First aid for burns. First aid for burns. Determination of the affected area
Burns are thermal- caused by fire, steam, hot objects and substances, chemical- acids and alkalis, and electrical- exposure to electric current or electric arc. According to the depth of the lesion, all burns are divided into four degrees: I - redness and swelling of the skin; II - water bubbles; III - necrosis of the superficial and deep layers of the skin; IV - charring of the skin, damage to muscles, tendons and bones.
If clothing on the victim caught fire, you need to quickly throw a coat over him, any thick fabric or knock down the flame with water. You cannot run in burning clothes, since the wind, fanning the flame, will increase and intensify the burn.
When providing first aid to the victim, in order to avoid infection, do not touch the burned areas of the skin with your hands or lubricate them with ointments, fats, oils, petroleum jelly, sprinkle with baking soda, starch, etc. Do not open bubbles, remove mastic, rosin or other resinous substances adhering to the burned area, since by removing them, you can easily peel off the burned skin and thereby create favorable conditions for wound infection.
For small-area burns of I and II degrees, a sterile bandage should be applied to the burned area of the skin.
Clothes and shoes from the burnt place must not be torn off, but must be cut with scissors and carefully removed. If pieces of clothing stick to the burned area of the body, then a sterile bandage should be applied over them and the victim should be sent to a hospital.
In case of severe and extensive burns, the victim must be wrapped in a clean sheet or cloth, without undressing him, covered and given warm tea, to create peace until the doctor arrives.
The burnt face must be covered with sterile gauze.
In case of eye burns, cold lotions should be made from the solution. boric acid(half a teaspoon of acid in a glass of water) and send the victim to a doctor immediately.
CHEMICAL BURNS
In case of chemical burns, the depth of tissue damage depends on the duration of exposure to the chemical. It is important to reduce the concentration of the chemical and the time of exposure as soon as possible. To do this, the affected area is immediately washed with a large amount of running cold water from the tap, from a rubber hose or bucket for 15-20 minutes.
If acid or alkali gets on the skin through clothing, then first rinse it off with water, and then carefully cut and remove the wet clothing from the victim, and then rinse the skin.
If sulfuric acid or alkali in the form of a solid comes into contact with the human body, it is necessary to remove it with dry cotton wool or a piece of cloth, and then rinse the affected area thoroughly with water.
With a chemical burn, it is not possible to completely wash off the chemicals with water. Therefore, after washing, the affected area must be treated with appropriate neutralizing solutions used in the form of lotions (bandages).
Further assistance for chemical burns is provided in the same way as for thermal ones.
BURNS WITH ACIDS AND ALKALI
In case of skin burns with acid, lotions (dressings) are made with a solution of baking soda (one teaspoon of soda per glass of water).
If acid in the form of liquid, vapors or gases gets into the eyes or mouth, rinse them with plenty of water, and then with a solution of baking soda (half a teaspoon per glass of water).
In case of skin burns with alkali, lotions (dressings) are made with a solution of boric acid (one teaspoon of acid per glass of water) or a weak solution of acetic acid (one teaspoon of vinegar per glass of water).
If splashes of alkali or its vapors get into the eyes and mouth, it is necessary to rinse the affected areas with plenty of water, and then with a solution of boric acid (half a teaspoon of acid in a glass of water).
If solid pieces of the chemical get into the eye, they must first be removed with a damp swab, as rinsing the eyes can injure the mucous membrane and cause additional injury.
If acid or alkali enters the esophagus, an urgent need to call a doctor. Before his arrival, you should remove saliva and mucus from the victim's mouth, put him in warmth, cover, and put “cold” on his stomach to relieve pain.
ELECTRIC SHOCK
In case of electric shock, it is necessary to release the victim from the action of the current as soon as possible, since the severity of the electric shock depends on the duration of the electric shock. This must be done carefully, in compliance with safety measures.
In all cases, the caregiver should not touch the victim who is under the influence of electric shock, without proper precautions, as this is life-threatening.
In all cases of electric shock, calling a doctor is mandatory, regardless of the condition of the victim. In the absence of an opportunity to quickly call a doctor, it is necessary to
urgently deliver the victim to a medical institution, providing for this the necessary vehicles or a stretcher.
If the victim is conscious, but before that he was in a state of fainting, he should be laid in a comfortable position (spread under him and covered with something from clothes on top) and, until the doctor arrives, ensure complete rest, continuously observing breathing and pulse.
If the victim is unconscious, but with a stable breathing and pulse, he should be laid flat and comfortably, unbuttoned his clothes, create an influx of fresh air, give ammonia to sniff, spray his face with water and ensure complete rest. If the victim does not breathe well - very rarely and convulsively - he should do artificial respiration and indirect (external) heart massage.
In case of electric shock, death is often clinical ("imaginary"), so you should never refuse to provide assistance to the victim and consider him dead due to lack of breathing, heartbeat, pulse. Only a doctor has the right to decide on the expediency or uselessness of measures to revive the victim and to make a conclusion on his death.
Send your good work in the knowledge base is simple. Use the form below
Students, graduate students, young scientists who use the knowledge base in their studies and work will be very grateful to you.
Posted on http://www.allbest.ru/
Posted on http://www.allbest.ru/
4 Federal State Treasury
educational institution of higher vocational education"St. Petersburg University of the Ministry of Internal Affairs of Russia"
Department of Forensic Science
Faculty of Investigative Workers Training
In the discipline "First Aid"
Theme: Burn.Views, the firsthelp andcontraindications for burns.
Completed:
Snisar Vyacheslav Andreevich
Checked:
Galtsev Yuri Viktorovich
St. Petersburg 2015
- Introduction
- 1. Thermal burns and first aid
- 2.
- 3.
- 4. Chemical burns and first aid
- 5. Contraindications for burns
- 6. Prevention and treatment of burns
- Conclusion
- Bibliography
Introduction
A burn is tissue damage resulting from local thermal, chemical, electrical, or radiation exposure.
Burns most often affect the skin (its volume is almost one-sixth the volume of the entire human body). This is not surprising, since it is the skin, performing a lot of functions in the body, protecting us, and is the first to meet many aggressors, including thermal effects. Peripheral skin is continuously dying epidermis. This feature of the skin "shedding" seems to be very important, since it causes, among other things, an increased ability to regenerate (restore). Sweat and sebaceous glands, especially hair follicles(follicles) determine the regeneration potential of the skin; their number and development affect the nature and degree of healing of burns.
Burns can be caused by flames, boiling water, steam, various chemicals: acids, alkalis; some medicines: iodine, ammonia; electric current, radioactive substances, sunlight, etc.
Depending on the cause of the burndistinguish between:
thermal, radiation, light, electrical, chemical, phosphoric.
Depending on the depth of tissue damage, burns of four degrees are distinguished:
Burns of the 1st degree - characterized by redness and swelling of the skin, burning sensation and pain in the affected area. After 4-5 days, skin peeling and recovery are noted;
· 2nd degree burn - accompanied by the appearance on the reddened and edematous skin of blisters filled with a transparent yellowish liquid. The burned area of the skin is sharply painful. When the blisters rupture or are removed, a painful, bright red surface is visible. In case of favorable, without suppuration, the course of the burn heals without scarring within 10-15 days;
A third degree burn - can be with damage to the skin itself throughout its entire thickness (III A degree) or with damage to all layers of the skin (III B degree). A gray or black scab forms on the skin. The dead skin areas are gradually separated, suppuration is noted, a sluggish healing wound is formed;
· 4th degree burn - manifested by the necrosis of not only the skin, but also the deep-lying tissues (fascia, muscles, bones).
1. Thermal burns and first aid
Thermal burns arise from exposure to high temperatures. In a combat situation, they can be observed from the effects of napalm, other fire mixtures, incendiary bombs, shells, clothing ignition, etc. In peacetime thermal burns can be due to careless handling of fire, hot water, non-observance of safety rules at work. Thermal burns are most often observed on the skin, but there may be burns to the eyes, mucous membranes of the mouth, pharynx, esophagus and even stomach.
