Scientific electronic library. Scientific Electronic Library Anti-Local Events at the Stages of Medical Evacuation
Traumatic shock - the response of the body into a heavy mechanical injury, accompanied by a violation of all functions in the body.
Epidemiology.
The frequency of traumatic shock in the wounded in modern conditions of conducting hostilities increases, reaching 25%. The shock for multiple and combined damage is met in 11-86% of victims, which averages 25-30% of all accidents. Etiology.Most frequent reasons development of traumatic shock: - damage to the pelvis, chest, lower extremities; - Damage internal organs; - Open damage with an extensive scramble of soft tissues when the limbs are separated. Shock may occur with a varied combination of damage and even with multiple heavy bruises.
Pathogenesis.
As a result of severe injury or injury, one or several (with multiple or combined injuries) of foci of damage to fabrics or organs is formed. At the same time, vessels of various caliber are damaged - bleeding occurs , an irritation of an extensive receptor field occurs - a massive afferent impact on the central nervous system, the more or less extensive volume of tissues is damaged, their decay products are absorbed into blood - endotoxicosis occurs.
In case of damage to the vital organs, there is a violation of the corresponding vital functions: damage to the heart is accompanied by a decrease in the contractile function of myocardium; lung damage - decrease in pulmonary ventilation; Damage to the pharynx, larynx, trachea - asphyxia.
As a result of these pathogenetic factors on an extensive afferent receptor apparatus and directly on organs and tissues, a non-specific adaptation program for the protection of the body is launched. The consequence of this is the release of adaptation hormones into the blood: ACTH, cortisol, adrenaline, norepinephrine.
There is a generalized spasm of capacitive vessels (veins), providing the release of blood reserves from the depot - up to 20% of the BCC; Generalized spasm Arteriole leads to centralization of blood circulation and contributes to the spontaneous stop of bleeding; Tachycardia ensures that the proper blood circulation is maintained. If the severity of injury and blood loss exceed the protective capabilities of the body, and medical care is delayed - hypotension and tissue hypoperfusion develop , being clinical and pathogenetic characteristics of traumatic shock III degree.
Thus, the mechanism for the development of traumatic shock monoethiological (injury), but polypatogenetic (bleeding, endotoxicosis, damage to vital organs, afferent impact on the central nervous system), in contrast to hemorrhagic shock (for example, with crushing wounds with damage to large vessels) where the pathogenetic factor is one - the sharp blood loss.
Diagnosis and classification of traumatic shock.
During the traumatic shock, two phases are distinguished: erectile and torpid.
- Erectile phase Relatively short. Its duration ranges from a few minutes to several hours. Patient in consciousness, troubled. Motive and speech excitement. Violated the criticism of the assessment of your own state. Pale. Pupils of ordinary sizes, the reaction to the light is alive. Pulse of good quality, rapidly. Blood pressure within the normal range. Increased pain sensitivity and skeletal muscle tone.
- Thorpid phase The shock is characterized by the oppression of vital functions of the body and, depending on the severity of the flow divided by three degrees:
— shock I degree. Consciousness is preserved, there are easy inhibition and slowness of the reaction. Pain reaction is weakened. Skin pale, acrocyanosis. Pulse of good quality, 90-100 per minute, systolic blood pressure 100-90 mm Hg. Light tachipne. Skeletal muscles tone reduced. Diuresis is not broken.
— shock II degree. By clinical picture It is similar to a shock of I degree, but is characterized by a more pronounced oppression of consciousness, a decrease in pain sensitivity and muscle tone and significant impairment of hemodynamics. Pulse of weak filling and voltage - 110-120 per minute, maximum blood pressure 90-70 mm Hg.
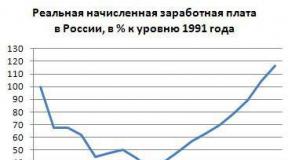
— shock III degree. Consciousness is darkened, the patient sharply slow down, the reaction to external stimuli is noticeably weakened. Skin covers pale gray, with a blue tint. Pulse of weak filling and voltage, 130 per minute and more. Systolic blood pressure 70 mm Hg. And below. Surface breathing, frequent. Muscular hypotension, hypotlexia, decreased diurea, up to Anuria. A large diagnostic value in determining the degree of shock is played by the Almeda index: the ratio of the heart rate to the level of systolic blood pressure. It is possible to approximately determine the degree of shock and the size of the bloodsture (Table 3).
Shoka Index
The late elimination of the reasons for supporting and deepening traumatic shock prevents the restoration of the vital functions of the body, and the III shock of the degree can go to the terminal state, which is the extreme degree of oppression of vital functions passing into clinical death.
Principles of medical care:
- the urgent nature of the provision medical care for traumatic shock, due to the threat of irreversible consequences of critical disorders of vital functions and, above all, circulatory disorders, deep hypoxia.
