What kind of disease is mononucleosis and how to treat it. Infectious mononucleosis Infectious mononucleosis code according to mcb 10
Infectious mononucleosis (mononucleosis infectiosa, Filatov's disease, monocytic tonsillitis, benign lymphoblastosis) - acute anthroponous viral infection with fever, damage to the oropharynx, lymph nodes, liver and spleen and specific changes in the hemogram.
The clinical manifestations of the disease were first described by N.F. Filatov ("Filatov's disease", 1885) and E. Pfeiffer (1889). Changes in the hemogram have been studied by many researchers (Berne J., 1909; Taydi G. et al., 1923; Schwartz E., 1929, and others). In accordance with these characteristic changes, American scientists T. Sprant and F. Evans called the disease infectious mononucleosis. The causative agent was first identified by the English pathologist M.A. Epstein and Canadian virologist I. Barr from Burkitt's lymphoma cells (1964). The virus was later named the Epstein-Barr virus.
What provokes Infectious mononucleosis:
The causative agent of infectious mononucleosis- DNA genomic virus of the genus Lymphocryptovirus of the Gammaherpesvirinae subfamily of the Herpesviridae family. The virus is capable of replicating, including in B-lymphocytes; unlike other herpes viruses, it does not cause cell death, but, on the contrary, activates their proliferation. Virions include specific antigens: capsid (VCA), nuclear (EBNA), early (EA) and membrane (MA) antigens. Each of them is formed in a specific sequence and induces the synthesis of the corresponding antibodies. In the blood of patients with infectious mononucleosis, antibodies to the capsid antigen first appear, and later antibodies to EA and MA are produced. The causative agent is unstable in the external environment and quickly dies when it dries, under the influence of high temperature and disinfectants.
Infectious mononucleosis is just one form of Epstein-Barr virus infection, which also causes Burkitt's lymphoma and nasopharyngeal carcinoma. Its role in the pathogenesis of a number of other pathological conditions is poorly understood.
The reservoir and source of infection is a person with a manifest or erased form of the disease, as well as a carrier of the pathogen. Infected persons shed the virus from the last days of incubation and for 6-18 months after the primary infection. In swabs from the oropharynx in 15-25% of seropositive healthy people also detect the virus. The epidemic process is supported by persons who have previously suffered an infection and have excreted the pathogen with saliva for a long time.
Transmission mechanism- aerosol, transmission route - airborne. Very often, the virus is excreted in saliva, so infection by contact is possible (with kissing, sexually, through hands, toys and household items). Transmission of infection is possible through blood transfusions, as well as during childbirth.
Natural susceptibility of people high, however, mild and erased forms of the disease predominate. The presence of innate passive immunity may be evidenced by the extremely low incidence of children in the first year of life. Immunodeficiency states contribute to the generalization of the infection.
The main epidemiological signs. The disease is widespread; mostly sporadic cases are recorded, sometimes small outbreaks. The polymorphism of the clinical picture, rather frequent difficulties in diagnosing the disease suggest that the level of officially registered morbidity in Ukraine does not reflect the true breadth of the spread of infection. Most often adolescents get sick, in girls the maximum incidence is recorded at 14-16 years old, in boys - at 16-18 years old. Therefore, infectious mononucleosis is sometimes also called "student disease". Persons over 40 years of age rarely get sick, but in HIV-infected people, reactivation of latent infection is possible at any age. When infected early childhood the primary infection proceeds in the form of a respiratory disease, at older ages it is asymptomatic. By the age of 30-35, antibodies to the virus of infectious mononucleosis are detected in the blood of most people, therefore, clinically expressed forms are rarely found among adults. Diseases are recorded throughout the year, somewhat less often in the summer months. Crowding, the use of shared linen, dishes, and close household contacts contribute to the infection.
Pathogenesis (what happens?) During Infectious mononucleosis:
Penetration of the virus into the upper sections respiratory tract leads to damage to the epithelium and lymphoid tissue of the oropharynx and nasopharynx. Edema of the mucous membrane, enlargement of the tonsils and regional lymph nodes are noted. With subsequent viremia, the pathogen is introduced into B-lymphocytes; being in their cytoplasm, it disseminates throughout the body. The spread of the virus leads to systemic hyperplasia of lymphoid and reticular tissues, and therefore atypical mononuclear cells appear in the peripheral blood. Lymphadenopathy, edema of the mucous membrane of the nasal concha and oropharynx develop, the liver and spleen enlarge. Histologically, hyperplasia of lymphoreticular tissue in all organs, lymphocytic periportal infiltration of the liver with minor dystrophic changes in hepatocytes is revealed.
Replication of the virus in B-lymphocytes stimulates their active proliferation and differentiation into plasma cells. The latter secrete immunoglobulins of low specificity. At the same time, in the acute period of the disease, the number and activity of T-lymphocytes increase. T-suppressors inhibit the proliferation and differentiation of B-lymphocytes. Cytotoxic T-lymphocytes destroy virus-infected cells by recognizing membrane virus-induced antigens. However, the virus remains in the body and persists in it throughout subsequent life, causing chronic course diseases with reactivation of infection with a decrease in immunity.
The severity of immunological reactions in infectious mononucleosis makes it possible to consider it a disease of the immune system, therefore it is referred to the group of diseases of the AIDS-associated complex.
Symptoms of Infectious Mononucleosis:
Incubation period varies from 5 days to 1.5 months. A prodromal period with no specific symptoms is possible. In these cases, the disease develops gradually: for several days, subfebrile body temperature, malaise, weakness, increased fatigue, catarrhal phenomena in the upper respiratory tract - nasal congestion, hyperemia of the mucous membrane of the oropharynx, enlargement and hyperemia of the tonsils are observed.
With an acute onset of the disease body temperature rises quickly to high numbers... Patients complain of headache, sore throat when swallowing, chills, increased sweating, body aches. In the future, the temperature curve can be different; the duration of the fever varies from several days to 1 month or more.
By the end of the first week of the disease, the height of the disease develops. The appearance of all major clinical syndromes: general toxic phenomena, tonsillitis, lymphadenopathy, hepatolienal syndrome. The patient's state of health worsens, they note a high body temperature, chills, headache and body aches. There may be nasal congestion with difficulty in nasal breathing, nasal voice. Lesions of the throat are manifested by an increase in sore throat, development of sore throat in catarrhal, ulcerative-necrotic, follicular or membranous form. Hyperemia of the mucous membrane is not sharply expressed, friable yellowish easily removable plaques appear on the tonsils. In some cases, plaque can resemble diphtheria. On the mucous membrane of the soft palate, hemorrhagic elements may appear, the posterior wall of the pharynx is sharply hyperemic, loosened, granular, with hyperplastic follicles.
