Axistid aid to a private medical clinic. Emergency and emergency medical care. Algorithm of actions for emergency conditions The main urgent states and 1 assistance
Slowly, European medical standards are beginning to be introduced in Russia.
From the new 2014 comes into force new order providing emergency medical care, which is developed in accordance with the Law "On the Fundamentals of the Protection of Citizens in Russian Federation».
The main innovations will be:
- The regulator on the arrival of the ambulance carriage is set to the location of the call in the layer of up to 20 minutes. He used to be in such a temporary range, but its implementation was a difficult task due to the lack of the necessary infrastructure. To fulfill such a standard, innovation No. 2 is introduced.
- Formation of posts that will be paved on the territory of service depending on the transport accessibility. The appearance of such posts and auto traces is expected.
- Introduction of such posts is assumed in existing hospitals with more than 500 beds with the opening of diagnostic and resuscitation departments in them
- For emergency medical help, it will be possible to contact the hospital directly. Now such departments are already working in pilot mode in St. Petersburg, Naberezhnye Chelny and Kazan
- As accepted in European countries, phone number emergency It will begin with the digit "1" and the challenge will be at the number - 103
- Ambulance cars will be additionally equipped:
- modules of GLONASS and GPS systems to monitor the movement of the brigades
- dVR, for fixing cars that impede and not inferior to the passage of ambulances
- "Alarm button" to supply alarm signal in the case of an attack on a brigade
- Spinal shield with head lock for transportation patients with spinal fractures and ribs
- Defibrillators, artificial ventilation devices (IVL), portable pulse oximeters.
(From the words of the Director of the Department of Medical Prevention, ambulance, primary health care and the sanatorium-resort business of the Ministry of Health of the Russian Federation, Alexey Andreev, the equipment of reanimal class "C" by 95% corresponds to American and European sets.)
- Outdated drugs are eliminated from the list of vital drugs and new, incl. Preparations for stopping massive bleeding. Narcotic analgesics will also be present in the first aid kit the ambulance team.
- Introduction of a new post - driver-driver.
What is the difference between emergency and emergency assistance?
Emergency ambulance It turns out for the states of threatening life - a violation of consciousness, respiratory disorders, bleeding, sudden pain syndrome, threat of interrupting pregnancy, etc.
Under states requiring medical intervention but not pose a threat to life - it turns out urgent Care .
The decision on the targeted provision of a particular assistance takes the dispatcher or paramedic. If there are no emergency calls at the time of the challenge to provide emergency care, then the first released "ambulance" team is sent to the urgent call. In other cases, the call is redoneed into the clinic and the doctor will be sent to the patient. π.
Clinical manifestations
First health care
With a neareetative form of chisosis, the sequence of actions:
1) to introduce 4-6 ml of 1% furosemide solution intravenously;
2) introduce 6-8 ml of 0.5% solution of dibazole dissolved in 10-20 ml of 5% glucose solution or 0.9% sodium chloride solution, intravenously;
3) introduce 1 ml of 0.01% clofelin solution in the same dilution intravenously;
4) introduce 1-2 ml of 0.25% droperidol solution in the same dilution intravenously.
With water-salt (empty) form of chisosis:
1) enter 2-6 ml of 1% furosemide solution intravenously once;
2) to introduce 10-20 ml of a 25% magnesium solution of sulfate intravenously.
With convulsive form of chisosis:
1) introduce intravenously 2-6 ml of 0.5% diazepam solution divorced in 10 ml of 5% glucose solution or 0.9% sodium chloride solution;
2) hypotensive drugs and diuretics - according to the testimony.
With a crisis associated with a sudden cancellation (termination of admission) of hypotensive drugs: to introduce 1 ml of 0.01% clofelin solution, divorced in 10-20 ml of a 5% glucose solution or a 0.9% sodium solution of chloride.
Notes
1. To enter drugs should be sequentially, under the control of blood pressure;
2. In the absence of a hypotensive effect for 20-30 minutes, the presence of an acute violation of cerebral circulation, cardiac asthma, angina is required hospitalization into a multidisciplinary hospital.
Angina
Clinical manifestationss - m. Nursing in therapy.
First aid
1) stop physical load;
2) to put a patient with a support on the back and with lowered legs;
3) under the tongue to give it a nitroglycerin or validol tablet. If the heartache does not stop, repeat the reception of nitroglycerin every 5 minutes (2-3 times). If the improvement has not come, call a doctor. Before it arrives to go to the next stage;
4) in the absence of nitroglycerin, it is possible to give under the patient with 1 tablet of nifedipine (10 mg) or Molidomin (2 mg);
5) give a drink aspirin tablet (325 or 500 mg);
6) Suggest a patient to drink with small sips hot water or put a mustarder on the heart;
7) In the absence of the effect of therapy, the hospitalization of the patient is shown.
Myocardial infarction
Clinical manifestations - See the nursing case in therapy.
