Extragenital pathology in obstetrics: Iodine deficiency diseases. Iodine deficiency states: symptoms, description and treatment features Risk groups for iodine deficiency diseases
Transcript
1 MINISTRY OF HEALTH OF THE REPUBLIC OF BELARUS BELARUSIAN STATE MEDICAL UNIVERSITY 1st DEPARTMENT OF CHILDREN'S DISEASES A. V. Solntseva, N. I. Yakimovich IODINE DEFICIENCY DISEASES IN CHILDREN 2008 Teaching aid
2 UDC (075.8) LBC I 73 C 60 Approved by the Scientific and Methodological Council of the University as a teaching aid, minutes 10 Reviewers: Cand. honey. Sciences, Assoc. 1st department internal diseases of the Belarusian State Medical University Z. V. Zabarovskaya; Cand. honey. Sciences, Assoc. 1st department of internal diseases of the Belarusian State Medical University A.P. Shepelkevich C 60 Solntseva, A. V. Iodine deficiency states in children: study guide. allowance / A. V. Solntseva, N. I. Yakimovich. Minsk: BSMU, p. ISBN The modern aspects of etiopathogenesis, classification, clinical manifestations, diagnostics, prevention and treatment of iodine deficiency diseases in children of different ages are summarized. Designed for students of pediatric and medical faculties, trainee doctors. UDC (075.8) LBC i 73 ISBN Design. Belarusian State Medical University,
3 List of abbreviations WHO World Health Organization ID iodine deficiency IDD iodine deficiency diseases TAB fine-needle aspiration biopsy TRG thyrotropin-releasing hormone TSH thyroxine-binding globulin TSH thyroid-stimulating hormone T3 triiodothyronine T4 thyroxine st3 free triiodine thyroid test Thyroxine st3 free triiodine
4 Introduction Chronic iodine deficiency and related diseases determine wide range medical and social problems due to their high prevalence and serious clinical complications. According to the World Health Organization, more than a third of the world's inhabitants are deficient in iodine, 740 million people have an enlarged thyroid gland (endemic goiter), 43 million suffer from mental retardation resulting from a lack of this microelement. In the practice of a pediatrician, the main problem of ID is not the obvious manifestation of the latter (an increase in the size / volume of the thyroid gland), but the negative effect of iodine deficiency on the developing brain of the fetus and newborn and the subsequent intellectual development of the child. Against the background of chronic iodine deficiency, endemic goiter and neonatal hypothyroidism, the maturation and differentiation of the child's brain are disturbed with the manifestation of various pathological conditions: from a mild decrease in intelligence to severe forms of myxedema and neurological cretinism. Studies have shown that children born with ID have an IQ by points lower than their peers from iodine-rich areas. ID also causes impaired puberty and reproductive function, the formation of congenital malformations, and an increase in perinatal and child mortality. For Belarus, the problem of iodine deficiency is extremely urgent. According to the results of a large-scale study (A.N. Arinchin et al., 2000), conducted jointly with the WHO and the International Council for the Control of Iodine Deficiency Disorders, Belarus was classified as a country with mild and moderate natural ID (the median ioduria of the examined children in the country was 44 , 5 μg; continuous iodized salt intake ranged from 35.4 to 48.1%). The results obtained formed the basis for the development of a state strategy for the elimination of ID in our country, which is currently ongoing. Physiological role of iodine in the child's body Iodine is one of the vital microelements. As a structural component of thyroid hormones, it is involved in almost all metabolic processes human body... This microelement is a part of many natural organic compounds or is present in inorganic salts in the form of an iodide anion. 4
5 Iodine enters the body in inorganic and organic forms (Fig. 1). It is completely absorbed into small intestine(100% bioavailability). In the gastrointestinal tract, the organic "carrier" of the microelement is hydrolyzed, and iodide enters the bloodstream. In the blood, iodine circulates in the form of iodide or in a state associated with proteins. The concentration of the trace element in the blood plasma with an adequate intake is μg / l. From the blood, it easily penetrates into various tissues and organs. A significant part of the absorbed iodine (up to 17% of the administered amount) is selectively absorbed by the thyroid gland. Partially iodine accumulates in the organs that excrete it from the body: in the kidneys, salivary and mammary glands, gastric mucosa. Pool (reserve) of iodine 150 μg Iodine food, preparations 150 μg Thyroid pool Iodine tissues (liver, 12 mg of muscle bile, etc.) GIT 135 μg (urine) Hormonal pool 15 μg (feces) Fig. 1. Exchange of iodine in healthy person upon admission of 150 mcg per day Two-thirds of the incoming trace element is excreted in the urine (up to 70% of the administered amount), feces, saliva, and sweat. Iodine entering the body through the gastrointestinal tract makes up the majority of the extracellular pool. An additional pool of inorganic extracellular iodine is formed as a result of deiodination of thyroid hormones in the tissues and thyroid gland and during the release of iodine by thyrocytes. The total extracellular iodine pool is about 250 μg. The main depot of the microelement is the thyroid gland. After entering the blood, inorganic iodine is actively absorbed by the thyroid gland against the concentration gradient under the action of iodide / sodium symporter and ATP. The transport of iodine in the gland is regulated by the body's need for this trace element. 5
6 Secretion and metabolism of thyroid hormones The thyroid gland secretes μg T4 and 5 10 μg T3 per day. The following phases of thyroid hormone biosynthesis are distinguished: the first retention of iodides in the basement membrane of thyrocytes through active transport with the participation of iodide / sodium symporter and ATP (iodine mechanism); the second is the oxidation of iodide to molecular iodine by the action of the enzyme peroxidase and hydrogen peroxide; the third organification of iodine (iodization of tyrosine residues in thyroglobulin). Iodine in molecular form is highly active and quickly binds to the tyrosine amino acid molecule embedded in thyroglobulin. Depending on the quantitative ratio between iodine and free tyrosyl radicals, one or two iodine atoms are bound to one tyrosine molecule. Formed monoiodotyrosine or diiodotyrosine; fourth condensation. At the stage of oxidative condensation, the main product T4 is formed from two molecules of diiodotyrosine, from monoiodotyrosine and diiodotyrosine T3. In the blood and various biological fluids of the body, under the action of deiodinase enzymes, T4 is converted to more active T3. Approximately 80% of the total amount of T3 is formed as a result of T4 deiodination in peripheral tissues (mainly in the liver and kidneys), 20% is secreted by the thyroid gland. The hormonal activity of T3 is 3 times higher than that of T4. Deiodination of T4 at position 5 "increases biological efficiency, deiodination at position 3" cancels biological activity. Only L-isomers of thyroid hormones are biologically active. An alternative pathway of T4 metabolism is the formation of the positional T3 isomer of the reverse T3. The latter has no hormonal activity and does not inhibit the secretion of TSH. The total daily production of reverse T3 is 30 μg. With all violations of the formation of T3 from T4, the content of reverse T3 in serum increases. Free and bound thyroid hormones. Thyroid hormones are present in serum in free and bound forms. Only free T3 and T4 have hormonal activity. The content of free fractions is respectively 0.03 and 0.3% of their total serum concentration. The predominant amount of T3 and T4 is associated with transport proteins, primarily with thyroxine-binding globulin (75% bound T4 and more than 80% bound T3). Other proteins transthyretin (thyroxine-binding prealbumin) and albumin bind approximately 15% and 10% of T4, respectively. 6
7 Changes in binding protein concentrations affect thyroid hormone levels. With an increase in TSH values, the serum indicators of the general forms of T4 and T3 increase, with its deficiency, they decrease. There is a dynamic balance between the content of total and free fractions of thyroid hormones. An increase in TSH concentration initially leads to a short-term decrease in st4 and st3. The secretion of T3 and T4 increases compensatory. The total content of thyroid hormones in serum is increased until normal levels of st4 and st3 are restored. Thus, the levels of free T3 and T4 in serum do not change; therefore, the intensity of the processes regulated by them in the target tissues remains. Factors affecting the concentration of TSH are given in table. 1. Table 1 Factors affecting the content of thyroxine-binding globulin Excess TSH Pregnancy Acute hepatitis Chronic active hepatitis Estrogen-secreting tumors Reception of estrogens Narcotic substances (heroin, etc.) Idiopathic Hereditary TSH deficiency Nephrotic syndrome Hypoproteinemia Acromegaly Chronic liver diseases (cirrhosis) Androgen-secreting tumors Reception of androgens High doses of glucocorticosteroids or alterations of alloys lower affinity for these proteins than TSH. Hypothalamic-pituitary-thyroid system. The main stimulant of the production of T4 and T3 is TSH. In turn, TSH secretion is controlled by the mechanisms shown in Fig. 2. The peptide hormone thyroliberin (TRH) is formed in the nuclei of the hypothalamus and enters the portal system of the pituitary gland. Regulation of the secretion of TRH and TSH is carried out using a negative feedback mechanism and is closely related to the levels of T3 and T4. Thyroid hormones directly inhibit the production of TSH according to the principle of negative feedback, acting on the thyroid-stimulating cells of the adenohypophysis. In addition to TRH and thyroid hormones, other factors (estrogens, glucocorticoids, growth hormone, somatostatin) directly or indirectly affect TSH secretion, but their role is not so significant. 7
8 Fig. 2. The hypothalamic-pituitary-thyroid system. Mechanisms of regulation Physiological need for iodine According to modern international recommendations for the consumption of micronutrients, the daily intake of iodine is increased at the prenatal stage of development and during infancy. Table 2 provides a comparative analysis of these recommendations. Table 2 Recommendations for a person's daily iodine requirement (μg / day) Population category WHO / ICCIDD dose, Geneva (2001) Children: 0 to 5 years 90 6 to 12 years 120 Adolescents (> 12 years) and adults 150 Pregnant and lactating women 200 National Academy of Sciences, USA (2001) Children: 7 to 12 months 1 to 8 years 9 to 13 years Adolescents (> 14 years old) and adults 150 Pregnant women 220 Breastfeeding women 290 8
9 The main natural sources of iodine for humans are: products of plant and animal origin, drinking water and air (Fig. 2). The concentration of iodine in drinking water reflects its content in the soil. In iodine-deficient areas, the level of trace element in water is less than 2 μg / l. Most of the iodine enters the body through food. The largest amount of this trace element (about μg / kg) is found in seafood. Seaweed is especially rich in iodine. A significant amount of the trace element is found in fish oil. Vegetables, fruits, cereals do not have the ability to concentrate iodine, therefore, its content in them completely depends on the microelement composition of the soil. In plants grown on soils poor in iodine, its level is reduced and often does not exceed 10 μg / kg, compared to 100 μg / kg dry weight in plants grown on soils with a sufficient content of the trace element. Sources of iodine intake in the human body Vegetable products 34% Animal products 60% Drinking water 3% Air 3% Fig. 3. Main natural sources of iodine for humans Definition of IDD IDD refers to pathological conditions that develop in a population as a result of iodine deficiency and can be prevented with normal iodine intake (WHO, 2001). The lack of intake of this microelement in the body triggers the triggering of adaptive mechanisms aimed at maintaining the functional activity of the thyroid gland by changing the synthesis and secretion of its hormones. If ID persists long enough, then there is a breakdown of the adaptive mechanisms with the subsequent development of IDD (Table 3). The term "iodine deficiency diseases" was introduced by WHO in 1983. This emphasized that thyroid pathology is not the only and most severe consequence of iodine deficiency. The entire spectrum of IDD, depending on the period of the child's life, is presented in table. 3.9