Boiling water burn characterized in that the possible temperature is 100 ° C or slightly more. This circumstance, combined with the fact that fluids cool on the way to the skin, leads to the fact that the lesions caused are superficial.
Steam burn. Some features have burns caused by the action of water vapor, especially used in industry. In the latter case, it can be overheated (under pressure), which means that its temperature is 120 ° C and a continuous defeat of large areas is possible. It is even worse if the burn is caused by the steam of boiling alkalis or other aggressive chemical solutions. Hot bitumen, resins, glue adhere tightly to the skin, transferring the entire supply of heat to the skin. They cannot be shaken off, wiped off, so their validity period is always long. Appearance from bitumen burns, especially if the face is affected, frightening: a black tar film gives the impression of a deep skin lesion.
First aid rules: removal of bitumen from the skin is difficult, time-consuming and requires solvents. It is not necessary to do this when providing first aid. It is enough to free the mouth, nose, eyes, ears.
Flame burns. The most severe burns are caused by flames, especially if burning clothes are saturated with kerosene, gasoline, or alcohol. Ignition of clothing leads to severe burns if it is not removed from the victim due to loss of consciousness or due to helplessness (children, old people; people in a state of alcoholic intoxication, poisoning).
First aid rules: the longer the clothes burn, the more the degree of burn will be afterwards, the more percent of the skin surface will be damaged. If the clothes are on fire - in no case run - it will flare up even more. First of all, you must try to throw it off or roll it on the floor until the flame goes out. If you want to help a burning man, pour it over cold water, throw sand or throw a coat, bedspread, tarpaulin over it (it is necessary to block the flame from access to air). A person in burning clothes should not be wrapped upside down, as this can lead to defeat respiratory tract and poisoning with toxic combustion products. However, keep in mind that when burning clothing is pressed against the skin, the heat will last longer and, therefore, a deeper burn is possible. To prevent this, the draped cloth must be removed immediately after the flame has been extinguished.
To reduce the time for fabrics to overheat and prevent severe burns, after extinguishing the fire, pour cold water over the burn or cover with snow for 15-20 minutes. This reduces pain and prevents tissue swelling.
The surface of the burn is thoroughly cleaned to prevent infection. An ointment containing an antibiotic and protecting from the external environment is applied to the damaged surface. Then it is necessary to apply a sterile gauze bandage or from any also sterile tissue that is at hand (handkerchief, cloth napkin, etc.). The surface of the burn can only be covered with non-stick material or sterile gauze. The gauze is removed after soaking in water. The victim needs to drink more fluids.
Before the arrival of an ambulance, the victim may have chills, then he needs to be warmed: cover with a warm blanket, and give any alcohol-containing food liquid to drink to relieve pain shock. If necessary, tetanus vaccination is carried out.
If your hands are burned, then in the first days it is necessary to keep them in a raised position, which reduces swelling and pain.
Molten metal burns. Molten metal burns are almost always deep, they often happen in production (metallurgical plants). The combination in the molten metal is high temperature and physical properties liquid creates opportunities for the greatest contact with the skin surface. The temperatures of molten metals fluctuate between 800-1500 ° C, therefore, with such burns, tissues located deeper than the skin (muscles, tendons, bones) also suffer.
First aid rules for thermal burns of the retina: It is necessary to rinse the eyes with water, drip a 20% sodium sulfacyl solution into the eyes; 0.25% solution of chloramphenicol; 0.02% furacilin, put 1-5% synthomycin emulsion behind the eyelid; 1% tetracycline ointment; 1% erythromycin ointment, lubricate the wound surface of the skin with antibiotic ointment. Apply an aseptic bandage.
2. Electrical burns and first aid
Electrical burns occur when an electric current is passed through a person's tissues or due to the resulting heat. Electrical and chemical burns require special attention. The severity of tissue damage from an electrical burn is difficult to assess because internal damage can be much more serious than it might initially appear. Electric burns that ignite clothing can also lead to thermal burns.
First aid:
The main thing is to take the victim out of the zone of exposure to the current - to de-energize the source of injury or try to drag the person away with the help of any object that does not conduct an electric current, so as not to get an electric shock yourself. Then:
1. Immediately turn off the electricity - unscrew the plugs or pull out the plug, or turn off the electricity completely.
2. If necessary, help yourself with a broomstick or wooden chair while standing on a dry rubber mat, book, or folded newspaper to move the victim away from the electrical appliance or wire.
3. If an electrical burn causes dangerous heart rhythm disturbances or cardiac or respiratory arrest, resuscitation should be initiated immediately.
4. When the victim is safe, check their breathing and pulse.
5. If necessary, artificial respiration and chest compressions.
6. Lay the victim on their side if unconscious.
7. Treat burns at points where electric current entered and exited the body by cooling them with water. Never pour water while the victim is still touching the electrical wire.
8. Apply a sterile or clean wipe and bandage.
With regard to high voltage electrical wires, contact with them, for example with a high voltage line, is usually fatal for the victim. You too can be electrocuted if you are 18 meters or less from the source. Do not allow approach to the victim and other people and call the law enforcement authorities immediately.
3. Sunburn and first aid
Sunburn occurs when you are in the sun for too long. They are accompanied by heatstroke. In this case, the normal heat regulation of the body is disrupted and the body temperature rises. The victim develops lethargy, redness of the face, profuse sweating, headache, coordination of movements is impaired. In more severe cases, breathing becomes more frequent, the face turns pale, and loss of consciousness occurs. With a sunburn of open areas of the skin, uneven redness of the skin, burning and pain when touched is observed, on the second day - itching and pain. After 5-10 days, the skin begins to become covered with watery blisters and peel off.
First aid:
First, the victim must be transferred to a shady, cool place, take off his clothes, moisten his head and chest, take a cold or cool shower. If there is no breathing or severe weakness, give artificial respiration.
Secondly, you need to drink plenty of fluids (tea, milk, fruit drink) to restore the balance of water in the body.
Thirdly, among the first aid methods for severe sunburns, lubricate the skin with boric petroleum jelly or make a compress from a calendula solution. For a compress, it is necessary to dilute the calendula tincture in cold water in a ratio of 1:10.
Fourth, if the temperature rises, you need to drink any antipyretic agent, for example, aspirin.
If the victim has a massive burn, a doctor should be called. The doctor will administer an anesthetic and prescribe treatment.
4. Chemical burns and first aid
Chemical burns occur when concentrated acids, alkalis, phosphorus come into contact with the skin, this happens in industry, agriculture, in everyday life: detergents, cleaning products, etc.
The first help:
First, remove chemical-soaked clothing before giving first aid.
Secondly, in case of chemical burns, regardless of the substance that caused them, the damaged parts of the body are exposed to a stream of water for 10-15 minutes. At the same time, the concentration of the chemical decreases, and it is mechanically removed from the surface of the body. An exception is quicklime, which, when combined with water, generates a lot of heat, therefore, parts of the body that have been burnt with quicklime should not be washed with water, they should be greased with some kind of fat, then a bandage with zinc or boric ointment should be applied and sent to a doctor.
Thirdly, you need to know that first aid for chemical burns includes neutralizing the action of chemicals. If you get acid burns, wash the damaged area with soapy water or 2% baking soda solution (this is 1 teaspoon of baking soda in 2.5 cups of water) to neutralize the acid. If you burn yourself with alkali, then wash the damaged area of the skin with a 1-2% solution of boric or acetic acid. The process takes 15-20 minutes.
Fourth, apply a dry gauze bandage and see a doctor. But if suddenly you conducted experiments with phosphorus and as a result of its contact with the skin got a burn, then it can be neutralized with a 5% solution of copper sulfate (copper sulfate), and immediately consult a doctor.