From the very first days it develops lymphadenopathy... Enlarged The lymph nodes can be found in all areas accessible to palpation; the symmetry of their defeat is characteristic. Most often, with mononucleosis, the occipital, submandibular and especially the posterior cervical lymph nodes increase on both sides along the course of the sternocleidomastoid muscles. The lymph nodes are indurated, mobile, painless or slightly painful on palpation. Their sizes range from a pea to walnut... The subcutaneous tissue around the lymph nodes may in some cases be edematous.
In most patients, during the height of the disease, an increase in the liver and spleen is noted. In some cases, icteric syndrome develops: dyspeptic symptoms (decreased appetite, nausea) intensify, urine darkens, icterus of the sclera and skin appears, serum bilirubin increases and the activity of aminotransferases increases.
Sometimes exanthema of a maculopapular character appears. It has no specific localization, is not accompanied by itching and quickly disappears without treatment, leaving no changes on the skin.
Following the period of the peak of the disease, lasting on average 2-3 weeks, there comes recovery period... The patient's state of health improves, body temperature normalizes, tonsillitis and hepatolienal syndrome gradually disappear. In the future, the size of the lymph nodes is normalized. The duration of the convalescence period is individual, sometimes low-grade body temperature and lymphadenopathy persist for several weeks.
The disease can last for a long time, with a change in periods of exacerbation and remission, because of which its total duration can be delayed up to 1.5 years.
The clinical manifestations of infectious mononucleosis in adult patients differ in a number of features. The disease often begins with the gradual development of prodromal phenomena, fever often persists for more than 2 weeks, the severity of lymphadenopathy and tonsil hyperplasia is less than in children. At the same time, in adults, manifestations of the disease associated with the involvement of the liver in the process and the development of icteric syndrome are more often observed.
Complications of infectious mononucleosis
The most common complication is accession bacterial infections caused by Staphylococcus aureus, streptococci, etc. Meningoencephalitis, obstruction of the upper respiratory tract with enlarged tonsils are also possible. In rare cases, bilateral interstitial infiltration of the lungs with severe hypoxia, severe hepatitis (in children), thrombocytopenia, and rupture of the spleen are noted. In most cases, the prognosis of the disease is favorable.
Diagnosis of Infectious Mononucleosis:
Infectious mononucleosis should be distinguished from lymphogranulomatosis and lymphocytic leukemia, angina coccal and other etiology, oropharyngeal diphtheria, and viral hepatitis, pseudotuberculosis, rubella, toxoplasmosis, chlamydial pneumonia and ornitosis, some forms of adenovirus infection, CMV infection, primary manifestations of HIV infection. Infectious mononucleosis is distinguished by a combination of the main five clinical syndromes: general toxic phenomena, bilateral tonsillitis, polyadenopathy (especially with damage to the lymph nodes along the sternocleidomastoid muscles on both sides), hepatolienal syndrome, and specific changes in the hemogram. In some cases, jaundice and (or) maculopapular exanthema are possible.
Laboratory diagnostics of infectious mononucleosis
Most characteristic feature- changes in the cellular composition of the blood. The hemogram reveals moderate leukocytosis, relative neutropenia with a shift leukocyte formula to the left, a significant increase in the number of lymphocytes and monocytes (more than 60% in total). The blood contains atypical mononuclear cells - cells with a wide basophilic cytoplasm that have different shape... Their presence in the blood has determined the modern name of the disease. An increase in the number of atypical mononuclear cells with a wide cytoplasm is of diagnostic value to at least 10-12%, although the number of these cells can reach 80-90%. It should be noted that the absence of atypical mononuclear cells with characteristic clinical manifestations the disease does not contradict the alleged diagnosis, since their appearance in the peripheral blood can be delayed until the end of the 2-3rd week of the disease.
During the period of convalescence, the number of neutrophils, lymphocytes and monocytes gradually normalizes, but quite often atypical mononuclear cells persist for a long time.
Virological diagnostic methods (isolation of the virus from the oropharynx) are not used in practice. PCR can detect viral DNA in whole blood and serum.
Serological methods have been developed for the determination of antibodies of various classes to capsid (VCA) antigens. Serum IgM to VCA antigens can be detected already in incubation period; in the future, they are detected in all patients (this serves as a reliable confirmation of the diagnosis). IgM to VCA antigens disappear only 2-3 months after recovery. After the transferred disease, IgG to VCA antigens are preserved for life.
In the absence of the possibility of detecting anti-VCA-IgM, serological methods for the detection of heterophilic antibodies are still used. They are formed as a result of polyclonal activation of B-lymphocytes. The most popular are the Paul-Bunnel reaction with ram erythrocytes (diagnostic titer 1:32) and the more sensitive Hoff-Bauer reaction with horse erythrocytes. Lack of specificity of reactions reduces their diagnostic value.
All patients with infectious mononucleosis or suspicion of it need to undergo 3-fold (in the acute period, then after 3 and 6 months) laboratory examination for antibodies to HIV antigens, since mononucleosis-like syndrome is also possible at the stage of primary manifestations of HIV infection.
Treatment for Infectious Mononucleosis:
Patients with mild and moderate infectious mononucleosis can be treated at home. The need for bed rest is determined by the severity of intoxication. In cases of illness with manifestations of hepatitis, a diet is recommended (table number 5).
No specific therapy has been developed. They carry out detoxification therapy, desensitizing, symptomatic and restorative treatment, rinsing the oropharynx with antiseptic solutions. Antibiotics are not prescribed in the absence of bacterial complications. With a hypertoxic course of the disease, as well as with the threat of asphyxia caused by edema of the pharynx and a pronounced increase in the tonsils, a short course of treatment with glucocorticoids is prescribed (prednisolone inside daily dose 1-1.5 mg / kg for 3-4 days).
Prevention of Infectious Mononucleosis:
General preventive measures are similar to those in ARVI. No specific prophylaxis measures have been developed. Non-specific prophylaxis is carried out by increasing the general and immunological resistance of the organism.
