Keloid scar Code on the ICD. The consequences of thermal and chemical burns, frostbite, wounds. What it is
The keloid scar (ICD 10) is a scar formation that is formed on the area of \u200b\u200baffected skin. Damage must be processed, otherwise the traces can remain for life. The keloid scar also testifies to the imminent healing of destroyed skin fabrics.
The keloid scar of the Code of MKB 10 is classified as a physiological phenomenon. This is the result of the restoration of fabrics deformed artificial way. Often, the scars are healing and become inconspicuous, but the keloid is distinguished by a pronounced character and appearance.
Keloid - dense thigh, which externally can resemble a tumor, differs in the following features:
- The scar is beyond the boundaries of the damaged area. It grows in a horizontal direction.
- The keloid is a scar scar, which is characterized by sharp pains, itching. A bright example is a feeling of skin tightening.
- If over time it becomes almost invisible, then the colloidal does not change the colors, size. This is due to the fact that blood vessels grow inside.
Causes and symptoms of education
Even minor skin defects lead to the formation of disease scars. Among the main reasons are allocated:
- Independent treatment of the wound. If the cutting edges are connected incorrectly, the skin is deformed and the disease cannot be avoided. This error may be allowed to be allowed.
- The keloid appears as a consequence of infectious infection. Disinfection and application of appropriate means - a prerequisite for safe treatment of the wound.
- As the code is confirmed on the ICD 10, it is formed after too much skin tension during the overlay of the seams. This spoils the appearance initially and in the future becomes a factor of destructive impact.
- Medical surveys define keloids as a result hormonal imbalance. Including immunodeficiency among the causes.

International Classification Diseases take into account hereditary predisposition. The abundance of scars in relatives can talk about the high probability of forming a keloid scar.
Possible complications
The international classifier does not record keloids as dangerous diseaseconstituting a threat and leading to grave complications. It will not be the cause of the future tumor, malignant educationwhich is risk for life.

Removal and change of scars is initiated for two reasons:
- Aesthetic. It looks ugly on the outdoor skin. The scar is not masked under the tan and during germination blood vessels stand out on the body.
- Practical. Scars located on the skeleton of the joints are shoved. When wearing dense tight clothes, discomfort and itching from rubbing occurs.
Prevention of appearance
To warn the appearance of a keloid in the following ways:
- Bandages. Special dressings, creating strong pressure, localize the focus of distribution. However, not every wound allows such solutions.
- Balanced treatment. Timely appeal to the doctor will help disinfect the wound and develop individual program recovery. The use of vinegar and other aggressive means leads to side effects.
- Caution. Suggest an affectionate or massaging the scar from behind the ferrous. It says O. inflammatory process, so you should contact a specialist.
- Cold peace. Baths, saunas and high temperatures are contraindicated with patients with keloids.
In most, the deformation of scars is a consequence of injury infection. Upon receipt of abrasion or mechanical damage to the skin, the main thing is to consult a doctor on time, do not load the deformed tissues and do not engage in self-medication.
Rough scars and scars on the face or body today do not serve the decoration of real men and, even more so, women. Unfortunately, the possibilities of modern medical cosmetology do not allow to completely get rid of scar defects, offering only to make them less noticeable. The process of correction of scars requires perseverance and patience.
"Scar" and "Scar" - words synonyms. Scar is a domestic, everyday name of the scar. The scars on the body are formed due to healing of various skin damage. The impact of mechanical (injuries), thermal (burns) agents, skin diseases (pedestal) lead to a violation of the physiological structure of the skin and its substitution with a connective tissue.
Sometimes the scars behave very cunning. With normal physiological scarring, the skin defect with time is tightened and pale. But in some cases, the scarring is pathological nature: The scar acquires brightly crimson color and increases in size. In this case, immediate assistance is needed. The problem of the correction of scars is engaged in the Commonwealth, dermatocamestologists and plastic surgeons.
The formation of scars.
In its formation, the scar passes 4 consistently replacing each other step: I - stage of inflammation and epithelialization.It takes from 7 to 10 days from the moment of injury. It is characterized by a gradual decrease in edema and skin inflammation. Granulation fabric is formed, rapping the edges of the wound, the scar is absent yet. If there is no infection or discrepancy between the wound surface, the wound heals the primary tension with the formation of a barely noticeable thin scar. In order to prevent complications at this stage, the atraumatic seams, gentle fabrics, are applied daily dressings with local antiseptics. The physical activity is limited to avoid the discrepancy of wound edges. II - stage of education "young" scar.
Covers the period from the 10th to the 30th day from the moment of injury. It is characterized by the formation of collagen-elastin fibers in the granulation tissue. The scar of the immature, loose, easily stretched, bright pink (due to the enhanced wound blood supply). At this stage, the secondary injury of wounds and enhanced physical exertion should be avoided. III - the stage of education "mature" scar.
Lasts from the 30s to the 90s from the day of injury. Elastin and collagen fibers grow into bundles and are built in a certain direction. The blood supply to the scar is reduced, which is why it is compacted and pale. At this stage there are no restrictions on physical activity, but the repeated injury of the wound may cause the formation of a hypertrophic or keloid scar. IV - Stage of the final transformation of the scar.
Starting from 4 months after injury and up to the year, the final ripening of the scar occurs: the fiber of the vessels, the tension of the collagen fiber. The scar is condensed and pale. It is in this period that the state of the scar and further tactics of its correction becomes clear to the doctor.
Get rid of scars once and is forever it is not possible. With the help of modern methods, you can only make a rough, wide scar of cosmetically more acceptable. The choice of techniques and the effectiveness of treatment will depend on the stage of forming a scarsing defect and from the type of scar. At the same time there is a rule: the sooner you applied for medical care, the better the result will be.
The scar is formed due to disruption of the integrity of the skin (operation, injury, burn, piercing) as a result of the processes of closing defect with a new connective tissue. Surface damage to the epidermis heals without the formation of scars, because the cells of the basal layer have a good regeneration ability. The deepends the damage of the layers of the skin, the longer the healing process and a pronounced scar. Normal, uncomplicated scarring leads to the formation of the normatrophic scar: flat and having the color of the surrounding skin. The violation of the collapse flow at any stage can lead to the formation of a coarse pathological scar.
Types of scars.
Before choosing the treatment method and the optimal period of one or another procedure, the type of scars should be determined.Nimmotrophic scars are usually not delivered to patients of large chagrins.They are not so noticeable, TD their elasticity is close to normal, they have a pale or bodily painting and are at the level of surrounding skin. Without resorting to radical methods of treatment, such scars can safely get rid of microdermabrasion or chemical surface peeling.
Atrophic scars may arise due to acne and poor-quality removal of moles or papillom. Stretch marks (Strya) are also this type of scars. Atrophic scars are below the level of surrounding skin, are characterized by the flabbiness of the tissues arising from the decrease in collagen production. The lack of skin growth leads to the formation of pits and scars creating a visible cosmetic defect. Modern medicine has a lot in his arsenal effective ways eliminating even enough extensive and deep atrophic scars.
Hypertrophic scars have a pink color, are limited to a damaged area and protrude over the surrounding skin. Hypertrophic scars can partially disappear from the surface of the skin for two years. They are perfectly treatable, so do not wait for their spontaneous disappearance. You can affect small scars with laser grinding, dermabrasia, chemical peeling. Introduction to the scar zone hormonal drugs, Diprospan and Kenaloga injections. Electro- and ultrafonophoresis with constructubex, lidase, hydrocortisone give a persistent positive effect in the treatment of hypertrophic scars. maybe surgery, in which scar tissues are excised. This method gives the best cosmetic effect.
Keloid scars have a sharp limit, protruding over the surrounding skin.Kellloid scars are often painful, in the places of their formation it is sensible and burning. This type of scars is poorly treatable, recurrence of the occurrence of keloid scars of even large sizes are possible. With all the complexity of the task, aesthetic cosmetology has a lot of examples of a safe solution to the problem of keloid scars.
Features of keloid scars.
The success of the treatment of any disease largely depends on the correct diagnosis. This rule is not an exception and in the case of eliminating keloid scars. Avoid mistakes in tactics of treatment, it is possible only clearly defining the type of scar, TD on external manifestations of keloid scars often resemble hypertrophic scars. The essential difference is that the size of hypertrophic scars coincide with the dimensions of the damaged surface, while the keloid scars go beyond the borders of the injury and the area can exceed the size of traumatic skin damage. The usual places of occurrence of keloid scars are the region of the chest, ear sinks, less often, the joints and the area of \u200b\u200bthe face. Celaoid scars in their development are four stages.Stage of epithelization. After the injury is obtained, the damaged area is delayed with a thin epithelial film, which is compacted within 7-10 days, it grives, acquires a pale color and remains in this form 2-2.5 weeks.
