Cooling the burned surface with cold water is shown. Catastrophe medicine tests. Absolute signs of bone fractures include
The cause of the burn is the impact on the body of high temperature, certain types of radiant energy (rays of the sun, x-ray, radium), as well as a number of chemicals. The most common thermal and chemical burns are found. Their severity depends on the area of \u200b\u200bthe burned surface and the degree of burn. The burn of one third of the body surface is dangerous for the life of the victim. Depending on the nature of the changes in burned tissues, three degrees of burns are distinguished.
Signs of burn i degree It is redness of burnt fabrics, swelling of them and pain.
Burn II degree It is characterized by the formation of bubbles filled with liquid.
To burn III degree Non-critical changes (samples) of burnt fabrics are characteristic. In the most difficult cases there are charring them.
I degree burns are dangerous only with a large lesion area. It should be borne in mind that the changes characteristic of burns of the I degree precede the formation of bubbles and with burns of the II. Therefore, often after 10 - 15 minutes after the burn, only redness is observed, bubbles appear later. The latter with cities are usually breaking through, at the same time deep skin layers are exposed, which can be very easily infected. An even greater danger of infection of burnt parts of the body occurs when burns III burns.
The victims of burns are often falling into a difficult state. It is associated with the overexcitation nervous system painful irritations, as well as the action of formed in burnt fabrics toxic substances. Changing the nervous and cardiovascular system may determine development heavy Shock. At the same time, the state of general excitation is often observed.
Providing first assistance to the victim, It should be released from the clothes an burnt surface of the body (clothing is cut by seam).
In cases where clothes are burning on the victim, it is impossible to allow the burned run, rushing, because it only enhances the flame. In these cases, you need to immediately disrupt the burning clothes or to sneak the fire by throwing on the affected blanket, coat, chinel.
When providing assistance to the victim with signs of burns I degree, impose a bandage, moistened with wine alcohol, or to treat the burned surface with a saturated solution of potassium mangartage. Therapeutic effect These funds are associated with their dubbing action, which largely prevents the development of further pathological changes and the formation of bubbles.
When first aid, it should be careful to clean the skin around the bubbles with wine alcohol carefully and treat it with a solution of potassium mangartage. After that, it is necessary to impose a aseptic bandage on the burned surface. Obtain bubbles in the provision of prefigure help.
When burning items, a aseptic bandage is superimposed on the burned surface. If the victim is subject to evacuation, the burnt limbs must be immobilized.
Due to the danger of infection of open wounds, when assisting an exeed, it is necessary to comply with the observance of aseptics. All victims with extensive burns, with burns of lower extremities, as well as in contamination of the burned surface of the body, the earth is necessarily introduced anticipating serum.
In connection with the possibility of the development of shock, it is necessary to carefully observe the general state of the burnt, not allow them to cool them, be very careful during transportation. It is advisable to drink baked sweet hot tea.
In case of chemical burns, first of all, it is necessary to produce a rich and long-term washing of the burned surface with water.
For burns with acids for neutralizing the acid, the burned surface is wetting with 5% solution of soda, and with alkalis burns - boring or 2% acetic acid.
With phosphorus burns, it continues to burn it in the skin (they are very clearly visible if you enter the victims of the darkened room), in these cases it is necessary to make an abundant washing of the burnt surface with water, remove particles of phosphorus with tweezers and impose a bandage, moistened with 5% copper sulphate.
In front of burn phosphorus, it is necessary to take into account the possibility of introducing phosphorus particles into the mucous age and the conjunctival of the eyes. In these cases, flushing the eyes of the injured water, it should be immediately delivered to the point of medical medical care. In the daily life of burns I and II degree often occur after long-term skin irradiation with straight rays of the sun. Burns from sunlight, capturing a significant surface of the body, are often accompanied by an increase in temperature. With these burns, it is necessary to protect the skin from the further action of the rays; It is recommended to lubricate the burned surface with sterile fat. With the defeat of the body, other types of radiant energy requires medical care.
Burning - These are damage caused by the action of high temperature (flame, hot steam, boiling water) or caustic chemicals (acids, alkali). Special form of burns - raughter burns (solar, radiation, x-ray, etc.).
Modern extreme situations are very often accompanied by the emergence of victims of burns of varying degrees.
The degree of burns.
There are 4 degrees of burns (depending on the depth of tissue damage):
- I degree is characterized by hyperemia (redness) of the skin, swelling and feeling of pain. Under the action of high temperatures, the capillaries and the education of edema occur;
- II degree is accompanied by hyperemia, edema, the formation of bubbles filled with a transparent yellowish liquid. Serous accumulation, accumulating, peers epidermis, which causes the formation of bubbles, whose magnitude may be the most different;
- III degree is accompanied by a leather color with the formation of a stamp, which occurs as a result of coagulation of fabric proteins.
Burns of III degrees are divided into degree of IIIA burns, in which the death is capturing only the surface layer of the skin, part of the spun layer of the epidermis remains, and IIIIB, in which the whole thickness of the skin with the sprout layer of the epidermis remains.
- IV degree - accompanied by char harness and deep tissue (muscles, tendons, up to bone).
Usually, the affected burns are combined by various degrees. Face burns may be accompanied by eye burns, it is possible to burn the upper respiratory tract.
The severity of the burn depends not only from the depth of the tissue damage, but also from the size of the burn area. The larger the burn area, the hardest it is the current.
When changing clothes, they try to lose it, knock off the flame of water, the earth or press the burning fabric to the ground, immerse the burning sections into the water. The clothes rextant to the surface are not removed, and the wound can be closed as a aseptic or special anti-slim bandage.
It is very dangerous to enter the bunch of combustible substances on the skin and clothing.
With large limb burns, transport tires are superimposed.
With the extensive burn burns, it is necessary to wrap the victim into a sterile sheet or impose an anti-breakele.
Help need to be very careful not to strengthen pain sensations.
Give pain meals, hot drink. With a favorable situation and opportunities, medical care should be as soon as possible.
If the burning injury is obtained during a fire in a closed room or in a focus of the defeat of the incendiary mixture, the victims of the fire and smoke from the zone are affected as quickly as possible. A dry aseptic bandage is applied to the burned surface. It is not recommended to clean the burned surface and calculating bubbles. With chemical burns with acids and alkalis, it is necessary to wash them off from the skin with a stream of cold water and neutralize the effect of the acid with soapy water, and alkali is a weak solution of vinegar. After neutralization, an aseptic bandage is superimposed. In cases of asphyxia (choking) arising from the thermochemical effects or poisoning of combustion products, the victim is purified by the oral cavity and the pharynx against mucus and the vomit and proceed to artificial respiration.
Thermal burn arises from the impact on the skin of boiling water, flame, molten, red-hot metal. To reduce pain and prevent tissue edema, it is necessary to immediately substitute the burned hand (leg) under the stream of cold water and hold to the sacrament of pain.
Then the first degree (when the skin is blushed only) lubricate the affected area with alcohol or cologne. We can not apply a bandage. It is enough several times a day to handle the burned skin with special aerosols of type "Levian", "vinendula", "oxycycloosol", "panthenol", which are designed to treat surface burns and sold in a pharmacy without a recipe.
When burning a second degree (when bubbles were formed, some of them burst and impaired the integrity of the epidermal cover - the top layer of the skin) to process the burn area with alcohol, as it causes severe pain and burning. In any case, it is impossible to pour bubbles: they protect the burn surface from infection. On the burn area, impose a sterile bandage (sterile bandage or stroking fabric).
The burned skin should not be lubricated with a fat, a greenflaw, strong heatman solution. It will not bring facilitations, and the doctor will be difficult to determine the degree of lesion of tissues.
If not at hand, sketch on the affected blanket, dense fabric. But keep in mind: the effect of high temperature on the skin is the more descended than the longer and densely pressed to it smoldering clothes. Man in burning clothes can not be baked with head to avoid defeat respiratory tract and poisoning toxic combustion products.
Having haunted the flame, quickly remove with the injured clothes, cutting it. Affected body sections for 15-20 minutes. Pour the jet of cold water.
With extensive lesions, cover the victims of the stroked towels, a sheet, tablecloth. Give him 1-2 analgin or amidopyrin tablets, call "ambulance" or deliver it to a medical institution.
Chemical burn causes concentrated acids, alkalis, salts of some heavy metals. Chemical substance should be removed as quickly as possible! First of all, remove the chemicals on the affected clothes on which chemicals hit. Try to do it so that you yourself do not get burns. Then the affected body surface rinse under the abundant jet of water from the crane, soul, hose for 20-30 minutes. It is impossible to use a tampon moistened with water, since any chemical substance is rubbed into the skin and penetrates its deep layers.
If the burn is caused by alkali, washed with water affected skin area trees with a solution of citric or boric acid (half a teaspoon on a glass of water) or a table vinegar, half-diluted with water.
Plots of the body, burned with some kind of acid (except for fluid), rinse with an alkaline solution: soapy water or food soda solution (one teaspoon of soda on a glass of water). With a burning acid that is incoming, in particular, the brake fluid, it is necessary to remove the fluorine ions in it for a very long time, 2-3 hours, rinse the skin under the jet of water, as the fluorine penetrates it deep into it.
If the burn is caused by a negro lime, it is impossible to wash it off! In the interaction of lime and water, heat is distinguished, which can aggravate the thermal injury. First, carefully remove the lime from the body surface with a piece of clean fabric, and then rinse the skin with running water or treat with any vegetable oil.
On the burn area, impose a dry sterile bandage.
In all cases of burn, chemicals after providing first aid of the victim must be delivered to the medical institution.
Frostbite is damage to any part of the body (up to death) under the influence of low temperatures. Most often, frostbite occurs during the cold winter time at ambient temperature below -10 ° C - -20 o C. With long stay outside the room, especially with high humidity and strong wind, frostbite can be obtained in autumn and spring at the air temperature above zero.
Close and wet clothing and shoes, physical overwork, hunger, forced long immovable and inconvenient position, preceding cold injury, weakening the body as a result of diseased diseases, foot sweating, chronic vascular diseases of the lower extremities and cardiovascular system, severe Mechanical damage with blood loss, smoking, etc.
Frunce I degree (the most light) usually occurs with the short exposure of the cold. The affected skin of the skin is pale, after heating, turns, in some cases it has a crimson-red shade; Developing edema. Skin leather does not arise. By the end of the week, after frostbite, there is a slight peeling of the skin. Complete recovery comes to 5-7 days after frostbite. The first signs of such frostbite is a feeling of burning, tingling with the subsequent numbness of the amazed plot. Then appear skin itch And pains that can be insignificant, and sharply pronounced.
