Celiac disease (celiac disease): causes, symptoms, treatment. Enteropathy Tests after diagnosis
Clinical symptoms of various chronic diseases small intestine have much in common, which often leads to an erroneous interpretation of their etiology. Chronic recurrent diarrhea in combination with malabsorption syndrome and metabolic disorders of varying severity are the most typical clinical manifestations in diseases of the small intestine different etiology... The main pathophysiological factors of chronic diarrhea are intestinal hypersecretion, an increase in osmotic pressure in the intestinal cavity, intestinal hyperexudation (exudative enteropathy), and accelerated transit of intestinal contents.
Intestinal hypersecretion is provoked by bacterial toxins, deconjugated bile acids, inflammatory mediators, which cause damage to the protective parietal mucous barrier of the small intestine, enterocyte membranes with the formation of inflammatory mediators and neuropeptides. Toxins and these stimuli are perceived specific receptors on the membranes of enterocytes and activate the synthesis of cyclic AMP inside the cell from ATP. This promotes a selective increase in the permeability of enterocyte membranes for water, chloride and sodium ions into the intestinal lumen, i.e. secretion, while inhibiting the absorption of sodium ions.
An increase in osmotic pressure in the intestinal cavity (osmotic diarrhea) is observed in congenital fermentopathies (lactase deficiency, celiac disease), when taking osmotic drugs (magnesia, sorbitol, lactulose), operated stomach, short bowel syndrome, exocrine pancreatic insufficiency.
Lactase deficiency is the most common form of interstitial fermentopathy. The presence in the lumen of the intestine of unsplit, nonabsorbable milk sugar causes the flow of interstitial fluid from the walls of the intestine into its lumen along the gradient of osmotic pressure, increasing the volume of intestinal contents and accelerating its passage of osmotic diarrhea. In the large intestine, bacterial degradation of undigested glucose occurs to water and organic acids (lactic, acetic, etc.), which also stimulate the mechanoreceptors of the mucous membrane, accelerating peristalsis. At the same time, acidification of intestinal contents is noted (pH 4.54.0). Undigested nutrients in the intestinal lumen contribute to the reproduction of opportunistic microflora, dysbiosis develops, causing deconjugation of bile acids, an increase in the permeability of the protective mucous barrier and damage to the epithelium of the intestinal mucosa due to exposure to bacterial toxins. Penetrating through damaged lipoproteins of the intercellular membranes of enterocytes, macromolecules of uncleaved proteins and sugars cause allergic reactions and food intolerance, which occurs in 530 patients of this profile (A.M. Nogaller, 1994; V.K. Mazo, 1997). Connection atopic dermatitis with an allergic reaction deserves serious attention to determining the etiology of impaired intestinal functions, taking into account the food history.
Intestinal hyperexudation exudative enteropathy can be primary (idiopathic) and secondary, which is a consequence of changes in intestinal permeability in other enteropathies (Menetrie's disease, spruceliakia, Crohn's disease, tuberculosis, Whipple's disease, radiation enteritis, intestinal lymphoma, carcinoma and abdominal lymphoma). ... The pathogenetic basis is the increased permeability of the intestinal mucosa with an increased supply of plasma proteins (albumin, g-globulin) to its lumen through ectazed intestinal lymphatic vessels and their enhanced catabolism.
Motor functional diarrhea is characteristic of irritable bowel syndrome (IBS), thyrotoxicosis, collagenosis. The most common form of functional IBS diarrhea occurs with impaired functions of the small and large intestine (motility, secretion, sensitivity), which is due to a change in the balance and interaction of neurotransmitters and hormones (serotonin, motilin, enkephalins, neurotensin, cholecystokinin, somatomedin, etc.), characteristic of brain and nerve plexuses intestine axis: cerebro-intestinal-brain (A.M. Ugolev, 1972, 1995; Grossman, 1982; J. Fioramonti, 1997).
Often, several pathophysiological mechanisms of secretory, exudative, motor are involved in the complex pathogenesis of enteritis, which is characteristic of terminal ileitis (Crohn's disease), ethanol and iatrogenic (medicinal) enteritis after administration antibacterial drugs, non-steroidal anti-inflammatory and laxatives, radiation damage. Effects antibacterial therapy are manifested by dysbiosis of varying severity, secretory diarrhea. Taking broad-spectrum antibiotics (kanamycin, lincomycin, neomycin, rifampicin) causes the eradication of normal intestinal microflora and promotes overgrowth of clostridia that produce enterotoxins A and B, which cause swelling of the intestinal mucosa and ulceration; pseudomembranous enterocolitis with severe bleeding: diarrhea, sometimes intoxication, high fever, leukocytosis. The use of clindamycin is the main risk factor for the development of this pathology in debilitated patients. This is why this drug should only be used to treat serious infections.
