Difference between BCG vaccine and BCG vaccine. BCG vaccination - what is it and why it is given to newborns What dose is the BCG vaccine given?
Instructions for vaccination and revaccination against tuberculosis with BCG and BCG-M vaccines
II. Application of the tuberculosis vaccine (BCG) dry for intradermal administration
The drug is a live mycobacterium of the BCG-1 vaccine strain, lyophilized in 1.5%. sodium glutamate solution. A porous mass, powdery or in the form of a white or cream-colored tablet, is hygroscopic.
The inoculation dose contains 0.05 mg in 0.1 ml of solvent.
Biological and immunological properties.
Appointment.
The drug is intended for specific prophylaxis of tuberculosis.
Methods of application and dosage.
BCG vaccine is administered intradermally at a dose of 0.05 mg in a volume of 0.1 ml. Primary vaccination is carried out to healthy newborns 3-7 days of age.
Revaccination is subject to children aged 7 and 14 years old who have a negative reaction to the Mantoux test with 2 TE PPD-L. The reaction is considered negative in the absence of infiltration, hyperemia, or in the presence of a prick reaction (1 mm). Children infected with tuberculosis mycobacteria who have a negative reaction to the Mantoux test are not subject to revaccination. The interval between setting the Mantoux test and revaccination should be at least 3 days and no more than 2 weeks.
Vaccinations should be carried out by specially trained medical personnel of a maternity hospital (department), a nursing department for premature babies, children's clinics or feldsher-obstetric points. Vaccination of newborns is carried out in the morning in a specially designated room after the children are examined by a pediatrician. In polyclinics, the selection of children to be vaccinated is preliminarily carried out by a doctor (paramedic) with compulsory thermometry on the day of examination, taking into account medical contraindications and anamnesis data. If necessary, consult with specialist doctors, blood and urine tests. The history of the newborn (medical record) indicates the date of vaccination, the series and control number of the vaccine, the manufacturer, the expiration date of the drug.
For vaccination (revaccination), disposable tuberculin syringes with a capacity of 1.0 ml with tightly fitted pistons and thin needles with a short cut are used. Do not use expired syringes, needles or needleless injectors. After each injection, a syringe with a needle and cotton swabs are soaked in a disinfectant solution (5% chloramine), then centrally destroyed. It is forbidden to use for other purposes the instruments intended for the vaccination against tuberculosis. In the vaccination room, the vaccine is stored (in the refrigerator, under lock and key) and diluted. Persons not related to BCG vaccination are not allowed into the vaccination room. In order to avoid contamination, it is unacceptable to combine the vaccination against tuberculosis with other parenteral procedures on the same day.
Vaccine ampoules are carefully inspected before opening.
The drug is not subject to use:
In the presence of foreign inclusions or flakes that do not break when shaking in a diluted preparation.
The dry vaccine is diluted immediately before use with a sterile 0.9% sodium chloride solution attached to the vaccine. The solvent must be transparent, colorless and free from foreign matter.
The neck and head of the ampoule are wiped with alcohol, the sealing point (head) is filed and carefully, using tweezers, break off. Then the neck of the ampoule is filed and broken off by wrapping the sawn end in a sterile gauze napkin.
To obtain a dose of 0.05 mg of BCG in 0.1 ml, a sterile syringe with a capacity of 2.0 ml, with a long needle, 2 ml of 0.9% sodium chloride solution is transferred into an ampoule with a 20-dose vaccine, and into an ampoule with 10- dose vaccine - 1 ml of 0.9% sodium chloride solution. The vaccine should be completely dissolved within 1 minute after 2-3 times shaking. No sediment or floc formation that does not break when shaken is allowed.
The reconstituted vaccine must be protected from sunlight and daylight (black paper cylinder) and consumed immediately after reconstitution. Unused vaccine is destroyed by boiling for 30 minutes, autoclaving at 126 ° C for 30 minutes, or immersion in a disinfectant solution (5% chloramine solution) for 60 minutes.
For one vaccination, 0.2 ml (2 doses) of the diluted vaccine is taken with a syringe, then 0.1 ml of the vaccine is released through a needle into a sterile cotton swab to displace the air and bring the syringe plunger to the desired graduation - 0.1 ml. Before each set, the vaccine must be carefully mixed with a syringe 2-3 times. Only one child can be given the vaccine with one syringe.
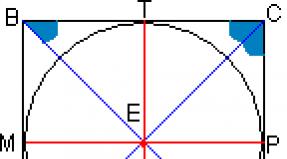
BCG vaccine is administered strictly intradermally at the border of the upper and middle third outer surface left shoulder after pretreatment of the skin with 70 ° alcohol. The needle is inserted with a cut upward into the surface layer of the stretched skin. First, a small amount of the vaccine is injected to make sure that the needle is inserted exactly intradermally, and then the entire dose of the drug (only 0.1 ml). With the correct injection technique, a whitish papule with a diameter of 7-9 mm should form, usually disappearing after 15-20 minutes.
It is forbidden to apply dressings and treatment with iodine or other disinfectant solutions the place where the vaccine was administered.
Reaction to the introduction
At the site of intradermal administration of the BCG vaccine, a specific reaction develops in the form of a papule 5-10 mm in diameter.
In newborns, a normal vaccine reaction occurs after 4-6 weeks. The reaction undergoes a reverse development within 2-3 months, sometimes over a longer period. In revaccinated persons, a local reaction develops in 1-2 weeks. The site of reaction should be protected from mechanical irritation, especially during water procedures.
In 90-95% of those vaccinated at the vaccination site, a superficial scar up to 10.0 mm in diameter should form. Complications after vaccination and revaccination are rare and usually local in nature.
Contraindications
For vaccination:
1) Prematurity 2-4 degrees (with a birth weight of less than 2500 g).
2) Vaccination is postponed for acute diseases and exacerbations chronic diseases(intrauterine infection, purulent-septic diseases, hemolytic disease newborns of moderate and severe form, severe lesions nervous system with severe neurological symptoms, generalized skin lesions, etc.) until the clinical manifestations of the disease disappear.
3) Immunodeficiency state (primary).
4) Generalized BCG infection detected in other children in the family.
5) HIV infection in the mother.
Children who are not vaccinated during the neonatal period, after excluding contraindications, are prescribed the BCG-M vaccine.
For revaccination:
1. Acute infectious and non-infectious diseases, exacerbation of chronic diseases, including allergic ones. Vaccination is carried out 1 month after recovery or remission.
2. Immunodeficiency states, malignant neoplasms of any localization. When prescribing immunosuppressants and radiation therapy the vaccination is carried out no earlier than 6 months after the end of treatment.
3. Tuberculosis, a history of MBT infection.
4. Positive and questionable Mantoux reaction with 2 TE PPD-L.
5. Complicated reactions to the previous administration of BCG vaccine ( keloid scar, lymphadenitis, etc.).
In contact with infectious patients in the family, childcare, etc. vaccinations are carried out at the end of the quarantine period or the maximum period incubation period for a given disease.
Persons temporarily exempted from vaccinations should be taken under observation and registration and vaccinated after complete recovery or removal of contraindications. If necessary, appropriate clinical and laboratory examinations are carried out.
Children who are not vaccinated during the neonatal period receive the BCG-M vaccine. Children aged 2 months and older undergo a preliminary Mantoux test 2 TE PPD-L and vaccinate only tuberculin-negative.
Other prophylactic vaccinations can be given at least 1 month apart before and after BCG revaccination.