Stage of swelling. At this stage, the scar increases, towers over adjacent skin, becomes painful. In continuation of 3-4 weeks, painful sensations weaken, and the scar acquires a more intense reddish color with a cyanotic tint.
Seal stage. There is a seal of the scar, dense plaques arise in its separate places, the surface becomes a buggy. The outer picture of the scar represents a keloid.
Stage softening. In this stage, the scar finally acquires a keloid character. It is distinguished by pale colorful, softness, mobility and painlessness.
When choosing treatment tactics proceed from the statute of the statute of scars. Keloid scars from 3 months to 5 years of existence (young keloids) are actively growing, differ in a smooth shiny surface, red with a cyanotic tint. The scars over 5 years old (old keloids) are pale, acquire a wrinkled uneven surface (sometimes there is a sunset of the central part of the scar).
The cause of keloid scars can be surgical interventions, vaccination, burns, insect bites or animals, tattoos. Such scars may occur even without traumatic damage. In addition to substantial aesthetic discomfort, keloid scars deliver to patients the unpleasant sensation of itching and pain. The reason for the development of this type of scars, and not hypertrophic, currently not established doctors.
A little about shrill.
Information about the scar will be incomplete if it is silent such a procedure as shouting or scarification - artificial applying to the skin of decorative scars. For some, this is a new-fashioned direction of Body Art - a way to disguise already available scars, for others - an attempt to give their appearance masculinity and brutality. Unfortunately, thoughtless passion for young people with similar procedures, as well as other artificial lesions of the skin (tattoos, piercing) leads to irreversible consequences. Fashion passes, and scars remain forever.Pronounced skin pigmentation. Defined localization of initial damage (region of the deltoid muscle, chest, ear dump). Pregnancy is a puberty.
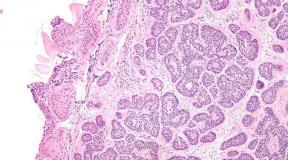
Patomorphology
In histological examination, elongated convoluted bundles of eosinophio colored hyalinized collagen, thinning of the papillars of the dermis and decrease the elasticity of fibers. Morphological basis
it is an excessive growing immature connecting tissue with a large number of atypical giant fibroblasts, a long time in functionally active condition. IN
keloid
little capillaries, fat and plasma cells.
Celaoid: Symptoms, Symptoms
Clinical picture

Pain sickness hyperesthesia itching solid smooth raising over the skin surface scars with butched borders at the beginning of the disease can be the pallor or light erythema skin scar occupies a large area than initial damage even years
Continue to grow and can form clawed grows.
Symptoms of keloid scars
Keloid and hypertrophic scars are accompanied by redness (hyperemia), painful sensations After pressing the scar. In this place, the fabric is characterized by increased sensitivity. Scars begin to hide. Celoids are developing in two stages:
- Active is distinguished by the dynamic growth of keloid tissues. This is accompanied by itching, numbness of affected places and diseases of the tissues. This stage begins with the epithelization of the wound and continues until the year.
- In the inactive period, the final formation of the scar occurs. It is called stabilized, acquiring the usual skin color. The resulting scar does not deliver the owner of the concern, but in open areas of the body looks unesthetically.
Two types of keloids differ. True towers above the skin and have whiten or pink color. Scars are dense, with a smooth shiny surface with a minimum capillary content.
The formation of keloids is accompanied by the following symptoms:
- hyperemia (red) in the scar region;
- painful sensations under pressure;
- increased sensitivity in the area of \u200b\u200baffected fabrics;
- itching during combing.
The development of keloids takes two stages - active and inactive.
During the active stage, a dynamic growth of the keloid tissue occurs, which causes physical discomfort in the patient: itching, soreness and / or numbness of affected fabrics. This stage begins with the moment of the epithelization of the wound and can last up to 12 months.
The inactive stage is completed by the final formation of the scar. Such a keloid is called otherwise stable, since its color resembles the natural color of the skin, and the scar himself does not cause special concern, with the exception of the inesttic species, especially in open areas of the body.
Keloid: Diagnosis
The true (spontaneous) and false keloid are distinguished.

Differential diagnosis
Hypertrophic scars of dermatofibrome Infiltrating basal cell cancer (confirm with biopsy).
Conservative treatment
Keloid scar - how to get rid of it with conservative treatment? First diagnostics, biopsy is prescribed to eliminate malignant neoplasms.
Treatment begins with conservative techniques. They help well if the scars are not yet fat, formed no more than a year ago.

During the compression, the pressure on the affected area is applied. The growth of the keloid stops by squeezing. The power of the scar tissue is blocked, its vessels are compressed. All this contributes to the arrangement stop.
Ointment from keloid scars is only auxiliary method. As an independent direction, the means is rarely used. Mazi is usually prescribed as additional preparations with antibacterial, anti-inflammatory and reducing blood circulation by actions.
Different techniques are used as a cosmetic correction of acne-keloid: dermabrasion, peelings. All of them are aimed at changing external view scars.
Mesotherapy and other cosmetic methods are carried out only for the upper skin layer, in order to avoid growing connective tissue. Correction is shown only for old scars.
In other cases, three main conservative methods are most often used to remove them. The first way, how the keloid scar is removed: treatment with silicone plates.
They begin to be used immediately after the first healing of the wounds. Silicone plates are mainly shown to people who have a tendency to form keloids.
The essence of the technique is based on squeezing capillaries. As a result, the synthesis of collagen decreases and moisturizing the tissues is stopped. Special plaster with plates is used per day from 12-24 hours. Course therapy - from 3 to 18 months. Compression is a variety this method.
The second method: Treatment of keloid scars using corticosteroids is shown for local use. Injection is made to the convexity, which includes suspension of triamcinolone acetonide. Per day is allowed to injected from 20 to 20 milligrams of the drug, for each scar is spent by 10 mg.
The purpose of injections is to reduce collagen production. This decreases the division of fibroplasts, which produce it, and increases the number of collagenase.
Treatment is most effectively for non-solar scars. In this case, for therapy is sufficiently small doses.
After a month, the course of treatment is repeated until the scars are equal to the skin surface.
The third main method, how to get rid of keloid scars, is called cryodestruction. This is the destructive effect on the scar tissue with liquid nitrogen. As a result, a crust appears on the processed place.
Healthy fabrics are formed under it. After the end of the process, the crust disappears independently, leaving an almost imperceptible mark. The cryodestruction method is effective only for new keloid and hypertrophied scars.
Aggressive removal of keloid scars is made in two ways - surgically or with a laser. In the first case, during the operation, not only the resulting fabrics are excised, but also affected skin.
The surgical method has its drawbacks - there is a high probability of formation of new keloid scars.
This risk is somewhat reduced by removing the affected skin area. Nevertheless, recurrences are observed in 74-90 percent cases. Surgical operation is shown only when conservative treatment It turned out ineffective.
With the help of laser therapy, keloid scars are removed or burned out, which minimized the surrounding fabrics. Correction is applied in complex treatment and combined with corticosteroid and local methods. Laser therapy recurrences are far less frequently - in 35-43 percent.

The treatment of the keloid on the ear is due to a specific scheme. The diprospan or kenologist-40 is assigned first.
Injections are made in scar tissue. One month after the start of treatment, laser therapy is carried out using the bundle.
The patient wears a special squeezing clips on the ear (at least 12 hours daily).
At the end of therapy for fastening the effect, phono and electrophoresis with collagenase or lidase are prescribed. At the same time, ointments and gels are prescribed (Lioton, hydrocotone, etc.).
If after that the growth of the scar tissue does not stop, then native radiospecus radiotherapy is added to the treatment. In severe and complex cases, Methotrexate is made.
The keloid scar after Cesarean can be treated in many ways. In some cases, a deep chemical peeling helps to get rid of keloid scars.
First, the scar is processed by fruit acids. After that, chemicals are applied.
This method is ineffective, but also the most budget.
For therapy of the keloid batch after the removal of the mole or cesarean section Plates and gels containing silicone are prescribed. There are many emergency tools with the basis of collagenase.
