, B2-agonists of long-term action as monotherapy or in combination with prolonged theophyllines are prescribed patients with a medium-heavy, heavy or extremely heavy COPD. Xanthines are effective when COPD, but taking into account their potential toxicity are the preparations of the "second line". They can be added to regular inhalation bronchhalytic therapy with a more severe course of the disease.
Anticholinergic drugs (AHP). The inhalation purpose of anticholinergic preparations (M-cholinolithics) is advisable for all degrees of the severity of the disease. Parasympatic tone is a leading reversible component of bronchial obstruction when COPD. Therefore, AHP is the means of the first choice in the treatment of COPD. Anticholinergic preparations of short action.
The most famous of the AHP short action is the bromide-based bromide, produced in the form of a dosage aerosol inhaler. The bromide is inhibited by the bromide nerve reflexes, being an antagonist of acetylcholine, the mediator of the parasympathetic nervous system. It is dosed by 40 μg (2 doses) four times a day.
The sensitivity of M-cholinoreceptors of the bronchi does not weaken with age. This is especially important, as it allows to use cholinolics in elderly patients with COPD. B.
lagodar Low absorption through the mucous membrane of the bronchi ipratropy Bromide practically does not cause systemic side effects, which allows it to be widely used in patients with cardiovascular diseases.
AHP do not have a negative impact on the secretion of bronchial mucus and the processes of mucocyllular transport.
M-cholinolics of short action have a longer broncholy effect compared to B2 agonists of short action.
In many studies, it has been shown that the long-term use of bromide is more efficient to treat COPDs than long-term short-acting B2-agonist monotherapy.
The Bromide Ipratropy with long-term use improves sleep quality in patients with COPD.
Experts of the American Thoracic Society offer to apply the bromide and bromide "... so long, as long as the symptoms of the disease will continue to cause inconvenience to the patient."
IPratropy Bromide improves the quality of life of patients with COPD when applied 4 times a day and reduces the number of diseases of the disease compared with the use of B2 ~ short-acting agonists.
The use of an inhalation antiholinergic drug is a bromide 4 times a day improves the overall state.
The use of IB as monotherapy or in combination with B2-agonists of short action reduces the frequency of exacerbations, thereby reducing the cost of treatment.
Anticholinergic preparations of long-term action.
The representative of the new generation of AHP is Tiotropia Bromide (Spiriva) in the form of capsules with a powder for inhalations with a special dosed powder inhaler Handi Haler. In one inhalation dose of 0.018 mg of the drug, the peak of action - after 30-45 minutes, the duration of action - 24 hours.
The only drawback is relatively high cost.
A significant duration of the type of tyotropy of bromide, which gives it possible to apply it 1 time per day, is ensured by slow dissociation with M-cholinoreceptors of smooth muscle cells. Long-term brightness (24 h), recorded after one-time inhalation of the tyotropy of bromide, is maintained and during its long-term reception for 12 months, which is accompanied by an improvement in the indicators of bronchial pavement, regery of respiratory symptoms, improving the quality of life. With prolonged treatment of patients with COPD, the therapeutic superiority of the tyotropy of bromide over the bromide and Salmetherol is proved.
2. B2 agonists
b2-agonists short action.
With a slight course of COPD, the use of inhalation bright-acting inhalation "on demand" is recommended. The effect of short-acting B2-agonists (salbutamol, phenoterol) begins for a few minutes, reaching a peak in 15-30 minutes, and continues for 4-6 hours.
Patients in most cases noted the relief of respiration immediately after the use of B2 agonist, which is the undoubted advantage of drugs.
The bronchyolitic effect of B2 agonists is ensured by stimulating the B2 receptors of smooth muscle cells.
In addition, due to an increase in the concentration of AMP under the influence of B2-agonists, not only the relaxation of the smooth muscles of the bronchi, but also the increase in the bio of the epithelial cilia and the improvement of the function of mukiciliary transport. The bright effect is higher than the distal predominant violation of bronchial patency.
After applying the B2 agonists of short action, patients per few minutes feel a significant improvement in the state, the positive effect of which is often revalued by them.
The regular use of short-acting B2 agonists is not recommended as a monotherapy when COPD.
Preparations of this group can cause systemic reactions in the form of transient tremors, excitation, increase blood pressure, which may have a clinical value in patients with concomitant IBS and AG.
