Increased carbon dioxide in the blood. Analysis of blood gases. Arterial gases
Analysis on arterial blood gases measures acidity, carbon dioxide and oxygen level in blood from the artery. This analysis shows how well your lungs deliver oxygen into blood.
When blood passes through your lungs, it is saturated with oxygen and then spreads it throughout the body. At the same time, carbon dioxide from the blood is removed light. The analysis of blood gases is taken from the artery, because arterial blood does not have time to give oxygen to the tissues of the body, and the real ratio of carbon dioxide and oxygen in the blood can be measured.
In addition, with the help of analysis of gases, arterial blood can be measured:
- Partial oxygen pressure. The partial oxygen pressure is an indicator of how easily oxygen falls from the lungs into the blood.
- Partial pressure of carbon dioxide. The partial pressure of carbon dioxide is an indicator of how easily carbon dioxide leaves blood.
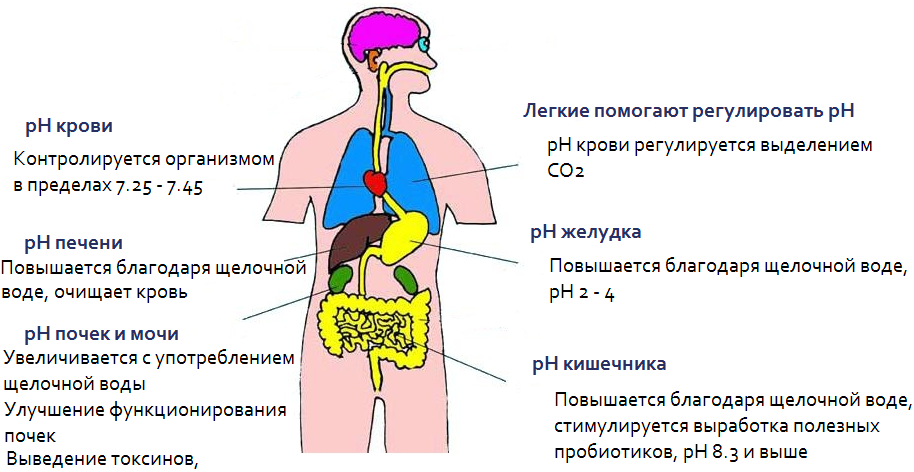
- pH. The pH level shows the content of hydrogen ions in the blood. The blood pH blood level is usually between 7.35 and 7.45. If the pH level is below 7.0, then it is considered acid. Level above 7.0 - it is alkaline. Normal blood Slightly alkaline.
- Bicarbonate. (HCO3). Bicarbonate is a chemical that supports the desired pH level in the blood.
Our clinic has specialized professionals on this disease.
(7 specialists)
2. Why is the analysis?
Analysis of blood gases is done in order to:
- Diagnose the problems of respiration and diseases of lungs: asthma, fibrous-cystic degeneration and chronic obstructive pulmonary disease;
- See how taking the treatment of lungs;
- Determine whether additional oxygen is required (mechanical ventilation of the lungs);
- Measure acid Alkaline Balance blood from people with heart or renal failure, diabetes, sleep disorder, severe infections.
3. How is the analysis?
How to prepare for blood gases analysis?
Tell your doctor if:
- You are taking roofing and other drugs;
- You are allergic to anything.
How is blood gas analysis?
Blood analysis per gases is carried out after taking blood from the artery. Blood fence is carried out according to the standard procedure.
What are the risks of blood gas analysis?
The risks of blood gas analysis are conjugate with the type of blood from the artery and include:
- Bruise at the point of puncture;
- Dizziness, nausea during blood fence;
- Bleeding;
- Damage to the nerve needle (in rare cases).
4. What can interfere with blood gases analysis?
The reasons why the analysis on blood in the blood can become a non-response:
- Heat or reduced temperature;
- Anemia or erythrocytosis. They affect the amount of oxygen that can be transferred to blood;
- You smoked, breathed tobacco smoke or were in a gasped room immediately before surrender.
What should I know about?