Preparations from hyaluronidase are used. Help to eliminate the keloid scars for hormonal basis, with vitamins and oils.
Physiotherapy is assigned to remove mature scars: phono electrophoresis. These are effective and painless procedures. As a last resort, plastic surgery or laser grinding is made. A more sparing method - microdermabrasion. During the procedure, aluminum oxide microparticles are used.

There are many ways to treat keloid scars by folk methods. Scars are not completely removed, but becomes less visible.
Funds are used on a vegetable basis. For example, 400 g is taken sea buckthorn oil and mixed with 100 g of bee wax.
The solution is heated on a water bath for 10 minutes. Then the gauze napkin is lowered into the mixture and superimposed on the scar.
The procedure is carried out twice a day. The course of treatment is three weeks.
To remove scars, compresses are made with camphor, in which the bandage is wetted. Then it is applied to the scope. The compress is done daily within a month. Only after that the result will be visible.
You can make a tincture of the dolphinium. Roots plants are very crushed. They are added alcohol and water mixed in equal proportions. Capacity is removed for two days in a dark place. Then the gauze napkin is impregnated into the liquid and applied to the keloid log.
Owls based on Japanese ceiling. A pair of glasses of beans plants are crushed and mixed with a barzuchery or goose fat in the same proportion.
The mixture is insteaded for 2 hours in a water bath. Then, with an interval, twice heats up per day.
After that, the mixture is boiled, stirred and shifted into a ceramic or glass jar.
Keloid scars do not pose a threat to health or life, but may cause nervous disorders due to an inesthetical appearance of the body. In the earlier degree of neoplasma is treated much easier than in the launched version.
According to statistics, the keloid scars are found not very often - only 10 percent of cases. This disease is most susceptible to women. To prevent scars, it is necessary to comply with all the prescriptions of doctors and do not engage in self-medication.
The nature of the keloid was not fully studied, so today the universal treatment technique has not been developed. Methods choose a doctor individually for each patient, depending on clinical picture Diseases.
Treatment methods can be divided into conservative and aggressive (radical).
It is preferable to start with conservative, especially if young scars are not older than one year. The most effective are the three methods:
- use of silicone coating / gel;
- corticosteroid injection therapy;
- cryotherapy.
The use of silicone plates
It is necessary to start using silicone plates in the form of a plaster immediately after the initial healing of the wound in people who have a predisposition to the development of keloids.
The mechanism of this technique is based on squeezing capillaries, reducing the synthesis of collagen and hydration (moisturizing) of the scar. The plaster must be used from 12 to 24 hours a day.
Treatment period - from 3 months to 1.5 years.
A type of this method of treatment can be considered compression (squeezing), as a result of which the growth of the keloid ceases, the power of the scar is blocked and the vessels of the scar are compressed, which leads to a stop of its growth.
Injection corticosteroids
This technique is used locally. With the help of injection, suspension of triamcinolone acetonide is introduced inside the scar.
On the day you can enter 20-30 mg of the drug - 10 mg per each scar. Treatment is based on a decrease in collagen synthesis.
At the same time, the division of fibroblasts producing collagen is oppressed, and the concentration of collagenase - the enzyme splitting collagen increases.
Treatment in small doses effectively with fresh keloid scars. After 4 weeks, treatment is repeated to comparing scars with the skin surface. If a therapeutic effect There is no suspension of triamcinolone containing 40 mg / ml.
Treatment with steroids can cause complications:
Treatment
Tactics of keeping
The most effective local injections of the GC pressure on the damaged region prevents development
Apply bandages that create pressure over the place of damage to 24 mm RT. Art. , for 6-12 months. Bandage can be removed by no more than 30 min / day radiation therapy in combination with GK - with the ineffectiveness of other methods of treatment.
Surgery
it is shown only with the extensive lesion and inefficiency of local treatments. Celebrate a high frequency of relapses, so surgical treatment is recommended to hold no earlier than 2 years after education
with immediately preventive treatment (as formed
Drug therapy
In one day, the drug can be introduced in 3 scars (10 mg per each scar) The needle should be administered in different directions for a better distribution of the drug the effectiveness of the method above with fresh keloid scars, treatment is repeated every 4 weeks before comparing scars with the skin surface in the absence of effect Apply a suspension of triamcinolone containing 40 mg / ml with surgical excision.
keloid
you can apply a mixture of a R-RA of triamcinolone (5-10 mg / ml) with topless essential means. For the prevention of relapses after the operation - the injection of the GC into the scar of the scar after 2-4 weeks and then 1 p / month for 6 months.
Four and forecast
Under the action of triamcinolone
reduced for 6-12 months, leaving flat light rutters.
MKB-10 L73. 0 Uchri Keloid L91. 0 keloid scar.
Tags:
Did this article help you? Yes -0 No -0 If the article contains an error. Click here 47 Ricing:
Prevention
To reduce the risk of recurrence after surgical operations to remove the keloid, it is customary to carry out preventive measures in the process of forming a new scar (for 10-25 days).
All therapeutic (conservative) methods are used as prevention measures. After the operation, you need to constantly use sunscreen with high levels protection.
Included: states that are grounds for observation, hospitalization or other obstetric care of the mother, as well as for cesarean sections before the start of childbirth
Excluded: Listed states with difficulty (O65.5)
- double uterus
- curry uterus
Mother's medical care at:
- polyp body uterus
- royal Fibroid
Excluded: Mother's Medical Assistance with Tumor Tumor (O34.4)
Mother's Medical Assistance at the RubE from the preceding cesarean section
Excluded: childbirth through the vagina after the preceding cesarean section of the BDU (O75.7)
Eashabilization of the neck with a circular seam with reference to cervical insufficiency or without it
Shov on the hikodka (Shirodkar Suture) with reference to or without cervical insufficiency
Mother's medical care at:
- polype of cervix
- preceding cervical operation
- stricture and stenosis of the cervix
- tumors cervix
Provision medical care Mother with:
- infringement of pregnant uterus
- launcher pregnant uterus
- retter to pregnant uterus
Mother's medical care at:
- preceding the operation on the vagina
- dense virgin peg
- vagina partition
- stenosis of the vagina (acquired) (congenital)
- stricture vagina
- vagina tumors
Excluded: Mother's Medical Assistance varicose expansion vests vagina during pregnancy (O22.1)
Mother's medical care at:
- crotch fibrosis
- the preceding operation on the perineum and vulva
- rigidine crotch
- tumors vulva
Excluded: Mother's Medical Assistance in varicose distribution of the perineum and vulva during pregnancy (O22.1)
Mother's medical care at:
- cytocele
- plastic pelvic bottom (a history)
- distribution abdominal
- rektorzel
- rigid Taza Dn.
In Russia International Classification of Diseases 10th revision ( MKB-10.) adopted as a single regulatory document for accounting for incidence, reasons for people's appeals in medical institutions All departments, causes of death.
MKB-10. Introduced into the practice of health throughout the territory of the Russian Federation in 1999 by order of the Ministry of Health of Russia from 27.05.97. №170
A new revision (ICD-11) is planned to be planned in 2022.
Source: MKB-10.com
Postoperative scar of the uterus, requiring the provision of medical care of the mother
Definition and general information [edit]
The scar (scars) is a dense formation, consisting of a hyalineized, rich in the collagen fibers of the connective tissue, resulting from the reparative regeneration of the tissue in violation of its integrity.
The scar in the uterus - the zone of the uterus, in which previous operational interventions were made (cesarean section, momectomy, reconstructive plastic surgery)
According to various authors, the scar on the uterus after the cesarean section is available in 12-16% of pregnant women, and every third abdominal labor subsequently is repeated. The prevalence of Cesarean section in the Russian Federation over the past 30 years (since 1980) has increased 3 times and is 22-23%. The number of pregnant women with the scar in the uterus after Momectomy is increasing. If this is done by laparoscopic or laparotomic access in the presence of an interstitial component, the scar is also formed. The frequency of insolvent scars after momectomy reaches 21.3%.
Wealthy scar in the uterus.