- the feasibility of a differentiated approach
in the treatment of wounded in a state of traumatic shock. Treated should not shock as
Such, not a "typical process" or "specific pathophysiological reaction". The anti-coaxing assistance turns out to be concrete wounded with hazardous violations of vital activity, which is based on severe injury ("Morphological substrate" of shock) and, as a rule, sharp blood loss. Pronounced circulatory disorders, respiration and other vital functions are caused by severe morphological damage to vital organs and organism systems. This position in severe injuries acquires the meaning of the axioms and aims the doctor to urgently search for a specific cause of traumatic shock. Surgery with shock is effective only with the rapid and accurate diagnosis of localization, nature and severity of damage.
- leading value and emergency surgical treatment with traumatic shock. The anti-shifting assistance is simultaneously an anesthesiologist-resuscitation and surgeon. From effective action The first depends fast recovery and maintenance of passability respiratory tract, gas exchange as a whole, the beginning of infusion therapy, anesthesia, medical support for cardiac activity and other functions. However, pathogenetic meaning has urgent surgical treatment, eliminating the cause of the traumatic shock - stopping bleeding, eliminating the tense or open pneumothorax, elimination of the tamponade of the heart, etc.
Thus, the current tactics of active surgical treatment of the seriously edged occupies a central place in the program of anti-shock events and does not leave the place to the outdated thesis - "First bring out of the shock, then operate." A similar approach proceeded from incorrect ideas about traumatic shock as a purely functional process with predominant localization in the central nervous system.
Anti-shock events at the stages of medical evacuation.
The first and prefiguration assistance includes:
- Stop outdoor bleeding by temporary methods, to the wounds to impose aseptic bandages.
- Analgesic injection with syringe - Tubes.
- Immobilization of fractures and extensive damage by transport tires.
- Elimination of mechanical asphyxia (exemption of the upper respiratory tract, overlaying an occlusal bandage with pneumothorax).
- Early start of infusion of bloodstream solutions using field disposable plastic infusion systems.
- The priority careful transportation was injured for the next stage.
First medical care.
The wounded in the traumatic shock should first be directed into the dressing room.
Anti-slip assistance should be limited to the necessary minimum of urgent measures, so as not to delay the evacuation into a medical institution where surgical and resuscitation assistance can be provided. It should be understood that the purpose of these events is not to eliminate from shock (which is impossible under conditions under conditions), but stabilization of the state of the wounded for further priority evacuation.
Causes revealed in the dressing heavy condition The wounded and implement measures to eliminate them. With acute respiratory disorders — the asphyxia is eliminated, external breathing is restored, sealed pleural cavity With an open pneumothorax, a pleural cavity is drained with a strained pneumothorax, inhalation of oxygen is carried out. With outer bleeding, its temporary stop is performed, and in the presence of a hemostatic harness - a harness is controlled.
An intravenous infusion is carried out 800-1200 ml of crystalloid solution (Mafusol, lactasol, 0.9% solution of sodium chloride, etc.), and with massive blood loss (2 l and more), additional infusion of the colloidal solution (polyglyukin, etc.) in the amount of 400 -800 ml. Infusion continues in parallel with the implementation of medical measures and even during the subsequent evacuation.
The obligatory anti-deposit event of the first medical care is anesthesia. All wounded with traumatic shock are introduced narcotic analgesics. However, the best method of anesthesia is novocaine blocks. Transport immobilization is monitored. When internal bleeding, the main task of the first medical care is the organization of immediate evacuation of the wounded to the stage of providing qualified or specialized medical care, where it will be implemented by an emergency operation to eliminate the source of bleeding.
Qualified and specialized assistance.
The wounded with the signs of the shock should first be sent to the operating room for emergency operations (asphyxia, tamponade of the heart, stressful or open pneumothorax, continuing internal bleeding, etc.) either in the ward of intensive therapy for the wounded - in the absence of indications for an emergency operation ( To eliminate disorders of vital functions, preparation for the performance of urgent surgical interventions or evacuation).
In the wounded, in need of urgent operations, the anti-slip therapy should begin in the receiving and sorting department and continue under the leadership of the anesthesiologist-resuscitator simultaneously with the implementation of surgical intervention. In the future, after surgery, the anti-mask therapy is completed in the ward of intensive therapy. The average dedication period of the wounded from the state of the shock at war is 8-12 hours. At the stage specialized assistance After removing from the shock, the wounded with the terms of treatment not exceeding 60 days is carried out a full course of treatment. The rest of the wounded evacuate into the rear hospital.