First aid
1) to put or sit down the patient, unbutton the belt and collar, provide fresh air access, full physical and emotional peace;
2) with systolic blood pressure at least 100 mm Hg. Art. and heart rate greater than 50 in 1 min give a nitroglycerin tablet under the interval of 5 minutes. (but not more than 3 times);
3) give a drink of aspirin tablet (325 or 500 mg);
4) to give a tablet of propranolol 10-40 mg under the tongue;
5) introduce intramuscularly: 1 ml of 2% propellane solution + 2 ml of 50% analgin solution + 1 ml of 2% diploma solution + 0.5 ml of 1% sulfate atropine solution;
6) with systolic blood pressure less than 100 mm Hg. Art. It is necessary to intravenously to introduce 60 mg of prednisolone in dilution with 10 ml of saline;
7) introduce heparin 20,000 units intravenously, and then - 5000 units subcutaneously into the zone around the navel;
8) Transport the patient to the hospital follows the position lying on the stretcher.
Pulmonary edema
Clinical manifestations
It is necessary to differentiate swelling of the lungs from cardiac asthma.
1. Clinical manifestations of cardiac asthma:
1) frequent surface breathing;
2) exhalation is not difficult;
3) the position of orthopne
4) with auscultation dry or whistling wheels.
2. Clinical manifestations of alveolar edema of the lungs:
1) choking, bubbling;
2) orthopne
3) pallor, skin sinusiness, humidity of skin;
4) tachycardia;
5) Isolation of a large number of foamy, sometimes colored sputums.
First aid
1) give a sick position to the patient, impose harnesses or cuffs from a tonometer on lower limbs. Reassure the patient to ensure fresh air;
2) introduce 1 ml of the 1% mortar solution of hydrochloride dissolved in 1 ml of physiological solution or in 5 ml of 10% glucose solution;
3) give nitroglycerin at 0.5 mg under the tongue every 15-20 minutes. (up to 3 times);
4) under the control of blood pressure to introduce 40-80 mg of furosemide intravenously;
5) with high blood pressure introduce intravenous 1-2 ml of a 5% pentamine solution dissolved in 20 ml of physiological solution, 3-5 ml with an interval of 5 minutes; 1 ml of 0.01% clofelin solution dissolved in 20 ml of saline;
6) to establish oxygen therapy - inhalation of hydrated oxygen with a mask or nasal catheter;
7) make the inhalation of oxygen, moistened with 33% ethyl alcohol, or introduce 2 ml of 33% solution ethyl alcohol intravenously;
8) to introduce 60-90 mg of prednisolone intravenously;
9) in the absence of the effect of therapy, the growth of pulmonary edema, the adhesive adhesion is shown artificial ventilation of the lungs;
10) hospitalize the patient.
Fainting may occur with a long stay in the stuffy room due to lack of oxygen, if there is a tight, shying the breath of clothing (corset) healthy man. Repeating fainting are a reason for a visit to the doctor in order to exclude serious pathology.
Fainting
Clinical manifestations
1. Short-term loss of consciousness (10-30 p.).
2. In history, there are no indications of diseases of cardiovascular, respiratory systems, gastrointestinal tract, not an obstetric and gynecological history.
First aid
1) give the body with a sick horizontal position (without a pillow) with a bit raised legs;
2) unbutton the belt, collar, buttons;
3) spray face and chest with cold water;
4) to lose the body with dry hands - hands, legs, face;
5) give the patient to breathe a pair of ammonia alcohol;
6) intramuscularly or subcutaneously introduce 1 ml of a 10% caffeine solution, intramuscularly 1-2 ml of a 25% solution of Cordiamine.
Bronchial asthma (attack)
Clinical manifestations - See the nursing case in therapy.
First aid
1) put a patient, help take a comfortable position, unbutton collar, belt, provide emotional peace, fresh air access;
2) distracting therapy in the form of a hot foot bath (water temperature at the level of individual tolerance);
3) introduce 10 ml of 2.4% solution of euphilline and 1-2 ml of 1% diploma solution (2 ml of 2.5% solution of the promethazine or 1 ml of 2% chloropiramine solution) intravenously;
4) to carry out inhalation by aerosol of broncholists;
5) In the hormone-dependent form of bronchial asthma and information from the patient about violating the course of hormone therapy, introduce prednisone at a dose and with the method of administration, corresponding to the main course of treatment.
Astmatic status
Clinical manifestations - See the nursing case in therapy.
First aid
1) calm the patient, help take a convenient position, provide fresh air access;
2) oxygen therapy with a mixture of oxygen with atmospheric air;
3) when stopping the breath - IVL;
4) introduce refooliglukin intravenously drip in the volume of 1000 ml;
5) introduce 10-15 ml of 2.4% solution of euphilline intravenously during the first 5-7 minutes, then 3-5 ml of 2.4% solution of EUFILIN intravenously drip in an infusion solution or 10 ml of 2.4 % Euphillin solution every hour in a dropper tube;
6) introduce 90 mg of prednisone or 250 mg of hydrocortisone intravenously;
7) introduce heparin to 10,000 units intravenously.