NSAIDs (indomethacin, brufen, acetylsalicylic acid) suppress the activity of cyclooxygenase (COX1) and inhibit the synthesis of prostaglandins, which affects the composition of intestinal parietal mucus, reduces its protective properties, contributing to protein loss, ulceration, perforation, bleeding.
It should be borne in mind that long-term use of laxatives from the group of anthraglycosides (senna, buckthorn bark, rhubarb, aloe) and diphenolic laxatives (bisacodyl, oxyphenisatin) damage the intercellular connections and cell membranes, increase the permeability of the mucous membrane, desquamation of the epithelium. With prolonged use of laxatives, drug diarrhea with dehydration, hypokalemia, sodium loss, and malabsorption syndrome is observed. Among the side effects, irreversible changes in the intestinal mucosa, cancer of its various departments are described.
In recent years, intestinal tuberculosis is not a rare diagnosis in chronic diarrhea. The most common localization is the terminal section of the small intestine. The differential diagnosis is carried out between Crohn's disease, bowel tumor and tuberculosis according to the histological examination of a biopsy sample from the affected area. Identification of epithelioid granulomas with Pirogov-Langhansa cells confirms the diagnosis of intestinal tuberculosis.
Radiation enteritis is manifested not only by dysbiosis. Radiation exposure induces chromosomal damage to the DNA of enterocytes, increases apoptosis, edema of the mucous membrane, an increase in its permeability, exudation of plasma proteins into the intestinal lumen.
In ischemic enteritis (atherosclerosis of the superior mesenteric artery, systemic vasculitis), a violation of mesenteric blood flow causes hypoxia of the intestinal wall, inhibition of the synthesis and activity of enzymes synthesized by enterocytes (disaccharidase, alkaline phosphatase, etc.), which causes malabsorption syndrome.
More rare forms of enteropathy are caused by variable immunodeficiency, Whipple's disease, lymphoproliferative diseases, carcinoid syndrome, hepatoma, HIV infection.
With a variety of etiological factors of chronic enteropathies, there is a general pattern in the development of diarrheal syndrome, loss of fluid and electrolytes, disruption of the structure and function of the mucous barrier of the small intestine, and a decrease in its cytoprotective properties. However, given the complexity of the pathophysiological mechanisms of chronic diarrhea, the determination of its etiology is a prerequisite for the appointment of rational therapy. It should be emphasized that the term "chronic enteritis" without indicating the etiology of the disease and confirmed morphological signs of the inflammatory process in the intestinal mucosa is not a full-fledged diagnosis, i.e. a nosological concept (A.L. Aruin, 1994), and is not used in the WHO nomenclature (ICD 10), in foreign literature and in clinics for more than 20 years.
However, the incomplete bacteriological analysis of the "disgroup" widespread in general medical practice without determining Yersinia, Campylobacter, Klebsiella and other rarer microorganisms, due to its truncation, is not highly informative and therefore does not allow a significant category of patients to reliably exclude the bacterial etiology of enteritis. However, in this situation, only antibiotic therapy can provide an antiseptic effect. In addition, in the therapeutic aspect, serious problems arise due to the fact that in recent years a change in the pathogenicity and sensitivity to antibiotics of "wild" pathogens of mutant strains has been established, in contrast to the previously known ones, i.e. "Collection" strains. The frequent occurrence of resistant, including multidrug-resistant, forms of intestinal infections led to a change clinical symptoms these diseases, which also complicates the diagnosis. These mutants show resistance to standard antibacterial therapy, for example, to penicillins, tetracycline, cephalosporins, sulfamides, due to the production of exoenzyme b-lactamases by them, which destroys the b-lactam ring of penicillins and cephalosporins. That is why the use of new antiseptics Intetrix, nifuroxazide with a minimum bactericidal concentration and a wide range antibacterial action against causative agents of gastrointestinal diseases, including mutant strains, is very relevant both in acute and chronic bacterial diarrhea. A valuable property of Intetrix with good tolerance is the preservation of the balance of the saprophytic flora of the host and the restoration of eubiosis.
Medicinal enteritis is stopped by the exclusion of provoking drugs. With pseudomembranous enterocolitis, it is recommended to discontinue clindamycin (lincomycin, neomycin, rifampicin) and administer oral vancomycin at a dose of 125,500 mg 4 times a day for 1014 days and metronidazole 250 mg 3 times a day for 1014 days, followed by taking probiotics.
