Treatment. Acute appendicitis. Etiology. Pathogenesis. Classification. Clinic. Diagnostics. Treatment OA - right-sided renal colic
Acute appendicitis - literally inflammation of a worm-like process. A worm-shaped process departs from the head-frenched segment of the blind intestine in the place where the three tape muscles of the blind intestine begin. It is a subtle convolve tube whose cavity on one side is reported to the cavity of the blind intestine. The process ends blindly. Its length ranges from 7 to 10 cm, often reaching 15 - 25 cm, the diameter of the channel does not exceed 4 - 5 mm.
The Cell-shaping process from all sides is covered with peritoneum and in most observations has a mesentery that does not prevent his movement.
Depending on the position of the blind intestine, a worm-shaped process may be in the right iliac hole, above the blind intestine (at a high position), below the blind intestine, in a small pelvis (at its low position), together with a blind intestine among loops fine intestine In the midline, even in the left half of the abdomen. Depending on its location and an appropriate disease clinic arises.
Acute appendicitis- non-specific inflammation of a worm-like process caused by gloty microbes (streptococci, staphylococci, enterococci, intestinal wand, etc.).
Microbes enter it enterogenic (the most frequent and most likely), hematogenic and lymphogenic path.
With palpation of the abdominal abdominal abdominal muscles, the muscles of the front abdominal wall are tense. The pain in the localization site of the heart-shaped process during palpation is the main, and sometimes the only sign of acute appendicitis. To a greater extent, it is expressed in destructive forms of acute appendicitis and especially when perforations of a worm-like process.
An early and equally important sign of acute appendicitis is the local stress of the muscles of the anterior abdominal wall of the abdomen, which is more often limited to the right iliac region, but can spread to the right half of the abdomen or throughout the front abdominal wall. The degree of tension of the muscles of the anterior abdominal wall depends on the reactivity of the body on the development of the inflammatory process in a worm-like process. With reduced reactivity of the body in exhausted patients and elderly, this symptom may be absent.
In suspected of acute appendicitis, vaginal (in women) and rectal research should be carried out, at which it is possible to determine the soreness of the pelvic peritoneum.
An important diagnostic value in acute appendicitis has a symptom of brush-blubberg. To determine it with the right hand, carefully pressed onto the front abdominal wall and after a few seconds it takes off from the abdominal wall, while there is a sharp pain or a noticeable increase in pain in the field of inflammatory pathological focus in the abdominal cavity. With destructive appendicitis and especially with perforations of a worm-like process, this symptom is positive throughout the right half of the abdomen or throughout the abdomen. However, the symptom of Brush - Blumberg may be positive not only with acute appendicitis, but also with other acute diseases of the abdominal organs.
The symptoms of Voskresensky, Rovzing, Sitkovsky, Bartaje, Michelson, Exello, have a certain meaning in the diagnosis of acute appendicitis.
With symptom Resurrectionthe pain appears in the right iliac region with the rapid palm through the tight shirt of the patient along the front wall of the belly to the right of the root edge down. On the left, this symptom is not defined.
Symptom Rovingand caused by pressing or pushing the palm in the left ileal area. At the same time, in the right iliac region, the pain occurs, which is binding to the sudden movement of gases from the left half of the large intestine to the right, as a result of which fluctuations in the walls of the intestine and the inflamed worm-like transformation transmitted to inflammatory-changed parietal peritoneum.
With symptom Sitkovskyin a patient lying on the left side, a pain appears in the right iliac region, caused by the tension of the inflammatoryly altered peritoneum in the area of \u200b\u200bthe blind intestine and the mesentery of a worm-like process due to its climbing.
Symptom Batomier - Michelson- pain in palpation of the right iliac region in the position of the patient on the left side.
Symptom Example- pain in palpation of the right iliac region at the time of raising the straightened right leg.
The critical and objective assessment of these symptoms is expanding the possibility of establishing a diagnosis of acute appendicitis. However, the diagnosis of this disease should not be based on one of these symptoms, but on the comprehensive analysis of all local and general signs of this acute disease of the abdominal organs.
To form a diagnosis of acute appendicitis, blood test is of great importance. Changes in the blood are manifested by an increase in leukocytes. The severity of the inflammatory process is determined using the leukocytic formula. The leukocytic formula shift is left, i.e., an increase in the number of laid neutrophils or the appearance of other forms with a normal or insignificant increase in the number of leukocytes, indicates severe intoxication in the destructive forms of acute appendicitis.
Several forms of acute appendicitis are isolated (according to histology):
1) catarler;
2) phlegmonous;
3) gangrenous;
4) gangrenous-perforative.
Differential diagnosis of acute appendicitis
The acute diseases of the abdominal organs have a number of major symptoms:
1) pain of different character;
2) reflex vomiting;
3) disorder of the normal leaving of intestinal gases and feces;
Prior to the establishment of a specific diagnosis of acute abdomen's disease, painkillers cannot be prescribed (drug use relieves pain and smoothes the clinical picture of acute abdominal organs), rinse the stomach, apply laxative, cleansing enemas and thermal procedures.
The acute diseases of the abdominal organs are easier to differentiate in initial stage Diseases. Subsequently, when peritonite develops, its source is very difficult to determine its source. It is necessary to remember in this regard to the figurative expression Yu. Yu. Janelidze: "When the whole house flares - it is impossible to find a fire source."
Acute appendicitis must be differentiated from:
1) acute diseases Stomach - acute gastritis, food toxicoinfection, perforative stomach ulcers and duodenal gut;
2) some acute diseases of the gallbladder and the pancreas (acute cholecystitis, bile sickness, acute pancreatitis, acute cholecystopancatitis);
3) some bowel diseases (acute enteritis or enterocolite, acute ileit, acute diverticulitis and its perforation, acute intestinal obstruction, crown disease, terminal ileit
4) certain diseases of the female sexual sphere (acute inflammation of the mucous membrane and the walls of the uterus, pelvioperitonite, ectopic pregnancy, ovarian break, twisted ovarian cysts);
5) urological diseases (renal disease, renal colic, pelitis);
6) other diseases that simulate acute appendicitis (acute diaphragmal pleuritis and pleuropneumonia, heart disease).
Treatment of acute appendicitis
Currently, the only method of treating patients with acute appendicitis is an early emergency operation, and the earlier it is carried out, the better the results. Mr. Mondor (1937) indicated: when all doctors infiltrate this thought, when they would understand the need for quick diagnosis and immediate operational intervention, they do not have to deal more with severe peritonitis, with cases of heavy suppuration, with those distant infectious complications, Which and currently too often darken appendicitis forecast.
Thus, the diagnosis of acute appendicitis requires an immediate operation. The exceptions are patients with the presence of limited appendicular infiltrate and patients requiring short-term preoperative preparation.
The phenomena of acute appendicitis can be found in patients with myocardial infarction, severe pneumonia, with acute violations of cerebral circulation, decompensated heart disease. For such patients set dynamic observation. If in the process of observation, the clinical picture does not subside, then according to life indications they are resorted to the operation. With acute appendicitis complicated by peritonitis, despite the severity of a somatic disease, after the corresponding preoperative preparation of the patient operates.
A number of authors indicate that in a complex of therapeutic measures in this category of patients with acute appendicitis, preoperative preparation is of great importance, which serves as one of the means of reducing the risk of operational intervention, improves the overall condition of the patient, normalizes the indicators of homeostasis, strengthens the immuno-proof mechanisms. It should not last more than 1 - 2 hours.
If at appendectomy it is impossible to use intubation anesthesia with muscle relaxants, then local infiltration anesthesia is used with a 0.25% novocaine solution, which can be combined with neuroleptanalgesia with the corresponding indications.
However, it is necessary to give preference to modern endotracheal anesthesia using muscle relaxants, in which the surgeon has a maximum possibility to conduct a thorough audit of the abdominal organs.
With light forms of acute appendicitis, where the operation is short, Appendectomy can be carried out under masculine anesthesia using muscle relaxants.
The most common access with uncomplicated acute appendicitis is the oblique incision of Volkovich - McBernia. Several less often the incision proposed by Lennander is applied during the atypical arrangement of a worm-like process, a common purulent peritonitis caused by perforation of a worm-like process, as well as with the possible appearance of peritonitis from other sources, when a wider audit of the abdominal organs is necessary. The advantage of the incision of Volkovich - Mac Bernia is that it corresponds to the projection of the blind intestine, the nerves and muscles do not charge with it, which reduces the frequency of appearance in this area of \u200b\u200bhernia.
Transverse access is convenient because it can be easily expanded by medially, by crossing the abdominal muscle.
In most cases after appendectomy abdominal cavity Scroll tightly.
If, with a probulizing appendicitis in the abdominal cavity, there is a lot of effusion, which is removed by gauze tampons, electrotoxos, then a thin rubber tube (polychlorvinyl) is inserted into it for intraperitoneal administration of antibiotics.
With destructive forms of acute appendicitis in the postoperative period, antibiotics are prescribed intramuscularly, while the patient's sensitivity is taken into account.
The proper maintenance of patients in the postoperative period largely determines the results of operational intervention, especially in destructive forms of acute appendicitis. The active behavior of patients after surgery warns the development of many complications.
With uncomplicated forms of acute appendicitis, the patient's condition is usually satisfactory, and in the postoperative period of special treatment is not required.
After delivery from the operating room in the ward, the patient can immediately be allowed to rotate on the side, change the position of the body, breathe deeply, flick.
Stacking from bed must begin gradually. On the first day, the patient can sit in bed and start walking, but he should not overpowance for the sake of early row. To this question, it is necessary to approach strictly individually. A crucial role is played by good health and mood of the patient. It is necessary to start early nutrition of patients, which reduces the frequency of intestinal paresis and contributes to the normal function of the digestive organs. Patients prescribe easily digestible food, without overloading the gastrointestinal tract, from the sixth day they are translated into a shared table.