Arterial blood gases should be measured together with other indicators, because They alone do not give enough information to diagnose the disease. If a lot of material needs to analyze the gases of arterial blood, then it can be assembled through the catheter.
The blood of a person is connective tissue The organism, which includes plasma and cells (erythrocytes, leukocytes, platelets). Define gas composition blood is the content of carbon dioxide and from the diagnostic and practical side.
The excess of an acceptable threshold (more than 7.8) threatens the patient not only by heavy diseases, but also fatal. The decrease in the pH (less than 6.7) warns the occurrence of pathological processes.
Biosynthesis, the supply of tissues and organs with oxygen, nervous and muscular transmission, stimulating cell fermentation - all this depends on the acidity of blood and the stability of the reactions inside the human body. To cope with these difficult tasks, there are schemes of weak bases and acids mitigating a blow that are called "buffered" and is biomechanisms of physiological nature that ensure the concentration of hydrogen in the blood. Let us turn to the table of the gas composition of the human blood.
The bicarbonate buffer system of blood consists of potassium bicarbonate and sodium with coal-doser acid (H2CO3). The scheme of its impact is simple: if the body is found in the body of free acids and the acidity of the medium is increasing, the sodium bicarbonate deactivates this process by binding them. This reaction gives coal biennial acid (H2CO3), separated from the body.
If there is an excess blood alkalis, then coal dibasic acid (H2CO3) begins to act and split them on sodium bicarbonate and water, neutral and harmless to life.
A different path leading to pH stability has a phosphate system. This is a compound of monohydrophosphate and sodium phosphate. When penetrating extra acids into blood, it forms a salt, neutral for humans. Thus, contributing to the normal acidity of blood.
The most powerful protective system in the blood consists of hemoglobin. This complex protein includes a histidine amino acid, which has both acids and their base.
Using the amide and carboxylic systems, which include hydrogen and anions of coal dioxide acid, the launch of the sodium bicked (NaHCO3). It copes perfectly with the support of blood acid and alkaline equilibrium. Carbohemoglobin, created by the described reaction in a compound with carbon dioxide, also protects the acidity of unwanted oscillatory processes.
Another protective system is called protein. They have alkaline and acid properties, capable of transformation with a violation of equilibrium. Their small percentage does not interfere with the correction of the gas composition of the blood.
Acid-alkaline balance stabilization
The gastrointestinal tract that performs the functions of food processing and extraction of useful elements, light and other organs carry out a major role in bringing an acid-alkaline balance rate.
Lights are intended to separated coal biennic acid from the blood fluid (H2CO3), which with the interaction of bicarbonic salts decomposes on carbon dioxide and water (H2O). From the cells of the body in the gaseous form, carbon dioxide is removed, and its largest part in the liquid state is transported to the blood plasma and respiratory organs.
The role in the stabilization of equilibrium is performed by the kidneys. Watering has an acidic medium, and the kidney becomes the filter, the acidic and alkaline excess are binding through the sodium bicked and remove them from the body, adjusting the acid and alkaline balance.
Human digestive organs have not the most important value for adjusting the gas composition of blood in the body. Pancreas produces a bicarbonate sodium, hydrogen chloride and during their flow in the direction they provide assistance, normalizing the gas composition in the blood. With intestinal functionality disorders and gastric tract A pH imbalance may occur.
Latching the blood fluid appears due to the increased acidity of the stomach with many unpleasant diseases, for example, gastritis or ulcer.
PH values:
- an acceptable indicator of the pH-7,30 - 7.50;
- partial pressure -36-44 mm.rt;
- bicarbonate - 21-29 mmol / l;
- protective bases - their surplus or insufficiency 45-65 mmol / l.
These figures characterize the body absolutely healthy man. But when pathologies occur, they change. If the gas composition of the blood of a person is oxidized, doctors call this process "acidosis", and if there is a lacheling - "alkalosis".
The nature of the changes of the gas composition is respiratory and metabolic. Respiratory is in full dependence on carbon dioxide rate. Metabolic is associated with a reaction to changes in the presence of sodium bicarbonate in the blood fluid.