Frunce II of degree occurs with a longer exposure to cold. In the initial period there is a pale, cooling, loss of sensitivity, but these phenomena are observed with all degrees of frostbite. Therefore, the most characteristic sign - Education in the first days after injury bubbles filled with transparent content. The complete restoration of the integrity of the skin occurs within 1-2 weeks, granulation and scars are not formed. When frostbite II degree after heating pain intensively and longer.
When frostbite III degree, the duration of the cold exposure period and temperature reduction in tissues increases. The bubbles formed in the initial period are filled with bloody contents, the bottom of their blue-bugs, insensitive to irritation. The death of all skin elements with development in the outcome of the frostbite of granulation and scars occurs. The naked nails do not grow again or grow deformed. The rejection of dead tissues ends on the 2-3rd week, after which the scarring occurs, which continues up to 1 month.
The frostbite of the IV degree occurs with the long exposure of the cold, the decrease in the temperature in the tissues with it is the largest. It is often combined with frostbite III and even II degree. Dimensate all layers of soft tissues, bones and joints are often affected.
The damaged section of the limbs is sharply shiny, sometimes with marble colors. The enemy develops immediately after heating and increases rapidly. Leather temperature is significantly lower than on the surrounding area of \u200b\u200bcloth frostbite. Bubbles are developing in less frostbed sites, where there is a frostbite of III-II degree. The absence of bubbles with a significant exemplary, loss of sensitivity indicate a degree frostbite.
Under conditions of long stay at low air temperature, not only local lesions are possible, but also the overall cooling of the body. Under the general cooling of the body, it is necessary to understand the condition that occurs when the body temperature decreases below 34 o C.
The first aid is to stop cooling, warming the limb, the restoration of blood circulation in the cold fabrics affected by the cold and prevention of infection. The first thing to be done in the signs of frostbite is to deliver the victim to the nearest warm room, remove the stuffing shoes, socks, gloves. Simultaneously with the implementation of first aid activities, it is necessary to urgently call a doctor, ambulance to provide medical care.
When I froze the I degree, the cooled areas should be warm up to reddish with warm hands, light massage, rubbing woolen cloth, breathing, and then apply a cotton-gauze bandage.
When frostbite II-IV degree, rapid warming, massage or rubbing should not be made. Enter the heat insulating bandage (layer of gauze, a thick layer of wool, again a layer of gauze, and on top of a melted or rubberized cloth from above). The amazed limbs are fixed with the help of the girlfriend (plate, a piece of plywood, a dense cardboard), overlapping and bothering them on top of the dressing. You can use vitro, fuels, wool fabrics as a heat insulating material, etc.
The victims give hot drink, hot food, a small amount of alcohol, aspirin tablet, analgin, 2 tablets "but-shpa" and papaverine.
It is not recommended to break patients with snow, since the blood vessels of the brushes and stop is very fragile and therefore they are damaged, and the arms of the skin on the skin contribute to the introduction of infection. It is impossible to use the rapid warming of the frostbed limbs by the fire, it is uncontrolled to apply the heating and the like sources of heat, as it worsens the procendency. An unacceptable and inefficient first aid option is rubbing oils, fat, rubbing with alcohol tissues with deep frostbite.
In practice, there are also cold injuries arising from contact with warm skin with a cold metal object. It is worth a curious baby to grab naked hand for some piece of iron or, worse, licking it with a tongue, as he tightly sticks to her. You can free yourself from the shackles, only by moving them together with the skin. The picture is still a heartbreaking: the child squeals pain, and its bloody hands or mouth leads parents in shock.
Fortunately, the "iron" wound is rarely deep, but still it must be urgently disinfected. First, rinse it with warm water, and then hydrogen peroxide. Released oxygen bubbles remove the dirt that fell inside. After that, try to stop the bleeding. It helps the hemostatic sponge attached to the wound, but you can do and folded several times with a sterile bandage, which you need to press and keep to a complete bleeding stop. But if the wound is very big, you should urgently apply to the doctor.
It happens that the adhesive child does not risks himself to break away from the cunning piece of hardware, and his calls on the rescue. Pour the stuck with warm water (but not too hot!). Warred, metal will definitely let go of his unlucky prisoner.
There are some simple rules that will allow you to avoid hypothermia and frostbite on a strong frost:
- Do not drink alcohol - alcoholic intoxication causes a greater heat loss, at the same time causing the illusion of heat.
- Do not smoke in the cold - smoking reduces the peripheral circulation of blood.
- Wear loose clothing - it contributes to normal blood circulation. Dress up as a "cabbage" - while there is always a layer of air between the layers of clothing, perfectly holding heat. Outerwear must necessarily be waterproof.
- Close shoes, no insoles, raw dirty socks often serve as the main prerequisite for the appearance of scuffs and frostbite.
- Do not go to the frost without mobs, caps and scarf. The best option is mittens of moisture-repellent and unsuccessful fabric with fur inside. Gloves are made of natural materials, although it is convenient, but they do not save frost. Cheeks and chin can be protected by a scarf. In the windy cold weather before entering the street open areas of the body. Lubricate with a special cream.
- Do not shoot the shoes on the frost from frostbed limbs - they will be swollen and you will not be able to wear shoes again. If the hands froze - try to warm them under the mouse.
- Spicy wind - the probability of frostbite in the wind is much higher.
- Do not wet the skin - water spends heat significantly better than air. Do not go to the frost with wet hair after the shower. Wet clothes and shoes need to be removed, wipe water, if possible to wear in a dry and as soon as possible, deliver a person to heat. In the forest, it is necessary to ignite the fire, undress and dry clothes, during this time vigorously making exercise and basking from the fire.
- It is useful for a long-term walk in the frost. Separate a pair of replacement socks, mobs and thermos with hot tea. Before entering the frost, you need to eat - you might need energy.
Electricalrahy Most often occurs when contacting victims with uninsulated electric wires.
The volume of first aid depends on the degree of lesion and lies in the following events: bulk the circuit (turn off the switch or switch); Separate a current part of the victim (pull out the hands of a person, drag the victim from the current source). At the same time, it is impossible to take on bare hands for the current part of the victim. It is necessary to use items that are not conducted by electric current (dry stick, clothes, rope, rope, dry rag, cap, leather and rubber gloves, paper, etc.). For isolation from the Earth, you need to get up on a dry board, rubber (rubber rug, tire, etc.). You can refine or cut the current-carrying wires with an ax with a dry wooden handle and special laying (with insulated handles). Each phase of the wire must be chopped separately (so that there is no short circuit). You can get up on some insulated gasket (rubber mat, board).
If the victim is at the height, it is necessary to remove it from there (opening the chain to release the victim from the current can lead to a drop in its height).
At the place of the burn should be applied a aseptic bandage, if the overall condition of the victim does not require other urgent measures, and send to the doctor.
The effect of current on the body depends on its strength, voltage, resistance, as well as on the initial state of the nervous system of the victim. People who have undergone electric shock may lose disability for a long time.
A sharp muscle spasm during the passage of electric flow can lead to bone fractures, dislocation, squeezing of the vertebrae.
During the action of electric flow, the victims often occurs a violation of breathing and cardiac activity, the violations may be so deep that the stop of the heart and breathing is coming - clinical death. If such a victim, for 6-8 minutes, do not assist in the restoration of blood circulation and respiration, then it comes biological death.
First aid for clinical death lies in immediate (at the scene) artificial respiratory And indirect heart massage.
When teaching artificial respiration, it is necessary to recall the anatomy and physiology of respiratory organs.
Breathing is a physiological process at which gases occurs between the body and the external environment. At the same time, the body receives oxygen necessary to all its cells and tissues, and highlights carbon dioxide accumulated as a result of their livelihoods.
The respiratory authorities include air-axle paths (nasal cavity, larynx, trachea, bronchi) and lungs. Inhaled through the nose or mouth air through the larynx, the trachea, and then the bronchi enters the lungs. Bronchi in light branches on the branch of more and more small caliber. The smallest finite bright twigs end in alveoli bubbles. Through the thin wall of the alveoli and gas exchange occurs; Oxygen comes into the blood, carbon dioxide is released in the alveoli from the blood. Thus, exhaled air contains carbon dioxide More, and oxygen is less than air entering into the lungs when inhaling: in the inhaled oxygen oxygen, 20.94%, and carbon dioxide 0.03%, in exhaled -, respectively, 16.3 and 4%.
The process of respiration consists of rhythmicly repeated breaths and exhalations. When inhaling, thanks to the reduction of certain muscles (intercostal muscles, aperture), the chest expands, the air fills the bronchi and alveoli, as a result of which the lungs are expanding. Following this, the muscles relax, the chest falls down, squeezing the lungs and displacing air from them - exhale occurs. Respiratory frequency in a healthy adult is 16-18 per minute.
Each lightest lies in an isolated cavity lined with a shell - pleural. In the pleural cavity there is no air and the pressure in it is negative. In case of injury of the chest and damage to the pleura in the pleural cavity, air flows - the lung falls out and loses the ability to participate in breathing.
Getting Started with artificial respiration, it is advantageous if possible, it is necessary to ensure the influx for the victim of fresh air - to unbutton the collar, the belt, the belt and other shy of the breath of the clothing.
An index finger, wrapped with a handkerchief or a piece of gauze, purify the mouth of the victim from mucus, sand, etc. The simplest and at the same time, the most effective is artificial respiration in the method of "mouth to mouth". The head of the victim is maximizing back. To keep it in this position, something is put on the blades. Holding the head of the victim in the thumbnate one hand, the other gives him the lower jaw to the book in order for the mouth to be semi-open. Then, having made a deep breath that assists applies through a handkerchief or a piece of gauze his mouth to the mouth of the victim and exhales the air from its lungs into it. At the same time, the hands holding the head, he pushes the victim's nose. The chest of the victim is expanding - there is a breath. Air blowing stops, the chest falls down - exhalation occurs. The help rendering again makes breath, again blows the air into the lungs of the victim, etc. The air should be blown at a frequency corresponding to the respiratory frequency of a healthy person (Fig. 1). Air blowing into the lungs of the victim can be produced through a special tube - air duct (Fig. 2). If the jaws of the victim are tightly compressed, the air in its lungs need to be blown through the nose (the way "mouth into the nose"). To do this, the head of the victim is also held with one hand in the thorough position, and the other hand covers his mouth. Then the help, having made a deep breath, through the scarf covers his lips the nose of the victim and blows into it. As soon as the breasts of the victim expands, the help will take away his mouth from his nose and removes his hand from his mouth - it takes out.