Release form
In ampoules containing 0.5 mg (10 doses) or 1.0 mg of the drug (20 doses) complete with a solvent - 0.9% sodium chloride solution - 1 or 2 ml per ampoule, respectively.
One pack contains 5 ampoules of BCG vaccine and 5 ampoules of 0.9% sodium chloride solution (5 sets).
The shelf life of the BCG vaccine is 2 years.
Store the drug at a temperature of 5-8 ° C.
III. Application of tuberculosis vaccine (BCG-M) dry (for sparing primary immunization)
The drug is a live mycobacterium of the BCG-1 vaccine strain, lyophilized in a 1.5% solution of sodium glutamate. The porous mass is powdery or in the form of a white or cream-colored tablet. Hygroscopic. The inoculation dose contains 0.025 mg of the drug in 0.1 ml of solvent.
Biological and immunological properties
Live mycobacteria of the BCG-1 strain, multiplying in the body of the vaccinated, lead to the development of long-term immunity to tuberculosis.
Appointment
The drug is intended for sparing specific prophylaxis of tuberculosis.
Directions for use and dosage
BCG-M vaccine is used intradermally at a dose of 0.025 mg in 0.1 ml of solvent.
BCG-M vaccine is vaccinated:
1. In the maternity hospital of premature newborns weighing 2000 g or more, with the restoration of the original body weight - the day before discharge.
2. In the departments of nursing premature newborns of medical hospitals (2nd stage of nursing) - children weighing 2300 g or more before being discharged from the hospital home.
3. In children's polyclinics - children who have not received anti-tuberculosis vaccination in the maternity hospital for medical contraindications and are subject to vaccination in connection with the removal of contraindications.
4. In territories with a satisfactory epidemiological situation for tuberculosis, the BCG-M vaccine is used to vaccinate all newborns.
Children who have not been vaccinated in the first days of life are vaccinated during the first two months in a children's clinic or other medical and preventive institution without prior tuberculin diagnostics.
Children over 2 months of age need a preliminary Mantoux test with 2 TU PPD-L before vaccination. Children with a negative reaction to tuberculin are vaccinated. The reaction is considered negative in the absence of infiltration (hyperemia) or the presence of a prick reaction (1.0 mm). The interval between the Mantoux test and vaccination should be at least 3 days and no more than 2 weeks.
Vaccinations should be carried out by specially trained medical personnel of a maternity hospital (department), a nursing department for premature babies, children's clinics or feldsher-obstetric stations. Vaccinations of newborns are carried out in the morning in a specially designated room after the children are examined by a pediatrician. Vaccinations at home are prohibited. The selection of children to be vaccinated is preliminarily carried out by a doctor (paramedic) with compulsory thermometry on the day of vaccination, taking into account medical contraindications and anamnesis data. If necessary, consult with specialist doctors and blood and urine tests. In the medical history of the newborn (medical record), indicate the date of vaccination, the series and control number of the vaccine, the manufacturer, the expiration date of the drug.
For vaccination, disposable sterile tuberculin syringes with a capacity of 1.0 ml are used, with tightly fitted pistons and thin short needles with a short cut. Do not use expired syringes, needles or needleless injectors. After each injection, a syringe with a needle and cotton swabs are soaked in a disinfectant solution (5% chloramine), then centrally destroyed. It is forbidden to use for other purposes the instruments intended for the vaccination against tuberculosis. The vaccine is stored in the vaccination room (in the refrigerator, under lock and key) and diluted. Persons not related to BCG vaccination are not allowed into the vaccination room. In order to avoid contamination, it is unacceptable to combine the vaccination against tuberculosis with other parenteral procedures on the same day.
Vaccine ampoules are carefully examined before opening. The drug is not subject to use:
In the absence of a label on the ampoule or incorrect filling;
When the expiration date has expired;
In the presence of cracks and notches on the ampoule;
When it changes physical properties the drug (wrinkled tablet, discoloration, etc.);
In the presence of foreign inclusions or non-breaking flakes in the diluted preparation.
The dry vaccine is diluted immediately before use with a sterile 0.9% sodium chloride solution applied to the vaccine. The solvent must be transparent, colorless and free of foreign matter.
The neck and head of the ampoule are wiped with alcohol, the sealing point (head) is filed and carefully, using tweezers, break off. Then the neck of the ampoule is filed and broken off by wrapping the sawn end in a sterile gauze napkin.
To obtain a dose of 0.025 mg BCG-M in 0.1 ml, a sterile syringe with a long needle of 2 ml of 0.9% sodium chloride solution is transferred into an ampoule with a vaccine. The vaccine should be completely dissolved within 1 min after 2-3 times shaking.
No sediment or floc formation that does not break when shaken is allowed.
The reconstituted vaccine must be protected from sunlight and daylight (black paper cylinder) and consumed immediately after reconstitution. Unused vaccine is destroyed by boiling for 30 minutes, autoclaving at 126 ° C for 30 minutes or immersion in a disinfectant solution (5% chloramine solution) for 60 minutes.
For one vaccination, 0.2 ml (2 doses) of the diluted vaccine is taken with a sterile syringe, then 0.1 ml of the vaccine is released through a needle into a sterile cotton swab to displace the air and bring the piston to the desired graduation - 0.1 ml. Before each set of two doses, the vaccine must be gently mixed with a syringe 2-3 times. Only one child can be given the vaccine with one syringe.
The BCG-M vaccine is administered strictly intradermally at the border of the upper and middle third of the outer surface of the left shoulder after preliminary treatment of the skin with 70 ° alcohol. The needle is inserted with a cut upward into the surface layer of the stretched skin. First, a small amount of the vaccine is injected to make sure that the needle is inserted exactly intradermally, and then the entire dose of the drug (only 0.1 ml). With the correct injection technique, a whitish papule with a diameter of at least 7-9 mm should form, usually disappearing after 15-20 minutes.
The introduction of the drug under the skin is unacceptable, as this may form a cold abscess.
It is forbidden to bandage and treat with iodine and other disinfectant solutions of the vaccine injection site.
Reaction to the introduction
At the site of intradermal injection of the BCG-M vaccine, a specific reaction develops in the form of a papule 5-10 mm in diameter.
In newborns, a normal vaccine reaction occurs after 4-6 weeks. The reaction undergoes a reverse development within 2-3 months, sometimes over a longer period.
The site of reaction should be protected from mechanical irritation, especially during water procedures.
Complications after vaccination are rare and usually local in nature.
Contraindications for vaccination with BCG-M vaccine of newborns
1. Prematurity - birth weight less than 2000 g.
2. Vaccination is postponed in case of acute diseases and exacerbations of chronic diseases (intrauterine infection, purulent-septic diseases, hemolytic disease of newborns of moderate and severe form, severe lesions of the nervous system with pronounced neurological symptoms, generalized skin lesions, etc.) until the disappearance of clinical manifestations diseases.
3. Immunodeficiency state (primary).
4. Generalized BCG infection detected in other children in the family.
5. HIV infection in the mother.
Persons temporarily exempted from vaccinations should be taken under observation and registration, and vaccinated after complete recovery or removal of contraindications. If necessary, carry out the appropriate clinical and laboratory examinations.
Children who have not been vaccinated during the neonatal period receive the BCG-M vaccine after the abolition of contraindications.
Release form
In ampoules containing 0.5 mg of the drug (20 doses) complete with a solvent - 0.9% sodium chloride solution, 2 ml in an ampoule.