However, with the inhalation administration of B2 agonists in therapeutic doses, these phenomena are rare.
long-term B2-agonists (Salmetterol and Formoterol), regardless of changes in the indicators of bronchial patency, can improve clinical symptoms and quality of life of hob patients, reduce the number of exacerbations.
b2-agonists of longer action reduce the bronchial obstruction due to the 12-hour elimination of the global muscles of the bronchi. In vitro shows the ability of Salmetherol to protect the epithelium of the respiratory tract from the damaging action of the bacteria (Haemophilus influenzae).
The prolonged B2-agonist Salmetterol improves the condition of the COPD patients when used in a dose of 50 μg twice a day.
Formoterol favorably affects the indicators of the function of external respiration, symptoms and quality of life in patients with COPD.
In addition, Salmetterol improves the reduction of respiratory muscles, reducing the weakness and dysfunction of respiratory muscles.
Unlike Salmetherol, Formoterol has a rapid start of action (after 5-7 minutes).
The duration of the prolonged B2 agonists reaches 12 hours without loss of efficiency, which allows us to recommend the latter for regular use in COPL therapy.
3. Combinations bronchussessing medicines.
The combination of inhalation B2-agonist (fast-acting or PEPPETING) and AHP is accompanied by an improvement in bronchial passability to a greater extent than when appointing any of these drugs as monotherapy.
With a moderate and serious current COPD, selective B2 agonists are recommended to be prescribed along with M-cholinolithics. Fixed combinations of drugs in one inhaler are very convenient and less expensive (Berodal \u003d IB 20 μg + phenoterol 50 μg).
The combination of bronchodulators with a different mechanism of action increases efficiency and reduce the risk of side effects in comparison with an increase in the dose of one drug.
With long-term reception (within 90 days or more) IB in combination with B2-agonists, tachofilaxia does not develop.
In recent years, the positive experience of the combination of cholinolithics with B2 agonists of prolonged action has become accumulated (for example, with Salmeterol).
It has been proven that to prevent the rate of progression of bronchial obstruction, priority is long and regular treatment with bronchologists, in particular AHP and prolonged B2-agonists.
4. Theophimines for a long action
Methylxantins are non-selective phosphodiesterase inhibitors.
The imaging effect of theophylline is inferior to such B2 agonists and AHP, but receiving inside (prolonged forms) or parenterally (inhaled methylxantins are not prescribed) causes a number of additional effects that may be useful in a number of patients: a reduction in systemic pulmonary hypertension, strengthening the diurea, stimulation of the central nervous Systems, strengthening the operation of respiratory muscles. Xanthans can be added to regular inhalation bronchhalytic therapy with a more severe course of the disease in case of insufficient efficacy of AHP and B2 agonists.
In the treatment of COPD, theophylline can have a positive effect, but in connection with its potential toxicity, inhalation bronchodylators are more preferred.
All studies that showed the effectiveness of theophylline during COPD relate to the preparations of prolonged action. The use of prolonged forms of theophylline can be shown at night manifestations of the disease.
Currently, theophyllins belong to the preparations of the second stage, i.e., prescribed after AHP and B2 agonists or their combinations.
It is also possible to the appointment of theophyllins and the patients "that cannot use inhalation means of delivery.
According to the results of the latest controlled clinical studies, combination therapy with the use of theophylline does not provide additional advantages in the treatment of COPD.
In addition, the use of theophylline at COPD is limited by the risk of unwanted adverse reactions.

Tactics of destination and the effectiveness of bronchology therapy.
Broncholitic agents in patients COPDs can be assigned both in need (to reduce the severity of symptoms in a stable state and in exacerbation) and regularly (with a prophylactic goal and to reduce the severity of symptoms).
The dependence of the dose-reaction, evaluated by the dynamics of the FEV, is insignificant for all classes of broutine.
The side effects of pharmacologically predictable and dose-dependent. Adverse effects are rare and permit more quickly with inhalation than when oral therapy.
Inhalation of inhalation therapy, special attention should be directed to the effective use of inhalers and patient training technique inhalation.
When using B2 agonists, tachycardia, arrhythmia, tremor and hypokalemia can develop.
Tachycardia, heart rate disorders and dyspepsia can also appear when taking theophylline, in which doses that provide bronchodiolitical effects are close to toxic.
The risk of undesirable reactions requires the attention of the doctor and control the heart rate, the level of potassium in serum and ECG analysis, however, the standard procedures for assessing the safety of these drugs in clinical practice does not exist.