Artificial respiration in other ways is made only when for any reason (for example, injury), the use of methods of "mouth to mouth" and "from mouth to the nose" is impossible.
Method of Sylvester. The victim lies on the back. The help becomes in his headboard, takes both his hands for the forearm and pulls over his head - there is a breath. Then bent B. elbow joints Hands of the victim he presses to his chest and, continuing to keep them for the forearm, puts pressure on the bottom department of the injured injured - exhalation occurs. Movement (breathing - exhale) repeat with a frequency of 16-18 per minute. The method is not applicable if you have injured damage to the hands or chest.
Along with the respiratory stop, the victim can stop the activity of the heart. This is based on the absence of a pulse, the expansion of pupils, as well as the absence of a heart jacket when listening to the ear attached to the left half of the chest in the nipple area. In this case, simultaneously with artificial respiration is made indirect heart massage. If two persons participate in assistance, then one makes an artificial respiration according to the method of "mouth in the mouth" or "from the mouth to the nose" the second, put on the left side of the victim, puts the palm of one hand to the lower third of his sterns, puts the second hand On the first and at the time when the victim occurs, the bottom of the palm rhythmically makes several (3-4) energetic push presses on the sternum, after each shock the rapidly rolled hands from the chest. If one person is assisted, then by making a few pressure on the sternum, he interrupts the massage and is blowing through the mouth or the breath of the air into the light victim, then again makes pressure on the sternum, again blows air, etc.
Just like when defeated electric shock, It turns out assistance to the injured when the lightning strikes. The view common among injecting persons that the electric current affected should be buried to the ground, erroneously. Do not do this.
Syncs is a short-term loss of consciousness due to a temporary shortage of blood in the brain. This usually occurs when the body's blood vessel is expanded, and then the amount of blood cannot maintain pressure at the top of the body. Sometimes fainting is caused by an unexpected healing of heartbeat. The most common causes are listed below.
Fine or superheated air.
Long standing.
Fear or severe chagrin.
Long cough.
Stress during defecation.
Symptoms
Pallor.
Sweating.
Dizziness.
Worsening vision.
Tinnitus.
Loss of consciousness.
The fall.
Help with fainting
1. Locate the patient to bed.
2. Raise its legs higher.
3. Estate cramped clothes.
The easiest degree of fainting - swoon - It begins with a sudden lung harnessing consciousness, dizziness, ringing in the ears, yawn. Patients pale, there is a cooling of hands and feet, sweat drops on the face. Actions: The patient must be immediately put on his back (in easy cases, you can simply be satisfied with a support with your back on the back of the chair, chairs). Note that it does not fit anything under the head! The head must be at least one level with the case. It is necessary to ensure good oxygen access (it is often one of this leads to the termination of fainting) - unbutton the collar if a lot of zooak crowded around the fallen person - to speak. It is necessary to calm the patient, the emerging fear can provoke a spasm of the brain arteries and enhance the brain ischemia. Can sprinkle on face cold water Or bring to the nose to the robe moistened with alcohol. Usually, the attack of lipotimia lasts a few seconds, but, in any case, if you have time to put the patient and provide it with oxygen access, you can be calm, it will not lose consciousness.
Simple faint It usually begins with boldness of consciousness (i.e., as well as lipotimia), and subsequently comes the complete loss of consciousness with the shutdown of the muscular tone, the patient slowly settles. Blood pressure is low, breathing superficial, distinguishable with difficulty. The attack lasts several tens of seconds (up to 4-5 minutes maximum), then the fast and complete restoration of consciousness follows. Actions: If the patient has already lost consciousness, you do not need to tele it or try to raise it. Consciousness will return when the normal blood supply to the brain will be restored, and this requires a horizontal position of the body (the tone of the vessels is sharply reduced and if we raise your head or body, the blood simply flies into the lower limbs and no good blood supply to the lower limbs). You do not need to try to find the pulse, because of the low pressure and the loss of the vascular tone, the pulse wave is very weak, and you can simply not grope it. Doctors determine the pulse on the neck in such cases, on the carotid artery (if you think you know where the carotid artery is located, you can try to find the pulse there). Otherwise, as well as during lipotimia - oxygen access, ammonia. Do not strive to pour the salmon on the patient's patient or wipe the whiskey - this is a solution of ammonia, and it does not restore the brain circulation, and stimulates the respiratory center through the nerve endings in the nasopharynk (a person makes a reflexian breath and a large portion of oxygen with inhale comes into the body. You can, continuing to keep the vaccine with the nashem at the nose, for a couple of seconds, cover the mouth with palm - all the inhaled air will go through the nose and the vapor of the nasya will fall into the nasal cavity. You can, at worst, just click on the tip of the nose - the pain stimulus is also sometimes able to stimulate the restoration of consciousness.
Convulsive fainting It is characterized by accession to the picture of the fainting seizure (common, generalized or single twitching of individual muscles). In principle, almost every brain hypoxia (disadvantage of oxygen), which is ongoing more than 20-30 seconds, can lead to the emergence of such symptoms. Actions do not differ from those with a simple faint, but it is necessary to ensure that there is no mechanical damage to the head, housing, hands during convulsion. Please note: the convulsions can be characteristic of an epileptic seal (while typical signs are a bite of the tongue, often there are screeching or moans at the beginning of the seal (vocalization of the seplide), often appear redness and silence of the face) and for a hysterical seal.
Bettoleppsia - This is a fainting arising against the background of chronic lung diseases. It is due to the fact that during the protracted kola's cough in the chest cavity, the pressure and the venous outflow of blood from the skull cavity is significantly imperative. True, in all these cases it is necessary to study the cardiovascular system to eliminate the pathology from the heart. Special actions do not require. The duration of fainting is most often small.
Drop Atachi. - These are unexpected, sudden drops of patients. At the same time, almost never loss of consciousness, although there may be dizziness, sharp weakness. Usually observed in patients with osteochondrosis of the cervical spine, complicated by the development of vertebro-basallast insufficiency, as well as well-healthy young pregnant women.
Vasodepressor fainting -more often in children, more often occurs when overwork, lack of sleep, emotional voltage, staying in the stuffy room. It has a rather complicated genesis of development. Actions do not differ from generally accepted, but careful examination is required to eliminate possible diseases of the nervous system.
Orthostatic fainting - occurs with a sharp transition from a horizontal position to vertical when the cardiovascular system Do not have time to rebuild for full provision of brain. Especially expressed with simultaneous reception of beta blockers, diuretics, nitrates, etc. More often, however, it happens not fainting, and so-called. Purests, expressed in sudden weakness, dizziness, darkening in the eyes when changing body position.
Hypersensitivity syndrome of carotid sinus -proceeds along the type of simple or less, convulsive faint. It is due to the hyperactivity of the carotid reflex (with carotid sinuses located on the front-side surfaces of the neck), which causes suddenly emerging bradycardia, short-term stopping of the heart, arrhythmia. By provoking factors, there may be a sharp turn of the head, wearing tight collars - from here and conclusion: Never forget when you assist weaken the collar, freeing the neck of the victim.
Arrhythmic fainting - Some arrhythmias can lead to loss of consciousness. The main violations of the rhythm capable of leading the loss of consciousness are paroxysmal forms of fluttering and flickering atrial, full transverse blockade, elongated Qt syndrome, paroxysmal ventricular tachycardia. Other form of arrhythmias extremely rarely lead to loss of consciousness, however, every patient suffering from arrhythmias (and especially the above-mentioned arrhythmias), it is desirable to consultant at the attending physician about the possibility of this complication of this complication and, together with the doctor, to work out the rules of conduct that would allow Minimize the risk of such complications.
Chemical burns Liquid or solid mineral and organic substances that actively interact with body tissues can cause such liquid or solid mineral and organic substances. Not only skin covers are affected (especially strong burns are observed when the substance is hooked up), but also mucous membranes. The burns of the mucous membranes and, especially, the cornea of \u200b\u200bthe eyes, as a rule, have more severe consequences than skin cover burns.
Chemical burn substances can belong to different classes of compounds: mineral and some carboxylic acids (for example, acetic, chloroacetic, acetylendicarbonovaya, etc.), acid chloride cries (for example, chlorosulfonic acid, chloride sulfuril and thionyl), phosphorus and aluminum halide Phenol, caustic alkalis and their solutions, alkali metal alcoholates, as well as neutral substances - liquid bromine, white phosphorus, dimethyl sulfate, silver nitrate, chlorine lime, nitro compound of aromatic series.
Chemical burns cause many organic matter. For example, phenol and most substituted phenols, falling on the skin, cause the appearance of waving lichen. With prolonged exposure, the tissue death occurs and scurvas appear. Most of the nitro compounds of a number of benzene, as well as polinutro- and nitro-compounds cause ancase. Halogendinitrobenzenesols and nitrosomethylmouris used to obtain diazomethane are particularly strongly. Chemical burns cause dialkyl sulfates, especially dimethyl sulfate.
Mineralic acids are most dangerous hydrofluoric and concentrated nitric acids, as well as a mixture of nitric acid with salt ("tsarist vodka") and a concentrated sulfuric ("nitruous mixture") with acids. Concentrated hydrofluoric acid is very fast corrosive skin and nails; At the same time, extremely painful and long non-healing ulcers are formed. In case of contact with the skin of concentrated nitric acid, a strong burning sensation is immediately felt, the skin is painted in yellow. With a longer contact, the wound is formed.
Concentrated sulfur and chlorosulfonic acids are also very dangerous, especially for the eyes. However, if sulfuric acid is immediately washed away from a damaged skin area with plenty of water, and then 5% sodium bicarbonate solution, burns can be avoided. Chlorosulfonic acid is more aggressive than sulfur, and its skin getting into the skin causes a strong chemical burn. With long-term contact, these acids cause the skin charring and the formation of deep ulcers. Intelligence of these acids in most cases leads to partial and even complete loss of vision. The least dangerous of mineral acids is salt. It causes only itching, not penetrating deep inside the tissues. The skin becomes tough and dry and after a while begins to peel.