One pack contains 5 ampoules of BCG-M vaccine and 5 ampoules of 0.9% sodium chloride solution (5 sets).
The shelf life of the BCG-M vaccine is 1 year.
Storage and transportation conditions
The drug is stored at a temperature of 5-8 ° C.
Transportation by all types of transport at a temperature of 5-8 ° C.
IV. Complications after the introduction of the BCG and BCG-M vaccines
The causes of complications after immunization with a tuberculosis vaccine, in addition to biological properties strain, there may be violations of the technique of intradermal administration of the drug, indications for vaccination, as well as concomitant pathology in a child before vaccination and during the development of a local vaccination reaction.
Complications are divided into four categories:
Considering the importance of timely detection and the need for adequate measures in cases of complications after the administration of the BCG or BCG-M vaccine, the following set of organizational actions is shown for the timely detection of the disease, subsequent treatment and dispensary supervision for children with this pathology.
The algorithm (sequence) of the doctor's actions includes the following stages of examining the child after the administration of the anti-tuberculosis vaccine:
Stage 1. When examined by a pediatrician in a children's clinic, it must be remembered that every child vaccinated intradermally with a tuberculosis vaccine is examined by a pediatrician at the age of 1, 3, 6, 12 months before the local vaccination reaction heals. On examination, the pediatrician draws attention to the place of vaccine administration and the state of the regional (cervical, axillary, supra- and subclavian) lymph nodes.
Ulceration at the site of vaccine injection of more than 10 mm or an increase of more than 10 mm in one of the indicated peripheral lymph nodes, or prolonged, over 6 months, non-healing of the local vaccination reaction is an indication for referring the child to a consultation with a pediatric phthisiatrician. An additional examination by a pediatric phthisiatrician is shown also for children with axillary (axillary), supra-, subclavian lymphadenitis, revealed by chance during an X-ray examination of organs chest about a slight increase in the lymph node, "bend" of tuberculin reactions, hypersensitivity to tuberculin, symptoms of tuberculous intoxication, frequent colds, the presence of a bone focus, regarded as osteomyelitis, chronic synovitis and arthritis.
Stage 2. In the conditions of a children's polyclinic, a phthisiatrician, based on the clinical manifestations of the disease, determines the volume diagnostic activities to confirm the diagnosis. Clinical criteria for post-vaccination complications to distinguish them from nonspecific lesions are given below.
Lymphadenitis (regional, more often axillary (axillary), sometimes supra- or subclavian, occur mainly in children early age):
Swollen lymph nodes up to IV ("beans"), V ("hazelnut") and later - VI (" walnut") sizes;
The consistency of the lymph nodes is initially soft, elastic, later - dense;
Palpation of the lymph nodes is painless;
The skin above them is unchanged or pinkish;
It may be accompanied by caseification with a breakthrough of caseous masses outward and the formation of a fistula with moderate or profuse purulent discharge.
The infiltrate develops at the site of vaccine administration:
There may be ulceration in the center,
Size from 15 to 30 mm - and more;
It is accompanied by an increase in regional lymph nodes.
Cold abscess (scrofuloderma):
Tumor-like formation without changes in the skin above it;
Palpation is painless, fluctuation is determined in the center;
Often accompanied by a reactive enlargement of the axillary lymph nodes;
Ulceration (in case of untimely diagnosis of a cold abscess and its spontaneous opening).
Ulcer (defect of the skin and subcutaneous fat at the injection site):
The size of the ulcer is from 10 to 20-30 mm in diameter (its edges are undermined, infiltration around is weak, the bottom is covered with abundant purulent discharge).
Keloid scar (tumor-like formation at the injection site of various sizes, rising above the level of the skin). Unlike a scar that forms during the normal course of the vaccine process, a keloid:
Has a dense, sometimes cartilaginous consistency;
In the thickness of the keloid there are capillaries clearly visible when viewed;
The shape of the scar is round, elliptical, sometimes stellate;
The surface is smooth, glossy;
Coloring from pale pink, intense pink with a bluish tint to brownish;
It is accompanied by a feeling of itching in its area, painful sensations join the itching.
Ostitis - defeat skeletal system (clinical picture corresponds to the lesion). The criterion for suggesting a post-vaccination etiology of the process is the child's age from 6 months. up to 1 year and limitation of the lesion focus
In the conditions of a children's clinic, the following additional studies are carried out:
Laboratory methods: general analyzes blood and urine,
Tuberculin diagnosis: Mantoux test with 2 TE PPD-L (if the complication is diagnosed 12 months or later after immunization with the tuberculosis vaccine),
Plain chest x-ray.
Stage 3. After clinical and X-ray examination, the child with suspicion of a complication is sent to a specialized anti-tuberculosis department to verify the diagnosis and prescribe treatment.
In the conditions of the anti-tuberculosis dispensary, an additional X-ray tomographic examination and verification of the diagnosis are carried out.
Tomographic examination of the chest organs is shown:
In the presence of pathological changes on the plain chest x-ray, requiring tomography of the mediastinum to verify the diagnosis;
When detecting osteoarticular pathology.
If you suspect BCG osteitis, an additional plain radiographs the affected section in two projections that allow you to identify characteristic signs pathologies, regional osteoporosis, bone atrophy, foci of destruction in the epimetaphyseal regions of long tubular bones with shadows of dense inclusions, sequesters, contact destruction of articular surfaces, narrowing of the joint space, thickening of the shadows of the soft tissues of the joints.
To verify the diagnosis of BCGitis, mainly bacteriological methods are used (isolation of the pathogen culture with proof of its belonging to M. bovis BCG by determining its biological properties: growth rate, morphology, tinctorial properties, nitrate reductase test, catalase activity, drug resistance, with special treatment attention to drug susceptibility to cycloserine). Whenever possible, molecular biological methods for identifying the pathogen are also used.
If it is impossible to verify that the pathogen belongs to Mbovis BCG, the diagnosis of post-vaccination complications is established on the basis of a comprehensive examination (clinical, radiological, laboratory). After the diagnosis is made, the phthisiatrician, based on the clinical manifestations of the disease, determines the scope of measures for the treatment of the child and prescribes anti-tuberculosis therapy.
Treatment of post-vaccination complications is carried out by a phthisiatrician, in the conditions of an anti-tuberculosis dispensary, according to general principles treatment of a child with extrapulmonary tuberculosis, with individualization depending on the type of complication and the prevalence of the process. Hospitalization in a specialized hospital is indicated in case of impossibility of adequate therapy on an outpatient basis. Conducting any other preventive vaccinations during the treatment of a child (adolescent) for a complication is strictly prohibited.
The final 4 stage of the algorithm of medical measures after the diagnosis of post-vaccination complications at the site of BCG vaccine administration is informing about the identified complication of medical institutions dealing with these problems, namely:
Immediately notify the head of the medical institution and send an emergency notification to the center of state sanitary and epidemiological surveillance;
Prepare a "Card for registering a patient with complications after immunization with a tuberculosis vaccine" (Appendix 1) and send it to the Republican Center for Complications of an Anti-Tuberculosis Vaccine of the Ministry of Health of Russia at the Research Institute of Phthisiopulmonology of the Ministry of Health of Russia;
All cases of complications and unusual reactions or inconsistencies in the physical properties of the tuberculosis vaccine are reported to the GISK im. L.A. Tarasovich of the Ministry of Health of Russia.