Most often after appendectomy, the chair itself happens on the 4th - 5th day. During the first two days, the gases are delayed due to the gash of the intestine, which is most often terminated independently.
In the postoperative period often there is a retention of urination as a result of the fact that most of the patients cannot urinate lying. To eliminate this complication to the crotch applied the heating. If the patient's condition allows, then it is allowed to get up near the bed, they are trying to cause a reflex to urinate, a stripping of the kettle. Intravenously can be administered with 5-10 ml of a 40% urotropin solution or 5 - 10 ml of a 5% solution of sulk acid magnesia. In the absence of the effect of these activities, the bladder catheterization with strict observance of the aseptic rules and mandatory washing after catheterization with a solution of furaticilline (1: 5000) or silver sulfate (1: 10 000, 1: 5000).
In the postoperative period, the healing physical education is of great importance.
If no changes were found during the operation of changes in a worm-like process, then the ileum revision should be conducted (for 1 - 1.5 m), so as not to miss the diverticulit.
Complications of acute appendicitis
Complications in the preoperative period. With a late treatment of a patient to a doctor, acute appendicitis can give a number of serious complications that threaten the life of the patient or for a long time deprive of its ability to work. The main, the most dangerous complications of the initially operated appendicitis are considered appendicular infiltrate, spilled purulent peritonitis, pelvic abscess, pylephlebit.
Apandicular infiltrate.This limited inflammatory tumor, which is formed around a destructively modified worm-like grip, to which fibrinous overlays, the intestinal loops are soldered, a large gland and close organs. Appendicular infiltrate is localized at the location of the draft-shaped process.
In the clinical course of appendicular infiltrate, two phases are distinguished: early (progression) and late (odds).
IN early stage Appendicular infiltrate just begins to form, it is soft, painful, without clear boundaries. His clinical picture is similar to the picture of acute destructive appendicitis. There are symptoms of peritonean irritation, leukocytosis with a leukocytic formula to the left.
In the late Stage clinical current It is characterized by a common satisfactory condition of the patient. The total and local inflammatory reactions subside, the temperature is in the range of 37.5 - 37.8 ° C, sometimes normal, the pulse is not participated. When palpation of the abdomen is determined by a low-skinned dense infiltration, which is clearly delimited from the free abdominal cavity.
After diagnosis, appendicular infiltrate is beginning to treat conservative: strict bed mode, food without a large amount of fiber, double-sided panefral blockade 0.25% novocaine solution in Vishnevsky, antibiotics.
After treatment, the appendicular infiltrate may resolve, with ineffective treatment - bother and form an appendicular abscess, replace with connecting tissue, not to dissolve and stored dense.
After 7-10 days after the resorption of the appendicular infiltrate, without writing the patient from the hospital, they are carried out by appendectomy (sometimes after 3 to 6 weeks after the resorption in a planned order during the reciprocal of the patient in the surgical hospital).
Apandicular infiltrate can be substituted with massive development connective tissue Without any tendency to resorption. Such form of infiltrate V. R. Brights called fibroplastic appendicitis. At the same time, a tumor-like formation is palpable in the right iliac region, and the symptoms of intermittent intestinal obstruction are manifested. Only histological examination after hemicultomy identifies the true cause of the pathological process.
If the appendicular infiltrate for 3 to 4 weeks is not absorbed, remains dense, then the presence of a tumor in the blind intestine should be assumed. For differential diagnosis, it is necessary to carry out irrigoscopy.
When the appendicular infiltration is transition to appendicular abscess, the patients have a high temperature of the intermitting nature, high leukocytosis with a leukocytic formula shift to the left, intoxication.
Pelvic appendicular abscess.May complicate pelvic appendicitis, and sometimes accompany phlegmonous or gangrenous forms of acute appendicitis.
In a pelvic appendicular abscess, purulent effusion falls on the bottom of the small pelvis and accumulates in the douglas space. Purulent content pushes up the loop thin gut, it is eliminated from the free abdominal cavity with spikes, which are formed between the intestinal loops, the large gland and the closed peritury.
Clinically pelvic appendicular abscess manifests pain in the depth of the pelvis, soreness when pressing over the pubic, bloating. In some cases, it may be vomiting, which causes relative dynamic intestinal obstruction due to the passage involved in the inflammatory process of loops of the small intestine.
For a pelvic appendicular abscess, a high temperature is characterized (up to 38 to 40 ° C), high leukocytosis with a leukocytic formula shift to the left. The tension of the muscles of the front abdominal wall of the belly is expressed weakly.
Of great importance for the diagnosis of the pelvic appendicular abscess have local symptoms of irritation adjacent to the antenna and tissues - the rectum, the bladder. At the same time there are frequent fruitless urges on the bottom, diarrhea with an admixture of mucus, the swelling of the mucous membrane around the rear passage, the sphincter is gaping. Urination is a rapid, painful, and sometimes its delay is observed. At the finger survey, the PER RECTUM on the front wall of the rectum is determined by fluctuating painful tumor-like education, which is detected by pus.
Treatment of pelvic infiltrate before the suppuration is the same as appendicular, with suppuration - operational (median incision with the drainage of the abdominal cavity).
Pilefelbit.This purulent thrombophlebitis of the portal vein is quite rare, but a very dangerous complication of acute appendicitis, which almost always ends with purulent hepatitis.
The initial symptoms of pylephlebit - an increase in temperature up to 38 - 40 ° C, the inventories indicating the developing purulent hepatitis, they are joined by a non-permanent nature of pain in the right hypochondrium. During palpation, a painful liver is determined, not very intense jaundice, high leukocytosis, is characteristic of the emerging. General state The patient is very heavy. With a x-ray study, there is a high standing and limiting the mobility of the right dome of the diaphragm, sometimes in the right pleural cavity Contracts.
Complications in the postoperative period.The classification of postoperative complications in acute appendicitis is based on a clinical and anatomical principle:
1. Complications from the operating room:
1) hematoma;
2) suppuration;
3) infiltrate;
4) the discrepancy between the edges without eventration;
5) the discrepancy between the edges with eventration;
6) ligatural fistula;
7) Bleeding from an abdominal wall wound.
2. Acute inflammatory processes in the abdominal cavity:
1) infiltrates and abscesses of the Ileocecal region;
2) abscesses Douglas Space;
3) interchess;
4) retroperitoneal;
5) subiaphragmal;
6) littering;
7) Local peritonitis;
8) Spilled peritonitis.
3. Complications from gastrointestinal tract:
1) dynamic intestinal obstruction;
2) acute mechanical intestinal obstruction;
3) intestinal fistula;
4) gastrointestinal bleeding.
4. Complications from the cardiovascular system:
1) cardiovascular failure;
2) thrombophlebitis;
3) pilephlegit;
4) Embolism of the pulmonary artery;
5) Bleeding in the abdominal cavity.
5. Complications from the respiratory system:
1) bronchitis;
2) pneumonia;
3) pleurisy (dry, exudative);
4) abscesses and gangrene of the lungs;
4) lung atelectasis.
6. Complications from the excretory system:
1) urine delay;
2) acute cystitis;
3) acute pylitis;
4) acute jade;
5) acute pyelcisitis.
Chronic appendicitis
Chronic appendicitis is usually evolving after an acute attack and is the result of the changes that occurred in the process during acute inflammation. In a draft-like process, there are sometimes changes in the form of scars, gears, adhesions with nearby organs that can cause a mucous membrane-like procession continues a chronic inflammatory process.
Clinical picture with different forms of chronic appendicitis, it is very diverse and not always quite characteristic. Most often, patients complain of permanent pain in the right iliac region, sometimes this pain wears an approaches.
If, after transferred to the attack of acute appendicitis, pain attacks in the abdominal cavity are periodically repeated, then such a form of chronic appendicitis is called recurrent.
In some cases, chronic appendicitis from the very beginning proceeds without an acute attack and is called primary chronic appendicitis or nevertheless.
In chronic appendicitis, some patients bind attacks in stomach pain with meals, others - with exercise, and many cannot call the reason for their appearance. Often they impose complaints about intestinal disorders, accompanied by constipation or diarrhea with uncertain pain at the bottom of the abdomen.
In the presence of patients with a history of one or more acute attacks of appendicitis, the diagnosis of chronic appendicitis sometimes does not pose much difficulties.
With an objective examination, patients with chronic appendicitis complain only for pain in palpation at the location of the draft-shaped process. However, this pain may be associated with other diseases of the abdominal bodies. Therefore, in the formulation of the diagnosis of "Chronic appendicitis", it is necessary to always exclude other diseases of the abdominal organs by careful and comprehensive surveys of the patient.
Chronic appendicitis must be differentiated from uncomplicated peptic disease stomach and duodenum, kidney disease, liver, etc.; chronic kidney diseases (pylits, renal disease); Chronic cholecystitis - duodenal probing, cholecystography. Women exclude chronic diseases Pods uterus. In addition, it is necessary to differentiate chronic appendicitis from glider invasion and tuberculous meso-aden.
Treatmentchronic appendicitis is surgical.
The technique of this operation is similar to the operation method with acute appendicitis.
Appendicitis is the pathological condition of the body, which is accompanied by the development of the inflammatory process in Appendix (the appointment of the rectum). This is a very dangerous phenomenon, so when the first symptoms appear, you need to immediately apply for medical help. Upon timely appeal to the doctor you can avoid serious consequences. What is appendicitis, how to remove and how to restore - all this will be discussed in this article.
