Russian recommendations for the treatment of acute coronary syndrome. Algorithm for the treatment of OX with the lifting of the ST segment - presentation. Biochemical myocardial damage markers
Update: October 2018
Under the term "acute coronary syndrome" implies a very life-threatening emergency condition. In this case, blood flow on one of the arteries that feed the heart decreases so much that a larger or smaller portion of myocardium or ceases to normally perform its function, or dies at all. The diagnosis is commemorate only during the first day of the development of this state, until the doctors differentiate - in humans did not appear stable angina Or it is the beginning of myocardial infarction. At the same time (while diagnostics), cardiologists take all possible measures to restore the damaged artery.
Acute coronary syndrome requires provision emergency care. If we are talking about myocardial infarction, then only for the first (from the appearance initial symptoms) 90 minutes can also be introduced a drug that solubles a thrombus in the body of the artery. After 90 minutes, doctors can only help the organism in every way to reduce the area of \u200b\u200bthe dies, maintain the main life functions and try to avoid complications. Therefore, a sudden heart pain has developed when it does not pass within a few minutes of rest, even if this symptom appeared for the first time, requires an immediate ambulance call. Do not be afraid to seem like a panicker and seek medical help, because with each minute, irreversible changes in myocardium accumulate.
Next, we will look at what kind of symptoms, except pain in the heart, you need to pay attention to what you need to do before the "ambulance" arrival. We will tell us about whether there have more chances of the development of acute coronary syndrome.
Learn more about Terminology
Currently, under acute coronary syndrome, two states showing similar symptoms are implied:
Unstable angina
Unstable angina - a condition in which on the background exercise Or rest appears pain for the sternum, having a pressure, burning or compressive character. Such a pain puts in the jaw, left, left blade. Maybe she manifests itself with their stomach pains, nausea.
About unstable angina say when these symptoms or:
- only originated (that is, before the person performed the load without heart pain, shortness of breath or unpleasant sensations in the stomach);
- began to occur at a lower load;
- have become stronger or last longer;
- began to appear alone.
At the heart of the unstable angina - a narrowing or spasm of the lumen of a greater or smaller artery that is powered, respectively, a greater or smaller portion of myocardium. Moreover, this narrowing should be more than 50% of the diameter of the artery in this area, or an obstacle on the path of blood (it is almost always an atherosclerotic plaque) is not fixed, but hesitates with blood current, then more, then less overlapping the artery.
Myocardial infarction
Myocardial infarction - without lifting ST segment or with the rise of this segment (it is possible to determine only by ECG). It occurs when more than 70% of the diameter of the artery is blocked, and in the case when "flying" plaque, a thrombus or a drop of fat clocked the artery in a particular place.
Acute coronary syndrome without lifting segment ST is either unstable angina, or infarction without lifting this segment. At the stage before hospitalization in a cardiological hospital, these 2 states do not differentiate - for this there are no necessary conditions and equipment. If the Cardiogram is visible to the rise of the ST segment, you can make a diagnosis of "acute myocardial infarction".
From how there will be a type of disease - with the rise of ST or without it - and the treatment of acute coronary syndrome depends.
If the ECG is immediately visible to the formation of a deep ("infarction") q teeth, a diagnosis of "Q-infarction of myocardium" is made, and not acute coronary syndrome. This suggests that the large branch of the coronary artery is amazed, and the focus of the dieting myocardium is quite large (large-quality myocardial infarction). Such a disease occurs with the complete blockage of the large branch of the coronary artery with a dense thrombotic mass.
When you need to suspect a sharp coronary syndrome
An alarm need to beat if you or your relative presents the following complaints:
- Breastache painwhose distribution is shown by a fist, not a finger (that is, a large plot hurts). The pain is burning, poury, strong. It is not necessarily determined to the left, but can be localized in the middle or on the right side of the sternum. Gives in the left side of the body: half the lower jaw, hand, shoulder, neck, back. Its intensity does not change depending on the position of the body, but may (this is characteristic of the syndrome with the segment of ST) there are several attacks of such pain, between which there are several practically painless "gaps".
It is not removed by nitroglycerin or similar drugs. Fear is joined to the pain, the sweat is in the body, may be nausea or vomiting. - Dyspneawhich is often accompanied by a feeling of a shortage of air. If this symptom develops as a sign of edema of the lungs, then grinding is growing, cough appears, pink foaming mocot can be cleaned.