Insolvent scar in the uterus.
a) Localization of the scar on the uterus after cesarean sections:
- in the lower uterine segment;
- partially in the lower segment, partly in the body (after the eldero-corporate cut in the uterus);
b) scar on the uterus after Momectomy before and during pregnancy:
- without opening the uterus;
- with an opening of the uterus;
- scar in the uterus after removing the subseroso-interstitial node;
- scar on the uterus after removing the cereal mioma.
c) the scar on the uterus after the uterus perforation [with intrauterine interventions (with abortion, hysteroscopy)].
d) scar on the uterus after ectopic pregnancy, located in the interstitial department of the uterine tube, in the cervix after removing the cereal pregnancy.
e) Rubet on the uterus after reconstructive plastic surgery (operation of Strasmann, the removal of rudimentary horns of the uterus, plastic is the cereal over the insolvent scar on the uterus after cesarean section).
The scar in the uterus is formed due to caesarean section, after momectomy, uterine perforations, tubectomy. Scarring - a biological mechanism of healing of damaged tissues. The healing of the dissected wall of the uterus can occur by both restitution (full regeneration) and the substitution (defective). With full regeneration, the healing of the wound occurs due to smooth muscle cells (myocytes), with the substitution - due to the beams of coarse fibrous connective, often hyalinized tissue.
Postoperative scar of the uterus, requiring the provision of medical care of the mother: diagnostics [edit]
Informative methods of diagnosing the state of the scar on the uterus in a non-heated woman are hysterography, and better hysteroscopy, ultrasound research (ultrasound).
Hysterography produced on the 7-8th day menstrual cycleBut not earlier than 6 months after surgery in direct and lateral projections. The method allows you to study changes in the inner surface of the postoperative scar on the uterus. The inconsistency of the postoperative scar indicates: change in the state of the uterus in a small pelvis (a significant displacement of the uterus of the switches, serrated and thinned contours of the inner surface of the uterus in the zone of the alleged scar, "niche" and the defects of its filling).
Hysteroscopy. It is produced on the 4-5th day of the menstrual cycle, when the functional layer of the endometrium is completely discounted, and the subject fabric is visible through a thin basal layer. The inconsistency of the scar usually indicate local retractions or thickening in the scar area. The whispering color of the scar cloth, the absence of vessels indicate a pronounced predominance of the connective tissue component, and the intensity of the intensity of myometrium as a result of defective regeneration. Non-Valisable uterine scar and a scar with a predominance of muscle tissue testify to anatomical and morphological usefulness.
Ultrasound procedure. The echoscopic signs of the insolvency of the scar in the uterus are: uneven contour At the rear wall of the filled bladder, thinning of the myometrium, the intermittentity of the scar contours, a significant amount of echoscient inclusions (connective tissue). With a two-dimensional ultrasound, pathological changes in the scar region on the uterus are found much less frequently than with hysteroscopy (56% and 85%, respectively). But with the advent of the Dopplerometry method and the 3D reconstruction, the publication of ultrasound for evaluating the state of the scar on the uterus significantly increased, as it became possible to evaluate the hemodynamics of the scar (the development of the vascular network). The results obtained for additional methods for diagnosing the state of the scar on the uterus outside of pregnancy are recorded in an outpatient card and are taken into account when solving the issue of the possibility of planning follow-up pregnancy.
If there is an insolvent scar on the uterus at the stage of pregnancy planning, with the aim of preventing her rupture, during subsequent pregnancy, a reconstructive operation was shown - plastic is the coil of the uterus, which is produced in a gynecological hospital with a highly qualified surgeon-gynecologist of laparotomous or laparoscopic access.
Careful selection of pregnant women for spontaneous delivery.
Careful cardiographic and ultrasonic control in the process of spontaneous delivery.
Adequate anesthesia in the process of spontaneous delivery.
Exhausting the insolvent scar on the uterus with a re-caesarean section.
Postoperative scar of the uterus, requiring the provision of medical care of the mother: treatment [edit]
Maintaining pregnant women with a scar on the uterus after cesarean sections
Careful analysis of anamnesis, which includes information about the cesarean section produced in the past on the basis of an extract from the obstetric hospital.
Information on scar research on the uterus held out and during pregnancy.
Parity: whether there were spontaneous delivery to surgery; The number of pregnancies between surgery and real pregnancy than they ended (abortion, miscarriage, undeveloping pregnancy).
The presence of living children, whether there were still foreigners and the death of children after previous birth.
b) physical examination
Palpator study of the scar on the front abdominal wall and on the uterus; measurement of the sizes of the pelvis and the alleged mass of the fetus; Assessment of the state of generic pathways and the preparedness of the body to childbirth in 38-39 weeks of gestation.
c) instrumental research methods
Ultrasound of the fetus with the use of dopplerometry of vessels of umbilical umbilicals, aortic, the average-creation artery of the fetus and placenta, starting from the end of the II trimester of pregnancy.
Cardiomonitorial observation of the state of the fetus.
Uzi scar on the uterus every 7-10 days after 37 weeks of pregnancy.
The tactics of pregnant women with the wealthy scar in the uterus is not different from the generally accepted.
Be sure to be made as soon as possible ultrasound. The main purpose of this study is to determine the place of attachment of the fetal egg in the uterus. If it is located in the region of the cowith on the front wall of the uterus (in the scar zone after cesarean section in the lower uterine segment) from a medical point of view, it is advisable to interrupt pregnancy, which is made using a vacuum aspirator; Since the proteolytic properties of chorion as pregnancy progressing can lead to inferiority of even the wealthy scar on the uterus, to the prelationship and shooting of the placenta to the scar and to the rupture of the uterus. The question of the preservation or interruption of pregnancy is in the competence of the woman itself. With an uncomplicated course of pregnancy and the presence of a scar at the uterus, the next comprehensive examination is carried out in 37-38 weeks of gestation in the hospital, where it is assumed to be a pregnant woman (obstetric hospitals III level).
Rhodework of pregnant women with a scar in the uterus after cesarean sections
The question of the method of the delivery should be necessarily agreed with a pregnant woman. The task of the obstetrician explains it in detail by all the advantages and risk, both re-caesarean sections and spontaneous delivery. The final decision is made by a woman herself in the form of a written informed consent to one of the methods of delivery. In the absence of absolute testimony to the planned caesarean section, preference should be given to childbirth through natural generics, and, which spontaneous to their beginning.
Conducting birth through natural generic paths is permissible when complying with a number of conditions:
- one caesarean cross section in a history of cross-section in the uterus in the lower segment;
- the absence of extragnenitial diseases and obstetric complications that served as indications for the first operation;
- availability of a wealthy scar at the uterus (according to the results of clinical and instrumental research);
- localization of placenta outside the scar on the uterus;
- head prevention of the fetus;
- matching the size of the pelvis of the mother and the head of the fetus;
- the presence of conditions for emergency delivery by caesarean section: highly qualified medical personnel; The possibility of performing caesarean section in an emergency order no later than 15 minutes after deciding on the operation.
Indications for repeated abdominal childbirth in the presence of a scar on the uterus after cesarean section:
- scar on the uterus after corporate cesarean section;
- Insolvennaya scar in the uterus on clinical and echoscopic signs;
- scar on the uterus after plastle
- Prelation of the placenta into the scar;
- Two or more scars on the uterus after cesaric sections in the lower uterine segment;
With a re-caesarean section, a prerequisite is the excision of the insolvent scar in the uterus, which significantly reduces the risk of complications during subsequent pregnancy.
Conducting birth to women with a scar in the uterus after Momectomy
When choosing a rowor separation method in women with a scar in the uterus after Miomectomy, it belongs to the character, volume and method (laparotomy or laparoscopic) performed operation. The risk of rupture of the uterus on the header after momectomy in the process of spontaneous delivery is determined by the depth of the tumor in myiometry.
Indications for Cesarean section after momectomy outside pregnancy:
- the scar in the uterus after removing the interstitial or subseroso-interstitial nodes located on the rear wall of the uterus;
- the scar on the uterus after removing the cervical misa;
- the scar in the uterus after the removal of Intriligative Mioma;
- scars on the uterus after removing several interstitial-subseasonal nodes of large sizes;
- burdened obstetric history;
- pelvic prevention of the fetus;
- FPN (fetoplacentar failure);
- age-old age older than 30 years;
- scar after momectomy produced by laparoscopic access.
When preparing for pregnant women with a scar in the uterus after momectomy outside the pregnancy and the absence of testimony to cesarean section, spontaneous delivery is preferred.
The scar in the uterus after Miomectomy produced during pregnancy is a testimony to Cesarean section.