Appendicitis - how to remove
Restaurant, Cell-shaped process or Appendix is \u200b\u200ba tubular formation, the length of which is 4-8 cm. The internal cavity of the appendix is \u200b\u200bfilled with lymphatic fluid, and the process itself is responsible for performing the protective functions of the body. Inside the process is useful microorganisms that contribute to the normalization of intestinal microflora. Many, unfortunately, do not know where the appendix is. It is located in the lower right of the belly. If a person suffers from a mirror disease, then appendix, respectively, is located on the left side of the abdominal cavity.
On a note! Among all countries, only in the United States it is customary to remove Appendix immediately after the birth of the child. Doctors argue that this process keeps in itself a lot of food waste, negatively affecting the condition of the whole organism. But, according to various studies, such operations negatively affect immune system Child.
Causes of inflammation
Despite the rapid development of modern medicine, doctors can not yet establish the exact causes of appendicitis. It is known only about two causal factors contributing to the development of alert:
- infection of intestines by pathogenic microorganisms;
- obrament of the lumen of appendix or blockage. In this case, the message disappears between the intestinal lumens and a worm-like process.
The following factors may result in blockage of the lumen:
- the accumulation of feces in the lumen of appendix. In this case, there is hardening of the feces, as a result of which infection may occur;
- excessive use of various bones from fruits or seeds. After the bones or seeds in large numbers fall into the bowel cavity, they can lead to blockage;
- the presence of foreign bodies (most often - small toy parts). As a rule, the presence of alien items acts as the reason for the development of appendicitis in small children, which are constantly pulling everything in the mouth.
The danger of the disease is that without providing timely medical care The patient may die. Therefore, it is imperative to be able to recognize the first signs of appendicitis to avoid serious complications.
Characteristic symptoms
Appendicitis differs from other diseases by gradual development: during the first few hours, Appendix swells and gradually fills the purulent mass. Without the assistance of the surgeon, the process can be broken, but this happens, as a rule, after 2-3 days. After breaking into the abdominal cavity of the patient, pus is poured out, which leads to the development of peritonitis. In this case, the patient's condition is extremely severe.
The most common symptom of inflammation of the appendix is \u200b\u200bthe pain in the right side of the abdomen, which gradually can change the location by moving up or down. In rare cases, painful sensations can be given to the rear pass or back.
Related symptoms for which you need to pay attention to:
- increasing body temperature;
- problems with the work of the intestine (diarrhea, constipation);
- attacks of nausea and vomiting;
- constant tension of the patient's abdominal muscles;
- even minor touch to the stomach lead to severe pain. In pressed the legs to the stomach, they can weaken a little.
Elderly patients and children require special attention, since neither those nor others can clearly describe the character of symptoms. Loss of appetite in a child, low-luxity and constant concerns may indicate the development of appendicitis. The elderly has the risk of late diagnosis of the disease due to the fact that they have painfulness Not so pronounced (smoothing more).
Diagnostic features
At first suspicious symptoms, you need to immediately contact the doctor for the diagnostic examination, which lasts not for a very long time. The doctor must find out the reason for the appearance painful sensations In the stomach, since signs of appendicitis may coincide with the signs of other abdominal pathologies. Diagnosis is necessarily carried out in the clinic. For a start, the doctor asks the patient about the state of his health, heers complaints. At this stage of diagnostics, you need to learn more about the symptoms.
During the visual inspection, it is necessary to take into account the posture in which the patient lies or sits, as well as a gait. The fact is that pain, which often occur with this pathology, can adjust the patient's position. Another body temperature can be high. The condition of the abdominal wall should also be assessed and taken into account. Performing a palpation of the abdomen, the doctor should pay special attention to those sites, with the examination of which the patient feels pain. As noted earlier, the inflammation of the appendix is \u200b\u200baccompanied by the appearance of acute pain in the right side of the abdomen. Crawling this patient's body section, the doctor will be able to identify the intensity and character of pain.
In addition to visual inspection, the doctor may assign urine and blood laboratory tests under which the number of leukocytes is determined. If a woman is examined, the doctor often prescribes a pregnancy test. Such analyzes make it possible to identify inflammation if it is, or the availability of adhesions.
On a note! For a more accurate picture, other types of diagnostics are needed, for example, computer tomography, ultrasound, x-ray research, etc. With their help, it is possible to identify pathological changes in the patient's internal organs, including appendix.
In rare cases, when the symptoms of appendicitis are not expressed, the doctor prescribes an additional diagnostic procedure - laparoscopy. But before this, the patient must undergo a survey from a anesthesiologist. Based on the results of the analyzes carried out, the doctor will be able to put an accurate diagnosis. If it is still appendicitis, then immediate surgical intervention is required.
Types of operations
It is worth noting that in some European countries they are treated acute form Apandicitis with help antibacterial drugs. But almost everywhere requires surgery. This operation, during which the surgeon removes Appendix, is called appendectomy in medicine. There are two methods for removing the inflamed appendix - a classic method and with laparoscopy. Now more about each of the methods.
Classic method
This is a long surgical surgical operation. general anesthesia. On the surface of the patient's patient, the doctor makes a small incision with a scalpel. Then the process is neatly removed, and the tail made is sewn. The method is simple and cheap, but after it on the body of the patient, traces of seams remain on the body, so during the recovery period the patient is forced to take special preparations, resorpting seams.
Another way to surgically remove the appendix, which differs from the previous low injury. The duration of the reducing period after laparoscopy is quite small, but despite such advantages, this type of operation has many different contraindications. Therefore, when choosing a method of operational intervention, the doctor must fully inform the patient about all possible risks.
Important! If you suspect that you have appendicitis, you can not engage in self-medication to relieve symptoms. Many apply hot or cold compresses to the patient place, take painkillers. But all this can only aggravate the already difficult situation.
Recovery after surgery
Upon completion of the operation, the patient is assigned bed regime, which must be observed for 24 hours. On the second day it is permitted a little walk, but only provided that there are no complications. Regular, but moderate loads allow you to speed up the recovery process, as well as avoid the occurrence of adhesions. As a rule, the removal of postoperative seams occurs on 6-7 days after the removal of appendix. But for the full formation of the scar after performing a classic operation, much more time is required (about 6 months). This is provided that the patient will correctly comply with all the prescriptions of the doctors.
The recovery period includes not only the avoidance of heavy physical exertion. The patient must also comply with a special diet and take medical preparations, accelerating scar healing. Consider each of the recovery stages separately.
Medication tools
For tightening postoperative scars, different drugs are used, each of them is characterized by its composition, properties or cost. But not all of them can help in your case, so you need to use only those tools that your attending physician. Below are the most common preparations used during the recovery period.
Table. Pharmacy preparations for the care of the scars.
| Title of the drug, photo | Description |
|---|---|
| Effective anti-infective drug that protects the postoperative scar from various types of infections. With regular use, you can completely get rid of the unattractive scar on the surface of the abdomen. |
| Part this drug The highly purified silicone polymers include a gel on the surface of the patient's surface a special protective film. Designed to treat various types of scars, including postoperative. |
| Another drug for the treatment of scars and scars. Allantoin and celapin are as active ingredients. Output in the form of ointments, the drug has anti-inflammatory and fibrinolytic properties. Promotes rapid regeneration of damaged tissues, improves blood circulation in the seam area after a surgical operation. |
| Effective medication Based on silicone. It is used in medicine not only for the treatment of scars and scars on the body, but also to smooth the patient's solar skin defects. Polysiloxane (organic substance) and silicon oxide protrudes as an active ingredient. The drug is used as follows: a small amount of gel is applied on dry skin and left there until complete drying. After that, the remnants of the gel need to be washed with warm water. Repeat the procedure 2-3 times a day until the complete disappearance of the traces of the operation. |
| The unique composition of the cream allows you to use it from acne, pigment spots on the skin or stretch marks. He also perfectly copes with postoperative scars. The drug contains exclusively natural componentsThanks to which the cream has become so popular. Its action lies in deep penetration into epidermal layers, due to which the skin of the patient is enriched with oxygen and is restored. |
| Used in the treatment of acne, acne or postoperative scars. The effect of the drug lies in the removal of inflammatory processes and accelerate the regeneration of the skin. This allows not only to eliminate existing skin defects, but also to prevent the emergence of new ones. Vehicle is used for the whole body. It must be applied to the problem area and wait until the tool is dry. Repeat the procedure several times a day. |
On a note! After laparoscopy, the patient is written out in about 3-4 days, after the classical method - no earlier than in a week. Throughout the recovery period, which lasts 6 months, doctors recommend to refrain from intense physical exertion.
Food
Immediately after the anesthesia ceases to act after the completion of the operation, the patient begins to torment a strong thirst. But drinking water during this period is impossible, you can only moisten the lips. In rare cases when there is no strength to endure thirst, the doctor may allow drinking a small amount boiled water. If the recovery period is not accompanied by any serious complications, then, starting from the second day, the patient can eat food. Of course, everything should be strictly according to plan.
The diet after the removal of appendix looks like this:
- 1-2 day after surgery. In the diet should be a porridge, low-fat soup, water. You need to eat on the second day after the procedure to start the job digestive system. If the patient is not able to eat independently (he has no strength left), then he should help with this;
- for 3 days It is allowed to eat some cream oil and bread from solid wheat varieties. It is in addition to the above products;
- starting from 4 days The patient may gradually expand its menu by adding various products. Of course, all actions must be agreed with the doctor.
During the recovery period after the removal of appendix, it is imperative to comply with all the recommendations of the doctor and inform him of all suspicious symptoms that may arise. From the use of harmful products, smoking and alcoholic beverages, it is necessary to refuse, as this will only slow down the recovery process. The correct mode will allow not only to speed up the recovery process, but also prevent serious complications.