RCHD (Republican Center for Healthcare Development of the Ministry of Health of the Republic of Kazakhstan)
Version: Clinical protocols MH RK - 2017
Immunodeficiency due to a hereditary defect caused by epstein-barr virus (D82.3), Infectious mononucleosis (B27)
Infectious diseases in children, Pediatrics
general information
Short description
Approved
Joint Commission on the Quality of Medical Services
Ministry of Health of the Republic of Kazakhstan
dated August 18, 2017
Protocol No. 26
Infectious mononucleosis- This is an acute viral disease (mainly the Epstein-Barr virus), which is characterized by fever, damage to the oropharynx, lymph nodes, liver, spleen and peculiar changes in blood composition (lymphomonocytosis, atypical mononuclear cells).
INTRODUCTORY PART
ICD-10 code (s):
| ICD-10 codes | ||
| B27 | Infectious mononucleosis | |
| B27.0 | Mononucleosis Caused by Gamma Herpes Virus Mononucleosis Caused by Epstein-Barr Virus | |
| B27.1 | Cytomegalovirus mononucleosis | |
| B27.8 | Other infectious mononucleosis | |
| B27.9 | Infectious mononucleosis, unspecified | |
| D82.3 | Immunodeficiency due to an inherited defect caused by Epstein-Barr virus | |
Date of development / revision of the protocol: 2017 year.
Abbreviations used in the protocol:
| EA | - | early EBV antigen of the Epstein-Barr virus |
| EBNA | - | Epstein-Barr virus nuclear antigen |
| IgG | - | immunoglobulins class G |
| IgM | - | class M immunoglobulins |
| VCA | - | Epstein-Barr virus capsular antigen |
| Hiv | - | AIDS virus |
| GP | - | general doctor |
| VEB | - | Epstein-Barr virus |
| DNA | - | Deoxyribonucleic acid |
| Gastrointestinal tract | - | gastrointestinal tract |
| ELISA | - | linked immunosorbent assay |
| ICD | - | international classification diseases |
| NSAIDs | - | non-steroidal anti-inflammatory drugs |
| UAC | - | general blood analysis |
| OAM | - | general urine analysis |
| PCR | - | polymerase chain reaction |
| ESR | - | erythrocyte sedimentation rate |
Protocol users: ambulance doctors emergency care, paramedics, general practitioners, pediatricians, pediatric infectious disease specialists, pediatric surgeons.
Evidence level scale:
| A | High-quality meta-analysis, systematic review of RCTs, or large RCTs with very low likelihood (++) of bias whose results can be generalized to the relevant population. |
| V | High-quality (++) systematic review of cohort or case-control studies or High-quality (++) cohort or case-control studies with very low risk of bias or RCTs with low (+) risk of bias that can be generalized to the relevant population ... |
| WITH |
A cohort or case-control study or controlled study without randomization with a low risk of bias (+). The results of which can be generalized to the relevant population or RCTs with very low or low risk of bias (++ or +), the results of which cannot be directly extended to the relevant population. |
| D | Case series description or uncontrolled research or expert opinion. |
| GPP | Best Clinical Practice. |
Classification
Classification:
Complications:
Early complications (1-3 weeks of illness): rupture of the spleen, asphyxia (due to pharyngotonsillar edema), myocarditis, interstitial pneumonia, encephalitis, cranial nerve palsy, including Bell's palsy, meningoencephalitis, polyneuritis, Guillain-Barré syndrome;
· Late complications (later than 3 weeks of illness): hemolytic anemia, thrombocytopenic purpura, aplastic anemia, hepatitis, malabsorption syndrome, etc., as a result of an autoimmune process.
Typical form characterized by fever, damage to the oropharynx, lymph nodes, liver, spleen and peculiar changes in blood composition (lymphomonocytosis against the background of leukocytosis and atypical mononuclear cells in an amount of 10% or more).
Atypical forms of infectious mononucleosis:
Erased form: proceeds with mild and rapidly passing forms, symptoms or under the mask of acute respiratory diseases, is diagnosed mainly in epidemic foci;
· Asymptomatic form: proceeds with the absence of clinical symptoms, is diagnosed on the basis of examination by hematological, serological methods and by the method of epidemiological analysis;
Visceral form: characterized by a severe course with multiple organ damage, involving the cardiovascular, central and peripheral nervous systems, kidneys, adrenal glands and other vital organs.
Diagnostics
DIAGNOSTIC METHODS, APPROACHES AND PROCEDURES
Diagnostic criteria:
| Complaints: |
|
... sore throat; ... fever (subfebrile / febrile, up to 2-4 weeks, sometimes more); ... weakness; . headache; ... sweating; ... fatigue (syndrome " chronic fatigue»); ... enlarged lymph nodes; ... Difficulty nasal breathing; ... pain in joints, muscles; ... rash. |
|
Anamnesis: ... acute / gradual onset of the disease; ... the appearance of a detailed clinical picture of the disease by the end of the 1st week of the disease; ... persistence of fever and intoxication for 1-4 weeks; ... combination of angina with systemic enlargement of lymph nodes, enlargement of the liver and spleen; ... possible appearance of a rash on the 3-5th day; ... the rarity of multiple organ lesions. Epidemiological factors: ... the presence of contact with a similar disease, or with a confirmed diagnosis of infectious mononucleosis. |
| Physical examination: |
|
... fever; ... enlargement of lymph nodes (symmetric), mainly anterior and / or posterior cervical (symptom of "bull's neck"), axillary and inguinal; ... angina; ... splenomegaly; ... hepatomegaly; ... adenoiditis; ... a rash, often of a maculopapular nature (in 10% of patients, and with ampicillin treatment - in 80%); ... periorbital edema; ... rashes in the sky; ... jaundice (intermittent symptom). |