Notes
1. Receiving sedative, antihistamine, diuretic products, calcium and sodium preparations (including saline) contraindicated!
2. Multiple consistent use of bronchoditics is dangerous due to the possibility of fatal outcome.
Lonantic bleeding
Clinical manifestations
Isolation of bright scarlet blood blood from mouth during coughing or practically without coughing jolts.
First aid
1) calm the patient, help him take a half-time position (to relieve an expectoration), prohibit getting up, talking, call a doctor;
2) to the chest put a bubble with ice or cold compress;
3) to give a patient to drink cold liquid: a solution of a cooking salt (1 tbsp. L salt on a glass of water), decoction of nettle;
4) to carry out hemostatic therapy: 1-2 ml of 12.5% \u200b\u200bdicinone solution intramuscularly or intravenously, 10 ml of 1% calcium solution intravenously, 100 ml of 5% solution of aminocaproic acid intravenously drip, 1-2 ml 1 % Vikasol solution intramuscularly.
In case of difficulty determining the type of coma (hypo-or hyperglycemic), the first help is beginning with the introduction of a concentrated solution of glucose. If a coma is connected with hypoglycemia, then the victim begins to recover, skin covers pink. If there is no response, then the coma is most likely hyperglycemic. At the same time, clinical data should be taken into account.
Hyogolcemic Coma
Clinical manifestations
2. Dynamics of the development of a comatose state:
1) feeling of hunger without thirst;
2) anxious concern;
3) Headache;
4) increased sweating;
5) excitement;
6) overweight;
7) loss of consciousness;
8) cramps.
3. No symptoms of hyperglycemia (dry skin and mucous membranes, decreased leather turgora, softness eye apples, the smell of acetone from the mouth).
4. Fast positive effect from intravenous administration 40% glucose solution.
First aid
1) enter intravenously inkjet 40-60 ml of 40% glucose solution;
2) In the absence of effect, re-introduce 40 ml of a 40% glucose solution intravenously, as well as 10 ml of a 10% calcium solution of chloride intravenously, 0.5-1 ml of 0.1% solution of adrenaline hydrochloride subcutaneously (in the absence of contraindications );
3) when improving well-being, give sweet drinks with bread (to prevent recurrence);
4) Patients are subject to hospitalization:
a) with the first arising hypoglycemic state;
b) in the event of hypoglycemia in a public place;
c) with the ineffectiveness of emergence of emergency medical care.
Depending on the state, hospitalization is carried out on stretchers or on foot.
Hyperglycemic (diabetic) coma
Clinical manifestations
1. Diabetes In history.
2. The development of a comatose state:
1) lethargy, extreme fatigue;
2) loss of appetite;
3) indomitable vomiting;
4) dry skin;
6) frequent abundant urination;
7) decreased blood pressure, tachycardia, heart pain;
8) Adamina, drowsiness;
9) Sportor, coma.
3. Dry skin, cold, dry lips, cracked.
4. Raspberry language with a dirty gray raid.
5. The smell of acetone in exhaled air.
6. Sharply reduced tone of eyeballs (soft to the touch).
First aid
Sequencing:
1) to rehydrate with a 0.9% sodium solution of chloride intravenously drip at a rate of administration 200 ml in 15 minutes. under the control of the level of blood pressure and independent respiration (the brain swelling is possible with too fast rehydration);
2) Emergency hospitalization in the resuscitation department of a multidisciplinary hospital, bypassing the reception office. Hospitalization is carried out on stretchers, lying.
Acute belly
Clinical manifestations
1. Pain in the stomach, nausea, vomiting, dry mouth.
2. Painting with palpation of the front abdominal wall.
3. Symptoms of irritation of peritoneum.
4. Language is dry, covered.
5. Subfebrile, hyperthermia.
First aid
Actually deliver a patient into a surgical hospital on stretchers, in a convenient position for it. Anesthesia, water and food intake are prohibited!
Acute belly and similar states may occur with a variety of pathology: diseases digestive system, gynecological, infectious pathologies. The main principle of first aid in these cases: cold, hunger and peace.
Gastrointestinal bleeding
Clinical manifestations
1. The pallor of the skin, mucousse.
2. Vomiting with blood or "coffee grounding".
3. Black tar eyed chair or volatile blood (with bleeding from the rectum or rear pass).
4. Soft belly. There may be soreness when palpation in the epigastric area. Abdominal irritation symptoms are missing, wet language.