Rhodework of pregnant women with a scar in the uterus after reconstructive plastic operations, uterus perforations and ectopic pregnancy
Indications for Cesarean section:
- the scar in the uterus after the metroplasty (Strassmann operation, the removal of rudimentary horns of the uterus with an opening of the uterine cavity, the plastic is the cereal over the insolvent scar on the uterus after cesarean section);
- the scar after the uterus perforation, located in the reverse wall area;
- Scar after removing the cereal pregnancy, pregnancy in Rudimentary Rog of the uterus, a cult of remote pipes.
After giving birth through the natural generic paths with the scar at the uterus, it is necessary to carry out a control manual examination of the walls of the uterus.
Prevention of the insolvency of the scar on the uterus
Creating optimal conditions for the formation of a wealthy scar in the uterus during operations in the uterus: sewing a cut on the uterus with individual muscle-muscular seams or continuous seam (but not reverse) using synthetic residuous suture threads (Vinciles, monophil, etc.).
Prevention, timely diagnosis and adequate therapy of postoperative complications.
An objective assessment of the state of the scar in the uterus before the occurrence of pregnancy.
Source: wikimed.Pro.
Birth with a scar in the uterus Code on the ICD 10
The scar (Cicatrix) is a dense formation consisting of a hyalinized, rich in the collagen fibers of the connective tissue, resulting from the regeneration of the tissue in the violation of its integrity.
The scar in the uterus - the zone of the uterus, in which surgical interventions [Caesarean section (COP)], momectomy, reconstructive optical operations) were produced.
It should be noted that the concepts of "scar on the uterus after the cesarean section", adopted in our country, not quite successful, since it is often not discovered when repeated operation. Foreign authors usually use the terms "previous caesarean section" and "transferred Miomectomy".
Code of the ICD-10
O34.2 Postoperative scar of the uterus, requiring the provision of mother's medical care.
O75.7 Birth through the vagina after preceding the cesarean section.
O71.0 Tarve the uterus before the start of childbirth.
O71.1 Tarve the uterus during childbirth.
O71.7 Obstetric pelvis hematoma.
O71.8 Other refined obstetric injuries.
O71.9 Obstetric injury is unspecified.
According to the various authors, the scar on the uterus after cesarean section is noted in 4-8% of pregnant women, and about 35% of abdominal genera in populations are repeated. The prevalence of cesarean section in Russia over the past decade has increased 3 times and is 16%, and according to foreign authors, about 20% of all genera in developed countries ends with the operation of cesarean section.
Statistical indicators of the number of pregnant women with the scar at the uterus after Miomectomy and reconstructive-plastic operations do not exist, but at present, in connection with the development of the uterine, at earlier age, fast growth Tumors in female reproductive age and its large sizes that prevent the onset and tooling pregnancy, Miomectomy included in the complex of pregraving preparation. Upon the occurrence of pregnancy, women with the Mioma of the Uterus, obsuchethelectrics also produce momectomy more often than 10-15 years ago. Thus, the number of pregnant women with the scar in the uterus after Momectomy is constantly increasing.
Allocate a wealthy and untenable scar in the uterus. There is also a classification depending on the cause of the scar in the uterus.
· Scar on the uterus after cesarean section.
- in the lower uterine segment.
- Corporate log in the uterus.
- Eastic-corporate scar in the uterus.
· Scar on the uterus after conservative momectomy before and during pregnancy.
- without opening the uterus.
- With the opening of the uterus.
- scar on the uterus after removing the subserosozno-interstitial node.
- scar in the uterus after removing Intriligative Mioma.
· Scar in the uterus after the uterus perforation [with intrauterine interventions (abortions, hysteroscopy)].
· Scar on the uterus after ectopic pregnancy, located in the interstitial department of the uterine tube, at the place of the message of rudimentary horns of the uterus with the main cavity of the uterus, in the cervix after removing the cereal pregnancy.
· Scar in the uterus after reconstructive optical operations (operation of Strasmann, removal of rudimentary horns of the uterus).
The scar in the uterus is formed after cesarean section, conservative momectomy, uterine perforation, tubectomy, etc.
Scarring - Biological mechanism of healing damaged tissues. Healing of the dissected wall of the uterus can occur by both restitution (full regeneration) and the substitution (defective regeneration). With full-fledged regeneration, wound healing is due to smooth muscle cells (myocytes), with the substitution - the beams of coarse fibrous connective, often hyalinized tissue.
Clinical picture of the rupture of the uterus
The uterus breaks in dystrophic changes in the myometrium or the presence of scar tissue flows without a pronounced clinical picture (the "asymptomatic" is incorrectly called). Despite the estimated and unbearable nature of the disease, the symptoms take place and they need to know.
With the postoperative scar, the gaps can occur both during pregnancy and during childbirth.
By clinical flow The same stages are distinguished as in the mechanic-sk - the threatening, which began and the uterus breakdowns.
Symptoms of the gap of the uterus on the header during pregnancy
Symptoms of threatening rupture of the uterus on the header during pregnancy are due to reflex irritation of the wall of the uterus in the area of \u200b\u200bthe sprawling scar cloth:
·nausea;
· Vomiting;
· Pain:
- in the epigastric region, followed by localization at the bottom of the abdomen, sometimes more on the right (imitate the symptoms of appendicitis),
- in the lumbar region (imitate kidney colic);
· Painness, sometimes local, in the postoperative scar in the field of palpation, where it is forgiven
deepening.
The symptoms of the beginning breaking of the uterus on the header during pregnancy are determined by the presence of hematoma in the wall of the uterus due to the appearance of its walls and vessels. The symptoms of the threatening break are joined:
· Hypertonus of the uterus;
· Signs of acute hypoxia of the fetus;
· Possible blood discharge from sex tract.
The symptoms of the gap of the uterus during pregnancy: to the clinical picture of threatening and
the breakdowns began to be disgusted with the symptoms of pain and hemorrhagic shock:
· Worsen general state and well-being;
· Weakness appears, dizziness, which initially can be reflex genesis, and subsequently
determine blood loss;
· Explicit symptoms inside abdominal bleeding and hemorrhagic shock - tachycardia, hypotension, pallor of skin.
When the gap that occurred on the scar tissue, the li-shoe large amount of vessels, the bleeding in the abdominal cavity can be moderate or insignificant. In such cases, symptoms associated with acute fetal hypoxia are symptoms.
Rales of the uterus on the rubber in childbirth
Rassengers of the uterus in labor in childbirth occur in the presence of postoperative scars on the uterus or dystrophic changes in it, in the most meant.
The threatening rupture of the uterus in childbirth is characterized by the following symptoms:
·nausea;
· Vomiting;
· Pain in epigastrics;
· Various options for violation of contractual activity of the uterus - Discordination or weakness of generic activity, especially after the influence of spindle water;
· Pains of bouts that are not suitable for their strength;
· Restless behavior of the feminine, combined with a weak generic activity;
· Delayed fetus progress with complete cervical disclosure.
When the uterine breaks began in the first period of labor in connection with the presence of hematoma in the uterus wall appear:
· Permanent, not relaxing voltage of the uterus (hypertonus);
· Palcision in palpation in the field of the lower segment or in the region of the alleged scar if available;
· Signs of fetal hypoxia;
· Blood selection from sex tract.
· Most of the labels of the time interval from the appearance of sympto-mov started the gap until the moment
the percent is calculated by a minute.
The clinic of the gap of the uterus on the header is similar to the observed during pregnancy - mostly these signs of hemorrhagic sho and the antenatal fetal death.
With a vaginal study, it is characteristic of the definition of a single-standing movable head, previously pressed or tight in the entrance to the pelvis.
If the rupture of the uterus on the heading occurs in the second period of birth, the symptoms are not clear:
· Weak, but painful swells, gradually weakening up to termination;
· Pain at the bottom of the abdomen, the sacrum;
· Blood discharge from the vagina;
· Acute hypoxia of the fetus with its possible death.
Sometimes the rupture of the uterus on the heading occurs with the last fertilization. In this case, the diagnostic break is very difficult. The child is born sau-reproduce, alive, without asphyxia. Independently separates the placenta, it is born, and only the sympto, associated with hemorrhagic shock, which seems to be "undue" hypo-tenys, sometimes gradually increasing the symptoms of the epigastrics. It is possible to clarify the diagnosis only with a manual examination of the uterus or with laparoscopy.
The incomplete rupture of the uterus can occur in any period of childbirth.
Diagnosis of pregnancy complications in women with a scar at the uterus is based on a thorough collection of history, physical examination data and laboratory data.