A similar effect on the skin is tionyl chloride, phosphorus halides and aluminum chloride. Hydrolyzing skin moisture, they decompose with the formation of hydrochloric and phosphoric acids, which cause a chemical burn.
Catering alkalis and their solutions cause heavier chemical burns than acids, as they cause swelling of the skin and therefore cannot be quickly washed with water from the affected place. With prolonged action, very painful deep burns are formed. Delete alkali solution from affected location is recommended not to water, but a diluted solution of acetic acid.
Enhancing in the eye almost always causes full blindness.
Alcohboles and their alcohol solutions act on the skin and mucous membranes in the same way as caviar alkalis, but they are more aggressive.
Special caution must be observed when chopping solid alkalis, calcium carbide, lithium hydride and sodium amide, which cause severe lesions of not only skin cover, but also the mucous membranes of the respiratory tract and eye. When performing these works, in addition to the mandatory use of protective gloves and masks (and not glasses), you should wear a gauze bandage, a prevention nose and mouth.
First aid:
- With chemical burns, the affected space was washed with water jets from under the tap for a long time - at least 15 minutes.
- Next, when burns with acids and acid-like migrating substances, we apply a row with 2% solution of sodium bicarbonate, and with alkalis burns - 2% solution of acetic, lemon or wine-eyed acids.
- If the aggressive substance fell on the skin through clothes, it should be cut before removing scissors, so as not to increase the lesion area.
- Synthetic clothing It can be dissolved in some aggressive substances, for example, in sulfuric acid. When washed with water, the polymer coagulates and covers the skin with a sticky film. In this case, the washing does not reach the goal. It is first necessary to carefully erase the acid from the skin with dry cotton cloth and then rinse with water.
Resuscitation is a complex of special measures aimed at the revival of a person who is in a state of clinical death.
Upon the occurrence of clinical death, breathing and cardiac activity are absent. This is manifested as follows: the lack of consciousness, ripples on carotid arteries, respiration, sharply expanded pupils, cyanosis, or a sharp poverty of the skin and mucous membranes.
The loss of consciousness is determined by the absence of a response of the victim to the sound or tactile stimulus (the case, patting the cheek, slightly shake it).
The absence of a pulse at the carotid artery is regarded as a sign of "catastrophe". It is determined by the index and middle fingers to retreat by 2-3 cm away from the thyroid cartilage protruding on the neck or along the inner contour in the middle of the breast-eyed muscle.
Stop breathing is easy to notice in the absence of breathing motions of the chest or aperture. To clarify, you can attach an ear to your mouth or nose, to bring the affected smooth item to the mouth - the melon cover, the glass of the compass or the mirror - and whether it fogges or not.
Expansion of pupils and the absence of their reaction to light are detected by opening upper century and eye lighting. If the pupil is significantly expanded (in the entire iris) and does not sneak into the light, then this feature is always anxious.
Clinical death is a stage of dying, convertible only by resuscitation. The maximum duration of clinical death is 5-6 minutes.
The success of human revival depends largely on the sequence of recovery techniques, which is carried out in the following order:
A - free the respiratory tract from mucus and foreign bodies;
In - to start artificial ventilation of the lungs (artificial respiration) according to the method of "mouth in the mouth" or "from the mouth to the nose";
C - restore blood circulation by outdoor heart massage.
To ensure the maintenance of the respiratory tract, the maximum extension of the injured head is needed. The help providing one hand on the back surface of the neck, another in the forehead area and produces a light, but energetic head extension of the head. It can be achieved by placing a roller from rolled clothes under the patient's shoulders. Next you need to inspect the oral cavity, clean foreign languages (a finger, wrapped with a napkin or handkerchief) and dry the mouth with a grain material. At the end of the toilet, the oral cavity immediately proceed to artificial ventilation (IVL).
Artificial ventilation of the lungs in the method of "mouth in the mouth": After a deep breath, completely covered by the mouth of the victim and holding his nose with his fingers, make a sharp energetic exhalation in his respiratory tract, after which they get their head aside. The effectiveness of the blowing can be seen by increasing the volume of the chest and the noise of exhaled air. For hygiene purposes, impose on the mouth of the victim or handkerchief. IVL should be carried out with a frequency of 12-15 times in 1 min.
If the IVL is carried out by a child, the air blowing should be done carefully, without using the entire life tank of the lungs, in order to avoid the break of the pulmonary fabric. For breast-age children, there is enough air volume in the oral cavity. IVL should be carried out with a frequency of 20 times in 1 min.
Technique outdoor heart massage. The victim is placed on the back on a rigid and even base (gender, land). The helping occupies the side of the patient on the side of the patient, grips the end of the sternum, and at a distance of 2 transversely arranged fingers in the direction upwards, it imposes a palm of the brush with the widest part of it perpendicular to the longitudinal axis of the body. The second palm puts the cruciform from above. Not bending hands produces a strong pressure on the sternum. Push-squeezing produce quickly, using the efforts of the shoulder belt and body weight. After that, the pressure is stopped, allowing the chest to deal with, without tearing hands from the surface of the chest. During this time, the heart is passively filled with blood. These movements are repeated with a frequency of at least 60 per 1 min. Compress the chest should be vigorously under dosage pressure to cause a pulse wave in a carotid artery.
The outer massage of the heart in children is carried out according to the same rules, but with one hand and with a frequency of 80 pressing in 1 min., In infants - tips (2 and 3) two fingers, pressed into the middle part of the sternum with a frequency of 120 pressing in 1 min.
The effectiveness of massage is judged by changing the color of the skin of the face, the appearance of the pulse on the carotid artery, the narrowing of pupils.
If the help is provided by one person, the ratio of the manipulations carried out should be 2 to 15. For every 2 rapid blowing of air in the lungs, there should be 15 massage sores of the sternum.
If the help has 2 people, then the ratio of receptions must be 1 to 5. One conducts an outer massage, the other is an artificial respiration after each 5 squeezing of the sternum at the time of the breastsets.
Table of contents of the topic "Thermal burns. Burning disease. Urgent Care With burns. Specialized medical care for burning. ":1. First aid for thermal burns. Thermal burns. Pathogenesis of thermal burns. Classification of burns.
2. Manifestations (clinical signs) burn. Diagnosis of lesion depth of skin when burn. Determination of the area of \u200b\u200bthe burn surface.
3. Burn disease. What is burning disease? Stages of burn disease.
4. Signs (clinic) of burn disease. Diagnosis of burn shock. Setting the diagnosis of the burn shock.
5. Breathing of the respiratory tract (ODE). Diagnosis of ODP. Diagnosis of the burn of the respiratory tract.
6. Emergency care for burns. First assistance in burns. Methods of first aid for burning.
7. Emergency care at the site of burning burns. Local treatment with a burn. Burn therapy.
8. The volume of emergency care before transportation to the hospital. Medical care for burning before transportation.
9. Help the patient with a burn during transportation to the hospital. Qualified medical care for a burn. Treatment of burns in the hospital.
10. Specialized medical care for a burn. Disinfecting therapy for burning toxmia.
Emergency care at the site of burning burns. Local treatment with a burn. Burn therapy.
1. Terminal Agent carried out by all possible methods. You can use water, snow, sand and other technicians. Use the primary fabric items should be larger, since they create conditions for a longer exposure to high temperatures on the victim. After eliminating the impact of the thermal agent, the rapid cooling of the burnt sections should be made.
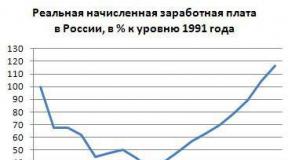
2. Cooling of burnt surfaces It is often practically the only efficient method of local impact in the first aid. It can be carried out using a long washing with cold water, applying polyethylene packets or rubber bubbles with ice, snow, cold water, etc. Cooling should be carried out at least 10-15 minutes., Without delaying the transportation of the victim. It prevents the heating of driving tissues (thereby contributing to the restriction of the depth of thermal damage), reduces the pain and degree of edema development. In the absence of the possibility of using cooling agents, the burned surfaces should be left open to air cooling (R. I. Maraziang, N. R. Panchenkov, 1982).
3. Purchase syndrome. The use of narcotic drugs in generally accepted doses, for example, 1-2% solution of priedol in an amount of 1-2 ml. In the absence of narcotic analgesics, any other painkillers (analgin, barallgine, etc.) can be used.
4. Processing the wound surface at the scene. It is strictly forbidden to remove the part of the burnt clothing from the affected surface, open burn bubbles. Parts of the burnt clothing should be left in the wound, cutting off their scissors from the whole tissue. The affected surface should be closed with a sterile bandage, richly moistened with a solution of any antiseptic (for example, furaticillin). It is permissible to close the wound with a dry sterile bandage, but this is not the optimal option, since its rapid adhesion is occurring (primacy) to the burn surface, resulting in injury to the wound with the subsequent removal of the bandage. It is not recommended at the first aid stage to use fatty preparations (ointments, fats), since they create conditions that prevent the formation of dry stamp, they have "thermostatic" properties, thereby contributing to the rapid reproduction of microorganisms (R. I. Mraziang, N. R. Panchenkov, 1982). In extreme cases, the burned area is possible for several hours (the transport stage) leave without a dressing (V. M. Burmistrov, A. I. Blaguev, 1986).
5. Abundant drink. Prior to the arrival of the brigade of the joint venture, with extensive burns and the absence of nausea and vomiting, warm tea, coffee, alkaline water, etc. If the patient does not even feel thirst (this happens rarely), the perseverance should be shown and convincing it at least 0, 5-1 l liquid, especially if the period of subsequent transportation takes several hours. This is necessary for the correction of developing hypovolemia.
Bone crepitia
5. Painful swelling in the injury zone
Relative features of fractures include
1. pain in the injury zone
2. painful swelling
3. hemorrhage in the injury zone
4. Capital
Absolute signs of penetrating injury of the chest are:
1. Dyspnea
2. pallor and cyanosis
3. gray wounds
4. air noise in the wound when inhaling and exhaling
5. subcutaneous emphysema
Characteristic symptoms Card injuries are:
1. excited state after the restoration of consciousness
2. headachedizziness after the restoration of consciousness
3. retrograde amnesia
4. Causes
5. loss of consciousness at the time of injury
1. With indirect heart massage
3. From a precondial strike
4.