5. Tachycardia, hypotension.
6. In anamnesis - ulcerative disease, oncological disease gasts, liver cirrhosis.
First aid
1) give the patient there are ice with small pieces;
2) with a deterioration of hemodynamics, tachycardia and decreased blood pressure - polyglyukine (REOPOLIGLUKIN) intravenously before stabilizing systolic blood pressure at 100-110 mm Hg. st.;
3) introduce 60-120 mg of prednisone (125-250 mg of hydrocortisone) - add to infusion solution;
4) introduce up to 5 ml of 0.5% dopamine solution intravenously drip in an infusion solution at a critical drop of blood pressure, not amenable to correction of infusion therapy;
5) cardiac glycosides according to indications;
6) Emergency delivery to a surgical hospital lying on a stretcher with a lowered head end.
Renal colic
Clinical manifestations
1. Top-like pains in the lower back one or two-sided, irradiate in groin, scrotum, sexual lip, the front or inner surface of the hip.
2. Nausea, vomiting, bloating with a stool delay and gases.
3. Dysuric disorders.
4. Motor anxiety, the patient is looking for a posture at which pain will be reduced or will cease.
5. The stomach is soft, slightly painful in the course of the ureters or painless.
6. Pickup sickness sickness painfully, peritonean irritation symptoms Negative, wet language.
7. Renal disease in history.
First aid
1) to introduce 2-5 ml of the 50% analgin solution intramuscularly or 1 ml of 0.1% solution of atropine sulfate subcutaneously, or 1 ml of 0.2% solution of hydrotathe platoofillin subcutaneously;
2) to put a hot heater or (in the absence of contraindications) to put the patient in the hot bath. Do not leave it alone, control overall well-being, pulse, chdd, blood pressure, color of skin;
3) Hospitalization: with the first appearance for the first time, with hyperthermia, the unsuccessful binding of the attack at home, with a re-attack during the day.
Renal colic is a complication urolithiasisresulting in disruption of metabolism. The cause of the painful attack is the displacement of the stone and its hit in the ureters.
Anaphylactic shock
Clinical manifestations
1. Communication of the state with the introduction medicinal preparation, vaccines, taking specific food, etc.
2. Feeling fear of death.
3. Feeling of lack of air, stubborn pain, dizziness, noise in the ears.
4. Nausea, vomiting.
5. Causes.
6. Sharp pallor, cold sticky sweat, urticaria, swelling of soft tissues.
7. Tachycardia, threaded pulse, arrhythmia.
8. Sharp hypotension, diastolic blood pressure is not determined.
9. Comath state.
First aid
Sequencing:
1) with a shock caused by the introduction of intravenously drug-allergen, the needle is left in Vienna and use it for emergency anti-shock therapy;
2) immediately stop the introduction medicinal substancewhich caused the development of anaphylactic shock;
3) Give a patient a functionally advantageous position: limbs raise at an angle of 15 °. Rotate the head, with the loss of consciousness to put forward low jaw, remove dental prostheses;
4) to carry out oxygen therapy with 100% oxygen;
5) introduce intravenously 1 ml of 0.1% solution of the adrenaline hydrochloride, divorced in 10 ml of 0.9% sodium chloride solution; the same dose of adrenaline hydrochloride (but without dilution) can be administered under the root of the language;
6) Polyglyukin or other infusion solution to begin to introduce inkid after stabilization of systolic blood pressure per 100 mm Hg. Art. - continue the infusion therapy drip;
7) introduce 90-120 mg of prednisone (125-250 mg of hydrocortisone) into the infusion system;
8) introduce 10 ml of a 10% calcium solution chloride into an infusion system;
9) in the absence of an effect from the treatment carried out, repeat the administration of hydrochloride adrenaline or introduce 1-2 ml of 1% mesaton solution intravenously inkjet;
10) at bronchospasm to introduce 10 ml of a 2.4% solution of euphilline intravenously;
11) during laryingospasm and asphyxia - conicotomy;
12) If the allergen was introduced intramuscularly or subcutaneously or an anaphylactic reaction arose in response to the insect bite, it is necessary to comply with the place of injection or bite 1 ml of 0.1% solution of adrenaline hydrochloride, diluted in 10 ml of 0.9% sodium chloride solution ;
13) If Allergen entered the body orally, it is necessary to rinse the stomach (if the patient's condition allows);
14) for convulsive syndrome introduce 4-6 ml of 0.5% diazepam solution;
15) for clinical death Conduct cardiovascular resuscitation.
In each procedural office, it must be in stock a first-aid kit to provide first aid for anaphylactic shock. The most often anaphylactic shock is developing during or after the introduction of biological preparations, vitamins.
Sweet Qincke
Clinical manifestations
1. Communication with an allergen.
2. Itchy rash in different parts of the body.
3. The edema of the rear of the brushes, stop, tongue, nasal moves, oroglotka.
4. Wildness and cianoz face and neck.
6. Mental excitement, motor anxiety.
First aid
Sequencing:
1) stop introducing allergen to the body;
2) introduce 2 ml of a 2.5% solution of the promethazine, or 2 ml of a 2% solution of chloropyramine, or 2 ml of a 1% solution of DIMEDROL intramuscularly or intravenously;
3) to introduce 60-90 mg of prednisolone intravenously;
4) to introduce 0.3-0.5 ml of a 0.1% solution of adrenaline hydrochloride subcutaneously or, dilute the preparation in 10 ml of a 0.9% sodium solution of chloride, intravenously;
5) to carry out inhalation with bronchoditics (phenoterol);
6) be ready for conforming;
7) hospitalize the patient.