Traumatic shock is an acutely developing due to injury, a polypatogenetic pathological process, characterized by significant violations of the functions of life support systems, primarily blood circulation, against the background of the extreme voltage of regulatory (adaptation) mechanisms of the body. Traumatic shock is one of the manifestations of the acute period of traumatic disease. The polyethology of the traumatic shock is determined by the fact that its formation occurs as a result of the interaction of circulatory disorders caused by blood loss; disorders of the pulmonary and tissue gas exchange; the organism poisoning with products of destroyed tissues and impaired metabolism, as well as toxins of microbial origin; powerful stream of neuroral impulses from the damage zone in the brain and endocrine system; violations of the function of damaged vital organs.The main link pathogenesis of traumatic shock are primary disorders of microcirculation. Acute insufficiency of blood circulation, lack of perfusion of tissues with blood leads to inconsistencies between reduced microcirculation capabilities and energy needs of the body. At traumatic shock, in contrast to other manifestations of the acute period of traumatic disease, hypovolemia due to bloodstures is the lead, although not the only reason for hemodynamic violations.
An important factor determining the state of blood circulation is the work of the heart. For most victims with severe injuries, the development of a hypendynamic type of blood circulation is characteristic. With a favorable course, its permanent volume after injury can remain elevated throughout the acute period of traumatic disease. This is explained by coronary artery Not involved in general vascular spasm, it remains satisfactory venous return, cardiac activity is stimulated through vascular chemoreceptors of unsophisticated exchange products. However, with a preserving hypotension, after 8 hours after injury, a single and minute heart performance in patients with traumatic shock can decrease by about twice as compared to the norm. The increase in the heart rate and the total peripheral resistance of the vessels is not able to maintain a minute volume of blood circulation on normal values \u200b\u200b(Pashkovsky E.V. et al., 2001).
Inadequate cardiac ejection At traumatic shock is due to the depletion of urgent coping mechanisms due to the hypoxia of myocardium, the development of metabolic disorders in it, a decrease in the content of catecholamines in myocardium, a decrease in its reaction to sympathetic stimulation and catecholamines circulating in the blood. Thus, the progressive decrease in one-time and minute performance of the heart will be a reflection of developing heart failure, even in the absence of direct damage (injury) of the heart (V.V. Timofeev, 1983).
Another main factor determining the state of blood circulation is the tone of the vessels. A regular reaction to injury and blood loss is the strengthening of the functions of a limbico-reticular complex and a hypothalamic-adrenal system. As a result, the traumatic shock includes urgent compensatory mechanisms aimed at maintaining blood circulation of vital organs. One of the compensation mechanisms is to develop a common vascular spasm (first of all arterioles, metharcyteries and prokapillary sphincters) aimed at emergency decrease in the capacity of the vascular bed and bring it into line with the BCC. The total vascular reaction does not apply only on the artery of the heart and brain, which are practically deprived of? -Adrenoreceptors implementing the vasoconstrictor effect of adrenaline and norepinephrine.
The mechanism of urgent compensation, also aimed at eliminating the inconsistency between the BCC and the capacity of the vascular bed, is autogriego. In this case, the reinforced movement of the fluid from the interstitial space in the vascular is. The fluid yield in interstics occurs in functioning capillaries, and its entry goes to non-functioning. Together with interstitial liquid in capillaries penetrate the products of anaerobic metabolism, which reduce sensitivity? -Adrenororeceptors to catecholaminams. As a result, non-functioning capillaries expand, and functioning, on the contrary, narrow. With a shock due to an increase in the concentration of adrenaline and norepinephrine, the ratio between the functioning and non-functioning capillaries is dramatically changed in favor of the latter. Thus, conditions are created to increase the reverse current of the fluid into the vascular channel. Autohemodiliation is also amplified by the dominance of oncotic pressure not only in venular (as under normal conditions), but also in the arterilar ends of functioning capillaries due to a sharp decrease in hydrostatic pressure. The mechanism of autoghemodilia is quite slow. Even with bloodwall exceeding 30-40% OCC, the rate of flow of fluid from an interstice into the vascular channel does not exceed 150 ml / h.
In the reaction of urgent compensation of blood loss, a renal mechanism of water and electrolyte delay has a certain meaning. It is associated with a decrease in the filtering of the primary urine (decrease in filtration pressure in combination with spasm of renal vessels) and an increase in the reabsorption of water and salts in the tubing apparatus of the kidneys under the action of antidiuretic hormone and aldosterone.