In case of chemical burns of the eyes or mucous membrane of the mouth, throat, they should be rinsed with water, and then, in case of burns with alkali, neutralized with a 1% solution of boric acid; for acid burns - 1% soda solution. Neutralization of chemicals that have entered the eye should be carried out for a long time, sometimes for an entire hour or more, until the opacity of the cornea passes and the vision that has disappeared from the moment of the burn returns to the victim. After that, 1-2 drops of sterile petroleum jelly or sunflower oil are instilled into the eyes, a bandage is applied and sent to a specialist.
burn chemical electrical medical
5. Contraindications for burns
Do not apply natural ice to burnt skin, as this can lead to the death of skin cells and not regenerate in the future. Do not treat the skin with alcohol, cologne. Do not pierce the resulting blisters (they protect the wound from infection). Do not tear off the parts of clothing adhering to the burn site, touch the burned area with your hands (this leads to the penetration of infection). The victim should not be allowed to move independently (shock is possible). Do not spray bubbles and charred skin with water. Do not lubricate burns with egg yolk, fat, brilliant green, a strong solution of potassium permanganate, cover with powders, sunflower oil, lard, ointments, etc. (this will complicate further treatment, as well as contribute to the contamination of the burned surface and the further development of pus).
6. Prevention and treatment of burns
Bandage method
Protects the burned area from contamination and external influences (mechanical injury, cooling), well absorbs purulent discharge, reduces the evaporation of water from the wounded surface. It is necessary in case of damage to the contacting surfaces of the body, circular burns of the trunk and extremities. Without bandaging, transportation of the burned is impossible. When using the closed method, optimal conditions are created for local drug treatment burn wounds. Under the bandage, the increased activity of wound proteases is maintained, providing enzymatic melting of dead tissues. The closed method of treatment can be used both in a hospital and in an outpatient practice. Its disadvantages are laboriousness, high consumption of dressings, soreness of dressings; squeezing the skin, direct contact with a thermal factor, impair its protective properties.
Bandagelessmethod
Devoid of these shortcomings. Acceleration of the formation of a dense scab on the burnt surface under the influence of the drying effect of air, ultraviolet irradiation or lubrication of the burn wound with some coagulating protein substances helps to reduce the intoxication (poisoning) of the victim with the decay products of dead tissues. With open treatment, it is possible to constantly monitor the changes occurring in the burn wound and the effectiveness of medical procedures. The use of concentrated solutions of tanning, coagulating and dyes (tannin, silver nitrate, aniline dyes, ferric chloride, saturated solution of potassium permanganate - "potassium permanganate") for the formation of a scab in the open treatment of burns makes it difficult to diagnose the depth of the lesion.
Open treatment deep burns does not prevent the development of purulent inflammation in the wound. Superficial burns of the II-III degree with an open method of treatment heal on their own. There was no significant difference in the healing time and the incidence of complications with open and closed methods of treating superficial burns. They need to be used depending on the patient's condition, the conditions in which the treatment is carried out, the localization and depth of the burn, the stage of the process.
The open method should be used mainly for burns of the face, genitals, perineum, where dressings impede care and physiological functions. However, its use does not mean a complete rejection of dressings for burns and these localizations. Open treatment is used for multiple residual small wounds that heal slowly under the bandage and therefore prolong the healing period for a long time. A burn wound left open 3-4 times a day is lubricated with any ointment containing antibiotics or antiseptics (Silvederm, Betadine, Dermazin)
Conclusion
A burn injury is not only local tissue damage in the area of action of the damaging agent, but also a complex reaction of the body to the damage received. The consequences of a burn injury can be divided into three large groups: burn disease, endogenous intoxication syndrome, and burn infection with burn sepsis.
Burn disease
Burn disease is a complex response of the body to burn injury. This condition occurs with superficial burns, if they occupy more than 30% of the body in adults; with deep burns (3-4 degrees) - more than 10% of the body in adults and 5% in children; in weakened persons with concomitant diseases, it can develop with deep burns of 3% of the body surface. There are four main stages of development:
1. Burn shock... Lasts 12-48 hours, in severe cases - up to 72 hours. Burn shock by the mechanism of occurrence is hypovolemic, it is primarily a violation of microhemodynamics as a result of pathological redistribution of blood circulation.
2. Acute burn toxemia... Lasts until infection in wounds occurs from 3 to 12 days, more often - 8-9 days. It arises as a result of the entry into the blood of the decay products of tissues that have undergone a burn.
3. Burnseptic tank toxemia... The stage from the moment of the appearance of suppuration in the wounds to the moment of their healing or surgical treatment. Lasts from several weeks to several months. It is the body's response to the vital activity of the microflora that develops in the wound.
4. Recovery... It starts after the burn wounds have healed and closed. The wound is cleaned (independently or surgically), the bottom of the wound is covered with granulations or epithelialized, depending on the depth of the lesion.
Also, burn disease can be aggravated by various complications, which are divided into local and general, primary and secondary, early and late. As a result of these complications, lymphadenitis, purulent cellulitis, abscesses, gangrene of the extremities can develop.
Endogenous intoxication syndrome
Endogenous intoxication syndrome is a complex of symptoms that develops as a result of the accumulation of catabolic products, the level of which increases due to insufficient liver and kidney function, overloaded with the processing and elimination of decay products of damaged tissues.
Burn infection and burn sepsis
A burn injury stimulates all links of immunity, but the accumulation of tissue decay products and massive bacterial aggression through damaged skin leads to the depletion of all links of the immune defense, and secondary immunodeficiency is formed. The body becomes vulnerable to the surrounding microflora.
Bibliography
1. First aid for life-threatening conditions: a practical guide / ed. prof. Yu.V. Galtseva. SPb .: Publishing house of St. Petersburg University of the Ministry of Internal Affairs of Russia, 2013. - 88 p.
2. Military medical training. Tutorial for medical schools. M .: Medicine, 2010.
3. First aid; Popular encyclopedia. Ch. editor acad. RAMS V.I. Pokrovsky. M .: Great Russian Encyclopedia. 2012.254 p.
4. Belov V.I. Encyclopedia of Health. M .: "Chemistry", 2005.
5.http: //primamunc.ru/public/article/article-0020.shtml
Posted on Allbest.ru
...Similar documents
A burn as damage to body tissues caused by high temperatures or the action of certain chemicals is one of the most common traumatic injuries in the world. The concept and types of injuries. Principles and rules of first aid.
presentation added on 04.24.2014
Rendering first medical care to the victim. A person is struck by electric shock or lightning. Features of rendering first aid to the victim with thermal and chemical burns. The course and severity of burns. Signs and symptoms of frostbite.
presentation added 04/27/2016
Causes of occurrence, degree and main signs of chemical burns. Features of chemical burns of eyes, esophagus and stomach. Rules for working with acids and alkalis. First aid for getting a chemical burn. Preventive measures for chemical burns.
test, added 05/14/2015
Brief medical characteristic wounds and bleeding, first aid for them. The scheme of providing emergency care for arterial bleeding. Burn classification and first aid. Signs of limb and spine fractures, assistance.
test, added 01/31/2010
Actions for respiratory arrest and cardiac arrest, drowning, injury and bleeding. Protection of the wound from secondary contamination (infection). Bruises, sprains and ligament ruptures. First aid for head injuries, thermal and chemical burns.
abstract, added 05/24/2009
Signs and symptoms of thermal burns, the need to call an ambulance. First aid for wounds and bleeding, the rules for applying a tourniquet. Assistance to the victim in case of frostbite, hypothermia, poisoning, the rules for its transportation.
presentation added 09/09/2013
Occupational safety and health. Types of effects of electric current on the human body. Types of briefings, the order of their conduct. The first first aid with thermal, chemical, electrical burns. Combustion; fire and explosion hazardous substances.
test, added 12/27/2008
First aid for bleeding. Emergency care for sudden cardiac arrest. First aid for injuries, concussions and bruises of the brain, fractures of the ribs, sternum, clavicle and scapula, traumatic shock, thermal burns, frostbite.
abstract, added 06/11/2004
First aid measures for bruises, sprains, dislocations, organ damage abdominal cavity... Types of wounds and their characteristics. First aid for burns, frostbite, heat and sunstroke. Diseases and their causative agents, methods of transmission.
term paper, added 08/19/2013
Acquaintance with the peculiarities of first aid for burns, frostbite, electric shock, drowning, suffocation, ground cover. Description of the methods of careful transportation of the victim to the hospital.