Careful history of the history should include obtaining information about the COP time produced in the past, the presence of spontaneous delivery to operational intervention and after, the number of pregnancy between the operation and the present pregnancy, their results (abortion, miscarriage, underdeveloped pregnancy), On the presence of living children, cases of grams and death of children after previous birth, about the course of real pregnancy.
It should be palpatorically evaluate the scar on the front abdominal wall and in the uterus, measure the size of the pelvis and determine the intended mass of the fetus. In 38-39 weeks, gestation is evaluating the preparedness of the body pregnant to childbirth.
·General blood analysis.
·General urine analysis.
· Biochemical blood test (determination of the concentration of general protein, albumin, urea, creatinine, residual nitrogen, glucose, electrolytes, direct and indirect bilirubin, activity of alanine-substransferase, aspartate aminotransferase and alkaline phosphatase).
· Coagulogram, hemostasiogram.
· Hormonal status of FPK (concentration of placental lactogen, progesterone, estriot, cortisol) and assessment of the content of A-fetoprotein.
· Ultrasound of the fetus with dopplerometry of vessels of umbilical bodies, fetal aorts, fetal average artery and placenta are shown since the end of the II trimester of pregnancy.
· Cardiomonitorial observation of the state of the fetus.
· Ultrasound scar on the uterus every 7-10 days.
Diagnostics of the state of the scar on the uterus outside pregnancy
All women with the scar on the uterus after the cesarean operation should be taken to the dispensary accounting immediately after discharge from the hospital. The main purpose of the dispensary observation is early diagnosis and the treatment of late complications of the operation (genital fistulas, dupal education) and pregnancy prevention during the first year after surgery. During lactation for the purpose of hormonal contraception, Linestrenol (Gestagen) is used, which does not provide negative influence on a newborn. After the end of the lactation, estrogentaged contraceptives are prescribed.
In a complex of measures to prepare for the next pregnancy, an important role is played by the status of the state of the scar in the uterus. Informative methods for determining the state of the scar on the uterus in the discern, consider hysterography, hysteroscopy and ultrasound examination (ultrasound).
· Hysterography is produced on the 7th or 8th day of the menstrual cycle (but not earlier than 6 months after surgery) in a straight and lateral projection. With this method, you can study changes in the inner surface of the postoperative scar in the uterus. Highlight the following signs The inconsistency of the postoperative scar: change in the state of the uterus in a small pelvis (a significant displacement of the uterus of the sworded), served and thinned contours of the inner surface of the uterus in the zone of the alleged scar, "niche" and defects.
· Hysteroscopy is made on the 4th or 5th day of the menstrual cycle, when the functional layer of the endometrium is completely discounted, and through a thin basal layer is visible to be fabric. In the insolvency of the scar, they usually mark retraction or thickening in the scar. The whispering color of the scar cloth, the absence of vessels indicate a pronounced predominance of the connective tissue component, and the intensity of the intensity of myometrium as a result of defective regeneration. The forecast for nullifying pregnancy and delivery through the natural generic paths is borticulture. An unmarried dairy scar and a scar with a predominance of muscle tissue serve as a sign of its anatomical and morphological usefulness. These women have a pregnancy on 1-2 years after surgery.
· The ultrasound signs of the insolvency of the scar in the uterus include an uneven contour on the rear wall of the filled bladder, thinning of the myometrium, the intermittent of the contours of the scar, a significant amount of hyperheogenic inclusions (connective tissue). With a two-dimensional ultrasound, pathological changes in the area of \u200b\u200bthe scar on the uterus are found much less frequently than with hysteroscopy (in 56 and 85% of cases, respectively). However, due to the Dopplerometry and three-dimensional reconstruction, with the help of which hemodynamics can be estimated in the RubE (development of the vascular network), the informativeness of the ultrasonic assessment of the state of the scar in the uterus increased significantly.
The obtained results of additional methods for diagnosing the state of the scar on the uterus outside of pregnancy are entered into an outpatient card and they are taken into account when solving the question of the possibility of planning subsequent pregnancy.
Differential diagnosis is needed between the true threat of the abortion of pregnancy and the presence of an insolvent scar on the uterus (Table 52-6). Also necessary differential diagnosis acute appendicitis and kidney colic. Clarification of the diagnosis is carried out in hospital conditions on the basis of clinical symptoms, Data ultrasound, effect of therapy. In the presence of an insolvent scar on the uterus, the pregnant woman should be in the hospital before the delivery. In this case, a clinical assessment of the condition of pregnant, fetus and scar in the uterus is carried out daily. Ultrasound repeat every week. With increasing clinical or ultrasound symptoms of the insolvency of the scar, the uterus shows the operational delivery on the life testimony from the mother, regardless of the period of pregnancy.
Table 52-6. Differential diagnosis Threats of abortion of pregnancy and failure of the scar on the uterus after cesarean section in the lower uterine segment
Indications for consultation of other specialists
The consultation of the anesthesiologist is shown in case of the need for anesthesiological support of operational delivery or in order to anestheticing of labor.
· Pregnancy 32 weeks. Head prepayment of the fetus. Inspectorate in the uterus after Cesarean sections in 2002, Majdanka pregnant. Anemia I degree.
· Pregnancy 38 weeks. Head prepayment of the fetus. Scar in the uterus after the cesarean section in 2006 placental insufficiency. SIR I degree. Combined gestosis middle degree Severity 8 points against the background of arterial hypertension.
· Pregnancy 37 weeks. The scars on the uterus after Momectomy and the Small Caesarean section in 2000 an elderoous elderoous.
· Pregnancy 36 weeks. Pelvic prevention of the fetus. Scar in the uterus after corporate cesarean sections in 1999 anemia.
Complications of gestation in the presence of a scar on the uterus
Pregnancy during the presence of a scar on the uterus after cesarean section has a number clinical features. These patients have a low location or prelation of the placenta, the true rotation of it, the improper position of the fetus, and during the localization of the placenta in the scar region in the uterus it is often developing Mon.
One of the most frequent complications of the process of gestation in pregnant women with the scar in the uterus is the threat of abortion. Symptoms of the threat of interrupts in the first trimester of pregnancy do not have etiological communication with the presence of a scar in the uterus. The preserving therapy is prescribed according to the established diagnosis (insufficiency of progesterone synthesis, hyperandrogenation, APS, etc.). Perhaps treatment in outpatient conditions is possible, but if there is no effect, hospitalization is required to clarify the diagnosis and correction of the therapy. When identifying erection - cervical insufficiency, the surgical correction of this pathology in this contingent of patients is not shown, since the presence of a scar on the uterus in combination with the threat of pregnancy interruption can lead to a rupture of the uterus. The treatment of this complication includes antispasmodic therapy, the purpose of magnesium sulfate, bedding, the use of unloading vaginal pessary. The treatment of other pregnancy complications in women with the operated uterus is not fundamentally different from the generally accepted.
Maintaining pregnant women with scar in the uterus
During pregnancy (in the first trimester), a general examination is carried out, and if necessary, consultation of related specialists. Be sure to appoint an ultrasound, the main purpose of which is to determine the place of attachment of the fetal egg in the uterus. If it is located in the region of the coil on the front wall of the uterus (in the scar zone after cesarean section in the lower uterine segment) it is advisable to interrupt pregnancy, which is made using a vacuum aspirator. This tactic is related to the fact that the proteolytic properties of chorion as pregnancy progressing can lead to inferiority of even the wealthy scar on the uterus and its discontinuity, and only a repeated caesarean section is the outcome of this pregnancy. However, absolute contraindications for prolongation of pregnancy in this case are not, and the question of the abortion of pregnancy is solved by the woman itself. The following screening examination, including ultrasound and study of the hormonal status of the fetoplacentar complex (FPK), are carried out on the period of 20-22 weeks of pregnancy and its goal is to diagnose the malformations of the fetus, compliance with its size of gestation, signs of placental insufficiency (PN), especially when the placenta is located in the scar area. For the treatment of PN is shown hospitalization in the hospital. With an uncomplicated course of pregnancy and a wealthy scar, the next integrated examination is carried out on the period of 37-38 weeks of gestation in the hospital, where they are supposed to carry out a pregnant women.
In childbirth, antispasmodic, sedative and antihypoxic preparations are used, medicinal products, Improving populatory blood flow.