When the activities of buffer protective systems, acidosis and alkalosis are unprofitable, and are often compensated. But if there is no balancing of the gas composition of the blood, the pH level goes for the permissible threshold. The situation is immediately carried out dangerous, and the progressiveness of these disorders leads to the mass of diseases and even a fatal outcome.

Laboratory tests
There are analyzes by which the gas composition is determined. They are carried out if a doctor has a suspicion of primary hyperventilation or respiratory failure.
It is carried out laboratory methods and the main indicators to pay attention to are the concentration of oxygen and carbon monoxide. The detection of the content of these dissolved gases in plasma and body tissues shows the oxygen treatment or light ventilation.
Acidness rate (pH): The change in the concentration of hydrogen ions reflects either a normal blood reaction, or a sour or alkaline Normal value pH \u003d 7.36 -7.44.
Paco 2. - partial pressure of carbon dioxide in arterial blood. This is the respiratory component of the regulation of the acid-base state. It depends on the frequency and depth of breathing (or adequacy holding IVL). Hypercapnia (PACO 2\u003e 45 MMHG) is a consequence of alveolar hypoventilation and respiratory acidosis. Hyperventilation leads to hypocretion - a decrease in the partial pressure of CO 2 below 35 mmHG and respiratory alkalosis
PAO 2. - Partial oxygen pressure in arterial blood. This value does not play a primary role in the control of Kos, if within the normal range (at least 80 mmHg).
SPO 2 -saturation of hemoglobin arterial blood oxygen.
BE (ABE) - deficit or excess grounds. In general, the number of blood buffers reflects. Anomal high mean Characteristic for alkalosis, low - for acidosis. Normal value - ± 2.3
HCO 3 - - Plasma Bicarbonate. The main renal component of the regulation of the brass. Normal value of 24 meq / l. The decrease in bicarbonate is a sign of acidosis, an increase in alkalosis.
Homeostasis is the constancy of the body's interior.
It is necessary to preserve KS. - quantitatively characterized by the concentration of ions H + - POWER HYDROGENE - hydrogen power. Enzymatic reactions in the body flow in a narrow diapass of pH -7.3-7.5
As a result of the metabolism of proteins in the body, non-volatile acids are formed (sulfur, phosphoric). During the day only when nutrition in the body, so many acids would have formed that pH would be 2.7, but the body neutralizes these acids. In the cage and the intercellular pH substance relatively constantly in the blood, 7.35- 7.45. In the cytoplasm 7.0- 7.3V of lysosomes 4.5, 5.5 in the pH2 stomach, in the intestine, where bicarbonates, pH 8 are present. The kidneys can also be separated by the acids and bases of the pH in the kidneys of 4.8-7.5.
Acids and bases.
Acids are able to give protons of H +, the bases are capable of taking protons. Water
Dissociates on H + and it_ behaves like an acid and as a base.
In the body, everything in-in is in the water. The HCL in water behaves like an acid, giving a proton turns into Cl, and forms protonated water molecules, it, H2O, H +.
In acid-primary reactions take part acid and the base conjugate to it.
The total concentration of cations (Na +, Mg, K +, Ca +, H +) anions (CL-, HCO2-, PO4-,
SO4-). 310 155 mmol \\ l of them Na + 142 mmol \\ l, CL 103 mmol \\ l 27 mmol \\ l NSO3 and 15 mmol \\ L proteins. NSO3 and proteins - buffer systems.
The main paths of exchange H +.
Acceptor H + is O2, forming water. O2 comes from an external environment with the participation of mechanisms of controlling ventilation, blood circulation, reversible binding from O2, its diffusion through an interstitial space to cells and activation in mitochondria. In addition to O2, there are several intermediate accepters of N +-dehydrooginases, NADF, FAD, which are contained in hyaloplasm and mitochondria, carrying out the transfer H \u003d O2 and for the synthesis of ATP, with a lack of accects, these enzymes are either completely saturated with protons and stop their dehydrogenic functions, or tolerate Protons to capable of adopting their substrates of adjacent metabolic pathways. (This is a lactial path H \u003d can connect amicransport, they all bind protons and release dehydrogenases)
In the compensation of the pH shifts, the extracellular space is always involved in the non-surprising substrates at increased metabolism and with a lack of O2. This movement is provided by the H + concentration gradient, on both sides of the cell membrane.