Burns in most cases are caused by exposure to high temperatures. Such burns are called thermal burns. There are three degrees of these burns: mild, moderate and severe.
In addition, careless handling of alkalis and acids can lead to chemical burns. Ultraviolet radiation the sun can cause sunburn.
Providing first aid for thermal burns, you must:
- - remove the source of the burn from the surface of the body;
- - cool the burnt surface with ice packs (cold water) for 5-10 minutes;
- -- healthy skin treat the burn with a solution of alcohol (brilliant green, potassium permanganate);
- - apply a sterile bandage;
- - if necessary, give the victim an anesthetic; - deliver the victim to a hospital.
Unacceptable: Removal of remnants of clothing, dirt from damaged skin; burn treatment with alcohol, iodine, fat, ointments, powders; the imposition of tight bandages.
In case of sunburn, the skin should be lubricated with a moisturizer (yogurt, kefir). You can apply cold lotions.
In case of contact with the skin of alkali or acid, it is necessary:
- - take off clothing soaked in the chemical;
- - rinse the skin with running water;
- - wash the damaged area (for burns with alkali - 1-2% solution of acetic acid, for burns with acid - 2% solution of baking soda);
- - give the victim an anesthetic and send him to a hospital.
Prevention of burns consists in observing the rules of fire safety, handling acids and alkalis, taking safety measures when being in places where high temperatures are used and aggressive environments are used (hot production, chemical enterprises, research institutions), when carrying out welding, forging, soldering work and at home. To avoid sunburn, you should strictly dose the duration of sunbathing and refrain from taking them on days of increased sun activity.
First aid for a burn depends on its type and degree of damage.
There are burns: thermal (exposure to flame, steam, hot liquid and metal objects); electrical (electric shock);
chemical (aggressive substances).
To assess the degree of burns, a classification is usually used,
providing for the I - IV degree of damage:
I degree - pain, skin redness, swelling;
II degree - pain, skin redness, swelling, blisters;
III degree - large blisters with bloody fluid, gray or yellowish scabs;
IV degree - brown or black dense scabs, charring of the skin, muscles, tendons, bones.
With a burn of III - IV degree, which covers 10 - 40% of the skin surface, burn shock occurs. An IV degree burn with an area of 50% or more is fatal
Thermal burn
Do not allow the person on whom the clothing caught fire to run.
The wind blows up the flames and intensifies the burn. Throw a tarp, coat or blanket over the victim, try to knock down the flames with water or sand.
Move the victim out of the fire area. Do not touch the burned area of the skin, lubricate it with ointments, fats, etc.
It is forbidden to open bubbles, remove mastic, rosin and other resinous substances adhered to the burnt place. Clothes and shoes cannot be torn off from the burnt place; they must be carefully cut and carefully removed.
For a 1st degree burn, pour cold water over the affected area for at least 10 minutes, and then put on a sterile synthetic bandage.
If the burnt clothing is stuck to the burn site, it is not removed, but a sterile dressing is applied over it.
For severe or extensive burns, wrap the victim in a clean sheet, cover warmly and create peace while waiting for the doctor.
If there is no vomiting, the victim should be given an abundant saline drink (0.5 teaspoon of baking soda and salt per 1 liter of water), as well as sweet tea and coffee.
Electrical burn (electric shock)
When approaching someone with an electric shock, you must take appropriate precautions to avoid becoming another victim yourself. Disconnect the current if possible. If this is not possible, then you must isolate yourself before touching the victim. To do this, you must wear rubber gloves, rubber boots, or stand on a rubber mat. The electrical wires can be pushed away from the victim with a wooden stick, chair, or other non-conductive object. After that, you need to check whether the victim has breathing and heart contractions.
If the victim is not breathing, artificial respiration should be started immediately.
In case of cardiac arrest, it is necessary to do an indirect massage. Call for help. If the victim is breathing, cool the burned areas of the body with cold water and cover them with a clean, lint-free cloth. Electrical burns should be treated in the same way as thermal burns. Treatment should include the use of pain relievers, prevention and management of shock, and infection control.
Electrical burns can be accompanied by paralysis, respiratory center, loss of consciousness and instant death.
Chemical burn
It is important to reduce the concentration of the chemical and the time of exposure as quickly as possible. Cut and remove shreds of clothing.
Rinse the affected area with plenty of running cold water for 15 to 20 minutes. Try to prevent the waste water from getting on other parts of the body or the rescuer himself, treat the burn area with a neutralizing solution (lotion), dry it with a swab and apply a sterile bandage. Neutralizing solutions for burns:
- ? acids - 1 teaspoon of baking soda in a glass of water;
- ? alkalis - 1 teaspoon of boric acid in a glass of water or table vinegar mixed with water.
If organophosphorus compounds come in contact with the skin, rinse it abundantly with 2 - 3% baking soda solution.
Chemical eye burn. Open the victim's eyelids with clean fingers. Carefully, with a clean swab, remove the chemical (without any effort). Rinse your eye liberally without letting the used water get onto other parts of your face. Apply a sterile bandage and send urgently to a hospital.
Chemical burn of the esophagus. Call a doctor immediately. Do not flush your stomach. If vomiting occurs, give the victim no more than 2 to 3 glasses of clean water to drink. It is good to drink milk egg whites, dissolved starch.
Topic 18. BURNS, FREEZING. ELECTRIC INJURIES. Drowning. FIRST AID
18.1. Types of burns. Thermal burns
A burn is damage to tissues and organs caused by the action of high temperature (thermal burn), chemicals (strong acids, alkalis, heavy metal salts - chemical burns). Possible burns from the action of electric current (electric burns), from the action of penetrating radiation ( radiation burns).
Thermal burns... Depending on the depth of the lesion, four degrees of severity are distinguished. 1 degree. It arises from the action of a relatively low temperature (60–70 ° C). Is happening
expansion of skin capillaries, sweating of blood plasma through the walls of blood vessels. The victim complains of burning pain, skin hyperemia, edema. There is no deep tissue damage. After 3-5 days, all the phenomena disappear, sometimes there is a slight peeling of the skin.
2nd degree. It is characterized by a more pronounced disorder of local blood circulation. Against the background of hyperemia, edema, bubbles appear filled with a yellowish liquid (i.e., there was a detachment of the upper layer of the epidermis). The bottom of the bubbles is the germ layer. After 10-15 days, the skin is restored without a scar, since the growth layer is not disturbed.
Grade 3 occurs as a result of prolonged, intense exposure to high temperatures and is characterized by necrosis of the entire thickness of the skin, although surgeons subdivide partial necrosis of the skin itself (3a) and necrosis of all layers (3b). Coagulation of tissue proteins occurs with the formation of a dense crust - a scab. After rejection of the scab, healing occurs by secondary intention with the formation of a rough scar.
Stage 4 arises from the action of very high temperature (flame). This is the most severe form of burns - charring, characterized by total tissue damage, right down to the bone.
Usually burns varying degrees They fit together.
The severity and danger of a burn depends not only on the degree, but also on the area of the lesion. So, a burn of 1/3 (in children 1/4) of the entire surface is life-threatening. A burn up to 50% or more (in children up to 1/3) of the body surface is usually fatal. Although in a number of cases, it is possible to save a person with a defeat of up to 80% or more. It depends on the state of the body, the conditions in which the patient is being treated (burn center).