In general, the use of bronchoditics makes it possible to reduce the severity of shortness of breath and other symptoms of COPD, as well as increase the tolerance to physical activity, reduces the frequency of exacerbations of the disease and hospitalization. On the other hand, the regular reception of the bronchoditics does not prevent the progression of the disease and does not affect its forecast.
With a slight course of COPD (Stage I) during the remission, therapy is shown by the brief action on demand.
In patients with a medium-heavy, heavy and extremely severe course of COPD (STACI II, III, IV), the bronchological therapy is shown by one drug or combination of broutine.
In some cases, patients with severe and extremely severe COPD (stage III, IV) require regular treatment with high doses of bronchodulators with nebulizer administration, especially if they noted a subjective improvement from such treatment previously used in the exacerbation of the disease.
To clarify the need for inhalation nebulizer therapy, picofloumometry monitoring is required for 2 weeks and continued nebulizer therapy in the presence of significant improvement in indicators.
Bronchutors are one of the most effective symptomatic means for COPL therapy.

Ways to deliver bronchhalytic drugs
There are various ways of delivering bronchodilics under COPL therapy: inhalation (bromide, tiotropia bromide, salbutromol, phenooterol, formoterol, salmeterol), intravenous (theophylline, salbutamol) and subcutaneous (adrenaline) injections, taking drugs inside (theophylline, salbutamol).
Given that all the bronchophists are capable of providing clinically significant adverse reactions during their systemic purpose, the inhalation method of delivery is more preferable.
Currently, the domestic market has preparations in the form of a dosage aerosol, powder inhalers, a nebulizer solutions.
When choosing a method for delivering inhalation bronchodens, first of all, from the ability of the patient to properly use a dosage aerosol or another pocket inhaler.
For elderly patients or patients with mental violations, it is advantageously recommended to use a dosage aerosol with Spencer or Nebulizer.
The defining factors in the choice of means of delivery are also their availability and cost. M-cholinolics of short-acting and B2-agonists of short-acting are mainly used in the form of dosage aerosol inhalers.
To increase the efficiency of the drug delivery to the respiratory tract, spacers are used to increase the flow of the drug in the air-and-axis paths. With the III and IV stages of COPD, especially with respiratory muscles dysfunction syndrome, the best effect is achieved when using nebulizers. Allowing to increase the delivery of the drug into the respiratory tract.
When comparing the main means of delivering the bronchoditics (dosage aerosol inhaler with a spacer or without it; a nebulizer with a mouthpiece or face mask; a dosage inhaler of dry powder) is confirmed by their identity.
However, the use of nebulizers is preferable to heavy patients who, due to pronounced shortness of breath, cannot accomplish an adequate inhalation maneuver, which naturally makes it difficult for the use of metered aerosol inhalers and spatial nozzles.
Upon the achievement of clinical stabilization, patients are "returned" to the usual means of delivery (dosage aerosols or powder inhalers).

Glucocorticosteroids with stable current COPD
The healing effect of GKS at COPD is much less pronounced than at Ba, therefore their use in COPD is limited to certain indications. Inhalation corticosteroids (ICX) are appointed additionally to bronchhalytic therapy - in patients with OFVG<50% от должной (стадия III: тяжелая ХОБЛ и стадия IV: крайне тяжелая ХОБЛ) и повторяющимися обострениями (3 раза и более за последние три года).
Regular treatment of ICCC is shown in patients with severe and extremely severe course of the disease in annual or more frequent exacerbations over the past three years.
To establish the feasibility of systematic ICCC application, it is recommended to carry out a trial therapy with system GCS at a dose of 0.4-0.6 mg / kg / day inside (by prednisone) for 2 weeks.
Long reception of system GCS (more than 2 weeks) with a stable current COPD is not recommended due to the high risk of unwanted phenomena.
The effect of steroids should complement the effects of constant bronchological therapy.
The ICCC monotherapy for COPD patients is unacceptable.

Corticosteroids are preferable to assign in the form of dosage aerosols.
Unfortunately, even the inhalation long-term use of GKS does not reduce the rate of annual decline in FEV in patients with COPD.
The combination of ICCC and B2-agonists of a long-term action is more efficient to the root of COPD than the use of individual components.
Such a combination demonstrates synergism of action and allows you to affect the pathophysiological components of the COPD: bronchial obstruction, inflammation and structural changes in respiratory tract, mucocylliory dysfunction.
The combination of B2-agonists of long-term action and ICCC causes more winning ratios "risk / benefit" compared to individual components.