Send your good work in the knowledge base is simple. Use the form below
Students, graduate students, young scientists who use the knowledge base in their studies and work will be very grateful to you.
Posted by http.:// www. allbest.. ru/
- fainting
- Collapse
- Hypertensive crisis
- Anaphylactic shock
- Stenokard attack
- Acute myocardial infarction
- Clinical death
Algorithms for the provision of first medical care during urgent states
Fainting
Fainting - a fit of a short-term loss of consciousness due to the transient brain ischemia associated with the weakening of cardiac activity and the acute violation of the regulation vascular tone. Depending on the severity of factors contributing to the violation of the cerebral circulation.
Allocate: brain, heart, reflex and hysterical types of trimming states.
Stages of faint development.
1. Prerefficers (pre-corrosive condition). Clinical manifestations: discomfort, dizziness, noise in the ears, lack of air, the appearance of cold sweat, numbness of fingertips. It lasts from 5 seconds to 2 minutes.
2. Violation of consciousness (actual faint). Clinic: loss of consciousness lasting from 5 seconds to 1 minute, accompanied by pallhery, reduced muscle tone, expansion of pupils, weak response to light. Surface breathing, bradypognoe. Pulse labile, more often bradycardia to 40 - 50 per minute, systolic blood pressure decreases to 50 - 60 mm. RT. Art. With deep fainting, convulsions are possible.
3. Post-clean (recovery) period. Clinic: It is properly oriented in space and time, a pallor, rapid breathing, labile pulse and low blood pressure can be maintained.
Algorithm medical events
2. Unbutton collar.
3. Provide fresh air access.
4. Wipe the face with a wet cloth or irrigating cold water.
5. Inhalation of the vapor of ammonium alcohol (reflex stimulation of respiratory and vessels).
With the ineffectiveness of the listed events:
6. Caffeine 2.0 V / V or V / m.
7. Cordiamine 2.0 V / m.
8. Atropine (in bradycardia) 0.1% - 0.5 p / k.
9. When leaving trimming state Continue dental manipulations with the adoption of measures to prevent recurrence: treatment horizontal position Patient with adequate premedication and with sufficient anesthesia.
Collapse
Collapse is a severe form of vascular failure (reduction of the vascular tone), manifested by a decrease in blood pressure, the expansion of venous vessels, a decrease in the volume of circulating blood and the accumulation of it in the blood depot - liver capillary, spleen.
Clinical picture: sharp deterioration general status, pronounced pallor of skin, dizziness, chills, cold sweat, sharp decrease in blood pressure, frequent and weak pulse, frequent, surface breathing. Peripheral veins are inserted, the walls are falling down, which makes it difficult to perform venopunction. Patients retain consciousness (with fainting patients lose consciousness), but indifferent to what is happening. Collapse can be a symptom of such severe pathological processes as myocardial infarction, anaphylactic shock, bleeding.
Algorithm of therapeutic measures 1. Patient give a horizontal position.
2. Ensure the influx of fresh air.
3. Prednisolone 60-90 mg in / c.
4. Norainerenaline 0.2% - 1 ml of V / B by 0.89% solution of sodium chloride.
5. Meston 1% - 1 ml in / in (to increase the venous tone).
6. Corglukol 0.06% - 1.0 V / in slowly 0.89% sodium chloride solution.
7. Polyglyukine 400.0 V / in a drip, 5% glucose solution in / in drip 500.0.
Hypertensive crisis
Hypertensive crisis is a sudden rapid increase in blood pressure, accompanied by clinical symptoms from the organs of targets (more often than brain, retina, heart, kidneys, gastrointestinal tract, etc.).
Clinical picture. Sharp headaches, dizziness, ears, often accompanied by nausea and vomiting. Violation of sight (grid or fog before eyes). The patient is excited. At the same time, there is a trembling of hands, sweating, sharp redness of the skin of the face. Pulse is tense, blood pressure is increased by 60-80 mm. RT. Art. Compared to normal. During the crime, angina attacks may occur, an acute violation of cerebral circulation.
The algorithm of therapeutic measures 1. intravenously in one syringe: dibazole 1% - 4.0 ml with papaverine 1% - 2.0 ml (slow).
2. Ply severe course: Clofelin 75 μg under the tongue.
3. Intravenously laziks 1% - 4.0 ml on a physiological solution.
4. Anaprilin 20 mg (with pronounced tachycardia) under the tongue.
5. Sedatives - Elenium inside 1-2 tablets.
6. Hospitalization.
It is necessary to constantly monitor blood pressure!
first Medical Synch
Anaphylactic shock
Typical form of medicinal anaphylactic shock (LASH).