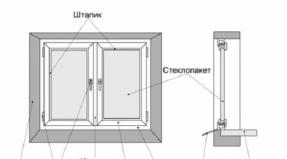
There are several methods for determining the area of burns. The "nines" method. According to this method, it is generally accepted that:
head and neck - 9% of the entire body surface (these are the most dangerous parts);
Fruits - 9%;
yoga - 18%;
the front surface of the body (chest, abdomen - 18%);
the back of the body (back, lumbar region – 18%).
Postnikov's method- a transparent sterile film lined with centimeter squares is applied to the treated burn surface. The contour of the burn is traced and the area of the lesion is calculated.
18.2. Burn disease
With extensive lesions, 10% or more of the entire surface of the body, severe and long-term violations of the general condition of the body are always observed.
The aggregate of a severe burn with the accompanying general severe phenomena is called burn disease, i.e. suffering of the whole organism.
By clinical course burn disease is divided into 4 periods:
1) burn shock;
2) toxemia;
3) septic toxemia;
4) recovery.
Burn shock is a type of traumatic shock that occurs as a result of over-irritation of the central nervous system by pain impulses. The area of the lesion affects the development of shock more than the depth.
defeat. During this period, there is a loss of a large amount of the liquid part of the blood - plasma. Plasma loss can reach 2-3 liters or more per day. This promotes blood thickening, impaired microcirculation in tissues, and complicates metabolic processes.
Clinical picture burn shock has specific features. Its duration can be up to 2-3 days from the moment of the burn. The phase of excitement is acutely expressed and prolonged. The victims are agitated, groaning, rushing about, complaining of a sharp pain. A state of euphoria is sometimes noted. Pulse - fast, blood pressure - normal or slightly elevated. In the phase of inhibition, the victims are apathetic, indifferent, and do not present any complaints. The temperature is lowered, the skin is pale, the facial features are pointed. There is dryness of the mucous membranes, thirst, and sometimes vomiting. Respiration is frequent, shallow. The blood pressure is lowered. An important sign of burn shock is a violation of the urinary function of the kidneys - oleguria, sometimes anuria. Other organs (liver, heart, central nervous system) suffer at the same time.
The period of toxemia is conventionally considered from three days and lasts up to two weeks. There is no sharp boundary between periods. Along with pain, intoxication comes to the fore. The absorption of decay products of dead tissues plays an important role in the development of toxemia. The period of toxemia proceeds with a high body temperature, patients are inhibited, sluggish. Pulse - fast, shallow breathing, no appetite, insomnia, nausea, vomiting. In the blood, anemia, leukocytosis.
Subsequent period septic-toxemia difficult to separate from toxemia. A secondary infection joins the vast wound surface due to a decrease in the general resistance of the body. The phenomena of sepsis come to the fore. The fever takes on a hectic character, anemia increases.
The wound surface is covered purulent bloom, purulent foci are formed in various organs. In patients, burn exhaustion develops, accompanied by a large loss of proteins and electrolytes.
Death can occur from burn shock in the first 2-3 days, from toxemia - after 1-2 weeks, and after a few weeks - from septic-toxemia.
 recovery period areas of necrosis are rejected, the wounds are cleaned, covered with granulations, and then coarse scar tissue forms. In order to accelerate the healing of an extensive wound, as well as to prevent the development of rough tightening scars, patients undergo skin transplantation.
First aid for burns... When providing first aid, remove the victim from the high temperature zone. Take off, extinguish burning clothes. To extinguish a fire, you can douse with water, throw a blanket, coat over a burning one, but without covering your head, otherwise the mucous membrane of the respiratory tract can burn with hot air and smoke. It is impossible to extinguish burning napalm (fire mixture) with water, since it instantly turns into steam, explodes, splashes and the area of damage increases.
All measures in the provision of first aid should be aimed at preventing shock and infection of the burn surface. To do this, the patient is injected with painkillers and the wound is closed with an aseptic bandage. Applying cold to the affected area has a positive effect.
Do not apply fat-based ointment dressings. Cover the victim, give plenty of drink, deliver to a hospital.
18.3. Chemical burns
Chemical burns are less common than thermal ones. They arise when various chemicals (acids, alkalis, salts of heavy metals) are exposed to tissues. More often, chemical burns are found in production, less often in everyday life.
For acid burns dehydration and coagulation of tissue proteins occurs. A dense crust forms at the site of the burn - a scab. By the color of the scab, you can tell which acid has entered. A white scab gives hydrochloric acid, yellow - nitric, dark - sulfuric acid. When alkalis are exposed to the tissues, the latter, reacting with fats, form soap, deeper tissue damage occurs with the formation of a soft white crust.
In case of chemical burns, it is necessary to wash off the ingested substance as soon as possible with a strong jet of water, while the concentration of the substance decreases at the same time. Neutralize the remnants of the embedded substance with a substance of the opposite action, i.e. for acid burns, apply a bandage soaked in 1–2% alkali solution (baking soda). In case of burns with alkali, apply a bandage soaked in 1–2% citric and acetic acid solution.
Phosphorus burns proceed in a peculiar way: once on the fabric, they continue to burn for a long time, it can be extremely difficult to extinguish them. For the purpose of extinguishing, it is recommended to immerse the affected area in a bath of water, and remove the pieces of burning phosphorus with tweezers. Then a bandage soaked in a 5% solution of copper sulfate is applied to this area or sprinkled with talcum powder. Further treatment is carried out in a medical institution.
Radiation burns occur from contact with radioactive substances as a result of skin contamination. The severity of the lesion depends on the dose rate, duration of action, and the nature of the radiation. The area of the lesion and localization matter. With radiation burns, tissue ionization occurs, complex chain reactions occur with disruption of intracellular metabolic processes. This significantly distinguishes radiation burns from thermal burns. Radiation burns can turn into a trophic ulcer, and the ulcer can turn into cancer.
18.4. Frostbite, degree of frostbite. Total freezing
Frostbite is damage to tissues and organs resulting from the action of low temperatures. Usually develops after long acting cold air 0 ° C and below degrees. However, it can also occur at a temperature of + 3 ... 7 ° C, if there are conditions that increase the heat transfer of the body (strong wind, high air humidity, tight shoes, wet clothes, prolonged immobility, etc.). Fatigue, exhaustion, vitamin deficiency, infection, bleeding, alcohol intoxication of the victim predispose to frostbite. The time factor is important. The quantity
è the nature of the damage caused by cold, manifests itself after warming the affected area.
 during the period of low temperature, the skin color changes (blanching), sensuality decreases. There is still no tissue death during this period. Therefore it is calledlatent period... Cooling is accompanied by a slowdown in blood circulation, and with a further decrease in temperature, there is a complete cessation (stasis). Tissues lose their ability to absorb oxygen and nutrients. Toxic waste products are not excreted from them. Paralysis of the capillaries sets in, the permeability of their walls increases, which leads to edema. Blood clots form in the dilated vessels. All this leads to tissue death.
According to the severity and depth of changes in the tissues, four degrees of frostbite are distinguished.
It is possible to determine the exact extent of the lesion only after warming up, sometimes after several days.
1 degree - circulatory disorders of the skin area, itching, burning, pain, loss of sensitivity. The skin is swollen, has a variegated color (red, blue or purple spots on a pale background). There is no deep defeat. After 3-5 days, all phenomena disappear. Hypersensitivity of the affected area to the effects of cold may persist.
Grade 2 - deeper circulatory disorders and the formation of blisters filled with clear liquid. The bottom of the blisters is the growth layer of the skin. Sensitivity is impaired. The nail plates of the fingers and toes are rejected. But all changes are reversible. Healing lasts 10-12 days without scarring, the nail plates are restored.
Grade 3 - accompanied by necrosis of all layers of the skin and underlying tissues. The depth of damage is revealed in a few days. In the early days, edema is noted and bubbles appear filled with a liquid of a dark brown color. The swelling gradually decreases. By 9-10 days, a demarcation line appears; a line that delimits dead tissue from healthy ones. After the final rejection, resorption of necrotic tissues after 1–2 months, scar healing gradually begins. The nail plates are not restored. The general phenomena are pronounced. There is an increase in temperature, chills, torrential sweats, poor sleep, appetite.