The combination of Salmetterol / Fluticazone Propionate (Soldid) is potentially able to increase the survival rate of COPD patients.
Each dose of the sewage (two inhalations for the dosage inhaler) contains 50 μg of xinafoate salmeterol in combination of 100 μg of the propionate fluctaisone, or with 250 μg or 500 μg of the propionate fluctuation.
It is advisable to use a fixed combination of formoterol and budesonide (symbiotic) in patients with COPD of medium-heavy and severe flow compared with the separate use of each of these drugs.

Other medicines
Vaccines. In order to prevent the exacerbation of the COPD during epidemic outbreaks of influenza, the vaccine is recommended for the use of vaccines containing killed or inactivated viruses appointed once in October-first half of November annually. The flu vaccine is 50% capable of reduce the severity of flow and mortality in patients with COPD.
A pneumococcal vaccine containing 23 virulent serotypes is also used, but data on its effectiveness during COPD is insufficient.
Nevertheless, according to the Committee of Immunization Practice Advisors, patients with COPDs refer to persons with a high risk of a pneumococcal infection and are included in the target group for vaccination. Preferably, polyvalent bacterial vaccines used orally (ribomunyl, bronchomunal, bronchovakov).
Antibacterial drugs. According to the modern point of view, antibiotics for the prevention of exacerbations COPD is not prescribed.
The exception is the exacerbation of the hob with the advent of purulent sputum (the appearance or strengthening of "nepidity"), along with an increase in its number, as well as signs of respiratory failure.
It should be borne in mind that the degree of eradication of etiologically significant microorganisms determines the duration of remission and the deadlines for the onset of the subsequent relapse.
When choosing the optimal antibiotic for this patient, it is necessary to focus on the range of major pathogens, the severity of the exacerbation, the likelihood of regional resistance, the safety of the antibiotic, the convenience of its use, the cost indicators.
The first row preparations in patients with non-heavy exacerbations hob are amoxiclav / clavulanic acid or its unprotected form - amoxicillin. Eradication of causative agents of infections of the respiratory tract allows us to break the vicious circle of the course of the disease.
In most patients, the Kob is effective macrolides despite the resistance of S. pneumoniae and the low natural sensitivity of N. influenzae.
This effect can be partially due to the anti-inflammatory activity of macrolides.
Among macrolides are mainly used azithromycin and clarithromycin.
An alternative to protected penicillins may be respiratory fluoroquinolones (sparfloxacin, moxifloxacin, levofloxacin), which have a wide range of antimicrobial activity against gram-positive and gram-negative microorganisms, penicillin-negative strains S. pneumoniae and N. influenzae.
Respiratory fluoroquinolones are capable of creating a high concentration in bronchial content, have almost complete bioavailability when taking inside. In order to ensure the high compliance of patients, the prescribed antibiotic should be accepted inside 1-2 times a day and for at least 5, it is desirable 7 days, which complies with the modern requirements of antibacterial therapy during the exacerbation of Khob.
Mulitatic means
Mulcolics (mucocinetics, muffinulators) are shown a limited contingent of patients with stable COPD with viscous sputum. The effectiveness of the musolithics in the treatment of COPD is small, although in some patients with a viscous wet, the condition can improve.
Currently, based on existing evidence, the widespread use of these drugs cannot be recommended with a stable course of COPD.
When the hob is most effective, ambroxol (Lazolyvan), acetylcysteine. Invalid is previously practiced the use of LRGOLOLYTIC enzymes as the flourities.
For the prevention of exacerbation of COPDs, a long-term use of N-acetylcysteine \u200b\u200bpulic (NAC) is promising, which has antioxidant activity simultaneously.
Reception NAC (floivucill) for 3-6 months at a dose of 600 mg / day is accompanied by a significant decrease in the frequency and duration of COPD exacerbations.
Other pharmacological products. Purpose of psychotropic drugs An older patient COPD for treating depression, anxiety, insomnia should be carried out with caution due to their oppressive effect on the respiratory center.
With severe COPD with the development of drugs, there is a need for cardiovascular therapy,
In such cases, treatment may include IAPF, BKK, diuretics, it is possible to use digoxin.
The purpose of adrenergic blockers is contraindicated.
Non-media treatment With a stable current COPD.
1. Oxygen therapy.
2. Surgical treatment (see below in the section "Emphysema Treatment").
3. Rehabilitation.
Oxygen therapy. The main cause of the death of patients COPD is the bottom. Correction of hypoxemia with oxygen - the most pathophysiologically substantiated method of day therapy.