- Violations of rhythmthat are felt like interruptions in the work of the heart, discomfort in the chest, sharp shoes of the heart of the edges, pauses between cardiac abbreviations. As a result of such nertrum cuts, in the worst case, the loss of consciousness occurs, in the best - the headache is developing, dizziness.
- The pain can be felt in the upper stomach departments and accompanied by the relaxation of the chair, nausea, vomitingwhich does not bring relief. It is also accompanied by fear, sometimes - the feeling of a rapid heartbeat, a neurotic reduction in the heart, shortness of breath.
- In some cases, acute coronary syndrome can begin with loss of consciousness.
- There is a variant of the course of acute coronary syndrome, manifested dizziness, vomiting, nauseaIn rare cases - focal symptomatic (asymmetry of the face, paralysis, paresis, violation of swallowing, and so on).
A wrapping should also be enhanced or the frequent pain for the sternum, about which a person knows that it is so manifolds his angina, intensified shortness of breath and fatigue. After a few days or weeks after that, 2/3 people develop acute coronary syndrome.
Particularly high risk of developing acute cardiac syndrome in such people:
- smokers;
- overweight persons;
- abusant alcohol;
- fans of saline dishes;
- leading low-wear lifestyle;
- coofers;
- having a violation of lipid metabolism (for example, high levels of cholesterol, LDL or LPONP in blood analysis on a lipidogram);
- with a diagnosis of atherosclerosis;
- with a diagnosis of unstable angina;
- if in one of the corneous (which feed the heart) arteries are determined atherosclerotic plaques;
- which have already transferred myocardial infarction;
- lovers have chocolate.
First aid
Assistance should be started at home. At the same time, the first action should be a "ambulance". Next, the algorithm is as follows:
- It is necessary to put a person on the bed, on the back, but at the same time the head and shoulders should be raised, making up an angle of 30-40 degrees with a torso.
- Clothes and belt need to unbutton so that the breath of man does not constrain anything.
- If there are no signs of pulmonary edema, give a person 2-3 aspirin tablets ("Aspectant", "Aspetor", "Cardiomagnet", "Aspirin-Cardio") or "clopidogrel" (that is, 160-325 mg aspirin). They must be checked. This is how the probability of dissolution of the thrombus increases, which (by itself, or layering on an atherosclerotic plaque) overlap the clearance of one of the arteries that feed the heart.
- Open the windows or windows (if necessary, the person needs to be covered): so the patient will receive more oxygen.
- If blood pressure is more than 90/60 mm Hg, give a man 1 nitroglycerin tablet under the tongue (this drug expands the vessels that feed the heart). Repeated nitroglycerin can be given 2 more times, with an interval of 5-10 minutes. Even if after 1-3 times the reception, the person has become better, the pain passed, to refuse hospitalization in no case!
- If a person has taken preparations from a group of beta blockers ("Anaprilin", "Metoprolol", "Atenolol", "Corvitol", "Bisoprolol"), after Aspirin, he needs to give 1 tablet of this drug. It will reduce the need of myocardial in oxygen, giving him the opportunity to recover. Note! The beta-blocker can be given if the blood pressure is greater than 110/70 mm Hg, and the pulse is more often 60 shots per minute.
- If a person takes antiarrhythmic drugs (for example, "arrhythmila" or "cordaron"), and it feels a violation of the rhythm, you need to take this tablet. In parallel, the patient himself should begin deeply and strongly cough until the "ambulance" arrival.
- All the time before the "ambulance" arrive next to the person, watching his condition. If the patient is in consciousness and feel a sense of fear, panic, it needs to calm down, but not to disappear by Valerian-mother (resuscitation may need, and it can only interfere with the full stomach), and soothe words.
- In convulsions, a number of people should help ensure permeability respiratory tract. For this, it is necessary, taking over the corners of the lower jaw and the area under the chin, move the lower jaw so that lower teeth turned out to be ahead of the top. From this situation you can make an artificial respiration to the mouth into the nose, if self-breathing is gone.
- If a person stopped breathing, check the pulse on the neck (from two sides of the Kadyk), and if there is no pulse, proceed to perform resuscitation activities: 30 pressing straight hands on the bottom of the sternum (so that the bone is shifted down), after which - 2 inhale in the nose or mouth. At the same time, the lower jaw should be kept for the area under the chin so that the lower teeth be ahead of the upper.
- Find ECG and preparations that take the patient to show them to medical professionals. It will be necessary for them not primarily, but it will be necessary.