In the exhaustion of the above-described compensation mechanisms, microcirculation disorders are progress. Intensive selection of histamine damaged and stylish tissues, bradykinin, lactic acid, possessing vasodilative action; admission from the intestine of microbial toxins; reduction due to hypoxia and acidosis sensitivity of smooth muscle elements of vessels nervous influences and catecholamines lead to the fact that the phase of vasoconstriction is replaced by the phase of vasodilation. There is a pathological deposit of blood in those who have lost the tone of metharrioles and extended capillaries. Hydrostatic pressure in them increases and becomes more oncotic. Due to the influence of endotoxins and hypoxia of the vascular wall itself, its permeability increases, the liquid part of the blood leaves in interstics, the phenomenon arises " internal bleeding" The instability of hemodynamics, violation of the tone of the vessels due to damage to the regulatory function of the brain in such a form of an acute period of traumatic disease, as a traumatic coma (severe crank-brain injury, the injury of a severe brain) usually develop later - by the end of the first day.
An important link of pathogenesis of traumatic shock, even with non-cleaning injury, is an acute respiratory failure. In character, it is usually parenchymal and ventilation. The most typical manifestation is the progressive arterial hypoxemia. Reasons for the development of the latter are the weakness of respiratory muscles under conditions of circulatory hypoxia; pain "brake" breathing; Embolization of the microShosudes of the lungs due to intravascular coagulation, fat globul, the yatrogenation of transfusions and infusions; interstitial pulmonary edema due to increasing the permeability of the membranes of microscopes of endotoxins, hypoxia of the vascular wall, hypoproteinemia; Microelectsization due to reducing the formation and reinforced destruction of the surfactant. The predisposition to the atelectasis, the tracheoobronchitis and pneumonia is exacerbated by the aspiration of blood, gastric content, increasing the release of mucus with bronchial glands, the difficulty of flipping against the background of insufficient blood supply to the tracheobronchial tree. The combination of pulmonary, hemic (due to anemia) and circulatory hypoxia is a key point of traumatic shock. It is hypoxia and tissue hypoperfusion that determine the metabolic disorders, immune status, hemostasis, lead to increasing endotoxicosis.
In victims with severe breast injury (multiple fractures of ribs, the formation of the rib valve, a tense pneumothorax, injury injury) in combination with a non-heavy trauma of other anatomical regions, the acute period of traumatic disease is primarily a sharp respiratory failure. For such victims, normal numbers of systolic blood pressure (more than 100 mm Hg) are characterized in combination with a decrease in hemoglobin saturation arterial blood Oxygen is less than 93%, subcutaneous emphysens, intense pneumothorax, cyanosis of the skin. In addition, when admitted, the patient's contingent has an increase in the fibrinolytic activity of blood due to the activation of the plasminine system as a result of damage to the lung tissue. The predominance of hypercoagulation with the consumption of antosverting factors in arterial blood over venous against the background of the oppression of fibrinolytic activity plays a significant role in the pathogenesis of respiratory distress syndrome.
The role of nociceptive impulsation in the etiopathogenesis of traumatic shock is also very significant. It is based on the basis of the flow of nociceptive impulses, a stress reaction of the body is largely formed in response to injury. In its genesis, afferent impulse with inter -ceptor is also essential. of cardio-vascular system, especially with a decrease in the BCC caused by acute massive blood loss.
The deepening of metabolic disorders, microcirculation disorders during traumatic shock is associated with endotoxicosis, which begins to appear after 15-20 minutes. After injury or injury. Optional and obligate endotoxins are medium molecular polypeptides (simple and complex peptides, nucleotides, glycopeptides, humoral regulators, derivatives of glucuronic acids, fragments of collagen and fibrinogen). The middle molecules pool is an important, but not the only supplier of toxic substances. The final toxic properties have finite spree products of protein, especially ammonia. Endotoxicosis is also determined by free hemoglobin and myoglobin, peroxide compounds. The immunoreaction arising from shock is not only protective, but can also act as a source of toxic substances, such as pro-inflammatory cytokines (protein or polypeptide compounds produced by activated cells immune system) - Interleukin-1, tumor necrosis factor, etc.
The essence of immune disorders during traumatic shock is associated with the extremely high risk of early development of immune failure. For traumatic shock, an unprecedented high antigenemia from the foci of alteration of fabrics is characteristic. The barrier function of local inflammation is lost, and its mediators (pro-inflammatory cytokines) come into systemic blood flow. Under these conditions, the adaptation reaction of the immune system should be the so-called "preimmune response" when the level pro-inflammatory cytokines It is finely controlled by the production of anti-inflammatory cytokines. With the unfavorable course of the acute period of traumatic disease, the scale of damage and the volume of foci of development of the inflammatory response does not allow the body to use this adaptation reaction. As a result, immune failure is developing with a decrease in the number and development of the functional insufficiency of cells involved in immune reactions, on the background of an imbalance in the regulatory link of immune homeostasis.