The use of oxygen in patients with chronic hypoxhemia should be permanent, long and, as a rule, are carried out at home, therefore such a form of therapy is called long-term oxygen therapy (DCT).
Accounts today is the only method of therapy that can reduce the mortality of patients with COPD.
Another favorable physiological and clinical effects of the DCC are:
reverse development and preventing the progression of pulmonary hypertension;
reduction of shortness of breath and improving tolerance to physical exertion;
reduction of hematocrit;
improving the function and metabolism of respiratory muscles;
improving the neuropsychological status of patients;
Reducing the frequency of hospitalization of patients.
Indications for long-term oxygen therapy. Long-term hydrocerapy is shown to patients with severe COPD.
Before appointing a sickness of the DCT, it is also necessary to make sure that the possibilities of drug therapy are exhausted and the maximum possible therapy does not lead to an increase in O2 above border values. It has been proven that long-term (more than 15 hours per day) oxygen therapy increases the life expectancy of patients from the day.
The purpose of long-term hydroatherapy is the increase in RAO2 at least up to 60 mm Hg. Art. Alone and / or SAO2 at least 90%. It is considered optimal maintenance of RAO, in the range of 60-65 mm Hg. Art.
Permanent oxygen therapy is shown at:
- RAO2.< 55 мм рт. ст. или SaО2 < 88% в покое;
- RAO2 56-59 mm RT. Art. or Sao2 \u003d 89% in the presence of HLS and / or erythrocytosis (HT\u003e 55%).
"Situational" oxygen therapy is shown at:
- Reduced RAO2.< 55 мм рт. ст. или Sa02 < 88% при физической нагрузке; - снижении РаО2 < 55 мм рт. ст. или Sa02 < 88% во время сна.
The DCT is not shown in patients with moderate hypoxemia (RAO2\u003e 60 mm Hg. Art.).
The parameters of the gas exchange, which are based on testimony to the DCT, should be estimated only during the stable state of patients, i.e., 3-4 weeks after the exacerbation of COPD, since it is that time is required to restore gas exchange and oxygen transport after a period of acute respiratory failure ( One).
Rehabilitation. Assigned to all COPD phases. Depending on the severity, the disease phase and the degree of compensation of the respiratory and cardiovascular systems, the attending physician defines an individual rehabilitation program for each patient, which includes regime, exercise, physiotherapy procedures, spa treatment. Therapeutic respiratory gymnastics is recommended for the patient COPD even with a pronounced obstruction.
An individually selected program leads to an improvement in the quality of the patient's life. It is possible to use percutaneous electrostimulation of the diaphragm. To give up smoking.
The cessation of smoking is an extremely important event that improves the disease forecast.
It should take the first place in the treatment of this pathology. The cessation of smoking reduces the degree and speed of the fall of the FEV1
The use of auxiliary artificial ventilation of the lungs can be considered as an increase in PC02 and a decrease in blood pH in the absence of an effect from the therapy listed.
Indications for hospitalization: the ineffectiveness of treatment in outpatient conditions; the increase in the symptoms of obstruction, the impossibility of moving around the room (for a previously mobile person); rapidness of shortness of breath while eating and in a dream; progressive hypoxemia; the emergence and / or increasing of hypercaps; the presence of concomitant pulmonary and extrapultural diseases; The emergence and progression of the symptoms of the "pulmonary heart" and its decompensation; Mental disorders.
Hospital treatment
1. Oxigenotherapy. In the presence of severe exacerbation of the disease and pronounced respiratory failure, constant oxigen therapy is shown.
2. Broncholy therapy is carried out by the same drugs as in the conditions of outpatient treatment. Spraying B2-adrenomimetics and cholinolics are recommended using a nebulizer, carrying out inhalation every 4-6 hours.
In case of insufficient effectiveness, the multiplicity of inhalation can be increased. It is recommended to use combinations of drugs.
For therapy through the nebulizer, it can be made within 24-48 hours.
In the future, bronchoditics are prescribed in the form of a dosage aerosol or dry powder. If the inhalation therapy is insufficient, it is prescribed to / in the introduction of methylxantins (Eutillin, aminoophyllin, etc.) at a rate of 0.5 mg / kg / h.
3. Antibacterial therapy is assigned to the presence of the same testimony that was taken into account on the outpatient stage of treatment. In case of ineffectiveness of primary antibiotic therapy, the selection of the antibiotic is carried out taking into account the sensitivity of the spruce of the patient's sputum to antibacterial drugs.