In the treatment of ischemic enteritis, the main role is played by angioprotectors and antiplatelet agents. The effectiveness of treatment for Whipple's disease is achieved long-term use antibacterial drugs: cotrimoxizole 480 mg 2 times a day (12 months), tetracycline 2 g per day for 612 months. Treatment can last up to two years. In carcinoid syndrome, regression of severe clinical manifestations(persistent diarrhea, temperature rises) is observed after prolonged therapy with sandostatin.
Therapeutic tactics provides for a combination of etiotropic therapy with pathogenetic. So, with chronic diarrhea, additional astringents, sorbents are prescribed: Smecta, bismuth preparations. Smecta increases the thickness of the mucin layer of the intestine, adsorbs viruses, bacterial toxins, intestinal gases and bile acids, protecting the mucous membrane, restores normal microflora intestines, reduces the secretion of electrolytes, water, normalizes motor skills, eliminates flatulence. The protective properties of Smecta against various aggressors make it the drug of choice for chronic diarrhea.
According to indications, metabolic disorders are corrected by parenteral administration of electrolyte mixtures, protein preparations, fat-soluble vitamins A, D, K, calcium preparations. Deficiency of intestinal enzymes (dipeptidases, disaccharidases) due to inflammation and destruction of the intestinal mucosa is advisable to compensate for the appointment of pancreatic enzymes. To restore the intestinal microecological system, its stability, probiotics are prescribed. Their sanitizing effect is due to the production of antibacterial metabolites that inhibit the growth of potentially pathogenic microbes and a high adhesion ability to adhere to the mucosal layer, to the intestinal epithelium. This increases the colonization anti-infectious resistance of the intestinal barrier, which stimulates the lymphoid apparatus, enough level secretory Ig A.
Enteropathy is a collective concept that implies the development of a chronic pathological process of non-inflammatory genesis. As a rule, the development of such a disease in adults or in children is due to a violation or complete absence of the production of certain enzymes that are involved in the absorption and processing of nutrients.
Intestinal enteropathy can be both congenital (primary) and acquired (secondary) forms. In both the first and second cases, the progression of such a disease leads to the development of an inflammatory process. The next stage will be erosion and atrophy of the mucous membrane with all accompanying complications.
The clinical picture is characterized by dysfunction of the stomach: nausea and vomiting, diarrhea, rumbling in the abdomen, increased gas production.
Diagnosis is based on physical examination, laboratory and instrumental methods survey. Treatment is aimed at eliminating the underlying factor. Symptomatic and etiotropic therapy is also used.
The prognosis will vary depending on the cause of the development of the pathological process, as well as on the clinical and morphological picture of the disease. Lack of treatment can lead to serious complications, including T-cell lymphoma.
Etiology
Protein-losing enteropathy, like any other form, can be caused by the following etiological factors:
- infection with pathogenic organisms;
- intolerance to gluten and other substances;
- excessive or prolonged use of medications;
- toxic and radiation effects on the body;
- pathology of the lymphatic and hematopoietic system;
- malfunctions endocrine system;
- kidney disease;
- weak immune system;
- pathology connective tissue;
- chronic gastroenterological diseases with frequent relapses;
- a genetically determined violation of the production of enzymes;
- allergic reactions to certain substances, including the food form.
It should be noted that allergic enteropathy in a child is most often genetically determined and is congenital.
Classification
The classification of this pathological process implies its division into types according to the clinical and morphological picture, as well as the nature of the course.
According to the clinical and morphological picture, the following types of this disease are distinguished:
- allergic enteropathy - occurs as a result of an allergic reaction to food, almost any product, both daily and exotic, can act as an allergen;
- autoimmune enteropathy - a specific dysfunction that is associated with lymphoid tissue, is more often diagnosed in males, genetically determined;
- exudative enteropathy - in this case, there is a loss of plasma proteins through the gastrointestinal tract;
- diabetic enteropathy - dysfunction gastrointestinal tract on the background heavy course ;
- mucoid enteropathy is an insufficiently studied form of the disease, which is diagnosed only in animals, and most often in rabbits;
- necrotizing enteropathy - characterized by ulcerative-necrotic lesions of the intestinal mucosa, characterized by extremely unfavorable prognosis, this form of the pathological process includes cytostatic disease in its clinical picture;
- HIV enteropathy - this form develops against the background of too weakened immune system.
Allergic enteropathy, in turn, is classified according to the mechanism of development:
- the allergen passes through the intestinal wall and enters the bloodstream;
- antigen interacts with antibodies that are located in the submucosa of the intestine;
- violation of the integrity of the vascular and intestinal wall;
- granulomatous inflammation of the intestinal wall.
By the nature of the flow, such forms are distinguished as:
- sharp;
- chronic enteropathy.