The central metabolic reaction at traumatic shock is hyperglycemia. It is due to an increase in the hormone hormone, somatotropic hormone, glucocorticoid and glucagon. Due to this, glycogenolysis and gluconeogenesis is stimulated, the synthesis of insulin and its activity is reduced mainly in muscle tissue. Glucose synthesis enhancement is an urgent compensatory reaction, indicates an increased energy request for tissues. Due to the reduction in the consumption of glucose in the muscles, the body "protects" glucose to ensure the energy of vital organs. Glucose is the only source of energy in anaerobic conditions, the main energy substrate to ensure the reparation of tissues. Other metabolic reactions typical of traumatic shock are hypoproteinemia due to enhanced catabolism, the release of low-dispersed fractions in interstics, disaming disams and disamincing in the liver and acceleration of lipolysis due to the activation of lipases for the transformation of neutral fat in free fatty acid - Energy source.
The electrolyte disorders characteristic of traumatic shock appear to the loss of potassium ions by cells due to the inefficiency of the energy-intensive potassium-sodium pump, the delay in sodium ions of aldosterone, the loss of phosphorus cations due to the violation of the synthesis of ATP and the loss of chlorine anions due to the output of them to the gastrointestinal tract and Concentrations in the damage zone.
Tissue hypoxia leads to the accumulation of osmotically active substances (urea, glucose, sodium ions, lactate, pyruvate, ketone bodies, etc.), which is consistently causes hyperosmolability in cells, interstics, plasma and urine.
For victims in a state of traumatic shock, metabolic acidosis is characterized, which takes place in 90% of patients, and in 70% of them, this disruption of the acid-base state is noncompensated.
trauma shock clinic pathogenesis
Of the numerous theories of pathogenesis of traumatic shock deserve attention to the neurogenic, plasma and blood loss, as well as toxmic. However, each of the listed theories as it was proposed by the authors with a claim to universality, does not withstand serious criticism.
Neurogenic theory - He was proposed by Entrepreneurs to the First World War as the theory of exhaustion, supported by scientists of our country (N.N.Burdenko, I.R.Petrov). As a result of excessive irritation in the cells of the cortex of the brain, exhaustion comes, and to prevent them from death, diffuse braking is developing, which is then applied to subcortical formations, as a result of which the oppression of respiratory centers and blood circulation occurs, decrease in temperature, etc. However, numerous clinical observations and experimental data do not fit into this theory. First, the diffuse braking is observed during sleep and anesthesia, and when the shock was injured in consciousness. Secondly, if braking begins in the crust for its protection against exhaustion and death, this contradicts the evolution and the occurrence of a person: braking should arise in more ancient structures to protect from death of younger. Thirdly, neurophysiologists have proven that braking is not a passive process, but an active, and it comes in the Talalamic region, therefore the excess flow of pulses does not enter the reticular formation, which is responsible for the emotional color of human behavior, and the cerebral bark. Therefore, it is caught in indifference, indifference to the surrounding, Adamina and others symptoms of trapidity, but it is not the symptoms of spilled braking! Attempt to apply stimulating substances in the treatment heavy Shock They were not justified. Nevertheless, it is not necessary to discard this theory. From the position of the neurogenic theory, it is possible to explain the launcher of the shock.
Plasmo and blood loss theory The most common among American scientists, but has a significant number of supporters and in our country (A.N. Berkutov, N.I. Egypt). Indeed, with any mechanical injury, blood loss is observed. Thus, with a closed fracture of the hips, even without damage to the main vessels, it can be up to 1.5 liters, but not simultaneously, and during the day, and, thus, from the position of this theory, it is impossible to explain the launcher of the shock. In the future, blood circulation disorders and at traumatic shock, and with hemorrhagic wear the same type. Especially well studied disorders of microcirculation.
Toxmia theory Offered in 1918 by the American pathophysiologist V. Kennon. Of course, toxemia takes place, especially in the late period as the accumulation of toxins due to the impairment of peripheral blood circulation. Therefore, in the treatment, it is necessary to include drugs for detoxifying the body, but not to start with them! From the position of this theory, it is also impossible to explain the launcher of the shock. It is suitable for explaining the pathogenesis of the turnstip shock and traumatic toxicosis.
Attempting to combine these three theories in one have not yet found wide support, although many scientists, including extreme supporters of the theory of blood loss (G.N. Titsibulak, 1994), recognize the presence of all three mechanisms in the pathogenesis of shock. The essence of the idea is that at each individual stage of the post-traumatic reaction, the leading reason for the shock is one of the factors at the next stage - another.