Complications of appendicitis
Despite the development of modern medicine, it is not always possible to avoid severe consequences. Failure to comply with the recommendations of the doctor or mistakes during the operation can lead to different complications, including:

Development funny processes In the area of \u200b\u200bthe abdomen, it often leads to the occurrence of fistulas. This requires additional treatment. It is worth noting that most complications can be prevented if you fulfill all the prescriptions of doctors during the recovery period.
Video - removal of appendicitis with laparoscopy
Send your good work in the knowledge base is simple. Use the form below
Students, graduate students, young scientists who use the knowledge base in their studies and work will be very grateful to you.
Posted by http://www.allbest.ru/
Donetsk State Medical University. M. Gorky
Department of Surgery and Oteroolaryngology PhiPi
abstracton the topic:« Acute appendicitis»
Executor:
Samarchenko D.V.
Donetsk 2016.
Plan
1. Relevance
2. Etiology, pathogenesis OA
3. Pathological anatomy
4. Classification
5. Clinical picture
6. Diagnostics
8. Treatment
Bibliography
1. Relevance
OA (OA) is the most common surgical disease. The incidence of OA reaches 4-5 cases per 1000 persons of the population, and patients with OA are 20-50% of all patients with surgical hospitals. Appendectomy is 70-80% of all surgical interventions performed in the duty order. The disease is most often found at the age of 10-40 years. Women almost twice often sick OA than men
The postoperative mortality rate is 0.2-0.3% - small, but considering that for the year in Ukraine there are about 300,000 appendectomy, the total number of dead is large. Analyzing the causes of death from OA found that in the first place there is a later appeal of patients for help, in second place - errors in diagnosis. Among the medical errors in the diagnosis of OA, which predetermine the late diagnosis, the fate of district therapists accounts for 55%, ambulance doctors - 35%, surgeons - 10%.
2. Etiology, pathogenesis OA
OA - acute polyethological inflammation of the Cell-shaped outflow of a blind intestine. The main factor in the development of the disease is infectious. The implementation of its pathogenic effect can occur only in the presence of contributing local factors that are:
1. Proceedings of the lumen of a worm-like process, causing stagnation of contents or the formation of a closed cavity. These states may be due to coprolites, lymphoid hypertrophy, foreign bodies, helminths, mucous corks, deformations of the process.
2. Conductive disorders leading to the development of vascular stagnation, vessel thrombosis, the emergence of segmental necrosis.
3.Nogenic violations, accompanied by the enhancement of peristaltics, extracting the process, increased mucus formation, microcirculation disorders.
There are also common factors contributing to the development of acute appendicitis:
1. Alimentary factor.
2. The foundation in the body of the focus of infection with its hematogenous distribution.
3. Immunodeficiency.
4. Allergization of the body.
Influenced by the listed etiological factors begins serous inflammation. At the same time, microcirculation is even more disturbed, necrobiasis develops. Against this background, the reproduction of microorganisms is enhanced. The concentration of bacterial toxins increases. As a result, serous inflammation is replaced by destructive forms, complications are developing.
The most serious of them is peritonitis, since it is he who is the cause of the most serious negative consequences of the disease, including deaths. Despite the fact that the peritonitis in acute appendicitis is secondary in nature and develops against the background of an already unfolded pathogenesis of the causal disease, it makes significant changes during the disease and is characterized by larger impaired homoseostasis.
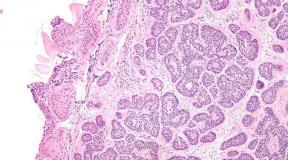
The peritonitis reactive phase begins with irritation of peritoneum by microflora and bacterial toxins that apply to inflammatory exudate. When perforation, the process is more powerful factor is intestinal content. As a result, serous-fibrinous inflammation of the peritoneum, disorders of microcirculation in the form of hyperemia, the state, the formation of erythrocytic aggregates and blood clots in the microcirculatory vessels. The permeability of the vascular wall increases progressively, which enhances the exudation and leads to the output of the cellular elements of the blood beyond the vessels.
Macroscopically determined by swelling of the peritoneum, the formation of fibrinous films and superimposes. In a microscopic study, insignificant leukocyte infiltration with the presence of a small amount of macrophages and lymphocytes. Phagocytosis is not very pronounced. Sometimes in the exudate detected mesothelial cells with included bacterial bodies. As is known, mesothelial cells are not capable of phagocytosis, but it is believed that the lunch of cells with the included bacteria is a kind of local protective reaction of the peritoneum.
Systemic changes at least, clinically significant, into the reactive phase of appendicular peritonitis are mainly reflexive. The most famous of them is the voltage of the muscles of the front abdominal wall, the disorders of hemodynamics. Tachycardia at this stage can be the nature of the reaction to the pain stimulus. Hypotension can be considered as a consequence of the reflex expansion of the peripheral vascular bed, including the peritoness itself. We should not forget that the same changes are related to the changes already existing changes. In the same stage of the development of the disease, violations of the gastrointestinal tract are beginning to be manifested, which at first are reflexive in nature.
Pathological changes of the organs are beginning to be formed into the reactive phase, which then cause polyorgan deficiency: grainy dystrophy and focal damage to cardiomyocytes, small-flowered liver dystrophy, changes in cholinergic nerve fibers in the intestine wall.
With beneficial anatomical conditions, the falling fibrin can contribute to the transition of peritonitis into a limited form to form inflammatory infiltrate, which can later be resolved or abscess. In such cases, it is impossible to talk about the consistent change of all the stages of the development of peritonitis. The process is frozen on the reactive stage with a predominance of local and reflex reactions. Although there is endotoxicosis, but it is compensated in nature. Endotoxicosis increases when the infiltrate is absced, and especially when the abscess breakthrough into the abdominal cavity. With this development, the toxic phase proceeds especially hard, as it is superimposed on the current endotoxicosis.
In the absence of conditions for elimination, peritonitis applies, taking the character of fibrinous-purulent. The leukocyte-macrophage infiltration of peritoneum increases, and a large number of dystrophically altered neutrophilic leukocytes appear. The phagocytic ability of neutrophils and macrophages is reduced. The number of microbial cells in the peritoneal exudate is growing. Progress disorders of microcirculation in the peritoneum.
The phenomena are violently and steadily, which are combined with the name "intoxication" in everyday life. Peritonitis goes into the toxic phase. Its pathogenetic base is four syndrome:
1.Sindrome of water-electrolyte disorders and disorders of acid-alkaline equilibrium (acid-base state, Kos);
2. Sinth of protein metabolism;
3. Endogenous intoxication (endotoxicosis);
4.Sinteral insufficiency.
Endogenous intoxication syndrome begins to form before the development of peritonitis, when there is inflammation of only a heart-shaped process. Initially, the accumulation of toxic products in the focus of inflammation occurs. They then penetrate the vehicles and accumulate in biological fluids. But the powerful source of endotoxicosis is still developing peritonitis. The main factors of endotoxicosis are: bacterial toxins, low and medium molecular weight substances, proteolytic enzymes, lipid peroxidation products, immune complexes, biologically active substances and mediators.
Sources of bacteriamia and bacterial toxinemia are an inflamed black-shaped process, an inflamed peritonean and intestinal lumen. The main bacterial factor of toxmia are endotoxin of intestinal sticks, staphylococcular enzymes (hyaluronidase and coagulaz) and an anaeroba, capable of damaging cell membranes due to high enzyme activity.
Enteral insufficiency syndrome is characterized by disorders of motor, secretory and intestinal absorption functions. It is an important link of the pathogenesis of peritonite of appendicular origin. The basis of this syndrome is the acute dynamic paralytic intestinal obstruction. First of all, literally in the first hours of the disease, the motor activity of the intestine suffers. Probably, during this period, the cause of peristaltic disorders is the formation of pathological entero-gastral and entero-enteral reflexes associated with the focus of inflammation in the ileocecal zone, and then with the irritation of the peritoneum. The direct impact of microbial toxins on the smooth muscles of the intestine is not excluded. Further discirculatory electrolytic violations And endotoxicosis increases the oppression of the motility of the gastrointestinal tract.
Pathogenesis OA, complicated by peritonitis, is very complex and multifaceted. An important part of it is made up of changes in the level of the whole organism. The processes started in a small volume and value of a worm-like procession, initiate and maintain severe systemic pathological disorders. Operating injury further aggravates them. In addition, the operation does not cure the disease, but only eliminates the source of systemic metabolic disorders, creates conditions for effective correction of violations of all types of homeostasis. Therapeutic activities should be planned taking into account pathogenesis.
3. Pathological anatomy
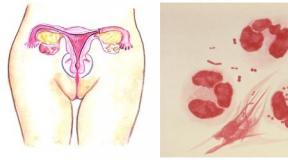
As morphological changes are rapid changes, the following forms of OA are distinguished in a worm-like process:
1. Appendicular colic, as the OA functional phase, when morphological changes in appendix have not come;
2. Simple (superficial) - swelling, hyperemia of the entire process, microscopically necrotic damage limited to the mucous membrane;
3. FLEGMONOSIC - more expressed swelling, fibrin raid on the surface of the process, and morphologically: destructive changes are distributed to all layers of appendix;
4. Gangrenoz - Appendix macroscopically dark crimson, black or dark green with purulent layers;
5. Perforated - from microperphoration to the self-impassment of the appendix;
6. Appendicular infiltrate is a local peritonitis, a conglomerate of inflammatoryly elapsed organs (blind intestine, loops of the small intestine, the sealance, parietal peritoneum), in the center of which is located destructively altered Apandix. The evolution of appendicular infiltrate may be a double - either resorption, or suppuration with subsequent complications.
4. Classification
Among the classifications, the most common proposed V.I. Kolelyov, according to which allocate:
І. Acute appendicitis
1. Appendicular colic
2. Acute simple (superficial) appendicitis
3. Acute destructive appendicitis
a) phlegmonous,
b) gangrenous,
c) perforated,
d) an empieme of a worm-like process.