The imposition of the heat insulating bandage patients with frostbite is required:
1. in the pre-reactive period
2. In the reactive period
Cooling the burned surface with cold water is shown:
1. in the first minutes after injury
2. only when I burn I degree
3. Not shown
The optimal position for a patient with acute left-selling deficiency is the position:
1. Lying in an elevated foot end
2. Lying on the side
3. sitting or half-sidia
The priority event in acute left-selling deficiency is:
1. Introduction of stanfantine intravenously
2. the introduction of Lazix intramuscularly
3. Dacha Nitroglycerin
4. Overlay venous harnesses on the limb
5. Arterial pressure measurement
Promotion lower jaw:
1. eliminates the scarce of language
2. Warns the aspiration of the contents of the rotogling
3. Restores the passability of the respiratory tract at the level of the larynx and trachea
Introduction of the duct:
1. eliminates the spares of language
2. prevents the aspiration of the contents of the rotogling
3. Restores respiratory tract
The appearance of the pulse on the carotid artery during the indirect heart massage indicates:
2. the correctness of the massage of the heart
3. On the revitalization of the patient
Required conditions when conducting artificial ventilation The lungs are:
1. elimination of the spares of language
2. Application of the air duct
3. sufficient exposure
4. Roller under the scaves of the patient
The patient's chest movement during artificial ventilation lungs testify:
1. The effectiveness of resuscitation
2. on the correctness of the artificial ventilation of the lungs
3. On the revitalization of the patient
Signs of the effectiveness of resuscitation are:
1. Pulsation at the carotid artery during a heart massage
2. Chest movements during IVL
3. reducing cyanosis
4. narrowing Zrachkov
5. Expansion of Zrachkov
Effective resuscitation continues:
5. before restoring vital activity
Inefficient resuscitation continues:
3. 30 minutes
5. Before the restoration of vital activity
The imposition of venous harnesses during cardiac asthma shows:
1. With low blood pressure
2. with high arterial pressure
3. With normal hell
The optimal position for the patient in the comatose state is the position:
1. On the back with the lowered head end
2. On the back with the lowered foot end
3. on the side
4. On the stomach
The patient in a coma is given a steady lateral position with the purpose of:
1. Language warehousing
2. aspiration Prevention Mass Mars
3. Warnings of Shock
Patients in a comatose state with their spinal injuries are transported in position:
1. On the side on ordinary stretchers
2. On the belly on ordinary stretchers
3. On the side on the shield
4. on the back on the shield
The patient with an unspecified nature of the coma nurse should:
1. provide respiratory tract
2. start inhalation of oxygen
3. enter intravenous 20 ml of 40% glucose
5. Watch intramuscularly Cordiamine and caffeine
The optimal position for the patient with shock is:
1. Position on the side
2. Position half-sidia
3. raised limbs
Three main prophylactic anti-shock events In patients with injuries
1. Introduction vesseloring drugs
2. Inhalation of oxygen
3. Anesthesia
4. stop outdoor bleeding
5. immobilization of fractures
In the cold season, the hemostatic harness is superimposed:
1. for 15 minutes
2. for 30 minutes
3. for 1 hour
4. For 2 hours
With a fracture of edges, the optimal position for the patient is the position:
1. Lying on a healthy side
2. Lying on the sick side
3. Sitting
4. Lying on the back
Patients with sharp poisoning are hospitalized:
1. Ply severe condition Patient
2. In cases where the stomach could not be washed
3. With the unconscious state of the patient
4. in all cases of sharp poisoning
The conditions under which nitroglycerin should be stored:
1. Temperature 4-6 ° C
2. Darkness
3. Hermetic packaging
Contraindications for the use of nitroglycerin are:
1. low arterial pressure
2. Myocardial infarction
3. acute violation of cerebral circulation
4. brain-brain injuries
5. Hypertensive crisis
Patients with electricians after assistance:
2. Do not need further examination and treatment
3. hospitalized ambulance
On the burned surface superimposed:
1. Headband with Furacillin
2. Bandage with syntomicin emulsion
3. dry sterile bandage
4. Headband with tea soda solution
With penetrating injuries, the nurse must:
1. Enter the outward organs
2. put an armband on the wound
3. Give inside hot drink
4. enter an anesthetic
With penetrating injuries eyeball The bandage is superimposed:
1. on the sore eye
2. on both eyes
3. Bandage imposition is not shown
With a sudden falling of blood pressure in a patient with myocardial infarction, a nurse must:
1. Enter adrenaline intravenously
2. introduce stanfantine intravenously
3. enter Meston intramuscularly
4. lift the foot end
5. Enter Cordiamine P / K
For electricians, assistance should begin:
1. With indirect heart massage
2. With artificial ventilation of the lungs
3. From a precondial strike
4. with termination of electric current
3. disseminate clothes
4. put the patient on the side
5. call a doctor
Air blowing and grinding of the chest during resuscitation carried out by one resuscator are carried out in the ratio:
1. 2: 30
Air blowing and grinding of the chest at reanimation conducted by two resuscitations are made in the ratio:
2. 2: 30
Indirect heart massage is carried out:
1. On the border of the upper and middle third of the sternum
2. on the border of the middle and lower third of the sternum
3. 1 cm above the sword-shaped process
Ground compression with an indirect heart massage in adults is made with frequency
1. 40-60 per minute
2. 60-80 per minute
3. 80-100 in Min.
4. 100-120 per minute
If the patient has no consciousness in the patient, but there are no visible respiratory disorders and blood circulation, the nurse must:
1. Make intramuscularly Cordiamine and caffeine
2. Give sniffing the ammonia alcohol
3. disseminate clothes
4. put the patient on the side
5. call a doctor
6. start inhalation of oxygen
1. Put
2. give nitroglycerin
3.
5.
With a cardiac asthma clinic in a patient with high arterial pressure, a nurse must:
1. give a sideling position
2. give nitroglycerin
3. start inhalation of oxygen
4. Enter stanfantine or Corglikon intravenously
5. Enter prednisone intramuscularly
6. introduce lazikes intramuscularly or give inside
With a cardiac asthma clinic in a patient with low arterial pressure, a nurse should:
1. Give nitroglycerin
2. To impose venous harnesses on the limbs
3. start inhalation of oxygen
4. Enter strokentant intravenously
5. Enter Laziks intramuscularly
6. introduce prednisolone intramuscularly
The hemostatic harness is superimposed:
1. for arterial bleeding
2. With capillary bleeding
3. With venous bleeding
4. With parenchymal bleeding
When the bone turning bones, the tire is superimposed:
1. From the ray-taking joint to the top third of the shoulder
2. from the tips of the fingers to the upper third of the shoulder
3. From the base of the fingers to the upper third of the shoulder
With a turn of the shoulder bone, the tire is superimposed:
1. From the fingers to the blade from the sore side
2. from the fingers to the blade with a healthy side
3. From the ray-taking joint before the blade with a healthy side
With open fractures, transport immobilization is carried out:
1. First of all
2. secondly after stopping bleeding
3. In third time after stopping bleeding and imposing bandages
With a fracture of bones of the tire of the tire imposes:
1. From the fingertips to the knee
2. From the tips of the fingers to the upper third of the thigh
3. from the ankle joint to the upper third of the thigh
With a fracture of the hip, the tire is superimposed:
1. From the fingertips to the hip joint
2. From the fingertips to the armpit
3. from the lower third of the tibia to the armpit
The imposition of an airproof dressing when penetrating the injury of the chest is carried out:
1. directly on the wound
2. Open vatodymarlev
Prefigure help The patient with acute myocardial infarction includes the following activities:
1. Put
2. give nitroglycerin
3. provide full physical peace
4. Immediately hospitalize passing transport
5. if possible, introduce painkillers
Resuscitation must be carried out:
1. Only doctors and nurses of resuscitation offices
2. all specialists who have medical education
3. All adult population
Resuscitation shows:
1. In each case, the death of the patient
2. Only for sudden death Young patients and children
3. with suddenly developed terminal states
When drowning B. cold water Duration of clinical death:
1. Crocheted
2. extlives
3. Does not change
In the pre-reactive period of frostbite characteristic
1. pallor skin
2. no skin sensitivity
4. feeling numbness
5. Skin hyperemia
For a typical attack of angina characteristic:
1. zagalized Localization of Pain
2. Duration of pain for 15-20 minutes
3. duration of pain for 30-40 min
4. duration of pain for 3-5 min
5. effect of nitroglycerin
6. pain irradiation
The main sign of a typical myocardial infarction is:
1. Cold sweat and sharp weakness
2. Bradycardia or Tachycardia
3. Low blood pressure
4. breast pain lasting more than 20 minutes
The patient with myocardial infarction in the acute period may develop the following complications:
1. shock
2. acute heart failure
3. False acute belly
4. circulatory stop
5. Jet pericarditis
The atypical forms of myocardial infarction include:
1. abdominal
2. astmatic
3. cerebral
4. asymptomatic
5. Trimming
With abdominal form of myocardial infarction, pain can be felt:
1. in the epigastric area
2. in the right hypochondrium
3. in the left hypochondrium
4. wear a fit
5. All over the stomach
6. Below navel
For cardiogenic shock characteristic:
1. restless behavior of the patient
2. mental arousal
3. lost, zaming
4. reduced arterial pressure
5. pallor, cyanosis
6. cold sweat
Cardiac asthma clinic and lung edema develops at:
1. acute left vehicles
2. acute vascular failure
3. bronchial asthma
d) acute worldwide failure
Situational tasks:
Task 1. From the river is removed by a person without signs of life. The pulse and breathing are absent, the tones of the heart are not listened, the pupil is maximally expanded, there is no reaction to the light. Tell the sequence of the provision of EMF.
Answer:
Determine the signs of biological death and in their absence to create a "drainage position".
Start the complex "ABC".
Determine the criteria for the effectiveness of the resuscitation complex for every 2 minutes.
Ensure a call to the scene of the Resuscitation Brigade
Task 2.You found a person on the street without signs of life: there is no consciousness, there is no chest excursions, the pulse on the carotid artery is not torn. How to establish in which phase of the body's dying is the victim?
Answer:
Determine the presence of signs of biological death (drying of the corneal shell of the eye, the symptom of the "cat eye", the presence of a body stuffing, the presence of body spots); If you have the presence of a challenge to the scene of the SMP and law enforcement brigade.
Task 3.Going ahead of you a man suddenly cried and fell, visible convulsive twitching of the limbs at the time of your approach to it stopped. In case of inspection, hanging in his hand hanging from an electric pillar wire. What is the sequence of EMF in this situation?