V. Organization of vaccination of newborns
1. Organizes vaccination of newborns chief physician maternity hospital (head of the department).
2. The chief physician of the maternity hospital (department) assigns at least two nurses to undergo special training in the technique of administering the vaccine.
3. When sending an exchange card (registration form N 0113 / y) to the children's polyclinic, the maternity hospital (department) notes in it the date of intradermal vaccination, the series of vaccines, its expiration date and the name of the manufacturer.
4. The maternity hospital (department) informs the parents that 4-6 weeks after the intradermal vaccination, the child should develop a local vaccination reaction, upon the appearance of which the child must be shown to the local pediatrician. It is strictly forbidden to treat the place of reaction with any solutions and lubricate with various ointments.
5. Children born outside the maternity hospital, as well as newborns who, for whatever reason, have not been vaccinated, are vaccinated in a children's clinic (in children's department hospitals, at the feldsher-obstetric station) specially trained in the technique of intradermal vaccination by a nurse (paramedic).
To vaccinate newborns by the intradermal method in the children's room of the maternity hospital (department), you must have:
Refrigerator for storing BCG and BCG-M vaccines at a temperature not exceeding + 8 ° C.
Syringes 2-5 gram disposable for dilution of the vaccine - 2-3 pcs.
Disposable tuberculin syringes with a well-fitting piston and a thin short needle with a short oblique cut - at least 10-15 pcs. for one day of work.
Injection needles N 840 for vaccine dilution - 2-3 pcs.
Ethyl alcohol (70%) registration N 74 \ 614 \ 11 (12).
Chloramine (5%), registration N 67 \ 554 \ 250. Prepare on the day of vaccination.
All items necessary for intradermal vaccination should be kept locked in a separate cabinet. Using them for any other purpose is strictly prohibited.
When vaccinating children who were not vaccinated during the neonatal period, the polyclinic must additionally have instruments for conducting the Mantoux tuberculin test.
Vi. Organization of revaccination against tuberculosis
1. The Mantoux test with 2 TE PPD-L and anti-tuberculosis revaccination is carried out by the same composition of specially trained nurses in children's city, district and central district polyclinics, united in teams of 2 people.
2. The composition of the brigade and the schedules of their work are annually drawn up by the order of the chief physician of the corresponding medical and preventive institution.
3. Nurses on the team should be proficient in setting, evaluating Mantoux samples and administering vaccinations. Samples are administered by a single nurse, the sample should be evaluated by both team members, and vaccinations, depending on the number of persons involved, may be administered by one or both nurses. At the time of work, a medical worker of the institution is connected to the brigade, where they carry out mass tuberculin diagnostics and revaccination.
4. Local medical workers carry out sampling for samples and vaccinations, organize the flow, select and refer to the phthisiatrician persons in need of additional examination for tuberculosis; draw up documentation, draw up a report on the work done. Doctors of children's and adolescent institutions, employees of the state sanitary and epidemiological supervision and phthisiatricians control the work on the ground.
5. In the schedule of the work of the teams, it is necessary to provide for their repeated departure during the year to cover children and adolescents who were absent due to illness or had temporary medical dispensations during the first mass examination of the team.
6. In each anti-tuberculosis dispensary (department) there is a person responsible for anti-tuberculosis vaccinations, who is entrusted with monitoring the work of the district brigades, methodological assistance and revaccination of uninfected persons.
7. Full coverage of the contingents subject to anti-tuberculosis vaccinations, as well as the quality of intradermal revaccination, is ensured by the chief physician of the polyclinic, central and district hospitals, outpatient clinics, the district pediatrician, the chief physician of the anti-tuberculosis dispensary, the chief physician of the state center of sanitary and epidemiological surveillance and the persons directly performing this work ...
The chief doctors of the anti-tuberculosis dispensary (regional, district) should organize a doctor's appointment in the children's department for the treatment of children (early, school ages) with post-vaccination complications. Treatment should be carried out by a trained phthisiopediatrician, and children should be admitted on specific days.
Vii. Instrumentation for conducting the Mantoux test before revaccination and for revaccination
When using single-use tuberculin one-gram syringes, 150 syringes with well-fitting pistons with a short oblique cut are needed for one day of team work; 3-5 pieces of 2-5 gram syringes with needles for vaccine dilution. For a year, the number of syringes and needles is planned based on the number of persons subject to revaccination: for schoolchildren of the 1st grade - 50%; 9th grade - 30% of students.
List of reusable instruments:
Bix 18 x 14 cm for cotton wool - 1 pc.
Sterilizers - storage for 5.0 syringes; 2.0 gr. - 2 pcs.
Syringes 2-5 ml - 3-5 pcs.
Injection needles N 804 for extracting tuberculin from the vial and for diluting the vaccine - 3-5 pcs.
Anatomical tweezers 15 cm long - 2 pcs.
File for opening ampoules - 1 pc.
Millimeter rulers 100 mm long (made of plastic) - 6 pcs. or special calipers.
Vials for medicines with a capacity of 10 ml - 2 pcs.
Bottle with a capacity of 0.25-0.5 liters. for disinfectant solutions - 1 pc.
To carry out tuberculin diagnostics and revaccination in large collectives by the brigade method, when 2 nurses work simultaneously, in conditions of a continuous flow of examined persons, a set of instruments should be used in accordance with the "Instructions for the use of tuberculin samples".
Instrumentation for the production of a tuberculin test and revaccination must be separate and appropriately labeled. With one sterile syringe, tuberculin or BCG vaccine can only be given to one person.
VIII. Drawing up a vaccination plan and monitoring its implementation
1. Drawing up a plan for anti-tuberculosis vaccinations is entrusted to the chief doctors of the center of state sanitary and epidemiological surveillance, a maternity hospital, a children's and general clinic, an anti-tuberculosis dispensary (within the region and the scope of activities of each institution).
2. The consolidated plan of vaccinations against tuberculosis in the district, city, region is drawn up by the center of state sanitary and epidemiological supervision together with the chief pediatricians and anti-tuberculosis dispensaries.
3. In terms of revaccination in the district, city, region, provide:
registration of the number of children and adolescents subject to anti-tuberculosis vaccinations;
the calendar plan for the survey of the contingents and the BCG revaccination, taking into account the time of other vaccinations;
training of medical personnel for vaccinations and their instruction.
4. The registration of persons subject to vaccination in children's and adolescent groups is carried out by doctors of the general pediatric network serving these groups and institutions.
5. When drawing up a vaccination plan, the birth rate in a given district, city, revaccination plan is taken as a basis - the number of children, adolescents and adults subject to revaccination, taking into account the percentage of people who react negatively to the Mantoux test with 2 TE PPD-L.
6. Control over the implementation of the plan for anti-tuberculosis vaccinations in the field is carried out by the State Sanitary and Epidemiological Surveillance Center, to which a monthly report is submitted in form N 086 / at the institutions conducting the vaccinations.
7. The need for tuberculin is calculated on the basis of two doses of 0.1 ml for each examined person. It should be borne in mind that in ampoules of 3 ml - 30 doses - for examination 15 people. One liter of tuberculin contains 10,000 doses, which are used to examine 5,000 people.
8. The need for BCG and BCG-M vaccines for vaccination of newborns is calculated at the rate of 20-30 ampoules of dry tuberculosis vaccine for intradermal administration and solvent (included) per month per maternity ward, where 5-10 children are born per day. In this case, it is also necessary to take into account the presence of a 10- or 20-dose BCG vaccine.