One of the ways to release the cell from CO2 and H2O is to turn them into H2 CO3, which dissolves more in water and binds to buffer systems. It depends on the function of circulatory and breathing. With SSI DN, an additional stage of CO2 + H2O + H2CO3 -----NO-NSO3 The resulting proton is associated with HB and is transported to a light, ANSO3- In exchange for CL leaves the cell and binds to the NA ions, the main buffer component is increasing. Systems. This reaction occurs in the presence of carbanese (enzyme containing zinc). Carboangeerase is contained in the epithelium of the stomach, pancreas in the kidneys, pulmonary capillaries and in red blood cells. Everywhere, where there is carboangestrase takes place this reaction.
Buffer systems.
Systems supporting a certain concentration of H +.
The BS function, prevents the pH shifts by the interaction with both acid and base. The effect of the BS is directed mainly to the neutralization of acids The buffer system is a combination of weak acid and a salt of formed by this acid and a strong base. When the buffer systems are turned on, a strong acid (or base) is replaced with a weak, the number of free H + decreases.
The main buffer systems: bicarbonate, phosphate, protein and HB. The blood plasma is significant protein and bicarbonate system, phosphate and HB cells. Bicarbonate accounts for 53%.
Buffer systems are transport. They transport compounds to excretory systems, respectively depend on the state of hemodynamics and the functions of the isolation organs.
The bicarbonate buffer system is represented by coalic acid components2 CO3 and Bicarbonate anion NSO. H2CO3 proton donor NSO proton acceptor. With normal blood pH, the NSO3 is 20 times higher in the blood than H2CO3. With a high concentration of H in the blood, it binds to the NSO3, it is formed by H2CO3, which disintegrates on H2O, and CO2 and is removed by light, due to hyperventilation under the action of carboangendresses. If there are more bases in the blood, they interact with H2 CO3, it is formed H2O and NSO3 because it is weak acid and it dissociates. The larger the cells are formed in the cells, the greater the NSO3 consumption occurs and the kidneys are connected, which in the extraction of H + and the number of NSO3 is restored. BBS is presented in the form of sodium and potassium salts that are easily dissociated. CN2 CO3, NA NSO3
Phosphate BS. NA H2 PO4 and NA NR4 are represented by these systems can also bind H + and on-FBS provides tissue and renal regulation of the COP. The function is mainly in the regeneration of the bicarbonate buffer. In the kidneys at the first stage of the formation of urine. The glomerular filtration is formed by the plasma ultrafiltrate in composition. A similar plasma contains a significant amount of NSO3. When filtering, the NSO3 level drops in the proximal tubules with the participation of carboangendresses begins the reabonservation process of the renal impermeable tubing for NSO3 and reabsorption goes through intercellular spaces. But this is not enough for the NSO3 in the body in the body, it is necessary to constantly replenish in the enlightement of the tubules, CO2 is formed that diffuses in the cells and under the action of carbanenshydrase forms H2CO2 CO3 again dissociates and forms 3 and N.Tho so-called new bicarbonate.