10 Fetus Life period Newborns Children and adolescents of all ages Spectrum of iodine deficiency diseases in children (WHO, 2001) Table 3 Pathology Abortions Stillbirth Congenital anomalies Increased perinatal and infant mortality Neurological cretinism (mental retardation, deafness, strabismus) short stature) Psychomotor disorders High infant mortality Neonatal hypothyroidism Impaired mental and physical development Impaired reproductive function Goiter Hypothyroidism Impaired cognitive function Increased absorption of radioactive iodine in nuclear disasters Etiology of IDD Insufficient iodine intake is the main cause of IDD. Allocate: 1. Absolute ID: low levels of iodine intake from food; violation of iodine extraction from food and its resorption; reception of enterosorbents. 2. Relative ID (increased need): pregnancy; childbirth; lactation; active growth and puberty in children; intensive physical labor; high psycho-emotional stress; prolonged febrile conditions. 3. Violation of iodine organization: hypoxia and energy balance disturbance; binding of iodine with strumogenic substances. 4. Mixed type. ten
11 The most frequent reasons leading to the formation of absolute ID: the low social status of the population does not allow sufficient quantities of iodine-rich products (seafood, sea fish) to be consumed; dependence on irrationally organized meals (closed-type children's institutions); use of diets; long experience of diseases gastrointestinal tract; helminthic invasions. The reasons for relative ID can be: natural strumogens (due to the content of thiocyanates and isocyanates in them: plants belonging to the cruciferous family (cabbage, cauliflower, broccoli, Brussels sprouts, turnips, turnips, horseradish, lettuce, rapeseed and its seeds); products, containing cyanogenic glycosides (cassava, maize, corn, sweet potatoes, lima beans); flavonoids (stable compounds found in many fruits, vegetables and cereals (millet, sorghum, beans, groundnuts)); substances that block the transport of iodide to thyroid cells (nitrite, periodate, perchlorate, thiocyanate); drugs that interfere with the organification of iodine (para-aminobenzoic acid, thiourea and thiouracil derivatives, aminothiazole, some sulfanilamide drugs; resorcinol; aminosalicylic acid); iodine (excess amount) contained in medications(amiodarone 75 mg / ma6l; Lugol's solution 6.3 mg / drop; iodine tincture 40 mg / ml; radiopaque substances repografin mg / ml; iodized oil 380 mg / ml); phenol derivatives used in agriculture as an insecticide, herbicide; dihydroxypyridines found in cigarette smoke; lithium (goitrogenic effect depends on the content of protein and iodine in the diet); genetic defects in the biosynthesis of thyroid hormones (when deiodination is disturbed, a large amount of monoidiodotyrosines enters the bloodstream, which are secreted by the kidneys, as a result of which iodine recirculation is disturbed); diseases of the gastrointestinal tract with changes in absorption processes; humic substances that disrupt the absorption of iodine. An imbalance in trace minerals can exacerbate the clinical manifestations of ID. Deficiency of zinc, manganese, selenium, molybdenum, cobalt, copper and excess calcium play a significant role in the formation of iodine-11
12 cystic goiter and are mediated through disturbances in the formation and activity of coenzymes, enzymes, vitamins and other biologically active compounds. So, in areas endemic for goiter, the lack of copper in soils has a negative effect by reducing the activity of iodinase, which is involved in the addition of iodine to the tyrosyl radical, as well as through a decrease in the activity of cytochrome oxidase, ceruloplasmin. The goitrogenic effect of cobalt deficiency is carried out with insufficient activity of thyroid iodine peroxidase, which leads to a slowdown in the processes of biosynthesis of thyroid hormones. Selenium is involved in the metabolism of thyroid hormones, since it is a component of deiodinases of the selenoenzyme family, which include selenocysteine. The expression of selenium-dependent deiodinases is controlled by selenium in the diet. With a lack of selenium, the activity of deiodinases is inhibited, the level of T4 increases and the concentration of TZ in peripheral tissues decreases, and the manifestations of ID are aggravated. Selenium deficiency aggravates the manifestations of iodine deficiency, causing not only thyroid dysfunction, but also necrotic, fibrotic changes in the thyroid gland, as well as cell proliferation. The impact of negative factors aggravates the manifestations of even a mild degree of ID in children with genetic characteristics of changes in the biosynthesis of thyroid hormones and the functioning of the hypothalamic-pituitary-thyroid system. The role of ID in the development of thyroid pathology in children Insufficient intake of iodine in the child's body causes the development of a compensatory reaction, the formation of goiter. Maintenance of normal secretion of thyroid hormones can be achieved only as a result of rearrangement of the functioning of the thyroid gland. There are several options for adapting to ID. 1. All adaptive reactions are controlled by the activation of the thyrotropic function of the pituitary gland. According to the principle of feedback, the synthesis of TSH is enhanced, which has a stimulating effect on all stages of the biosynthesis of thyroid hormones. With prolonged overproduction of TSH, its strumogenic effect develops: the size of the thyroid gland increases due to hypertrophy and hyperplasia. This is considered as a compensatory reaction of the body to insufficient secretion of thyroid hormones (an increase in their production due to an increase in the number of "working" thyrocytes). But an increase in the level of TSH and / or an increase in the sensitivity of thyrocytes to it is not the only factor in the pathogenesis of iodine deficiency goiter. 12
13 An important role belongs to autocrine growth factors, such as insulin-like growth factor-1 (IGF-1), epidermal growth factor (EGF), main fibroblast growth factor (OFGF), which, in conditions of low iodine content in the thyroid gland, have a stimulating effect on thyrocytes. With ID, the formation of iodolipids of substances, which are the main physiological blockers of the production of autocrine growth factors, decreases. The sensitivity of thyrocyte growth factors to the growth effects of TSH increases, the production of a transforming growth factor, an inhibitor of proliferative processes, decreases. 2. With a lack of iodine, its capture of the thyroid gland increases 4 to 8 times. Enhanced synthesis and metabolism of thyroid hormones contribute to the acceleration of the processes of iodine turnover, which allows the body to manage with smaller amounts of this microelement. 3. The nature of the biosynthesis of thyroid hormones changes. There is a predominant production of the more active hormone T3, while its production requires fewer iodine atoms. 4. Violates the ratio of the concentration of peripheral hormones. Initially, there is a decrease in the biosynthesis of thyroxine with a decrease in the levels of its total and free fraction, the concentration of TZ remains normal or slightly increased, the content of TSH is normal or increased. These hormonal changes are caused not only by the predominant secretion of TZ thyroid gland, but also by an increase in the peripheral conversion of T4 into TZ. 5. Excretion of iodine by the kidneys decreases. Reutilization of endogenous iodine is enhanced, which increases the biosynthesis of thyroid hormones. 6. The content of this microelement in the colloid decreases (due to the predominant synthesis of monoiodotyrosine, and not diiodotyrosine) and thyroglobulin due to increased proteolysis. An early compensatory change in the thyroid gland in conditions of ID is diffuse goiter. Subsequently, due to the active proliferation of a group of cells or follicles, areas or nodes different from the surrounding tissue are formed, so a nodal or many nodular goiter... A node is rarely single. Multiple nodes are found in several segments of the thyroid gland. With prolonged exposure to ID, individual actively dividing thyrocytes are capable of autonomously, outside the regulatory effects of TSH, to produce thyroid hormones. Clinically, this is manifested rarely observed in childhood functional autonomy of the thyroid gland. Functional autonomy can be asymptomatic, with thyroid hormone levels remaining within the normal range. Thyroid scintigraphy reveals areas 13
14 active absorption of the isotopes I31 or Tc99m. Hot knots. This autonomy is called compensated. If the production of T3 and T4 by autonomous formations exceeds the physiological need, then the clinic of thyrotoxicosis develops. This may be due to the natural course of the disease or the intake of an additional amount of iodine with food additives or drugs. Decompensated functional autonomy is clinically manifested as nodular or multinodular toxic goiter... In some cases, autonomy can be diffuse due to the formation of autonomously functioning areas in the entire thyroid gland. Thus, the formation of iodine-deficient thyroid pathology includes several successive stages: diffuse non-toxic goiter; nodular (multinodular) non-toxic goiter; functional autonomy of the thyroid gland; iodine-induced thyrotoxicosis. ID Assessment To assess the severity of ID, the recommendations developed by WHO, UNICEF and the International IDD Control Board are used. The most important indicators characterizing iodine deficiency include thyroid gland size, urinary iodine excretion, serum TSH and thyroglobulin levels. Table 4 presents the epidemiological criteria for assessing the severity of iodine deficiency conditions in the surveyed population. Table 4 Epidemiological criteria for assessing the severity of IDD (WHO, 2001) Criteria Population Severity of IDD group mild moderate severe Goiter frequency (palpation) Schoolchildren 5.0 19.9% 20.0 29.9%> 30.0% Thyroid volume> 97 percentiles Schoolchildren (sonography) 5.0 19.9% 20.0 29.9%> 30.0% Urine iodine concentration Schoolchildren (median, μg / L)<20 Частота уровня ТТГ >5 IU / L Newborns at neonatal screening 3.0 19.9% 20.0 39.9%> 40.0% Urinary iodine excretion is currently considered as the main epidemiological indicator of iodine availability in the region. This criterion is highly sensitive and responds quickly to changes in iodine intake. Therefore, it is used to characterize the epidemiological situation and to monitor pro-14
15 lactics IDD. Table 5 shows the results of the assessment of iodine consumption by the population, based on the median concentration of iodine in the urine of school-age children, Table 5 Criteria for assessing the consumption of iodine by the population Median iodine (μg / l) Iodine consumption Epidemiological situation in the region<20 Недостаточное Тяжелый йодный дефицит Недостаточное Йодный дефицит средней тяжести Недостаточное Йодный дефицит легкой степени Адекватное Нормальная йодная обеспеченность Превышает норму Риск развития йодиндуцированного тиреотоксикоза >300 Excessive Risk of developing adverse health effects (iodine-induced hypothyroidism, autoimmune thyroid diseases) Determination of the frequency of goiter in the population. Changes in the volume of the thyroid gland are associated with the level of iodine intake into the body and occur gradually over several years. The degree of thyroid enlargement is influenced by the severity of ID, the duration of residence in conditions of iodine deficiency, preventive measures, gender, age, etc. At present, the prevalence of goiter as a criterion for assessing iodine supply has practically ceased to be taken into account. This is due to the fact that the main emphasis is shifted towards monitoring the implementation of the universal salt iodization program. The prevalence of goiter is an indirect indicator of the level of iodine consumption and the severity of ID and changes long after the normalization of iodine consumption. Determining the frequency of goiter in a population is of some importance only for assessing the severity of ID, which is carried out before the start of preventive measures. The most appropriate is to study the prevalence of thyroid enlargement in children 8-10 years old. In children under 8 years of age, determining the volume of the thyroid gland presents certain technical difficulties. When examining older children, interpretation of the results is difficult due to differences in the timing of the onset of sexual development and the rate of linear growth. To assess the degree of increase in the size of the thyroid gland by palpation, the classification recommended by the WHO is used (Table 6). The sensitivity and specificity of the palpation method for assessing the degree of goiter is rather low. For accurate determination of the size and volume of the thyroid gland, visualization nodules an ultrasound examination is recommended. 15