One of the obligatory vaccines is BCG vaccination for children, which is given for the first time immediately in infancy - even in the hospital, 3-4 days after the birth of the baby. There are many myths about her, various gossip and stories about terrible consequences and complications. After listening to them, many parents take responsibility and refuse this vaccination without understanding it well. Although their first responsibility is to find out in detail from doctors what BCG is, and evaluate all the pros and cons of this vaccination.
What is BCG - a foreign abbreviation that stands for BCG - Bacillus Calmette, that is, bacillus Calmette-Guerin. Despite its obligation and relevance in modern world, not everyone has an idea of what BCG is and from what this vaccine is given. This is a vaccine against tuberculosis, it is prepared from a strain of a live, but weakened tuberculosis bacillus of a cow. It is not dangerous to humans, as it is specially grown in an artificial environment. Its main features: the goal is the prevention of tuberculosis; protects not from infection, but from the overflow of a hidden infection into an open disease; prevents the development of severe forms of the disease - tuberculous meningitis, infection of joints and bones, dangerous forms of lung infection; allows you to achieve a significant reduction in the percentage of morbidity among children.
Since all the importance of such vaccination is taken into account, the BCG vaccination in newborns is given as early as possible: in the absence of contraindications, even in the hospital. Then, if necessary, it is carried out twice more - this process is called revaccination. The more information parents know about why, where and when they are vaccinated with BCG, the calmer they will be. Vaccination One of the most exciting questions about vaccinations is how many times children are vaccinated with BCG. According to the generally accepted calendar, three times: 3–7 days immediately after the baby is born; at 7 years old; at 14. Sometimes in the maternity hospital, for some reason, vaccination against tuberculosis is not carried out (for example, the baby has some contraindications). If at 2 months the doctor still offers to be vaccinated, there will be no special problems. But after this period (for example, at 3 months), before that you will have to do a Mantoux test. And if only the result is negative, it will be possible to vaccinate. They do the same at the age of 7 and 14. This technique allows you to increase the immunity of a small organism to tuberculosis, to increase the percentage of resistance to the effects of mycobacteria. Moreover, revaccination at the age of 7 and 14 is mandatory if the child is in contact with a patient with tuberculosis (for example, someone among the relatives is infected).
The second question that worries parents is where the BCG vaccine is given to newborns and is it not dangerous. The usual injection site is the outer side of the left shoulder, the border between the upper and middle 1/3 of the shoulder is chosen. The vaccine is administered intradermally: subcutaneous and intramuscular injections are excluded. If there are any reasons that prevent the vaccine from being injected into the shoulder, a different place is chosen where there is a thick skin, into which an injection can be easily delivered - most often this is the thigh.
Despite the fact that all the information about BCG vaccination for newborns is open and available to parents today, there are still many refusals. The question is very relevant today, what is more in the BCG vaccination: benefits or harm to the health of the baby? Among the advantages are such as: minimum consequences; complications are rare; no hassle when caring for the injection site: parents often ask if it is possible to wet the BCG vaccine - yes, but do not scratch it or smear it with anything; reduces the risk of infection with a tubercle bacillus; when infected, it allows the disease to proceed in more easy form; does not allow death in tuberculosis. If this vaccination has so many positives, then why is it collecting so many negative reviews? There are reasons for this: a number of dangerous complications due to non-compliance with contraindications or incorrect administration of the vaccine; in rare cases - a slow tightening of the injection site: all parents are interested to know how long the BCG vaccination takes to heal, since this process takes place within a whole year after vaccination; widespread and persistent rumors that the BCG vaccine includes such components as formalin, mercury salts, phenol, polysorbate and even aluminum hydroxide - this information has no scientific basis.
The decision to vaccinate the baby is made by the parents, having previously weighed all the pros and cons, after a comprehensive examination is carried out for the presence of contraindications for BCG vaccination. After all, it is they in most cases that cause the development of further complications after vaccination. Contraindications The following contraindications exist for vaccination: prematurity (if the child weighs no more than 2,500 grams); diseases during an exacerbation (vaccination is given after recovery); intrauterine infection; hemolytic disease; purulent-septic diseases; neurological symptoms in severe lesions of the nervous system; large-scale skin lesions; malignant neoplasms; primary immunodeficiency; taking immunosuppressants; tuberculosis in other family members; radiation therapy; HIV infection in the mother. For revaccination (after 2 months) there is a slightly different list of contraindications: acute diseases; allergic reactions; immunodeficiency; questionable or positive Mantoux reaction; malignant neoplasms; radiation therapy; taking immunosuppressants; tuberculosis; complicated reaction to a previous vaccination; contact with a tuberculosis patient.
The doctor is obliged to identify the presence of these contraindications in the child before vaccinating him, since it is their non-observance that leads to violations of the norm and complications. It is by the reaction after the BCG vaccination that it is deciphered: whether the vaccination was successful, that is, whether the baby has developed immunity against tuberculosis. For a whole year, doctors observe what happens to the injection site: parents are also interested to know how BCG vaccination is deciphered in children.
Small organisms all react very differently to TB vaccination, so the consequences of BCG vaccination in children can be very different. It is useful for parents to know which of them are developing within the normal range and should not cause unnecessary worries, but which should be treated more attentively and promptly reported to the doctor. If the BCG vaccine turns red, this reaction is considered quite normal for a whole year after the vaccination. For some, this happens within a week, for some - by the end of the second month, and for others - only by six months. In this case, you should not immediately rush to a doctor's consultation, but it is necessary to inform the district pediatrician during a routine examination that the vaccination has turned red. Parents are especially frightened by the abscess formed at the injection site. Panic begins, as many have no idea what to do if the BCG vaccine festers some time after vaccination. Indeed, within several months an abscess with a white head in the middle forms at the puncture site. It gradually becomes covered with a crust, which can neither be torn off nor smeared with anything, and then it flies off by itself, and the site of inoculation is healed. So do not be alarmed if the BCG vaccine has festered - this does not mean at all that you did not properly care for it or that the baby has any health problems. Everything is as it should be. In rare cases, parents turn to doctors with such a problem that after a whole year after vaccination, their child does not have a scar after BCG vaccination, like most children. There may be several reasons for this phenomenon: the vaccine was injected incorrectly (that is, too deep, so no traces may remain on the surface), individual characteristics child's body, immunity to the bacillus was not formed. The most dangerous factor, which can provoke such a consequence, is the last reason. So, if after the BCG vaccination there is no trace on the baby's handle, an additional examination will be needed. Next, you will need to follow the doctor's recommendations, whether it is worth repeating the vaccination again. One of the consequences can be an increased temperature for several days after the BCG vaccination. If it is not critical and passes after 2-3 days, you do not need to be afraid: the body actively reacts in this way to the bacteria introduced into it. If the temperature is too high and lasts longer than 3 days, you should immediately contact for medical help... Associated with this consequence is the question of when it is possible to bathe a child after BCG vaccination: there are no contraindications for this (not to be confused with the Mantoux test). However, with elevated temperature it is better to wait for the body with water procedures so as not to aggravate the baby's condition. Such consequences of BCG vaccination in children are usually not dangerous and should not cause fear in parents. For complete peace of mind, you can always consult with your doctor about those reactions that cause concern. Throughout the first year of a child's life, regular, fairly frequent examinations by a pediatrician are carried out, with whom you can always consult about how the child's body's reaction to vaccination is going.
Sometimes there are serious complications after BCG vaccination, if the necessary contraindications have not been observed. So they are dangerous to the health of the child.