The patient is acute a state of discomfort with uncertain sensations. There is a fear of death or a state of internal anxiety. There is nausea, sometimes vomiting, cough. Patients complain of harsh weakness, feeling of tingling and itching the skin of the face, hands, head; Feeling of blood tide to the head, face, feeling of chest or gravity chest; The appearance of pain in the field of heart, the difficulty of breathing or the inability to do exhale, for dizziness or headache. The disorder of consciousness occurs in the terminal phase of shock and is accompanied by violations of speech contact with patients. Complaints arise immediately after receiving a drug.
Clinical picture of LASH: hyperemia of skin or pallor and cyanosis, edema of the face, abundant sweating. Breathing noisy, tachipne. Most patients develop motor anxiety. Midship is noted, the reaction of pupils into light is weakened. Pulse frequent, sharply loosened on peripheral arteries. Hell decreases quickly, in severe cases, diastolic pressure is not determined. A shortness of breath appears, difficulty breathing. Subsequently develops clinical picture Emirates of the lungs.
Depending on the severity of the flow and time of the development of symptoms (from the moment of administration of the antigen), the lightning (1-2 minutes) is distinguished, heavy (in 5-7 minutes), middle severity (up to 30 minutes) shape of shock. The shorter time from the administration of the drug to the occurrence of the clinic, the hardest shock flows, and the less chances for the prosperous outcome of treatment.
The algorithm of therapeutic measures urgently provide access to Vienna.
1. Stop the introduction of the medicine that caused anaphylactic shock. Call "on yourself" by the ambulance brigade.
2. Put the patient, lift the lower limbs. If the patient is unconscious, turn your head on the side, push the lower jaw. Inhalation of hydrated oxygen. Lung ventilation.
3. Intravenously introduce 0.5 ml of 0.1% adrenaline solution in 5 ml of isotonic sodium chloride solution. With the difficulty of venopunction, adrenaline is injected into the root of the tongue, perhaps intraterably (puncture of the trachea below the thyroid cartilage through a conical ligament).
4. Prednisolone 90-120 mg V / c.
5. Dimedrol solution 2% - 2.0 or Supratine solution 2% - 2.0, or a solution of diprage 2.5% - 2.0 V / c.
6. Cardiac glycosides according to the testimony.
7. When obstruction respiratory tract - oxygen therapy, 2.4% solution of euphilline 10 ml / in physical. solution.
8. If necessary, endotracheal intubation.
9. Hospitalization of the patient. Identification of allergies.
Toxic reactions to anesthetics
Clinical picture. Anxiety, tachycardia, dizziness and weakness. Cyanosis, muscle tremor, chills, convulsions. Nausea, sometimes vomiting. Respiratory disorder, decreased blood pressure, collapse.
Algorithm of therapeutic events
1. Give a sick horizontal position.
2. Fresh air. Give breathe a couple of ammonia alcohol.
3. Caffeine 2 ml p / k.
4. Cordiamine 2 ml n / k.
5. In the oppression of breathing - oxygen, artificial respiration (according to indications).
6. Adrenaline 0.1% - 1.0 ml per nat. solution in / c.
7. Prednisolone 60-90 mg V / c.
8. TAVEGIL, Supratin, Dimedrol.
9. Cardiac glycosides (according to indications).
Stenokard attack
Stenokard attack - Paroxism of pain or other unpleasant sensations (heaviness, compression, pressure, burning) in the heart area duration from 2-5 to 30 minutes with characteristic irradiation (in the left shoulder, neck, left blade, lower jaw) caused by the excess of myocardium intake In oxygen over its admission.
Provoking the attack of the angina increase arterial pressure, psycho-emotional tension, which always takes place before and during the treatment of a dentist's doctor.
Algorithm of therapeutic measures 1. Termination of dental intervention, peace, fresh air access, free breathing.
2. Nitroglycerin in tablets or capsules (capsule to greet) 0.5 mg under the tongue every 5-10 minutes (only 3 mg under the control of AD).
3. If the attack is stopped, the recommendations of the outpatient surveillance of the cardiologist. The resumption of dental benefits - to stabilize the state.
4. If the attack is not stopped: barallgan 5-10 ml or analgin 50% - 2 ml in / in or in / m.
5. In the absence of the effect - a challenge of ambulance and hospitalization team.
Acute myocardial infarction
The acute myocardial infarction is the ischemic necrosis of the heart muscle, resulting from an acute inconsistency between the need of a portion of myocardium in oxygen and its delivery according to the relevant coronary artery.
Clinic. The most characteristic clinical symptom It is pain that is more often localized in the sternum heart region, less often captures the entire front surface of the chest. Irradiate B. left, shoulder, shovel, inter-documenny space. Pain is usually waveled: it is strengthened, it weakens, it continues from several hours to several days. Objectively marked the pallor of the skin, cyanosis lips, increased sweating, decreased blood pressure. Most patients are broken heartbeat (Tachycardia, extrasystole, flickering arrhythmia).