4. Indications for the appointment and scheme of appointment of magnutocorticoid hormones are the same as on the outpatient stage of treatment. In case of severe disease, the introduction of GCS is recommended.
5. In the presence of edema, diuretic drugs are prescribed.
6. In severe exacerbation of the disease, heparin is recommended.
7. Auxiliary artificial ventilation of the lungs is used in the absence of a positive effect from the above therapy, with an increase in PC02 and the fall in the pH.
Non-drug treatment methods are used primarily in order to facilitate sputum isolated, especially if the patient is treated with expectorant means, heavy alkaline drink.
Positioning drainage - sprinkling sputum with deep forced exhalation in a position optimal for wetting. Calciation is improved when using vibratory massage.
Forecast
In the outcome of COPD - the development of chronic pulmonary heart and pulmonary heart failure.
Prognostably unfavorable factors are an elderly age, severe bronchial obstruction (according to the indicators of the FFV1), the severity of hypoxemia, the presence of hypercaps.
The death of patients usually comes from such complications as acute respiratory failure, pulmonary heart decompensation, heavy pneumonia, pneumothorax, heart rate disorders.
The disease under consideration is an inflammatory disease, which strikes the distal departments of the lower respiratory tract, and which is chronic. Against the background of this pathology, the pulmonary fabric and vessels are modified, and the passability of the bronchi is significantly violated.
The main sign of COPL is the presence of obstructive syndrome, in which the patients may be diagnosed with inflammation of the bronchi, bronchial asthma, secondary emphysema of the lungs, etc.
What is COPL - the causes and mechanism of the occurrence of chronic obstructive pulmonary disease
According to the World Health Organization, the Deals in question heads the 4th place in the list of causes of mortality.
Video: Chronic obstructive pulmonary disease
This pathology is formed under the influence of not one, but a number of factors to which include:
- Tobacco This harmful habit is the most common cause of the development of COPD. Interesting is the fact that the inhabitants of the village are chronic obstructive pulmonary disease flows in heavier forms, rather than the residents of cities. One of the reasons for this phenomenon is the lack of screening of the lungs in smokers after a 40-year-old age in Russian villages.
- Inhalation of harmful microparticles in production. In particular, this concerns cadmium and silicon, which is entered into the air during the processing of metal structures, as well as due to the combustion of fuel. In an increased risk zone, miners, railway workers, construction specialties are often contacted with cement-containing mixtures, agricultural workers, which are recycling cotton and grain crops.
- Adverse ecological situation.
- Frequent respiratory infections in preschool and school periods.
- Related diseases of the respiratory system: Bronchial asthma, tuberculosis, etc.
- The presence of babies. When birth, their lungs do not disclose completely. This is displayed on their functioning and can cause serious exacerbations in the future.
- Congenital lack of proteinWhat is produced in the liver, and is intended to protect the tissue of the lungs from the destructive effect of elastase.
Against the background of genetic aspects, as well as unfavorable natural factors, inflammatory phenomena occur in the inner shell of the bronchi, which acquire chronic.
The specified pathological state leads to the modification of bronchial mucus: it becomes more, its consistency changes. It causes failures in bronchial passability, and provokes development degenerative processes in pulmonary alveoli. The overall picture can be exacerbated by the addition of bacterial exacerbations, which provokes the re-infection of the lungs.
In addition, the disease in question may cause violations in the heart of the heart, which is displayed on the blood supply to the respiratory system. This condition for chronic forms is the cause of death in 30% of patients with a diagnosis of "chronic obstructive pulmonary disease".
Signs and symptoms of chronic obstructive lung disease - how to notice in time?
At the initial stages of development, the pathology considered is often not manifest itself. A typical symptomatic picture is manifested in medium-stage stages.
Video: What is COPL and how to detect it in time?
This pulmonary disease is distinguished by two typical features:
- Cough. It makes itself felt most often after awakening. In the process of cough, a certain amount of sputum is separated, viscous consistency. When involving the pathological process of bacterial agents, the sputum becomes purulent and abundant. Patients often associate a similar phenomenon with smoking or working conditions, in a medical institution for consultation, therefore not often appeal.
- Saddy. At the beginning of the development of the disease, a similar symptom manifests itself with rapid walking or climbing a hill. With the development of the COPD, the man suffocates even when it passes the rig. Such a pathological state causes the patient to move more slowly than healthy people. In some cases, patients complain about shortness of breath during stripping / dressing.