Before getting vaccinated, doctors are required to advise parents about the dangers of BCG vaccination if contraindications are not followed. Complications are so serious that they leave their mark on the whole life of a little man. However, prudent and literate parents should at the same time understand that this happens only if contraindications are not observed. To the most common side effects, dangerous for the life of children, include: lymphadenitis - inflammation of the lymph nodes means that mycobacteria have penetrated from the skin into the lymph nodes, which is unacceptable: if the diameter of the inflammation is more than 1 cm, you will need surgical treatment; too extensive, large-scale, and not local, as expected by the norm, the area of suppuration - this is usually associated with immunodeficiency; osteomyelitis can begin when using a low-quality vaccine; a cold abscess develops in 1–1.5 months. after vaccination, if the drug was injected subcutaneously instead of intradermally, it will require surgical intervention; an extensive ulcer with a diameter of more than 10 mm means that the child has a high sensitivity to the components of the drug - therapy is limited to local treatment, but information about such a complication is mandatory entered into a personal medical record; a keloid scar in the form of red, swollen skin at the injection site: it will be a signal to doctors that BCG cannot be injected into this child again; generalized BCG infection is a very rare but serious complication in the presence of immune disorders in children; osteitis (the so-called bone tuberculosis) develops 0.5–2 years after vaccination; it is also a rare, but very dangerous reflection of serious disorders in the immune system of babies.
Those parents who doubt whether or not their babies need to be vaccinated with BCG are usually even more frightened after such an impressive list of complications and refuse to vaccinate. Much also depends on the doctors, who must give the parents all the necessary explanations. There are no contraindications - no and dangerous consequences... But there will be confidence that the child's body is protected from such a terrible disease as tuberculosis, if not 100%, then at least only a mild form of the disease is guaranteed. You need to weigh the pros and cons before making such a responsible decision on which the health of your baby will depend.
Despite great medical advances in prevention dangerous diseases, about 10 million cases of tuberculosis are recorded annually. The TB vaccine is one of the first to be given right after birth. BCG is a complex vaccine against tuberculosis, which allows you to develop strong immunity to the disease. Its introduction requires examination of newborns and the creation of favorable conditions for vaccination. Unfortunately, there is no absolute guarantee that a vaccinated child will not develop tuberculosis in the future.
The history of breeding the desired strain of mycobacteria has almost a century of history. It was created by two scientists from France, figures of microbiology - Calmette and Guerin - in the second decade of the 20th century. BCG is shorthand. On Latin the decoding of the abbreviation looks like "bacillus Calmette-Guerin" or BCG.
The vaccine is based on the bovine tubercle bacillus. The bacterium that causes "pearl disease" in livestock is well adapted to human body... It is processed in such a way that it is not able to infect, but retains the ability to form protective immunity. The BCG vaccine is not dangerous, but there are rare cases of complications based on the individual's response to the bacterium.
What does BCG vaccine look like, its composition and form of release?
The BCG composition remained the same as it was created and was first used on humans in 1921. The work on the removal of the desired strain lasted more than 10 years. All research data in the course of searching for the desired subtype of mycobacteria are stored in the WHO archives.
The main method for obtaining bacteria of the desired type is sowing in a nutrient medium. The required number grows a week. To get the desired homogeneous mass, a lot of manipulations are carried out. The finished vaccine against tuberculosis includes not only live bacteria, but also dead ones.
The modern BCG vaccine contains the same strains:
- Tokyo 172;
- Danish 1331;
- French "Pasteur" 1173 P2;
- Strain "Glaxo" 1077.

The effectiveness of drugs is manifested in equally... In our country, vaccination against tuberculosis is carried out in two formulations - BCG and BCG-M. It is imperative to take into account the individual indications of the body when using a particular vaccine.
pharmachologic effect
The need for BCG vaccination in newborns is due to the risk of developing the disease. The effectiveness of the development of persistent immunity depends on the timing of the introduction of the vaccine against tuberculosis. The most pronounced resistance immune system in front of the carrier of the disease manifests itself in the case of a child being vaccinated in the first week of life.
The final immunity will form a year after vaccination, and it will last for more than seven years.
A scar at the site of inoculation is a consequence of local skin tuberculosis. If it is clearly visible, it means that the body has developed a strong immune defense. If the scar did not appear or is hardly noticeable, the result suggests otherwise.
Terms of sale, storage and shelf life
The tuberculosis vaccination is free of charge. If for some reason it was not done in the first days of life, you can do it yourself in a specialized institution. The vaccine is freely available in the pharmacy network. It is important to comply with the storage and transportation conditions. No prescription required to purchase. The purchase is accompanied by the issuance of a certificate, which is presented at the place of vaccination.
Storage and transportation of BCG and BCG-M is carried out in special refrigerating chambers with temperatures from +2 to +8 degrees Celsius. Direct sunlight should not be allowed on boxes with ampoules. Violation of these conditions leads to damage to the vaccine.
The shelf life of both types of vaccine is the same and is two years. The tuberculosis vaccine is not given after the specified period. Ampoules are disposed of physically or chemically. Vessels that have been stored or transported in an improper way are also subject to destruction.
To get the vaccine, the area of skin with the greatest density is selected. BCG is injected intradermally; administration of the vaccine subcutaneously or into muscle tissue is strictly contraindicated. As a result of improper injection, a mass with a large accumulation of pus is formed.
Vaccination can only be performed by a qualified specialist. It is important to quickly and accurately follow the correct sequence of actions, according to the instructions. Only whole ampoules are used, on which the expiration dates are clearly read. The contents of the solvent vial must be free of sediment. The vaccine itself is dry, in the form of a powder from white to cream shade.
Before breaking the ampoule, it must be sterilized with a napkin. The diluent is added to the vaccine with a syringe. A special tuberculin syringe is used to carry out the vaccination.

The BCG vaccination technique must be followed. The injection site is being processed ethyl alcohol... The intradermal route involves an injection at a 15-degree angle with a slow injection of the vaccine. The skin at the site of inoculation is not processed.
Within half an hour from the moment of vaccination, the patient is subject to monitoring for the occurrence of allergic reactions. This time is sufficient for manifestation in most cases. If the drug is well tolerated and there is no allergy, the patient can be free. It is forbidden to wet the vaccine for a day.
Information about the date of vaccination and the series of vaccines is entered into the development chart of the child. Within 6-8 weeks, the formation of immunity occurs. Until the end of the specified period, the child is prohibited from contacting an adult at risk of tuberculosis.
Where to get vaccinated against tuberculosis, where the injection is given and in which arm
An incorrectly given tuberculosis vaccine can backfire. First of all, the injection site and the hand matter.
The injection point is the border between the upper and middle lobes of the shoulder. If the composition of the BCG vaccine cannot be injected into this place, the vaccination is performed in the left thigh, also choosing the border and the injection site. The tuberculosis vaccine given to the thigh or shoulder has the same immune response.
BCG-M is the same vaccine, only weakened. Differs in BCG-M concentration. One dose contains half the mycobacteria. 0.1 milliliter of BCG-M vaccine contains only 0.025 milligrams of active bacteria. Instructions for application of BCG-M and the grafting technique - like that of BCG.

Who is the BCG vaccine shown to, what is it for?
- newborns up to 12 months of age in subjects with a large number of cases of tuberculosis;
- newborns, as well as children under 15 years old, in subjects with a small number of cases of tuberculosis;
- adults in contact with tuberculosis patients, especially in its resistant form.