4. Complicated acute appendicitis
a) appendicular infiltrate,
b) appendicular abscess
c) peritonitis of appendicular origin,
d) other complications (pylephlebit, sepsis and others).
II.. Chronic appendicitis
1. Primary-chronic appendicitis.
2. Residual chronic appendicitis.
3. Recuse chronic appendicitis.
5. CLinical picture
General symptomatics
The attack of acute appendicitis begins, as a rule, with abdominal pain. In 20-40% of cases, pain occurs first in the epigastric region, then moves to the right iliac region (C-M Volkovich-Kochra), but it may be localized from the very beginning in the right iliac region. Apandicitis surgical disease
For OA, there is a gradual increase in pain, permanent character, lack of irradiation, moderate intensity. A sharp increase in pain indicates the perforation of appendix.
2-3 hours from the beginning of the disease in 50% of cases of patients are concerned about nausea, vomiting, more often disposable, stool delay, gases. In children with toxic forms of OA, you can observe diarrhea.
At the same time, with the development of the inflammatory process in Appendix, an increase in body temperature is increased to 38 ° C.
Often, when painted patients, it turns out that similar attacks had a place in the past.
With an objective study of patients, tachycardia occurs, which first corresponds to the temperature, and with peritonitis exceeds it. In a clinical analysis of blood, there is a moderate leukocytosis to 10-12 * 109 / l, neutrophilez, neutrophil shift to the left. A day later, the SE is rising from the beginning of the disease.
Local symptomatics
With an objective study of the abdominal organs, many pain symptoms are determined, which described more than 200. The most informative of them are as follows:
1. Triad DieleoFua (Classic Triad OA):
Spontaneous pain in the right iliac yam;
The tension of the muscles of the right iliac region during the palpation of the abdomen;
Hyperesthesia of the skin of the right iliac region.
2. The symptom of roving - pain in the right iliac yampecker with peasant movements in the projection of the descending division of the colon in the roasted sigmoid.
3. The symptom of exemplary is an increase in pain when pressed in the right iliac yam during the bending of the right leg in the hip joint.
4. Symptom of Ivanov - cuts of the distance from the navel to the right upper front axle ileal bone in comparison with the left side.
5. Symptom of Resurrection 1 - Strengthening pain in the right iliac yam during a sliding palpation through a stretched shirt from the epigastria to the right iliac region (symptom of the shirt).
6. Sytkovsky's symptom - the appearance of drawing pain in the right iliac yam, if the patient lies on the left side.
7. The symptom of Bartaye-Michelson - pain during palpation in the right iliac yammer is more pronounced if the patient lies on the left side than on the back.
8. Symptom of Yaure-Rozanova - Palpation pain in the Petitov region of the triangle on the right side (with a retrocecal OA).
9. The symptom of the COOP 1 is pain in the right iliac yam in the passive refilting of the right leg in the hip joint.
Since, with OA, the inflammatory process quickly goes to visceral and parietal peritoneum. Local peritoneal symptoms are determined early - the symptoms of peritonean irritation in the right iliac yam.
These symptoms belong:
The tension of the abdominal muscles;
S-M Brush-Blüsterberg - sharp pain in a sudden decompression when palpation of the abdomen;
S-M Rydolsky - pain at percussion of the abdomen;
Identification of stomaching sites at percussion of the abdomen;
No peristaltics during auscultation.
In the study of the patient, it is necessary to carry out a finger study of the rectum, and in women in addition - a bimanual study. At the same time, special attention is paid to identifying the symptoms of pelvic peritonitis:
Painful hanging of the front wall of the rectum (Douglas pocket), or the rear vessel of the vagina in women.
6. Diagnostics
It is based on the identification of characteristic complaints of a constant pain in the right iliac yam, or the symptom of Volkovich-Kochker, nausea, an increase in body temperature, with an objective study - detection of tachycardia, positive symptoms of roving, resurrection, extinguished, Sitkovsky, bartome-Michelson, also symptoms of irritation The peritoneum in the right iliac region, the tension of the muscles, the brush-blubberg, Razdolsky. To confirm the diagnosis make a clinical analysis of blood and urine. In the analysis of blood, leukocytosis, neutrophileenesis, neutrophilic shift to the left are detected. But often the clinical picture is atypical and has to expand the amount of additional studies, conducting a differential diagnosis with one or another urgent disease. In such cases, instrumental studies are additionally used to diagnose kidney diseases, biliary tract, genitals in women, including the puncture of the vaginal rear axle. Sometimes, in particularly difficult to diagnose cases, laparoscopy or diagnostic laparotomy are performed.
7. Differential diagnosis
OA is the soda ulcer of the stomach and a 12-rosewoman.
The general principle of the disease with pain in the epigastric area is common to OA and sample ulcers, and especially later, when the contents of the stomach, the 12-pocket guts are lowered along the right side flank and accumulates in the right iliac yam. In the case of covered perforation, the symptoms of the peritonean irritation in the upper floor of the belly subsided, and dominate the right iliac yam, as with OA. Both diseases predetermine the infection of the abdominal cavity and therefore are accompanied by an increase in body temperature, tachycardia, leukocytosis, symptoms of intoxication.
Different for OA and sizes, which allows them to differentiate them, is:
From anamnesis - pain under perforation occurs suddenly "as a strike of a dagger", sharp burning, unbearable, sometimes with irradiation into the on-shifted areas;
With OA, the pain is displayed at first in the epigastrium (solar plexus) stupid, less intense, without irradiation, begins gradually.
From the history of the patients with OA - there were bouts of pain in the right half of the abdomen, and the second - a history of ulcerative disease.
In an objective study, the patients with perforative ulcer turns out to be a significant tension of the muscles in all the departments of the abdomen (abandoned stomach), and with the OA, the muscle voltage is only in the region of the right iliac yam.
Percussier - the disappearance of hepatic stupidity (symptom of the operator).
Of additional methods Studies decisive is review radiography, or -skopia of the abdominal cavity organs in the FAS and the profile on which the presence of free gas (pneumoperitoneum) is detected, and in cases where the gas is missing by gastrography with a 30% water-soluble iodine solution, or pneumogress. Laparocentsis, laparoscopy apply for diagnostics.
OA is sharp cholecystitis.
Common for them is the acute principle of the disease with the appearance of pain in the right half of the abdomen, which is accompanied by nausea, vomiting, an increase in body temperature, leukocytosis. Especially similar symptoms of OA on acute cholecystitis happens in patients with the sub-arrangement of Appendix.
Despite this, you can state the difference:
In history - pain in OA is often moved from the epigastria into the right iliac hole, less intense, permanent character, without irradiation, while pain in acute cholecystitis are quite intense, periodic (parodial) with irradiation of the reptile right blade, into the right-hand-screw area, vomiting OA is disposable, and with acute cholecystitis often repeats, with an admixture of bile, does not bring relief, in the history of patients with acute cholecystitis - attacks of hepatic colic, which were often accompanied by jaundice;
In an objective study in cases of acute cholecystitis detect characteristic symptoms Murphy, Mussi-Georgievsky, Boas, and with OA - C-We are Rovoving, Sitkovsky, Bartom-Michelson;
Instrumental methods of research are particularly informative in acute cholecystitis - on ultrasound, the biliary tracting stones are detected, an increase in the size of the gallbladder, the double circuit of its walls, in cases of extremely difficult to diagnose doubt are solved on the operating table, and the operational access should be right-sided Paralegal (Lennanander) From which you can perform operation and on the biliary ways, continuing upwards and appendete-miu, in the case of OA.
OA - acute pancreatitis.
There is a common for them that in the first hours of the disease and in the first and in second cases there are constant pain in the epigastric region, which is accompanied by nausea, vomiting, bloating. And later, as the accumulation of pancreatic effusion in the right side flank and the right ile yum of the abdominal cavity, acute pancreatitis can simulate OA.
With a more attentive and detailed study of patients, you can identify the difference:
In the history of the diseases of patients with acute pancreatitis - a gall-stone disease, often the beginning of the disease patients are associated with the use of oily, acute food, alcoholic beverages;
In an objective study in acute pancreatic, the body temperature is normal, and with OA - elevated, in the study of the abdomen, characteristic symptoms for acute pancreatitis are revealed: Voskresensky II, Kerte, Meio-Robson, Chukhrienko, Mondor, with OA - Rovzing, Sitkovsky, barter Michelson, exemplary and others;
Additional laboratory methods Research: a clinical analysis of blood - with acute pancreatitis characteristic hyperlaycitosis (up to 20x109 / l and more), with OA - moderate leukocytosis, with acute pancreatitis - hyperamilasemia, hyperamilazuria (urine diastast - above 128 units.);
Instrumental research methods: In severe cases, more informative cases - ultrasound procedureIn acute pancreatitis, an increase in the size of the pancreas, increase and echogenicity, hydrophilicity, the formation of liquid accumulations in the gland bag, and with OA - liquid accumulation in the right iliac yammer and the douglas pockets are revealed. The laparoscopy is especially informative - with acute pancreatitis, hemorrhagic content in the abdominal cavity can be revealed, hemorrhagic peteers in the peritoneum, a particularly large seal (with hemorrhagic pancreatic) or stearic plaques (with fatty pancreatic).
OA is acute intestinal obstruction.
To individual forms of acute intestinal obstruction, which can be similar to OA, belong to the ileocecal invagination of the intestine, the vicious intestine. With these diseases, as with OA, the main symptoms are the bouts of pain in the right iliac region, which is accompanied by nausea, vomiting, the delay of stool and gases, and leukocytosis is observed in blood tests. It is even more difficult to recognize these diseases in the later stages when perforation comes, which predetermines diffuse peritonitis. Then the symptoms of severe peritoneal endotoxicosis, symptoms of peritonean irritation appear. And on the overview radiograph of the abdominal organs in all cases, cubeball bowls are provided.