Clinical criteria for the diagnosis of infectious mononucleosis:
| Sign | Characteristic |
| Fever | High, long |
| Syndrome of defeat of the mouth and nasopharynx | Tonsillitis syndrome with or without plaque, adenoiditis, pharyngitis |
| Lymph Node Syndrome | Predominantly an increase in the anterior and / or posterior cervical groups of lymph nodes, intra-abdominal lymph nodes, most often at the gate of the liver and spleen, hypertrophy of the palatine and pharyngeal tonsils |
| Hepatosplenomegaly syndrome | Enlargement of the liver and spleen |
| Syndrome of cytolysis of liver cells and disorders of pigment (bilirubin) metabolism of the Liver | Increased alanine aminotransminase, aspartate aminotransminase. Violation of liver pigment metabolism, manifested by jaundice and increased bilirubin |
| Exanthema syndrome | The rash is maculopapular, less often hemorrhagic with localization on the face, trunk, extremities, more often in the proximal regions, bright, abundant, sometimes draining. Itching, swelling of the face is possible. Appears on the 5-10th day of illness. |
Criteria for assessing the severity of infectious mononucleosis by clinical signs :
| Sign | Feature characteristic | |||
| Mild severity | Moderate severity | Severe severity | ||
|
Expressiveness and duration intoxication |
Missing or light severity, 1-5 days |
Moderate 6-7 days |
Pronounced more than 8 days |
|
|
severity and duration of fever |
temperature increase up to 38 ° С, duration 1-5 days |
temperature increase from 38.1 to 39 ° С, duration 6-8 days |
temperature increase more than 39.0 ° C, duration more than 9 days |
|
|
Character inflammatory changes in the roto and nasopharynx |
Inflammatory changes catarrhal character or with insular, thin blooms, lasting 1-3 days; obstruction of the nasal breathing 1-4 days |
Inflammatory changes with lacunar patches, lasting 4-6 days; difficulty nasal breathing 5-8 days |
Inflammatory changes with plaque, in some patients pseudo-membranous or necrotic, duration more than 7 days; difficulty in nasal breathing for more than 9 days |
|
|
Degree hypertrophy palatine tonsils, nasopharyngeal tonsils |
I degree |
II degree |
III degree |
|
|
Degree increase lymphatic knots |
Anterior cervical lymph nodes up to 1.0-1.5 cm; posterior cervical - up to 0.5-1.0 cm |
Anterior cervical lymph nodes up to 2.0-2.5 cm; posterior cervical up to 1.5-2.0 cm, single or "chain"; possible increase intra-abdominal lymph nodes |
Anterior cervical lymph nodes more than 2.5 cm; posterior cervical more than 2.5 cm or "packages"; increase intra-abdominal lymph nodes |
|
|
Degree increase liver, spleen |
Enlargement of the liver 1.0-1.5 cm; spleen 0.5 cm below the costal margin |
Enlargement of the liver 2.0-2.5 cm; spleen 1.0-1.5 cm below the edge of the costal arch |
Enlargement of the liver more than 3.0 cm; spleen - more than 2.0 cm below the costal margin |
|
|
The reverse development symptoms |
By the end of the 2nd week |
Clinical symptoms lasts 3-4 weeks |
Clinical symptoms more than 4-5 weeks |
|
| Complications | No | There are | There are | |
Laboratory research :
| UAC | leukopenia / moderate leukocytosis (12-25x109 / l); lymphomonocytosis up to 70-80%; neutropenia; increase in ESR up to 20-30 mm / h; atypical mononuclear cells (absence or increase from 10 to 50%). | |
| Serological (ELISA with determination of the avidity index) | detection of specific antibodies IgM VCA to EBV and IgG VCA, IgG EA, IgG-EBNA to EBV with determination of the avidity index | |
|
Additional laboratory tests: |
||
| Molecular genetic method (PCR) | detection of DNA of the Epstein-Barr virus in the blood. | |
|
Biochemical analysis blood (with hepatomegaly and jaundice) |
determination of the concentration of bilirubin and ALAT in the blood: moderate hyperenzymemia, hyperbilirubinemia. | |
| Bacteriological examination mucus from the tonsils and the posterior pharyngeal wall for aerobic and facultative anaerobic microorganisms | to identify the bacterial etiology of acute tonsillitis. | |
Criteria for laboratory confirmation of the diagnosis:
| Sign | Criteria |
| Atypical mononuclear cells | Detection of atypical mononuclear cells in the peripheral blood over 10% (from 2-3 weeks of illness) |
| Lymphomonocytosis | Detection of lymphomonocytosis in peripheral blood |
| IgM VCA VCA, IgG-EBNA of Epstein-Barr virus |
In the acute period: IgM VCA since development clinical signs diseases and the next 4-6 weeks are present and decrease, IgG EA from the first week of the disease builds up to several years after it, persists at a low level, IgG VCA is detected a few weeks after the appearance of IgM VCA, increases, persists for life at a high level, IgG- EBNA-1, 2- absent or in small quantities. During the recovery period: IgM VCA are absent or present in small quantities, IgG EA persist for life at a low level, IgG VCA persist for life IgG EBNA for several weeks after the onset of clinical signs and persist are detected after life at a low level |
| Determination of the avidity index | Detection of low avidity IgG with or without IgM indicates primary (recent) infection. The presence of highly avid IgG antibodies indicates a convalescence period |
| Epstein-Barr virus DNA in blood and saliva | Detection of virus DNA by PCR in blood (1-2 weeks after the onset of clinical symptoms), saliva. |
Instrumental research: no.
Indications for specialist consultation:
Consultation with an otorhinolaryngologist: with adenoiditis, the formation of a paratonsillar abscess, inflammatory processes from the side paranasal sinuses nose;
· Consultation with a hematologist: with the progression of hematological changes;
· Consultation with a surgeon: with severe abdominal pain syndrome.