Ammoniogenez: a tubule kidney allocated anions silnyhneotrganich and org acids videammoniynyht soleykletki tubules deamination and amino deamidated form ammonia main source glutaminkotory deaminated glutaminase forming amiak40% ammonia produced from alanine and glitsinaAmiak secreted into the lumen of the tubule forming NH4 in distal tubules in urine secreted by H + ions which bind to NR4 or NN3 in the channel filtrate, and the NSO3 returns to the plasma, the secretion of non-volatile organic acids occurs. Phosphate and ammonium buffer systems are involved in the formation of bicarbonates. NA n RO4 disintegrates sodium exchanges on H + OIN and returns to the plasma, H2 ROCH is displayed with urine. When the phosphate buffer is exhausted, ammonium BS in the blood is glutamine combined with H2O and glutamate and nn4 Titrate urine acids Na2 HPO4 + H \u003d Na2PO4
The HB buffer system takes the 2nd place after bicarbonate depends on the concentration of NV. CO2 in erythrocytes under the action of carboanhydrase turns into H2 CO3. Which dissociates on H + and NSO3 at the same time H is captured by HV and phosphates, and the NSO3 returns to the blood. Exchangeing on Chloro Erythrocytes chlorine connects with potassium forming KCl. In the lungs, the nautical NVO binds to potassium, KNO and chlorine is displaced into the blood and connects with sodium. . Belle buffer system
Proteins can bind and n + and on-. Due to the amino group, the NN2 can connect or give H + cleavage of amino acids occurs in mitochondria, the formation of hydrogen ions from carbohydrates and fats. The exchange of NN3 and protons are conjugate. When interacting with water NH3, NN4 ONT.E.Dech is formed. It is displayed by the kidney by the form of the NN4 SL. Then. The acids formed by the metabolism are proceeding under the control of buffer systems. CO2 is distinguished through Lögkik, and non-volatile acids are excreted by the kidneys. The renal mechanism during acidosis begins to act in 12 hours. Renal RH maintenance mechanisms include NSO3 reabsorption in proximal tubules, ion excretion
The role of DS in the regulation of Kos. With the accumulation of CO2 ions, the DC and the hyperventilation is irritated, due to CO2, with a decrease in CO2 concentration hypoventilation. Pulmonary mechanisms provide temporary compensation for acidosis. In this case, the dissociation curve of the NVO left to the left and decreases the container of arterial blood.
The role of the gastrointestinal tract and skin in the regulation of the brass.
Power affects the body of the body. When receiving vegetation food, acidic products are formed less and vice versa. Protein food of animal origin boils the inner medium because Salts of sulfur and phosphoric acids. Alcoholic beveragesMineral, also lead to a change in brass.
NCL is formed in the stomach. Under the action of carboangendresses in the stomach cells, hydrogen ions are also formed, chlorine anions enter the cells in exchange for bicarbonate from the sodium of plasma chlorine but does not occur. In the intestine chlorine, chlorine is absorbed into the blood in the 12 host enzymes of the pancreas, which have an alkaline character. But they are quickly absorbed into the blood. It does not turn out to be a significant effect on the CBO. In the liver, the oxidation of organic acids, lactic acid in the Krebs cycle occurs, the amino acids, the formation of ammonia, which is excreted by the kidneys occurs. The skin also derives non-volatile acids, especially when the kidney function is violated.
Laboratory indicators.
pH indicator Kos,
rSO2 indicator of partial voltage CO2 in the blood is normal 40mmrt, reflects functional state DS.
pO2 The calculator of the partial pressure O2 blood \u003d 80-100 mm RT Art may be a reflection of DS and tissue metabolism.
Bb buffer bases plasman. The sum of all components of BS-biccarbonate, HB, protein, phosphate- 31,8-65 mmol \\ l.
Weiring of buffer bases (3.2-0.98 mmol \\ l
SV - The standard plasma bicarbonate is determined at CO2 40 MMRT ST, O2 100 mm RTSTT 37GS (21-25mm \\ L)
Avto True Blood Bicarbonate taken in a patient without contact with air at t 38GS. (18.5-26 mmol \\ l)
NVV The sum of all major patient buffer systems under standard conditions, pH urine indicator H \u003d reflects the functional state of the kidneys, the intensity of ammoniogenesis and acidogenesis.
Classification of braid disorders.
1 Acidosis and alkalosis.
Acidoc - when excess acid appears
Alkalosis excess grounds.
CBC violations can be respiratory (changes in the content of RSO2 and non-irispiratory (RN shift due to the change in the level of the NSO3, can be exogenous due to an increase in the receipt of non-volatile acids or bases from outside and endogenous - with a violation of the exchange of NSO3 and chlorine between the EXC and AUC. And excretory - When the delay or in the excess of the removal of acids and the bases are mainly through the kidneys.