16 Classification of goiter (WHO, 1994) Table 6 Grade Thyroid characteristics of goiter 0 No goiter (the volume of each lobe does not exceed the volume distal phalanx thumb of the examined) 1 The goiter is palpable, but not visible in the normal position of the neck. This also includes nodules that do not lead to an increase in the thyroid gland itself 2 The goiter is clearly visible with the normal position of the neck.The total volume of the thyroid gland is calculated by adding the products of the width (W), length (D) and thickness (T) of each lobe with an ellipsoidal correction factor of 0.479: Thyroid volume = [(W D T) right lobe + (W D T) left lobe] 0.479. In children, it is advisable to use thyroid volume standards, calculated relative to the body surface area (BST), which is determined by the nomogram or by the formula: BST = M 0.425 P 0.725 71, where M is the body weight in kg, P is the child's body length in cm. The thyroid gland in children for epidemiological studies was proposed by the WHO and the International Council for the Control of IDD (Table 7). Table 7 Standard indicators of thyroid volume in children for epidemiological studies (upper limit of normal values 97 percentile) (WHO, 2003) Surface area 0.7 0.8 0.9 1.0 1.1 1.2 1.3 1.4 1.5 1.6 bodies (m 2) Boys 2.62 2.95 3.32 3.73 4.2 4.73 5.32 5.98 6.73 7.57 Girls 2.56 2.91 3 , 32 3.79 4.32 4.92 5.61 6.4 7.29 8.32 In the Republic of Belarus, using ultrasound, the thyroid gland volume was studied in healthy children and adolescents (Table 8). Table 8 Volume (cm 3) of palpable thyroid not enlarged in children, depending on gender and age according to ultrasound (V.M.Drozd, O.N. Polyanskaya, 1993) Age, years Girls, X ± Sx Boys, X ± Sx 4 2.56 ± 0.12 2.69 ± 0.15 5 2.76 ± 0.17 2.87 ± 0.20 6 3.09 ± 0.20 2.73 ± 0.27 7 3.41 ± 0.22 3.03 ± 0.21 8 3.83 ± 0.21 3.56 ± 0.18 16
17 End of table. 8 Age, years Girls, X ± Sx Boys, X ± Sx 9 4.22 ± 0.26 4.07 ± 0.43 ± 0.27 4.75 ± 0.76 ± 0.22 5.24 ± 0, 82 ± 0.23 6.02 ± 0.96 ± 0.33 6.45 ± 1.03 ± 0.42 8.08 ± 0.61 ± 0.72 8.31 ± 0.00 ± 0.62 8 , 86 ± 0.41 A formula for calculating the proper volume of the thyroid gland of a particular child, taking into account his age and height is proposed: The proper volume of the thyroid gland = growth K growth / 1 ± 0.25, where K in children years of age 0.04; years 0.03. For adolescents, this formula is inapplicable due to the change in the correlation between thyroid volume and growth. Among other indicators used to assess iodine availability, the definition of TSH is used to screen for congenital hypothyroidism. The threshold TSH level is considered to be 5.0 IU / L in whole blood (or more than 10.0 IU / L in serum). In iodine-deficient areas, the number of newborns with a TSH level of 5.0 honey / l exceeds 3%. Clinical presentation and diagnosis of simple goiter An early clinical sign of chronic ID is a gradual diffuse increase in the size of the thyroid gland. Simple (non-toxic) goiter (endemic diffuse goiter; diffuse goiter associated with iodine deficiency; diffuse non-toxic goiter) is the most common manifestation of ID, which develops as a result of exposure to goitrogenic factors. In childhood, a simple (non-toxic) goiter is most often characterized by a diffuse (uniform and uniform) increase in the thyroid gland without impairing its function (euthyroid state). The term "endemic" goiter implies diffuse or focal thyroid enlargement, which occurs in more than 10% of the population living in the region. The term "sporadic goiter" means goiter observed in residents of non-endemic areas as a result of the action of a combination of environmental factors and / or congenital dyshormonogenesis. From the point of view of the clinician, the distinction between these two terms is problematic due to the coincidence of clinical manifestations and the lack of data on iodine consumption in the patient's region of residence. 17
Therefore, the term “endemic” goiter is recommended for use in epidemiological studies. In clinical practice, it is preferable to use the term "simple (non-toxic)" goiter. The clinical picture of simple (non-toxic) goiter in children mainly depends on the degree of thyroid enlargement. In conditions of mild and moderate ID, a slight increase in the thyroid gland is detected only with a targeted examination of the child. In severe iodine deficiency, the goiter can reach visible sizes or be accompanied by nodulation even with a small thyroid gland. For a long time, patients do not present any complaints. The appearance of the latter depends on the thyroid function of the presence or absence of subclinical or clinical hypothyroidism. At the same time, the child complains of increased fatigue, drowsiness, poor tolerance of normal mental or physical exertion, decreased mood, memory impairment, frequent respiratory diseases, dry skin, unmotivated weight gain, a feeling of chilliness, and constipation. In children, there may be a lag in physical and sexual development. In girls of puberty, the formation of menstrual function is impaired, different types dysfunctions, up to uterine bleeding... Clinical hypothyroidism in children living with prolonged ID of mild or medium severity, is often the result of a chronic autoimmune process in the thyroid gland, manifesting and proceeding against the background of endemic goiter. On palpation examination, there is an increase in the size of the thyroid gland with an elastic, diffuse or heterogeneous surface. With ultrasound of the thyroid gland in case diffuse goiter an increase in the proportions compared with age norm; smoothness of the angle of transition of the isthmus into lobes; the echo structure of the gland tissue can be somewhat heterogeneous, mainly fine-celled or medium-celled; echogenicity is not changed or slightly diffusely reduced; vessels are visualized in the dorsal parts of the lobes, the capsule is hyperechoic and thickened. With colloid goiter, the structure is coarse-celled, resembles many cystic cavities, but unlike true cysts, the accumulation of colloid does not have pronounced walls. Laboratory study of indicators of thyroid function. In clinically euthyroid patients, thyroid hormone parameters are normal or there is a slight increase in st3 with a tendency to decrease in st4 and normal level TSH. In subclinical hypothyroidism, st4 levels are closer to the bottom, and st3 values are closer to the upper limit of normal fluctuations in healthy people, TSH concentrations moderately exceed the upper values in the control. eighteen
19 Hypothyroidism is characterized by low concentrations of st3 and st4, TSH levels are higher than the upper limit of indicators for the test set. TAB of the thyroid gland and cytological examination. Cytological signs of simple (non-toxic) goiter are the presence of a large number of cubic and / or flattened thyroid epithelium cells, the absence of colloid in most cases, and a significant admixture of blood due to abundant thyroid vascularization. With colloid goiter in the punctate there is a large number of homogeneous masses of colloid, the epithelial component is less abundant. In punctate of nodular colloidal goiter, colloid or hemorrhagic fluid with an admixture of fresh or altered erythrocytes, macrophages, dystrophic altered thyrocytes, cells of cubic and squamous thyroid epithelium, lymphoid elements. Scintigraphy with I 131 thyroid gland. There is an increased uptake of I 131. In case of nodular endemic goiter, a "cold" thyroid nodule is revealed on the scan. Treatment of simple goiter in children Children under the age of 6 years with simple (non-toxic) goiter of the 1st and 2nd degrees are prescribed potassium iodide preparations in a daily dose of μg for 6 months. In children from 6 to 18 years old, potassium iodide is used in a daily dose of 200 mcg for 6 months. Before starting monotherapy with potassium iodide and after 6 months of taking the drug, it is recommended to study the levels of TSH, st4 in the blood serum, ultrasound of the thyroid gland. If after 6 months of monotherapy with potassium iodide there is a significant decrease or normalization of the size of the thyroid gland, it is recommended to continue taking iodine preparations in an age-related prophylactic dose in order to prevent recurrence of the disease. If there is no effect in monotherapy with potassium iodide, the treatment regimen includes levothyroxine at a dose of 2.6 3 μg / kg of body weight per day or its combination with μg of iodine per day. The appropriate dose of levothyroxine is adjusted according to the TSH level. After normalization of the size of the thyroid gland, according to the ultrasound performed every 6 months, it is recommended to switch to long-term intake of preventive doses of iodine. 19
20 Endemic cretinism Endemic cretinism and related neurological disorders are the most severe manifestations of IDD in children. Endemic cretinism is characterized by the following features: an epidemiological relationship with severe ID and endemic goiter; the possibility of preventing the epidemic of this serious disease by eliminating iodine deficiency. The incidence of cretinism ranges from 5 to 15% in goiter-endemic areas. There are 2 types of cretinism: neurological and myxedema. Neurological type is the most common and occurs in all regions with severe ID. The myxedema type of cretinism is characteristic only for certain geographical areas (Nepal, East China, Zaire). All patients, regardless of the form of cretinism, have the same spectrum of persistent specific neurological disorders: severe mental retardation, deafness, strabismus, pyramidal and extrapyramidal disorders, motor disorders, changes in the emotional sphere. The nature of neurological disorders is due to intrauterine damage to the nervous system of the fetus in the 1st and 2nd trimesters of pregnancy due to prenatal deficiency of thyroid hormones in the mother and the fetus. Differences in the clinical picture of forms of endemic cretinism are associated with the duration and severity of postnatal hypothyroidism, which determines the severity of myxedema, the degree of growth retardation, skeletal immaturity and delayed puberty. With the neurological variant, patients often lack clear signs of hypothyroidism, the body length corresponds to the child's genetic growth corridor, and there is no lag in bone age. The laboratory determines the normal (closer to the lower limit of the norm of the diagnostic set) serum T4, an increased basal TSH level and an increased TSH response to stimulation with thyroliberin. The neurologic form can be prevented with iodine prophylaxis before pregnancy. The myxedema variant is characterized by severe hypothyroidism (more often against the background of thyroid aplasia), combined with severe growth retardation and puberty. Decompensated hypothyroidism is the cause of high mortality in children with endemic cretinism. In the genesis of myxedema variant of cretinism, in addition to ID, additional factors play a significant role: selenium deficiency, thiocyanate toxicity, autoimmune aggression, etc. Thyroid hormone replacement therapy in endemic cretinism is carried out for life. Its low efficacy in treatment is 20
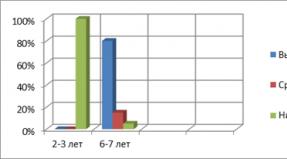
21 is associated with the lack of adequate restoration of the function of the central nervous system and the normal physical and sexual development of the child. Prevention of IDD in IDD risk groups and the resulting lack of thyroid hormones at the stage of intrauterine development and in early childhood lead to serious disorders in the formation and maturation of the child's nervous system. These processes are irreversible and practically not amenable to treatment and rehabilitation. But timely adequate preventive measures can prevent all IDD in children, including those caused by impaired brain development. There are the following types of prevention of chronic ID in the population: mass; group; individual. Mass iodine prevention consists in the use of iodine in the most consumed food products (salt, water, bread, milk, vegetable oil and others) in all regions of goiter endemic without taking into account the degree of iodine deficiency. The main method of preventing IDD in terms of its effectiveness, including economic, is the universal salt iodization carried out in our country. Two chemicals are used for iodization: potassium iodate (KJO3) and potassium iodide (KJ). The iodine content in potassium iodate is 59.5%, in iodide 76.5%. The main advantage of using potassium iodate is its stability, including when heated. Group and individual prevention of chronic ID in the population. At certain periods of life, the human body's need for iodine increases, so there is a need for additional prescription of physiological doses of iodine in the form drugs containing a precisely standardized dose of a trace element. Risk groups requiring individual and group iodine prophylaxis include children under 3 years of age, adolescents, pregnant and lactating women. The recommended daily intake of iodine is presented in table. 2. When carrying out group and individual prophylaxis of ID, potassium iodide preparations are used in tablets of 100 or 200 mcg. With the improvement of control over the use of iodized salt in mass prevention, the group is losing its relevance. Individual prophylaxis consists in recommendations for a specific patient on the use of potassium preparations in age-related dosages or vitamin complexes with a known content of 21