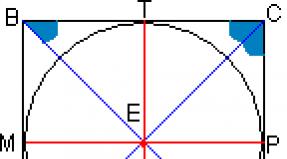
Diagnostic algorithm:(scheme)
Differential diagnosis
Differential diagnosis and justification for additional research :
| Diagnosis | Rationale for differential diagnosis | Surveys |
Exclusion criteria diagnosis |
| Adenovirus infection |
Fever, polyadenopathy, enlargement of the spleen and liver, pharyngitis, tonsillitis |
Detection of the virus in smears-prints from the nasal mucosa by immunofluorescence analysis. |
Lymph nodes are moderately enlarged, single, painless; rhinorrhea, productive cough, swelling of the tonsils is weak, overlap on them is rare. Often conjunctivitis, tonsillitis, pharyngitis, and diarrhea. |
| Measles |
Fever, polyadenopathy, puffiness of the face, rash |
Revealing immunoglobulins class M to measles virus ELISA method |
Polyadenopathy, maculopapular rash with a characteristic staged rash, pronounced catarrhal phenomena, rhinorrhea, redness of the eyes, Filatov-Koplik-Belsky spots |
|
CMVI (mononucleosis-like the form) |
Fever, polyadenopathy, hepatolienal syndrome, increased activity liver enzymes, adenoiditis, tonsillitis |
Leukopenia, lymphocytosis, atypical mononuclear cells more 10% Microscopy of urine and saliva to identify cytomegalocytes Detection of IgM- antibodies by ELISA PCR of urine and blood |
Lateral cervical lymph nodes rarely increase, tonsillitis and pharyngitis are characteristic. |
|
HIV (mononucleosis-like syndrome) |
Fever, polyadenopathy, rash, hepatolienal syndrome |
Leukopenia, lymphopenia, atypical mononuclear cells up to 10% ELISA Immunoblotting PCR |
Individual lymph nodes of different groups are enlarged, painless, bilateral damage to the cervical nodes is not typical, tonsillitis is not typical, rash is frequent, not associated with ampicillin intake, ulcerative lesions of the oral mucosa and genital organs, manifestations of opportunistic infections (candidiasis). |
| Acute tonsillitis | Tonsillitis, lymphadenitis |
Neutrophilic shift leukocytosis to the left, increased ESR, atypical mononuclear cells are not observed. Allocation of β- hemolytic group A streptococcus in swabs from the tonsils. |
Sharp intoxication, chills, bright hyperemia of the tonsils, as a rule, purulent tonsillitis, pharyngitis is not observed, there is no enlargement of the spleen, only the maxillary lymph nodes are enlarged and painful. |
|
Diphtheria of the oropharynx, localized, toxic |
Tonsillitis with overlays tonsils, fever, lymphadenitis, swelling of the neck is possible. |
Moderate leukocytosis, neutrophilia, atypical mononuclear cells absent. Isolation of a toxigenic strain C.diphtheriae from swabs from the tonsils. |
With localized diphtheria, the plaque on the tonsils is dense, white or gray, monotonous; with toxic diphtheria, it extends beyond the tonsils, cannot be removed with a spatula, does not dissolve and does not sink in water. No pharyngitis. Hyperemia with toxic diphtheria in the pharynx is bright, edema of the tissue covers the submandibular region, then the neck and spreads to the subclavian region and chest. The maxillary and anterior cervical lymph nodes are enlarged. |
| Viral hepatitis |
Hepatosplenomegaly yellowness of the skin and mucous membranes, dark urine, acholic stools, hepatic symptoms intoxication |
· Leukopenia, neutropenia, relative lymphocytosis, atypical mononuclear cells are absent. OAM (urobilin, bile pigments) Biochemical analysis blood (an increase in the level of bound bilirubin, transferase activity). Viral markers hepatitis PCR |
Typical epidemiological history. Acute / gradual onset. The presence of a cyclical course, the preicteric period in the form of a combination of syndromes - asthenovegetative, dyspeptic, flu-like, arthralgic; possibly an increase in the symptoms of hepatic intoxication, the appearance hemorrhagic syndrome against the background of the appearance of jaundice. Hepatosplenomegaly, with more characteristic changes in the size of the liver. |
|
Benign lymphoreticulosis |
Polyadenopathy, fever, enlargement of the spleen |
· The blood picture is not typical. Atypical mononuclear cells are absent. PCR ELISA Lymph node biopsy examination |
Axillary, ulnar, less often parotid and inguinal lymph nodes are affected, the cervical group is not affected. General symptoms are observed at a later date with suppuration of the lymph nodes. Characterized by traces of cat scratches, primary affect. |
| Lymphogranulomatosis |
Polyadenopathy, fever, enlargement of the spleen |
Neutrophilia, lymphopenia, high ESR, atypical mononuclear cells are absent Histological biopsy examination lymph nodes |
Pharyngitis, tonsillitis are absent. Mainly, the lymph nodes of one group increase, which form a conglomerate, dense, painless. Fever accompanied by sweating, weight loss. |
Treatment abroad
Undergo treatment in Korea, Israel, Germany, USA
Get advice on medical tourism
Treatment
Preparations ( active ingredients) used in the treatment
Treatment (outpatient clinic)
TACTICS OF TREATMENT AT THE AMBULATORY LEVEL
Children with mild severity receive treatment on an outpatient basis. Etiotropic therapy is carried out in combination with IFN drugs. Antibiotics are prescribed for purulent-inflammatory changes in the oropharynx and inflammatory changes in blood tests.
Non-drug treatment:
Mode:
Half-bed (during the entire period of fever);
· Observance of patient hygiene: care of the mucous membranes of the oral cavity, eyes, nasal toilet;
Diet:
· Table number 13 (fractional warm drink, milk-vegetable diet).
Drug treatment:
With purulent tonsillitis of staphylococcal or streptococcal etiology (Staphylococcus aureus, Streptococcus pyogenes) - azithromycin the first day 10 mg / kg 1 time / day inside, then 5 mg / kg 1 time / day for four days or clarithromycin inside 7.5 mg / kg 2 times / day for 7 days.
:
List of additional medicines :
| Pharmacological group |
International generic name LS |
Mode of application | UD |
| Propionic acid derivatives | Ibuprofen | Suspension and tablets for oral administration. Suspension 100 mg / 5 ml; tablets 200 mg; | V |
| Macrolides | Azithromycin | for oral administration of capsules and tablets 125 mg, 250 mg, 500 mg, suspensions 100 mg / 5 ml and 200 mg / 5 ml in 20 ml vials | A |
| Macrolides | Clarithromycin | Oral suspension 125 mg / 5 ml. 250 mg / 5 ml | A |
Surgical intervention: no.
Further management
:
· Discharge to the children's team after clinical recovery;
Limitation of insolation and dispensary observation within 1 year;
· A blood test for atypical mononuclear cells and ALAT once every 3 months.
· Medical withdrawal from vaccination in mild and moderate form for 3 months and severe form for 6 months.
Medical withdrawal from classes physical education for 3 months.
Performance indicators:
· Stable temperature normalization for 3 days or more;
· Lack of intoxication;
· absence inflammatory process in the oropharynx;
· Reduction in the size of the lymph nodes;
· Normalization / significant reduction in the size of the liver and spleen;
· Normalization of the level of transaminases (ALAT);
· No recurrence of the disease.
Treatment (hospital)
STATIONARY TREATMENT TACTICS
At the inpatient level, children with moderate and severe forms of infectious mononucleosis receive treatment. Treatment includes pathogenetic and symptomatic therapy. The following factors influence the choice of treatment tactics:
· Period of illness;
· The severity of the disease;
· The patient's age;
· The presence and nature of complications.
Antibiotics are prescribed for severe forms of the disease, with purulent-necrotic changes in the oropharynx and inflammatory changes in blood tests.