Answer:
Observing personal safety rules to eliminate the effects of electric current on the injured body.
According to the testimony, proceed to the ABC complex.
Act according to the "EMF algorithm with a sudden death."
Task 4.In the garage, you found a man lying at the car with a working engine. When inspection: Against the background of the skin's pallor, bright red spots are visible on it, there is no breathing, the pulse is not determined, the pupils are wide, rare deaf heart tones are listened. What about the victim? Rate his condition. What events do you have to provide? Sequence EMF.
Answer:
1. Acute inhalation poisoning of exhaust gases of internal combustion engine.
2. The agonal period of the dying of the body.
3. Remove the victim from the garage to the open space.
4. Start the complex "ABC".
5. Ensure a call to the scene of the SPP specialized brigade.
Task 5.A man suddenly fell on the bus. Muscles of the face, neck, limbs are randomly reduced. The convulsions are accompanied by sharp turns of the body to the parties, a foam liquid was separated from the mouth, the face is a blue, thought-out, respiration is noisy, reinforced. After 3 minutes, the cramps disappeared, breathing is even, like a sleeper person, involuntary urination. What disease does a man suffer? What is dangerous paroxysm? The order of EMF in this situation.
Answer:
1. Epilepsy.
2. Renewing the seal with its transition to epileptic status.
3. Determine the presence of possible mechanical injuries at the time of the fall.
4. Ensure the passability of the upper respiratory tract; prevent the possibility of tongue bite; Specialized SMP brigade in the scene.
Task 6.A woman of 62 years old suddenly received the news of the death of her husband, screamed, lost consciousness, fell. The skin is pale, heart rate 92 per minute, blood pressure 100/60 mm RT Art, breathing deep, 15 per minute. What about the sick? Real EMF.
Answer:
1. fainting (if the loss of consciousness is no more than two minutes).
2. Ensure fresh air access, weaken the shy clothes.
3. Raise legs, sprayed with cold water.
4. If possible, to breathe a pair of ammonia alcohol.
5. In the presence of medicines to parenterally enter analgesics.
Task 7.3 hours after eating boiled mushrooms, all family members appeared abdominal pain, saliva, headache, vomiting, liquid stools. What happened? What is the order of EMF? Is stationary treatment, if hemodynamics have all the victims stable, within age norms?
Answer:
1. Enteral poisoning of poisonous mushrooms.
2. Give inside activated carbon on the background of abundant drinking with a callound of re-vomiting.
3. Call the SMP specialized brigade with the subsequent hospitalization of acrelated.
Task 8. In the toilet, the patient felt dizziness, followed by the loss of consciousness. Pale, covered with cold later, pulse 130 per minute of weak filling. In the toilet, a large amount of liquid is tiny color, with a sharp unpleasant reeling odor. Your estimated diagnosis? What is the reason for the occurrence of this state? The order of EMF.
Answer:
1. Collapse.
2. Gastrointestinal bleeding as a complication of peptic ulcer.
3. Inside to give pieces of ice, carry out cooling of the epigastric area.
4. Calling a SMP brigade for emergency hospitalization in surgical hospital, infusion therapy
Task 9.As a result of the bites of an unknown dog on her feet, a woman was found many ribbons wounds, moderately bleeding. What is the procedure for emergency medical care? Does an anti-execution vaccination need?
Answer:
1. Aseptic bandages on the wounds of the lower limbs with the temporary stop of bleeding.
2. Transportation in a traumatological point or surgical hospital with compulsory introduction of an anti-cancer vaccine according to the scheme.
Task 10.30 minutes after the start of the ABC complex, independent heart activities and respiration were not resumed. Pupils are wide, there is no reaction to the light, the symptom of the "cat eye" is not. What does the patient examination indicate? How do you do in this situation?
Answer:
1. The lack of signs of narrowing the pupil during the resuscitation complex for 30 minutes, as a cardinal criterion of efficiency, indicates the beginning of the biological death of the body.
Resuscitation activities in this situation must be discontinued due to the danger of the development of "social death" as a result of decortication
Topic 17. Organization of psychological and psychiatric assistance to the population and participants of the liquidation of consequences emergency situations. Deontological aspects in organizing and conducting medicine measures to eliminate the effects of emergency situations.
Content: The organization and results of the work of the Center for Psychological Assistance at the Emergencies Ministry (Moscow). The issues of ethics of workers of the QMS and MS GO in the admission, conducting medical sorting and medical care to victims in emergency. Relationship with victims, compliance with the principles of protecting the interests of victims. Providing optimal medical care to the victim. Good attitudes of the medical worker to traditions, rites and religious beliefs of victims. Relationships with third parties. Configuring confidentiality in relation to the victims.
Control questions:
1. Deontological aspects in organizing and conducting medical measures to eliminate the effects of emergency situations.
2. Organization of psychological and psychiatric assistance to the population and participants in the elimination of the effects of emergency situations
1. Sumin S.A., Rudenko M.V., Borodinov I.M. - Anesthesiology, resuscitation and intensive therapy - M.: MH of the Russian Federation, 2002. - p.
2. Sakno I.I., Sakhno V.I. Extreme medicine (organizational issues) / tutorial For students of higher medical and pharmaceutical educational institutions. - M.: GOU WONMTS MH RF, 2002. - 560 pp.
3. Zilber A.P. "Medicine of Critical States", Publisher
4. Petrozavodsky University, Petrozavodsk 1995.
5. Galkin R.A., Dvini S.I. Nursing in Surgery
6. Moscow, 1999
7. Negovsky V.A.s Sovt.Postrethniciasis - M, 1972
8. Order of the Ministry of Health of Russia of 04.03.03 No. 73 "On Approval
9. Instructions for the definition of criteria and the procedure for determining
10. Moments of the death of man, termination of resuscitation events "
11. Nursing business (under the editorship of Koteelnikova), Moscow, 2004, 2
12. Ryabov GS Critical state syndromes. "Medicine,". Moscow, 1994- 351 pages
13. Guidelines for anesthesiology and resuscitation, edited by Professor Yu.S. Polishina / \\ St. Petersburg, 2004
14. Federal Law of N 68-FZ dated November 11, 1994 "On the protection of the population and territories from natural and technogenic emergencies"
15. Trifonov S.V. Selected lectures on medicine disasters / Tutorial for students of higher medical schools. - M: Gootar-Med., 2010
16. Civil Defense: Tutorial / Ed. V.N. Zavyalova. - M. Medicine, 1989.
The list of resources of the information and telecommunication network "Internet" necessary for the development of discipline.
1. Electronic library system "BookFond" http://www.knigafund.ru
2. Electronic library system "Student Consultant" http://www.studMedlib.ru
3. Electronic library system "Yuratt" www.biblio-online.ru
4. Scientific electronic library http://elibrary.ru
5. Electronic Journal "Health" http://m.e.zdravohrana.ru/
6. Medical electronic library http://meduniver.com/medical/book/
7. Medical information and search site "Cell Navigator" http://www.mednavigator.ru/
8. Electronic Medical Library. Electronic versions Medical Literature http://www.booksmed.com/
The composition of the skin includes the following layers:
- epidermis ( outdoor skin);
- derma ( skin Connecting);
- hydrometer ( subcutaneous fabric).
Epidermis
This layer is superficial, providing the body a reliable protection against pathogenic environmental factors. Also, the epidermis is multi-layered, each layer of which is different in its structure. These layers provide continuous skin updates.The epidermis consists of the following layers:
- basal layer ( provides skin breeding process);
- whipped layer ( provides mechanical protection against damage);
- granular layer ( protects the seaside from the penetration of water);
- shiny layer ( participates in the process of cell orog);
- horny layer ( protects the skin from introducing pathogenic microorganisms into it).
Dermis
This layer consists of connective tissue and is located between the epidermis and hypoderma. Derma, due to the content of collagen and elastin fibers in it, gives the skin elasticity.The dermis consists of the following layers:
- popple layer ( includes loops of capillaries and nervous endings);
- mesh layer ( contains vessels, muscles, sweat and sebaceous glandsas well as hair follicles).
Hypodermis
This skin layer consists of subcutaneous fatty fiber. Fatty fabric accumulates and retains nutrients, thanks to which the energy function is performed. Also, the hypoderma is a reliable protection internal organs from mechanical damage.When burns, the following lesions of the layers of skin occur:
- surface or complete lesion of the epidermis ( first and second degree);
- surface or complete dermis lesion ( third A and third sec);
- defeat of all three layers of skin ( fourth degree).
It should also be noted that in burn lesions, the protective function of the skin is significantly reduced, which can lead to penetration of microbes and the development of infectious inflammatory process.
Blood leather system is well developed. The vessels passing through the subcutaneous fat fiber, reach the dermis, forming a deep skin-vascular network on the border. From this network, the blood and lymphatic vessels depart up to the dermis, nutrition of nerve endings, sweat and sebaceous glands, as well as hair follicles. Between the papilla and mesh layers, the second surface skin-vascular network is formed.
The burns cause a microcirculation violation, which can lead to dehydration of the body due to the massive movement of the fluid from the intravascular space in the output. Also, due to damage to the tissues, a liquid begins to flow out of small vessels, which subsequently leads to the formation of edema. With extensive burn wounds destruction blood vessels can lead to development burning Shock.
Causes of burns
 Burns may develop due to the following reasons:
Burns may develop due to the following reasons:
- thermal impact;
- chemical impact;
- electrical impact;
- radiation impact.
Thermal impact
Burns are formed due to direct contact with fire, boiling water or steam.- The fire. When exposed to fire, the face and upper respiratory tract are most often affected. With the burns of other parts of the body, difficulties arise in the removal of burnt clothing, which may cause the development of the infectious process.
- Boiling water. In this case, the burn area can be small, but quite deep.
- Couple. When exposed to steam in most cases, a shallow lesion of tissues occurs ( often amazed upper respiratory tract).
- Hot items. With damage to the skin with the help of hot objects at the site of exposure remains clear boundaries of the subject. These burns are deep enough and characterized by the second - the fourth degrees of the lesion.
- temperature of influence ( the higher the temperature, the stronger the defeat);
- the duration of exposure to the skin ( the longer the contact time, the heavier the degree of burn);
- thermal conductivity ( what it is higher, the stronger the degree of defeat);
- the condition of the skin and health of the victim.