Rostroduction of pregnant women with a scar in the uterus
Rhodework of pregnant women with a scar in the uterus after cesarean sections
Most obstetrics have a major postulate when pregnant with pregnant women with a scar in the uterus after Cesarean sections: one caesarean section is always a cesarean section. However, both in our country and abroad, it has been proven that 50-80% of pregnant women with a operated uterus are not only possible, but also preferably genera through natural generic paths. The risk during re-caesarean section, especially for the mother, is higher than the risk in spontaneous childbirth.
Spontaneous childbirth in pregnant women with a scar on the uterus after cesarean section
Conducting birth through natural generic paths in the presence of a scar on the uterus after cesarean section is permissible when complying with a number of conditions.
· One caesarean cross section in a cross-cut in the uterus in the lower segment.
· Lack of extragenital diseases and obstetric complications who served as indications for the first operation.
· The wealth of the scar in the uterus (according to the results of clinical and instrumental research).
· Localization of placenta outside the scar on the uterus.
· Head prediction of the fetus.
· Compliance of the size of the pelvic of the mother and the head of the fetus.
· The presence of conditions for emergency delivery by the cesarean section (highly qualified medical personnel, the possibility of carrying caesarean section in an emergency order no later than 15 minutes after the decision on the operation).
The question of the method of delivery should be necessarily agreed with a pregnant woman. Akuster should explain in detail all the advantages and risk, both re-caesarean section and childbirth through natural generic paths. The final decision must be taken by the Woman herself in the form of a written informed consent to one of the methods of delivery. In the absence of absolute testimony to the planned caesarean section, preference should be given to childbirth through natural generics, and, with their spontaneous principle.
Childbirth in the presence of a scar in the uterus, as a rule, proceed according to the standard mechanism characteristic of primary or repeatedly. The most frequent complications of childbirth in women with the scar in the uterus are the late influence of the oily water, the anomalies of the generic activity (which should be considered as a threat of the uterus breaking), the clinical inconsistency of the size of the pelvic of the mother's pelvic and the head of the fetus (caused by more frequent than in the population, the location of the fetus head in In addition), the appearance of signs of the uterine threatening break. In the process of childbirth, continuous cardiomonitorial control over the state of the fetus is needed, with clinical assessment The nature of the generic activity and state of the scar on the uterus. Births should be conducted with an expanded operating room, with an infusion system connected. In addition to clinical (palpation) assessment of the state of the scar in the uterus in the process of spontaneous delivery, you can use the ultrasound, with the help of which, in addition to estimating the state of the scar, in the uterine period, clarify the type and position of the fetus, the location of the fetus head in relation to the planes of the small pellery pelvic, produce cervicometry (Ultrasonic registration of the opening of the uterine zoom), due to which the number of vaginal research is reduced, which is useful in terms of the prevention of infectious complications in the fever with a high probability of operational delivery.
The anesthesia of childbirth in women with the scar in the uterus is carried out according to the generally accepted rules, including using epidural analgesia. The method of anesthesiological manual in childbirth depends on the nature of an extragnenital or other obstetric pathology.
The scar in the uterine after cesarean sections do not consider contraindication to use in the birth of other obstetric and anesthesiological benefits, such as generics or relatives. With the period II, the period of childbirth or the hypoxia of the fetus began to speed up the crotch dissection. With acute hypoxia of the fetus and the head, which is in a narrow part of the cavity of the small pelvis, the birth can be completed by the imposition of obstetric tongs or vacuum extractor.
Mandatory consider manual examination of the uterus immediately after delivery in the absence of ultrasound control.
The symptoms of the uterine break may appear through considerable time after the delivery, therefore it is advisable to repeated ultrasound 2 hours after delivery in order to diagnose separating retrosic hematomas, which are due to the undiagnosed breaking of the uterus.
Indications for Cesarean section with a scar on the uterus after cesarean section:
· Scar on the uterus after corporate cesarean sections.
· Insolvennial scar in the uterus on clinical and eultrazvoy.
· Prelation of the placenta.
· Two or more scars on the uterus after cesaric sections.
· Categorical failure of a woman from childbirth through natural generic paths.
Conducting birth to women with a scar in the uterus after Momectomy
When choosing the method of root separation in women with the scar in the uterus after the Miom Extractive, the character and volume of the operation performed is determined. The frequency of insolvent scars after momectomy reaches 21.3%. The risk of rupture of the uterus on the header after momectomy in the process of spontaneous genera depends on the depth of the tumor in the myometry (interstitial, submosozno-interstitial, sub-sisterial or submucose mioma) before surgical intervention, methods of operation, the localization of the scar on the uterus. Indications for operational delivery are absolute and relative. Absolute readings to Cesarean section after momectomy outside pregnancy are shown below.
· Scar on the uterus after removing the interstitial or subserosan-interstitial node located on the rear wall of the uterus.
· Scar on the uterus after the removal of intraline matoma.
· Scars in the uterus after removing several interstitial-tore-sized nodes.
When pregnant with pregnant women with the scar in the uterus after Miomectomy outside the pregnancy and the absence of absolute testimony to cesarean section, it is preferable to behave through the natural generic paths. In the presence of a burdened obstetric anamnesis, transferred pregnancy, the pelvic presence of the fetus, the Mon, the age of the primary older than 30 years of testimony to the cesarean section after Momectomy expand.
The scar in the uterus after Momectomy produced during pregnancy serves as a testimony to Cesarean section.
Conducting birth to women with a scar in the uterus after reconstructive plastic operations
· After the metroplasty, preference should be given to Cesarean section in order to prevent maternal injuries in spontaneous childbirth.
· After removing the rudimentary horns of the uterus without opening its main cavity, childbirth is possible through the natural generic paths.
Conducting birth to women with scar on the uterus after the uterus perforation
Births after the uterus perforation during intrauterine interventions is a complex and responsible task. The location of the perforation hole relative to the walls of the uterus is of great importance. The location of the scar in the region is considered prognostically unfavorable and on the rear wall of the uterus. When conducting such clans, uterine breaks, hypotonic bleeding, the pathology of the placenta separation, especially in women with a complicated flow of the operation itself and the postoperative period are possible.
The obstetric forecast is more favorable in those cases where the scar is located on the front wall of the uterus, and the operation was limited only by stitching the perforation opening without additional dissection of the uterus wall. In the absence of complicating circumstances, labor is possible through natural generics, followed by a control manual examination of the walls of the uterine cavity.
Conducting birth to women with scar on the uterus after ectopic pregnancy
The choice of the method of root separation after transferred ectopic pregnancy depends on the volume of the transferred operation and the age of a woman. Operational interventions about the cereal pregnancy, pregnancy in Rudimentary Rog of the uterus (if it has a message with the main cavity), the interstitial separation of the uterine pipe, the cult of remote early pipes serve as an indication to the cesarean operation.
Forecasting and prevention of gestation complications
Pregnant women with the scar at the uterus consider the risk group to develop the following obstetric and perinatal complications: spontaneous abortion, breaking uterus on the header, premature genera, mon, hypoxia and intrauterine death of the fetus, generic injuries of mother and fetus, high maternal and perinatal mortality. For the prevention of these complications, it is necessary to carefully dispensary observation For pregnant women, timely identification of complications and their treatment in multidisciplinary obstetric hospitals. The prevention of complications is based on the wide propaganda of the pregranting preparation of women with the scar on the uterus, which includes the following events.
· Informing about risk associated with the presence of a scar in the uterus.
- Mother's risk: uterus break through the head, bleeding, maternal mortality, purulent-septic complications; Unbearable pregnancy.
- risk for the fetus and newborn: prematurity, generic injury, neonatal complications various degrees severity.
· Diagnosis and treatment of related gynecological and extragenital diseases before pregnancy.
· Survey on infections transmitted by the sexual way (STIs) and the sanitation of foci of infection.
Treatment of complications in childbirth and postpartum period
The most terrible complication in childbirth is the rupture of the uterus on the head. When conducting birth through natural generics, women with the scar in the uterus should be given preference to the hyperdiagnosis of the uterus break, rather than the underestimation of such a serious complication. It is extremely difficult to evaluate the first symptoms of the beginning breaking of the uterus on the head. The diagnostics of the uterus breaks are carried out taking into account the clinical picture: pain in the epigastric region, nausea, vomiting, tachycardia, local pain, blood discharge from sex tract, shock, etc. Signs of deterioration of the state of the fetus, the weakening of the contractile activity of the uterus can be the symptoms of the starting break, and often first. Invaluable importance in childbirth additional methods diagnostics (ultrasound, turkey).