So, the launch mechanism is a neurogenic factor: The powerful stream of a specific pain and non-specific afferent impulsation enters the CNS (Talamus as the main collector of all kinds of sensitivity). Under these conditions, it is formed a new emergency functional system (FFS) in this minute from an imminent death in order to adapt the body's functions to suddenly changed the conditions of existence. Thus, the main meaning of the inclusion of new regulatory mechanisms is to translate high level Life activity on a more ancient, primitive level, ensuring the activity of the heart and CNS by disconnecting all other organs and systems. Hydobiosis develops (according to D.M. Sheherman), which is clinically manifested by a drop of blood pressure, the onset of adamisia, a decrease in muscle and skin temperature and as a result of all this (which is extremely important!) - Reducing oxygen consumption by tissues! If the FSF does not have time to form, then with severe injury comes primary collapse and death. Thus, from a communist point of view shock - defensive reaction organism.
In the second stage of the post-traumatic reaction, the leading link of the pathogenesis of the shock is circulatory disorders (on the theory of blood loss), the essence of which can be reduced to the following:
- 1. "Circulatory Centralization" - after falling blood pressure under the influence of blood-thrown into the blood at the time of the injury of adrenaline and norepinephrine, there is a spasm of arteriole, preacapillars, due to this, the total peripheral resistance of the arteries increases, the blood pressure increases and the venous blood return to the heart increases, but when this tissue turns out Disabled from "blood supply".
- 2. The second adaptive reaction is the opening of arterio-venous shunts, according to which the blood will arrive at the veins bypassing the capillaries.
- 3. Disturbances of microcirculation - a large number of unsafected products accumulates in the disconnected tissues, including histamin-like, under the influence of whom the Sapinters of the capillaries are opened, and blood rushes into extended capillaries. There is a discrepancy between the ECC of the increased capacity of the functioning capillaries ("bleeding to own capillaries"). In extended capillaries, blood flow is slowed down. At the same time, under conditions of hypoxia, the preparation of the capillary wall increases, and the liquid part of the blood begins to go into the interstitial space, the electrostatic charge of the erythrocyte shell falls, their interoperability decreases, so-called. "Sweet" red blood cells. Developed by DVS syndrome (dissiminary intravascular coagulation). Disorders of microcirculation acquire a universal character. As a result, generalized hypoxia develops, i.e. suffer all fabrics and organs
The signals are received by the continuing deterioration of the organs of organs in the central nervous system, and according to the law of feedback, a new FFS is being formed to exit. However, if it turns out to be insolvent, the process is progressing.
In the third stage of post-traumatic reaction, the leading factor in the development of shock is toxmia. All toxins can be divided into 3 groups. The first is the decay products damaged at the time of the tissue injury. The second is unsocusted exchange products. In hypoxia, all types of metabolism suffer, first of all - carbohydrate. Under normal conditions, under the aerobic path of oxidation from one glucose molecule, 38 ATP molecules are formed, which comes to the replenishment of the energy consumption that provide the vital activity of the cell. In hypoxia, an anaerobic oxidation path predominates, in which one glucose molecule only gives ATP molecules to form a huge number of non-surfacing products. Glucose consumption is clearly uneconomical - "This is a pillaby road to death" (VB Lemus). Glucose reserves are rapidly depleted, which leads to neuholikolizu: fats and proteins become sources of energy, and again with the formation of non-surfacing products. In addition, as a result of hypoxia, individual cells are dying with admission to the blood of freed cellular (lysosomal) enzymes, which leads to the body self-defense. The third group of toxins is the toxins of intestinal flora entering the bloodstream from the intestinal lumen, since the intake of the intestinal wall increases with hypoxia. Due to hypoxia, barrier and disinfecting liver functions are sharply violated. With low hell, the kidney does not work. Therefore, toxins are not derived from the body. The irreversibility of shock is formed.
Thus, the launching mechanism of shock is a neurogenic factor, then the dominant value is acquired by circulatory disorders, and at the third stage - toxmia. Such an understanding of the pathogenesis of shock provides a rational construction of a shock treatment program.
Traumatic shock is called a generalized response to a heavy mechanical injury. Since such injuries are almost always accompanied by massive blood loss, traumatic shock is conventionally called complicated hemorrhagic shock.
Pathogenesis of traumatic shock
The main starting factors for the development of traumatic shock are heavy multiple, combined and combined traumatic injuries in combination with massive blood loss and pronounced pain syndrome, which induce a whole cascade of changes in the body aimed at reimbursement and maintaining basic functions, including vital. The primary response of the body into the above factors is a massive emission of catecholamines (adrenaline, norepinephrine, etc.). The biological effect of these substances is so pronounced that under their influence in the shock state there is a cardinal redistribution of blood circulation. The reduced volume of circulating blood (BCC) as a result of blood loss is not able to adequately ensure the oxygenation of peripheral tissues in the presence of a preserved volume of blood supply to vital organs, therefore a systemic drop in blood pressure is observed. Under the action of catecholamines, peripheral vazospasm occurs, which makes blood circulation in peripheral capillaries impossible. Low blood pressure further exacerbates the phenomenon of peripheral metabolic acidosis. The overwhelming amount from the OCC is in the main vessels, and this achieves compensation for blood flow in vital organs (heart, brain, lungs). This phenomenon is called "Circulatory Centralization". It is not able to make compensation for a long time. When tying the timely anti-deposit measures, the phenomenon of metabolic acidosis on the periphery is gradually beginning to acquire a generalized character, causeing polyorganic insufficiency syndrome, without treatment, quickly progressing and leading ultimately to death.
