Etiology and pathogenesis of neuroinfection. Infectious diseases of the brain: treatment and symptoms. Consequences and prevention
Encephalitis, their mixed forms, differing from each other in manifestations, diagnostic capabilities.
The issue of brain infection in children is especially relevant, since at this age the body is extremely sensitive to various pathogens and can quickly develop. nervous system and the development of severe symptoms. At the same time, several types of such diseases are distinguished: coma, other life-threatening conditions.
The main causes of occurrence
Any neuroinfection is based on the infection of a person, his central nervous system with various microorganisms: bacteria, viruses or fungi. In this case, an infectious process develops, characterized by the development of inflammation and cell damage. In addition, infection can lead to:
- , in particular with the phenomenon prolonged compression structures of the brain;
- prolonged hypothermia;
- the use of non-sterile instruments during surgical procedures on the head;
- a viral infection that can serve as a factor in weakening the immune system.
As a result of the action of such factors, infection of the central nervous system with microorganisms can occur. In this case, there are three main types of damage to the central nervous system:
- Meningitis - characterized by development inflammatory process in the meninges.
- - inflammation and infection are associated with direct damage to the brain tissue.
- Mixed form- elements of meningitis and encephalitis are combined.
Different forms of the disease may differ in their main manifestations, which can be used in the diagnosis of neuroinfection of the brain and in determining the tactics of treatment.
Symptoms of neuroinfections
Symptoms of brain infections have both common features and distinctive features... With meningitis, general cerebral manifestations come to the fore, such as:
- headache sometimes accompanied by vomiting;
- a significant rise in the patient's body temperature up to 39–40 o С;
- stiffness of the back muscles of the neck;
- phenomena of general intoxication with muscle pain, weakness and increased fatigue.
With encephalitis, there are practically no individual neurological symptoms, which makes it possible to distinguish it from meningitis. In the latter case, the symptoms of neuroinfection of the brain are predominantly focal in nature:
- headaches of varying intensity;
- impaired movement or sensitivity in the limbs;
- eye movement disorders, decreased visual acuity or loss of its fields;
- various violations of gait, coordination of movements;
- cognitive impairment (decreased memory, thinking ability);
- temperature rise to 38–39 o C.
In this case, the manifestations of meningitis are characterized by individual neurological defects associated with direct damage as a result of inflammation of specific brain regions.
Diagnostic measures
The most important place in the diagnosis of neuroinfections is occupied by an external examination of the patient with the determination of his neurological status. Already at this stage, the attending physician may suspect the form of the lesion, determine the localization of the pathological process.
 However, to clarify the diagnosis and determine the site of the lesion, laboratory and instrumental methods are used:
However, to clarify the diagnosis and determine the site of the lesion, laboratory and instrumental methods are used:
- Neuroimaging methods: computed and magnetic resonance imaging, allow you to assess the state of the tissue of the central nervous system, meninges.
- Electroencephalography is used to assess the functioning of brain cells and can reveal the extent and severity of nerve tissue damage.
- Electroneuromyography is used to determine the severity of damage to the conducting nerve pathways in the presence of paresis or paralysis in a patient.
- Lumbar puncture followed by analysis cerebrospinal fluid allows you to identify the inflammatory process in the central nervous system, to determine its pathogens (viruses or bacteria).
- Clinical and biochemical analysis blood helps to identify the inflammatory process in the body.
The correct use of the described methods, together with the collection of complaints and the conduct of a neurological examination, makes it possible to make the correct diagnosis and prescribe rational treatment.
Treatment of neuroinfection
The main approach to treatment is etiological. It is necessary to select a drug aimed at combating the causative agent of the disease. For this purpose, either antibacterial agents are used for bacterial lesions, or antiviral agents for viral neuroinfections.
It is very important to start therapy as early as possible: treatment begins with drugs wide range actions, proceeding further on medications to which the identified pathogen is sensitive.
In addition, to improve metabolic processes in neurons (Phenotropil, Piracetam) and antioxidants (Dihydroquercetin, alpha-tocopherol) can be used. Patients are prescribed massive infusion therapy (isotonic solutions, Disol, Trisol), glucocorticosteroids, vasoactive drugs (Cerebrolysin, Cavinton).
It is very important to start rehabilitation measures as early as possible, consisting of the use of:
- medicines (antioxidants, nootropics);
- massage and remedial gymnastics;
- physiotherapy.
Early rehabilitation can improve the prognosis for recovery and reduce residual neurological symptoms. Any medications should be selected by the attending physician in a hospital setting. In no case should you practice self-treatment neuroinfections.
Infectious damage to the central nervous system is a serious disease that leads to the appearance of severe symptoms, possible neurological deficits in the future (paralysis, dementia). If you experience any of the symptoms described above, you must urgently seek medical help in self-referral or call an ambulance. medical care... It is necessary to start therapeutic measures as early as possible.
Bacterial (purulent) meningitis
Etiology
In most cases bacterial meningitis caused by one of the following three microorganisms:
- Neisseria meningitidis(meningococcus)
- Haemophilus influenzae (type B) (rarely observed with initiation of vaccination)
- Streptococcus pneumoniae(Pneumococcus).
Other organisms, especially Mycobacterium tuberculosis, can be found in patients at risk, i.e. with immune deficiency (Table 1).
Table 1. Rare Causes of Bacterial Meningitis in Risk Groups
Epidemiology
In developed countries, meningitis occurs in 5-10 people out of 100,000 per year.
The above three microorganisms have characteristic clinical manifestations:
- meningitis caused by meningococcus can be epidemic
- H. influenzae more often affects children under 5 years of age
- pneumococcal infection more common in older patients and is associated with alcoholism and splenectomy. It can cause meningitis by spreading through the bloodstream from nearby organs (ears, nasopharynx) or from the lungs.
Clinical manifestations
Headache can be associated with stiff neck and back muscles, vomiting, and photophobia. The headache builds up quickly (from minutes to hours), although not as quickly as with subarachnoid hemorrhage. Depression of consciousness and epileptic seizures are possible.
Clinical examination reveals signs of infection, including fever, tachycardia, shock. A number of patients have a primary source of infection (pneumonia, endocarditis, sinusitis, otitis media). Many patients with meningococcal meningitis have petechial eruptions.
Neurological symptoms include:
- meningeal syndrome - a manifestation of irritation of the membranes stiffness of the neck muscles when trying to passively flex it, a high "meningeal" cry in children, Kernig's symptom
- depression of consciousness
- increased intracranial pressure - disc edema optic nerve, tense fontanelle in children
- cranial nerve damage and other focal symptoms.
Examinations and diagnostics
- Lumbar puncture for untreated acute bacterial meningitis reveals:
- clouding of CSF
- high blood pressure
- polymorphonuclear leukocytosis (hundreds or thousands of cells per microliter)
- high protein content (more than 1 g / l)
- a decrease in glucose concentration (less than half of the content in the blood, not always recognized).
The causative agent of meningitis is identified by Gram staining, by cultivation in a special medium, using the polymerase chain reaction.
- Contraindications to lumbar puncture in patients with suspected meningitis: edema of the optic nerve head, depression of consciousness and focal neurological deficit. In these patients, CT is required before puncture to exclude a neoplasm, for example, in the posterior fossa, which can produce a picture similar to meningitis.
- Other examinations:
- detailed clinical blood test (neutrophilia is detected)
- coagulation stages (presence of disseminated intravascular coagulation syndrome)
- electrolyte levels (possible hyponatremia)
- a blood culture to check for microflora (results may be positive even with sterile CSF)
- radiography chest and skull ( paranasal sinuses nose) to identify the primary source of infection.
Complications
Acute complications of meningitis: epileptic seizures, abscess formation, hydrocephalus, excessive secretion of antidiuretic hormone and septic shock.
Severe manifestation septic shock with the development of the syndrome of disseminated intravascular coagulation and hemorrhage in the adrenal glands can be a complication of meningococcal meningitis (Waterhouse-Friederiksen syndrome). Meningococcal meningitis can also be complicated by the development of septic arthritis or immune-mediated arthropathy.
Treatment
- Bacterial meningitis can be fatal within hours, so early diagnosis and intravenous administration high doses of antibiotics.
- Benzylpenicillin- the drug of choice in the treatment of infectious diseases caused by meningococcus or pneumococcus (although a significant number of strains that are insensitive to penicillin appear). The first dose is 2.4 g, subsequent doses (1.2 g) are administered every 2 hours. When clinical improvement occurs within 48-72 hours, the frequency of administration can be reduced to once every 4-6 hours, but with the same the same daily dose (14.4 g). Treatment should be carried out within 7 days after the temperature has returned to normal (14 days for pneumococcal infection).
- With meningitis caused N. Influenzae, high-dose intravenous administration of chloramphenicol, cefotaxime, or ceftriaxone is effective.
- If the nature of the pathogen is unknown, a combination of benzylpenicillin with cefotaxime or ceftriaxone should be used.
- If meningococcal meningitis is suspected, the general practitioner should give the first dose of benzylpenicillin intravenously or intramuscularly and admit the patient.
- If lumbar puncture is delayed prior to CT, antibiotic treatment should be started before neuroimaging, immediately after blood culture is taken.
- Other General requirements to treatment: bed rest, analgesics, antipyretic, anticonvulsant for seizures and supportive measures for coma, shock, increased intracranial pressure, disorders electrolyte balance and circulatory disorders. The early use of corticosteroids along with antibiotics is believed to reduce mortality in bacterial meningitis.
Prophylaxis
- Persons who have been in contact with patients with meningococcal meningitis are shown prophylactic use of rifampicin or ciprofloxacin
- Immunization against infection caused by H. Influenzae, recommended for children aged 2, 3 and 4 months (vaccines H. Influenzae type B); the use of the vaccine significantly reduces the risk of illness.
Forecast
The mortality rate from acute meningitis is about 10%, with most of it from infection with Streptococcus pneumoniae.
Pneumococcal infection causes a large number of complications (up to 30% of patients), including hydrocephalus, cranial nerve damage, optic and movement disorders as well as epilepsy. Children with acute bacterial meningitis can develop behavior disorders, learning difficulties, hearing loss, and epilepsy.
Other bacterial infections
Brain abscess
Etiology
Brain abscess is less common than bacterial meningitis, it can be a complication of otitis media (in particular, abscess of the temporal lobe and cerebellum) and other local infectious processes (for example, with paranasal sinusitis). Its development is also possible with remote foci of inflammation localized in the lungs (bronchiectasis), renal pelvis or heart (bacterial endocarditis and congenital heart disease).
Clinical manifestations
A local accumulation of pus is accompanied by quite expected symptoms of a volumetric effect on the brain:
- increased intracranial pressure
- focal neurological deficit (dysphasia, hemiparesis, ataxia)
- epileptic seizures.
A high temperature is possible, but its appearance is not an obligate sign. Symptoms develop over days, sometimes weeks, and may resemble a brain neoplasm.
Diagnostics
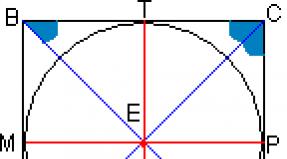
- If an abscess is suspected, CT or MRI is required (Fig. 1).
- Lumbar puncture is contraindicated (risk of wedging).
- A detailed blood test (neutrophilic leukocytosis) and culture to identify microflora.
Rice. 1. MPT, sagittal section. Multicameral abscess of the brain. There is a characteristic decrease in the intensity of the signal in the center and its strengthening along the periphery of the foci after intravenous administration of a contrast agent (gadolinium preparation). The surrounding area of edema is revealed (hypointense shadow)
Treatment
- Neurosurgical intervention It is carried out in order to reduce the compression of the brain and empty the abscess, as well as to establish a bacteriological diagnosis.
- Broad spectrum antibiotics(cefotaxime with metronidazole) are prescribed early and administered before the nature of the microflora is established.
- Corticosteroids(used along with antibiotics) may be needed to combat cerebral edema.
Parameningeal infections
Pus can collect in the epidural space, especially in the spinal canal. The main pathogen is Staphilococcus aureus coming from infected wounds. Possible osteomyelitis of the vertebrae and infection of the intervertebral discs in combination with an epidural abscess. Patients have severe back pain, fever (however, it can be very mild) and rapidly increasing paraparesis. The examination includes an MRI scan of the corresponding section of the spine and blood cultures. Treatment is carried out with antistaphylococcal antibiotics; if there are signs of compression of neural structures, early surgical intervention is indicated.
Local infections in the face and scalp can spread into the subdural space ( subdural empyema) and into the intracranial venous sinuses, causing purulent sinusitis and cortical vein thrombosis.
Tuberculosis
TB meningitis is usually less severe than bacterial meningitis, so clinical diagnosis it is quite difficult to establish. Patients with impairments immune system, ethnic minorities and expats are at risk. The main clinical symptoms are persistent headache, fever, epileptic seizures and focal neurological deficits that develop over several weeks. CSF flows under high blood pressure and contains several hundred leukocytes per microliter (lymphocytes predominate), the protein content is increased, and glucose is reduced. Microorganisms can be detected by Auramine or Ziehl-Nielsen staining, but they are most often undetectable and multiple CSF retests and cultures are required. A valuable diagnostic test is the detection of mycobacterial nucleic acid by polymerase chain reaction. Treatment should not be postponed even if there is a suspicion of the tuberculous nature of the process; isoniazid (with concomitant administration of pyridoxine), rifampicin, pyrazinamide, and a fourth drug, usually ethambutol or streptomycin, are prescribed. Anti-TB treatment should be continued for up to 12 months or more under the supervision of a specialist. Corticosteroids are usually used in combination with anti-TB drugs to suppress inflammation and possible cerebral edema.
Mycobacterium tuberculosis can also cause chronic caseous granulomas ( tuberculomas) which, like intracranial neoplasms, have a volumetric effect on the brain. Tuberculomas can develop as a consequence of transplanted tuberculous meningitis or as an isolated disease. Spinal tuberculosis can cause compression spinal cord(Pott's disease).
Syphilis
Currently, neurosyphilis is relatively rare, mainly in homosexuals. There are several well-defined clinical forms.
- Moderately severe, self-limiting meningitis due to secondary syphilis.
- Meningovascular syphilis: inflammation of the meninges and cerebrospinal arteries in tertiary syphilis, manifested by subacute meningitis with focal neurological deficits in the form of cranial nerve damage, hemiparesis or paraparesis, atrophy of the muscles of the hands ( syphilitic amyotrophy).
- Gumma- focal meningovascular lesion, proceeding as an intracranial neoplasm and clinically manifested by epileptic seizures, focal symptoms, increased intracranial pressure.
- Dorsal tabes (tabes dorsalis)- damage to the posterior roots of the spinal cord (Fig. 2).
- Progressive paralysis- parenchymal brain disease (Fig. 2).
- Congenital neurosyphilis.

Rice. 2.
The diagnosis of neurosyphilis is established with positive serological tests in the blood and CSF. In the CSF, up to 100 lymphocytes / μl, an increased content of protein and oligoclonal proteins can be detected. Treatment includes intramuscular injection of procainepenicillin, 1 million units. per day for 14-21 days. Concomitant administration of corticosteroids at the start of penicillin treatment is recommended to prevent Jarisch-Herzheimer reactions- a severe toxic reaction to the massive death of spirochetes under the influence of an antibiotic.
Lyme disease
Spirochete infection Borrelia burgdorferi transmitted by a tick bite can cause neurological manifestations in combination with systemic manifestations of the disease. In the acute phase, during the first month after the bite, meningism may develop along with fever, rash, and joint pain. Chronic illness develops within a few weeks or months after the bite, is characterized by meningitis, encephalitis, cranial nerve (especially facial) paralysis, damage to the spinal roots and peripheral nerves. Serologic tests confirm the clinical diagnosis. The body is usually sensitive to cefotaxime or ceftriaxone.
Leprosy
Mycobacterium leprae- one of the few microorganisms that invade directly into the peripheral nerves. Patients with "tuberculoid leprosy," milder and less contagious form diseases that suffer from partial sensory neuropathy with palpable thickened nerves and depigmented numb skin areas. This disease is very rare in Europe and North America; worldwide, leprosy is one of the main causes of multifocal neuropathy.
Bacterial toxins
Damage to the nervous system can develop under the influence of toxins produced by some microorganisms.
- Tetanus caused by toxins produced Clostridium tetani falling into the wound. Signs: tonic spasms of the jaw muscles ( lockjaw) and torso ( opisthotonus), fever with painful paroxysmal spasms of the entire musculature and arching of the back and extended limbs. Treatment in the intensive care unit includes the use of muscle relaxants, mechanical ventilation, administration of human tetanus immunoglobulin, penicillin, and wound toilet. This disease can * be eradicated by active immunization of the population.
- Botulism caused by a toxin produced Clostridium botulinum, - a poisonous substance that enters the body when eating poorly sterilized canned foods and, less often, from infected wounds. Patients experience vomiting and diarrhea, followed by paralysis within two days of poisoning. Weakness usually "descends" in its development - first there are ptosis, diplopia and accommodation paralysis, then weakness of the bulvar muscles and muscles of the limbs. Usually required artificial ventilation lungs; recovery is delayed for months and even years.
- Diphtheria the toxin can cause polyneuropathy; Fortunately, with the advent of immunization (vaccination), this condition is very rare in developed countries.
Viral infections
Viral meningitis
Caused by some viruses (mumps virus, enterovirus, etc.), the disease has a benign, self-limiting course, not accompanied by serious complications inherent in acute bacterial meningitis. An increase in CSF pressure and the presence of several hundred leukocytes in a microliter are possible; in most cases, lymphocytes with single neutrophils are detected, with the exception of the early stages of the disease. The protein content may be slightly increased, the glucose level is normal. Differential diagnosis performed with meningism, also a common condition aseptic meningitis, in which sheath symptoms and moderate lymphocytosis in the CSF are possible (Table 2).
Table 2. Differential diagnosis aseptic meningitis
|
Partially healed bacterial meningitis Viral meningitis and meningoencephalitis Tuberculous meningitis Leptospirosis, brucellosis - in risk groups Cerebral malaria Fungal meningitis Parameningeal infection - spinal or intracranial abscess, venous sinus thrombosis, latent infection of the paranasal sinuses Endocarditis Malignant neoplasm with meningeal syndrome - carcinoma, lymphoma, leukemia Subarachnoid hemorrhage Chemical meningitis - a condition after myelography, the use of certain drugs Sarcoidosis Autoimmune disease, vasculitis, Behcet's disease Mollare meningitis is a recurring fever, meningeal syndrome, and CSF lymphocytosis, possibly associated with herpes infection. |
Viral encephalitis
Etiology and pathogenesis
A viral infection of the brain can cause a lymphocytic inflammatory response with necrosis of neurons and glia.
Herpes simplex virus Is the most common cause of sporadic encephalitis. Other viral pathogens: herpes zoster virus, cytomegalovirus and Epstein-Barr virus (herpes viruses often lead to the development of encephalitis in patients with impaired immune system), adenoviruses and mumps virus. Encephalitis can be epidemic in nature as a consequence of arbovirus infection in regions where mosquitoes can carry the disease.
Patients experience headache and depression of consciousness for hours and days, epileptic seizures and focal neurological deficits are possible, which indicates dysfunction of the cerebral hemispheres or the brain stem. Hemispheric symptoms (dysphasia, paraparesis) make it reasonable to assume that encephalitis is caused by the herpes simplex virus.
Diagnostics
- CT and MRI of the brain can exclude a neoplasm and establish the presence of cerebral edema. The characteristic manifestations of herpes simplex virus encephalitis (Fig. 3) can develop over several days.
- CSF pressure is usually increased, lymphocytosis, increased protein content with normal glucose levels are detected. When diagnosing encephalitis caused by the herpes simplex virus, the determination of the titer of viral antibodies can only have a retrospective value. Early diagnosis possible with the help of immunoassay to detect the antigen and using the polymerase chain reaction to detect the DNA of the virus.
- When registering EEG, pronounced diffuse changes... With encephalitis caused by the herpes simplex virus, characteristic feature are periodic beats present in the temporal region.

Rice. 3. Encephalitis caused by the herpes simplex virus. Note the asymmetric decrease in density in the temporal lobes
Treatment
Application acyclovir(10 mg / kg IV every 8 hours for 14 days) revolutionized the treatment of herpes simplex encephalitis, significantly reducing mortality. Death and severe residual events (epilepsy, dysphasia, and amnestic syndrome) still occur, especially with late initiation of treatment. If herpetic encephalitis is suspected, acyclovir should be started immediately, without waiting for the results of CSF analysis, sometimes a brain biopsy is required.
There is no specific treatment for other types of encephalitis; only for encephalitis caused by cyclomegalovirus, use ganciclovir... Patients are prescribed supportive measures and symptomatic treatment, including anticonvulsants for epileptic seizures and administration of dexamethasone or mannitol for increased cerebral edema.
Herpes zoster
The varicella-zoster virus, which is inactive in the dorsal horn of the spinal cord for many years after infection, can reactivate and manifest clinically as herpes zoster. In this case, the patient, as a rule, experiences local pain and burning sensation, which precede the appearance of a characteristic one-sided rash, spreading in the area of one separate dermatome or a number of adjacent dermatomes. In most patients, the rash is located on the trunk. After the rash disappears, pain that does not respond well to treatment ( postherpetic neuralgia).
The virus can cause various diseases:
- Herpes zoster ophthalmic- the rash affects the eye branch trigeminal nerve, which is associated with the risk of corneal damage and the threat of postherpetic neuralgia.
- Ramsey-Hunt Syndrome- with unilateral facial peripheral paralysis of facial muscles and rashes in the external auditory canal or in the oropharynx. Severe pain in the ear canal, systemic dizziness and hearing loss ( ear herpes zoster).
- Motor herpes zoster- muscle weakness, including damage to myotomes at the same level as dermatomes affected by rashes. So, for example, the development of unilateral paresis of the diaphragm with homolateral rashes on the neck and shoulder (dermatomes C3, C4, C5).
Although herpes zoster usually clears up without treatment, oral acyclovir is required at higher doses of acyclovir than is required for treating herpes simplex infection to speed recovery, reduce pain, and reduce the risk of complications.
Herpes infection can have various clinical manifestations, especially in patients with impaired immune system, including generalized rashes and the development of encephalitis. Some patients have selective damage to the spinal cord (herpetic myelitis) or cerebral arteries, causing hemiplegia.
Retroviral infections
Infections in people with HIV can lead to neurological complications for two reasons. First, this virus has an affinity for nerve tissue, i.e. it is neurotropic as well as lymphotropic. Meningitis can occur in the setting of seroconversion. In the future, slowly progressive dementia and involvement of other parts of the nervous system, in particular the spinal cord and peripheral nerves, may develop. Secondly, the risk of accidental infection and unusual infectious lesions of the nervous system may be the result of a compromised immune system in the case of an advanced clinical picture of AIDS.
- Cerebral toxoplasmosis in AIDS patients, it is characterized by lesions of the cerebral hemispheres (hemiparesis, dysphasia, extrapyramidal disorders), cerebellum (ataxia), and cranial nerves. It is often accompanied by headache, epileptic seizures, and on CT and MRI - signs of focal or multifocal encephalitis. Antitoxoplasmosis therapy is performed with pyrimethamine, sulfadiazine, or clindamycin. Brain biopsy is indicated in patients who do not respond to therapy.
- Cryptococcal meningitis- fungus Cryptococcus neoformans; the most common cause of cryptococcal meningitis in AIDS patients. Clinically manifests itself in acute or subacutely growing headaches, fever, and sometimes epileptic seizures, but focal neurological symptoms are rarely detected. CSF analysis (after CT excluding intracranial neoplasm) reveals lymphocytosis, usually with increased content protein and reduced - glucose. Cryptococci can be detected by a sample with specific staining or based on the presence of antigen in the CSF or blood. Combination treatment antifungal agents(amphotericin B or flucytosine) may not be effective. Cryptococcal meningitis can be a complication of other immune system disorders, such as a condition after organ transplantation that requires the use of immunosuppressants.
- Herpesviruses- cytomelagovirus infection; more often in patients with AIDS. Can cause encephalitis and spinal cord injury (myelitis). Other herpes viruses, such as herpes simplex and herpes zoster viruses, can cause localized or diffuse encephalitis.
- Progressive multifocal leukoencephalopathy (PML) It is caused by opportunistic papovaviruses (JC and others) and is manifested by multiple lesions of the white matter of the cerebral hemispheres. The disease proceeds with progressive dementia and focal neurological deficits, such as hemiparesis and dysphasia. Death occurs within months. PML develops in conditions where the immune system is impaired, for example, in diseases of hematopoiesis, tuberculosis, sarcoidosis.
- Cerebral lymphoma- focal or multifocal lesion in the cerebral hemisphere or posterior cranial fossa; has a clear clinical picture, is detected during CT or MRI. In the absence of the effect of the ongoing anti-toxoplasma therapy, the diagnosis can be made with a brain biopsy.
In developed countries, all of these complications have become less common due to the introduction of highly active antiretroviral therapy (HAART or HAART).
Retroviruses other than HIV are also characterized by neurotropic properties. Thus, the HTLV-1 virus, which is widespread in certain regions, for example in the Caribbean, is associated with tropical spastic paraparesis(HTLV-1-associated myelopathy, HAM).
Other viruses
- Polio rare in developed countries due to the introduction of the vaccine. During an epidemic, most patients experience mild illness with headache, fever and vomiting 7-14 days after the virus enters the body through the intestines or Airways... Some patients are in a preparative state, which manifested itself as meningitis, pain in the back and limbs, while the virus was gaining access to the CSF. Due to the tropism to the cells of the anterior horn of the spinal cord and homologous cells of the brain stem, paralytic damage with progressive muscle weakness develops within several days. The clinical symptoms are the same as with damage to the peripheral motor neuron, with the difference that the muscle damage is partial and asymmetric, there are fascicular twitchings on early stages diseases and subsequent atrophy and areflexia. Few patients develop bulbar disorders and respiratory failure. Despite the fact that after the paralytic stage there is a partial recovery, many patients remain with persistent paresis and paralysis and require prolonged mechanical ventilation. Post-polio syndrome is a rather ambiguously characterized condition, since with a late deterioration in the condition of patients with poliomyelitis, the cause of the increase in neurological deficit is the influence of other diseases.
- Rabies eradicated in Great Britain and some other countries, however, it is often found in the world. The disease is usually transmitted through the bite of an infected dog, but can also be transmitted through the bite of other mammals. The virus spreads from the site of the bite to the central nervous system slowly (over several days or weeks) and causes an inflammatory reaction with diagnosed intracytoplasmic inclusions ( corpuscles of Negri) found in neurons after death. If the inflammatory process predominantly affects the brain stem, rabies has a "lightning" course, the disease develops after a period of precursors in the form of fever and mental disorders... Those who are ill experience laryngospasm and fear when drinking water - rabies... If the inflammation mainly affects the spinal cord, there is flaccid paralysis. When symptoms of rabies are established, the outcome of the disease is always fatal. Prophylactic immunization is possible for animals - potential carriers of infection, in addition, active and passive immunization should be undertaken immediately after being bitten by such animals, along with washing and surgical treatment of the wound.
Post-viral phenomena
- Subacute sclerosing panencephalitis- a late and almost always fatal complication of measles, fortunately rare nowadays due to the availability of immunization.
- Acute disseminated encephalomyelitis- a rare continuation of a viral infection.
- Guillain-Barré Syndrome in most patients associated with a prior infection, usually.
- Other neurological and psychiatric symptoms, such as weakness, impaired attention and memory, can complicate the recovery process from viral infections. In particular, Epstein-Barr virus infection is associated with post-viral weakness syndrome.
Other infectious and contagious diseases
Protozoa
- Malaria should be considered in patients with fever unclear genesis returning from areas endemic for the disease. The disease is well diagnosed by blood tests. Infection Plasmodium falciparum causes hemorrhagic encephalitis.
- Toxoplasmosis, mentioned as a cause of multifocal encephalitis in AIDS, can also develop in utero causing hydrocephalus, intracranial calcification and chorioretinitis.
- Trypanosomiasis common in African tropical countries; proceeds as relatively light form encephalitis with excessive sleepiness and epileptic seizures ("sleeping sickness").
Metazoa
The encapsulated tapeworm larva is capable of causing cerebral lesions:
- in the presence of echinococcal cysts the disease can proceed as an intracranial neoplasm, rupture of the cyst can lead to chemical meningitis;
- at cysticrosis numerous cysts lead to epilepsy, increased intracranial pressure, focal or multicentric neurological deficits, or hydrocephalus. Treatment is with praziquantel and steroids.
Infectious lesions of the nervous system are one of the most common forms of neurological pathology, which accounts for at least 42% of all diseases in this area.
The prognosis in most cases is disappointing.
Neuroinfection of the brain is classified depending on the localization of the pathological process, based on which, they are distinguished:
encephalitis(inflammation of the brain tissue due to infection); myelitis(inflammatory process of the spinal cord caused by pathogens); arachnoiditis (infectious inflammation affects the arachnoid meninges); meningitis(infectious inflammation spreads to the lining of the brain).
In addition to the listed types of neuroinfection, combined pathologies develop, for example, encephalomyelitis, meningoencephalitis.
The combined forms of infection of the nervous system are much more difficult to diagnose, despite the fact that in recent years the diagnostic capabilities of neuroinfections have improved significantly.
Depending on the duration of the pathogenic process, there is an acute (meningitis, encephalitis), subacute and chronic (arachnoiditis, arachnoencephalitis) course of an infectious lesion of the central nervous system.
The main route of transmission is airborne: infection most often occurs through contact with a virus carrier, a sick person, during his coughing or sneezing. Infection is transmitted, including through a kiss, if saliva gets on the mucous membrane of healthy people.
A predisposing factor is the presence of erosions on the gums or their inflammation, as well as microscopic injuries of the mucous epithelium of the oral cavity - if the above circumstances are relevant, it will be easier for the pathogen to enter the body and begin to circulate in it, developing an infection.
The hematogenous route of infection is no less common. The pathological process passes to the brain and spinal cord when the body has a focus of chronic infection, including damage to the vessels supplying these important centers. Such predisposing pathologies are otitis media, brain abscess, thrombosis of the cerebral sinuses.
Neuroinfection develops, among other things, due to the lymphogenous transmission pathway, when there are hidden complications of the transferred craniocerebral and spinal injuries in the patient's body. Especially if it is burdened with liquorrhea.
The infection is not transmitted by household contact, therefore, if you use personal funds and belongings of the virus carrier, infection will not occur. The seasonality of the pathology - hot summer - such a condition is most favorable for the spread of infection, therefore, inhabited places with arid, sultry climate are more susceptible to neuroinfection.
Summarizing, it should be noted that an infection affecting the nervous system can be caused by both viral, bacterial, and fungal etiology.
Voicing the diagnosis, taking into account the origin of the pathogen, the penetration of which into the body gave rise to the infection. Therefore, the "bacterial", "viral", "fungal" (meningitis, encephalitis, etc.)
The causes of neuroinfection of the brain are:
previous traumatic brain injury(especially, accompanied by prolonged compression); hypothermia(exposure to low temperature air without a hat); if during surgery on the brain or spinal cord, medical instruments or consumables were used, low-quality sterilization level; if surgical or therapeutic intervention was complicated by a violation of the integrity of the doctor's gloves or was carried out without their use; carried over viral diseases (more often - flu).
Neuroinfection often occurs as a nosocomial disease and can be the result of visiting a dentist who used insufficiently disinfected instruments during his work.
Predisposing factors include: 
low immunity(especially if the patient has HIV, tuberculosis, syphilis or other diseases that undermine the protective properties of the body); the presence of foci of purulent infection(tonsillitis, otitis media), their latent course or rapid transition from an acute stage to a chronic form; ignoring the control examination after past illnesses as well as cranial or spinal cord injuries.
In neurosurgical and neurological practice, the following types of infections of the nervous system are encountered.
Meningitis is an inflammation of the lining of the brain and / or spinal cord. Infection occurs hematogenous, lymphogenous or airborne  drip.
drip.
Pathogens - viruses, bacteria, fungi; predisposing factors are the presence (including latent) purulent or inflammatory chronic processes in the sinuses of the nasopharynx or the auditory canal, as well as hypothermia.
The symptoms of meningitis are quite specific: by visualizing them, you can quickly diagnose this type of neuroinfection by starting its treatment.
The most pronounced manifestations:
neck stiffness(the patient cannot tilt his head forward); intense headache that is always accompanied by vomiting(this symptom raises doubts among experts as to whether the patient has meningitis or concussion - the determining factor is the history); an increase in body temperature to a high mark.
Treatment involves bed rest and antibiotic therapy. drugs broad-spectrum antimicrobial. The forecast is favorable.
Arachnoiditis is an inflammatory process, the localization of which is in the arachnoid membrane of the brain. The development of arachnoiditis is determined by the transferred head injuries, the presence of rheumatism, and the timely treatment of ENT infection.
The symptoms of this type of neuroinfection are: 
severe, persistent headache, making it impossible to perform even elementary actions; deterioration of vision; weakness; nausea, the attack of which ends with vomiting; increased body temperature; possible development of nosebleeds due to cerebrovascular accident; insomnia; in severe cases - impaired consciousness or lack of it.
The prognosis for the patient is favorable only if the diagnosis is made in a timely manner and treatment is performed. Therapy for this disease is aimed at eliminating the inflammatory process, stabilizing cerebral circulation and general strengthening of the patient's body.
Encephalitis - inflammation of the brain tissue is a consequence of tick-borne lesions, as well as the penetration and exposure of bacteria and viruses. If the patient neglects to seek medical help, the prognosis is poor and even fatal. The symptoms of this type of neuroinfection are pronounced:
the headache increases in the supine position, is stable (it is poorly and for a short time relieved by analgesics); there is an increase in body temperature; weakness and feeling of weakness are growing, as manifestations of general intoxication of the body.
 Oculomotor disorders are part of the symptom complex characteristic of this type of neuroinfection: the patient develops ptosis (drooping of the eyelid), a feeling of double vision, and general visual impairment.
Oculomotor disorders are part of the symptom complex characteristic of this type of neuroinfection: the patient develops ptosis (drooping of the eyelid), a feeling of double vision, and general visual impairment.
Dyspepsia is manifested by nausea, which is especially common after movement by transport; vomiting occurs.
Hospitalization presupposes further therapy with antibiotics, hormonal drugs and general tonic.
The most informative type of research is MRI, CT, and also an encephalogram. The laboratory part of the diagnosis involves the study of blood and urine.
An analysis of cerebrospinal fluid is also carried out - cerebrospinal fluid, in which elevated level squirrel. Each of these diagnostic procedures allows visualizing the state of the brain and spinal cord, determining the localization of the pathogenic process, the degree of infection and involvement of tissues in the inflammatory process.
Treatment for neuroinfection is as follows:
Having established the diagnosis, the patient is hospitalized. Vein catheterization performed(an indwelling intravenous catheter is installed). Antibiotic therapy is prescribed... The antimicrobial drug is chosen by the doctor taking into account which pathogen triggered the development of neuroinfection: only by adhering to this, one can count on the success of the treatment. Antibiotics are given intravenously or by drip (via infusion), as this ensures instantaneous ingestion medicinal substance into the blood, as opposed to performing intramuscular injections. Frequently used drugs include Cefepim, Medaxone, Ceftazidime. The patient is prescribed hormonal drugs - mainly, Prednisolone and Dexamethasone, the dosage of which is determined by the severity of the patient and the form of pathology. If the neuroinfection is combined, then the dosage of the hormonal substance should be higher than with a separate infectious disease of the nervous system. Patient immunity is maintained the introduction of vitamin complexes. Level correction blood pressure carried out by introducing sulphate magnesia. For to reduce the degree of cerebral edema, the patient is injected with diuretics: Furosemide, Lasix. Throughout the patient's stay in the hospital, vital signs are monitored his body. Maintaining them at a normal level is ensured by continuous infusion therapy of the patient with saline solutions and glucose. Carry out diuresis control sick. In order to prevent exhaustion, it is performed parenteral nutrition sick; carry out hygienic care.

The most severe consequences of neuroinfection include death; disability; dementia. These consequences are a good reason not to postpone seeking medical help, undergo an examination and follow all the doctor's prescriptions.
It is possible to prevent the development of neuroinfection: for this, ENT and dental pathologies should be promptly treated, contact with infected people should be avoided, a headdress should be put on at low air temperatures and immunity should be strengthened.
Neuroinfection - what is it? What are the reasons for the development of such diseases, effective ways of treatment? Such questions are faced by people who first heard from a doctor that they are developing a neuroinfection.
In medical reference books, this disease is interpreted as an infectious disease caused by fungi, viruses or bacteria, which affects the nervous system, while having heavy course with a high mortality rate.
Neuroinfection includes a fairly large list of diseases, many of which are fatal to the brain. All of them can have an acute form of the course or turn into a chronic one and proceed quite sluggishly. As medical practice shows, these diseases can pass in an acute form once and no longer bother the patient or have frequent and vivid relapses until the end of his days.
Among all diseases in this group, acute forms include:
Encephalitis - the substance of the brain becomes inflamed. The most common reason becomes the tick-borne encephalitis virus. Meningitis - the lining of the brain becomes inflamed. Here, both the brain and the spinal cord can be affected. Tetanus. Rabies. Myelitis - the spinal cord becomes inflamed due to an infection launched in it. Arachnoiditis - the arachnoid membrane of the brain becomes inflamed.
TO chronic forms include:
neurosyphilis; neuroAIDS; leprosy; damage to the nervous system by tuberculosis; neurobrucellosis; brucellosis.
Regardless of the type and location of the lesion, neuroinfection of the brain and spinal cord manifests itself in three striking symptoms:
General intoxication of the body. The patient's body temperature rises sharply, very often to critical levels, general weakness appears in the body, and the ability to work decreases. CSF Syndrome. In the cells of the cerebrospinal fluid, the amount of protein and cells, which prevail over proteins, significantly increases. Symptoms of cerebrospinal fluid hypertension. Patients indicate that in the supine position their headache increases significantly, especially in the morning, confusion or distraction of consciousness may be noted, there are cases of tachycardia and low blood pressure.

Neuroinfections in children are manifested quite often, while they have a severe course. Due to the fact that the baby's immune system is not yet fully formed, the defeat often occurs through the hemophilic rod. Based on medical research, it can be concluded that such lesions occur in children who have a history of congenital malformations of the nervous system: cerebral palsy, hypoxia during childbirth.
For the treatment to be effective and correct, it is necessary to undergo the following examinations:
Examination by a neurologist. Here the doctor will conduct a study of all reflexes of the body: coordination of movements, sensitivity, which will help to immediately distinguish neuroinfectious diseases from other neurological ones. Laboratory blood tests. At this stage, it is extremely important to identify the causative agent of the disease and investigate the ability of the immune system to resist it. Diagnostic tests of the immune system. In the case when the infection enters through the bite of a mosquito or tick, it is necessary to correctly assess the ability to resist the disease. MRI. During the study, foci of lesions of the brain or spinal cord will be determined, it is possible to recognize tumor diseases that give similar symptoms. Electroneuromyography. It is done to recognize an infection of the peripheral nerves or spinal cord.
Treatment for a disease caused by a virus, bacteria or fungus will depend on its location and the type of infection itself. The main objectives of drug therapy will be:
the restoration of the correct functioning of the nervous system of the whole organism. restoration of the body's immune system; cessation of pathways for the development of infection; elimination of the causative agent of the infection; Viral encephalitis.
When a diagnosis of viral encephalitis is made, the patient is immediately placed in intensive care, since careful monitoring of the respiratory function in the body and blood circulation processes is necessary. In the first few days, drugs are administered to lower the temperature, antiviral and anticonvulsant. The consumption of water by sick people is minimized.
Meningitis.
This disease requires urgent medical attention. Treatment takes place in a hospital setting, since serious complications are always likely, and death can also occur.
As a treatment, antibiotics of a wide spectrum of action are used and antibacterial drugs that remove the specific virus that caused the development of the disease. Basis for appointment drug treatment there will also be age and blood pressure indicators.

Fungal neuroinfection.
In this type, the disease is extremely difficult to immediately diagnose. The causes of brain damage can be fungi of the genus Candida or cryptococci, which enter the body through the mucous membranes of the nose, throat or ears. Most susceptible to this disease are people who have a concomitant diagnosis of AIDS. In such a group of people, fungi are activated against the background of a sharp decrease in the body's immune defenses and affect parts of the brain.
Dangerous in this type of disease is that symptomatic manifestations do not always immediately make themselves felt, but the development of the disease entails a danger to human life. Development can be suspected by regular head pains and increased drowsiness.

Today, fungal meningitis is treatable, but only in 50% of patients. Earlier, before the invention of the drug Amphotericin B, it was 100% death. Also, doctors recommend using the drug Fluconazole and antibiotic therapy... Everything therapeutic measures carried out only in a hospital, under the strict supervision of a doctor. Daily blood tests are extremely important, which show the further development of inflammatory processes.
This type of neuroinfection is considered one of the most severe and dangerous for humans. With damage to the spinal cord, serious complications almost always remain: nerve cells die, which leads to paralysis, dysfunctions of the intestines, bladder.
As a treatment, drugs of the glucocorticosteroid group and broad-spectrum antibiotics will be used. It is very important to pass timely treatment in the hospital in order to immediately stop the development of concomitant diseases, which will be activated against the background of myelitis.

Since in almost all cases of myelitis paralysis occurs, it is extremely important to organize proper care for the patient and his skin, use means that prevent the appearance of pressure sores.
The most terrible and serious consequences are those that were transferred in utero. Here there will be violations in the formation of organs, the nervous system, malformations.
In an adult, after suffering diseases, a headache remains, constant pain in the back, which are worse when the weather changes. Many doctors also state that after recovery in such patients, memory deteriorates, problems with memorization are noted, hearing and vision may be impaired. There are isolated cases when a neuroinfectious disease leads to complete disability, a person loses sight or hearing.
Neuroinfection is a group serious illnesses that pose a danger to human life. Only attention to your body and a quick visit to a doctor can minimize the development of complications or the likelihood of death.
Are you having occasional or regular torment headache attacks Presses the head and eyes or "hits with a sledgehammer" on the back of the head or knocks on the temples Sometimes with a headache you feel sick and dizzy? It all starts enrage, it becomes impossible to work! Do you splash your irritability on your relatives and colleagues?
Stop putting up with it, you can no longer wait, dragging out the treatment. Read what Elena Malysheva advises and find out how to get rid of these problems.
 meningitis, encephalitis, their mixed forms, differing from each other in manifestations, diagnostic capabilities.
meningitis, encephalitis, their mixed forms, differing from each other in manifestations, diagnostic capabilities.
The issue of brain infection in children is especially relevant, since at this age the body is extremely sensitive to various pathogens and can quickly develop brain neuroinfections - serious infectious diseases with damage to the central nervous system and the development of severe symptoms. At the same time, several types of such diseases are distinguished: coma, other life-threatening conditions.
Any neuroinfection is based on the infection of a person, his central nervous system with various microorganisms: bacteria, viruses or fungi. In this case, an infectious process develops, characterized by the development of inflammation and cell damage. In addition, infection can lead to:
traumatic brain injury, in particular with the phenomenon of prolonged compression of the structures of the brain; prolonged hypothermia; the use of non-sterile instruments during surgical procedures on the head; a viral infection that can serve as a factor in weakening the immune system.
As a result of the action of such factors, infection of the central nervous system with microorganisms can occur. In this case, there are three main types of damage to the central nervous system:
Meningitis is characterized by the development of an inflammatory process in the meninges. Encephalitis - inflammation and infection is associated with direct damage to brain tissue. Mixed form - elements of meningitis and encephalitis are combined.
Different forms of the disease may differ in their main manifestations, which can be used in the diagnosis of neuroinfection of the brain and in determining the tactics of treatment.
The symptoms of brain infections have both similarities and differences. With meningitis, general cerebral manifestations come to the fore, such as:
headache, sometimes accompanied by vomiting; a significant rise in the patient's body temperature up to 39–40 ° C; stiffness of the back muscles of the neck; phenomena of general intoxication with muscle pain, weakness and increased fatigue.
With encephalitis, there are practically no individual neurological symptoms, which makes it possible to distinguish it from meningitis. In the latter case, the symptoms of neuroinfection of the brain are predominantly focal in nature:
headaches of varying intensity; impaired movement or sensitivity in the limbs; eye movement disorders, decreased visual acuity or loss of its fields; various violations of gait, coordination of movements; cognitive impairment (decreased memory, thinking ability); temperature rise to 38–39 ° C.
In this case, the manifestations of meningitis are characterized by individual neurological defects associated with direct damage as a result of inflammation of specific brain regions.
The most important place in the diagnosis of neuroinfections is occupied by an external examination of the patient with the determination of his neurological status. Already at this stage, the attending physician may suspect the form of the lesion, determine the localization of the pathological process.
 However, to clarify the diagnosis and determine the site of the lesion, laboratory and instrumental methods are used:
However, to clarify the diagnosis and determine the site of the lesion, laboratory and instrumental methods are used:
Neuroimaging methods: computed and magnetic resonance imaging, allow you to assess the state of the tissue of the central nervous system, meninges. Electroencephalography is used to assess the functioning of brain cells and can reveal the extent and severity of nerve tissue damage. Electroneuromyography is used to determine the severity of damage to the conducting nerve pathways in the presence of paresis or paralysis in a patient. Lumbar puncture with subsequent analysis of cerebrospinal fluid allows you to identify the inflammatory process in the central nervous system, to determine its pathogens (viruses or bacteria). A clinical and biochemical blood test helps to identify the inflammatory process in the body.
The correct use of the described methods, together with the collection of complaints and the conduct of a neurological examination, makes it possible to make the correct diagnosis and prescribe rational treatment.

Description:
Neuroinfections can be classified according to their site of origin into (infectious inflammation of the brain), myelitis (infectious inflammation of the spinal cord), (infectious inflammation of the spinal cord), meninges), (infectious inflammation of the meninges) and combined forms (encephalomyelitis, and so on).
Symptoms:
Any infectious lesion of the nervous system is accompanied by three clinical syndromes:
1. Intoxication (weakness, decreased ability to work, increased body temperature).
2. CSF (there is a syndrome of cellular-protein dissociation, ie the amount of protein and cells in the cerebrospinal fluid is increased, but cells significantly prevail over protein).
3. Syndrome of cerebrospinal fluid hypertension (headache increases in the supine position, occurs in the morning, there may be weakness, impaired consciousness, and also Cushing's triad - and tachypnea against the background of low systolic blood pressure).
Causes of occurrence:
Infectious damage to the nervous system can be associated with a viral, bacterial infection, can be caused by protozoa or fungi, and in some cases, there is the development of specific inflammation of the nervous structures (tuberculous, syphilitic).
Treatment:
For treatment are prescribed:
Treatment depends on the pathogen. For the treatment of bacterial infections, antibiotics of a wide spectrum are used before the pathogen is identified, after which specific antibiotic therapy is used. For viral infections, use antiviral drugs, mainly interferon. In addition to etiotropic therapy, pathogenetic and symptomatic treatment is also carried out - infusion therapy, diuretics, vascular drugs, neuroprotectors, nephrotrophic drugs, nootropics, vitamins of group B and C.