Algorithm of therapeutic events
1. Urgent cessation of intervention, peace, fresh air access.
2. Call a cardiac ambulance brigade.
3. With systolic blood pressure? 100 mm. RT. Art. Under 0.5 mg nitroglycerin in tablets every 10 minutes (total dose of 3 mg).
4. Mandatory relief of pain syndrome: Baralgin 5 ml or analgin 50% - 2 ml in / in or in / m.
5. Inhalation of oxygen through a mask.
6. Papaverin 2% - 2.0 ml in / m.
7. Eufillin 2.4% - 10 ml per nat. R-re / c.
8. Relanyium or Sedukene 0.5% - 2 ml 9. Hospitalization.
Clinical death
Clinic. Loss of consciousness. No pulse and heart tones. Stop breathing. Pallor and sinusiness of the skin and mucous membranes, no bleeding from the operating wound (tooth hole). Expansion of pupils. The respiratory stop is usually preceded by a heart stop (in the absence of breathing, the pulse is preserved on carotid arteries and pupils are not expanded), which is taken into account when resuscitation.
Algorithm of therapeutic measures Resuscitation:
1. To put on the floor or couch, throw back the head, push the jaw.
2. Clean the respiratory tract.
3. Enter the air duct, carry out artificial ventilation of the lungs and the outer heart massage.
when resuscitation by one person in the ratio: 2 breaths on 15 sander of the sternum; When resulsion together in the ratio: 1 breath on 5 soreness of the sternum. Consider that frequency artificial respiratory - 12-18 per minute, and the frequency of artificial blood circulation - 80-100 per minute. Artificial ventilation The lungs and the outer massage of the heart are held before the arrival of the "resuscitation".
During resuscitation, all drugs are administered only intravenously, intracardular (adrenaline preferably - interphoneal). After 5-10 minutes of injection repeat.
1. Adrenaline 0.1% - 0.5 ml in breeding 5 ml. Phys. Enormous solution or glucose (preferable - inter-tech).
2. Lidocaine 2% - 5 ml (1 mg per kg of weight) V / B, intracardiac.
3. Prednisolone 120-150 mg (2-4 mg per kg of weight) V / B, intracardiac.
4. Sodium bicarbonate 4% - 200 ml in / c.
5. Ascorbic acid is 5% - 3-5 ml in / c.
6. Cold to the head.
7. Laziks according to the testimony of 40-80 mg (2-4 ampoules) in / c.
Resuscitation is carried out taking into account the available asistolis or fibrillation, for which the data of electrocardiography is necessary. When diagnosing fibrillation, a defibrillator is applied (if the latter is available), preferably prior to medication therapy.
In practice, all listed events are held simultaneously.
Posted on Allbest.ru.
...Similar documents
Causes of development and clinical picture of anaphylactic shock. Emergency medical care in arterial hypotension, attacks of angina, myocardial infarction, collapse and bronchial asthma. Pathogenesis and the main causes of fainting.
abstract, added 03/13/2011
Conducting urgent events at all stages of medical care in urgent states threatening the patient's life and health. The procedure for assisting in bleeding, fractures, thermal lesions, solar and thermal blows.
methodology, added 04/17/2016
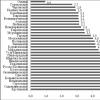
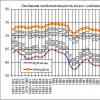
The causes of I. clinical manifestations Hypertensive crisis, its types and typical complications. Electrocardiographic changes in hypertensive crisis. First aid, drug therapy. Algorithm actions of the medical sister.
presentation, added 12/24/2016
general characteristics Hypertensive crisis: etiology, pathogenesis, kinic picture. Basic symptomsomplexes for distinguishing crises of the first and second orders. Typical complications for the disease, the order and methods of providing first emergency care.
presentation, added 03.12.2013
Causes of hypertensive crisis, its main signs. Mechanisms due to the rise of blood pressure. Symptoms of a hypertensive crisis with a predominance of neareegetative syndrome. First medical care for hypertensive crisis.
presentation, added 09/26/2016
The concept of urgent states. The main types of urgent states and emergency care for outpatient dental interventions. Preparations to provide urgent assistance in the office of the dentist. Allergy reaction to a particular anesthetic.
presentation, added 30.10.2014
The concept and assessment of the prevalence of hypertensive crises, the causes and prerequisites of their occurrence, classification and types. Diagnostic criteria for this pathology, features of questioning and inspection. Tactics and main stages of medical care.
presentation, added 11/14/2016
The concept and clinical picture of bleeding; Their classification by origin, the form of a bleeding vessel and the location of blood outpour. Rules imposing arterial harness. Causes of traumatic shock; Principles of first aid.
presentation, added 10/21/2014
The study of the erectile and traumatic phases of traumatic shock. Diagnosis of shock degree. Determining the value of the shock index. Correction of respiratory failure. Algorithm of emergency medical care in urgent states at the prehospital stage.
report, added 23.12.2013
Hypertensive crisis as one of the most frequent and dangerous complications hypertensive disease, his clinical manifestations and characteristic symptoms, Forms and first aid rules. Differential diagnosis Hypertensive crises and its complication.