Chemical impact
Chemical burns arise as a result of entering the skin of aggressive chemicals ( for example, acids, alkali). The degree of damage depends on its concentration and duration of contact.Burns due to chemical impact These may arise due to the effect on the skin of the following substances:
- Acids.The effect of acids on the surface of the skin causes shallow lesions. After exposure to the affected area, a burning crust is formed in a short time, which prevents the further penetration of acids into the skin.
- Caustic alkalis. Due to the effect of alkali eating on the surface of the skin, its deep defeat occurs.
- Salts of some heavy metals ( for example, silver nitrate, zinc chloride). Skin lesions by these substances in most cases cause surface burns.
Electrical impact
Electrical burns occur when contact with conductive material. Electric current applies to tissues with high electrical conductivity through blood, spinal fluid, muscles, to a lesser extent - through the skin, bone or fatty tissue. Dangerous man is a current when its value exceeds 0.1 A ( ampere).Electrical injuries are divided into:
- low-voltage;
- high-voltage;
- super-voltage.
Radiation impact
Burns due to radiation impact may be caused:- Ultraviolet radiation. Ultraviolet lesions of the skin mainly occur in the summer. Burns in this case are shallow, but characterized by a large area of \u200b\u200blesion. When exposed to ultraviolet, surface burns of the first or second degree often occur.
- Ionizing radiation. This impact leads to the defeat of not only skin, but also nearby organs and tissues. Burns in a similar case are characterized by a shallow defect.
- Infrared radiation. It may cause eye defeat, mainly retina and cornea, as well as skin. The degree of lesion in this case will depend on the intensity of the radiation, as well as on the duration of exposure.
The degree of burns
 In 1960, it was decided to classify burns on four degrees:
In 1960, it was decided to classify burns on four degrees:
- I degree;
- II degree;
- III-A and III-B degree;
- IV degree.
| Degree of burn | Development mechanism | Features of external manifestations |
| I degree | The surface lesion of the upper layers of the epidermis occurs, the healing of the burns of a given degree occurs without the formation of scars | hyperemia ( redness), swelling, pain, violation of the functions of the affected area |
| II degree | There is a complete defeat of the surface layers of the epidermis | Pain, formation of blisters containing inside transparent liquid |
| III-A | All layers of epidermis to the dermis are damaged ( derma can affect partially) | Dry or soft burn brake is formed ( scab) light brown |
| III-B | All layers of epidermis, dermis, as well as partially hypoderma are affected. | Dry dry brown brace brown |
| IV degree | All layers of leather, including muscles and tendons, are affected up to dice | It is characterized by the formation of a grinding crust of dark brown or black |
There is also a classification of the degrees of the crubich burn, which highlighted five degrees of the burn. This classification differs from the previous one that III-to the degree is called the fourth, and the fourth degree - fifth.
The depth of damage during burns depends on the following factors:
- the nature of the thermal agent;
- the temperature of the active agent;
- the duration of exposure;
- the degree of heating of deep layers of the skin.
- Surface burns. These include burns of the first, second and third and degree. These lesions are characterized by the fact that they are capable of independently, without surgery to heal full, that is, without the formation of a scar.
- Deep burns. These include burns of the third-b and fourth degree, which are not capable of full-fledged independent healing ( there is a rough scar).
Symptoms of burns
 Localization highlights burns:
Localization highlights burns:
- persons ( in most cases, leads to eye damage);
- scalp;
- upper respiratory tract ( there may be pain, voice loss, shortness of breath, as well as cough with a small amount of sputum or cooty residences);
- upper and lower extremities ( when burns in the joints, there is a risk of limb functions);
- torso;
- crotch ( can lead to disorder of the operational organs).
| Degree of burn | Symptoms | Photo |
| I degree | With a given degree of burn, redness, swelling and pain is observed. The skin at the place of lesion of bright pink color, sensitive when the touch and slightly protrudes over a healthy skin area. Due to the fact that with a given degree of burn, only the surface lesion of the epithelium occurs, the skin in a few days, harsh and wrinkling, forms only a small pigmentation, which independently passes after a while ( on average for three to four days). |  |
| II degree | With a second degree of burn, as well as at the first, there is a hyperemia, swelling, as well as a pain of a burning character. However, in this case, due to the pinch of the epidermis on the surface of the skin, small and unknown blisters filled with light yellow, transparent liquid appear. In case the blisters are revealed, the erosion of reddish color is observed in their place. Healing of this kind of burns occurs on its own on the tenth - twelfth day without the formation of scars. |  |
| III-A | In the burns of this degree, the epidermis and partially dermis are defeated ( hair bulbs, hasty and sweat glands are saved). Nursing the necrosis of tissues, as well as, due to pronounced vascular changes, there is a spread of edema to the entire thickness of the skin. With a third-agree, dry light brown or soft white-gray burn crust is formed. Tactful-pain sensitivity of the skin is preserved or reduced. On the affected skin surface, bubbles are formed, the dimensions of which vary from two centimeters and above, with a dense wall filled with a thick jelly-like yellow liquid. Epithelization of the skin on average last four to six weeks, however, when the inflammatory process appears, healing can last for three months. |
|
| III-B | With the third-b burns, necrosis struck the whole crowd of epidermis and dermis with partial seizure of subcutaneous fatty fiber. With a given degree, there is a formation of bubbles filled with hemorrhagic fluid ( with strengths of blood). The resulting burn crust is dry or wet, yellow, gray or dark brown. There is a sharp decline or absence of pain. Independent healing of wounds does not occur at a degree. | |
| IV degree | With the fourth degree burns, not only all layers of skin, but also muscles, fascia and tendons are affected up to the bones. On the affected surface, the burn crust of dark brown or black color is formed, through which the venous network is viewed. Due to the destruction of nervous endings, there is no pain at this stage. At this stage, there is a pronounced intoxication, there is also a high risk of the development of purulent complications. |  |
Note: In most cases, when burning the degree of lesion is often combined. However, the severity of the patient's condition depends not only on the degree of burn, but also from the area of \u200b\u200bthe lesion.
Burns are divided into extensive ( defeat 10 - 15% of the skin and more) and unconditional. With extensive and deep burns with surface lesions of skin more than 15 - 25% and more than 10% with deep lesions, a burn disease may occur.
Burning disease is a group clinical symptoms With thermal lesions of the skin, as well as nearby fabrics. It occurs in the massive destruction of tissues with the release of a large number of biologically active substances.
The severity and course of the burn disease depends on the following factors:
- age of the victim;
- burn location;
- the degree of burn;
- defeat area.
- burn shock;
- burning toxemia;
- burning septicotoxemia ( burn infection);
- reconvation ( restoration).
Burn shock
The burn shock is the first period of burn disease. The duration of the shock is from several hours to two to three days.The degree of burning shock
| First degree | Second degree | Third degree |
| It is characteristic of burns with leather damage not more than 15 - 20%. At a given degree, a burning pain is observed on the affected areas. Heart frequency up to 90 shots per minute, and blood pressure within the normal range. | It is observed in burns with a lesion of 21 - 60% of the body. The frequency of heart abbreviations in this case is 100 - 120 shots per minute, blood pressure and body temperature are reduced. For the second degree, the feeling of chills, nausea and thirst are also characteristic. | For the third degree of burning shock, the defeat of more than 60% of the body surface is characteristic. The state of the victim in this case is extremely severe, the pulse is practically not tested ( filiform), blood pressure 80 mm RT. Art. ( millimeters of mercury pillar). |
Burn toxmia
Acute burning toxemia is due to the effect on the body of toxic substances ( bacterial toxins, protein decay products). This period begins from the third to the fourth day and continues within one to two weeks. It is characterized by the fact that the victim is observed inxication syndrome.For intoxication syndrome, the following features are characterized:
- increase body temperature ( up to 38 - 41 degrees with deep lesions);
- nausea;
- thirst.
Burning septicotoxide
This period conditionally begins with the tenth days and continues until the end of the third - fifth week after injury. It is characterized by accession to the affected area of \u200b\u200binfection, which leads to the loss of proteins and electrolytes. With a negative dynamics, it can lead to the depletion of the body and the death of the victim. In most cases, this period is observed in the burns of the third degree, as well as at deep lesions.The following symptoms are characterized for burn septicotoxmia:
- weakness;
- increasing body temperature;
- chills;
- irritability;
- the jaggility of the skin and scool ( with the damage to the liver);
- pulse increase ( tachycardia).
Reconvision
In case of successful operational or conservative treatment There comes healing of burn wounds, restoration of the internal organs and recovery of the patient.Definition of burns of burns
 In the assessment of the gravity of thermal defeat, in addition to the depth of burn, its area has its importance. In modern medicine, several ways to measure burn areas are used.
In the assessment of the gravity of thermal defeat, in addition to the depth of burn, its area has its importance. In modern medicine, several ways to measure burn areas are used. The following methods for determining the burnt area are distinguished:
- rule nine;
- palm rule;
- method Postnikov.
Rule nine
The simplest and affordable way to determine the burn area is considered "Rule of nines". According to this rule, almost all parts of the body are conditionally divided into equal sections of 9% of the total surface of the entire body.| Rule nine | Photo |
| Head and Neck 9% |  |
| Upper limbs (each hand) 9% |
|
| The front surface of the body18% (9% chest and belly) |
|
| Rear surface torso18% (upper back and lower back 9%) |
|
| lower limbs ( each leg) 18% (hip 9%, shin and stop 9%) |
|
| Crotch 1% |
Palm rule
Another method of determining the area of \u200b\u200bthe burn is the "Rule of Palm". The essence of the method lies in the fact that the area of \u200b\u200bthe palm of the burnt is taken in 1% of the area of \u200b\u200bthe entire body surface. This rule is used for small burns.Method Postnikov
Also in modern medicine uses a method for determining the area of \u200b\u200bthe burn in the postal service. For measuring burns, sterile cellophane or gauze is used, which is applied to the affected place. On the material indicate the contours of the burnt places, which are subsequently cut and impose on a special millimeter paper to determine the burn area.First assistance in a burn
 First assistance in burns is the following actions:
First assistance in burns is the following actions:
- elimination of the source of the existing factor;
- cooling of burnt areas;
- overlay aseptic dressing;
- anesthesia;
- call ambulance.