Maybe acidosis, alkalosis and mixed forms of disorders:
1 primary respiratory acidosis, secondary irregular alkalosis,
Primary irregular acidosis, secondary respiratory alkalosis, - primary suspension alkalosis and secondary irregular alkalosis,
Secondary irregular alkalosis and secondary respiratory acidosis.
Respiratory is due to the accumulation of CO2 - Ventilation - waters of lungs. In this case, gas exchange between alveoli and blood or external environment is disturbed. (Central, lactatacidosis, respiratory center, chemoreceptors, restrictive, obstructive diseases, COPL, MIASTENIAHT. At COP COP2 reaches up to 100 mm Hg. Under acute hypercaping, the level of NSO3 increases by 1M \\ eq for every 10 ml of RT of the CO2. COPL 4 M \\ EQ per 10 mm RTCT. Respiratory acidosis is always accompanied by hypoxy. Hypercapnia leads to the oppression of the respiratory renal compensatory mechanisms9 Highlighting H + and the reabsorption of the NSO3 act slowly. Compensation mechanism. The increase in CO2 stimulates the pulmonary velocity, The identification of H \u003d and CL is rising. Under the action of carbicherrydases is formed by the NSO3. Decompensation occurs when the rate of increasing CO2 exceeds the formation of the NSO3.
Clinic - Against the background of hypercupinia Paralytic extension of the vessels of the brain, intracranial hypertension, the products of the liquor increases, compensatory hyperkathecholamine comaments comes compensate, the heart activity of tachycardia increases, the CV, IOC, UO increases. The tone of arterioles, hypertension, arrhythmias increases, against the background of CH progression, bradycardia hypotension. ETC.
Unpiratoric acidosis.
Protecting the inner medium due to non-volatile acids. RN decreases, BS concentration
Unpiratory metabolic acidosis - when many acidic products and kidneys cannot synthesize enough NSO3, the selection of H \u003d, the freedoms are depleted, reduced CO2.
Irregular acidosis can be
Ketoneacidozorates many ketone bodies with the complication of SD, alcohol abuse, long starvation,
Acidosis milk acids when lactate is formed, with a decrease in the delivery of O2 tissues,
Heating with organic acids ethylene glycol, salicylates, methanol.
The irregular excitatory acidosis is the loss of the alkali of pancreatic juice, intestinal, with the OPN.
Canaltage proximal acidosis is isolated when the NSO3 reabsorption and distal tubular acidosis are reduced when the secretion of H + is reduced and the decrease in the formation of a new NSO3
Hypercalem sewage acidosis
Renspiratory with excessive reduction of SO2 and hyperventilation develops. Below 34 The decrease in the content of H2 CO3 is accompanied by a decrease in the NSO3 at the same time the acidity of urine decreases and the content in it is NN4 CL
Hypochemium to height, diseases of light anemia, injuries, damage to the central nervous system, psychogenic hyperventilation, fever, etc. Dyspnea, with gas alcohol, hypocrisy causes a decrease in the excitability of the respiratory center up to the appearance of periodic respiration. At the same time, hypoxia arises, the breathing center is deproed to reduce the garden, decreases the UO, IOC and tissue blood flow at the same time, metabolic acidosis is joined due to the intensive removal of potassium and sodium, osmotic blood pressure drops, the diuresis increases with the dehydration of the body of hypochalemia leads to muscle adamas heart Rhythm, hypocalcemia leads to convulsive syndrome.. The gas compensation is aimed at a bicarbonate in the blood plasma, which belongs to the kidney in this, which intensively distinguish the bicarbonates and reduce the release of H \u003d from the erythrocytes. Chlorine ions displaces sodium ions from Nacano3, form H2 CO3 and restores the ratio of bicarbonate buffer and braid.
Renal compensation in respiratory alkalosis develops slowly.
Clinic decreased tissue blood flow, microcirculation disruption, decreased tissue metabolism, CNS disorder, hypocalcemia, convulsions. . Unregulated alkalosis when there is little in blood n \u003d. , raising pH, buffer grounds.