It is possible to determine exactly what form of the pathological process takes place only with the help of diagnostics - laboratory and instrumental.
Symptoms
The main clinical sign of this disease is frequent diarrhea: attacks can be up to 10-15 times a day. The feces are liquid, foamy in nature.
In addition, the following symptoms are present:
- decreased or complete lack of appetite;
- nausea and vomiting;
- temperature increase;
- pain in the epigastric region, which are expressed, are spastic in nature, and are similar in type of manifestation;
- dizziness;
- general weakness, growing malaise.
With an allergic form, the clinical picture is supplemented by the following signs:
- increased lacrimation;
- swelling of the mucous membrane, oral cavity, organs of the respiratory system;
- regurgitation in babies;
- blood in feces Oh.
Against the background of such a clinical picture, a person has a decrease in body weight, pains in the navel area may periodically appear.
In view of the fact that similar symptoms can occur in many gastroenterological diseases, self-medication is strongly discouraged. You need to see a doctor.
Diagnostics
First of all, the gastroenterologist conducts a physical examination, during which he finds out the following:
- when the first symptoms began to appear, the nature of their manifestation;
- whether there are chronic diseases of the gastrointestinal tract or any other type;
- whether the patient is currently taking any medications, whether he is following diets;
- diet.
Further diagnosis may include the following activities:
- general and biochemical analysis blood - there is a decrease in the level of hemoglobin, an acceleration of ESR, an increase in C-reactive protein;
- analysis of feces;
- radiography small intestine with passage of barium;
- endoscopy;
- MSCT organs abdominal cavity;
- gliadin samples;
- biopsy of the mucous membrane of the small intestine;
- test for antibodies to red blood cells.
It is necessary to differentiate the pathological process with respect to the following diseases:
Based on the results diagnostic activities, the doctor determines the form and severity of the course of the disease and prescribes the treatment of enteropathy.
Treatment
In this case, symptomatic, specific and etiotropic therapy is used. Without fail, a diet is prescribed, nutrition according to which implies the exclusion of trigger foods.
The pharmacological part of the treatment is selected by the doctor individually, depending on the form of the disease.
The following drugs may be prescribed:
- non-steroidal anti-inflammatory;
- antihistamines;
- antibiotics;
- glucocorticoids;
- immunosuppressants;
- aminosalicylates;
- iron and calcium preparations;
- the introduction of albumin;
- vitamin and mineral complexes.
As for the diet, it must be observed constantly, since the use of products that are provocateurs of the development of the pathological process can lead to a relapse in an even more severe form.
Prophylaxis
Prevention of enteropathy is based on simple measures:
- compliance with the regime proper nutrition, rational diet (if necessary);
- competent treatment of diseases of the small intestine;
- strengthening the immune system, which is especially important in cases of similar incurable diseases;
- exclude smoking, drinking in large quantities,.
Periodically, it is necessary to undergo a medical examination, especially if there is a gastroenterological disease of a chronic nature in a personal history. Self-medication is unacceptable, since exudative enteropathy and any other form of this disease can only lead to an aggravation of the pathological process.
Is everything in the article correct from a medical point of view?
Only answer if you have proven medical knowledge
Diseases with similar symptoms:
Inflammation of the lungs (officially pneumonia) is inflammatory process in one or both respiratory organs, which is usually infectious in nature and is caused by various viruses, bacteria and fungi. In ancient times, this disease was considered one of the most dangerous, and although modern means of treatment allow you to quickly and without consequences get rid of the infection, the disease has not lost its relevance. According to official data, in our country every year about a million people suffer from pneumonia in one form or another.
Intestinal enteropathy is the general name for non-inflammatory chronic intestinal diseases, which are based on fermentopathy or congenital anomalies in the structure of the intestinal wall. Gluten enteropathy (European sprue, non-tropical sprue, adult celiac disease, idiopathic steatorrhea) is a rare hereditary disease (fermentopathy) of the intestine, characterized by the absence or decreased production of the intestinal wall of enzymes that break down gluten (gluten) - a polypeptide found in some cereals, wheat, barley, oats). The absence (or relative insufficiency) of the production of this peptidase is especially manifested in case of nutritional disorders, the predominance of cereals containing gluten in food, with intestinal infections... Products of incomplete digestion of gluten (gliadin, etc.) are toxic to the intestinal wall.Diarrhea is common when you eat foods made from wheat, rye and barley. With the progression of the disease, polyhypovitaminosis, disorders electrolyte balance, exhaustion. In advanced cases, chronic enteritis with malabsorption syndrome develops. Known assistance in differential diagnosis tests with a load of gliadin (a rapid increase in the level of glutamine in the blood after oral administration gliadin at a dose of 350 mg / kg), the presence of signs of the disease from early childhood, exacerbation of the symptoms of the disease with a significant addition to the diet of products from wheat, rye, barley, oats, as well as the reverse development of the symptoms of the disease when the patient is transferred to a gluten-free diet (gluten is absent in all animal products, in corn, rice, soybeans, potatoes, vegetables, fruits, berries and other foods).