The need for early vaccination childhood justified by the fact that it is in newborn children that tuberculosis develops into severe forms, which almost always lead to death.
Vaccination against tuberculosis does not guarantee complete protection against the disease, but the developed immune defense after vaccination prevents the development of severe forms that lead to death.
When BCG is given, vaccination schedule for newborns and older children
Within the territory of Russian Federation the National Calendar of preventive vaccinations for children has been developed, where the timing of vaccinations is prescribed. Vaccination against tuberculosis is mandatory and is included in the schedule three times:
- before discharge at the hospital, on the 5th ... 7th days;
- at 7 years old (if indicated);
- at the age of 14 (with testimony).
Russia is among the countries where the likelihood of contracting tuberculosis is high. Because of this, BCG is done in the maternity hospital for newborns, for everyone, without exception, who have no contraindications. More developed countries, with a small percentage of cases, vaccinate only those children who are at risk.
All newborns are vaccinated against tuberculosis without contraindications in the period from the 3rd to the 7th days from the moment of birth. Before manipulation, children are examined by a pediatrician. Vaccinations are performed in a specially designated office.

It is mandatory to vaccinate newborns in Russia, because more than half of the country's population in adulthood can be carriers of mycobacteria. Statistics show that over 70 percent of children develop tuberculosis in the first seven years of life. Lack of vaccination during infection leads to the development of meningitis with severe damage to the nervous system or extrapulmonary forms of the disease.
What to do if the vaccine was not given at the hospital
If, for some reason, the BCG vaccination in the hospital was not carried out, it is important to perform it without fail up to a year. When it is possible to get vaccinated, only a doctor can calculate, based on the determination of the necessary parameters and taking into account contraindications. In such cases, the vaccination schedule is drawn up individually.
If the BCG vaccination is not done, then when the child reaches two months, a Mantoux test is put before it. It allows you to detect the presence of antibodies to the causative agent of tuberculosis. You can vaccinate a baby only with a negative reaction. A positive result indicates infection. Accordingly, a thorough examination is required to prevent the development of severe forms of the disease.
Vaccinations against tuberculosis for children
If the child was vaccinated in a timely manner, the Mantoux result may be negative. Then, at the age of seven and fourteen, a mandatory revaccination is carried out. The lack of a reaction indicates that the body has not developed immune defenses, which means that the child may be susceptible to infection.
BCG vaccination is performed two to three days after hepatitis B vaccination. While the body is developing a reaction to the vaccine, it is forbidden to enter other vaccinations (6-8 weeks).

During pregnancy and lactation
The use of BCG vaccine is prohibited during pregnancy and breastfeeding.
BCG: how many times do it in life
Due to the fact that immunity from vaccination lasts for 7 years, it is done three times: in the first week of life - vaccination, at 7 years - BCG revaccination and at 14 years - another revaccination. Statistics show that a sharp increase in the number of patients is associated with the beginning of visits to children's educational institutions... The peak occurs at the age of 14 years. Every year, to prevent mass morbidity in children, the Mantoux test is performed.
Is it worth getting the BCG vaccine?
Vaccination is mandatory, but no one can force parents to do it either. There must be very good reasons for refusal, for example, serious contraindications. The developed countries boast a good epidemiological situation in terms of the spread of tuberculosis. However, do not forget that the main transmission route is airborne. Therefore, a person can become infected simply by being in a public place.
How BCG vaccination heals
Immediately after the administration of the BCG vaccine to the newborn, a white papule forms at the injection site. After 15-20 minutes after vaccination, it disappears. The vaccine takes a long time to heal. The body's immune response is developed due to the formation of a local tuberculous focus at the injection site.
The reaction proceeds in different ways - redness, suppuration, hyperemia. In this regard, the stages of healing are distinguished.
Healing stages
Immunity is formed within 45 days from the date of vaccination. A month after vaccination, redness or a bump may develop at the injection site. A bubble of fluid or even pus may appear. This is a completely normal reaction to the injected vaccine. The formation that has appeared may begin to boil, therefore, itching will appear. Scratching of the wound, as well as pressure on the injection site, should not be allowed.

When the reaction is over, a crust forms at the site of the abscess. When it falls away, you can see the scar from BCG - the one that adorns left hand all children and adults.
The more active the reaction and the larger the scar, the longer the immunity to tuberculosis is formed in the body.
What to do after BCG vaccination. Care features
It is important to follow some rules after vaccination. On the first day, you cannot wet the injection site. During the period of inflammation and abscess in the injection area, it is impossible to treat with disinfectants, as well as iodine. When pus flows out, do not wash the wound or apply bandages. To avoid infection, do not scratch the site of inflammation. For the same reason, you cannot tear off the formed crust on your own.
BCG vaccination - reactions and complications
There are often different reactions to the BCG vaccine. Their complexity and nature is also influenced by the quality of the vaccine itself. In some newborns, within half an hour after the BCG vaccination, allergic reaction... If it is not there, then everything is fine.
The next reaction, as a rule, appears after a month, when there is a habituation to the introduced strain of bacteria. The reaction occurs according to the scheme:
- inflammation with the formation of a small tubercle;
- sore at the injection site with the formation of a crust;
- scar formation.
If the vaccine is not given correctly, a cold abscess can form. Required medical treatment... As complications, general malaise associated with an abscess abscess and the manifestation of severe soreness can also appear.
No trace of BCG injection
The effect of the vaccine after the vaccination can be assessed after 1, 3, 6 and 12 months. As a rule, a scar is formed. But its absence is also possible. In such cases, there is a mandatory re-vaccination of BCG children by age. The absence of a scar indicates the ineffectiveness of the vaccination performed and the lack of formation of immunity to tuberculosis.

Formation of immunity after vaccination
The final formation of immunity after vaccination occurs after 2 months. If there is a risk of infection from others, the child should be isolated from them until the end of this period. The maximum duration of immune protection after BCG vaccination is 7, and in some cases even more, years.
How long can you get other vaccinations
No other vaccine injections should be given for 45 days after the BCG vaccination.
Where to get the BCG vaccine
Vaccination against tuberculosis is done at the hospital. If it was not completed in a timely manner, then it can be done in the TB dispensary. Medical institutions also have the right to carry out this manipulation, but only in cases where there is a special permit, equipped premises and qualified personnel. It is possible to perform the injection of the strain by a specialist with a visit to the house for a set fee.
Revaccination of BCG
Revaccination against tuberculosis is required. It is carried out at the age of 7 due to the end of the immune protection from the first vaccination. At this age, the child enters school, which means that he is surrounded by new people who may be carriers of the bacteria.

At the age of 14, BCG revaccination is carried out only if there is a negative Mantoux reaction, which indicates a lack of immunity to tuberculosis.
Which countries are vaccinated against tuberculosis
Vaccination against tuberculosis is carried out in all newborns in most countries of the world with an increased epidemiological risk of contracting this disease, including India, China, Japan, Brazil, Mexico. Russia is one of them. In some developed countries, vaccinations are given only to children at risk.
Price where to buy
You can buy the vaccine at most pharmacies. However, when transporting it, certain temperature conditions must be observed. You can order through specialized pharmacy points with delivery to the points of issue. All the conditions will be met there. The price for the vaccine varies within 400 rubles per package.
Analogs
Today you can find analogues of the Russian vaccine for vaccination against tuberculosis. These are imported medicines, which may not differ in the quality of the developed immunity. It should be borne in mind that from abroad, these drugs travel a long way, in which the necessary conditions of transportation and storage cannot always be observed.