Shock - the acutely developing overall reflex pathological response of the organism on the effect of extreme stimuli, characterized by a sharp oppression of all life functions and has the basis of deep parabiotic disorders in the central nervous system.
Shock caused irritants:
The power, intensity and duration of the irritant should be:
· Unusual
· Emergency
· Excessive
· Extreme stimuli:
Examples of stimuli:
· Discharge of soft tissues
· Fractures
· Chest damage and abdominal cavity
· Firearms
· Extensive burns
· Blood incompatibility
· Antigenous substances
· Histamines, peptons
· Electric shock
· Ionizing radiation
· Mental injury
Types of shock:
· Tramistry
· Operational (surgical)
· Burning
· Postghemotransfusion
· Anaphylactic
· Cardiogenic
· Electric
· Radiable
· Psychic (psychogenic)
Traumatic shockdefined as the most common clinical form The severe state of the wounded, developing due to severe mechanical injury or injury and manifests the syndrome of a low minute volume of blood circulation and hypoperfusion of fabrics.
Clinical and pathogenetic The basis of the traumatic shock is a syndrome of an acute circulatory disorder (hypocyculation), which arises due to the combined effect on the organism of the injured life of injury - acute blood lossDamage to vital organs, endotoxicosis, as well as nervous influences. The main link pathogenesis of traumatic shock are primary disorders of microcirculation. Acute insufficiency of blood circulation, lack of perfusion of tissues with blood leads to inconsistencies between reduced microcirculation capabilities and energy needs of the body. At traumatic shock, in contrast to other manifestations of the acute period of traumatic disease, hypovolemia due to bloodstures is the lead, although not the only reason for hemodynamic violations.
An important factor determining the state of blood circulation is the work of the heart. For most victims with severe injuries, the development of a hypendynamic type of blood circulation is characteristic. With a favorable course, its permanent volume after injury can remain elevated throughout the acute period of traumatic disease. This is due to the fact that coronary arterys are not involved in the common vascular spasm, it remains satisfactory venous return, cardiac activity is stimulated through vascular chemoreceptors of unsophisticated exchange products. However, with a preserving hypotension, after 8 hours after injury, a single and minute heart performance in patients with traumatic shock can decrease by about twice as compared to the norm. Increasing heart rate and total peripheral resistance of vessels is not able to maintain a minute volume of blood circulation on normal quantities
Insufficient cardiac release at traumatic shock is due to the depletion of urgent copins mechanisms due to myocardium hypoxia, the development of metabolic disorders in it, a decrease in the content of catecholamines in myocardium, a decrease in its reaction to sympathetic stimulation and catecholamines circulating in blood. Thus, the progressive decrease in one-time and minute performance of the heart will be a reflection of developing heart failure, even in the absence of direct damage (injury) of the heart (V.V. Timofeev, 1983).
Another main factor determining the state of blood circulation is the tone of the vessels. A regular reaction to injury and blood loss is the strengthening of the functions of a limbico-reticular complex and a hypothalamic-adrenal system. As a result, the traumatic shock includes urgent compensatory mechanisms aimed at maintaining blood circulation of vital organs. One of the compensation mechanisms is to develop a common vascular spasm (first of all arterioles, metharcyteries and prokapillary sphincters) aimed at emergency decrease in the capacity of the vascular bed and bring it into line with the BCC. The total vascular reaction does not apply only on the artery of the heart and brain, which are practically deprived of? -Adrenoreceptors implementing the vasoconstrictor effect of adrenaline and norepinephrine.
The mechanism of urgent compensation, also aimed at eliminating the inconsistency between the BCC and the capacity of the vascular bed, is autogriego. In this case, the reinforced movement of the fluid from the interstitial space in the vascular is. The fluid yield in interstics occurs in functioning capillaries, and its entry goes to non-functioning. Together with interstitial liquid in capillaries penetrate the products of anaerobic metabolism, which reduce sensitivity? -Adrenororeceptors to catecholaminams. As a result, non-functioning capillaries expand, and functioning, on the contrary, narrow. With a shock due to an increase in the concentration of adrenaline and norepinephrine, the ratio between the functioning and non-functioning capillaries is dramatically changed in favor of the latter.