Treatment in severe cases of the disease is carried out in a hospital. The patient is transferred to a completely gluten-free diet with a high content of vitamins, enveloping and astringent affinities are prescribed orally. As the condition improves, the diet is expanded, but the content of gluten-containing foods in the daily diet is left limited. Disaccharidase deficiency enteropathies are hereditary diseases caused by the absence or insufficient production of disaccharidases (lactase, maltase, invertase, etc.) by the mucous membrane of the small intestine.
), as a result of which the parietal hydrolysis in the intestine of the corresponding disacrose-lactose, maltose, sucrose is disrupted. The type of inheritance is not exactly established. Clinically, there is intolerance to one (or several) disaccharides and an increase in fermentation processes when they are taken in normal and especially in high doses; there are symptoms of fermentation dyspepsia, rumbling in the abdomen, flatulence, diarrhea, polyfecal matter with an acidic reaction of feces. Diagnosis and differential diagnosis with others chronic diseases small intestine are based on a number of specific tests: 1) improvement of the clinical picture of the disease after exclusion of the corresponding disaccharides from the diet; 2) the study of glycemic curves after ingestion of various disaccharides-sucrose, lactose, maltose by the patient (the absence of an increase in blood sugar after taking one of the disaccharides and its increase after taking monosaccharides that make up their composition is a sign of a violation of the cleavage of this disaccharide).
Congenital disaccharide intolerance usually manifests itself from childhood. However, the violation of enzyme production can be acquired as a result of severe enteritis. In the latter case, impaired production of disaccharidases is usually combined with impaired production of intestinal epithelium and other enzymes. The course in most cases is not severe, but over time, with a high content of sugary substances in the diet and other unfavorable conditions, as a result of prolonged secondary irritation of the intestinal mucosa by products of increased fermentation, chronic enteritis, accompanied by a syndrome of insufficient absorption, can develop.
Treatment. Strict adherence to the diet with the exclusion of the corresponding disaccharide from the diet (or a sharp restriction of the content); in more severe cases, the appointment of enzyme replacement therapy. Exudative enteropathy (exudative hypoproteinemic lymphangiectasia) is a rare disease that occurs mainly in young people. The etiology and pathogenesis have not been clarified.
It is characterized by pathological expansion of lymphatic vessels and increased permeability of the intestinal wall, diarrhea, significant loss of protein through the gastrointestinal tract, hypoproteinemic edema. In severe cases, general exhaustion develops. Hypochromic anemia, minor leukocytosis with a tendency to lymphopenia are not uncommon. Hypoproteinemia is observed mainly due to a decrease in the content of albumin and gamma-tobulins; hypocholesterolemia; hypocalcemia.
Stool has an increased content of neutral fat, fatty acids and soaps. Special laboratory research methods detect increased content protein in the small intestinal secretion and its increased excretion with feces. A radioisotope study of the excretory function of the small intestine makes it possible to determine an increase in the radioactivity of feces and rapid decline blood radioactivity after intravenous administration serum albumin labeled with 1131 or 51Cr, i.e.
Confirms increased loss of protein from the body through the intestines. In biopsies from the intestinal mucosa, there is an expansion of the lymphatic vessels, inflammatory tissue infiltration. In dilated lymphatic vessels and mesenteric sinuses lymph nodes- lipophages containing microdroplets of fat in the protoplasm. Differential diagnosis is carried out with enteritis, enterocolitis, as well as non-inflammatory disaccharidase deficiency enteropathies, sprue, celiac disease.
Enterobiopsy allows to reliably establish the diagnosis of exudative enteropathy. The disease is chronic and slowly progresses. Patients are prone to intercurrent infections (pneumonia, purulent infections, tonsillitis, etc.)
), which can cause their death. In severe cases, the prognosis is poor. Treatment during an exacerbation is carried out in a hospital. Prescribe a diet with a high content of protein, vitamins, fluid restriction and table salt.
Plasma is transfused intravenously. Vitamins are administered, with hypocalcemia - calcium preparations. With edema, diuretics are prescribed simultaneously with transfusions of plasma and various protein preparations.
Attention! The described treatment does not guarantee a positive result. For more reliable information, ALWAYS consult a specialist.