22 iodine in 1 tablet (μg of iodide) or preparations with high concentration iodine (seaweed, sea fish). Prevention of IDD in the prenatal period. Thyroid hormones are of particular importance for the differentiation and maturation of the child's brain, the formation of intelligence. In the early stages of intrauterine life, under the influence of the thyroid hormones of the mother, the anatomical and morphological establishment of the main components of the central nervous system occurs. Until the 1st week of gestation, important cerebral structures of the fetus are formed: the cortex, corpus callosum, subcortical nuclei, striatum, cochlea, eyes, facial skeleton. A deficiency in the synthesis of T4 and T3 in a pregnant woman leads to impaired development of the child's brain, which sharply impairs his future intellectual and motor functions. In the 2nd trimester of pregnancy, the thyroid hormones of the mother and fetal thyroid gland regulate the maturation of neurons in the cerebral cortex and basal ganglia, as a result, the volume of the child's intellectual capabilities is formed. As a result of transient maternal hypothyroxinemia, dysontogenesis of higher mental functions is observed in the developing brain of the child. Such disorders, which occur in conditions of moderate and mild iodine deficiency, are a prerequisite for impaired cognitive functions of the child. Normalization of the endocrine status of a pregnant woman ensures the functional activity of the fetal thyroid gland. The daily intake of potassium iodide at a dose of 200 mcg in the form of pharmacological preparations during pregnancy is sufficient to prevent gestational hypothyroxinemia and damage to the nervous system of the fetus, the formation of goiter in the mother. Prevention of IDD in newborns and infants. After birth, the effect of the child's own hormones on the development of the brain and the formation of cognitive functions is manifested in the process of maturation of the hippocampus and the formation of the cerebellum (during the first year of life), myelinization of the processes of neurocytes (during two years of postnatal development). The reason for the increased sensitivity of newborns to iodine deficiency is the combination of a fairly low iodine content in their thyroid gland with a high level of intrathyroid iodine metabolism. With a decrease in iodine intake to 30% of the optimal level, subclinical hypothyroidism develops, causing irreversible changes in the central nervous system of the newborn. The synthesis of an adequate amount of thyroid hormones and the formation of an iodine depot in a full-term newborn are possible only with the intake of 15 μg of iodine per 1 kg of body weight per day, and in premature infants 30 μg / kg. 22
23 in early age the recommended food for the baby is breast milk. But breast milk ensures the normal development of the baby only if it has a full-fledged balanced composition. It contains not only inorganic iodine, but also thyroid hormones. According to WHO / IAEA standards, the concentration of iodine in the milk of healthy women from iodine-rich regions is μg / l. The content of this trace element in breast milk below 20 μg / l causes a lag in the infant's physical and neuropsychic development. In the vast majority of lactating women who did not receive iodine prophylaxis during pregnancy, the concentration of iodine in colostrum is sharply reduced by the third day after childbirth. Prescribing iodine pharmacological preparations for lactating women is the most effective way prevention of prenatal "debt" for food supply of iodine to the fetus and newborn. For breastfed children, a sufficient intake of this microelement is carried out by the mother's regular intake of pharmacological preparations of iodine (Table 8). In the absence of iodine prophylaxis against the background of lactation, the child needs a daily intake of at least 75 mcg of iodine from birth to 6 months, and then up to 3 years of 100 mcg. For children who do not receive breast milk, the optimal food products are milk formula enriched with this microelement and cereals prepared on their basis. At the same time, the iodine content should be at least 100 μg / l in mixtures for full-term, and twice as much for premature newborns. But these products, due to the reduction in their consumption, starting from the 6th month of a child's life, do not cover the age-related needs and require additional administration of iodine pharmacological preparations (Table 8). Feeding with all other mixtures requires the mandatory use of a potassium iodide drug subsidy. Recently, more than 60 iodine-fortified cereals have been presented on the market. The iodine content in them ranges from 1.4 to 17.5 μg per 100 ml of the finished product. Due to the small amount of food eaten per day, the amount of iodine consumed by the child does not reach the optimal age requirement. From 7 months, the daily amount of iodine supplied to the body with cereals, the most enriched with this microelement, is about 25 μg. Only when feeding children with high-dose iodine products is this amount taken into account when assessing the iodine diet. The rest of the cereals are poor in terms of the iodine component and are not taken into account when analyzing the daily balance of the microelement. Such 23
There is also an approach with respect to the minimum amount of iodine contained in meat / fish purees and iodized bread. A bottle-fed child, depending on the use of a certain milk substitute with low or high iodine content, needs additional introduction of potassium iodide into the diet either from birth or from the second half of life (Table 9). Prescribing drugs to young children containing a standardized dose of potassium iodide makes it possible to effectively replenish the increased needs of the body for iodine. Table 9 Iodine prophylaxis in children of the 1st year of life Nature of feeding Age, breastfeeding months. the mother carrying out iodine prophylaxis of breast milk substitutes (iodine content in 1 liter of the mixture) 200 mcg of potassium iodide does not receive does not contain mcg 90 and> mcg mcg iodine mcg iodine (or mcg mcg iodized cereals) mcg iodine iodine iodine mcg iodine (or mcg 25 mcg iodine and iodinated mcg of iodine iodine porridge) Prevention of IDD in children over one year of age. For children over one year old, iodine prophylaxis remains relevant. The process of formation of the nervous system, which is sensitive to the lack of thyroid hormones, continues, so the child must receive an adequate amount of iodine. Prophylaxis using only iodized salt in young children is unacceptable due to physiological characteristics electrolyte excretory function of the kidneys. To compensate for the deficiency in this group, doses of a trace element are used, taking into account the age-related need in the composition of tableted preparations of potassium iodide or vitamin complexes with a known iodine content in 1 tablet. Prevention of IDD in adolescents. During puberty, the function of the thyroid gland undergoes certain changes caused by the adaptation of the child's body to rapid growth and development. At the beginning of puberty, a physiological increase in TSH levels occurs, followed by an increase in T4 concentration. An increase in thyroid volume is determined by the stimulating effect of TSH and a number of additional factors: increased peripheral conversion of T4 to T3, accelerated excretion of iodine, and increased TSH synthesis. The discrepancy between the increased physiological need for this microelement and its 24
The amount of intake in the body increases the sensitivity of thyrocytes to the stimulating effect of TSH. Potassium iodide preparations are considered the preferred method of preventing IDD. According to the WHO recommendation, children over 12 years old are prescribed the same prophylactic doses as adults 150 mcg per day. Side effects iodine With the prophylactic use of iodine preparations and its use in medicinal purposes in children, the side effects of this microelement, as a rule, are not noted. The development of iodine-induced hyperthyroidism is rare in pediatric practice and can be observed with a daily intake of more than 150 μg of potassium iodide by a child against the background of functional autonomy in the thyroid gland. Acute excess of iodine can have a number of side effects. Ultra-high doses of iodine (over 1 mg per day) can cause the development of iodine-induced hypothyroidism (the Wolf Chaikoff effect). In its genesis lies the violation of the processes of iodine organization. With an acute excess intake of a microelement, the thyroid gland reacts with a decrease in the production of thyroid hormones. The hypothalamic-pituitary-thyroid system, according to the principle of feedback, responds to a decrease in the levels of T4 and T3 by increasing the secretion of TSH, which stimulates the growth of the thyroid gland. Hypersensitivity when taking prophylactic doses of iodine preparations is rare. Clinically, this is manifested by the general serious condition of the child, iodine rhinitis, angioedema, skin reactions, fever, enlargement of the salivary glands. Literature 1. Iodine deficiency diseases in Russia. Simple solution of a complex problem / GA Gerasimov [and others]; ed. G.A. Gerasimova. M., p. 2. Danilova, LI Diseases of the thyroid gland and associated diseases / LI Danilova. Minsk Nagasaki, s. 3. Prevention and treatment of iodine deficiency diseases in high-risk groups / II Dedov [and others]; ed. I. I. Dedov. M., p. 4. Iodine deficiency in Belarus and methods of its correction and prevention: method. recom. / T. V. Mohort [and others]; ed. T.V. Mohort. Minsk, s. 5. WHO, UNICEF and ICCIDD. Assessment of Iodine Deficiency Disorders and Monitoring their elimination. Geneva: WHO / Euro / NUT /,
26 Iodine content in basic foodstuffs Appendix Product name Mkg of iodine per 100 g of product Pasteurized milk 1.8 4.7 Sour cream 7.1 8.6 Butter 2.9 3.1 Chicken egg 14.0 19.7 Drinking water, fortified with iodine 0.2 0.5 Beef 2.7 7.1 Pork 5.5 7.0 Chicken 3.8 4.7 Seafood after cooking Freshwater fish (raw) 243 Freshwater fish (cooked) 74 Fresh herring 66 Herring in sauce 6 Fresh shrimps 190 Fried shrimps 11 Fresh mackerel 100 Raw oysters 60 Oysters (canned) 5 Trout (cooked) 3.5 Black tin bread 9.6 Black 5.6 Rye-table 5.2 Table 4.6 Bread on maple leaves, iodized salt was used for baking 28.9 Wheat bread 2.0 26
27 Table of Contents Abbreviations ... 3 Introduction ... 4 Physiological role of iodine in the child's body ... 4 Secretion and metabolism of thyroid hormones ... 6 Physiological need for iodine ... 8 Definition of IDD ... 9 Etiology of IDD .. .10 The role of ID in the development of thyroid pathology in children ... 12 Assessment of ID ... 14 Clinical presentation and diagnosis of simple goiter ... 17 Treatment of simple goiter in children ... 19 Endemic cretinism ... 19 Prevention of IDD in risk groups. ..21 Side effects of iodine ... 25 Literature ... 25 Appendix
28 Educational publication Solntseva Anzhelika Viktorovna Yakimovich Natalya Ivanovna IODINE DEFICIENCY IN CHILDREN Educational-methodical manual Responsible for the issue A. V. Sukalo In the author's edition Computer typesetting N. M. Fedortsova Proofreader Yu. V. Kiseleva Signed to print. Format 60 84/16. Writing paper "Snow Maiden". Offset printing. "Times" typeface. CONV. print l .. Uch.-ed. l .. Number of copies. Order. Published and printed by Belarusian State Medical University. LI 02330 / from; LP 02330 / from, Minsk, Leningradskaya, 6.28
DEPARTMENT OF HEALTHCARE OF LIPETSK REGION GUZOT "CENTER FOR MEDICAL PREVENTION" INFORMATION BULLETIN "Prevention of iodine deficiency conditions" (for the population) LIPETSK 2017 AGREED Chief Specialist
ALL-RUSSIAN ACTION for the prevention of iodine deficiency diseases "SALT + IODINE: IQ SAVES" According to estimates, more than 20 million people suffer from iodine deficiency diseases in Russia. Iodine deficiency is the cause of 65% of cases
Iodine deficiency diseases: a simple solution to a complex problem Training within the framework of the All-Russian action "Salt + iodine: IQ will save" "Iron" - an organ that consists of secretory cells and produces certain
Chapter 4. Diseases of the thyroid gland How common are diseases of the thyroid gland and why they occur, how and when can a cure be achieved? These are the questions that concern most patients
DEPARTMENT OF ROSPOTREBNADZOR FOR THE ORLOV REGION Iodine, prevention of iodine deficiency conditions in the year 2010 The problem of iodine deficiency is relevant for many countries. More than 1 billion people on Earth live in unfavorable
INFORMATION LETTER FOR DOCTORS OF HMO - YUGRA Laboratory diagnostics of thyroid diseases. One of the reasons for the violation of the biosynthesis of thyroid hormones is the lack or excess of intake
ANALYSIS OF INCIDENCE IN THE POPULATION OF VOLGOGRAD REGION ASSOCIATED WITH MICRONUTRIENT INSUFFICIENCY, WITH THE FIRST TIME IN LIFE DIAGNOSIS ESTABLISHED IN 2012 To analyze the incidence of the population,
PREVENTION AND EFFICIENCY OF IODINE DEFICIENCY CORRECTION IN CHILDREN IM Shulga, I. V. Kataeva, S. M. Bezrodnova Municipal Healthcare Institution City Polyclinic 3 Stavropol State
The value of vitamins and minerals in the diet of a junior schoolchild. Prevention of vitamin deficiency. Vitamins and minerals are compulsory components of a primary school child's diet.