According to its clinical manifestations, this pulmonary pathology is divided into 2 types:
- Bronchitic. The symptomatic picture here is pronounced. This is associated with purulent-inflammatory phenomena in bronchi, which is manifested by a strong cough, abundant mucous discharge from bronchi. The patient increases the body temperature, it constantly complains about fatigue and lack of appetite. Skin covers get a shiny tint at the same time.
- Emphysematosis. It is characterized by a more favorable course - patients with such a type of COPD often live to 50 years of age. A typical symptom of emphysematous type of disease is escaped. The yard acquires a barrel shape, the skin becomes pink-gray.
Chronic obstructive pulmonary disease affects not only the operation of the respiratory system, it suffers almost the entire organism.
The most frequent disorders include:
- Degenerative phenomena in the walls of blood vesselsthat provokes the formation of atherosclerotic plaques - and increases the risk of thrombus.
- Error in the work of the heart. In patients with COPD, a systematic increase in blood pressure is often diagnosed, ischemic heart disease. The likelihood of acute myocardial infarction is not excluded.
- Atrophic processes in musclesWhat is involved in the respiratory function.
- Serious disorders in the functioning of the kidneys.
- Mental disorderswhose character is determined by the COPD development stage. Such violations can be represented by night apnea, poor sleep, difficulties in memorizing events, difficulties in thinking. In addition, patients often feel sadness and anxiety, often fall into depression.
- Reducing the protective reactions of the organism.
Stages COPD - Classification of chronic obstructive lung disease
According to the International Medical Classification, the disease under consideration in its development passes 4 stages.
Video: COPD. Why easy it is not easy?
At the same time, during the division of illness to specific forms, two main indicators take into account:
- The volume of forced exhalation - OFV .
- Forced Little Life Capacity - Fire - After taking drugs that bind symptoms of acute bronchial asthma. Normably, the flanks should not exceed 70%.
Consider the main stages of the development of the specified pulmonary pathology in more detail:
- Zero stage. Standard symptoms at this stage - regular cough with minor range of sputum. Easy to all work without disorders. The specified pathological state does not always develop into the COPD, but there is still a risk.
- First (Easy) Stage. Cough acquires chronic character, the sputum is produced regularly. Diagnostic events can identify small obstructive errors.
- Second (medium-heavy) stage. Obstructive violations are enhanced. The symptomatic picture becomes more pronounced during exercise. There are difficulties with breathing.
- Third (heavy) stage. Air flow when exhaling is limited in volumes. The exacerbations become regular phenomenon.
- Fourth (extremely heavy) stage. There is a serious risk to the life of the patient. Typical complications at this stage of development of COPD - respiratory failure, serious failures in the functioning of the heart, which affect the quality of blood circulation.
Chronic obstructive skin disease (the wording of the diagnosis of COPD) is a pathological process for which the partial restriction of air flow in the respiratory tract is characteristic. The disease causes irreversible changes in the human body, so there is a big threat to life if the treatment was appointed not on time.
The reasons
Pathogenesis COPD is not yet fully studied. But experts allocate the main factors causing the pathological process. As a rule, the pathogenesis of the disease includes the progressive obstruction of the bronchi. The main factors affecting the formation of the disease are:
- Smoking.
- Adverse conditions for professional activities.
- Raw and cold climate.
- Infection of mixed gene.
- Acute tightening bronchitis.
- Light diseases.
- Genetic predisposition.
What are the manifestations of the disease?
Chronic obstructive skin disease is a pathology that is most often diagnosed in patients aged 40 years. The first symptoms of the disease, which begins to notice the patient, cough and shortness of breath. Often this condition passes in combination with whistles with breathing and sputum discharges. Initially, it comes out in a small volume. A more pronounced symptoms are acquired in the morning.
Cough is the very first sign that bothers patients. During the cold season, respiratory diseases are aggravated, which play an important role in the formation of COPD. The obstructive disease of the lungs has the following symptoms:
- A shortness of breath, which is concerned when performing physical exertion, and then may affect a person during peace.
- With the effect of dust, cold air, shortness of breath is intensified.
- The symptoms complements the low-product cough with difficult to be highlighted by the wet.
- Dry wheezes of a high tempo when exhaling.
- Symptoms of emphysema lungs.
Stages
COOL CLASSIFICATION is based on the severity of the alend's current. In addition, it assumes the presence of a clinical picture and functional indicators.