Is an inflammatory disease of the small intestine of an allergic nature, which occurs when antigens enter the body, causing an excessive, increased response of the immune system. Most often, the disease develops in children early age... Allergic enteropathy is manifested by diarrhea, bloating, intestinal colic, regurgitation, and insufficient weight gain. Diagnostics includes examination by a pediatrician and an allergist-immunologist, laboratory tests and allergological tests, and intestinal examination. Treatment consists in stopping contact with the allergen, prescribing a hypoallergenic diet, antihistamines.

Allergic enteropathy (gastrointestinal form of food allergy) - damage to the mucous membrane of the small intestine when allergens enter the gastrointestinal tract. Most often, the disease occurs in young children and is associated with the appearance of hypersensitivity to proteins in cow's milk, soy and other products used in the introduction of complementary foods and the transition from breastfeeding to artificial.
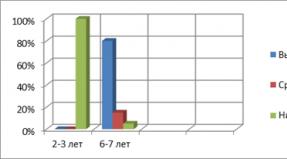
The prevalence of food allergies among children under the age of 3 years is about 6-8%, at 10-15 years old - 3-4%. At the same time, hypersensitivity to cow's milk protein was found in 2-2.5% of young children, to chicken protein - in 1-1.5%. As a rule, along with allergic enteropathy in children, there are signs of allergic damage to other organs and systems (skin, respiratory tract and etc.).
Causes of allergic enteropathy
More than 170 products are known that, upon penetration into the gastrointestinal tract, can cause the appearance of a gastrointestinal form of food allergy (allergic enteropathy), and their allergic activity is due to the presence of animal or plant proteins, glycoproteins, less often polypeptides.
In children under the age of one year, allergic enteropathy in most cases is caused by increased sensitivity to cow's milk protein, which contains more than ten antigens, of which αS1-casein and γ-casein have the greatest activity. In children school age and adults, the development of allergic reactions with intestinal damage is more common with protein intake chicken eggs, fish and seafood. The immune system often reacts to the dietary fiber of plant origin entering the body: wheat, rye, oatmeal, buckwheat and rice groats, soybeans, as well as some vegetables (carrots, celery, tomatoes) and fruits (bananas, citrus fruits).
In the development of food allergy in children and adults, the essential role of hereditary predisposition is undoubted. This is evidenced by the presence of allergic diseases in the patient's relatives, as well as common manifestations of allergies with lesions of the skin, bronchopulmonary system, which are common in the patient, and the identification of hypersensitivity not only to food products, but also to plant pollen, house dust, medicines and other allergens.
In the occurrence of allergic enteropathy, a decrease in the barrier function of the gastrointestinal tract (due to enzymatic insufficiency) and a violation of IgA production play a role. Allergic reactions that develop during the penetration of food antigens into the gastrointestinal tract can be IgE-mediated, non-IgE-mediated, immunocomplex and cell-mediated. Allergic intestinal lesions are characterized by non-IgE-mediated (with proctocolitis) and cell-mediated (with allergic enteropathy) reactions.
Symptoms of allergic enteropathy
Allergic enteropathy manifests itself as local characteristics lesions of the gastrointestinal tract (vomiting, intestinal colic, diarrhea), and various extraintestinal manifestations of allergies (atopic dermatitis, eczema, bronchial asthma). The severity of the manifestation of certain clinical symptoms of the disease will differ depending on the age of the patient.
In young children, allergic intestinal lesions are manifested by cramping abdominal pains like intestinal colic, regurgitation and vomiting, bloating, loose stools 5-6 times a day. Sometimes intestinal bleeding may occur with discoloration of the stool. Violated general state child: there is anxiety, general weakness, pallor of the skin, sleep disorder, appetite, hypotrophy. Often, allergic enteropathy at this age is accompanied by skin manifestations of the type of atopic dermatitis (dry damaged skin, polymorphic rash).
Timely elimination of the allergen from the diet leads to the cessation of symptoms in 2-3 days. If an allergic lesion of the gastrointestinal tract is caused by an increased sensitivity to casein in cow's milk, the manifestations of enteropathy usually disappear by 2-3 years of age, even with regular consumption of dairy products.
In schoolchildren, adolescents and adults, the picture of the disease becomes more erased and is more often characterized by dull pain in the navel, flatulence, unstable stools (constipation or diarrhea), decreased appetite, and nausea. Extraintestinal manifestations of allergies are rare. At the same time, allergens that cause allergic enteropathy at this age can sometimes be not only food, but also medications, plant pollen, household dust, etc.