Use of "Iod-Aktiv" in the prevention and treatment of iodine deficiency states With the participation of: Shakhtarin V.V., Tsyb A.F., Parshin V.S. Doroshchenko V.N., Bakanov K.B. Iodine endemic In Russia, 80% of the population is experiencing
Fedorenko E.V., 1 Kolomiets N.D., 2 Mohort T.V., 5 Filonov V.P., 3 Petrenko S.V., 2 Mohort E.G., Belysheva L.L., 4 Shukevich V A., 4 Skuranovich A. L., 4 Zenkovich A. L. IMPLEMENTATION OF THE ELIMINATION STRATEGY
Neonatal screening and the intellectual potential of the younger generation Scientific research in recent years has irrefutably proved the enormous influence of the thyroid gland on the development of the brain and its activity
081 Ecology of security and distribution of endemic a among residents of Jalal-Abad oblast in 2007-2010 Orozbaeva Zh.M. - ZHAGI Deficiency of iodine leads to serious consequences at all stages
From the moment of birth, the girl's body has more than 700 thousand follicles, some of which are maturing. This suggests that the reproductive system of a newborn is different from that of an adult.
Questions and tasks 1. What is the peculiarity of the organization of the autonomic nervous system? 2. What structural features are characteristic of the parasympathetic division of the autonomic nervous system, as opposed to the sympathetic?
INSTITUTE OF INCLUSIVE EDUCATION BSPU Academic discipline "ANATOMY, PHYSIOLOGY AND HUMAN PATHOLOGY" THYROID PATHOLOGY 2018 Skrigan TYPES OF DISTURBANCES OF THE THYROID GLAND Types of pathology
INFLUENCE OF IODINE ON THE INTELLECTUAL DEVELOPMENT OF A CHILD Lysenko A.A. Orenburg State Medical University Orenburg, Russia INFLUENCE OF IODINE ON THE INTELLECTUAL DEVELOPMENT OF THE CHILD Lysenko
Salts in medicine Mineral substances are not only a building material. They are necessary to regulate vital processes: metabolism, digestion, transmission of nerve impulses
TOPIC "Endocrine system" 1. Fluctuations in the sugar content in blood and urine of a person indicate disturbances in the activity of 1) the thyroid gland 2) the pancreas 2. Hormones, in contrast to enzymes
METHODOLOGICAL DEVELOPMENT for students for practical exercises and extracurricular independent work Discipline "CHILDREN'S ENDOCRINOLOGY" Topic: "DISEASES OF THE THYROID GREAS IN CHILDREN". Diffuse non-toxic
Hypothyroidism Hypothyroidism section: Pediatric endocrinology, date: 03/08/2017, author: Klyuchka R.A. Adapted from www.mayoclinic.org Hypothyroidism Hypothyroidism is a disease in which the thyroid gland does not perform
The main task of perinatal obstetrics is the birth of a healthy child. Due to serious changes in the health of the population of reproductive age, the development of a number of deficiency conditions (immunodeficiency,
MINISTRY OF HEALTH OF THE REPUBLIC OF BELARUS APPROVED First Deputy Minister of Health July 2, 2004 Registration 29 0304 V.V. Kolbanov ALGORITHM FOR EXAMINATION OF PERSONS EXPECTED TO RADIATION
28 Diseases of the thyroid gland during pregnancy and in postpartum period Z.M. Dubossary Department of Obstetrics, Gynecology and Perinatology of the Faculty of Postgraduate Education of the State
THYROID 1. In a typical diffuse toxic goiter, the secretion of thyrotropic hormone: 1) suppressed 2) increased 3) normal 2. The main method for diagnosing structural disorders of the thyroid gland
Periods of childhood - their characteristics and meaning. Simple tests 1) Specify age period, in which the child has a tendency to generalize the infection: a) infant b) neonatal c) preschool
Ministry of Education and Science of the Russian Federation FEDERAL STATE BUDGETARY EDUCATIONAL INSTITUTION OF HIGHER EDUCATION "SARATOV NATIONAL RESEARCH STATE UNIVERSITY
FSAU "National Medical Research Center children's health "of the Ministry of Health of Russia FSBEI DPO" Russian Medical Academy of Continuous vocational education"The Ministry of Health of Russia FGBUN" Federal
Features of the influence of endemic goiter on the indicators of the cardiovascular system and the level of stress. Gridina V.V., Puzyreva N.V. Republican clinical Hospital 1 Izhevsk, Russia Features of influence of
E. G. Kondyurina, V. V. Zelenskaya EXPERIENCE OF APPLICATION OF THE PREPARATION "COMPLIVIT-ACTIVE" IN CHILDREN OF YOUNG SCHOOL AGE Novosibirsk State Medical Academy, Outpatient department 2, DKB 4 Presentation
The provision of micronutrients to the population of the Kurgan region Deputy Head of the Sanitary Supervision Department of the Rospotrebnadzor Directorate for the Kurgan Region Sergeecheva N.S. MICRONUTRIENTS: vitamins
Chapter II. Neuro-humoral regulation physiological functions Topic: Endocrine glands Objectives: To study the types and functions of endocrine glands Pimenov A.V. Hormones of the hypothalamus and pituitary gland Features
I. S. Sidorova, I. O. Makarov, E. I. Borovkova PREGNANCY AND ENDOCRINE PATHOLOGY
Thyroid disease and pregnancy 1 Iodine deficiency diseases (IDD) According to WHO, IDD is the most common noncommunicable human diseases
Kyrgyz-Russian Slavic University Kyrgyz State Medical Institute for Retraining and Advanced Studies. Diabetic and Endocrinological Association of Kyrgyzstan Diseases
Underweight: ways to increase Inadequate nutrition Low nutrition Normal weight 18-25 years old BMI less than 18.5 BMI 18.5 19.4 BMI 19.5-22.9 26-45 years old BMI less than 19.0 BMI 19.0 19, 9 BMI 20.0-25.9 Reasons
Diagnosis of congenital hypothyroidism The diagnosis of congenital hypothyroidism must be established as early as possible. The first examination of children with congenital hypothyroidism established according to the survey data
MINISTRY OF HEALTH OF THE REPUBLIC OF BELARUS APPROVED First Deputy Minister D.L. Pinevich March 16, 2011 Registration 182-1110 PRIMARY PREVENTION OF THE MOST COMMON CONNECTED FAULTS
The vitamins and minerals you are missing. Part 2 No deficiency of nutrients! Getting enough vitamins and minerals for the body is very important. But not everyone succeeds in this. How
Chapter II. Nervous-humoral regulation of physiological functions At home: 6-13, test Topic: Violations neurohumoral regulation Tasks: To characterize the diseases that develop with hyper- and hypofunction
* Replenishes vitamin deficiencies * Increases the body's resistance to infections * Participates in the synthesis of acetylcholine * Participates in the regulation of redox processes * Takes part in
VSP_3_2008_BLOK_COLL.qxd 17.06.2008 12:25 Page 66 Lecture by E.A. Troshina, N.M. Platonov Endocrinological science Center, Moscow Iodine metabolism and prevention of iodine deficiency diseases in children and adolescents
Biology Test Role and Function endocrine system Grade 8 Option 1 1. Where do the hormones produced by the endocrine glands go directly? A. Into the intestine B. Into the tissue fluid B. C
New aspects of the use of cytoprotectors and statins in the treatment of autoimmune thyroiditis Associate Professor, Ph.D. V.V. Shevchuk AIT autoimmune disease thyroid, the most common reason hypothyroidism (Endocrinology:
OSTEOPOROSIS is a multifactorial metabolic disease characterized by a decrease in mass and a violation of the structure of bone tissue, manifested by a loss of mineral density and an increase in fragility
ESTIMATION OF THE EFFICIENCY OF PHARMACOLOGICAL PREVENTION OF COMPLICATIONS IN PATIENTS OPERATED FOR NODULAR COLLOID GOITER Oleneva IN, Likstanov MI, Zinchuk S.F. City clinical hospital 3 named.
MINISTRY OF HEALTH OF THE REPUBLIC OF BELARUS APPROVED First Deputy Minister of Health February 3, 2005 Registration 72 0804 V.V. Kolbanov ASSESSMENT OF THYROID STATUS IN PATIENTS WITH CHRONIC
Everything you need to know about vitamins and minerals. Part 2 More about minerals. In the first part of the article, we looked at the chemical compounds responsible for many of the body's functions vitamins. This time
MINISTRY OF HEALTH OF THE REPUBLIC OF BELARUS APPROVED First Deputy Minister D.L. Pinevich 6.2.206 Registration 097-6 METHOD FOR ASSESSING THE RISK OF DEVELOPMENT OF THYROID CARCINOMA IN CHILDREN IN LATE
Letter of the Ministry of Education of the Russian Federation dated September 5, 2003 27/3071 6 The Ministry of Education of Russia sends for information and use in work an information letter of the Ministry of Health of Russia dated 23.06.03
Different products are needed, different dishes are important Educational program "Proper nutrition" Grade 6 Gribenyuk G.V. Proper nutrition When it comes to proper nutrition, it is often said that in some foods
Organization of food The basic principles of organizing a balanced diet remain relevant for people of all ages. Let's call them: 1. Adequate energy value of the diet, corresponding
ON. KURMACHEVA, MD, DSc, Department of Prevention of Diseases of the Human Reproductive System with the Educational and Methodological Center for Reproductive Medicine, State Institution "Saratov Regional Center for Family Planning and Reproduction"
Federal State Budgetary Educational Institution higher education“First Saint Petersburg State Medical University named after I.P. Pavlova "of the Ministry of Health
May 25 World Thyroid Day The thyroid gland (thyroid) is the largest in the human endocrine system. The main function of the thyroid gland is the production of thyroid hormones. Thyroid hormones stimulate
Tests for radiological diagnosis of the endocrine system PRELIMINARY DIAGNOSIS: retrosternal goiter. Ultrasound: the thyroid gland is not detected. RIA: Т3-5.8 nmol / l, Т4-183 nmol / l. Choose the best research method
In most regions of Russia, the natural environment contains an insufficient amount of iodine. At the same time, it is known that iodine is a necessary component for the synthesis of thyroid hormones. Consequently, iodine deficiency in the natural environment leads to a decrease in the synthesis of thyroid hormones (TG), that is, it is the cause of a decrease in the functional activity of the thyroid gland.
It is noteworthy that the compensatory capabilities of the thyroid gland in restoring organ function under conditions of iodine deficiency are unusually large, which allows it to successfully adapt to conditions of mild iodine deficiency. In this case, the thyroid gland only slightly increases in size, and the function of the organ practically does not suffer. In conditions of pronounced iodine deficiency, as well as in the presence of other strumogenic factors that enhance the effect of iodine deficiency, compensatory mechanisms, including an increase in the size of the gland, are not able to completely eliminate the adverse effects of environmental factors. In this case, the patient develops a chronic deficiency of TGs, which are very important for a person's life. This circumstance is the reason for the formation of a whole series of so-called iodine deficiency diseases (IDD), adversely affecting the health and intellectual level of the population experiencing a lack of iodine. The IDZ spectrum is presented in.
Thyroid hormones have a wide range of action. Their role is important in the life of a person of any age, but the role of thyroid hormones in the period of intrauterine and early postnatal life is especially great. Most important action TG in childhood is anabolic. Unlike other anabolic hormones, TGs not only and even not so much control linear growth, but regulate the processes of tissue differentiation. It is under the influence of TG that children not only grow, but also mature and mature. During the period of intrauterine life, under the control of TG, the processes of embryogenesis are carried out, practically all organs and systems differentiate and mature.
The exclusive effect of TGs is on the formation and maturation of the brain. No other hormones have a similar effect. In the early stages of intrauterine life, under the influence of thyroid hormones, the basic functions of the brain are laid and formed. The timing of brain differentiation is clearly limited in time. Deficiency of TG at any of these stages leads to the fact that the brain stops in development, undergoes degenerative changes.
It is known that the unborn child's own thyroid gland begins to function only from the 12th week of intrauterine life. However, even in the early stages of pregnancy (1st trimester), the need for thyroid hormones is quite high, since at this stage of development, the processes of embryogenesis are carried out. This fact indicates that mothers' TGs overcome the fetoplacental barrier and take an active part in the development of the fetus, and above all in the formation of the brain.