However, with a more attentive examination of patients with Ileocecal invagination, you can identify the difference:
From the anamnesis - pain in acute intestinal obstruction is very intense, often accompanied by the "Ileis cry" of patients, wearing an approaching nature, and vomiting is very frequent, dominated in general symptoms, first the contents of the stomach, and later the intestine with unpleasant odorwhich does not happen with OA, with invagination patients complain about liquid stools with an admixture of mucus and blood in feces, whereas with OA, there are more difficult constipation;
With an objective study of patients with Ileocecal invagination, it is possible to identify the symptom of dance - the absence of a palpation of a blind intestine, and the right iliac pump is empty, revealed, the symptom of the roof - when the abdomen of the reveament of invaginate, and with the finger of the rectum, the symptom of the Obukhov hospital, or sometimes pinch the head of the invaginate, Blood in feces;
The final and most informative for the differential diagnosis of Ileocecal invagination from OA are instrumental research methods - irrigoscopy (contrast barium enema), or fibrocolonoscopy, through which it is possible not only to state the invagination of the intestine, but also to perform disinums, without resorting to surgical interference in the first hours of the disease.
It is much more difficult to carry out the differential diagnosis between the breakthorn of the blind intestine and OA. Fortunately, the sword of the blind intestine is observed very rarely. Clinical characteristic It is typical for the strange intestinal obstruction, however, often the turn of the blind intestine is recognized only on operations on OA.
OA - Rightsadnexitis and ectopic berechange.
In case of a pelvic arrangement of a worm-like transformation, OA can be confused with acute inflammatory processes of uterus's appendages, twisted of the ovary cyst, interrupting ectopic pregnancy. Both in one and in other cases, diseases are accompanied by the abdominal at the bottom of the abdomen, an increase in body temperature, nausea, vomiting, leukocytosis.
With a more attentive study of women with adexite, you can reveal:
In history, pain with irradiation in the seats, crotch is accompanied by purulent discharge from the vagina, in the past, artificial abortions, inflammation of the appendages of the uterus;
With objective, especially with a bimanual vaginal examination, it is stated with the palpation of the lower parts of the abdomen of the increase in pain when pressing the book during adnexite and upstairs - with OA, with the adexistence of the positive symptoms of the Union, Poshrurs, Prompatova, with OA - Rovzing, Sitkovsky, Barta-Michelson. Certain help can be obtained from the UZT and the puncture of the rear axle of the vagina.
For ectopic pregnancy, a number of features can have certain assistance:
From the anamnesis - the beginning of an attack from a fainting, a strong pain at the bottom of the abdomen with irradiation into the rectum, the lower back, the delay of menstruation, dark bloody discharge from the vagina, the general weakness, thirst, drowsiness;
Objectively: pallor skin, tachycardia, low arterial pressure, reduction of hemoglobin, hematocrit;
When the rear array of the vagina receives blood from the douglas pocket.
OA is right-sided renal colic.
With the retrocecal arrangement of Appendix, the pain, as under the right-sided kidney colic, may be observed nausea, vomiting, constipation, moreover, when the inflammatory appendix is \u200b\u200bdistributed to the ureter or the bladder, hematuria can be revealed in urine analysis.
The difference between right-hand renal columes and OA will be:
In anamnesis - pain with renal colic parotidic, and with OA constant and less intense, patient with kidney colic constantly changes the pose, with OA - it tries to move less, more often to lie on the right side with the thighs given to the belly, with the renal colic, the typical irradiation of pain is observed. on the inner surface of the right hip, the urethra, frequent, painful urination, which does not happen with OA;
With an objective study for OA, an increase in body temperature, tachycardia, though the pain per palpation in the right iliac yammer, positive symptoms of roving, Jaur-Rosanov, Kooup, Obraznova, is less pronounced. Under right-sided kidney colic - a positive symptom of Pasternatsky, pain when pressed along the right ureter;
Of the additional research methods, with OA in clinical analysis of blood leukocytosis, hematuria during renal colic can also be observed, but with it, red blood cells are aligned, the instrumental methods are particularly informative in difficult cases - ultrasound, chromocystoscopy, excretory urography.
8. Treatment
Since the only method of treatment of OA is an immediate operation of appendectomy, medical tactics on chipboard Consisions in the ambient transportation of the patient in the urgent surgical hospital. When providing first medical care patients with suspicion of OA, it is impossible to prescribe narcotic anesthesia, laxatives, stomaching, and stignwork.
Surgical tactics lies in the fact that all patients of OA, in addition to cases of appendicular colic and clearly deliberate appendicular infiltrates, are subject to immediate operation - appendectomy.
Anesthesia as a method of choice should be endotracheal anesthesia. Local infiltration anesthesia 0.25% novocaine solution is applied in cases in the absence of anesthesia conditions.
Operating access are used different:
Volkovich-Dyakonova (Mac-Burnea) - oblique in the right iliac hole, in parallel in the groin, whose center is the Mac-Burnea point;
Lexer - through the Mac-Bourneque point, like the previous one, but avoiding muscle injuries - through a spectional line;
Lennanander - right-sided paragreactive in cases of doubt in the diagnoses of OA - cholecystitis, OA - emergency Disease Pods of the uterus;
lower median laparotomy - in cases of common peritonitis of appendicular origin.
When dealing with Volkovich-Dyaconov, which is most often used, leather, subcutaneous fatty tissue, superficial belly fascia, aponeurosis, outdoor abdominal muscle, stratify the fibers of the inner oblique and transverse abdominal muscles, the transverse fascism of the abdomen, the peritoneum.
The blind intestine with a heart-shaped process is displayed in an operating wound. The mesentery of the process intersects between the clamps, is stitched and tied up. The base of the process is tied by a ketguet ligature, which is distally intersecting, leaving a culture of 3-4 mm. The latter is immersed in a brine serous-muscular seam with an additional Z-shaped seam.
The ligatural method of treating the cult of appendix, when the cult remains up to 5-7 mm long, and is supplied to the caproove thread, it is rarely used in cases of pronounced tiflite, when immersed by the cult of Appendix is \u200b\u200btechnically impossible, and children of the first years of life.
If it is impossible to eliminate the appendix to the wound, a retrograde appendectomy is used in the wound: two ligatures are injected through the appendix mesentery near its base: the proximal is ketgut, distal - cape. They tie ligatures and between them intersect appendix. The cult is immersed by an ordinary bride, sipping for a caprony thread portion crosses and tied up with a mesentery until complete mobilization of the process and remove it. In the destructive forms of appendicitis, the presence of a large amount of effusion, or fibrinous layers on the peritoneum, the abdominal cavity is drained by strips of glove rubber, or silicone tubes.
Laparoscopic appendectomy.
After creating carboxyperitoneum in the abdominal cavity, you must enter working trocars. The first is introduced 10 mm trocar under the navel strictly in the middle line. It is better to use a trocar with a triangular shape of the distal end, which is easier to pass the layers of anterior abdominal wall. The trocar is introduced with a slight drilling movement, using an index finger as a limiter.
A laparoscope is introduced through the first trocar and the abdominal cavity is carried out. When identifying the appendectomy, two more trochar are introduced. Before that, the patient must be translated into position with the lowered head end by 30 degrees and with turning the table to the left at 45 degrees.
The second trocar of 5 mm is entered at the Mac-Burnea point. If, during revision, it is established that the blind intestine is located above or there is a retrocecal position of a worm-like process, then this trocacar is introduced by 3-4 cm above the McCurnea point.
The third working trocar 10 or 12 mm is entered over the midline by 5-6 cm above the Lona.
Laparoscopic appendectomy technology is a number of actions and techniques, the sequence of which depends on the anatomical conditions, the nature of inflammatory changes, possible complications. The essence of it, of course, is the same as during the traditional operation. The two main techniques are also used: antitegrand and retrograde appendectomy.
Antegrand appendectomy is performed more often. At the same time, a worm-shaped process is captured in the top near the mesenteric edge with elastic tongs introduced in the right iliac region. The process pulls up up and right.
Fig. one. Laparoscopic appendectomy. The top of a worm-shaped process is captured by tongs.
As a result, it becomes accessible to the manipulations of the mesenzhechka process throughout the entire basis.
FENESTRATION OF ENERGY ENERGY DISESTRUMENT. Then, with the help of the clips-applicator, the mesenter is consumed with special clips 8-10 mm (Fig. 2), the number of which depends on the length of the mesenter. They can be from 3 to 8.
Fig. 2. Laparoscopic appendectomy. Clipping mesenzheyschka using clips applicator.
Fig. 3.. Laparoscopic appendectomy. Bryzezychka dishes between clips.
Clips can only overlap on the culture of mesenter; In this case, the hemostasis on the removed part is carried out using an electrocoagulation with a monopolar electrode. The mesenzhechka portionly intersects with scissors (Fig. 3), which completes the mobilization of the process.
It is possible to process mezezychka using electrocoagulation by bipolar tongs (Fig. 4).
Fig.4.. Laparoscopic appendectomy. Electro-coagulation balls.
At the same time, the mesentery is captured by the branches of the forceps and the electric approach is carried out for 20 seconds. On the line of electrocoagulation, the mesenter dishes scraps (Fig. 5).
Fig.5Laparoscopic appendectomy. Intersection of mesenter after electrocoagulation.
In deformations, the process and its atypical localization, as well as in the conditions of loose infiltrate and in connection with the difficulties already discussed, should be resorted to retrograde appendectomy. In laparoscopic execution, this technique is more complex and requires special care and methodical.