4 degree frostbite the most difficult. All layers die, seizing the bone. At the same time, it is not possible to warm the affected limb, it remains cold, absolutely insensitive. The demarcation line is revealed in 16–12 days. There is a persistent disappearance of muscle, pain and tactile sensitivity. The damaged area gradually turns black and begins to dry out (mummify). The general condition suffers sharply. After a clear designation of the border of dead tissues, the limb is amputated within the limits of healthy tissues.
First aid . First aid consists in warming the patient and restoring blood circulation
â the affected areas of the body. The victim must be taken to a warm room, given hot tea, coffee, alcohol, the affected parts of the body or the whole patient must be placed in a bath, gradually increasing the water temperature from 18 to 40 ° C during 20-30 minutes. Massage at the same time
the affected limb. When signs of restoration of blood circulation appear (warming and hyperemia of the skin, the appearance of sensitivity), the skin is wiped with alcohol and an aseptic bandage is applied, over which the limb is wrapped with a thick layer of cotton wool.
If it is impossible to use warm baths, blood circulation is restored with the help of massage. The massage is performed with clean hands, while moistening the affected skin and hands with alcohol or vodka. It is impossible to rub the affected areas of the skin with snow, since the snow cools the skin even more, and small pieces of ice injure it.
It is inappropriate to use fats, ointments, petroleum jelly for grinding. If there are already bubbles in the area of frostbite, then massage cannot be done. In such cases, the affected areas of the skin should be treated with alcohol, an aseptic bandage should be applied, wrapped with a thick layer of cotton wool and the patients should be sent for further treatment to the hospital.
General freezing, chills... Under the influence of prolonged exposure to low temperatures on the entire body, general, deep, irreversible changes can occur, leading to general freezing and death. A decrease in body temperature gradually slows down and then stops blood circulation. The first manifestations of general freezing are chills, drowsiness, stiffness of movements. With further cooling, an irresistible desire to sleep sets in. Cooling progresses rapidly during sleep. With a decrease in body temperature to 25 ° C and below, it is not possible to save a person. Death occurs as a result of cardiac and respiratory arrest.
With general freezing, the nature of the help is the same as with frostbite. However, all measures should be more vigorous, and in the absence of breathing, cardiac arrest, immediately begin artificial respiration and indoor massage hearts. The fastest warming is achieved by immersing the victim in the bath, gradually (within 20-30 minutes) increasing the water temperature from 18-20 to 35-40 ° C. If the victim is conscious, give hot tea, coffee, 30-50 ml of alcohol to drink. Simultaneously with warming up, an energetic full-body massage is performed. All victims after general freezing should be treated in a hospital, since in a later period they often develop pneumonia.
Chilliness occurs as a result of prolonged exposure to moderately low temperature or with repeated mild frostbite. Fingers, feet, ears, nose, cheeks are usually affected.
Clinically, this is expressed in chronic inflammation of the skin, which takes the form of red-blue spots with a purple tint. Itching, slight swelling, soreness is noted, hypersensitivity to the action of low temperature remains (washing hands in cool water causes discomfort). But often, even in warm weather and in summer, the hands and feet are cool due to a violation of the heat-regulating function of the skin vessels.
First aid and treatment: warming the affected areas, massage, dry heat, physiotherapy.
18.5. Electrical trauma
Types of electric shock, damaging effect... The effect of an electric current on a living organism, in contrast to the effect of other factors, is very peculiar and versatile. The severity and outcome of an electric shock depend on the resistance of the human body, the magnitude of the current strength and the duration of its passage, the type and frequency of the current, the path of current passage, the individual properties of the human body. Passing through the human body, electric current has a thermal, electrolytic and biological effect on various organs and systems:
thermal effect of current manifests itself in burns of individual parts of the body and heating to a high temperature of blood vessels, nerves, heart and brain;
electrolytic- in the destruction of organic fluid, including blood;
biological - in irritation and excitement of living tissues of the body and in violation of internal bioelectric processes.
All these types of effects of electric current can be of the nature:
1) local electrical injuries (external damage to the body) - burns, electrical current marks in the form of red stripes along the vessels, metallization of the skin (dark border around the burn), mechanical damage, electrophthalmia;
2) general (internal) lesions - electric shock.
Electric burns differ significantly from thermal ones. They are crater-shaped with dense eroded edges. Electric burns are less painful, as there is damage to the sensitive nerve endings, there is no redness in the area of damage.
Electric shock- the result of the biological effects of the current. This is the most dangerous species human lesions, accompanied by convulsive involuntary muscle contractions, including the muscles of the heart and bronchi of the lungs. Depending on the resulting consequences, electric shocks are divided into four degrees:
I - convulsive muscle contractions without loss of consciousness;
II - convulsive muscle contractions with loss of consciousness, but with preserved breathing and heart function;
III - loss of consciousness and impaired cardiac activity or breathing (or both together);
IV - a state of clinical death. The duration of this state can persist for 4-6 minutes.
The degree of electric shock depends on the type and frequency of the current. The most dangerous is alternating current with a frequency of 20 to 100 Hz at voltages up to 500 V. At more high values direct current becomes more dangerous than alternating frequency of 50 Hz. At a current frequency of 50 Hz, the danger in the form of electric shocks increases, a further increase in frequency reduces this danger, and at a current frequency of 450–500 Hz, it completely disappears, but the risk of burns remains.
The path of current passing through the human body is of great importance. The greatest danger arises when the current passes directly through the vital organs (heart, lungs, brain). The number of injuries with loss of consciousness during the passage of current along the "hand-arm" and "arm-legs" paths is higher than on the "leg-to-leg" path.
The longer the effect of an electric current on a person, the greater the severity of the lesion, since this reduces the resistance of the body. When the time of passage of current through the heart coincides in the diastole phase (relaxed state, its duration is 0.2 s), cardiac fibrillation occurs, i.e. chaotic and multi-temporal contractions of the fibers of the heart muscle. Acute heart failure develops.
The main factor determining the outcome of a person's injury when an electric current passes through it is the current strength.
To characterize the effect of an electric current on a person, three criteria have been established: threshold perceptible current, threshold non-releasing current, and threshold fibrillation current.
1. A person begins to feel the effect of an alternating current with a frequency of 50 Hz at its strength of 0.5–1.5 mA and a constant - 5-7 mA. Largest values these currents are usually called threshold sensible current.
2. With alternating current with a frequency of 50 Hz and a strength 10-15 mA and constant - with a force of 50-80 mA, irresistible convulsive contractions of the muscles of the hands appear and a person cannot unclench them to release them from the current-carrying part (wire). The smallest values of such a current were called threshold non-releasing... It is considered safe for humans only with a short-term passage through the human body.
3. Fibrillation variable industrial frequency currents are considered in the range from 0.1 to 5 A, and constant currents - from 0.3 to 5 A. Passing through the human body, they act on the heart muscle. After 1–2 s, fibrillation or cardiac arrest occurs, and subsequently the cessation of breathing. With a current value of more than 5 A of both types of current, immediate respiratory paralysis and cardiac arrest occur, bypassing the state of fibrillation. In this case, within a few seconds, severe burns and tissue destruction of individual organs occur.
Lightning - a discharge of atmospheric electricity - causes characteristic changes - stripes of hyperemia on the skin (a trace of the discharge of electricity passed through the skin). Usually hyperemia lasts 3-4 days, then disappears completely.
First aid for electrical injury consists primarily in the termination of the action of the current on the victim. This is achieved by turning off the current (switch, switch, plugs) or by diverting the electrical wires from the victim using a dry stick or rope. In the absence of breathing and cardiac arrest, artificial respiration, external heart massage, body massage, upper and lower limbs from the periphery to the center.