Unpiratory excretory alkalosis, loss of a large number of acidic components, the loss of H, Cl, the introduction of uncontrolled alkaline solutions, while the amount of NSO3, hypercupnia, respiratory thawing increases
Causes of kidney functions, indomitable vomiting, liver failure, the splitting of the aldesterone is disturbed, (sodium reabsorption is broken, hyperproduction of glucocorticoids - tumors of adrenal cortex, all this leads to hypoventilation. Potassium rushes into a cage, intracellular acidosis develops
The analysis on blood gases is very important. According to it, it is possible to determine the saturation of the human body by air, which helps to determine the effectiveness of the therapeutic treatment course, as well as diagnose patient respiratory failure and primary hyperventilation. The main indicators are the level of oxygen and carbon dioxide. The determination of the gas composition of blood can help in the diagnosis of a number of other diseases.
Basic concepts
In order to decipher the analysis of the gases of arterial blood, we try to explain the basic concepts without going into extra details. O 2 (oxygen) in human organism Used by cells in order to generate energy and produce in waste CO 2 (carbon dioxide). With the help of blood cells are supplied with oxygen and exempted from carbon dioxide.
The concept of gas exchange in the lungs means a process in which oxygen is transferred to blood from the atmosphere, and carbon dioxide is removed from it into the air. Based on the analysis of blood gases, it is possible to find out how the gas exchange is effective. The result shows the quantity of partial pressure O 2 and CO 2. Under partial pressure it is understood as the proportion of separate gas in general pressure. The amount of dissolved gas in arterial blood flow depends on what partial pressure. Gas moves from the site where partial pressure is high in a place with low partial pressure. In the blood, the partial level of carbon dioxide pressure (PCO 2) is higher, and the partial level of oxygen pressure (PO 2) is lower than in the air. This explains why O 2 of the alveoli passes into the blood, and CO 2 of the blood in the alveoli, until the partial pressure becomes equal.
Air consists of approximately 78 percent of nitrogen, 21 percent of oxygen and a small percentage of carbon dioxide. Inside the lung pressure due to humidification of air decreases. Gases in the blood contain a large amount of CO 2. The removal rate of carbon dioxide is interconnected with alveolar ventilation.
In pathologies, for example, pulmonary diseases, blood, passing through the capillaries of the patients with alveoli, is returned to artery with a lower content of O 2 and large CO 2 than it is supposed to normally.
Such blood is called shunting. The remaining healthy alveoli enhance exchange Process Air based on hyperventilation. As a result of this, the plasma through healthy alveoli is given to more CO 2, thus the normalization of the partial pressure of carbon dioxide gas (PCO 2) in the bloodstream of the arteries occurs.
The shunt plasma, on the contrary, contains a low amount of O 2. The plasma flowing through healthy alveoli is not able to carry more than O 2, so the partial pressure of O 2 in the bloodstream arteries decreases. Deciphering analyzing indicators will show this process in deviations from normal indicators.
The table shows the gas composition of the blood:
About indicators
The normal results of blood gases are given in the table:
On these four main parameters together with clinical picture You can define development dangerous disease In a patient who requires rapid decision-making.
If the norm is broken in blood tests for gases, then the following table shows how the human body will respond to it:
| Indicators | number | Arriving pathology |
| pH | Less 7.35 | Indicates a surplus of carbon dioxide |
| More than 7.45 | Indicates a surcharge of alkalis. | |
| PO2 (partial oxygen pressure level) | Fall below normal indicators | Hypoxia develops in the body, the support of the balance with carbon dioxide is violated. |
| PCO2 (partial level of carbon dioxide pressure) | Less than 35. | Hyperventilation is broken, in the body there is a lack of carbon dioxide |
| More than 45. | In the body there is an excess of carbon dioxide, which is expressed in reducing heart cuts, the patient has a sense of anxiety. | |
| Bicarbonate | Less than 24. | May be evidence of kidney disease, metabolic acidosisDehydration of the body. |
| More than 26. | It is observed in overdose of steroid substances, metabolic alkalosis, hyperventilation. |
The studies made will help the doctor in the accuracy of the diagnosis and appointment of an effective course of treatment.