Live mycobacteria of the BCG-1 strain, multiplying in the body of the vaccinated, lead to the development of long-term immunity to tuberculosis.
Release form
In ampoules containing 0.5 mg of the drug (20 doses) complete with a solvent - sodium chloride solution for injection 0.9%, 2 ml in an ampoule. One pack contains 5 ampoules of BCG-M vaccine and 5 ampoules of sodium chloride solution for injection 0.9% (5 sets).
Composition
For 1 dose:
Live mycobacteria of the BCG-1 vaccine strain - 0.025 mg of BCG microbial cells.
Excipient: sodium glutamate monohydrate (stabilizer) - no more than 0.15 mg.
1 dose is 0.1 ml of a diluted suspension.
The product does not contain preservatives or antibiotics.
It is produced complete with a solvent - sodium chloride solution for injection 0.9%.
Indications for use
Active specific prevention of tuberculosis
Contraindications
- Prematurity of a newborn - birth weight less than 2000 g.
- Acute diseases... Vaccination is postponed until the end acute manifestations diseases and exacerbations of chronic diseases (intrauterine infection, purulent-septic diseases, hemolytic disease of newborns of moderate and severe form, severe lesions of the nervous system with severe neurological symptoms, generalized skin lesions, etc.).
- Immunodeficiency state (primary), malignant neoplasms.
- When prescribing immunosuppressants and radiation therapy, the vaccination is carried out no earlier than 6 months after the end of treatment.
- Generalized BCG infection found in other children in the family.
- HIV infection in a child with clinical manifestations secondary diseases.
- HIV infection in a mother of a newborn who did not receive antiretroviral therapy during pregnancy.
Dosage regimen and method of administration
BCG-M vaccine is used intradermally at a dose of 0.025 mg in a volume of 0.1 ml.
BCG-M vaccine is vaccinated:
- In maternity hospitals of all healthy newborns on the 3rd-7th day of life on the eve of or on the day of discharge from the hospital in territories with an incidence rate of tuberculosis not higher than 80 per 100,000 population;
- In maternity hospitals for premature infants weighing 2000 grams or more, when the original body weight is restored, on the eve or on the day of discharge from the hospital;
- In the nursing departments of premature newborns of medical hospitals (2nd stage of nursing) - children weighing 2300 g or more before discharge from the hospital;
- In children's polyclinics for children who have not received anti-tuberculosis vaccination in the maternity hospital for medical contraindications and are subject to vaccination in connection with the removal of contraindications.
Children aged 2 months and older need a preliminary Mantoux test with 2 TU PPD-L before vaccination. Children with a negative reaction to tuberculin are vaccinated. The reaction is considered negative in the absence of infiltration (hyperemia) or the presence of a prick reaction (1.0 mm). The interval between the Mantoux test and vaccination should be at least 3 days and no more than 2 weeks.
Vaccinations should be carried out by specially trained medical personnel of maternity hospitals (departments), nursing units for premature babies, children's clinics or feldsher-obstetric points. Vaccination of newborns is carried out in the morning in a specially designated room after the children are examined by a pediatrician. In polyclinics, the selection of children for vaccination is preliminarily carried out by a doctor (paramedic) with mandatory thermometry on the day of vaccination, taking into account medical contraindications and anamnesis data. If necessary, consult with specialist doctors, blood and urine tests. In order to avoid contamination with live BCG mycobacteria, it is unacceptable to combine vaccination against tuberculosis with other parenteral procedures on the same day.
The fact of the vaccination is recorded in the established registration forms indicating the date of vaccination, manufacturer, batch number and expiration date of the vaccine.
The vaccine is dissolved immediately before use sterile
sodium chloride solution for injection 0.9%, attached to the vaccine. The solvent must be transparent, colorless and free of foreign matter.
The neck and head of the ampoule are wiped with alcohol. The vaccine is sealed under vacuum, so first file and carefully, using tweezers, break off the seal. Then the neck of the ampoule is filed and broken off by wrapping the sawn end in a sterile gauze napkin.
2 ml of sodium chloride solution for injection 0.9% is transferred to the ampoule with the vaccine with a sterile syringe. The vaccine should dissolve within 1 min. The presence of flakes is allowed, which should break with 2-4-fold stirring with a syringe. The dissolved vaccine looks like a turbid, coarsely dispersed suspension of light yellow color. If there are large flakes in the diluted preparation that do not break with 3-4-fold mixing with a syringe, or if the vaccine is not used, the ampoule is destroyed.
The reconstituted vaccine must be protected from sunlight and daylight (for example, with a black paper cylinder) and used immediately after reconstitution. The diluted vaccine is suitable for use for no more than 1 hour when stored under aseptic conditions at a temperature of 2 to 8 ° C. Be sure to keep a protocol indicating the time of dilution of the drug and destruction of the ampoule with the vaccine.
For one vaccination with a tuberculin syringe, 0.2 ml (2 doses) of the diluted vaccine is taken, then 0.1 ml of the vaccine is released through a needle into a sterile cotton swab in order to displace the air and bring the syringe plunger to the desired graduation - 0.1 ml. Before each set, the vaccine should be gently mixed 2-3 times with a syringe. Only one child can be given the vaccine with one syringe.
The BCG-M vaccine is administered strictly intradermally at the border of the upper and middle third of the outer surface of the left shoulder after preliminary skin treatment with 70% alcohol. The needle is inserted with a cut upward into the surface layer of the stretched skin. First, a small amount of the vaccine is injected to make sure that the needle is inserted exactly intradermally, and then the entire dose of the drug (only 0.1 ml). With the correct injection technique, a whitish papule with a diameter of 7-9 mm should form, usually disappearing after 15-20 minutes.
Precautions for use
The introduction of the drug under the skin is unacceptable, as this results in a "cold" abscess.
For vaccination, disposable sterile tuberculin syringes with a capacity of 1 ml with thin needles with a short cut are used. A disposable sterile syringe with a capacity of 2 ml with a long needle is used to add the solvent to the ampoule with the vaccine. It is forbidden to use syringes and needles that have expired and insulin syringes that do not have a graduation in ml. It is forbidden to vaccinate with a needleless injector. After each injection, a syringe with a needle and cotton swabs are soaked in a disinfectant solution (5% Chloramine B solution or 3% hydrogen peroxide solution), and then centrally destroyed. It is forbidden to use for other purposes the instruments intended for the vaccination against tuberculosis. The vaccine is stored in a refrigerator (locked) in the vaccination room. Persons not related to vaccination are not allowed into the vaccination room.
Vaccine ampoules are carefully examined before opening.
The drug should not be used for:
- the lack of labeling on the ampoule or incorrect filling of the labeling (must contain the abbreviated name of the drug (BCG-M vaccine), the number of doses, dosage - 0.025 mg / dose, batch number (alphanumeric designation), release date, expiration date);
- expired shelf life;
- the presence of cracks and notches on the ampoule;
- changes in the physical properties of the drug (color change, etc.).
It is forbidden to apply a bandage and treatment with iodine solution and other disinfectant solutions of the vaccine injection site during the development of a local vaccination reaction: infiltration, papules, pustules, ulcers, which should be sure to warn the child's parents.
More full information on the vaccine prevention of tuberculosis is presented in the Order of the Ministry of Health of Russia No. 109 "On improving anti-tuberculosis measures in the Russian Federation" dated March 21, 2003.