Patient observation chart, patient routing:
Drug-free treatment :
Mode:
Bed (during the period of fever), semi-bed;
· Patient hygiene: hygienic care of the mucous membranes of the oral cavity, nasal toilet.
Diet:
· Table No. 13, No. 5 (in case of liver damage) fractional warm drink, lacto-vegetable diet;
Drug treatment:
For relief of hyperthermic syndrome above 38.5 o C, paracetamol 10-15 mg / kg is prescribed with an interval of at least 4 hours, no more than three days by mouth or per rectum or ibuprofen at a dose of 5-10 mg / kg, no more than 3 once a day by mouth;
Infusion therapy is indicated for patients with a severe form of the disease (infusion volume from 30 to 50 ml / kg of body weight per day) with the inclusion of solutions: 5% or 10% dextrose (10-15 ml / kg), 0.9% sodium chloride ( 10-15 ml / kg);
· Hormonal therapy is used for complications - encephalitis and thrombocytopenic purpura;
With convulsions - diazepam 0.5% solution (0.2-0.5 mg / kg) IM; or i / v; or rectally;
· antibiotic therapy with purulent tonsillitis of staphylococcal or streptococcal etiology (Staphylococcus aureus, Streptococcus pyogenes) - cefuroxime 50-100 mg / kg per day IM 2-3 times a day for 5-7 days or ceftriaxone 50-80 mg / kg per day / m 1-2 times a day for 5-7 days.
NB! In infectious mononucleosis, the following antibiotics are contraindicated:
· Ampicillin - due to the frequent appearance of a rash and the development of a drug disease;
Chloramphenicol, and sulfa drugs- in connection with the suppression of hematopoiesis.
Essential Medicines List :
List of Complementary Medicines :
| Benzodiazepine derivatives | Diazepam | Solution for intramuscular and intravenous injection or per rectum, 5 mg / ml, 2 ml | V |
| Ceftriaxone | Powder for the preparation of a solution for intravenous and intramuscular administration 1 g | A | |
| Antibacterial drug - cephalosporin series | Cefuroxime | powder for preparation of solution for injection complete with solvent 250 mg, 750 mg, 1500 mg | A |
| Other irrigation solutions | Dextrose | solution for infusion 5% 200 ml, 400 ml; 10% 200 ml, 400 ml | WITH |
| Saline solutions | Sodium chloride solution | solution for infusion 0.9% 100 ml, 250 ml, 400 ml | WITH |
Surgical intervention: no.
Further management :
· Discharge of patients with infectious mononucleosis from the hospital is carried out after the disappearance of clinical symptoms, but earlier than 7 days from the moment of the disease;
· Dispensary observation by a doctor - pediatric infectious disease specialist / GP for 1 year;
· Examination by a doctor once a quarter to determine the severity of lymphadenopathy, hepatosplenomegaly, the presence of atypical mononuclear cells in the blood and the concentration of AlAt and AsAt.
· Compliance with diet No. 5 (if hepatitis is detected) within 6 months after suffering infectious mononucleosis;
· Medical withdrawal from physical education for 3 months;
· Recommendations for the patient - limitation of insolation for 1 year;
Convalescents who have undergone viral and bacterial pneumonia - clinical examination within 1 year (with control clinical and laboratory examinations after 3 ( light form), 6 (moderate) and 12 months (severe) after illness;
Convalescents who have suffered a defeat nervous system(meningitis, encephalitis, meningoencephalitis) - at least 2 years, with control clinical and laboratory examinations 1 time in 3 months during the first year, then 1 time in 6 months. in subsequent years.
Treatment effectiveness indicators:
Relief of general toxic syndrome (normalization of body temperature);
Relief of signs of tonsillitis / pharyngitis;
· Reduction of lymphadenopathy;
· Reduction of hepatosplenomegaly;
· No recurrence of the disease and complications;
Normalization of indicators general analysis blood;
· Negative result of PCR blood.
Hospitalization
INDICATIONS FOR HOSPITALIZATION WITH INDICATION OF THE TYPE OF HOSPITALIZATION
Indications for planned hospitalization : No.
Indications for emergency hospitalization:
• age up to 5 years with the presence of general signs of danger (cannot drink or suckle the breast, vomiting after every meal and drink, a history of convulsions of this disease and is lethargic or unconscious);
According to clinical indications, moderate and heavy course infectious mononucleosis;
Severe tonsillitis syndrome and / or sore throat syndrome, jaundice, airway obstruction, abdominal pain and the development of complications (surgical, neurological, hematological, from the cardiovascular and respiratory system, Reye's syndrome in specialized hospitals).