There is a complete gap and incomplete rupture of the uterus (bundle, spreading the scar) when the peritonean remains intact. Tactics When breaking the uterus consists in emergency cesarean sections. The volume of operational intervention depends on the extensity of the injury: when the uterus breaks only in the region of the scar after extracting the fetus, the scar is excised and sewing the uterus, and when the uterus, complicated by the formation of intraligent hematomas, produce its extirpation. With subsequent pregnancy, the operational delivery is shown.
The testimony to the cesarean section in childbirth is expanding with the negative dynamics of the state of the fetus, the appearance of clinical signs of the uterine threatening break, the absence of conditions for the careful spontaneous completion of labor.
Prevention of the rupture of the uterus on the head
The prevention of the uterine break through the header is to hold the following events.
· Creation of optimal conditions for the formation of a wealthy scar at the uterus at the first cesarean section (incision on the uterus on Derfler) and other operations in the uterus: sewing a cut on the uterus with individual muscle-muscular seams using synthetic absorbable suture threads (Vincle, Monophil, etc.) .
· Forecasting, prevention, timely diagnosis and adequate therapy of postoperative complications.
· An objective assessment of the state of the scar in the uterus before the occurrence of pregnancy and during gestation.
· Screening examination during pregnancy.
· Careful selection of pregnant women to keep births through natural generic paths.
· Careful cardiotokographic and ultrasound control in the process of spontaneous delivery.
· Adequate anesthesia in the process of spontaneous delivery.
· Timely diagnosis of threatening and / or start-up uterus.
Infiltrate after surgery is one of the most frequent complications after surgery. It can develop after any operation - if you cut out appendicitis, removed the hernia or even just made the injection.
Therefore, it is important to closely monitor your condition after operational intervention. To cure such a complication is quite simple if it is diagnosed on time. But if you tighten, it can turn into an abscess, and this is already fraught with a breakthrough of uphtic and infection of blood.
What it is?
The term itself is a merger of two Latin words: in - "B" and Filtratus - "Reussed". Doctologists call this word the pathological process when particles of cells accumulate inside the tissues or any organ (in the numbers), blood, lymph itself. Externally, it looks like a dense education, but simply a tumor.
There are 2 main forms of such a phenomenon - inflammatory (this is usually complications after surgery) and tumor. Inside the second formation is not innocent blood and lymph, but tumor cells, and very often - cancer. Sometimes doctors refer to the infiltrate of a plot on the body where anesthetic, antibiotic or other substances are introduced in the treatment. This species is called "surgical".
The inflammatory process can begin even before the operation. Particularly diagnose appendicular infiltrate, which develops almost in parallel with the inflammation of the appendix. It meets even more often than complication after the appendicitis surgery. Another "popular" option is a tumor in the mouth of the kids, the reason is a fibrous pulpit.
Varieties
Inflammatory infiltrate is the main type of such pathology, which often appears after operational intervention. There are several types of such inflammation, depending on which cells inside the tumor most.
- Purulent (inside polymorphous leukocytes gathered).
- Hemorrhagic (red blood cells).
- Circular cell, or lymphoid (lymphoid cells).
- Histiocyte-plasma-cell (inside plasma elements and histiocytes).
Inflammation of any nature can develop in several directions - or distribute over time (1-2 months), or turn into an ugly scar, or develop in abscess.
A special kind of inflammatory scientists consider infiltrate postoperative seam. Such a disease is particularly covered - it can "jump out" and in a week or other after the operation, and after 2 years. The second option is, for example, after cesarean section, and the risk that inflammation will turn into an abscess, quite high.
The reasons
From the emergence of purulent, hemorrhagic and other formations after surgery, no one is insured. Complication occurs in small children, and in adult patients, after a banal appendicitis and after the operation to remove the uterus (Paracervical and other tumors).
Specialists call 3 main reasons for such a phenomena - injury, odontogenic infections (in the oral cavity) and other infectious processes. If you fell to the doctor due to the fact that the postoperative seam inflamed, another number of reasons are added:
- infection fell into the wound;
- postoperative drainage was incorrectly carried out (usually in overweight patients);
- the supervision of the surgeon was damaged by a layer of subcutaneous fatty fiber, and hematoma appeared;
- suture material has a high tissue reactivity.
If the scar is inflamed only in a few months or years after surgical manipulations, it is the suture material. Such pathology is called ligatural (ligature is a dressing thread).
We also provoke pathology may also tend to allergies in a patient, weak immunity, Chronic infections, congenital diseases, etc.
Symptoms
Postoperative complication is not developing immediately - usually on the 4-6th day after hours x (surgery). Sometimes later - after a half or two weeks. The main signs of beginning inflammation in the wound is:
- subfebrile temperature (rises only for several divisions, but it is impossible to knock it down);
- when pressed to the inflamed place, pain feels;
- if you press very much, a small hole appears, which is gradually straightened;
- the skin in the affected area swell and blushes.
If the tumor arose after the operation to remove pahnova grozhiOther symptoms can be added. The pathological accumulation of cells in the abdominal cavity will be said to:
- painful pain in the field of peritoneum;
- problems with intestines (constipation);
- hyperemia (strong blood flow to patient places).
With hyperemia, swelling occurs and furunculay jump out, heartbeat, patients are tormented by headaches.
What is post-relieving infiltrate?
Infiltrate after an injection is one of the most frequent complications after injection, along with hematomas. It looks like a small tight shower on the place where the needle with a medicine was sticking. The predisposition to such a mini-complication is usually individual: someone has a seal on the skin after each injection, and someone has never come across such a problem with such a problem.
The following reasons may provoke a similar reaction of the body for a banal injection:
- the nurse had a bad antiseptic processing;
- the needle in the syringe is too short or stupid;
- incorrectly selected place for injection;
- injections make constantly at the same place;
- the medicine is injected too quickly.
Such sore can be cured by ordinary physiotherapy, iodine mesh or compresses with diluted domexide. Help I. folk Methods: Compresses from cabbage sheet, aloe, burdock. For greater efficiency, the compress can be lubricated with honey.
Diagnostics
Diagnose such postoperative pathology is usually not difficult. The doctor when making a diagnosis relies, first of all, on the symptoms: temperature (which and how much), the nature and intensity of pain, etc.
Most often, the tumor is determined during palpation - it is a dense formation with uneven and fuzzy edges, which spokes up with pricks. But if surgical manipulations were carried out on the abdominal cavity, the seal can hide deep inside. And with the finger inspection, the doctor simply will not find it.
In this case, more informative diagnostic methods come to the rescue - ultrasound and computed tomography.
Another mandatory diagnostic procedure is a biopsy. The tissue analysis will help to understand the nature of inflammation, find out which cells accumulated inside, install, whether there are malignant among them. This will determine the cause of the problem and correctly draw up a treatment scheme.
Treatment
The main goal in the treatment of postoperative infiltrate is to remove inflammation and prevent the development of abscess. To do this, it is necessary to restore blood flow in the sore place, remove the edema and eliminate pain syndrome. Used primarily conservative therapy:
- Antibiotic treatment (if infection is caused by bacteria).
- Symptomatic therapy.
- Local hypothermia (artificial decrease in body temperature).
- Physiotherapy.
- Bed regime.
Effective procedures are considered UV irradiation of wounds, laser therapy, mud and others. The only contraindication for physiotherapy is purulent inflammation. In this case, the warming and other procedures will only accelerate the spread of the infection and can cause abscess.
With the appearance of the first signs of abscess, a minimally invasive intervention is used first - the drainage of the affected area (under the control of ultrasound). In the most difficult cases, the shell is opened in the usual way using laparoscopy or laparotomy.
The treatment of postoperative seam with complications is also traditionally carried out with conservative methods: Antibiotics, Novocaine blockade, physiotherapy. If the tumor did not disappear, the seam is opened, cleaned and sewn again.
Infiltrate after surgery may form in a patient of any age and health status. By itself, this tumor is usually no harm, but it can serve as the initial stage of abscess - severe purulent inflammation. The danger also is that sometimes pathology develops a few years after the visit to the operating room when the scar is inflamed. Therefore, it is necessary to know all signs of such a disease and with the slightest suspicions to contact the doctor. This will help to avoid new complications and additional surgical interventions.
Article for site. "Health recipes" Prepared Nadezhda Zhukov.
* Pressing the "Send" button I agree with
Source: Zdorovieiuspex.ru.