Thus, conditions are created to increase the reverse current of the fluid into the vascular channel. Autohemodiliation is also amplified by the dominance of oncotic pressure not only in venular (as under normal conditions), but also in the arterilar ends of functioning capillaries due to a sharp decrease in hydrostatic pressure. The mechanism of autoghemodilia is quite slow. Even with bloodwall exceeding 30-40% OCC, the rate of flow of fluid from an interstice into the vascular channel does not exceed 150 ml / h.
In the reaction of urgent compensation of blood loss, a renal mechanism of water and electrolyte delay has a certain meaning. It is associated with a decrease in the filtering of the primary urine (decrease in filtration pressure in combination with spasm of renal vessels) and an increase in the reabsorption of water and salts in the tubing apparatus of the kidneys under the action of antidiuretic hormone and aldosterone.
In the exhaustion of the above-described compensation mechanisms, microcirculation disorders are progress. Intensive separation of histamine, bradykinin, lactic acid with damaged and stylish tissues with vasodilatory action; admission from the intestine of microbial toxins; The decline due to hypoxia and acidosis of the sensitivity of smooth muscle elements of the vessels to nervous influences and catecholaminams leads to the fact that the phase of vasoconstriction is replaced by the phase of vasodilation. There is a pathological deposit of blood in those who have lost the tone of metharrioles and extended capillaries. Hydrostatic pressure in them increases and becomes more oncotic. Due to the influence of endotoxins and hypoxia of the vascular wall itself, its permeability increases, the liquid part of blood leaves in interstics, the phenomenon of "internal bleeding" occurs. The instability of hemodynamics, violation of the tone of the vessels due to damage to the regulatory function of the brain in such a form of an acute period of traumatic disease, as a traumatic coma (severe crank-brain injury, the injury of a severe brain) usually develop later - by the end of the first day.
An important link of pathogenesis of traumatic shock, even with non-cleaning injury, is an acute respiratory failure. In character, it is usually parenchymal and ventilation. The most typical manifestation is the progressive arterial hypoxemia. Reasons for the development of the latter are the weakness of respiratory muscles under conditions of circulatory hypoxia; pain "brake" breathing; Embolization of the microShosudes of the lungs due to intravascular coagulation, fat globul, the yatrogenation of transfusions and infusions; interstitial pulmonary edema due to increasing the permeability of the membranes of microscopes of endotoxins, hypoxia of the vascular wall, hypoproteinemia; Microelectsization due to reducing the formation and reinforced destruction of the surfactant. The predisposition to the atelectasis, the tracheoobronchitis and pneumonia is exacerbated by the aspiration of blood, gastric content, increasing the release of mucus with bronchial glands, the difficulty of flipping against the background of insufficient blood supply to the tracheobronchial tree. The combination of pulmonary, hemic (due to anemia) and circulatory hypoxia is a key point of traumatic shock. It is hypoxia and tissue hypoperfusion that determine the metabolic disorders, immune status, hemostasis, lead to increasing endotoxicosis.
Traumatic shock flows into two phases - Excitation (erectile) and braking (torpid).
Erectile phase It comes immediately after injury and manifests itself with motor and speech excitement, anxiety, fear. The consciousness of the victim is preserved, but the spatial and temporal orientation is violated, the victim underestimates the severity of their condition. Questions are responsible correctly, periodically complains of pain. The skin pale, breathing is rapidly expressed tachycardia, pulses of sufficient filling and voltage, blood pressure is normal or slightly increased.
The erectile phase of shock reflects the compensatory reaction of the body to injury (mobilization stress) and hemodynamically corresponds to the centralization of blood circulation. It happens different duration - from a few minutes to several hours, and with very difficult injuries it may not be detected at all. It is noted that the shorter the erectile phase is, the harder the shock occurs in the subsequent.
Thorpid phase It develops as radiation failure increments. It is characterized by a violation of consciousness - the injured inhibitors, it does not complain about pain, lies motionless, his wandering look, no matter what is not fixed. Questions answers questions, to obtain an answer, it is often necessary to repeat the question. Skin cover and visible mucous membranes, with a gray shade. The skin can have a marble pattern (a sign of a decrease in blood flow and stagnation of blood in small vessels) is covered with cold sweat. The limbs are cold, the acricyanosis is observed. Surface breathing, rapid. The pulse is frequent, weak filling, the filamentoid - a sign of a decrease in the volume of circulating blood. Blood pressure is reduced.
The severity of the state in the flue phase of shock is estimated at the pulse frequency and arterial pressure And denotes the degree.
Read also ...
- The work of "Alice in Wonderland" in a brief retelling
- That transformation. "Transformation. Attitude towards the hero from the sister
- Tragedy Shakespeare "King Lear": the plot and the history of the creation
- Gargantua and Pantagruel (Gargantua et Pantagruel) Francois Rabl Gargantua and Pantagruel Brief