Information
Sources and Literature
- Minutes of meetings of the Joint Commission on the Quality of Medical Services of the Ministry of Health of the Republic of Kazakhstan, 2017
- 1) V.F. Uchaikin, N.I. Nisevich, O.V. Shamsheva. Infectious diseases in children; textbook - M .: GEOTAR - Media, 2010. - 688 p .: ill. 2) Simovanyan E.N. Infectious diseases in children. "Reference book in questions and 3) answers", publishing house "Phoenix" - Rostov n / a, 2011. - 767 p. 4) EBV infection (etiology, pathogenesis, clinical picture, diagnosis, treatment): tutorial / D.M. Sobchak [and others]. - Nizhny Novgorod: Publishing house Nizh GMA, 2010. - 72 p. 5) Infectious diseases in children: ed. prof. V.N. Timchenko. - 4th ed., Rev. and add. - SPb. SpetsLit, 2012 .-- 218-224 p. 6) Drăghici S., Csep A. Clinical and paraclinical aspects of infectious mononucleosis. 7) // BMC Infectious Diseases, 2013 .-- 13, Suppl 1. - P.65. 8) Sakamoto Y. et al. Quantification of Epstein-Barr virus DNA is helpful for evaluation of chronic active Epstein-Barr virus infection. // Tohoku J. Exp. Med. 2012. -V.227. - P.307-311. 9) Joo EJ., Ha YE., Jung DS. et al. An adult case of chronic active Epstein-Barr virus infection with interstitial pneumonitis. // Korean J.Intern. Med., 2011. - V.26. - P.466-469. 10) Green M., Michaels M.G. Epstein – Barr virus infection and posttransplant lymphoproliferative disorder. // American Journal of Transplantation, 2013. V.13. - P.41–54. 11) Hurt C., Tammaro D. Diagnostic Evaluation of Mononucleosis-Like Illnesses. // The Am. J. Med., 2007. - V. 120. - P.911.e1-911.e8. 12) Koufakis T., Gabranis I. Infectious mononucleosis skin rash without previous antibiotic use. // The Braz. J. Infect. Dis., 2015. - V.19 (5). - P.553. 13) Yan Wang, Jun Li, et al. The levels of liver enzymes and atypical lymphocytes are higher in youth patients with infectious mononucleosis than in preschool children. // Clin. Molecul. Hepatol., 2013. - V. 19. - P.382-388. 14) Infectious mononucleosis in Turkish children / A.B. Cengiz // Turk J Pediatr. - 2010. –Vol. 52, No. 3. - P. 245-254. 15) Usami O., Saitoh H., Ashino Y., Hattori T. Acyclovir reduces the duration of fever in patients with infectious mononucleosis-like illness. // Tohoku J. Exp. Med., 2013. - V. 299. P.137-142. 16) Banerjee I., Mondal S., Sen S. et al. Azithromycin-induced rash in a patient of infectious mononucleosis - a case report with review of literature. //J.Clin. and Diagn. Res., 2014. - Vol. 8 (8). - HD01-HD02. doi: 10.7860 / JCDR / 2014 / 9865.4729. 17) Rezk E., Nofal YH., Hamzeh A. et al. Steroids for symptom control in infectious mononucleosis. // Cochrane Database Syst Rev., 2015. - V.8 (11). - CD004402. doi: 10.1002 / 14651858.CD004402.pub3. 18) Kazama I., Miura C., Nakajima T. Nonsteroidal Anti-Inflammatory Drugs Quickly Resolve Symptoms Associated with EBV-Induced Infectious Mononucleosis in Patients with Atopic Predispositions. //Am.J. Case Rep., 2016. - V.17. - P.84-88. DOI: 10.12659 / AJCR.895399. 19) Large reference book of medicines / ed. L. E. Ziganshina, V. K. Lepakhin, V. I. Petrov, R. U. Khabriev. - M .: GEOTAR-Media, 2011 .-- 3344 p. 20) BNF for children 2014-2015
Information
ORGANIZATIONAL ASPECTS OF THE PROTOCOL
List of protocol developers with qualification data:
1) Efendiev Imdat Musa oglu - Candidate of Medical Sciences, Head of the Department of Pediatric Infectious Diseases and Phthisiology, State Medical University of Semey City.
2) Baesheva Dinagul Ayapbekovna - Doctor of Medical Sciences, Associate Professor, Head of the Department of Children's Infectious Diseases, JSC "Astana Medical University".
3) Kuttykuzhanova Galiya Gabdullaevna - Doctor of Medical Sciences, Professor, Professor of the Department of Pediatric Infectious Diseases of the Republican State Enterprise at the REM "Kazakh National Medical University named after S. D. Asfendiyarov.
4) Devdariani Khatuna Georgievna - Candidate of Medical Sciences, Associate Professor of the Department of Children's Infectious Diseases, Republican State Enterprise at the REM "Karaganda State Medical University".
5) Zhumagalieva Galina Dautovna - Candidate of Medical Sciences, Associate Professor, Head of the Course of Children's Infections State University them. Marat Ospanov ".
6) Mazhitov Talgat Mansurovich - Doctor of Medical Sciences, Professor, Professor of the Department clinical pharmacology, JSC "Astana Medical University".
7) Umesheva Kumuskul Abdullaevna - Ph.D. S. D. Asfendiyarov ".
8) Alshynbekova Gulsharbat Kanagatovna - candidate of medical sciences, acting Professor of the Department of Children's Infectious Diseases, Republican State Enterprise at the REM "Karaganda State Medical University".
No Conflict of Interest Statement: No .
Reviewers:
1. Kosherova Bakhyt Nurgalievna - Doctor of Medical Sciences, Professor of the RSE at the REM "Karaganda State Medical University" Vice-Rector for clinical work and continuous professional development, Professor of the Department of Infectious Diseases.
Indication of the conditions for revision of the protocol: revision of the protocol 5 years after its publication and from the date of its entry into force or if there are new methods with a level of evidence.
Attached files
Attention!
- Self-medication can cause irreparable harm to your health.
- The information posted on the MedElement website and in the mobile applications "MedElement", "Lekar Pro", "Dariger Pro", "Diseases: Therapist's Guide" cannot and should not replace an in-person consultation with a doctor. Be sure to contact medical institutions if you have any medical conditions or symptoms that bother you.
- The choice of medicines and their dosage should be discussed with a specialist. Only a doctor can prescribe the necessary medicine and its dosage, taking into account the disease and the condition of the patient's body.
- MedElement website and mobile applications "MedElement", "Lekar Pro", "Dariger Pro", "Diseases: Therapist's Guide" are exclusively information and reference resources. The information posted on this site should not be used to unauthorized changes in the doctor's prescriptions.
- The editors of MedElement are not responsible for any damage to health or material damage resulting from the use of this site.
Treatment of infectious mononucleosis in adults should be carried out comprehensively and immediately, so that the infection does not spread throughout the body and does not become a provocateur of serious complications.
The disease is characterized by a change in leukocytes in the blood, provoking the development reactive lymphadenitis, while the lymph nodes, liver and spleen increase in size.
DNA is a genomic virus, which is the causative agent of an infectious disorder, is in human saliva for a long time, the patient poses a danger to others within six months after infection.
Common routes of transmission:
- saliva while kissing;
- through personal hygiene and household items;
- when shaking hands;
- when carrying out a blood transfusion procedure;
- during intercourse;
- during childbirth.
The clinical picture of the disease
In adults, the incubation period lasts about 20-60 days, during which time the virus passes from the nasopharynx, digestive tract, genital tract and enters the bloodstream, is introduced into lymphocytes, which become carriers of infection.
In the acute stage, the following symptoms develop:
- general weakness of the body;
- drowsiness;
- muscle and headache;
- decrease in apatite;
- temperature rise up to 38 degrees;
- the lymph nodes increase in size.
There is a sore throat, coughing, perspiration, in addition, there may be a rash on the skin, which is similar to the signs of scarlet fever. If you don't start timely treatment, then after 2 weeks complications may develop.
Effects in children and adults
A ruptured spleen, in some cases an abscess or swelling of the throat may develop. Hepatitis occurs with severe jaundice, cardiac complications, psychosis, paralysis of facial muscles, pneumonia, respiratory tract diseases.