Eliminating the source of the current factor
To do this, the victim should be removed from the fire, put out burning clothes, stop contact with hot objects, liquids, ferry, etc. The faster this assistance will be provided, the less burns will be the depth.Cooling burned areas
It is necessary as quickly as possible to process the place of the burn with running water for 10 to 15 minutes. Water should be the optimal temperature - from 12 to 18 degrees Celsius. This is done in order to prevent the process of damage to healthy fabrics located next to the burn. Moreover, cold running water leads to a spasm of vessels and to reduce the sensitivity of nerve endings, and therefore, it has an anesthetic effect.Note:with the burns of the third and fourth degree, this first aid event is not produced.
Overlay aseptic dressing
Before applying aseptic dressing, it is necessary to gently cut clothes from burnt areas. In no case can you try to clean the burned areas ( remove the cliffs of clothing, resin, bitumen, etc.), as well as open bubbles. It is not recommended to lubricate the burned areas with vegetable and animal fats, solutions of mangartean or green.Dry and clean scarves, towels, sheets, sheets can be used as aseptic dressing. Aseptic bandage must be applied to a burn wound without preprocessing. If the fingers of the hands or legs were affected, it is necessary to pave an additional cloth between them to avoid gluing the skin of the skin among themselves. To do this, you can use a bandage or a pure handkerchief, which before overlaying should be wetted with cool water, and then squeeze.
Anesthesia
In case of severe pains during the burn, adhesive drugs should be taken, for example, ibuprofen or paracetamol. To achieve fast therapeutic effect It is necessary to take two pills ibuprofen in 200 mg or two paracetamol tablets of 500 mg.Ambulance call
There are the following testimony in which you need to call an ambulance:- with the burns of the third and fourth degree;
- in the event that a second degree burn in the area exceeds the size of the victim's palm;
- with the first degree burns, when the affected area is more than ten percent of the body surface ( for example, the whole area of \u200b\u200bthe abdomen or the entire upper limb);
- with damage to such parts of the body as a face, neck, joints, brushes, feet, or crotch;
- in the event that after the burn, nausea or vomiting appears;
- when after the burn is prolonged ( more than 12 hours) an increase in body temperature;
- with a worsening of the state on the second day after the burn ( strengthening pain or more pronounced redness);
- in case of numbness of the affected place.
Treatment of burns
Burn treatment can be two types:- conservative;
- operative.
- lesion area;
- depth of the lesion;
- localization of the lesion;
- the reason that caused the burn;
- development of burn disease in the victim;
- the age of the victim.
Conservative treatment
 It is used in the case of treating superficial burns, as well as this therapy is used before and after surgery in the case of deep lesions.
It is used in the case of treating superficial burns, as well as this therapy is used before and after surgery in the case of deep lesions. Conservative burning treatment includes:
- closed method;
- open method.
Closed method
This method treatment is characterized by imposing on the affected areas of the skin of the dressings with medicinal substance.
| Degree of burn | Treatment |
| I degree | In this case, it is necessary to impose a sterile bandage with anti-foam ointment. Usually, the replacement of the bandage is not required, since with the first degree of burn, the affected areas of the skin are healing for a short time ( up to seven days). |
| II degree | With a second degree on a burn surface, bandages with bactericidal ointments are superimposed ( for example, Levomecol, Silvacin, Dioxisol), which act oppressively on the livelihood of microbes. These dressings must be changed every two days. |
| III-A | With lesions of a given degree on the surface of the skin, a burn crust is formed ( scab). The skin around the resulting stamp must be treated with hydrogen peroxide ( 3% ), furacilin ( 0.02% water or 0.066% alcohol solution ), chlorhexidine ( 0,05% ) or other antiseptic solution, after which the sterile bandage should be applied. After two to three weeks, the burnive crust disappears and on the affected surface it is recommended to apply bandages with bactericidal ointments. Full healing of the burn wound in this case occurs approximately a month later. |
| III-B and IV degree | Under these burns, local treatment is applied with only the goal of accelerating the burning crust reassembly process. On the affected skin of the skin daily should be imposed bandages with ointments and antiseptic solutions. Burn healing in this case is only after surgery. |
There are the following advantages of a closed method of treatment:
- imposed dressings prevent infection of the burn wound;
- the bandage protects the damaged surface from damage;
- used medicinal products Microbes kill, and also contribute to the rapid healing of the burn wound.
- change the dressing provokes painful feelings;
- the dissolution of necrotic tissues under the bandage leads to an increase in intoxication.
Open method
For this method of treatment, the use of special equipment is characterized ( for example, ultraviolet irradiation, air cleaner, bacterial filters), which is only in specialized branches burn hospitals.
Open method of treatment is aimed at the accelerated formation of a dry burn crust, since soft and wet strateps is a favorable medium for reproducing microbes. In this case, two - three times a day various antiseptic solutions are applied to the damaged surface of the skin ( for example, diamond green ( zelenk) 1%, potassium permanganate ( manganese) 5% ), after which the burn wound remains open. In the ward, where the victim is located, the air is continuously cleaned by bacteria. These actions contribute to the formation of a dry stamp for one - two days.
According to this method, in most cases, facial, neck and crotch burns are treated.
There are the following advantages open fashion Treatment:
- contributes to the rapid formation of a dry stamp;
- allows you to observe the dynamics of tissue healing.
- loss of moisture and plasma from the burn wound;
- high cost of the method of treatment.
Operational treatment
 During burns, the following types of operational interventions can be applied:
During burns, the following types of operational interventions can be applied:
- necrotomy;
- necrectomy;
- page necrectomy;
- limb amputation;
- skin transplantation.
This operational intervention lies in the dissection of the resulting stamp with deep burning lesions. Necotomy is made urgently to ensure blood supply to fabrics. In case this intervention is not made in a timely manner, necrosis of the affected area can develop.
Nekratectomy
Necritomy is produced in the third degree burns in order to remove non-viable tissues with deep and limited lesions. This type of operation allows you to thoroughly clean the burn wound and prevent valuable processes, which contributes to the rapid healing of tissues.
Page necrectomy
This operational intervention is performed with deep and extensive skin lesions. However, the stage necratetomy is a more gentle intervention method, since the removal of non-viable tissues is made in several stages.
Ammputation limbs
The limb amputation is made in severe burns when treatment by other methods did not bring positive results or the development of necrosis, irreversible changes in tissues with the need for subsequent amputation, has occurred.
These methods of operational intervention allow:
- clean the burn wound;
- reduce intoxication;
- reduce the risk of complications;
- reduce the duration of treatment;
- improve the process of healing damaged tissues.
Skin transplantation
Skin transplantation is performed in order to close the burn wounds of large sizes. In most cases, autoplasty is produced, that is, its own skin of the patient from other parts of the body is transplanted.
Currently, the most widely applies the following ways to closing burn wounds:
- Plastic with local fabrics. This method is used for deep burning losses of small sizes. In this case, borrowing is borrowing to the affected area of \u200b\u200bneighboring healthy tissues.
- Free skin plastic.It is one of the most common skin transplant methods. This method is that with the help of a special tool ( dermatoma) At the affected body of a healthy body ( for example, thigh, buttock, belly) The necessary flap of the skin is excised, which is subsequently superimposed on the affected area.
Physiotherapy
Physiosocations are applied by B. complex treatment Burning wounds and are directed to:- oppression of the livelihood of microbes;
- stimulating blood flow in the exposure site;
- acceleration of the regeneration process ( recovery) damaged skin area;
- prevention of sub-scarring formation;
- stimulating the body's protective forces ( immunity).
| Type of physiotherapy | Mechanism of therapeutic action | Application |
| Ultrasound therapy
| Ultrasound, passing through the cells, launches chemical and physical processes. Also, acting locally, it helps to increase the body's resistance. | This method It is used to resolve the resulting scars and enhance immunity. |
| Ultraviolet irradiation
| Ultraviolet radiation Promotes the absorption of oxygen with tissues, increases local immunity, improves blood circulation. | This method is used to speed up the processes of regeneration of the affected skin. |
| Infrared irradiation
| Due to the creation of the thermal effect, this exposure contributes to improved blood circulation, as well as stimulating metabolic processes. | This treatment is aimed at improving the tissue healing process, and also produces an anti-inflammatory effect. |
Prevention of burns
 Solar burn is a common thermal lesion of the skin especially in the summer period.
Solar burn is a common thermal lesion of the skin especially in the summer period. Prevention of sunburn
In order to avoid solar burns, the following rules must be followed:- Direct contact with the Sun in the period from ten to sixteen hours should be avoided.
- In particularly hot days, it is preferable to wear dark clothes, as it is better than white things protects the skin from the sun.
- Before entering the street, it is recommended to apply sunscreen to open areas.
- During sunbathing, the use of a sunscreen is a mandatory procedure that needs to be repeated after each bathing.
- Since sunscreens have different protection factors, they need to be selected to a specific skin phototype.
- scandinavian ( first Phototype);
- flooking European ( second phototype);
- black Middle Eastern ( third phototyp);
- mediterranean ( fourth Phototype);
- indonesian or Middle Affairs ( fifth phototyp);
- african American ( sixth PhotoTip).
Prevention of household burns
According to statistics, the overwhelming part of burns arises in domestic conditions. Pretty often burned children who suffer because of the inattention of parents. Also, the cause of burns in domestic conditions is non-compliance with security rules.To avoid burns on living conditions, the following recommendations must be performed:
- Do not use electrical appliances with damaged isolation.
- Turning off the electrical appliance from the outlet, do not pull the cord, it is necessary to hold the base of the fork directly.
- If you are not a professional electrician, you should not repair the electrical appliances and wiring.
- Do not use electrical appliances in the raw room.
- Do not leave children without attention.
- It is necessary to ensure that there were no hot objects in the access zone of children ( for example, hot food or liquid, outlet, included iron, etc.).
- Those objects that can lead to burns ( for example, matches, hot objects, chemicals and others), should be kept away from children.
- It is necessary to conduct clarification activities with older children regarding their safety.
- It should be abandoned smoking in bed because it is one of frequent reasons fires.
- It is recommended to establish fire alarms throughout the house or at least in those places where the likelihood of ignition is higher ( for example, in the kitchen, room with fireplace).
- It is recommended to have a fire extinguisher in the house.
Read also ...
- The work of "Alice in Wonderland" in a brief retelling
- That transformation. "Transformation. Attitude towards the hero from the sister
- Tragedy Shakespeare "King Lear": the plot and the history of the creation
- Gargantua and Pantagruel (Gargantua et Pantagruel) Francois Rabl Gargantua and Pantagruel Brief