With light electric shock, when the victim experiences fright, nervous shock, fainting, short-term loss of consciousness, dizziness, headache etc. first aid consists in creating rest, prescribing analgin, bromine, valerian tincture and, necessarily, hospitalization in a medical institution.
In the future, it is necessary to constantly monitor the medical staff, since complications are possible up to spontaneous cardiac arrest, breathing, cerebral edema.
18.6. Drowning
Drowning is a form of mechanical asphyxia. In this case, there are two variants of asphyxia. The first is the "pale type", rapid drowning, when as a result of fright, sudden cooling, laryngospasm occurs, which prevents water from entering the trachea and lungs. The skin of such victims is pale. Reviving them is more successful if a person is under water even
up to 10 minutes.
With a slow drowning (the victim flounders, tries to stay on the surface, then floats, then hides under water), water fills the lungs.
At the same time, the skin is sharply cyanotic (cyanotic) - this is the second variant of asphyxia - "blue type". With the "blue type" after 3-5 minutes of being under water, it is difficult to count on a positive result of resuscitation.
There is a difference between drowning in fresh and seawater. Fresh water has a low osmotic pressure and quickly enters the bloodstream from the lungs, which leads to an increase in the mass of circulating blood and hemolysis (destruction) of erythrocytes. Pulmonary edema develops, which is difficult to treat. Sea water contains a lot of salts (in fact, it is a hypertonic solution), and therefore it is poorly absorbed into the bloodstream. If the period of stay under water does not exceed 2–4 minutes, then the outcome of resuscitation measures is more favorable.
When drowning, regardless of its type of asphyxia, there are various neurological symptoms, convulsions, delirium, retrograde amnesia, focal disorders, loss of consciousness. When drowning, after stopping breathing, after 1–2 minutes a person already loses consciousness.
First aid for drowning, if breathing and heartbeat are preserved, symptomatic therapy is used, which consists in inhaling vapors of ammonia, oxygen, warming, and the introduction of heart drugs. In the absence of breathing and palpitations, you should quickly clear the mouth of silt and sand, remove water from the upper respiratory tract and stomach, and immediately begin chest compressions and artificial respiration.
To remove water from the respiratory tract and stomach, the victim must be laid with his stomach on his bent knee upside down and press sharply on the back-lower sections chest... After that, proceed to resuscitation.
Control questions
1. Types of burns. The degree of thermal burns.
2. Burn disease.
3. Chemical burns.
4. Frostbite. The degree of frostbite. First aid.
5. General freezing. Chills.
6. Electrical trauma. Types of influence of electric current. First aid.
7. Drowning. Types of asphyxia. First aid.
Topic 19. COMBINED LESIONS, THEIR KINDS
19.1. Polytrauma, its types
Damage to homogeneous tissues in different parts of the body in one victim is called multiple injuries(multiple abrasions, bruises, fractures).
Damage to various organs and tissues in one victim is called concomitant injury(at the same time, limb injury, traumatic brain injury (TBI), damage to internal organs - chest, abdomen, pelvis, spine).
Most common reasons polytrauma: road accidents, natural disasters, catastrophes, explosions, collapses, blockages, gunshot wounds.
If with isolated (single) injuries, the mortality rate is 1.5–2%, then with concomitant injury, 28–29%, and with concomitant trauma, up to 90%.
First aid... The fate of victims with concomitant injury largely depends on the quality and timing of the provision of prehospital medical care. This is especially true for concomitant traumatic brain injury. At the same time, the unfavorable results of the treatment of severe concomitant injuries often depend on severe complications (asphyxia, shock, etc.).
Therefore, when providing assistance to the victim at the scene or in the outbreak, the following tasks are faced:
1) identification of life-threatening violations and their immediate elimination;
2) decision on the need for hospitalization or refusal of it;
3) determination of the place of hospitalization according to the damage profile;
4) determination of the sequence of hospitalization in case of massive injuries.
19.2. Combined radiation damage (CRP)
For the first time, combined injuries (CM) in medical practice became most widely known during the First World War (1914–1918), when toxic substances (OM) were used on the battlefield along with firearms. In the conditions of modern war, when using weapons of mass destruction, as well as firearms, various types of defeat can take place.
With the complex influence of factors of different nature, various types of combined lesions arise. Distinguish between 2-, 3-, 4- and 5-factor CP (R - radiation, M - mechanical, T - thermal, X - chemical, B - biological).
In addition, there can be combinations different types defeat with various forms mental disorders.
Combined radiation damage (CRP) Are lesions caused by the simultaneous or sequential action of factors nuclear explosion(shock wave, light radiation, penetrating radiation).
The first information about the PKK in people appeared after the Americans used nuclear weapons in Hiroshima and Nagasaki.
There are the following KRPs:
1) radiation-mechanical;
2) radiation-thermal;
3) radiation-mechanothermal.
The leading etiological factor in CRP is considered to be the one that causes more pronounced disturbances in the state of the body and poses the greatest danger to the life and health of the victim.
 In the clinical picture of CRP, there are four periods:
1 period - acute (primary reaction to radiation and non-radiation injuries);
Period 2 - the predominance of non-radiation components (latent period of radiation sickness (l / b));
3 period - the predominance of the predominantly radial component (the peak period l / b);
4th period - recovery.
By severity clinical manifestations all CRP are divided into four degrees.
1 degree - minor injuries - minor injuries, burns, combined with radiation at a dose of no more than 100 r. The prognosis for life and health is favorable. There may be a temporary disability.
2nd degree - defeat moderate, irradiation up to 200 r. The prognosis for life and health is determined by the effectiveness of medical care. About 50% of the victims return to work.
Grade 3 - severe injuries are severe mechanical and thermal injuries in combination with radiation with a dubious prognosis of up to 400 r. Return to work in isolated cases.
Grade 4 - extremely severe injury, severe trauma, radiation over 400 rubles. The prognosis is poor, even with all types of treatment. Symptomatic therapy is indicated.
In most cases, CRP develops a syndrome of mutual burdening (strengthening, weighting) of the pathological process. This syndrome occurs with II, III, IV degrees of CRP.
The essence of the syndrome of mutual aggravation is that the presence of radiation sickness worsens the course and outcomes of mechanical and thermal injury, and injuries and burns, in turn, worsen the prognosis of the course of radiation sickness.
Thus, the degree of mutual aggravation depends on the radiation dose, as well as the nature and severity of the injury and burn.
Features of the flow of the KRP.
1. With CRP, there is no latent period of l / b. This period is, as it were, "filled" with the clinic of burns or mechanical trauma. The peak period comes earlier and is more difficult. The recovery period is also longer.
2. There is a change in the general and local reactions of the body:
with CRP, shock is more common;
due to a decrease in the general and local resistance of the body, infection often develops in wounds and burns;
increased tissue bleeding is noted, which makes it difficult to carry out operations;
healing of wounds, burns, fractures slows down.
KRP are divided into two main groups:
Group 1 - a combination of mechanical and thermal injuries with general external radiation of the body;
Group 2 - burns and wounds contaminated with the products of a nuclear explosion.
Diagnosis of FCC is based on the following data:
1) anamnesis (survey);
2) clinical research;
3) laboratory research;
4) dosimeter readings.
First aid in the outbreak... Put on a gas mask. Apply a sterile bandage to the wound, burn to prevent the entry of RV.
In case of contamination of a wound, a burn of RV, it is necessary:
apply a cotton-gauze bandage, as it adsorbs up to 50% of PB from the wound;
introduce pain relievers;
stop bleeding, immobilization of extremities according to indications.
The duration of the tourniquet on the limb is halved (in the summer - up to 1 hour, in the winter - up to
30 minutes).
Each victim needs complete or at least partial sanitization. Further
the treatment of these victims will be carried out in a surgical hospital in a suburban area. Combined chemical damage... In the conditions of modern war, along with others
types of weapons, it is possible to use OF due to its great lethality. This will cause the occurrence of combined chemical lesions (CCP):
thermal injury + OS;
mechanical damage + OS;
thermal + mechanical + RH.