Mobilization of a worm-like procession with retrograde appendectomy begins at its foundation. The dissector is phenestrated by mesenter and the titanium clips are superimposed on the base of the process (Fig. 6). After that, the process is cut off from the blind intestine between the clips superimposed on its mesenter (Fig. 7).
In some cases, mesenter can be tied using endopethi. When using this technique, the process is captured by forceps and moves up. If the mesenter is stretched, it is possible to bandage it with a preformed self-sinking node (Fig. 8).
Fig. 6. Laparoscopic retrograde appendectomy. FENESTRATION OF ENERGY BANGERS Using the Dissector. Clips are superimposed on the base of the process.
PC. 7. Laparoscopic retrograde appendectomy. The hipged process and its mesenter are intersect.
Fig. 8. Laparoscopic retrograde appendectomy. Laging mesenzheki endolytica with subsequent intersection.
The node is formed outside the abdominal cavity with the formation of the loop, which is carried out into the abdominal cavity with the help of a special guide through a working 10-12 mm Troacar. In the abdominal cavity of the loop, it is pounced on the mesentery through the process and is delayed with the help of a guide. Thus, the mesenter must be reduced twice. With a short or infiltrated mesenter, it is safer and easier to clone its portion.
The next stage of the laparoscopic appendectomy is the processing of the cult of a worm-like process. With antegradine appendectomy, a double ligature is superimposed on the base of the draft-shaped process: chrome-plated Ketguta, Vikrila (Ethicon) or polysorba ("Auto Suture") - a special conductor is introduced for ligatures to the abdominal cavity, which is a tube with internal Channel for thread. The ligature is carried out through the conductor, and the loop is created in its distal part for the subsequent intracorporeal node. The loop through the working trocar is introduced into the abdominal cavity. In the lumen of the hinges, a clamp is introduced, which is then captured by the top of the draft-like process. The loop descends to the base of the process, and the endolygatura is tied by 2-3 cm on the level of the wall of the blind intestine (Fig. 9).
Fig. 9. Laparoscopic apgeledectomy. Summing up endolytication to the base of the process.
The guide is extracted, and the thread intersects at a distance of 5 mm from the knotted node. The second loop is carried out in the same way, which is tied by 1-2 mm distal than the first. The third loop is tied up with a removable part of the process. This thread does not cut off and is used to extract the abdominal process.
The intersection of a worm-like process in all cases is carried out by scissors (Fig. 10).
Fig. 10. Laparoscopic appendectomy. The intersection of the process between Rundolygatures.
At the same time, at the moment of dissection, coagulation is not used due to the risk of burning superimposed ligatures. Cell-shaped process is advisable first to cross the 5/6 of the circle, after which it becomes available for processing its mucous membrane. The processing consists in point coagulation by the tip of scissors or a special button coagulator (Fig. 11). After that, the process is finally cut off.
Fig.11. Laparoscopic appendectomy. Coagulation of the mucous membrane of the process.
In cases where retrograde appendectomy is produced, the sequence of actions changes and consists in the following. After the fenestration of mesenzheyshka, the clip is imposed on the base of the process or, which is preferable, clip and endolygatura. Parallel to the first clips overlap two more, and, the third - at a distance of 6-8 mm from the second (Fig. 12).
Fig.12. Laparoscopic appendectomy. The crust of the process is clipped with three clips.
The Cell-shaped process intersects between the second and the third clips, followed by the coogulation of the mucous membrane of the cult.
Extremely propagating in endovidosurgery, mechanical seams found its use and with laparoscopic appendectomy. After flashing the process with its use, there is no need for additional peritonization. The device can be used in any method of appendectomy (Fig. 13.). Its use significantly simplifies the operation of the operation.
Fig. 13. Laparoscopic appendectomy. Freshing and crossing mesenzheki dark-shaped process using a surgical stapler.
After removing the process, it is necessary to aspirate the blood clots and the accumulated exudate. The operation zone is washed with an antiseptic with simultaneous evacuation. In all cases, it is necessary to drain the abdominal cavity with the use of a special valve drainage. The operation ends with the evacuation of gas from the abdominal cavity and the control of the effectiveness of hemostasis, including from the trocar wounds.
In the postoperative period, as a rule, a sufficiently double use of analgesics with an interval at 6 o'clock is enough to relieve pain. Patients with destructive forms of acute appendicitis during the first three days after surgery should be prescribed antibiotics of a wide range of action. With a favorable course of the postoperative period, the reception of the PER OS fluid is possible from 2 days, and food - from the 3rd day.
Drainages from abdominal cavity are usually removed by 2-3 days after surgery. Before removing drainage, it is advisable to produce rectal and vaginal research to eliminate the accumulation of fluid in a small pelvis. The extract of patients from the hospital is carried out by 4-5 days after the operation. With a favorable postoperative course, return to normal labor activity Our patients had a place two weeks after the operation.
In the postoperative period in the first 12 hours the patient requires a strict bed mode. At the end of the first day, the patient is allowed to rise from the bed, drink water, take liquid food, tea, kefir, raw eggs, from 2-3 days gentle diet - broths, rubbed soups, porridge, boiled meat. With the resumption of an intestinal passage from 7-10 days of patients, they transfer to a shared table.
After the operation, antibiotic therapy - cephalosporins II-III generations in optimal doses are prescribed to patients with destructive forms of OA. In case of infectious complications, combined antibacterial therapy with the use of metronidazole and other antibacterial drugs.
In recent years, a wide distribution of the unauthorized method of treatment in the hospital in patients without complications and shortened surgeons has been acquired when patients are issued for outpatient treatment by 4-5 days in order to prevent an intra-hospital infection of the wound. The polyclinic stage of treatment and rehabilitation of patients lasts 20-25 days, after which the patients are written to work, but for 1-2 weeks it is issued a certificate of LCK on the need to transfer to easy work.
The immediate results of the treatment of OA are good. Complications after operations are observed in 2.5-3% of cases, and mortality is 0.2%. The first day is possible complication - bleeding. The most difficult complications are peritonitis, infiltrates, abdominal abscesses, intestinal fistula, adhesive intestinal obstruction, pylephlebit, sepsis, as well as complications from light, cardiovascular system, kidneys, liver.
In long-term deadlines, as the consequences of operational treatment, are possible flashing disease intestines, postoperative ventral hernias, intestinal fistulas.
Bibliography
1. 50 lectures on surgery / ed. V.Saveleva - M.: Triada-X, 2004. - 752c.
2. Astafurov V.N. Diagnostic Handbook of the Surgeon. - Rostov-on-Don: Phoenix, 2003.
3. Atlas of Hyrurgіchny Opechair and Manіipulyatsii / Pіd Ed. L.Ya. Kovalchuk, V.M. Polischka, V.I. Tsimbalyuka Ta IN. - Ternopil-Rivne: Vertex, 1997. - 428 p.
4. Biseenkov L.N. Urgent chest surgery and abdomen. - St. Petersburg: Hippocrat, 2002. - 512 p.
5. Bolshakov O.P., Semenov G.M. Lectures on operational surgery and clinical anatomy. - St. Petersburg: Peter, 2000.
6. Grigoryan R.A. Abdominal surgery: in 2 tons. - M.: Medical Information Agency LLC, 2006. -608 p., 672 p.
7. Clinical recommendations For doctors on issues of organization and provision of medical care patients with acute surgical diseases of the abdomen (departmental instructions) / Z. Bereznitsky, V.V. Bookko M.E.Nichitail and others. - K.: "Dnipro-Val", 2004. - 353 p.
8. Kovalchuk L.Ya., Dzübanovsky І.Y. The atlas of operational VTRUCHAN on the organs of the Slunkovo-Kishovo tract І І Польій Черевній stіntzі. - Ternopil: "Ukrmedkniga", 2004.
9. Kovanov V.V. Operational surgery and topographic anatomy. - M.: Medicine, 2001. - 408 p.
10. Kuzin M.I. Surgical diseases. - M.: Medicine, 2005. - 784 p.
11. Mainrenko N.A., Movchan K.N., Volkov V.G. Emergency abdominal surgery. Workshop. - St. Petersburg: Peter, 2002. - 304 p.
12. Malarchuk V.I., Pathkin Yu.F. Surgical diseases. Course of Faculty Surgery. - in the Russian University of Friendship of Peoples, 2002 - 480 p.
13. Nevіdkladna Khіruurgіya / Red. L.Ya. Kovalchuk. - Ternopil: "Ukrmedkniga", 2000.
14. Guide for urgent surgery of abdominal organs / edited by B.C. Savelyev. - M., Publisher, 2005, - 640 p.
15. Facultytski Khіruurgіya / Red. V.O.Shidlovsky, M.P. Zaharash. - Ternopil: "Ukrmedkniga", 2002.
16. Khoronko Yu.V., Savchenko S.V. Emergency Surgery Handbook. -M.: Medpress-Inform, 2002. - 464 p.
Posted on Allbest.ru.