Diagnostics of the allergic enteropathy
The clinical manifestations of allergic enteropathy are nonspecific and occur in gastroenteritis and enterocolitis of various etiologies (including those caused by infectious agents viral and bacterial nature, helminths, protozoa, alimentary factors, chemical poisoning, inedible and poisonous products). To establish the correct diagnosis, it is necessary to carefully collect an allergic history, conduct a clinical examination of the patient (consultation with a gastroenterologist, an allergist-immunologist), perform the necessary laboratory and instrumental studies.
Analysis of the allergic history reveals the presence of hereditary burden ( allergic diseases from relatives). As a rule, a sick child was observed earlier or was present at the time of examination of skin or respiratory symptoms allergies. The appearance of clinical signs of allergic enteropathy (abdominal pain, vomiting, diarrhea) is associated with the ingestion of a food allergen (cow's milk, eggs, fish, peanuts, etc.). The condition improves significantly after eliminating the problem food from the diet.
In laboratory research in general analysis eosinophilia (an increase in the number of eosinophils) is detected in the blood. Stool analysis (coprogram) reveals an increased content of erythrocytes, eosinophils, neutrophils. Histological examination of biopsies of the mucous membrane of the small intestine reveals signs of inflammation (edema and hemorrhage), infiltration of the lamina propria with lymphocytes, mast and plasma cells. In some cases, it is revealed partial atrophy villi. When conducting a specific allergological study, the content of total IgE, as well as specific IgE and IgG is determined, skin allergy tests with a set of food allergens are used,
Differential diagnosis in allergic enteropathy is carried out, first of all, with celiac enteropathy, in which there are no extraintestinal manifestations of allergy, antigliadin IgA antibodies and antibodies to transglutaminase are found.
Allergic enteropathy treatment
Therapeutic measures for allergic enteropathy include the elimination of the allergen and the appointment of a hypoallergenic diet, the use of antihistamines and anti-inflammatory drugs, enterosorbents, enzymes and membrane stabilizers, symptomatic treatment of individual manifestations of the disease.
If breastfeeding is carried out, it is necessary to formulate a strict hypoallergenic diet for the mother, excluding potential food allergens and individually intolerable foods. Children who are bottle-fed are prescribed special therapeutic mixtures with whey and casein protein hydrolysates, as well as mixtures based on goat's milk. The timing of the introduction of complementary foods for children with allergic enteropathy is postponed to 5-6 months of life, while hypoallergenic cereals (buckwheat, rice, corn), one-part vegetable purees, meat (veal, horse meat, pork, rabbit, turkey) are used. Cow's milk, cottage cheese, fish and eggs are completely abandoned in the first year of life, peanuts are excluded for up to three years. Older children and adults follow an individually tailored hypoallergenic diet for at least six months.
From antihistamines in the first year of life, the use of dimetindene (in drops), chloropyramine (in tablets), cetirizine (in drops), and ketotifen is recommended. From one year old you can use loratadine, and from six years old - fexofenadine hydrochloride and ebastine. Enterosorbents are usually applied within one to two weeks during an exacerbation. According to indications, enzymes (pancreatin), preparations containing bifidobacteria and lactobacilli are prescribed, symptomatic remedies(defoamers, antiemetics).
Prevention of allergic enteropathy consists in the observance of a hypoallergenic diet by a pregnant and lactating mother, breastfeeding up to 4-6 months of life, the introduction of complementary foods to the child no earlier than the fourth month of life, the exclusion of potential allergens from the diet at an older age and in adults.
Celiac disease (celiac disease) is a disease of the small intestine that causes mucosal atrophy in response to gluten administration. The prevalence of celiac disease varies greatly across geographic areas. The disease occurs with the greatest frequency in European countries (1-3: 1000), with a lesser frequency in African countries. It is believed that at least 1% of the world's population suffers from this disease. Glutenic enteropathy is more common among women.
The defeat of the small intestine in celiac disease occurs under the influence of gluten, a protein found in cereals. Gluten consists of several components: prolamine, glutenin, albumin, globulin. Prolamine has a striking effect on the intestinal mucosa. Its amount in different cereals is not the same. So, millet, rye, wheat contain this protein in large quantities. In smaller amounts, prolamine is found in barley, oats, corn. Prolamine is heterogeneous in structure, wheat prolamin is called gliadin, barley prolamin is called hordein, and oat prolamin is called avein.

A key factor in the development of the disease is genetic predisposition. In people with this trait, when gluten comes into contact with the intestinal villi, specific antibodies are produced. This is how autoimmune inflammation of the intestinal tissues develops, leading to a gradual atrophy of the mucous membrane of the organ.