Emergency medical care - A complex of medical measures aimed at the treatment of life-proceeding states.
The main stages and methods for the provision of emergency medical care
Emergency medical care can have any prepared people: from the doctors of all specialties to employees of salvation services, internal affairs. Paramedics and specially trained volunteers are equal to them.
The provision of self-help can also be included in the general stage. But, officially medical help is considered only for the military.
The beginning of the provision of emergency medical care can be anywhere. The main criterion is, except for the most affected, the presence of at least one person prepared for this.
In the process of providing emergency medical care, several levels are distinguished. For emergency situations and disasters, they are considered as stages.
- first aid. It is not conducted by non-medical personnel prepared for this: firefighters, police, rescue services, specially trained volunteers.
- first before medical Help. Its junior and medium medical personnel. Paramedics are equal to them.
- first medical care. In its provision, doctors are involved wide specialties. Most often these are doctors ambulance and resuscitation.
- specialized medical care - doctors of narrow specialties.
Legal documents and legislation
In Russia, as almost all over the world, emergency medical care is on free grounds.
In the first stages, starting from the end of the 19th century, this prerogative was in the statement of private and public organizations, such as the Red Cross, the Society of Mercy, etc., only at the dawn of the last century, the first government structures on the provision of emergency medical care are born. And these were ambulance carriages. At the beginning, they had Feldscher and Sanitar, and then medical staff.
After the First World War and the Revolution, the first staffed "Emerral" units were established in Soviet Russia. And the experience of the Second World War poured into the creation of the stratification of emergency medical care. But, before the beginning of the last decade of the last century, there was no single document that would regulate emergency assistance.
Creature federal Law About medical care, where in chapter 39th, o "... emergency medical care" the first legal norms were drawn, the basis of future bills. Including the current law on the protection of the health of the citizens of the Russian Federation from 2012.
Basic urgent states
The main criterion of the urgent state is the time before the occurrence of death. For urgent states, not medical care can lead to death in the next few hours and days.
The main urgent states include:
- poisoning.
- injuries meaningful for the body of the departments.
- acute diseases vital organs.
Not medical care
Refusal to provide emergency medical care to persons (persons) obligated (MI) is a criminal violation.
There are only two situations when these persons may not provide emergency medical care:
- a person is not able to carry out his duties that do not depend on it. It may be injuries of the rescuer himself or another other state that does not allow him to fulfill its job responsibilities.
- terminal states caused by severe diseases and are not compatible with life injuries. In peacetime, it terminal state In cancer patients with 4 clinical groups. The latter refer to emergency situations and catastrophes when there is a large number of victims per unit providing medical assistance exceeding its functionality. This measure is adopted for more efficient work of medical professionals in the focus of the catastrophe.
The most important thing before the arrival of doctors is to end the influence of factors that worsen the well-being of the affected person. This step implies the elimination of the life-threatening processes, for example: to stop bleeding, overcoming asphyxia.
Determine the actual status of the patient and the nature of the disease. The following aspects will help this:
- what are the values \u200b\u200bof blood pressure.
- whether visually bleeding wounds are noticeable;
- present in the patient the reaction of pupils into light;
- whether the heart rhythm has changed;
- saved or no respiratory functions;
- how adequately a person perceives what is happening;
- the victim is conscious or not;
- if necessary - ensuring respiratory functions by accessing fresh air and gaining conviction in the absence of foreign objects in the blowers;
- carrying out non-invasive pulmonary ventilation (artificial respiration according to the "mouth in the mouth" method);
- the implementation of indirect (closed) in the absence of a pulse.
Quite often, the preservation of health and human life depends on the timely provision of high-quality first aid. With urgent states, all victims regardless of the type of disease requires competent emergency action before the arrival of a medical brigade.
First medical care for urgent states can not always be proposed by qualified doctors or paramedics. Each contemporary should own the skills of pre-departments and know the symptoms of common diseases: the result depends on the quality and timeliness of the measures, the level of knowledge, the availability of skills in witnesses of critical situations.
ABC algorithm
Emergency prefiguration actions suggest the implementation of a complex of simplerapeutic and preventive Mer Directly on the place of the tragedy or next to it. The first medical care for emergency conditions, regardless of the nature of the illness or obtained, has a similar algorithm. The essence of events depends on the nature of the symptoms of the affected person (for example: loss of consciousness) and from the alleged causes of occurrence emergency (for example: hypertensive crisis arterial hypertension). Rehabilitation activities within the provision of first medical care in emergency conditions are carried out according to unified principles - the ABC algorithm: these are the first English letters denoting:
- Air (air);
- Breathing (breathing);
- Circulation.