Later, in the 2nd trimester of intrauterine life, the fetus develops under the influence of the combined action of the mother's TG and her own hormones. This stage is extremely critical in terms of the formation of brain function. It is during this period that neurons of the cerebral cortex and basal ganglia differentiate and migrate, thus forming the volume of human intellectual capabilities. At the same stage, with the obligatory participation of TG, the cochlea differentiates and, therefore, hearing is formed. It is believed that TG deficiency during these periods (the beginning of the 2nd trimester) is the cause of the appearance of neurological symptoms characteristic of endemic cretinism.
The 3rd trimester of intrauterine life is characterized by a fairly high level of TG. During these periods of development, the thyroid gland of the fetus is actively functioning. It is at the end of pregnancy and the first weeks of postnatal life, with the direct and obligatory participation of TG, the process of myelination of nerve fibers occurs, the cerebral cortex finally differentiates, a person acquires the ability for associative and abstract thinking.
Therefore, the normal functioning of the thyroid gland in women during pregnancy and breastfeeding is important condition the birth of a healthy child and his normal development (primarily intellectual) in the future. In conditions of TG deficiency in the mother and fetus, the risk of giving birth to a defective child is significantly increased.
Most frequent manifestation deficiency of iodine in the environment is the presence of goiter endemic. A goiter in conditions of iodine deficiency is formed in a person at any age, most often at puberty.
In Russia, there have always been foci of endemic goiter. However, despite its widespread prevalence, endemic goiter in previous years did not have a significant negative effect on the growth, development and health of children in Russia.
Currently, the situation in the country has changed for the worse. The number of regions endemic for goiter has increased significantly. And in regions traditionally endemic for goiter, the intensity of goiter endemic is growing: an increasing number of children, and especially adolescents, have an increase in the size of the thyroid gland, pronounced forms of goiter, nodular goiter, thyroid cancer, and autoimmune thyroiditis have become more common.
There are three reasons for this. The first is that in recent years (more precisely, over the past 20 years), the country has eliminated the system that ensures iodine prophylaxis. The second reason is insufficient consumption of products containing iodine: meat, milk, sea fish. The third reason for the increase in the intensity of the thymus endemic is the deterioration of the ecological situation in the country. It is known that many environmental factors (in addition to iodine deficiency) in ecologically unfavorable regions contribute to the deterioration of the functional activity of the thyroid gland and, therefore, have a goitrogenic effect. Consequently, the deterioration of the ecological situation, as it were, enhances the effect of iodine deficiency and, thus, creates conditions for the growth of the intensity of goiter endemic.
The combined influence of these factors is often so significant that a compensatory, sometimes even significant increase in the size of the thyroid gland is not able to normalize its function. At the same time, manifestations of hypothyroidism are gradually increasing, although clinically pronounced forms of the disease are extremely rare in childhood and adolescence. At the same time, hormonal examination in more than half of children and adolescents with an enlarged thyroid gland reveals signs of the so-called subclinical hypothyroidism: there is a tendency to decrease or low level T4, normal or slightly elevated T3 values and increased TSH levels.
On a superficial examination, patients with subclinical hypothyroidism appear to be healthy children. However, when conducting large population studies, it is possible to identify a difference in the health status of children, and especially adolescents, with an enlarged and normal size of the thyroid gland. At the same time, it is noteworthy that children with goiter have the worst indicators of physical and sexual development, they study worse at school, their state of health is worse in many respects: they get sick more often and harder, more often have chronic diseases, changes in the cardiovascular system , blood counts, etc.
In older patients with endemic goiter, signs of subclinical, and in regions of pronounced iodine deficiency, clinical hypothyroidism can also be detected. The greatest danger of iodine deficiency for this category of persons is due to the threat of early development of atherosclerotic manifestations and cardiovascular disorders.
In women of childbearing age living in iodine-deficient regions, the symptoms of reproductive dysfunction come to the fore. This is the reason for frequent infertility or spontaneous abortions. In the case of pregnancy, the children of these women have poor Apgar scores, they often have congenital malformations, children do not adapt well in the neonatal period, often die in early infancy, and have difficulties in school.
Noteworthy is the high incidence of congenital hypothyroidism in children whose mothers live in iodine-deficient regions. The frequency of this pathology in regions with sufficient level iodine averages 1: 4000 newborns. In regions with severe iodine deficiency, the incidence of congenital hypothyroidism, according to screening data, can reach 9-11%. In older children, this pathology in the same area is much less common. This indicates that, firstly, children with congenital hypothyroidism often die at an early age, and secondly, the percentage of transient hypothyroidism is very high in iodine-deficient regions. The duration of this form of hypothyroidism in most cases is several weeks, much less often - several months after birth. However, this form of hypothyroidism is dangerous, as it leads to damage to the child's cerebral cortex. In transient hypothyroidism, TG deficiency occurs at the end of pregnancy and in the first weeks of postnatal life, i.e., precisely in that crucial period of the formation of the central nervous system, when the cerebral cortex is actively maturing. Subsequently, the function of the thyroid gland is restored, but violations of intellectual development remain for life.
The most severe iodine deficiency disease is endemic cretinism. Currently, there is no doubt about the fact that iodine deficiency is closely related to the formation of endemic cretinism. The only way to prevent the birth of such children is the introduction of adequate amounts of iodine before pregnancy, in extreme cases from the first weeks of pregnancy, that is, a well-established system of iodine prophylaxis is needed.
The pathogenesis of endemic cretinism at the present level of our knowledge can be represented as follows. A pronounced iodine deficiency in the region is the reason for a decrease in the functional activity of the thyroid gland of a pregnant woman, which leads to a decrease in the level of TG in the fetus during the extremely crucial period of intrauterine development - during the formation of the brain. Clinical signs of endemic cretinism are: a characteristic face, pronounced impaired intellectual development, deaf-dumbness (impaired formation of the cochlea), spastic rigidity of the extremities (mostly of the proximal lower extremities), gait disturbance, oculomotor disorders, thyroid pathology. It can be goiter with subclinical hypothyroidism or hypoplasia of the thyroid gland with clinical hypothyroidism.
It is noteworthy that in many children living in iodine-deficient regions and not having the classic signs of endemic cretinism, the intellectual level of development is still at a lower level than in children from regions with a sufficient level of iodine. On a cursory examination, they give the impression of being quite healthy children. However, a careful examination reveals some mental retardation and minimal motor impairment. Children study with difficulty in school, perform poorly on psychomotor tests, with a special neurological examination, they reveal a slight spasm and stiffness of the muscles of the proximal extremities, among them children with hearing and speech impairments are more common. In the future, these patients cannot master a complex profession. In regions with severe iodine deficiency, patients with mild psychomotor disorders can make up a significant segment of the population. This circumstance can have a significant bad influence on the social and economic development of the region.
There is no doubt that these disorders are closely related to iodine deficiency. So, in regions with a sufficient level of iodine, such children are practically not found. In iodine-deficient regions, there was a significant difference in the psychomotor development of children born to mothers receiving iodine throughout pregnancy, compared with children from mothers who did not carry out iodine prophylaxis.
So, iodine deficiency worsens the health of the population in the regions of goiter endemic. In this regard, the most urgent issue at the present time is the organization of preventive measures in such regions, which allow increasing the consumption of iodine by the population to the physiological level (). For this purpose, mass (blind), group and individual iodine prophylaxis is carried out.
Mass iodine prophylaxis involves the sale of iodized salt. Daily use of such salt in the usual amounts for the patient (5-10 g) allows you to receive 150-200 mcg of iodine per day. On the way to actively introducing mass iodine prophylaxis, at least two tasks must be solved: 1) uninterrupted supply of iodine-deficient regions with good quality iodized salt and 2) wide awareness of the population of these regions about the need to use only iodized salt in the household.
During iodine prophylaxis, population groups with the highest risk of developing IDD and the most severe consequences of iodine deficiency should be under special control: women of childbearing age, pregnant and lactating women, children and adolescents. For these population groups, group iodine prophylaxis should be organized, involving controlled intake of drugs containing iodine (potassium iodide 200). For the period when the process of organizing mass and group prevention has not yet been completed in an iodine-deficient region, it is necessary to ensure that people are aware of the need for daily intake of iodine-containing preparations, that is, of the need for individual iodine prophylaxis.
So, every person living in iodine-deficient regions and having a normal size of the thyroid gland should carry out iodine prophylaxis, and a patient with an enlarged thyroid gland should treat endemic goiter with preparations containing iodine or thyroxine. However, when deciding on the nature of goiter therapy, it should be remembered that in iodine-deficient regions, especially in cases where the region is environmentally polluted, in addition to endemic (iodine-deficient) goiter, autoimmune thyroiditis (AIT) can form. At the initial stages, AIT is characterized by the same clinical signs, as endemic goiter: diffuse increase in the size of the thyroid gland and clinically euthyroid state. Therefore, before starting therapy, in order to determine the tactics of goiter treatment, it is necessary to carry out a differential diagnosis of endemic goiter and AIT. This requirement is due to the fact that only thyroxine is used in the treatment of AIT - iodine preparations are absolutely ineffective in this disease, and it is possible that they can enhance the processes of autoaggression to the thyroid gland.
The expediency of differential diagnosis of these conditions is also due to the fact that in ecologically unfavorable regions (large industrial cities) the share of AIT in the structure of goiter endemic can reach very high numbers. At the same time, the diagnosis of AIT in childhood and adolescence presents certain difficulties. Due to the short duration of the AIT disease, most children and adolescents lack the classic signs of the disease characteristic of AIT in adults: a typical echographic picture and a high level of specific antibodies in the blood. So, according to our data, a typical echographic picture obtained using ultrasound was only in 21% of children and adolescents with a verified diagnosis of AIT (which was confirmed by cytomorphological examination of thyroid punctate), and specific antibodies in a high titer were detected only in 50% of them. Consequently, the absence of these signs in children and adolescents with goiter does not exclude the diagnosis of AIT and requires a fine-needle puncture biopsy of the thyroid gland with cytomorphological examination of the punctate. If AIT is excluded in a patient with goiter living in an iodine-deficient region, a diagnosis of endemic (iodine-deficient) goiter is established and treatment is prescribed. For a long time, the question of the principles of treatment of endemic goiter was controversial: what to prescribe - preparations containing iodine, or thyroxine. Today it has been established that in addition to iodine deficiency in the genesis of endemic goiter, the role of other strumogenic factors is also great. This allows us to reconcile the supporters of the treatment of this disease with iodine and thyroxine preparations and come to a single agreed decision. The consensus on the prevention and treatment of endemic goiter was developed by an expert group (E.P. Kasatkina, V.A. P. Andreichenko, N. Yu. Sviridenko, M. V. Veldanova) and was adopted at a meeting of chief pediatric endocrinologists of the RF subjects in 1999. The essence of the agreed decision is that when a diagnosis of endemic goiter is established, treatment is always started with the appointment of iodine. At the same time, practically physiological doses of iodine (150-200 μg / day) are used in children and adolescents. This therapy in the presence of iodine-deficient goiter is, of course, more pathogenetically justified, since it contributes, in the conditions of an adequate amount of iodine entering the thyroid gland, to the restoration of its function, normalization of the TG level and, consequently, the normalization of the size of the organ. However, in cases where, in addition to iodine deficiency, other strumogenic factors play a significant role in the genesis of goiter, iodine preparations are not able to restore the function of the thyroid gland and normalize its size. Therefore, if, against the background of treatment with iodine preparations, the thyroid gland for 6 months. does not normalize in size or does not have a clear tendency to normalize, then it is necessary to start treatment with thyroxine. According to most researchers, during treatment with iodine-containing drugs, the normalization of the size of the thyroid gland within 6-9 months. occurs in 50-65% of children and adolescents. In other patients, the thyroid gland remains the same size or even enlarges. It is these patients who need treatment with thyroxine.