If the treatment is carried out under the supervision of a doctor, then many of the consequences can be easily avoided. The main thing is not to self-medicate and consult a specialist at the first symptoms.
Treatment of the disease in adults
First ambulance:
- gargling with furacilin, iodinol;
- lowering the temperature with paracetamol;
- strengthen immunity through vitamin and herbal preparations;
- for problems with the respiratory system, take corticosteroids;
- avoid contact with young children;
- lead an active lifestyle, temper the body, eat right, devote time to physical activity.
In order for infectious mononucleosis, the microbial code 10 of which is B 27.9, to not spread throughout the body, it is necessary to direct therapeutic therapy to eliminate the symptoms of the violation and observe preventive measures to help avoid relapse.
What therapy is prescribed for adults?

Diet for infectious mononucleosis
When consumed drugs you need to drink plenty of liquid, add dairy food, fish, lean meats, salads, boiled vegetables, fruits, cereals, mashed potatoes, durum pasta to the menu.
In this case, you need to avoid heavy, fatty, fried, spicy, junk food, remove animal fats, beans, peas, sausages, semi-finished products, pickled products, lard and smoked meats, sweets, coffee, spices from the diet.
As for drinks, you need to give preference to herbal decoctions, fruit drinks from cranberries, currants, cook dried fruit compotes, tea with lemon, rosehip infusion, and so on. Alcohol and caffeinated formulations are taboo.
Traditional methods of treatment for infectious mononucleosis
 You can prepare medicinal infusions based on medicinal plants(chamomile, calendula, immortelle, string, chicory, burdock), pour a spoonful of raw materials with 500 ml of boiling water, soak in a thermos for 6-8 hours, drink a spoonful before each meal.
You can prepare medicinal infusions based on medicinal plants(chamomile, calendula, immortelle, string, chicory, burdock), pour a spoonful of raw materials with 500 ml of boiling water, soak in a thermos for 6-8 hours, drink a spoonful before each meal.
To get rid of the symptoms of intoxication, you can use linden or lingonberry tea, adding a slice of lemon to it. Elderberry infusion helps to improve immunity, take 2 tablespoons 6 times a day.
Before use folk recipes you need to consult with your doctor, so as not to aggravate the course of the disease. This is especially true for children, pregnant women, breastfeeding, the elderly.
Forecast
In most cases, the disease proceeds without complications and has a favorable outcome. Full recovery occurs in 1-2 months, the main thing is to strengthen immune system, avoid contact with carriers of the virus, listen to the instructions of the attending doctor.
In this case, the disease will recede without consequences and will not bother you anymore!
The onset is usually acute, but sometimes prodromal signs such as weakness, muscle pain, and fainting are noted. The temperature rises suddenly and reaches a level of 39-39.5C in 1-2 days. But sometimes in the first 8-10 days the temperature is kept at subfebrile numbers and only after this time it rises to the indicated febrile numbers.
In some cases, the temperature is kept at 38-39C for up to 2 weeks, and then at subfebrile numbers for up to 1-2 months. Against the background of an increase in temperature, angina and swelling of the lymph nodes develop. However, often all three symptoms occur at the same time.
A constant and main symptom of the disease is systemic enlargement and inflammation of the lymph nodes. The most typical is an increase in the cervical lymph nodes located along the posterior edge of the sternocleidomastoid muscle - (in 95% of cases). But the submandibular and occipital lymph nodes are also often enlarged. Less often, the inguinal and femoral lymph nodes are enlarged. Their size ranges from 1 to 3 cm in diameter, they are dense, mobile, not welded together, moderately painful on palpation. There are times when the lymph nodes do not enlarge. However, the lymph nodes are painful, which confirms their participation in the pathological process. Very rarely, there is an increase in the lymph nodes of the mediastinum and abdominal cavity. Cases of the disease are described, the clinical picture in which imitated acute appendicitis.
The most important symptom is angina. The forms of angina are very diverse: from catarrhal and follicular to ulcerative-necrotic and ulcerative-diphtheritic. Sometimes angina is accompanied by significant hyperemia of the mucous membrane of the pharynx and nasopharynx. In some cases, angina may precede characteristic changes in peripheral blood by 10-12 days. Very rarely, there is a petechial hemorrhagic rash on lower limbs or nosebleeds.
From the side internal organs 80-90% is characterized by an increase in the spleen 2-3 cm below the costal arch, to the touch it is dense, painless. The liver is enlarged in 65-70% of patients - approximately 1-3 cm below the costal arch. A fairly common symptom (20-30% of cases) is hepatitis with jaundice. Jaundice develops due to direct bilirubin, it is noted high level transaminases, lactate dehydrogenase. Sometimes hepatitis develops, which can lead to the death of the patient.
In addition, infectious mononucleosis is accompanied by symptoms of asthenia. Almost all patients have headache, blurred vision, weakness, sometimes abdominal pain with nausea and vomiting. In some cases, there may be photophobia, eye pain, cough, sometimes - skin erythema, thrombocytopenia, psychosis, cranial nerve paresis, radiculoneuritis.
In addition to the acute and subacute stages, in some patients the disease becomes chronic or recurrent. However, the prognosis for infectious mononucleosis is favorable. The main symptoms of the disease stop after 1-3 weeks, but asthenization persists for a long time.
The peripheral blood pattern is characterized by lymphocytosis, which reaches up to 30-40 109, mainly due to an increase in lymphocytes (up to 50-70%) and monocytes - from 10-12% at the onset of the disease to 40-50% at the height of the disease.
On microscopic examination, the nuclei in monocytes have a spongy structure and a more basophilic than usual cytoplasm. For monocytes with infectious mononucleosis, the phenomenon of a nuclear fragment is characteristic, which is localized separately in the cytoplasm and is a consequence of the destructive effect of the virus that enters the cell. In addition, there are atypical mononuclear cells, the presence of which is a pathognomonic sign. The same cells are observed in pharyngeal swabs and in cerebrospinal fluid.
Anemia is not typical for infectious mononucleosis, however, at the height of the disease, hemoglobin and the number of red blood cells decrease, especially when the main process is complicated by an autoimmune hemolytic anemia... The level of platelets usually remains within the normal range, and only in some cases does their number decrease. In the punctate of the bone marrow, a moderate increase in the level of lymphocytes, monocytes, plasma cells is found, 10% of which are atypical mononuclear cells.