Classification of COPD assumes 4 stages:
- The first stage - the patient does not notice any pathological deviations. It can be attended by cough chronic orientation. Organic changes are undefined, so it is not possible to make a diagnosis of COPD at this stage.
- The second stage - the disease proceeds not hard. Patients appeal to a doctor for advice on shortness of breath during exercise. Another chronic obstructive disease of the lungs is accompanied by an intense cough.
- The third stage of COPD is accompanied by a difficult flow. It is characterized by the presence of a limited air intake in the respiratory tract, so shortness of breath is formed not only during physical exertion, but also at rest.
- The fourth stage is an extremely difficult course. Cat symptoms arising from a dangerous nature for life. There is a blockage of bronchi and a lung heart is formed. Patients who diagnosed the 4th stage of COPD are disability.
Diagnostic methods
The diagnosis of the present disease includes the following methods:
- Spirometry is a research method, thanks to which it is possible to determine the first manifestations of COPD.
- Measuring the life capacity of lungs.
- Cytological examination of sputum. Such diagnostics makes it possible to determine the nature and severity of the inflammatory process in bronchi.
- The blood test allows you to detect the enlarged concentration of erythrocytes, hemoglobin and hematocrit.
- Radiography of lungs allows you to determine the presence of sealing and changing the bronchial walls.
- ECG allows you to obtain data on the development of light hypertension.
- Bronchoscopy is a method that allows you to determine the diagnosis of COPD, as well as briefcase and determine their condition.
Treatment

Chronic obstructive disease of the lungs is a pathological process, to cure that is impossible. However, the doctor appoints a certain therapy with its patient, thanks to which it is possible to reduce the frequency of exacerbations and extend the life of a person. The course of the prescribed therapy has a great influence of the pathogenesis of the disease, because it is very important to eliminate the reason for the occurrence of pathology. In this case, the following events are appointed by the doctor:
- COPD treatment implies the use of medicines whose action is aimed at an increase in the lumen of the bronchi.
- For the wet wet and its elimination, the treatment of therapy involves musolithic agents.
- Help to stop the inflammatory process with glucocorticoids. But their long-term use is not recommended, as serious side effects begin to arise.
- If there is an aggravation, this indicates the presence of its infectious origin. In this case, the doctor prescribes antibiotics and antibacterial drugs. Their dosage is appointed taking into account the sensitivity of the microorganism.
- For those who suffer on heart failure requires oxygen therapy. With exacerbation, the patient is prescribed sanitary-resort treatment.
- If the diagnosis confirmed the presence of light hypertension and COPD, accompanied by reporting, then the treatment includes diuretics. Eliminate the manifestations of arrhythmias help glycosides.
COPD - a disease whose treatment cannot do without a proposed diet. The reason is that the loss of muscle mass can lead to death.

The patient can put on stationary treatment if he is:
- a large intensity of the increase in the severity of manifestations;
- treatment does not give the desired result;
- new symptoms arises;
- violated heart rhythm;
- diagnostics determines the disease such as diabetes mellitus, pneumonia, insufficient kidney and liver;
- it is not possible to provide medical care in outpatient conditions;
- diagnosis difficulties.
Preventive actions
COPD prevention includes a set of events, thanks to which everyone can warn his body from this pathological process. It is to fulfill the following recommendations:
- Pneumonia and influenza are the most frequent causes of the formation of COPD. Therefore, it is necessary to put influenza vaccinations every year.
- Once in 5 years spend vaccinations from pneumococcal infection, thanks to which it is possible to protect its body from the damage to pneumonia. Appoint vaccination can only attending the doctor after the appropriate inspection.
- Taboo on smoking.
COOL complications can be the most diverse, but, as a rule, they all lead to disabled. Therefore, it is important to carry out treatment in time and all the time is under the control of the specialist. And best of all, it is best to carry out preventive measures to prevent the formation of a pathological process in lungs and warn itself from this ailment.
Is everything correctly in the article from a medical point of view?
Answer only if you have confirmed medical knowledge
Diseases with similar symptoms:
Asthma is a chronic disease, which is characterized by short-term attacks of choking, due to spasms in bronchops and the edema of the mucous membrane. A certain group of risk and age limitations does not have this disease. But, as medical practice shows, women are sick of asthma 2 times more often. According to official data, more than 300 million people in the world live in the world today. The first symptoms of the disease appear most often in childhood. Elderly people endure the disease much more difficult.