To achieve the maximum effectiveness of treatment, it is very important to establish the dose of thyroxine. The initial dose of the drug for the treatment of endemic goiter is 2.6-3.0 mcg / day. Then, under the control of the level of TSH in the blood, an adequate dose is selected for long-term treatment. It is at these doses of the drug that a rapid therapeutic effect is noted: in some patients (with a short life span and small goiter), the thyroid gland normalizes within the next 6 months. treatment, sometimes (large, long-term goiter) requires a longer treatment (up to two years). In case of unsatisfactory results of treatment, it is necessary to check the adequacy of the dose of the drug.
When the normal size of the thyroid gland is reached, regardless of the type of treatment, the patient, if he continues to live in an iodine-deficient region, is transferred to the prophylactic intake of iodine-containing drugs. In those cases when a relapse of goiter occurs against the background of taking iodine-containing drugs, the patient is transferred to treatment with thyroid drugs, since in the genesis of this goiter, in addition to iodine deficiency, other goitrogenic factors certainly play a leading role.
In conclusion, it should be noted that the main reason for the formation of goiter is iodine deficiency in the natural environment. In this regard, in the regions of goiter endemic, it is necessary first of all to determine the presence and severity of iodine deficiency (the median of ioduria is being investigated) and to start organizing mass and group iodine prophylaxis. Every person living in such a region should be aware of the need to consume only iodized salt, and people who are at increased risk of iodine deficiency diseases should use iodine-containing preparations every day.
| Any age | Goiter Subclinical hypothyroidism |
| Women of childbearing age | Infertility or miscarriage of pregnancy Severe pregnancy Anemia |
| Fetus Newborn | High perinatal and infant mortality Congenital malformations Congenital hypothyroidism Cretinism |
| Kids Teens | Delayed physical development Decreased physical and intellectual ability Difficulty learning at school High level morbidity Propensity to chronic diseases In adolescent girls, impaired formation of the reproductive system |
| Adults and Seniors | Decreased physical and intellectual performance Acceleration of atherosclerosis |
For citation: Fadeev V.V. Iodine deficiency diseases // BC. 2006. No. 4. P. 263
Iodine belongs to vital micronutrients: the daily requirement for it, depending on age, ranges from 100 to 200 μg (1 μg is 1 millionth of a gram), and over a lifetime a person consumes about 3-5 grams of iodine, which is equivalent to the content of about one teaspoon. The special biological significance of iodine lies in the fact that it is an integral part of the molecules of thyroid hormones: thyroxine (T4), which contains 4 iodine atoms, and triiodothyronine (T3), which contains 3 iodine atoms. For the formation of the required amount of hormones, a sufficient intake of iodine into the body is also required. With insufficient intake of iodine in the body, iodine deficiency diseases (IDD) develop. Contrary to popular beliefs, enlargement of the thyroid gland (that is, goiter) is far from the only and, moreover, a fairly harmless and relatively easily treatable consequence of iodine deficiency.
Iodine deficiency diseases (IDD), as defined by WHO, are all pathological conditions that develop in a population as a result of iodine deficiency, which can be prevented by normalizing iodine intake. IDD develops in a population when iodine intake falls below recommended levels and is a natural ecological phenomenon that occurs in many regions of the world.
Lack of iodine intake into the body leads to the deployment of a chain of sequential adaptive processes aimed at maintaining the normal synthesis and secretion of thyroid hormones. But if the deficiency of these hormones persists for a long time, then there is a breakdown of adaptation mechanisms with the subsequent development of IDD. This term was introduced by WHO, which thereby emphasizes the fact that thyroid diseases are far from the only and not the most severe consequence of iodine deficiency (Table 1).
IDD is a serious health problem in many regions of the world. According to the World Health Organization (WHO), 1570 million people (30% of the world's population) are at risk of developing IDD, including more than 500 million people living in regions with severe iodine deficiency and a high prevalence of endemic goiter. About 20 million people have mental retardation due to iodine deficiency.
Iodine deficiency diseases of the thyroid gland
Iodine deficiency hypothyroidism
The most severe consequence of severe iodine deficiency is iodine deficiency hypothyroidism. Hypothyroidism is indicated by clinical syndrome caused by a deficiency of thyroid hormones in the body. It is important to consider here that iodine deficiency hypothyroidism in the true understanding of the meaning of this term, with all its inherent phenomena (increased TSH levels) in adults can develop only with a sufficiently long and extremely severe (less than 20-25 μg per day) iodine deficiency in the diet. In the absence of any congenital thyroid enzymopathies in conditions of mild and even moderate iodine deficiency, the likelihood of developing hypothyroidism due to iodine deficiency is low. The main causes of primary hypothyroidism in regions with mild and moderate iodine deficiency are autoimmune thyroiditis and the consequences of surgery on the thyroid gland.
An important point follows from this: IDD is not always associated with the development of hypothyroidism, and these two concepts should not be confused. As will be shown below, a significant problem for regions with mild and moderate iodine deficiency is not hypothyroidism, but a high incidence of thyrotoxicosis in the older age group, due to the formation of functional autonomy of the thyroid gland (Table 2).
In newborns (due to a significantly higher level of thyroid hormone metabolism than in adults), moderate and mild iodine deficiency, leading to a decrease in the content of this trace element in the thyroid gland, can cause the development of the so-called transient neonatal hyperthyrotropinemia (a temporary increase in the level of TSH). This phenomenon can be detected during neonatal screening for congenital hypothyroidism, and its prevalence is considered as one of the indicators of the severity of iodine deficiency in the population.
Diffuse euthyroid goiter
Diffuse non-toxic goiter (DNZ) is the most famous disease, the prevalence of which in the past was considered as the main marker of the intensity of iodine deficiency. DNZ is a general (diffuse) enlargement of the thyroid gland (goiter) without impairing its function. There are many etiological factors of DND, but the most common cause (more than 95% of cases) is iodine deficiency.
The pathogenesis of an enlarged thyroid gland as a result of iodine deficiency in goiter is rather complicated. In essence, the formation of goiter is a compensatory reaction aimed at maintaining a constant concentration of thyroid hormones in the body in conditions of iodine deficiency. According to modern concepts, the theory of hyperproduction or hypersensitivity of thyrocytes to TSH cannot fully explain the pathogenesis of iodine-deficient goiter. It has been shown that TSH is not the only stimulator of thyrocyte proliferation, and the proliferative and trophic effects of TSH are often mediated by other factors. Over the past 10-15 years, the most popular theory has become that a decrease in the iodine content in the thyroid tissue leads to an increased production of local tissue growth factors. The most significant local growth factors are: type 1 insulin-like growth factor (IRF-1), epidermal growth factor (EGF), basic fibroblast growth factor (FGF), and transforming growth factor b (TRF-b). For example, it has been shown that the growth of isolated thyroid follicles containing a sufficient amount of iodine cannot be stimulated by TSH administration. In addition, it turned out that when blockade of IRF-1 receptors with specific antibodies, TSH is not able to exert trophic effects on thyrocytes.
The clinical picture of DNZ, based on its definition, will depend on the degree of enlargement of the thyroid gland, since there is no talk about any pronounced violation of its function.
The simplest method for diagnosing goiter is palpation of the thyroid gland. What does palpation of the thyroid gland reveal? Firstly, to identify the very presence of a goiter, and secondly, to assess its size (severity), as well as the presence and size of nodules in the thyroid gland. At present, the classification of goiter of the World Health Organization is accepted all over the world (Table 3).
If, on the basis of palpation, the doctor concludes that the patient has an enlarged thyroid gland or palpates nodules in it, the patient is shown a more differentiated study - ultrasound of the thyroid gland. Ultrasound of the thyroid gland allows you to determine its volume, assess the structure of the tissue, detect and determine the size of the nodules. If the volume of the thyroid gland in a woman exceeds 18 ml, she may be diagnosed with a goiter. The same can be said about a man whose gland volume exceeded 25 ml. The standards for the volume of the thyroid gland in children are a subject of debate, while the epidemiological aspects of this problem are mainly discussed, that is, the standards that are used to assess the intensity of iodine deficiency, since it is prepubertal children who are included in these studies. The use of epidemiological standards in clinical practice encounters a number of problems, especially in a situation where ultrasound is performed in the absence of direct indications, that is, in the absence of goiter according to palpation data.
The most optimal and etiotropic method of treating goiter associated with iodine deficiency is the appointment of preparations containing physiological doses of iodine. In accordance with the scheme presented in Figure 1, at the first stage of treatment, the overwhelming majority of children, adolescents and young people (under 40 years of age) are shown the appointment of potassium iodide at a dose of 100-200 μg per day ("Iodine balance", pharmaceutical company Nycomedes). The appointment of Iodine balance leads to a fairly rapid suppression of the hypertrophic component of the goiter (an increase in the size of thyrocytes). The effectiveness of therapy is monitored using ultrasound. If there is no effect after 6-12 months, levothyroxine (L-T4; for example, "Eutirox") can be added to therapy at a dose of 75-150 mcg per day, or a switch to L-T4 monotherapy is carried out.
A significant disadvantage of L-T4 monotherapy is the phenomenon of "recoil" - a relapse of goiter after drug withdrawal. The main advantage of the combined administration of iodine and L-T4 is the faster (compared to iodine monotherapy) achievement of a decrease in the volume of the thyroid gland (due to L-T4) and the leveling of the phenomenon of L-T4 cancellation (goiter recurrence) due to iodine.
Nodular and multinodular euthyroid goiter
Nodular goiter is a collective clinical concept that unites all palpable focal formations in the thyroid gland with different morphological characteristics. In other words, we are talking about a preliminary diagnosis, which, in fact, only states the presence of a certain formation in the thyroid gland. This formation can be:
- nodular colloid proliferating goiter (UKPZ);
- tumors of the thyroid gland (benign and malignant).
How can iodine deficiency contribute to the formation of a nodular (multinodular) colloid proliferating goiter (MCSP)? The fact is that initially in the thyroid gland, thyrocytes are not identical in their proliferative activity. This phenomenon is referred to as thyrocyte microheterogeneity. In other words, some thyrocytes more actively capture iodine, others more actively produce thyroid hormones, others more actively divide, and the fourth have initially low functional and proliferative activity. In conditions of iodine deficiency, the thyroid gland is under the influence of chronic hyperstimulation, the main reason for which is a decrease in the intrathyroid iodine pool. At the first stage, this hyperstimulation leads to a diffuse increase in the entire thyroid gland - a diffuse euthyroid goiter is formed. Indeed, if we consider the prevalence of ECD in a population living in an iodine-deficient region, the latter will be more often detected in young people, and practically only this form of goiter will be found in children.
Due to the fact that iodine deficiency leads to hyperstimulation of the entire thyroid gland, the process of nodulation, as a rule, is not limited to any one area or lobe - as a result, a multinodular goiter is formed. It is important to note that, despite the locality of manifestations (often only one node), the CPVD in a patient living in an iodine-deficient region, in essence, is a disease of the entire organ. This is of great clinical importance. It is this fact that explains the high incidence of postoperative relapses of nodular goiter in the absence of prophylactic therapy with iodine preparations after surgical removal of the nodular formation.
Functional autonomy of the thyroid gland
Functional autonomy (FA) of the thyroid gland is understood as the production of thyroid hormones independent of the regulatory influences of the pituitary gland. Against the background of microheterogeneity of thyrocytes, under conditions of chronic hyperstimulation of the thyroid gland, the cells with the highest proliferative potential gain preferential growth. The active division of these cells leads to the fact that reparative processes begin to lag behind in the genetic apparatus of cells, which leads to the formation of somatic mutations. Mutations leading to the autonomous functioning of thyrocytes are referred to as activating. Among the activating mutations of thyrocytes, the most famous mutation of the TSH receptor, leading to its persistent activation even in the absence of a ligand, as well as a mutation of the a-subunit of the Gs protein of the TSH-cAMP cascade, which also stabilizes it in an active state, is currently the most famous.