The degree of damage depends on the nature of mechanical, thermal damage and the dose of the chemical.
The ingestion of OM on the surface of a burn or wound causes general and local disturbances.
General changes appear in the form of a typical pattern characteristic of a given OM. In this case, all the symptoms of the lesion appear faster, since the OM immediately enters the bloodstream, the level of the dangerous dose of the OM decreases.
Control questions
1. Polytrauma, its types.
2. Combined radiation damage (CRP).
3. Periods and degrees of KRP.
4. Features of the flow of the KRP. First aid.
Topic 20. BASICS OF REANIMATION
20.1. Terminal states, their types
Resuscitation is a complex treatment measures aimed at restoring and temporarily replacing the extinct vital functions of the body - respiration, blood circulation, metabolism.
Resuscitation is a special type of medical care provided to an affected person who is in a terminal state.
Terminal states Is a condition in which the body is on the verge of life
è death. These include:
preagonal state;
agony;
clinical death.
A feature of terminal states is that they are fundamentally reversible and, under favorable circumstances (timeliness and correctness of the resuscitation), they allow the body to return to life.
All these severe, acutely developing conditions are necessarily accompanied by the development of oxygen deficiency (hypoxia) of organs and tissues. Hypoxia is the most destructive damaging factor that quickly causes severe changes in the body and can lead to death. The delivery of oxygen to the organs is provided by the respiratory and cardiovascular systems. It follows from this that in the process of resuscitation, all measures should be aimed at restoring breathing and blood circulation.
Pre-gonal state characterized by the preservation of consciousness and reflexes. At the same time, there is a frequent threadlike pulse, periodic absence of blood pressure (BP), shallow and rapid breathing. At the end of this state, there may be a slowdown in pulse and respiration.
Agony is a state of the body characterized by loss of consciousness, a sharp suppression of reflex activity, absence of blood pressure, convulsive breathing with the participation of auxiliary respiratory muscles.
The agony can last for several hours, although more often it is short-lived and turns into clinical death.
Clinical death- this is the state of the body after the termination of all clinical manifestations of life (cardiac arrest, respiration, lack of reflexes). This state lasts 3-5 minutes (with hypothermia of the body - longer). During this time, the cells of the cerebral cortex still retain the ability to restore their vital activity with the resumption of cerebral blood flow.
If irreversible changes occur in the cerebral cortex, then we should talk about the onset biological death and it is impossible to restore life in the body.
20.2. Indications and contraindications for resuscitation
From the foregoing, we can formulate the main tasks of resuscitation:
1) restoration of cardiac activity and blood supply to the brain;
2) restoration of gas exchange in the lungs;
3) restoration of the volume of circulating blood.
If special equipment is not always required to perform the first two tasks of resuscitation and they can be performed by almost any person, then restoring the volume of circulating blood implies the introduction of various medicinal solutions(blood, blood substitutes, anti-shock fluid, protein preparations, etc.). They are performed by medical workers with the help of droppers.
Resuscitation measures must be carried out in all cases of sudden cessation of blood circulation and respiration, which can occur as a result of:
myocardial infarction and acute heart failure;
reflex cardiac and respiratory arrest (with anesthesia);
electrical injuries;
acute poisoning;
suffocation;
drowning.
Resuscitation should not be performed if death has occurred as a result of:
progression malignant diseases with metastases in various organs;
heart failure of the 4th degree, in the stage of decompensation;
severe irreversible brain damage.
Initial assessment of the victim's condition ... An external examination determines:
lack of consciousness;
the skin and visible mucous membranes are pale;
to determine the function of breathing, a cool mirror or glass is brought to the mouth (fogs up or not);
the pupil is wide, weak reaction to light;
weak pulsation of the great vessels (carotid artery).
20.3. Basic methods of resuscitation
The simplest, but at the same time, effective resuscitation measures in case of clinical death are external (indirect) heart massage and artificial lung ventilation (ALV).
This allows you to maintain the circulation of oxygen-enriched blood in the body and prevent the development of irreversible changes in the brain for several hours, i.e. for the period until more qualified assistance. It is important not to stop resuscitation during the transportation of the victim.
Resuscitation can be effective if it begins in a timely manner, before the expiration of the critical deadlines. After 3 minutes of clinical death, the positive effect is 75%, after 4 minutes - 50%.
Preparing the victim for resuscitation:
release oral cavity from the contents (mucus, vomit). Wrap the index finger with a napkin, handkerchief, clean your mouth;
unbutton the collar, relax the belt (belt);
tilt your head back (put a roller under your back, while the airways are straightened),
prevent tongue retraction (pierce the tongue with a pin with a thread, tighten the tongue to the teeth, tie the thread to a shirt button);
lay on a hard surface.
It is necessary to alternately massage the heart and artificial ventilation lungs. Heart massage is carried out with the hands of both hands, superimposed on one another, so that the fingers are raised, and the pressure on the lower half of the sternum is produced by the wrists. If resuscitation is carried out by one person, then he first makes two quick blows of air, and then performs 14-15 chest compressions. If resuscitation is done by two people, which is undoubtedly easier, then the ratio of artificial respiration and heart massage is 1: 4, 1: 5. In this case, resuscitators should periodically change roles.
The principle of indirect massage is to periodically squeeze the heart between the sternum
è spine. At the same time, at the moment of compression, blood is pushed out of the left stomach of the heart into the aorta.
è to the vessels of the brain, and after the cessation of compression, the heart is unclenched, the blood from the superior vena cava again enters the right half of the heart. An absolute indication for indirect massage is to stop the pulsation of the carotid arteries. The victim is placed on a rigid base (table, shield, floor) and rhythmically pressed on the sternum with a frequency 60–70 times a minute. The deflection of the chest wall should be 4–5 cm. Rough manipulations can lead to rib fractures. For children, massage should be done with only one hand, and for newborns only with fingers. If the heart massage is carried out effectively, then pulsation appears on the carotid arteries, the pupils become narrowed, blood pressure rises to 60–80 mm Hg. Art.
For full ventilation of the lungs, artificial respiration is performed. In the mouth-to-mouth method, cover your mouth with a handkerchief, a napkin, pinch the patient's nostrils, take a deep breath and, tightly clasping the open mouth of the person to be revived, blow air into it with force until his chest rises. The exhalation of the victim is carried out passively, the rescuer withdraws at this time and takes the next deep breath. If the victim has an injury to the lower part
Burns are thermal, chemical and radiation. Thermal burns occur when exposed to the skin or mucous membranes ( integumentary tissues) high temperature, the source of which are flames, hot objects and liquids, hot gaseous substances, flammable substances, etc. Thermal burns ...(Labor protection in construction)
First aid for burns
Etiology and pathogenesis of burns Burn - damage to body tissues caused by excessive exposure to external factors such as temperature (thermal burns), acids and alkalis (chemical burns), electric current (electrical burns), ultraviolet (sunburn), X-ray (radiation ...Etiology and pathogenesis of burns
Burn - damage to body tissues caused by excessive exposure to external factors such as temperature (thermal burns), acids and alkalis (chemical burns), electric current (electrical burns), ultraviolet (sunburn), X-rays (radiation burns) and other radiation. Classification...(Life safety for pedagogical and humanitarian areas)
Etiology and pathogenesis of traumatic shock
Shock is a critical condition characterized by a disorder and suppression of the functions of vital organs and systems of the human body (central nervous system, cardiovascular, respiratory, excretory and other systems). Traumatic shock is a life-threatening condition of the victim, arising ...(Life safety for pedagogical and humanitarian areas)
(Life safety for pedagogical and humanitarian areas)
Recommended Procedure for Internal Bleeding
Difficulty stopping internal bleeding lies in the fact that neither the bleeding itself nor the amount of lost blood is visible, which does not allow timely determination of the severity of the victim and his hospitalization. It is difficult for a layman to determine the presence of internal bleeding. Together...(Life safety for pedagogical and humanitarian areas)