...Similar documents
Definition and prevalence of acute appendicitis - inflammation of a worm-shaped outflow of a blind intestine. Clinical picture and diagnosis of disease, expressed symptoms. Features of the course of the disease, treatment. Complications of acute appendicitis.
presentation, added 04.11.2014
Anatomy of the ileocecal zone and a heart-shaped process. The options for the location of the dome of the blind intestine with a worm-like process in the abdominal cavity. Blood supply of a heart-shaped process, his inflammation. The etiological factors of the emergence of acute appendicitis.
presentation, added 03/28/2016
Inflammation of a worm-shaped outflow of a blind intestine. Options for Appendix. The main mechanisms for the development of inflammation in a worm-like process. The main forms of acute appendicitis. Localization of pain at the beginning of the disease. Nausea and temperature reaction.
presentation, added 04.02.2015
Inflammation of the Cell-shaped outflow of a blind intestine due to the introduction of pathogenic microbial flora into its wall. Neokelsion forms of acute appendicitis and primary ischemia process. Surgical treatment of acute gangrenous-branched appendicitis.
history of the disease, added 18.11.2013
Acute appendicitis as an inflammation of a dark-shaped transformation of a blind intestine, prerequisites for the development of this disease, risk factors and an assessment of prevalence. Etiology and pathogenesis of appendicitis, options for its location, classification and varieties.
presentation, added 05/18/2015
Topography colon. Sintopia blind intestine. The position of the base of the heart-shaped process in the abdominal cavity, its inflammation as the cause of the irradiation of pain in the thigh. Diagnosis of acute appendicitis. Paths of the distribution of peritonitis with purulent appendicitis.
presentation, added 02/03/2016
The prevalence of inflammation of the Cell-shaped process of the blind intestine, options for the arrangement of appendix, etiology and pathogenesis of acute appendicitis. Methods surgical treatment and possible postoperative complications. Laparoscopic appendectomy.
presentation, added 05/16/2016
Localization of a blind intestine and a heart-shaped process. Acute appendicitis with a pelvic arrangement of a worm-like process. The diagnostic program plan with acute appendicitis, the main clinical symptoms of the patient. Complications of the postoperative period.
presentation, added 04/13/2014
Local signs of the disease. Clinic of acute appendicitis. Differential diagnosis of peritonitis. Pathological physiology and anatomy. Indications for the emergency operation of a worm-like process (appendectomy). Restoration of intestine microflora.
history of the disease, added 18.10.2015
Features of acute appendicitis, inflammation of a worm-shaped outflow of a blind intestine. Antegrand Appendectomy: Procedure Operations. Maloveraumatic method of treating acute and chronic appendicitis. Control audit, rehabilitation, abdominal drainage.
As soon as the child has a diagnosis of diabetes, parents are often sent to the library for information on this issue and are faced with the possibility of complications. After the period associated with this experiences, parents receive the following strike by learning the statistics of morbidity and mortality associated with diabetes.
Viral hepatitis in early childhood
Relatively recently hepatitis alphabet, in which hepatitis A, B, C, D, E, G, was replenished with two new DNA-containing viruses, TT and SEN. We know that hepatitis A and hepatitis E do not cause chronic hepatitis And that Hepatitis G ITT viruses are most likely "innocent spectators" that are transmitted vertically and do not affect the liver.
Measures on the treatment of chronic functional constipation in children
 In the treatment of chronic functional constipation in children, it is necessary to take into account important factors in the history of the child's illness; establish a good relationship between a medical officer and a child-family for the implementation of the proposed treatment properly; Much patience on both sides with the repetition of guarantees, that the situation will gradually improve, and courage in cases of possible relapses - make up the best way to treat children suffering from constipation.
In the treatment of chronic functional constipation in children, it is necessary to take into account important factors in the history of the child's illness; establish a good relationship between a medical officer and a child-family for the implementation of the proposed treatment properly; Much patience on both sides with the repetition of guarantees, that the situation will gradually improve, and courage in cases of possible relapses - make up the best way to treat children suffering from constipation.
Results of research scientists challenge the ideas about the treatment of diabetes
The results of a ten-year study undoubtedly proved that frequent self-control and maintenance of blood glucose in the limits close to normal leads to a significant decrease in the risk of late complications caused by diabetes, and reduce their degree of gravity.
The manifestations of rickets in children with a violation of the formation of hip joints
 In the practice of children's orthopedists traumatologists, the question of the need to confirm or eliminate disorders of the formation of hip joints (displaced joint joints, congenital dislocation of hips) in babies has become often raised. The article shows an analysis of the survey of 448 children with clinical signs Disorders of the formation of hip joints.
In the practice of children's orthopedists traumatologists, the question of the need to confirm or eliminate disorders of the formation of hip joints (displaced joint joints, congenital dislocation of hips) in babies has become often raised. The article shows an analysis of the survey of 448 children with clinical signs Disorders of the formation of hip joints.
Medical gloves as a means of providing infectious safety
Most nurses and doctors dislike gloves, and not in vain. In gloves, the sensitivity of fingertips is lost, the skin in the arms becomes dry and peeling, and the tool strives to slip out of the hands. But the gloves were and remain the most reliable means of protection against infection.
Ladant osteochondrosis
It is believed that every fifth adult man on Earth suffers like lumbar osteochondrosis, this disease occurs in young and in old age.
Epidemiological control over health workers who had contact with blood HIV-infected
 (to help medical professionals of medical institutions)
(to help medical professionals of medical institutions)
Methodical instructions covered issues of monitoring medical workers who had contact with the blood of the patient infected HIV. Actions are offered for the purpose of preventing professional HIV infection. An accounting magazine and an act of service investigation during contact with the blood of a HIV-infected patient are developed. The procedure for informing the higher bodies on the results of medical monitoring of health workers in contact with the blood of a HIV-infected patient was determined. Designed for medical workers of therapeutic and preventive institutions.
Chlamydial infection in obstetrics and gynecology
Chlamydia genitals is the most common among sexually transmitted diseases. Around the world, there is an increase in diseases by chlamydia among young women who have just entered during sexual activity.
Cycloferon in the treatment of diseases of infectious nature
Currently there is an increase in individual nosological forms infectious diseasesFirst of all, viral infections. One of the directions of improving treatment methods is the use of interferon, as important non-specific antiviral resistance factors. To which the cycloferon refers is a low molecular weight synthetic inductor of endogenous interferon.
Dysbacteriosis in children
The number of microbial cells present on the skin and mucous macro-organism in contact with the outer medium exceeds the number of cells of all its organs and tissues combined. The weight of the microflora of the human body is on average - 2.5-3 kg. The value of the microbial flora for healthy man First drew attention to the first time in 1914. I.I. Messenchi, who suggested that the cause of many diseases are various metabolites and toxins produced by various microorganisms that populate organs and human body systems. The problem of dysbacteriosis in recent years causes a lot of discusions with an extreme range of judgments.
Diagnosis and treatment of female genital infections
In recent years, all over the world and in our country there is an increase in the incidence of sexually transmitted infections among adults and, which causes special alarms, among children and adolescents. The incidence of chlamydia and trichomoniasis is growing. According to WHO, trichomoniasis ranks first in frequency among sexually transmitted infections. Every year, 170 million people are ill in trichomyoniasis.
Intestinal dysbiosis in children
Intestinal dysbiosis and secondary immunodeficiency state are increasingly found in clinical practice Doctors of all specialties. This is due to the changing living conditions, the harmful effects of the preformed environment on the human body.
Viral hepatitis in children
The lecture "Viral hepatitis in children" presents data on viral hepatitis A, B, C, D, E, F, G in children. All are given clinical forms viral hepatitis differential diagnosis, Treatment and prevention currently existing. The material is stated from modern positions and is designed for students of senior courses of all faculties of medical universities, doctors - interns, pediatricians, infectiousons and doctors of other specialties that are interested in this infection.
Nonspecific inflammation of a heart-shaped process. The Cell-shaping process is part of the gastrointestinal trader, which is formed from the wall of the blind intestine, in most cases departs from the rear-mounted wall of the blind intestine at the confluence of the three tapes of the longitudinal muscles and is directed from the blind bowel of the book and medial. Cylindrical processing form. Length 7-8cm, thickness 0.5-0.8 cm. Covered with peritoneum from all sides and has a mesentery, which has mobility. Blood supply according to A.APPendicularis, a branch of A.Ileocolica. Venous reaches v.Ileocolica in V.Mesenterica Superior and V.Porte. Sympathetic innervation Upper-hard and ventilating, and parasympathetic - fibers of wandering nerves.
It is prohibited to use locally warmth, heating on the abdomen, to introduce drugs and other painful, to give the laxative and use enema.
In the absence of spilled peritonitis - the operation of access Mac-Burnea (Volkovich-Dyakonov).
Cut the subcutaneous fatty tissue, then dissect the aponeurosis of the outer oblique muscle in the course of the fibers, then the outer slash itself.
After breeding, the edges of the wound detect the inner oblique muscle. In the center of the wound dissect perimisias of oblique muscle, then with two anatomical tweezers bluntly push the inner oblique and transverse abdominal muscles along the fibers. Hooks move deeper to keep the lifted muscles. The prettier fiber to the edges of the wound is stupid. The peritoneum is lifted by two anatomical tweezers in the form of a cone and cut into a scalpel or scissors throughout I see.
The edges of the dissected peritoness are captured by the clamps of the Mikulich type and the incision it is expanding up and the book is 1.5- 2 cm. Now all the layers of the wound, including the peritoneum, push out stupid hooks .. as a result, access is created, quite sufficient to remove from the abdominal cavity of the blind intestine and Draw-shaped process.
Then appendectomy. In extracting the process, the mesentery intersects it between the hemostatic clamps and tied up with thread; At the same time, it is necessary to ensure that the first one (nearest to the base of the process) is hitting the ligature. Appendicularis to avoid bleeding. The so-called ligatural method, in which the cult is not immersed in the pussy, is too risky; In adults, they should not use. Around the base of the process on the blind intestine is imposed (without tightening) with a brine seam. The base of the process is tied up with ligature, cut off the process, the culture is immersed in the intestinal lumen, after which the brush suture is tightened.
Having finished the removal of the process, checking the hemostasis and lowering the intestine into the abdominal cavity, remove gauze napkins.
Now the laparoscopic appendectomy was widely distributed - the removal of appendix through a small puncture of the BS. 3 punctures: one by 1 cm above the navel, another 4 cm under the navel and the third depending on the location of the process.