Over the years, given the persisting iodine deficiency, the number of autonomously functioning thyrocytes increases. Most often, they are grouped into nodules (monofocal or multifocal form of FA), but in about 20% of cases they are disseminated throughout the thyroid gland. An extreme manifestation of thyroid FA is nodular or, more often, multinodular toxic goiter (MTZ).
It is obvious that the process of development of the thyroid gland FA is significantly extended in time, since all these stages must pass. In this regard, multinodular toxic goiter (as an extreme manifestation of the functional autonomy of the thyroid gland), develops almost exclusively in persons of the older age group (after 60 years).
Many studies have shown that one of the most serious problems of even mild iodine deficiency is the high prevalence of thyrotoxicosis in the older age group. Clinically, this problem is very relevant because in elderly patients, thyrotoxicosis is more difficult to detect, since it has a relatively poor clinical picture.
IDD in the perinatal period
During pregnancy, under the influence of a complex of specific factors, the thyroid gland is significantly stimulated. Such specific factors are the overproduction of chorionic gonadotropin, estrogens and thyroxin-binding globulin (TSH), an increase in renal iodine clearance and a change in the metabolism of thyroid hormones in a pregnant woman in connection with the active functioning of the fetoplacental complex.
What is the physiological meaning of thyroid hyperstimulation in the first half of pregnancy? The laying of the thyroid gland in the fetus occurs at 4-5 weeks of intrauterine development, at 10-12 weeks it acquires the ability to accumulate iodine and synthesize iodothyronines. Only by the 16-17th week, the fetal thyroid gland is fully differentiated and begins to function actively. By this time, the laying and differentiation of the main structures of the central nervous system (CNS) is already taking place. The conclusion is obvious: the formation of the central nervous system in the fetus occurs under the predominant influence of the mother's thyroid hormones. This is precisely the physiological meaning of hyperstimulation of the thyroid gland of a woman in the first half of pregnancy.
For adequate development of the fetal nervous system, the production of mother's thyroid hormones from the earliest stages of pregnancy should increase by 30-50%. Iodine deficiency even before pregnancy forces the woman's thyroid gland to work at the limit of its reserve capacity. A further increase in the need for iodine can lead to relative functional gestational hypothyroxinemia (relative to the expected increase in thyroxine levels in early pregnancy with adequate intake of iodine in the body). Adequate brain development in the neonatal period largely depends on the intracerebral T4 level, which directly correlates with the level of free T4 plasma. With a deficiency of thyroid hormones in the fetus, there is a decrease in the mass of the brain and the content of DNA in it, as well as a number of histological changes.
All of the listed mechanisms of hyperstimulation of the thyroid gland of a pregnant woman are physiological in nature, ensuring the adaptation of the woman's endocrine system to pregnancy, and in the presence of adequate amounts of the main substrate for the synthesis of thyroid hormones - iodine, will not have any adverse consequences. Reduced iodine intake during pregnancy (and even just before it) leads to chronic stimulation of the thyroid gland and the formation of goiter in both the pregnant woman and the fetus.
According to the Belgian researcher D. Glinoer, in a region with moderate iodine deficiency, the volume of the thyroid gland in women by the end of pregnancy increased by 30%, while in 20% of all pregnant women the volume of the thyroid gland was 23-35 ml (the normal volume of the thyroid gland does not exceed 18 ml ). A goiter that develops during pregnancy undergoes only partial regression after childbirth, and pregnancy itself is one of the factors that causes an increased incidence of thyroid diseases in women compared to men.
The most serious iodine deficiency disease, as can be concluded from Table 1, is a violation of the intellectual development of the population living in the region of iodine deficiency. The indicators of mental development of the population (IQ-index) living in such regions are significantly (by 10-15%) lower than those in regions without iodine deficiency. The reason for this, as indicated, is the adverse effect of even a moderate iodine deficiency state during the formation of the central nervous system, primarily in the perinatal period.
Prevention of IDD
According to WHO recommendations, the daily requirement of an adult is 150 mcg of iodine per day. Pregnant women should receive at least 200 mcg of iodine per day (Table 4).
The most effective and cheapest method is mass iodine prophylaxis, which consists in the iodization of table salt. With universal salt iodization, the problem of iodine deficiency can be eliminated globally. WHO and a number of other international organizations regulate universal salt iodization as the main and sufficient method of mass iodine prophylaxis. The effectiveness of universal salt iodization has been demonstrated many times in many countries and regions and has a strong scientific base.
During periods of greatest risk of developing IDD, it is advisable to carry out individual iodine prophylaxis, which implies the intake of physiological doses of potassium iodide. Since the periods of pregnancy and breastfeeding are the most critical in terms of the development of iodine deficiency diseases, pregnant and lactating women are shown more reliable individual iodine prophylaxis. Individual iodine prophylaxis involves daily intake of potassium iodide in a dose of 200 mcg ("Iodine Balance 200").
Pathology name: Iodine Deficiency Disorders (IDD)
ICD-10 code: E00. Congenital iodine deficiency syndrome (00.0 - neurological form, 00.1. - myxedema form, 00.2. - mixed form).
E01. Diseases of the thyroid gland (thyroid gland) associated with iodine deficiency and similar conditions [E01.0. - diffuse (endemic) goiter associated with iodine deficiency; E01.1. - multinodular (endemic) goiter associated with iodine deficiency] E02. Subclinical hypothyroidism due to iodine deficiency.
Brief epidemiological data
According to the WHO, about 2 billion people of the Earth live in conditions of iodine deficiency. Insufficient iodine intake threatens the health of more than 100 million Russians, including threatening the normal physical and mental development of 32.8 million children living in the Russian Federation (Dedov I.I., Melnichenko G.A., Troshina E.A. and others, 2004). Diffuse euthyroid goiter is detected on average in 20% of Russians. The incidence of nodular colloid goiter associated with iodine deficiency in women over 30 in the Russian Federation reaches 30%.
Classification
The spectrum of iodine-deficient pathology in the population is very wide and includes (WHO, 2001):
In the prenatal period - intrauterine death (abortion), stillbirth, congenital anomalies, increased perinatal and infant mortality, neurological cretinism (mental retardation, deafness, strabismus), myxedema cretinism (mental retardation, hypothyroidism, dwarfism), psychomotor disorders;
- in newborns - neonatal hypothyroidism;
- in children and adolescents - disorders of mental and physical development;
- in adults - goiter and its complications, iodine-induced thyrotoxicosis;
- at any age - hypothyroidism, impaired cognitive function, increased absorption of radioactive iodine in nuclear disasters [Dedov II, Melnichenko GA, Fadeev VV, 2000; Gerasimov G.A. et al., 2002; Melnichenko G.A. et al., 2005].
In this section, we look at iodine prophylaxis and management of women with diffuse euthyroid and nodular / multinodular colloid goiter during pregnancy. [Melnichenko G.A., Fadeev V.V., Dedov I.I., 2003].
Diagnostics
Treatment
LITERATURE
1. Algorithms for the prevention and treatment of iodine deficiency diseases [Text] / Ed. G.A. Melnichenko. - M .: [b.i.], 2005. - 48 p.
2. Dedov I.I. Endocrinology [Text] / I.I. Dedov, G.A. Melnichenko, V.V. Fadeev. - M .: Medicine, 2000 .-- 632 p.
3. Iodine deficiency diseases in Russia. Simple solution to a complex problem [Text] / G.А. Gerasimov [and others]. - M .: Adamant, 2002 .-- 168 p.
4. Clinical guidelines of the Russian Association of Endocrinologists (RAE) for the diagnosis and treatment of nodular goiter [Text] / I.I. Dedov [et al.] // Clinical thyroidology. - 2004. - Vol. 2, No. 4. - S. 47-52.
5. Melnichenko, G.A. Diseases of the thyroid gland during pregnancy. Diagnostics, treatment, prevention [Text]: a guide for doctors / G.А. Melnichenko, V.V. Fadeev, I.I. Dedov. - M .: MedExpertPress, 2003 .-- 48p.
6. Prevention and treatment of iodine deficiency diseases in high-risk groups [Text] / II Dedov [and others]. - M .: [b.i.], 2004. - 56 p.
7. Modern concepts of clinical endocrinology [Text]. Abstracts of the Fifth Moscow City Congress of Endocrinologists (March 23-24, 2006) / M .: Geos, 2006 .-- 134 p.
8. American Association of Clinical Endocrinologists and Assocazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules. Endocr Pract., 2006 - V. 12, No. 1. - P. 63-102.
Iodine is part of the thyroid hormones, which in turn are involved in the development and normal functioning of the nervous system and intellect, and control the growth and physical development of the child. Thus, the spectrum of health disorders associated with iodine deficiency includes:
- spontaneous miscarriages
- premature birth
- anemia (decreased hemoglobin) in pregnant women
- congenital malformations of the child
- endemic neurological cretinism (mental retardation, deaf and dumbness, spastic diplegia, strabismus)
- endemic myxedema cretinism (growth retardation, mental retardation, psychomotor disorders)
- congenital hypothyroidism (decreased thyroid function)
- high infant mortality
- endemic goiter
- mental retardation
- retardation of physical development
- pathology of sexual development
- hypothyroidism (decreased thyroid function)
- infertility
- faster development
- cognitive impairment
- lack of immunity
- increased incidence of chronic diseases
You need to understand that iodine deficiency is not individual, its presence is established by research results in each specific region. According to research in the Tver region, there is a slight iodine deficiency. But even a mild deficiency of this trace element can lead to the formation of iodine deficiency diseases. Prevention of iodine deficiency states is mainly reduced to an increase in the consumption of iodine by the population in iodine-deficient areas.
Types of prevention
- Mass carried out in iodine-deficient areas by introducing iodine into the most common food products (table salt, bread, milk, infant formula). Iodized table salt is used in the Russian Federation. The population of iodine-deficient regions is recommended to add it to food at 5 g (1 teaspoon without "slide") per person per day. Control over the iodine content in table salt and bread at the stages of production, transportation, storage and sale of the product is carried out by the bodies of sanitary and epidemiological supervision.
- Group iodine prophylaxis- this is the appointment of iodine preparations under the supervision of specialists in groups at greatest risk of developing iodine deficiency diseases (children, adolescents, pregnant and lactating women), especially in organized contingents (kindergartens, schools, boarding schools, etc.).
- Individual iodine prophylaxis includes the use of iodine tablets, providing a physiological amount of this trace element. Potassium iodide preparations are used.
To meet the body's need for iodine, the following doses of iodine are recommended:
- 100 mcg for infants (first 12 months)
- 100 mcg for children younger age(from 2 to 6 years old)
- 120 mcg for school children (7-12 years old)
- 150 mcg for adolescents (12 years and older) and adults
- 200 mcg for pregnant and lactating women
Contraindications to the use of iodine preparations
- increased thyroid function
- toxic adenoma of the thyroid gland, nodular goiter (only under the control of an endocrinologist), except for the period of preoperative iodine therapy
- Dühring's dermatitis herpetiformis
- hypersensitivity to iodine
- pulmonary tuberculosis
- nephritis
- hemorrhagic diathesis
- nephrosis
- furunculosis
- acne
- pyoderma
There is a practice among the people to draw iodine nets on the skin of the neck, and also to take water or lumps of sugar or milk with iodine droplets in order to avoid iodine deficiency. This categorically cannot be done, since such methods can lead to an overdose of iodine and damage to the thyroid gland with provocation of the development of cancer.
If you are in doubt whether it is necessary to give iodine to a child for a preventive purpose, then consult a specialist. And, of course, in no case should iodine deficiency diseases in a child be treated on their own.