Atrophy of villi developing in celiac disease, dystrophic changes in enterocytes lead to a decrease in the absorption surface of the small intestine. As a result, the absorption of proteins, fats, carbohydrates, vitamins, and minerals is impaired. These changes lead to the appearance of characteristic clinical symptoms. Celiac disease can take three forms: classical, atypical, and latent. 
Glutenic enteropathy occurs mainly in childhood... Children are stunted, muscle weakness, apathy, an increase in the size of the abdomen, steatorrhea, and abdominal cramping are noted. Toddlers are emotionally labile and get tired quickly. But in some patients, the disease manifests itself not from childhood, but already in adulthood.
In general, the following symptoms are characteristic of classic celiac disease:
- Decrease in body weight (from 5 to 30 kg);
- Decreased appetite
- Weakness, fatigue;
- Stomach ache;
- Dyspeptic symptoms: flatulence, nausea,;
- Swelling;
- Glossitis;
- Iron deficiency;
- Hypocalcemia with osteoporosis;
- Hypovitaminosis.
 The most persistent symptom of celiac disease is recurrent diarrhea, which can be ten or more times a day. The stool is mushy, light, liquid, frothy.
The most persistent symptom of celiac disease is recurrent diarrhea, which can be ten or more times a day. The stool is mushy, light, liquid, frothy.
Constant, severe abdominal pain is not typical for celiac disease. However, people with celiac disease may experience cramping abdominal pain before or after a bowel movement. And with flatulence, there are dull, diffuse pains.
When examining a person with celiac disease, attention is drawn to an increase in the abdomen.
Symptoms of atypical celiac disease
In most cases, celiac disease is atypical. V clinical picture diseases may be absent or mild gastroenterological symptoms. Extraintestinal symptoms come to the fore:
- Anemia;
- Ulcerative stomatitis;
- , frequent fractures;
- Dermatitis herpetiformis (characterized by itchy papulo-vesicular rashes on the elbows and buttocks);
- Hemorrhagic syndrome;
- Associates autoimmune diseases (autoimmune thyroiditis, diabetes, Addison's disease);
- Defeat nervous system(, ataxia, epilepsy, polyneuropathy);
- Deterioration of potency, menstrual irregularities,.

If celiac disease is left untreated, complications of the disease can occur. The most common complications include:
- Malignancy;
- Chronic non-granulomatous ulcerative jejunoileitis and colitis;
- Neuropathy.
In patients with celiac disease and develop much more often than in the population. In addition, cancer of the esophagus, stomach, and rectum is also more common. An unreasonable deterioration in the patient's condition, as well as laboratory parameters, despite adherence to a gluten-free diet, should give rise to the idea of the likely development of a malignant process.

Chronic nongranulomatous ulcerative jejunoileitis and colitis is characterized by the appearance of ulcerative defects on the mucous membrane of the jejunum, ileum, and colon. Ulcers may bleed, perforate.
Neuropathy manifests itself in the form of numbness, tingling, weakness in lower limbs... The defeat of the nerve fibers of the upper extremities is less common. With damage to the cranial nerves, diplopia, dysphonia, dysarthria are observed.
Diagnostics
The symptoms of celiac disease are so varied and non-specific that studies should be done to confirm the presumptive diagnosis. Since genetic predisposition is a key factor in the development of gluten enteropathy, a family history of gluten intolerance is necessary.
The main diagnostic method is serological. In patients with celiac enteropathy, specific antibodies are determined in the blood:
- Antigliadin (AGA IgG, IgM);
- Endomysial (EMA IgA);
- Antibodies to tissue transglutaminase (tTG).
An equally important diagnostic method is the morphological examination of the mucous membrane of the small intestine. During endoscopy and histological examination of intestinal tissue, signs of atrophic lesions of the mucous membrane with shortening of the villi, lengthening of intestinal crypts are determined. 
Additional research methods:
- - anemia is determined;
- - hypoproteinemia, hypocalcemia, hypokalemia, hypomagnesemia are determined;
- Scatological examination - a large amount of fat and soaps is determined.
Treatment
Celiac disease is a disease that can be corrected with diet. If the diet is followed, the mucous membrane of the small intestine is restored and soon the person is no longer bothered by the unpleasant symptoms of the disease.
Diet principles for celiac disease:
- Exclusion of gluten-containing foods from the diet (bread, pasta and confectionery);
- Mechanical and thermal sparing of the digestive tract (dishes are steamed or boiled, used in pureed form or without grinding);
- Exclusion of products that enhance fermentation (milk, legumes);
- Restriction of foods that stimulate the secretion of the pancreas and stomach (rich meat broths, fatty meats).

With an exacerbation of the disease, in addition to a gluten-free diet, they carry out drug treatment in order to eliminate metabolic disorders. The following groups of drugs are used: