Instructions for the use of mertenil ®. Instructions for use of the drug Mertenil and its prices in pharmacies Mertenil side effects reviews
Instructions for use
Additional Information
Mertenil is a drug, the active ingredient of which is rosuvastatin. These pills lower total and "bad" blood cholesterol. They inhibit the development of atherosclerosis. Doctors prescribe them for the prevention of the first and repeated heart attacks, ischemic stroke and other complications of atherosclerosis. Watch the video to see if you need to take this medication or not.
Treatment with rosuvastatin and other statins reduces the likelihood of having to undergo stent surgery or coronary artery bypass grafting... The original drug is Crestor by AstraZeneca. Mertenil is a competing manufacturer's rosuvastatin tablets (Gedeon Richter) that are cheaper. Gedeon Richter is trying to prove that its drug is as effective as Crestor tablets. Below are instructions for use, written in clear language. Read the indications for use, dosages, contraindications, interactions with other medications. Find out what kind of cholesterol reduction you can expect when you start taking Mertenil. Understand what side effects are, how to reduce or completely eliminate them.
Drug card

| pharmachologic effect | Mertenil, like other rosuvastatin drugs, reduces the "bad" LDL cholesterol in the blood, partially blocking its production in the liver. Increases "good" HDL cholesterol. Reduces chronic sluggish inflammation in blood vessels. Improves C-reactive protein and other markers of inflammation. Blood test results begin to improve after 1–2 weeks, with maximum effect after 2–4 weeks. |
| Pharmacokinetics | Mertenil and other rosuvastatin tablets can be taken with food or on an empty stomach, the effectiveness does not change. Rosuvastatin is excreted from the body 90% by the liver through the intestines, 10% by the kidneys. It loads the liver systems less than other statins, which are involved in cleaning the blood from the active substances of drugs. As a result, it has fewer negative interactions with other drugs than the previous generation of statins. |
| Indications for use | High cholesterol in adults and adolescents. Inhibition of the development of atherosclerosis. Prevention of the first and repeated heart attack, ischemic stroke and other complications of atherosclerosis. After surgery to restore blood flow in the vessels affected by atherosclerosis. Elevated C-reactive protein in the blood in the presence of other cardiovascular risk factors, even if cholesterol is normal. Taking Mertenil tablets is not a substitute for maintaining a healthy lifestyle. Study the article "" and do what it says. Otherwise, the medicine will not help much. |
Read more about the treatment of diseases:

Watch also the video:
| Dosage | Start with a dosage of 5 or 10 mg per day. After 4 weeks, the dose of tablets can be increased, taking into account how the cholesterol levels in the blood have changed during this time and how the patient tolerates the treatment. Explore. Usually patients take rosuvastatin 10-20 mg per day. The maximum dose of 40 mg is prescribed mainly for people whose cholesterol is very high due to genetic disorders. Mertenil is prescribed in standard doses for the elderly, as well as for patients with mild renal or hepatic insufficiency. |
| Side effects | Mertenil, like other statins, can cause muscle pain, weakness, fatigue, impaired memory and thinking, rash, and indigestion. Study the article "" - find out how to alleviate unpleasant symptoms or remove them altogether. Rosuvastatin medications have their own specific side effects. Read more,. For people who are at high risk of heart attack and stroke, statins do more good than harm. They should be canceled only if the side effects are intolerable and cannot be alleviated. The danger of liver problems is exaggerated. Don't worry about them if you don't abuse alcohol. |
| Contraindications | Liver disease in the active phase. A significant increase in the liver enzymes ALT and AST in the blood. Severe renal dysfunction - creatinine clearance less than 30 ml / min. Hypersensitivity to rosuvastatin or other substances that make up the tablets. In Russian-speaking countries, the age of up to 18 years is considered a contraindication, although abroad rosuvastatin preparations are prescribed to adolescents starting from 10 years. |
| Pregnancy and breastfeeding | Mertenil, other rosuvastatin drugs and all other statins are categorically contraindicated during pregnancy. Women of childbearing age who are treated with statins should use reliable contraception. If an unplanned pregnancy occurs, then taking cholesterol pills should be stopped immediately. You cannot breastfeed during treatment with this drug. |
| Drug interactions | Rosuvastatin drugs have fewer negative interactions with other drugs than previous generation statins. But there is still considerable danger. There can be problems with antibiotics, drugs that affect immunity, birth control pills, blood thinners, and many other drugs. This can cause serious side effects such as liver and kidney damage. Talk to your doctor! Before you are discharged from Mertenil, tell your doctor about all medications, dietary supplements, and herbs you are taking. |
| Overdose | There is no specific treatment for an overdose with rosuvastatin tablets. Doctors carry out symptomatic treatment and supportive measures by monitoring liver function and the degree of creatinine phosphokinase activity. Hemodialysis does not help remove rosuvastatin from the body. |
| special instructions | Once you start treatment with Mertenil, continue your diet and healthy lifestyle. It is recommended to periodically monitor kidney function with blood and urine tests. If protein is found in the urine or its concentration increases - pay the attention of your doctor. If you have a hormone deficiency thyroid gland, then do not rush to take statins, but treat hypothyroidism to bring cholesterol back to normal. Rosuvastatin medications slightly increase blood sugar in people with diabetes and prediabetes. |
| Release form | Film-coated tablets, 5, 10, 20 and 40 mg. In a blister strip packaging made of foil, 10 tablets each. In a pack of cardboard, 3 blisters. |
| Storage conditions and periods | Store in a dry, dark place, out of the reach of children, at a temperature not exceeding 30 ° C. The shelf life is 3 years. |
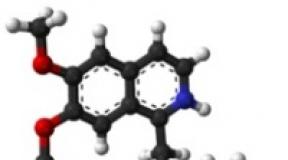
| Structure | The active ingredient is rosuvastatin calcium. Excipients - lactose monohydrate, magnesium hydroxide, crospovidone (type A), magnesium stearate. Tablet shell - talc, macrogol, titanium dioxide (E171), polyvinyl alcohol. |
Many patients are interested in what analogues of the drug Mertenil are cheaper. There are many such medicines on sale in the pharmacy. They are produced in the Russian Federation and the CIS countries, as well as imported from Europe and Asia. All these are tablets in which the active ingredient is rosuvastatin. Watch a video about possible substitutes for the drug Mertenil, so as not to be mistaken with the choice.
Keep in mind that Mertenil medicine is a combination of reasonable price and good European quality. If it helps you and you normally tolerate its reception, then it hardly makes sense to switch to analogues in order to save a little money. It may be better to take Crestor, the original rosuvastatin drug. However, it costs more.
Read more about analogues of the drug Mertenil
Mertenil: reviews
Application of the drug Mertenil
Mertenil is prescribed for people at high cardiovascular risk. Taking these pills reduces the likelihood of a first and repeated heart attack, ischemic stroke and other manifestations of atherosclerosis. If you are at high risk, then rosuvastatin medications will provide significant benefits. They will protect you from heart attack and stroke as well as no other drugs and dietary supplements can. The lives of patients who take statins are several years longer because they later die from cardiovascular disease. At the same time, Mertenil should not be prescribed to people who have high cholesterolbut there are no other cardiovascular risk factors. If the risk of heart attack and stroke is low, then statins will do more harm than good.
People at high cardiovascular risk are those diagnosed with arterial hypertension, prediabetes or diabetes mellitus, smokers, and especially patients who have already had a heart attack or stroke. People who are overweight or have poor C-reactive protein blood test results also need to take Mertenil and move on to a healthy lifestyle to avoid a cardiovascular accident. Statins must be prescribed for people who have undergone stenting or coronary artery bypass grafting. This reduces the likelihood that a second operation will be required.
The benefits of statins, including rosuvastatin, have been proven in dozens of clinical research... In the vast majority of these trials, participants were prescribed the original Crestor drug. For rosuvastatin tablets from other manufacturers, the evidence base is weaker, which is why they are cheaper. Gedeon Richter is a renowned Hungarian drug manufacturer. She is trying to prove that the drug Mertenil is not inferior in effectiveness to tablets. To this end, the company funds small-scale research and the publication of articles in medical journals. More on this below. You should not completely trust the results of clinical trials of drugs, because they are all paid for by pharmaceutical companies. Which rosuvastatin drug to choose should be decided by the doctor, taking into account the patient's financial capabilities.
Reducing "bad" cholesterol
It is believed that the higher the "bad" cholesterol, the greater the patient's risk of heart attack, stroke and other complications of atherosclerosis. Mertenil and other rosuvastatin drugs are the newest statins. They lower the "bad" LDL cholesterol more than any drug that has been invented before. Articles in medical journals show that Mertenil has been shown to lower LDL cholesterol to target levels in many patients who have not been helped by early statins.
On the basis of the Belarusian State Medical University, as well as others medical institutions the city of Minsk conducted a comparative study of the effectiveness of tablets Mertenil and cholesterol lowering. As a result of this study, several articles were published in Russian-language medical journals. One such article is "Comparative efficacy and safety of Mertenil in patients with hyperlipidemia" in the journal International Reviews: clinical practice and health "No. 5/2013. Patients who had high cholesterol were divided into two groups of 30 people. Those who entered the first group were prescribed Mertenil 10 mg per day, and in the second - the original drug Crestor in the same dosage.
Comparative effectiveness drugs Mertenil and Crestor
Mertenil reduced the "bad" LDL cholesterol by 46%, and Crestor in his group - by 43%. The authors of the study concluded that Mertenil was as effective as the original Crestor drug. This result should not be completely trusted because the research was paid for by the manufacturer. Also note that both drugs at the low dosage of 10 mg / day did not significantly affect important triglyceride and C-reactive protein levels. In foreign studies, rosuvastatin preparations are usually used in higher dosages - 20 or 40 mg per day.
To keep your good and bad cholesterol and triglycerides normal, switch to. This will allow you to reduce the dosage of Mertenil tablets or even completely abandon statin treatment. A low-carb diet is satisfying and delicious. It actually improves blood cholesterol levels. The "low-fat" diet, which is usually recommended by doctors, causes excruciating chronic hunger, and even does not help to lower cholesterol.
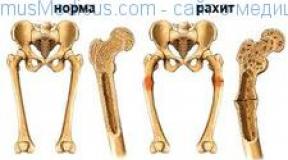
Atherosclerosis
Mertenil, like other rosuvastatin drugs, is prescribed for the treatment of atherosclerosis. If it is possible to bring atherosclerosis under control, then the patient's risk of the first and repeated heart attack, ischemic stroke, the need to perform stenting, coronary bypass grafting, and surgically restore blood flow in the legs is significantly reduced. Life is extended and its quality is improved. The main treatment for atherosclerosis is diet food and regular physical activity. Taking statins, even the most powerful of them rosuvastatin, can only complement the transition to a healthy lifestyle, but not replace it.
In 2006, the results of the ASTEROID study (A Study To Evaluate the Effect of Rosuvastatin On Intravascular ultrasound-Derived coronary atheroma burden) were published. In this study, scientists were able to demonstrate for the first time the ability of statins to reduce the size of atherosclerotic plaques in coronary arteries. This was done using rosuvastatin as an example. Later it was found that treatment with atorvastatin also gives such an effect. Third and fourth generation statins not only slow down the development of atherosclerosis, but also have a unique property - they affect cholesterol plaques that have already formed. In foreign studies of the effectiveness of rosuvastatin in atherosclerosis, patients were prescribed. It is not known whether Mertenil tablets can reduce the size of atherosclerotic plaques as well as Crestor.
After menopause occurs in women, the development of atherosclerosis accelerates due to changes in hormonal levels. Middle-aged women are less likely to have cardiovascular disease than men. But in old age they are catching up and even ahead of their male peers in terms of the frequency of heart attacks and strokes. The reason is a decrease in estrogen levels. During menopause, women are often worried about hypertension. Modern medicine pays a lot of attention to the problem of age-related metabolic disorders in women.
In the journal "Arterial hypertension" No. 6/2013, an article was published "The effect of Mertenil on the state of the vascular bed in women with arterial hypertension and dyslipidemia with hypoestrogenemia in premenopause." Hypoestrogenemia is a decrease in estrogen in the blood caused by the onset of menopause. The authors of the article found out the effect of the appointment of rosuvastatin in addition to the standard treatment of hypertension in middle-aged women. The study involved 52 patients. Of these, 32 took Mertenil 10 mg per day and pressure pills (Diroton), and 22 took only Diroton.
To assess how rosuvastatin influenced the development of atherosclerosis, the participants underwent ultrasound of the carotid arteries at the beginning of the study, and then again after 4 months. The thickness of the intima-media complex was measured, and the elongation coefficient, arterial stiffness index, and maximum systolic blood flow velocity were calculated. The thickness of the intima-media complex is a key indicator of the development of atherosclerosis, which is measured during ultrasound of the vessels. The lower the value, the better.
The effectiveness of the drug Mertenil against atherosclerosis
The addition of Mertenil improved the results of standard treatment of hypertension in middle-aged women. The lower the stiffness index and the higher the tensile coefficient, the more favorable the forecast. Because the better the arteries retain their natural flexibility, the lower the pressure required to pump blood through them. And the lower blood pressure, the less the heart wears out. Unfortunately, the article does not provide comparative data on cholesterol indicators in women who took rosuvastatin and those who limited themselves to just a medicine for hypertension.
This is not mentioned in most articles, but a large foreign study SATURN has shown that treatment with statins increases calcium deposits in the arteries. The arteries, on the walls of which calcium is present, become rigid and lose their natural flexibility. This is an advanced stage of atherosclerosis. It turns out that in the treatment of atherosclerosis with Mertenil and other statins, not everything is clear. These drugs slow down the development of atherosclerosis, but worsen the course of the disease. Study the detailed material "Statins and Atherosclerosis: Pros and Cons". Learn how to neutralize calcium problems in your arteries.
Mertenil, like other rosuvastatin drugs, slows down the development of coronary atherosclerosis. This improves the prognosis for patients suffering from ischemic disease hearts. Rosuvastatin, like atorvastatin, not only inhibits the appearance of new cholesterol plaques, but also reduces the size of those that have already formed. Probably, treatment with Mertenil reduces the risk of not only heart problems, but also cerebrovascular accidents, pain in the legs and other manifestations of systemic atherosclerosis.
The basis of the evidence base for rosuvastatin was the JUPITER study, the results of which were published in 2008. The study involved more than 15 thousand patients. Half of them were prescribed rosuvastatin 20 mg per day, and the other half received a placebo. In people who took the real medicine, "bad" LDL cholesterol dropped by an average of 50%, triglycerides by 17%, and C-reactive protein by 37%. But the main thing is that the incidence of cardiovascular diseases has significantly decreased.
JUPITER Study Results
As you can see, taking rosuvastatin significantly reduced the risk of complications of coronary heart disease. All participants were assigned. There is no exact information whether Mertenil tablets have how much good effect. The JUPITER study has been criticized for being completed ahead of schedule - 2 years later, not 5 years as planned. If the study had lasted 5 years, then the difference between the indicators in the rosuvastatin and placebo groups would probably not have been so significant.
Patients diagnosed with coronary artery disease are people who have a high cardiovascular risk. They need to take rosuvastatin or other statins to reduce the likelihood of heart attacks and strokes. The benefits of treatment with these pills will be higher than the possible troubles from side effects... Also read the article "" and follow the steps it describes. Taking Mertenil pills cannot replace the transition to a healthy lifestyle, but only complements diet, exercise and stress management
After suffering a heart attack
After suffering a heart attack, patients are usually prescribed rosuvastatin or other statins to normalize cholesterol, as well as reduce inflammation and C-reactive protein levels in the blood. It is believed that rosuvastatin lowers "bad" cholesterol more than other statins, therefore it is of increased interest among doctors and patients. In the 2000s, this drug was criticized for the lack of research data on it, which would involve patients with a heart attack. To date, such studies have been carried out, their results have been published.
In September 2014, a report on the results of IBIS-4 appeared on the website of the European Society of Cardiology - a study of the effectiveness of treatment with high doses of rosuvastatin in patients who have had myocardial infarction with an increase in the QT segment. 103 patients took the original drug Crestor 40 mg per day in addition to standard treatment. Doctors followed them for 13 months. Patients regularly underwent blood tests for cholesterol. They also underwent ultrasound of the arteries at the beginning and at the end of the term to assess whether atherosclerosis was developing.
After 13 months, 85% of patients had decreased atherosclerotic plaques in at least one coronary artery, and 56% - in both. "Bad" LDL cholesterol in the blood decreased by an average of 43%. Prior to the IBIS-4 study, the benefits of giving high doses of statins to patients with stable coronary artery disease were proven, and now also to those with heart attacks. It is noteworthy that the study was sponsored by the manufacturers of ultrasound machines, but not pharmaceutical companies... The authors of the report remind that dosages of rosuvastatin 40 mg per day have not yet been approved in many European countries. There is no evidence to what extent Mertenil is equivalent for people who have had a heart attack.
It is known that statins, together with the risk of heart attack, reduce the likelihood of stroke. The JUPITER study formed the basis of the evidence base for rosuvastatin. Among other breakthrough results, rosuvastatin was found to reduce the risk of stroke by as much as 51% for patients who had normal cholesterol but elevated C-reactive protein in their blood. In the group of patients taking the original drug Krestor, the frequency of ischemic stroke decreased significantly, and hemorrhagic stroke did not increase. The JUPITER study has been criticized for being stopped ahead of schedule. The patients were followed up for only 2 years. If they had been followed for longer, the results would probably not have been as sensational.
Small studies have shown the feasibility of prescribing simvastatin and atorvastatin as early as possible after a stroke. But for rosuvastatin no data have been found to date. Doctors from South Korea in 2010 tried EUREKA, a trial of early prescription of rosuvastatin to prevent recurrent stroke. But the study did not take place because they could not persuade enough patients to participate in it - at least 507 people were needed.
Read detailed articles:

There is no information whether Mertenil has the same effect for the prevention of the first stroke as. As for the prevention of recurrent stroke, there is no data even for Crestor tablets, and even more so for rosuvastatin drugs from other manufacturers. Therefore, today, it is probably better to choose not rosuvastatin, but atorvastatin or simvastatin for the prevention of recurrent stroke. Read also the material ““. Find out which medications lower the risk of stroke, how useful are pills for hypertension.
Type 2 diabetes mellitus
Mertenil, like other rosuvastatin drugs, increases blood sugar in type 2 diabetics. Also, this drug increases the risk of developing diabetes for patients who already have impaired carbohydrate metabolism. At the same time, it has significant benefits in reducing the risk of heart attack and stroke. No other medications and dietary supplements can help with cardiovascular problems as well as statins. You need to be diligently treated with your prescribed cholesterol drug. In doing so, take simple steps to keep your sugar in the normal range.
Japanese experts have found out how much atorvastatin and rosuvastatin increase blood sugar in diabetic patients. 514 diabetics were taking rosuvastatin, and another 504 patients were taking atorvastatin. They started with low dosages - the original drug Krestor 5 mg per day, and atorvastatin 10 mg per day. Doses of statins were gradually increased until it was possible to lower LDL cholesterol to the recommended values. It turned out that both drugs increase sugar in diabetic patients almost equally. The difference in plasma glucose values \u200b\u200bwas 0.16-0.22 mmol / L.
Patients were followed for only 12 months, so they were able to track only glucose and cholesterol levels, but not cardiovascular risk. At the low dosages indicated above, atorvastatin and rosuvastatin reduced bad cholesterol equally. They decided not to prolong the trial, because it has already been proven that statins reduce the risk of heart attack and stroke for diabetics. It is not known if Mertenil affects blood sugar in the same way or differently. Probably, the difference, if it exists, is not big.

Mertenil with diabetes: pros and cons
In 2015, the authoritative journal Lancet published the results of the PLANET I study - a comparison of the effectiveness of atorvastatin and rosuvastatin in protecting the kidneys in patients with type 2 diabetes. The study involved 353 patients. At the start of the study, all of them already had signs of diabetic kidney damage, were taking medications - ACE inhibitors or blockers angiotensin II receptors... The participants were divided into 3 groups:
- rosuvastatin 10 mg per day;
- rosuvastatin 40 mg per day;
- atorvastatin 80 mg per day.
Atorvastatin had a better effect on the ratio of albumin to creatinine in urine in patients than rosuvastatin at dosages of 10 and 40 mg per day. Kidney-related side effects were more common in the rosuvastatin group than in those taking atorvastatin. The results of this study can speak in favor of atorvastatin for patients with diabetes mellitus. They can be considered reliable because the trial was funded by AstraZeneca, the manufacturer of rosuvastatin. It turns out that diabetic patients are better off choosing some of the atorvastatin preparations, rather than Mertenil.
Rosuvastatin and other statins increase the risk of developing diabetes in patients who are predisposed to diabetes. People who are diagnosed with metabolic syndrome or impaired glucose tolerance should be wary of diabetes. Metabolic syndrome is a combination of symptoms: excess weight, fat deposits around the waist, arterial hypertension, poor blood cholesterol and triglyceride tests. Women who have already reached menopause, and all people who are overweight, are high-risk patients for diabetes. Learn how to prevent diabetes in the Metabolic Syndrome article. Follow the steps outlined there. However, keep taking Mertenil or other statins to reduce your risk of heart attack and stroke. Read also the detailed information ““. Find out which drugs carry the lowest risk of diabetes.
Systemic lupus erythematosus
Systemic lupus erythematosus is autoimmune diseasewhich gradually destroys vital organs and systems. It limits social and professional activity sick, often leads to premature death. In patients with lupus erythematosus, myocardial infarction develops 50 times more often than in their healthy peers. The reason is the early development of atherosclerosis against the background of autoimmune attacks. For lupus erythematosus, statins are often prescribed to improve blood cholesterol and C-reactive protein levels.
In the journal "Fundamental Research" No. 5/2013, employees of the Tyumen State medical academy on the effectiveness of the appointment of rosuvastatin to patients with systemic lupus erythematosus. The study involved 53 patients, of whom 29 prescribed Mertenil 10 mg per day in addition to standard treatment. The rest of the patients who did not take statins were included in the control group. All participants were followed for 12 months. Rosuvastatin improved cholesterol and triglyceride levels, atherogenic coefficient, and blood C-reactive protein levels.
Lipid changes in patients with lupus erythematosus during treatment with Mertenil
Patients with lupus erythematosus, who were prescribed Mertenil, tolerated the treatment well. They have improved not only blood cholesterol levels, but also the dynamics of atherosclerosis development, according to the results of ultrasound of the arteries. The results of the study presented above cannot be considered strictly scientific, because there were few patients involved. However, this information is useful for practice. Mertenil is one of the drugs suitable for slowing the development of the atherosclerotic process.
Hereditary hypercholesterolemia in adults
Hereditary hypercholesterolemia is a serious disease in which people have significantly increased total and "bad" cholesterol due to genetic disorders. The diet doesn't help much. Cardiovascular disease in people with this genetic disorder develops much earlier than in their healthy peers. If left untreated, hereditary hypercholesterolemia reduces life expectancy by at least 8 years. Therefore, patients are advised to begin treatment with statins as early as adolescence and take these drugs in the maximum tolerated doses.
Rosuvastatin is the most potent statin available today. Therefore, it can be the drug of choice for patients with hereditary hypercholesterolemia, for whom it is desirable to lower the "bad" LDL cholesterol in the blood by 50% or more from the initial values. The journal "Systemic Hypertension" No. 2/2014 published an article "Efficiency and safety
Mertenil (rosuvastatin) 40 mg / day in patients with familial hypercholesterolemia. The study involved 40 patients whose mean LDL cholesterol was 7.2 mmol / L. They were prescribed the drug immediately at a maximum dose of 40 mg per day, and after 16 weeks of taking it, repeated blood tests were done.
The results of taking Mertenil 40 mg per day
Apolipoprotein A1 is a beneficial protein that helps remove cholesterol from the walls of blood vessels. Taking rosuvastatin practically did not lower it. Apolipoprotein B is a carrier of "bad cholesterol". Its accumulation in the blood leads to the development of atherosclerosis. The medicine had a beneficial effect on this indicator.
In none of the patients who participated in the study, taking Mertenil tablets at a maximum daily dose of 40 mg did not cause serious side effects. C-reactive protein and uric acid levels in the blood decreased, which means that the treatment has a beneficial effect on metabolism. Thus, Mertenil can be recommended for people suffering from hereditary hypercholesterolemia. It is advisable to start treatment with statins at a young age. Rosuvastatin drugs cause fewer negative interactions with other drugs than simvastatin and atorvastatin. This is important for patients with hereditary hypercholesterolemia who have to take several powerful drugs at the same time.
High cholesterol in children
Children and adolescents have significantly increased blood cholesterol due to a hereditary disease - familial hypercholesterolemia. Statins are prescribed to treat this condition since adolescence. Rosuvastatin is by far the most potent of the statins, so it may be an appropriate drug for treating familial hypercholesterolemia at a young age.
An article was published in the Journal of the American College of Cardiology in March 2010 - a report on the results of research on the efficacy and safety of rosuvastatin for the treatment of familial hypercholesterolemia in children. The study involved 177 patients aged 10-17 years. Some of them prescribed rosuvastatin, first at 5 mg per day, and later increased the dosage to 10 and 20 mg per day. There was also a control group of patients who took a placebo rather than the real drug. The participants were followed up for 1 year.
How rosuvastatin lowers LDL cholesterol in adolescents
The drug did not cause serious side effects. There were no abnormalities in the growth and development of the adolescents who participated in the study. All participants accepted. There is no information whether Mertenil tablets can give the same good efficacy and tolerability in adolescent patients. Taking rosuvastatin 5-20 mg per day, only 40% of study participants were able to achieve the target normal level LDL cholesterol. But the dosage of this drug 40 mg per day is prohibited from prescribing to patients under 18 years of age.
conclusions
The article explains everything that patients need to know about the use of Mertenil to improve blood cholesterol levels. Patients at high cardiovascular risk take rosuvastatin tablets to prevent first and second heart attacks, ischemic stroke, leg problems, and other complications of systemic atherosclerosis. The side effects of statins are mostly the same, but rosuvastatin has its own nuances.
INN: Rosuvastatin
Manufacturer: Gedeon Richter JSC
Anatomical-therapeutic-chemical classification: Rosuvastatin
Registration number in the RK: No. RK-LS-5 No. 018356
Registration period: 23.11.2016 - 23.11.2021
KNF (drugs are included in the Kazakhstan National Formulary of Medicines)
UNIT (Included in the List of Medicines under the guaranteed volume of medical care to be purchased from a Single Distributor)
Maximum purchase price in the Republic of Kazakhstan: 139.18 KZT
Instructions
Tradename
Mertenil ®
International non-proprietary name
Rosuvastatin
Dosage form
Film-coated tablets, 5 mg, 10 mg, 20 mg, 40 mg
Structure
One tablet contains
active substance: rosuvastatin calcium 5.2 mg (equivalent to 5.0 mg rosuvastatin), 10.4 mg (equivalent to 10.0 mg rosuvastatin), 20.8 mg (equivalent to 20.0 mg rosuvastatin), 41.6 mg (equivalent to 40.0 mg rosuvastatin),
excipients: lactose monohydrate, microcrystalline cellulose 12, magnesium hydroxide, crospovidone type A, magnesium stearate,
film shell composition: opadry II white: polyvinyl alcohol, titanium dioxide (E171), macrogol 3350, talc.
Description
White or almost white film-coated tablets, round, biconvex, engraved on one side C33 (for a dosage of 5 mg), C34 (for a dosage of 10 mg), C35 (for a dosage of 20 mg), the other side without engraving.
White or almost white film-coated tablets, oblong, biconvex, engraved on one side C36 (for a dosage of 40 mg), the other side without engraving.
Pharmacotherapeutic group
Lipid-lowering drugs. Hypocholesterolemic and hypotriglyceridemic drugs. HMG CoA reductase inhibitors. Rosuvastatin
ATX code С10AA07
Pharmacological properties
Pharmacokinetics
Suction
The maximum plasma concentration of rosuvastatin is reached 5 hours after oral administration. The absolute bioavailability is approximately 20%.
Distribution
Rosuvastatin is absorbed mainly by the liver, which is the main site of cholesterol synthesis and the clearance of cholesterol metabolism - low density lipoprotein (LDL). The volume of distribution of rosuvastatin is approximately 134 liters. 90% of rosuvastatin binds to blood plasma proteins, mainly albumin.
Metabolism
Rosuvastatin undergoes limited metabolism (approximately 10%), it is not a substrate for metabolism by the cytochrome P450 enzymes. CYP2C9 is the main isoenzyme involved in metabolism, while isoenzymes CYP2C19, CYP3A4 and CYP2D6 are involved in metabolism to a lesser extent. The main metabolite is N-desmethyl, which is 50% less active than rosuvastatin. Lactone metabolites are pharmacologically inactive. More than 90% of the pharmacological activity in inhibiting circulating HMG-CoA reductase is provided by rosuvastatin, 10% - by its metabolites.
Withdrawal
Approximately 90% of the dose of rosuvastatin taken is excreted unchanged from the body through the intestines (including absorbed and non-absorbed rosuvastatin) , and the remainder is excreted unchanged by the kidneys. The half-life (T1 / 2) is 19 hours and does not change with increasing dose of the drug. Geometric mean plasma clearance is approximately 50 L / h (coefficient of variation 21.7%). As in the case of other inhibitors of HMG-CoA reductase, the membrane transporter, membrane cholesterol-cutaneous transport protein C of organic anions (OATP-C), is involved in the process of hepatic uptake of rosuvastatin. This carrier plays an important role in the excretion of rosuvastatin by the liver.
Linearity
The systemic effect of rosuvastatin increases in proportion to the dose of the drug. Pharmacokinetic parameters do not change with daily intake.
Pharmacodynamics
Rosuvastatin, the active substance of Mertenil®, is a selective and competitive inhibitor of HMG-CoA reductase, an enzyme that converts 3-hydroxy-3-methylglutaryl coenzyme A into mevalonate, which is a cholesterol precursor. The main target of Mertenil® action is the liver, where cholesterol (CS) synthesis and low density lipoprotein (LDL) catabolism are carried out.
Mertenil® increases the number of "hepatic" LDL receptors on the cell surface, increasing the uptake and catabolism of LDL.
It also inhibits the synthesis of very low density lipoprotein (VLDL) cholesterol in liver cells, thereby lowering total LDL and VLDL.
Mertenil® reduces increased content cholesterol - LDL, total cholesterol and triglycerides (TG), increases the content of high-density lipoprotein cholesterol (HDL-C), and also reduces the content of apolipoprotein B (ApoV), non-HDL cholesterol (total cholesterol content minus HDL cholesterol, cholesterol VLDL, TG-VLDL and increases the level of apolipoprotein AI (ApoA-I). Mertenil®, reduces the ratio of LDL-C / HDL-C, total cholesterol / HDL-C, non-HDL-C / HDL-C and ApoV / ApoA-I.
The therapeutic effect can be achieved within one week after the start of treatment, after 2 weeks 90% of the maximum possible effect... Usually, the maximum possible therapeutic effect is achieved after 4 weeks and is maintained with further administration of the drug.
Clinical efficacy
Mertenil® is effective in the treatment of adult patients with hypercholesterolemia with or without symptoms of hypertriglyceridemia, regardless of their race, gender or age, as well as in the treatment of a special category of patients with diabetes mellitus or hereditary form of familial hypercholesterolemia.
The drug in a dose of 40 mg should be prescribed to patients with severe hypercholesterolemia and high degree risk of developing cardiovascular diseases.
Indications for use
- primary hypercholesterolemia (type IIa, including familial heterozygous hypercholesterolemia) or mixed dyslipidemia (type IIb) as an adjunct to dietary therapy when diet and other non-drug therapies (eg, exercise, weight loss) are insufficient
Familial homozygous hypercholesterolemia as an adjunct to diet therapy and other lipid-lowering therapies (eg, LDL apheresis) or when such therapy is not effective enough
As an adjunct to diet to slow the progression of atherosclerosis in adult patients as part of therapy to lower total cholesterol and LDL cholesterol to target levels
Prevention of severe cardiovascular complications in patients at high risk of primary atherosclerotic cardiovascular disease, as an additional correction of other risk factors
Method of administration and dosage
Before starting treatment, the patient should follow a standard diet with low cholesterol content, which should be continued throughout the treatment period. Doses of the drug should be selected individually in accordance with the purpose of the treatment and the patient's therapeutic response to the therapy, taking into account the current generally accepted recommendations for target lipid levels.
The recommended initial dose of the drug is 5 mg or 10 mg 1 time per day both for patients who have not previously taken statins and for patients transferred to the reception this drug after therapy with other inhibitors of HMG-CoA reductase.
When choosing the initial dose of the drug, one should take into account the cholesterol level in each individual patient, as well as the possible risk of developing cardiovascular complications and the potential risk of side effects. If necessary, a dose adjustment can be made after 4 weeks.
Titration of the drug to maximum dose 40 mg should only be given in patients with severe hypercholesterolemia and a high risk of cardiovascular disease (in particular, with familial hypercholesterolemia), in whom the target cholesterol level was not reached with a dose of 20 mg, and who will be under medical supervision. When prescribing a dose of 40 mg, careful observation of patients is recommended. It is not recommended to prescribe a dose of 40 mg to patients who have not previously taken the drug. Mertenil® can be taken at any time of the day, orally, regardless of food intake, do not chew or grind, swallow it whole with water.
Use in elderly patients
Use in patients with renal failure
In patients with mild to moderate renal insufficiency, dose adjustment is not required. The recommended initial dose of the drug is 5 mg for patients with moderate renal insufficiency (CC less than 60 ml / min.).
Use in patientspredisposed to myopathy
Side effects
Often (> 1/100 do <1/10)
Dizziness, headache
Myalgia
Asthenia
Nausea, constipation, abdominal pain
Type II diabetes mellitus
Infrequently (> 1/1 000 do <1/100)
Itching, rash, urticaria
Rarely (> 1/10 000 do <1/1000)
Hypersensitivity reactions (including angioedema)
Pancreatitis
Myositis, rhabdomyolysis
Increased activity of "hepatic" transaminases
Proteinuria
Very rarely (<1/10000)
- polyneuropathy, memory loss
Jaundice, hepatitis
Arthralgia
Hematuria
Sleep disorders including insomnia and nightmares
Depression
Sexual dysfunction
Isolated cases - interstitial lung diseases.
Unspecified frequency
- immune-mediated necrotizing myopathy
Cough, shortness of breath
Steven Johnson Syndrome
Gynecomastia
Peripheral edema
The incidence of side effects is dose-dependent.
Contraindications
For tablets 5, 10, 20 mg
Hypersensitivity to rosuvastatin or any component of the drug
Liver failure with a score above 9 on the Childe-Pugh scale
Severe renal dysfunction (creatinine clearance less than 30 ml / min.);
Myopathy
- predisposition to the development of myotoxic complications
Myotoxicity while taking other MMC-CoA reductase inhibitors or fibrates in anamnesis
For 40 mg tablets
- hypersensitivity to rosuvastatin or any of the components of the drug
Liver diseases in the active phase, including a persistent increase in the activity of "hepatic" transaminases, as well as any increase in the activity of transaminases in the blood serum by more than 3 times compared with the upper limit of normal
Liver failure with a score above 9 on the Childe-Pugh scale
Severe renal dysfunction (creatinine clearance less than 60 ml / min.);
Myopathy
Simultaneous administration of cyclosporine
Hypothyroidism
Personal or family history of muscle disease
Predisposition to the development of myotoxic complications
Myotoxicity while taking other HMG-CoA reductase inhibitors or fibrates in anamnesis
Simultaneous reception of fibrates
Excessive alcohol consumption
Conditions that can lead to an increase in the concentration of rosuvastatin in blood plasma
Asian patients (Japanese, Chinese, Filipinos, Vietnamese and Koreans)
Congenital lactose intolerance, lactase deficiency, or glucose-galactose malabsorption
Pregnancy and lactation
Children and adolescents up to 18 years old
Drug interactions
Cyclosporine: while taking drugs, changes in the concentration of cyclosporine in the blood plasma were not detected, but it leads to an increase in the concentration of rosuvastatin in the blood plasma by 11 times.
Vitamin K antagonists: As in the case of other HMG-CoA reductase inhibitors, the initiation of therapy with Mertenil®, or an increase in the dose of the drug in patients receiving concomitant vitamin K antagonists (for example, warfarin or other coumarin anticoagulants) may lead to an increase in the international normalized ratio (INR). Cancellation or reduction of the dose of Mertenil® may cause a decrease in INR. In such cases, INR should be monitored.
Ezetimibe:simultaneous administration of Mertenil® and ezetimibe did not lead to changes in AUC or Cmax of any of the active substances. Gemfibrozil and other lipid lowering agents: Simultaneous administration of Mertenil® and gemfibrozil resulted in a 2-fold increase in C max and AUC of rosuvastatin.
Based on data from separate studies of drug interactions, pharmacokinetic interactions with fenofibrate are not expected, however, the development of pharmacodynamic drug interactions is possible. Gemfibrozil, fenofibrate, other fibrates and doses of niacin (nicotinic acid) in lipid-lowering doses (1 g or more per day) increase the risk of myopathy when co-administered with HMG-CoA reductase inhibitors, possibly due to the fact that they can cause myopathy and when taken in monotherapy.
Protease inhibitors: it is not recommended to prescribe Mertenil® and protease inhibitors at the same time in the treatment of patients with HIV; the half-life of rosuvastatin may be prolonged.
Antacids: the simultaneous administration of Mertenil® and antacids in suspension containing aluminum and magnesium hydroxide can lead to a decrease in the concentration of Mertenil® in blood plasma by about 50%. This effect is less pronounced if antacids are applied 2 hours after taking Mertenil®.
Erythromycin: simultaneous administration of Mertenil® and erythromycin led to a 20% decrease in AUC (0-t) and 30% Cmax of rosuvastatin. This relationship may be due to increased intestinal motility associated with the intake of erythromycin.
Oral contraceptives / hormone replacement therapy (HRT):concomitant use of Mertenil® and oral contraceptives led to an increase in the AUC of ethinyl estradiol and norgestrel by 26% and 34%, respectively. When selecting doses of oral contraceptives, it is necessary to take into account the possibility of increasing plasma concentrations.
Cytochrome P450 isozymes: Mertenil® is neither inhibitor nor inducer of cytochrome P450 isoenzymes. It is a rather weak substrate for these enzymes. There were no clinically significant interactions between Mertenil® and fluconazole (an inhibitor of CYP2C9 and CYP3A4) or ketoconazole (an inhibitor of CYP2A6 and CYP3A4). The simultaneous administration of itraconazole (a CYP3A4 inhibitor) and Mertenil® led to a 28% increase in the AUC of rosuvastatin.
Other medicines: no clinically significant interaction is expected while taking Mertenil® and digoxin.
special instructions
Effects on the kidneys
Proteinuria, mainly of tubular origin, was observed in patients taking high doses of Mertenil®, especially 40 mg, but in most cases it was intermittent or short-term. It has been shown that such proteinuria does not mean the onset of acute or progression of existing kidney disease. The incidence of serious renal impairment increases with 40 mg of rosuvastatin. It is recommended to monitor renal function indicators during therapy with Mertenil®.
Caution should be exercised when prescribing a dose of less than 40 mg.
Effects on skeletal muscle
When using Mertenil® in all dosages, and especially when taking the drug in a dose exceeding 20 mg, myalgia, myopathy and, in rare cases, rhabdomyolysis were detected. Very rarely, rhabdomyolysis occurred while taking ezetimibe and HMG-CoA reductase inhibitors. In this case, the pharmacological interaction of drugs cannot be ruled out, therefore, Mertenil® and ezetimibe should be used with caution together. The incidence of rhabdomyolysis increases with 40 mg of rosuvastatin.
Evaluation of creatine phosphokinase (CPK) activity
Determination of CPK activity should not be carried out after intense physical exertion that causes an increase in CPK, since this can complicate the interpretation of the results. With an increase in the CPK indicator before the start of therapy, more than 5 times the upper limit of the norm, a second measurement should be performed after 5-7 days. If repeated measurement confirms the initial CPK value (5 times higher than the upper limit of the norm), Mertenil® therapy should not be started.
Mertenil®, like other HMG-CoA reductase inhibitors, should be used with extreme caution in patients with existing risk factors for myopathy / rhabdomyolysis. These factors include:
Renal failure
Hypothyroidism
Personal or family history of muscle disease (for 40 mg dose)
A history of myotoxicity while taking other HMG-CoA reductase inhibitors or fibrates (for a dose of 40 mg)
Alcohol abuse (for 40 mg dose)
- age over 70
Conditions accompanied by an increase in the concentration of the drug in the blood plasma (for a dose of 40 mg)
Simultaneous reception of fibrates (for a dose of 40 mg)
In such patients, the risk-to-benefit ratio of therapy should be assessed and clinical observation should be carried out throughout the course of therapy.
During treatment
It is recommended to inform patients about the need to immediately inform the doctor about cases of sudden onset of muscle pain, muscle weakness or spasms, especially in combination with malaise or fever.
In such patients, it is imperative to monitor the activity of CPK. Treatment should be discontinued if the CPK level is more than 5 times higher than the upper limit of the normal or if muscle symptoms are pronounced and cause daily discomfort (even if the CPK activity is 5 times less than the upper limit of the normal). If symptoms disappear and CPK activity returns to normal levels, consideration should be given to re-prescribing Mertenil® or prescribing an alternative HMG-CoA reductase inhibitor in lower doses with close monitoring of the patient. Regular monitoring of CPK activity in patients in the absence of clinical manifestations is inappropriate.
However, an increase in the number of cases of myositis and myopathy has been identified in patients taking other inhibitors of HMG-CoA reductase in conjunction with fibric acid derivatives, including gemfibrozil, cyclosporine, nicotinic acid in lower doses, antifungal drugs, protease inhibitors and macrolide antibiotics. Gemfibrozil increases the risk of myopathy when combined with certain HMG-CoA reductase inhibitors. Therefore, the simultaneous administration of rosuvastatin and gemfibrozil is not recommended. The risk-to-benefit ratio should be carefully assessed when rosuvastatin is used together with fibrates or nicotinic acid in lipid-lowering doses (more than 1 g).
The drug Mertenil® should not be prescribed to patients with acute, severe diseases suggesting myopathy or with the possible development of secondary renal failure associated with rhabdomyolysis (for example: sepsis, arterial hypotension, surgery, trauma, severe metabolic, endocrine, electrolyte disturbances, uncontrolled convulsive seizures).
Effects on the liver
Like other HMG-CoA reductase inhibitors, Mertenil® should be administered with extreme caution to patients who abuse alcohol and / or have a history of liver disease.
It is recommended to determine the indicators of liver function before and 3 months after the start of treatment. If the activity of "hepatic" transaminases in the blood serum is 3 times higher than the upper limit of the norm, you should stop taking Mertenil® or reduce the dose taken. The frequency of severe liver dysfunctions (associated mainly with an increase in the activity of "hepatic" transaminases) increases with the intake of 40 mg of the drug.
In patients with secondary hypercholesterolemia due to hypothyroidism, nephrotic syndrome, therapy of the underlying disease should be carried out before starting treatment with Mertenil®.
Interstitial lung disease
Described are extremely rare cases of the development of interstitial lung disease when taking, especially long-term, individual statins. Clinical manifestations may include shortness of breath, dry cough, and worsening general condition (general weakness, weight loss, and fever). If a patient is suspected of developing interstitial lung disease, statins should be discontinued.
Diabetes
In patients whose fasting glucose was 5.6-6.9 mmol / L, rosuvastatin was associated with an increased risk diabetes mellitus.
In the course of pharmacokinetic studies, an increase in the systemic concentration of rosuvastatin among patients of Asian origin was found in comparison with the data obtained among patients of the European race.
Features of the effect of the drug on the ability to drive a vehicle and potentially dangerous mechanisms
There have been no studies examining the effect of Mertenil® on the ability to drive and use machines. At the same time, when driving a vehicle or other mechanisms, it must be borne in mind that dizziness may occur during treatment.
Overdose
Symptoms: severity of symptoms of side effects.
Structure
Each film-coated tablet contains:
Active substance:
Film-coated tablets, 5 mg: rosuvastatin calcium 5.2 mg (equivalent to 5 mg rosuvastatin);
Film-coated tablets, 10 mg: rosuvastatin calcium 10.4 mg (equivalent to 10 mg rosuvastatin);
Film-coated tablets, 20 mg: rosuvastatin calcium 20.8 mg (equivalent to 20 mg rosuvastatin).
Excipients:
Lactose monohydrate, microcrystalline cellulose 12, magnesium hydroxide, crospovidone type A, magnesium stearate.
Film casing composition:
Opadray II white (polyvinyl alcohol, titanium dioxide E171, macrogol 3350, talc).
Description
Film-coated tablets, 5 mg:
White or nearly white, round, biconvex film-coated tablets, approx. One side of the tablet is engraved with "C33".
Film-coated tablets, 10mg:
White or nearly white, round, biconvex film-coated tablets, approx. One side of the tablet is engraved with "C34".
Film-coated tablets, 20 mg:
White or nearly white, round, biconvex film-coated tablets, approx. One side of the tablet is engraved with "C35".
Pharmacotherapeutic group
HMG-CoA reductase inhibitors.
The codeATX: S10AA07
Pharmacological properties
Pharmacodynamics
Mechanism of action
Rosuvastatin is a selective and competitive inhibitor of HMG-CoA reductase, an enzyme that converts 3-hydroxy-3-methylglutaryl coenzyme A to mevalonate, which is a cholesterol precursor. The main target of rosuvastatin is the liver, where cholesterol (CS) synthesis and low-density lipoprotein (LDL) catabolism are carried out.
Rosuvastatin increases the number of "hepatic" LDL receptors on the cell surface, increasing the uptake and catabolism of LDL.
It also inhibits the synthesis of very low density lipoprotein (VLDL) cholesterol in liver cells, thereby lowering total LDL and VLDL.
Pharmacodynamic effects
Rosuvastatin lowers the high content of cholesterol - LDL (LDL-C), total cholesterol and triglycerides (TG), increases the content of high-density lipoprotein cholesterol (HDL-C), and also reduces the content of apolipoprotein B (Apo), non-HDL cholesterol (total cholesterol) minus the content of HDL cholesterol), cholesterol-VLDL, TG-VLDL and increases the level of apolipoprotein A-I (ApoA-I) (see table 1). Rosuvastatin reduces the ratio of LDL-C / HDL-C, total cholesterol / HDL-C, non-HDL-C / HDL-C and ApoV / ApoA-I.
Table 1. Dose-dependent effect in patients with primary hypercholesterolemia (type IIa and IIb) (mean adjusted percentage change from baseline).
| Dose | Number of patients | Cholesterol-LDL | General CS | Cholesterol-HDL | TG | Cholesterol-non-HDL | Apo B | Apo A-I |
| Placebo | 13 | -7 | -5 | 3 | -3 | -7 | -3 | 0 |
| 5 mg | 17 | -45 | -33 | 13 | -35 | -44 | -38 | 4 |
| 10 mg | 17 | -52 | -36 | 14 | -10 | -48 | -42 | 4 |
| 20 mg | 17 | -55 | -40 | 8 | -23 | -51 | -46 | 5 |
| 40 mg | 18 | -63 | -46 | 10 | -28 | -60 | -54 | 0 |
The therapeutic effect can be achieved within one week after the start of treatment, after 2 weeks 90% of the maximum possible effect is achieved. Usually, the maximum possible therapeutic effect is achieved after 4 weeks and is maintained with further administration of the drug.
Clinical efficacy
Rosuvastatin is effective in the treatment of adult patients with hypercholesterolemia with or without symptoms of hypertriglyceridemia, regardless of their race, gender or age, as well as in the treatment of a special category of patients - patients with diabetes mellitus or hereditary form of familial hypercholesterolemia.
Rosuvastatin is effective for the treatment of patients with Frederickson type IIa and IIb hypercholesterolemia (mean baseline LDL-C level of about 4.8 mmol / L). In 80% of patients who received 10 mg of rosuvastatin, the target values \u200b\u200bof the LDL-C level set by the European Society for the Study of Atherosclerosis (less than 3 mmol / l) were achieved.
In patients with heterozygous familial hypercholesterolemia who took rosuvastatin in doses from 20 to 80 mg according to the forced dose titration scheme, all doses taken had a significant effect on the change in the parameters characterizing the lipid content and on the achievement of the goal of therapy. As a result of titration of doses up to 40 mg per day (12 weeks of therapy), the content of LDL-C decreased by 53%. In 33% of patients, LDL-C values \u200b\u200b(below 3 mmol / L) were achieved, corresponding to the target standards of the European Society for the Study of Atherosclerosis guidelines.
In patients with homozygous familial hypercholesterolemia, who took rosuvastatin in doses of 20 and 40 mg, the average decrease in the content of LDL-C was 22%.
An additive effect is observed in combination with fenofibrate in relation to a decrease in the content of TG and with nicotinic acid (more than a day) in relation to an increase in the content of HDL-C.
In patients with a low risk of coronary heart disease (defined as a Framingham risk of less than 10% over a period of more than 10 years), with an average LDL-C content of 4.0 mmol / L (154.5 mg / dL) rosuvastatin dose of 40 mg / day significantly slowed the increase in the maximum value characterizing the thickening of the carotid artery wall in 12 segments, compared with placebo at a rate of -0.0145 mm / year (95% confidence interval (CI): from -0.0196 to -0.0093, at p
In patients with a high risk of coronary heart disease (Framingham risk more than 20%), a significant reduction in mortality from cardiovascular diseases, stroke and myocardial infarction was observed with rosuvastatin treatment. The overall mortality rate did not change in this risk group.
Children and adolescents
In a double-blind, randomized, multicenter, placebo-controlled 12-week study (N \u003d 176, 97 boys and 79 girls aged 10-17 years, according to the Tanner scale, girls not earlier than one year after menarche), LDL-C decreased by 38.3 %, 44.6% and 50.0% with a single daily dose of rosuvastatin at a dose of 5, 10 or 20 mg, respectively, compared with 0.7% in the placebo group.
At the end of 40 weeks of subsequent titration of the dose to a maximum of 20 mg once a day, in 40.5%, an LDL-C level of less than 2.8 mmol / L was achieved.
No effect of rosuvastatin on height, body weight, BMI (body mass index) or puberty after 52 weeks of treatment was identified. The experience of using rosuvastatin in children and adolescents is limited, the long-term effects of rosuvastatin (more than 1 year) on puberty are unknown.
Pharmacokinetics
Absorption: the maximum concentration of rosuvastatin in blood plasma is reached 5 hours after ingestion of the appropriate dose. The absolute bioavailability is approximately 20%.
Distribution: rosuvastatin is absorbed primarily by the liver, which is the main site of cholesterol synthesis and clearance of LDL-C metabolism. The volume of distribution of rosuvastatin is approximately. 90% of rosuvastatin binds to blood plasma proteins, mainly albumin.
Metabolism: undergoes limited metabolism (approximately 10%). Rosuvastatin is a fairly non-core substrate for metabolism by cytochrome P450 enzymes. CYP2C9 is the main isoenzyme involved in metabolism, while isoenzymes CYP2C19, CYP3A4 and CYP2D6 are involved in metabolism to a lesser extent. The main metabolite is N-desmethyl, which is 50% less active than rosuvastatin. Lactone metabolites are pharmacologically inactive. More than 90% of the pharmacological activity in inhibiting circulating HMG-CoA reductase is provided by rosuvastatin, the rest is provided by its metabolites.
Derivation: approximately 90% of the dose of rosuvastatin taken is excreted unchanged from the body through the intestines (including absorbed and unabsorbed rosuvastatin), and the remainder is excreted unchanged by the kidneys. The half-life (T1 / 2) is 19 hours, it does not change with increasing dose of the drug. The geometric mean plasma clearance is approximately 50 l / h (coefficient of variation 21.7%). As in the case of other inhibitors of HMG-CoA reductase, the membrane transporter of cholesterol across membranes, the transport protein C of organic anions, is involved in the process of hepatic uptake of rosuvastatin. This carrier plays an important role in the elimination of rosuvastatin by the liver.
Linearity: systemic exposure of rosuvastatin increases in proportion to the dose. Changes in pharmacokinetic parameters when taking the drug several times a day are not observed.
Pharmacokinetics in selected patient groups
Age and gender: gender and age do not have a clinically significant effect on the pharmacokinetic parameters of rosuvastatin in adults. The pharmacokinetics of rosuvastatin in children and adolescents with familial hypercholesterolemia did not differ from that in healthy adult volunteers.
Race: comparative studies of pharmacokinetics showed a twofold increase in the average AUC (area under the concentration-time curve) and Cmax (maximum plasma concentration of rosuvastatin) in patients of Asian origin (Japanese, Chinese, Filipinos, Vietnamese and Koreans) compared with those of representatives Caucasian race. The Indians had an approximately 1.3-fold excess of the mean AUC and Cmax. At the same time, the analysis of pharmacokinetic parameters for the entire study population did not reveal clinically significant differences in the pharmacokinetics of the drug among representatives of the Caucasian, Negroid races, and Hispanics.
Renal failure: in patients with mild to moderate renal failure, the plasma concentration of rosuvastatin or the N-desmethyl metabolite does not change significantly. In patients with severe renal insufficiency (creatinine clearance (CC) less than 30 ml / min), the concentration of rosuvastatin in the blood plasma is 3 times higher, and the concentration of the N-desmethyl metabolite is 9 times higher than in healthy volunteers. The plasma concentration of rosuvastatin in hemodialysis patients was approximately 50% higher than in healthy volunteers.
Liver failure: in patients with varying degrees of hepatic insufficiency with a score of 7 and below on the Child-Pugh scale, no increase in rosuvastatin exposure was detected. However, in 2 patients with scores of 8 and 9 on the Child-Pugh scale, an increase in systemic exposure was noted, approximately 2 times higher than that for patients with lower values \u200b\u200bon the Child-Pugh scale. There is no experience with rosuvastatin in patients with a score above 9 on the Child-Pugh scale.
Genetic polymorphism: the transport proteins OATP1B1 and BCRP are also involved in the pharmacokinetics of HMG-CoA reductase inhibitors, including rosuvastatin. Patients with SLCO1B1 (OATP1B1) and / or ABCG2 (BCRP) gene polymorphisms are at risk of increased exposure to rosuvastatin. Individual polymorphisms SLCO1B1 c.521СС and ABCG2 c.421АА are associated with a corresponding increase in the exposure of rosuvastatin (AUC) compared to genotypes SLCO1B1 c.521ТТ or ABCG2 c.421СС. In clinical practice, this type of genotyping has not been established, but a lower daily dose of rosuvastatin is recommended for patients who are known to have these types of polymorphisms.
Children and adolescents: The pharmacokinetic parameters of rosuvastatin in children with familial hypercholesterolemia aged 10 to 17 years are not fully described. The results of a small pharmacokinetic study of rosuvastatin (involving 18 children) show that the exposure of rosuvastatin in children does not differ from that in adult patients, and large deviations of pharmacokinetic parameters depending on the dose are not expected.
Indications for use
Treatment of hypercholesterolemia
Primary hypercholesterolemia in adults, children, and adolescents 10 years and older (type IIa, including familial heterozygous hypercholesterolemia) or mixed dyslipidemia (type IIb) as an adjunct to dietary therapy, when diet and other non-drug treatments (eg, exercise, weight loss) turn out to be insufficient. Familial homozygous hypercholesterolemia as an adjunct to diet therapy and other lipid-lowering therapies (eg, LDL apheresis) or in cases where such therapy is not effective enough.
to reduce the risk of severe cardiovascular complications in adult patients without clinical signs of coronary artery disease, but with an increased risk of its development (age over 50 for men and over 60 for women, increased concentration of C-reactive protein (\u003e 2 mg / l) in the presence of at least one of the additional risk factors, such as arterial hypertension, low concentration of HDL-C, smoking, family history of early onset of coronary artery disease).
Contraindications
hypersensitivity to rosuvastatin or any of the components of the drug; liver disease in the active phase, including a persistent increase in the activity of "hepatic" transaminases, as well as any increase in the activity of transaminases in the blood serum by more than 3 times compared with the upper limit of the norm; severe renal dysfunction (CC less than 30 ml / min); myopathy; concomitant use of cyclosporine; pregnancy and the period of breastfeeding; women of childbearing age who do not use reliable contraception; lactose intolerance, lactase deficiency or glucose-galactose malabsorption.
The use of rosuvastatin at a dose of 40 mg is contraindicated in patients with factors predisposing to the development of myopathy / rhabdomyolysis.
Such factors include:
Moderately severe renal dysfunction (creatinine clearance less than 60 ml / min); hypothyroidism; an individual or family history of hereditary muscle diseases; myotoxicity while taking other inhibitors of HMG-CoA reductase (3-hydroxy-3-methylglutaryl coenzyme A-reductase) or fibrates in anamnesis; alcohol abuse; conditions that can lead to an increase in the concentration of rosuvastatin in the blood plasma; belonging to the Mongoloid race; simultaneous intake of fibrates.
Carefully
Rosuvastatin in all doses, especially at a dose of 40 mg, should be taken with caution in the following cases: risk of myopathy / rhabdomyolysis - renal failure, hypothyroidism; a personal or family history of hereditary muscle disease and a previous history of muscle toxicity with other HMG-CoA reductase inhibitors or fibrates; excessive alcohol consumption; conditions in which an increase in the plasma concentration of rosuvastatin is noted; age over 70; a history of liver disease; sepsis; arterial hypotension; extensive surgical interventions; trauma; severe metabolic, endocrine or electrolyte disturbances; uncontrolled epilepsy; race (Mongoloid race); simultaneous reception of fibrates.
Application during pregnancy and during breastfeeding
Mertenil is contraindicated for use during pregnancy and during breastfeeding.
Women of childbearing age should use reliable and adequate contraception.
Pregnancy
Since cholesterol and cholesterol biosynthesis products are important for fetal development, the potential risk of inhibition of HMG-CoA reductase outweighs the benefits of its use during pregnancy.
In case of pregnancy, the drug should be stopped immediately.
Breastfeeding period
There are no data on the excretion of rosuvastatin in breast milk. If it is necessary to prescribe the drug during lactation, breastfeeding should be discontinued.
Fertility
There are limited data on reproductive toxicity (animal studies).
Method of administration and dosage
Before starting treatment, the patient should follow a standard low-cholesterol diet, which should be continued throughout the treatment period.
Doses of the drug should be selected individually in accordance with the purpose of the treatment and the patient's therapeutic response to the therapy, taking into account the current generally accepted recommendations for target lipid levels.
Mode of application
Inside, at any time of the day, regardless of food intake, do not chew or grind, swallow whole with water.
Treatment of hypercholesterolemia
The recommended initial dose of the drug is 5 mg or 10 mg 1 time per day both for patients who have not previously taken statins and for patients who have been transferred to this drug after therapy with other HMG-CoA reductase inhibitors.
When choosing the initial dose of the drug, one should take into account the cholesterol level in each individual patient, as well as the possible risk of developing cardiovascular complications and the potential risk of side effects. The dose can be increased if necessary after 4 weeks.
Since in the case of a dose of 40 mg, adverse reactions occur more often than with the use of lower doses, titration of the dose to a maximum of 40 mg should be performed only for patients with severe hypercholesterolemia and high cardiovascular risk (in particular, in people with familial hypercholesterolemia), in whom failed to achieve the desired result when taking a dose of 20 mg and which will be under the supervision of a specialist. At the beginning of the 40 mg dose, specialist supervision is recommended.
Prevention of cardiovascular complications
In a study to reduce the risk of cardiovascular events, rosuvastatin was used at a dose of 20 mg per day.
Children and adolescents
The use of rosuvastatin in children should only be carried out by a specialist.
Children and adolescents from 10 to 17 years old (boys - with secondary sexual characteristics on the Tanner scale of stage II and higher, girls - not earlier than a year after the first menstruation).
The usual starting dose for children and adolescents with familial heterozygous hypercholesterolemia is 5 mg per day. The usual dose range is 5 to 20 mg orally once a day.
Dose titration should be carried out individually in accordance with the patient's therapeutic response to the therapy and taking into account the tolerability, according to the recommendations for treatment in children and adolescents. Before starting treatment, the patient should follow a standard low-cholesterol diet, which should be continued throughout the treatment period.
The safety and efficacy of doses exceeding 20 mg have not been studied in children.
Children under 10 years old
The experience of using rosuvastatin in children under 10 years of age is limited. Therefore, Mertenil is not recommended for use in children under 10 years of age.
Elderly patients
Patients with renal impairment
In patients with mild to moderate renal impairment, dose adjustment is not required. The recommended initial dose of the drug is 5 mg for patients with moderate renal insufficiency (CC less than 60 ml / min). Appointment of the drug Mertenil in any dose is contraindicated in patients with severe renal failure (see section "Contraindications" and "Pharmacokinetics"). For patients with moderate renal insufficiency, the use of the drug at a dose of 40 mg is contraindicated.
Patients with hepatic impairment
An increase in the systemic concentration of rosuvastatin in patients with a Child-Pugh score of 7 or less was not detected. However, an increase in the systemic concentration of the drug was observed in patients with Child-Pugh scores of 8 and 9. In such patients, liver function should be monitored during therapy. There are no data on the use of the drug by patients with a Child-Pugh score above 9. Mertenil is contraindicated in patients with liver disease in the active phase.
Race
In patients of the Mongoloid race, an increase in the systemic concentration of rosuvastatin is possible. When prescribing doses of 10 and 20 mg, the recommended initial dose of the drug for patients of the Mongoloid race is 5 mg. The use of the drug in a dose of 40 mg is contraindicated in such patients.
Genetic polymorphism
It is known that certain types of genetic polymorphisms can lead to increased exposure to rosuvastatin (see section "Pharmacokinetics"). For patients known to have these types of polymorphisms, a lower daily dose of rosuvastatin is recommended.
Patients predisposed to myopathy
For patients predisposed to myopathy, the initial dose of the drug is 5 mg (see section "Precautions").
Concomitant therapy
Rosuvastatin is a substrate for various transport proteins (for example, OATP1B1 and BCRP). When the drug Mertenil is used together with drugs (such as cyclosporine, some HIV protease inhibitors, including the combination of ritonavir with atazanavir, lopinavir and / or tipranavir) that increase the concentration of rosuvastatin in blood plasma due to interaction with transport proteins, the risk of myopathy may increase (including rhabdomyolysis) (see sections "Precautions" and "Interaction with other drugs"). In such cases, the possibility of prescribing alternative therapy or temporary discontinuation of the drug Mertenil should be evaluated. If the use of the above drugs and rosuvastatin is necessary, you should evaluate the balance of benefits and risks of concomitant therapy and consider reducing the dose of Mertenil (see section "Interaction with other drugs").
Side effect
Side effects associated with taking Mertenil are usually mild and short-lived. In the course of controlled clinical trials, less than 4% of patients taking rosuvastatin discontinued treatment due to the development of side effects.
Based on clinical trial data and extensive post-marketing experience, Table 2 below presents the adverse drug reaction (ADR) profile for rosuvastatin.
ADRs are classified by their frequency of occurrence and by classes of organ systems. The incidence of ADR is presented as follows: often (≥1 / 100 to
Table 2. Adverse drug reactions
| Organ system class | Often | Infrequently | Rarely | Very rarely | Frequency unknown | |
| Blood and lymphatic system disorders | Thrombocytopenia | |||||
| Immune system disorders | Hypersensitivity reactions, including angioedema | |||||
| Endocrine system disorders | Type 2 diabetes mellitus1 | |||||
| Mental disorders | Depression | |||||
| Nervous system disorders | Headache dizziness | Polyneuropathy Memory loss | Peripheral neuropathy Sleep disturbances (including insomnia and "nightmares") | |||
| Respiratory, Chest and Mediastinal Disorders | Cough Shortness of breath | |||||
| Gastrointestinal disorders | Constipation Nausea Stomach pain | Pancreatitis | Diarrhea | |||
| Liver and biliary tract disorders | Increased activity of "hepatic" transaminases | Jaundice Hepatitis | ||||
| Skin and subcutaneous tissue disorders | Itchy skin Rash Urticaria | Stevens Johnson Syndrome | ||||
| Musculoskeletal and connective tissue disorders | Myalgia | Myopathy (including myositis) Rhabdomyolysis | Arthralgia | Immune-mediated necrotizing myopathy Tendon diseases in some cases are complicated by rupture | ||
| Kidney and urinary tract disorders | Hematuria | |||||
| Genital and breast disorders | Gynecomastia | |||||
| General disorders and disorders at the injection site | Asthenic syndrome | Peripheral edema | ||||
| 1 Frequency will depend on the presence or absence of risk factors (fasting glucose concentration ≥5.6 mmol / l, BMI\u003e 30 kg / m2, increased triglyceride concentration, history of hypertension). | ||||||
As with other HMG-CoA reductase inhibitors, the incidence of side effects is dose-dependent.
From the kidneys and urinary tract: when taking rosuvastatin, proteinuria was observed, mainly of tubular origin. Changes in urine protein content (from absence or presence of trace amounts to ++ and above) were found in less than 1% of patients taking 10 and 20 mg of rosuvastatin, and about 3% of patients taking 40 mg of the drug.
The minimum change in the amount of protein in urine, expressed as a change from zero or traces to the + level, was observed when taking the drug at a dose of 20 mg. In most cases, proteinuria diminished and resolved on its own during treatment. When analyzing data from clinical studies and post-marketing experience, no causal relationship was found between proteinuria and acute or progressive kidney disease.
In a number of patients treated with rosuvastatin, hematuria was observed, but data from clinical studies have shown that the incidence of such cases is low.
From the musculoskeletal and connective tissue: an effect on skeletal muscle causing myalgia, myopathy (including myositis) and, in rare cases, rhabdomyolysis with or without acute renal failure, has been observed in patients taking any dose of rosuvastatin, especially a dose above 20 mg. An increase in the content of creatine phosphokinase (CPK), depending on the dose taken, was detected in patients taking rosuvastatin, but in most cases these manifestations were insignificant, asymptomatic and temporary. If the content of CPK is 5 times higher than the upper limit of the norm, then treatment should be discontinued (see the section "Precautions").
From the liver and biliary tract: As with other HMG-CoA reductase inhibitors, an increase in the activity of "hepatic" transaminases, depending on the dose taken, was found in a small number of patients taking rosuvastatin. Moreover, in most cases, this increase was insignificant, asymptomatic and transient.
The following ADRs have been reported with some statins:
Sexual dysfunction; in extremely rare cases, interstitial lung disease, especially with prolonged therapy (see section "Precautions").
The incidence of rhabdomyolysis, serious kidney and liver disorders (mainly an increase in the activity of "hepatic" transaminases) was higher with a dose of 40 mg.
Children and adolescents
In children and adolescents, after exercise or significant physical exertion, an increase in CPK\u003e 10 × VGN and muscle symptoms were more often noted than in adults (see the section "Precautions"), although the safety profile of the use of rosuvastatin in children, adolescents and adults is the same.
Overdose
There is no specific treatment for overdose.
Interaction with other medicinal products
Effect of other drugs on rosuvastatin
Transport protein inhibitors: rosuvastatin is a substrate for several transport proteins, including the hepatic uptake transporter OATP1B1 and the efflux transporter BCRP. The simultaneous use of rosuvastatin and drugs that are inhibitors of these transport proteins may be accompanied by an increase in the concentration of rosuvastatin in the blood plasma and an increased risk of developing myopathy (see sections "Dosage and Administration", "Precautions" and "Interaction with other drugs", Table 3).
Cyclosporine: while taking rosuvastatin and cyclosporin, the AUC of rosuvastatin increased by 7 times compared with the values \u200b\u200bobtained in healthy volunteers (see Table 3). Rosuvastatin is contraindicated in patients receiving cyclosporine (see section "Contraindications"). Simultaneous administration of drugs does not affect the concentration of cyclosporine in blood plasma.
Protease inhibitors: although the exact mechanism of interaction is unknown, concomitant administration of rosuvastatin with protease inhibitors can lead to a significant increase in the exposure of rosuvastatin (see Table 3). In a pharmacokinetic study, while taking 10 mg of rosuvastatin and a combined preparation containing two protease inhibitors (300 mg of atazanavir / 100 mg of ritonavir), healthy volunteers showed a 3-fold increase in the AUC in the equilibrium state and a 7-fold increase in Cmax of rosuvastatin, respectively. Concomitant use of rosuvastatin and some combinations of protease inhibitors is possible after careful selection of the dose of rosuvastatin, based on the expected increase in the exposure of rosuvastatin (see sections "method of administration and dosage", "Precautions" and "Interaction with other drugs", Table 3).
Gemfibrozil and other lipid-lowering agents: concomitant administration of rosuvastatin and gemfibrozil leads to a 2-fold increase in Cmax and AUC of rosuvastatin (see section "Precautions").
Based on data from studies of specific interactions, an appropriate pharmacokinetic interaction with fenofibrate is not expected, however, a pharmacodynamic interaction is possible. Gemfibrozil, fenofibrate, other fibrates and nicotinic acid in lipid-lowering doses (1 g or more per day), when taken simultaneously with HMG-Co A reductase inhibitors, increased the risk of myopathy, possibly due to the fact that they can cause myopathy and taken as monotherapy. The simultaneous reception of 40 mg of rosuvastatin and fibrates is contraindicated (see sections "Contraindications" and "Precautions"). The initial dose of the drug Mertenil in patients of this group should not exceed 5 mg.
Ezetimibe: the simultaneous use of rosuvastatin at a dose of 10 mg and ezetimibe at a dose of 10 mg was accompanied by an increase in the AUC of rosuvastatin by 1.2 times in patients with hypercholesterolemia (see Table 3). An increase in the risk of side effects due to the pharmacodynamic interaction between rosuvastatin and ezetimibe cannot be ruled out (see section "Precautions").
Antacids: concomitant administration of rosuvastatin and antacids in a suspension containing aluminum or magnesium hydroxide can lead to a decrease in the concentration of rosuvastatin in blood plasma by about 50%. This effect is less pronounced if antacids are used 2 hours after taking rosuvastatin. The clinical significance of this interaction has not been studied.
Erythromycin: the simultaneous administration of rosuvastatin and erythromycin can lead to a decrease in the AUC (0-t) of rosuvastatin by 20% and the Cmax of rosuvastatin by 30%. This relationship may be due to increased intestinal motility associated with the intake of erythromycin.
Cytochrome P450 isozymes: the results of in vitro and in vivo studies have shown that rosuvastatin is neither an inhibitor nor an inducer of cytochrome P450 isoenzymes. In addition, rosuvastatin is a rather weak substrate for these enzymes. Therefore, any drug interactions associated with the metabolism of cytochrome P450 are not expected. There was no clinically significant interaction between rosuvastatin and fluconazole (an inhibitor of CYP2C9 and CYP3A4 isoenzymes) or ketoconazole (an inhibitor of CYP2A6 and CYP3A4 isoenzymes). The combined use of itraconazole (an inhibitor of the isoenzyme CYP3A4) and rosuvastatin increases the AUC of rosuvastatin by 28% (clinically insignificant).
Interaction with medicinal products requiring dose adjustment of rosuvastatin (see Table 3)
The dose of the drug Mertenil should be adjusted if it is necessary to use it together with drugs that increase the exposure of rosuvastatin. If an increase in exposure (AUC) of 2 times or more is expected, the initial dose of Mertenil should be 5 mg once a day. You should also adjust the maximum daily dose of the drug Mertenil so that the expected exposure of rosuvastatin does not exceed that for a dose of 40 mg taken without the simultaneous administration of drugs interacting with rosuvastatin. For example, the maximum daily dose of Mertenil® when used simultaneously with gemfibrozil is 20 mg (increase in exposure by 1.9 times), with atazanavir / ritonavir - 10 mg (increase in exposure by 3.1 times).
Table 3. Effect of concomitant therapy on exposure to rosuvastatin (AUC, data in descending order) - results from published clinical trials.
| Concomitant therapy regimen | Rosuvastatin regimen | Change in AIS rosuvastatin * | |
| Cyclosporin 75-200 mg 2 times a day, 6 months | 10 mg once a day, 10 days | Increase 7.1 times | |
| Atazanavir 300 mg / ritonavir 100 mg once daily for 8 days | 10 mg once | Increase 3.1 times | |
| Lopinavir 400 mg / ritonavir 100 mg 2 times a day, 17 days | 20 mg once a day, 7 days | Increase 2.1 times | |
| Gemfibrozil 600 mg 2 times a day, 7 days | 80 mg once | 1.9x magnification | |
| Eltrombopag 75 mg 1 time per day, 10 days | 10 mg once | Increase 1.6 times | |
| Darunavir 600 mg / ritonavir 100 mg 2 times a day, 7 days | 10 mg once a day, 7 days | Magnification 1.5 times | |
| Tipranavir 500 mg / ritonavir 200 mg 2 times a day, 11 days | 10 mg once | Increase 1.4 times | |
| Dronedarone 400 mg 2 times a day. | No data | Increase 1.4 times | |
| Itraconazole 200 mg once a day, 5 days | 10 mg once | 1.4x magnification ** | |
| Ezetimibe 10 mg once a day, 14 days | 10 mg once a day, 14 days | 1.2x magnification ** | |
| Fosamprenavir 700 mg / ritonavir 100 mg 2 times a day, 8 days | 10 mg once | Without changes | |
| Aleglitazar 0.3 mg 7 days | 40 mg, 7 days | Without changes | |
| Silymarin 140 mg 3 times a day, 5 days | 10 mg once | Without changes | |
| Fenofibrate 67 mg 3 times a day, 7 days | 10 mg, 7 days | Without changes | |
| Rifampin 450 mg once a day, 7 days | 20 mg once | Without changes | |
| Ketoconazole 200 mg 2 times a day, 7 days | 80 mg once | Without changes | |
| Fluconazole 200 mg once a day, 11 days | 80 mg once | Without changes | |
| Erythromycin 500 mg 4 times a day, 7 days | 80 mg once | Down 28% | |
| Baikalin 50 mg 3 times a day, 14 days | 20 mg once | Down 47% | |
* Data presented as fold change show the ratio of AUC when taken together to that when rosuvastatin monotherapy. The data, presented as% change, reflect the difference (%) in relation to monotherapy with rosuvastatin.
** Several drug interaction studies have been performed with different doses of rosuvastatin; the table shows the most significant deviations.
Effect of rosuvastatin use on other drugs
Vitamin K antagonists: As with other HMG-CoA reductase inhibitors, initiation of rosuvastatin therapy or an increase in the dose of the drug in patients receiving concomitant vitamin K antagonists (for example, warfarin or other coumarin anticoagulants) can lead to an increase in the international normalized ratio (INR). Cancellation or dose reduction of rosuvastatin may cause a decrease in INR. In such cases, INR should be monitored.
Oral contraceptives / hormone replacement therapy: concomitant use of rosuvastatin and oral contraceptives can lead to an increase in the AUC of ethinyl estradiol and norgestrel by 26% and 34%, respectively. Such an increase in plasma concentrations should be considered when choosing a dose of oral contraceptives. There are no pharmacokinetic data on the simultaneous use of rosuvastatin and hormone replacement therapy drugs, so a similar effect cannot be excluded when using this combination. However, this combination of drugs was widely used by women in clinical trials and was well tolerated.
Other medicines: based on data from studies of specific interactions, no clinically significant interaction is expected when rosuvastatin and digoxin are taken concomitantly.
Children
Interaction studies have only been performed in adults. The intensity of interactions in children is unknown.
Precautions
Renal effects
Proteinuria, mainly of tubular origin, has been observed in patients taking high doses of Mertenil, especially 40 mg, but in most cases it was intermittent or short-lived. It has been shown that such proteinuria does not mean the onset of acute or progression of existing kidney disease (see section "Side effects"). The incidence of serious renal impairment increases with 40 mg of rosuvastatin. It is recommended to monitor indicators of renal function during therapy with Mertenil.
From the musculoskeletal system
When using the drug Mertenil in all dosages, and especially when taking the drug in a dose exceeding 20 mg, myalgia, myopathy and, in rare cases, rhabdomyolysis were detected. Very rarely, rhabdomyolysis occurred while taking ezetimibe and HMG-CoA reductase inhibitors. In this case, the pharmacodynamic interaction of drugs cannot be ruled out, therefore, Mertenil and ezetimibe should be used together with caution (see the section "Interaction with other drugs").
The incidence of rhabdomyolysis increases with 40 mg of rosuvastatin.
Determination of creatine phosphokinase
The determination of CPK activity should not be carried out after intense physical exertion or in the case of another alternative cause causing an increase in CPK, as this may complicate the interpretation of the results. With an increase in the activity of CPK before the start of therapy, more than 5 times higher than the upper limit of the norm, a second measurement should be carried out in 5-7 days. If repeated measurement confirms the initial CPK value (5 times higher than the upper limit of the norm), therapy with Mertenil should not be started.
Before starting therapy
Mertenil, like other HMG-CoA reductase inhibitors, should be used with extreme caution in patients with existing risk factors for myopathy / rhabdomyolysis. These factors include:
Renal failure; hypothyroidism; personal or family history of muscle disease; a history of myotoxicity while taking other HMG-CoA reductase inhibitors or fibrates; alcohol abuse; age over 70; conditions accompanied by an increase in the concentration of the drug in the blood plasma (see sections "Dosage and Administration", "Interaction with other drugs" and "Pharmacokinetics"); simultaneous reception of fibrates.
In such patients, the risk-to-benefit ratio of therapy should be assessed and clinical observation should be carried out throughout the course of therapy. You should not start treatment in case of a significant increase in the initial CPK value (5 times higher than the upper limit of the norm).
During therapy
It is recommended to inform patients about the need to immediately inform the doctor about cases of sudden onset of muscle pain, muscle weakness or spasms, especially in combination with malaise or fever!
In such patients, it is imperative to monitor the activity of CPK. Treatment should be discontinued if the CPK activity is more than 5 times the upper limit of the normal or if muscle symptoms are pronounced and cause daily discomfort throughout the day (even if the CPK activity is 5 times less than the upper limit of the normal). If symptoms disappear and CPK activity returns to normal, consideration should be given to re-prescribing Mertenil or prescribing an alternative HMG-CoA reductase inhibitor in lower doses with close monitoring of the patient. Regular monitoring of CPK activity in patients without symptoms of rhabdomyolysis is inappropriate.
There have been very rare cases of immune-mediated necrotizing myopathy, clinically manifested by persistent proximal muscle weakness and increased serum creatine kinase activity, during treatment or after stopping treatment with statins, including rosuvastatin. Additional studies of the muscular and nervous system, serological studies, and therapy with immunosuppressive drugs may be required.
However, an increase in the number of cases of myositis and myopathy was found in patients who took other inhibitors of HMG-CoA reductase in conjunction with fibric acid derivatives, including gemfibrozil, cyclosporine, lipid-lowering nicotinic acid, antifungals of the azole group, protease inhibitors and macrolide antibiotics. Gemfibrozil increases the risk of myopathy when combined with certain HMG-CoA reductase inhibitors. Therefore, the simultaneous administration of rosuvastatin and gemfibrozil is not recommended. The risk-to-benefit ratio should be carefully assessed when rosuvastatin is used together with fibrates or nicotinic acid in lipid-lowering doses (more than 1 g). The simultaneous administration of rosuvastatin at a dose of 40 mg and fibrates is contraindicated (see the sections "Interaction with other medicinal products" and "Side effects").
Mertenil should not be administered to patients with acute, severe diseases suggesting myopathy, or with the possible development of secondary renal failure associated with rhabdomyolysis (for example: sepsis, arterial hypotension, surgery, trauma, severe metabolic syndrome, uncontrolled convulsions, endocrine disorders, electrolyte disturbances (see the section "With care").
Effects on the liver
Like other inhibitors of HMG-CoA reductase, Mertenil should be used with extreme caution in patients who abuse alcohol or have a history of liver disease.
It is recommended to determine the indicators of liver function before and 3 months after the start of treatment. If the activity of "hepatic" transaminases in the blood serum is 3 times higher than the upper limit of the norm, you should stop taking the drug Mertenil or reduce the dose taken (see section "Dosage and Administration"). The frequency of severe liver dysfunctions (associated mainly with an increase in the activity of "hepatic" transaminases) increases with the intake of 40 mg of the drug.
In patients with secondary hypercholesterolemia due to hypothyroidism or nephrotic syndrome, therapy for the underlying disease should be carried out before starting treatment with Mertenil.
Race
In the course of pharmacokinetic studies, an increase in the systemic concentration of rosuvastatin among patients of the Mongoloid race was revealed in comparison with the data obtained among patients - representatives of the Caucasian race (see sections "Dosage and Administration", "Contraindications" and "Pharmacokinetics").
HIV protease inhibitors
In the course of co-administration of rosuvastatin and a combination of various HIV protease inhibitors with ritonavir, an increase in the systemic exposure of rosuvastatin is observed. It is necessary to carefully evaluate both the benefits of reducing the concentration of lipids in the blood while taking rosuvastatin, and take into account the possible increase in the concentration of rosuvastatin in the blood plasma at the beginning of treatment and during the period of increasing the dose of the drug in patients with HIV taking HIV protease inhibitors. Concomitant administration with HIV protease inhibitors is not recommended without dose adjustment of rosuvastatin (see sections "Dosage and Administration" and "Interaction with other drugs").
The drug contains lactose, so it should not be taken by patients with rare hereditary diseases such as galactose intolerance, Lapp lactase deficiency or glucose-galactose malabsorption syndrome.
Interstitial lung disease
With the use of some statins, especially for a long time, isolated cases of interstitial lung disease have been reported (see section "Side effects"). Symptoms include shortness of breath, unproductive cough, and deterioration in general well-being (weakness, weight loss, and fever). If interstitial lung disease is suspected, statin therapy should be discontinued.
Type 2 diabetes mellitus
There is evidence that statins, as a class of drugs, cause an increase in the concentration of glucose in the blood and in some patients at high risk of developing diabetes mellitus in the future they can provoke the level of hyperglycemia at which standard diabetes treatment is indicated. However, this risk is outweighed by the reduced risk of developing vascular complications, so there is no reason to discontinue statin treatment. In patients at risk of hyperglycemia (fasting glucose concentration from 5.6 to 6.9 mmol / L, BMI\u003e 30 kg / m2, increased triglyceride concentration, arterial hypertension), clinical and biochemical parameters should be monitored in accordance with national recommendations.
Children and adolescents from 10 to 17 years old
It is known that the effect of rosuvastatin on height, body weight, BMI and the development of secondary sexual characteristics according to the Tanner scale in children and adolescents aged 10 to 17 years was assessed only for one year.
Impact on the ability to manage vehicles and to work with mechanisms
Studies to study the effect of the drug Mertenil on the ability to drive vehicles and work with mechanisms have not been carried out. However, based on the pharmacodynamic properties of the drug, it can be assumed that Mertenil should not have such an effect. At the same time, when driving vehicles or other mechanisms, it must be borne in mind that dizziness may occur during treatment.
Release form
10 film-coated tablets in a blister of PA / Al / PVC film and aluminum foil.
3 blisters in a cardboard box with instructions for use.
Storage conditions
Store at a temperature not exceeding 30 ° C, in the original packaging to protect from light. Keep out of the reach of children!
Shelf life
Do not use after the expiration date printed on the package.
Terms of dispensing from pharmacies
On prescription.
Manufacturer
Mertenil is a drug for lowering cholesterol levels - this is how it can be described in a simple way. It is used as an addition to the diet (not a substitute for it!) In the treatment of hypercholesterolemia and mixed dyslipidemic conditions. The active ingredient - rosuvastatin calcium - reduces the high content of low-density lipoprotein cholesterol, total cholesterol and triglycerides. Rosuvastatin is a selective, competitive inhibitor of HMG-CoA reductase, an enzyme that converts 3-hydroxy-3-methylglutaryl coenzyme A to mevalonate, a cholesterol precursor.
The effectiveness of the drug has been clinically proven for adult patients with hypercholesterolemia. After oral administration, the maximum concentration of rosuvastatin in blood plasma is reached after approximately 5 hours. The bioavailability of the active substance is approximately 20%. The therapeutic effect of Mertenil can be achieved within one week after the start of treatment, after 2 weeks 90% of the maximum possible effect is achieved. The maximum therapeutic effect is achieved after 4 weeks and is maintained with further administration of Mertenil tablets.
The drug is effective in the treatment of adult patients with hypercholesterolemia with or without symptoms of hypertriglyceridemia, as well as in the treatment of patients with diabetes mellitus or a hereditary form of the disease.
The active substance is effective for the treatment of patients with Fredrickson type IIa and IIb hypercholesterolemia (average baseline LDL-C level of about 4.8 mmol / l). In 80% of patients who received 10 mg of the active substance, the target values \u200b\u200bof the LDL cholesterol level (less than 3 mmol / l) were achieved.
Indications for use
What does Mertenil help from? Tablets are prescribed to patients with the following pathological conditions:
- Increased blood cholesterol;
- Hereditary hypercholesterolemia;
- Hypertriglyceridemia in the composition complex therapy together with a diet;
- High risk of atherosclerotic deposits on the walls of large blood vessels;
- Prevention of the development of pathologies from the cardiovascular system in obese patients, arterial hypertension, recently suffered a stroke or heart attack;
- Hypertriglyceridemia (Fredrickson type IV) as an adjunct to diet.
- The age of patients is over 60 years old, who, moreover, are overweight.
Instructions for use Mertenil, dosages
It is important to follow a therapeutic diet and consume products with a low cholesterol content before using Mertenil. If the rules of nutrition are not followed, the therapeutic effect is significantly reduced, so the diet must be followed during the entire period of treatment. Doses of the drug are selected individually in accordance with the purpose of the treatment and the patient's therapeutic response, taking into account the current generally accepted recommendations for target lipid levels.
Mertenil tablets are taken orally, regardless of food, swallowing whole and drinking water. The recommended starting dose is 5 mg or 10 mg once a day. Cholesterol levels, the possible risk of cardiovascular complications and the potential risk of side effects in each individual patient should be considered when choosing an initial dose. If necessary, dose adjustments can be made after 4 weeks.
After a month of taking the minimum dose, according to laboratory tests, the doctor can leave the dosage unchanged or increase, in proportion to the indicators.
The dosage is 40 mg / day. it is prescribed only in cases of extreme necessity, with low efficacy of lower doses, as well as in patients with severe hypercholesterolemia and an increased risk of developing diseases of the cardiovascular system.
Contraindications and side effects
The main contraindications to the use of Mertenil:
- Pregnancy and lactation, as well as women of childbearing age who do not use reliable contraception;
- Against the background of a predisposition to the development of myotoxic complications;
- With myopathy;
- Simultaneously with cyclosporine and fibrates;
- Against the background of liver failure;
- Against the background of hypersensitivity to the components (active or auxiliary) of the drug, as well as with lactose intolerance and lactase deficiency, or glucose-galactose malabsorption;
- With severe renal dysfunction;
- In pediatrics up to 18 years old.
According to the instructions for use, Mertenil 40 mg tablets are contraindicated to take against the background of: Hypothyroidism and liver diseases occurring in the active phase. Excessive alcohol consumption. Personal or family history of muscle disease.
With caution, Mertenil is prescribed against the background of severe metabolic, endocrine or electrolyte disorders, the risk of myopathy. With uncontrolled epilepsy and liver disease. Elderly age, trauma and surgery.
Overdose
Strengthening of side effects, their possible manifestation in the absence of normal dosages.
There is no specific treatment for an overdose of Mertenil. Symptomatic therapy is recommended. Liver function and the degree of CPK activity should be monitored. Hemodialysis is ineffective.
Side effects
The most common side effects of Mertenil are:
- the development of type II diabetes mellitus;
- asthenic syndrome;
- headache;
- constipation;
- myalgia;
- nausea;
- dizziness;
- stomach ache.
It is extremely rare that a rash and itchy skin, myopathy, rhabdomyolysis, develop pancreatitis. With regular intake of 40 mg Mertenil tablets, myalgia, proteinuria and myopathy may develop. There is a risk of an increase in the concentration of bilirubin and glucose, as well as a malfunction of the thyroid gland.
Side effects in many cases, they depend on the dosage of the drug. So the instructions for the use of Mertenil must be followed strictly, exceeding the dosage is unacceptable. If you missed the time of taking the drug, take it at the next scheduled hour.
If you experience unexpected muscle pain or muscle weakness, accompanied by general malaise and fever, stop taking the medication immediately and see your doctor.
Analogues of Mertenil, list of drugs
The drug is a generic rosuvastatin, therefore the complete structural analogs of Mertenil are active substance are the following drugs, list:
- Suvardio.
- Rosucard.
- Acorta.
- Ro-statin.
- Tevastor.
- Roxer.
- Rosulip.
- Rosart.
- Crestor.
- Rosuvastatin.
- Rustor.
- Rosistark.
Important - instructions for the use of Mertenil, the price and reviews do not apply to analogues and cannot be used as a guide to the use of drugs of similar composition or action. All therapeutic appointments must be made by a doctor. When replacing Mertenil with an analogue, it is important to consult a specialist, you may need to change the course of therapy, dosages, etc. Do not self-medicate!
Effective overcoming of hypercholesterolemic conditions is possible only with an integrated approach - dietary food with a reduced fat and salt content, physical activity and taking medications recommended by the attending physician.