What should do the ambulance doctors
Medical assistance in acute coronary syndrome begins with simultaneous actions:
- provision of vital functions. For this, oxygen is supplied: if the breath is independent, then through the nasal cannula, if there is no breathing, then spend the intubation of the trachea and artificial ventilation. If blood pressure is critical, start to enter into a vein special preparationswho will increase it;
- parallel registration of electrocardiogram. They look through it, there is a rise of ST or not. If there is a lift, then if there is no possibility of rapid delivery of a patient to a specialized cardiological hospital (provided that sufficient staffing of the team who left the brigade) can begin to carry out thrombolysis (tomb dissolution) in conditions outside the hospital. In the absence of a lift St, when the probability that clogged the artery of the Fresh Trombus, which can be dissolved, is taken into a cardiological or multidisciplinary hospital, where there is a resuscitation separation.
- elimination of pain syndrome. For this, narcotic or nonarcotic pain relief drugs are administered;
- in parallel, with the help of express tests (strips, where a drop of blood is dripped, and they show, negative result or positive) the level of troponins is determined - Markers of myocardial necrosis. Normally, the level of troponins must be negative.
- if there are no signs of bleeding, anticoagulants are injected under the skin: "Kleksan", "Heparin", "Fractional" or others;
- if necessary, "nitroglycerin" or "flavor" is introduced intravenously;
- an introduction of intravenous beta blockers may also begunreducing the need of myocardium in oxygen.
Note! Transport the patient into the car and from it can only be in a lying position.
Even the lack of changes to the ECG against the background of complaints characteristic of acute coronary syndrome is an indication of hospitalization in a cardiological hospital or separation of intensive therapy of a hospital in which there is a cardiology department.
Treatment in hospital
- Against the background of continuing therapy, needed to maintain vital functions, re-remove the ECG in 10 leads.
- Repeated, already (preferably) the quantitative method, determine the levels of troponins and other enzymes (MB creatine phosphocainos, asthma, moglobin), which are additional markers of myocardial death.
- When lifting the ST segment, if there are no contraindications, the thrombosis procedure is carried out.
Contraindications to thrombolesis are such conditions:- internal bleeding;
- card and brain injury, transferred less than 3 months ago;
- "Top" pressure above 180 mm Hg.st. or "lower" - above 110 mm Hg;
- suspicion of aortic bundle;
- transferred stroke or brain tumor;
- if a person has long been taking anticoagulant drugs (thinning blood);
- if there was an injury or any (even laser correction) operation in the next 6 weeks;
- pregnancy;
- aggravation of ulcerative disease;
- hemorrhagic eye diseases;
- the last stage of cancer of any localization, severe degrees of lack of liver or kidney.
- In the absence of lifting the ST segment or its decrease, as well as in the inversion of the teeth T or the newly emerging blockade of the left leg of the beam of Gis, the question of the need for thrombolysis is solved individually - on the Grace scale. It takes into account the age of the patient, the frequency of its heart abbreviations, the level of blood pressure, the presence of chronic heart failure. In the calculation, it was also taken if there was a stop of the heart before entering whether ST is elevated, high whether troponins. Depending on the risk on this scale, cardiologists decide whether there is indications for conducting therapy that dissolves the thrombus.
- Myocardium damage markers determine every 6-8 hours in the first day, regardless of whether thrombolytic therapy was carried out or not: they are judged by the process dynamics.
- Other works of the body are defined: levels of glucose, electrolytes, urea and creatinine, lipid metabolism. Radiography of the chest ulness organs is performed to assess the state of the lungs and (indirectly) heart. Heart ultrasound with doppler photography is carried out - to assess the blood supply to the heart and its current state, to predict the development of such complications as the aneurysm of the heart.
- Strict bed regime - in the first 7 days, if the coronary syndrome ended with the development of myocardial infarction. If a diagnosis of unstable angina, a person is allowed to get up earlier - for 3-4 days of the disease.
- After transferred acute coronary syndrome, several drugs are prescribed for permanent reception. These are inhibitors angiotensin-converting enzyme ("Enalapril", "Lisinopril"), statins, bloodstanding agents ("Prasugrel", "Clopidogrel", "Aspirin-Cardio").
- If necessary, for prevention sudden deathMounted artificial rhythm driver (pacemaker).
- After some time (depending on the state of the patient and the nature of changes to the ECG), if there are no contraindications, such a study is carried out as coronary artwork. This is a radiological method, when through the catheter, conducted through the femoral vessels in the aorta, a contrast agent is introduced. It falls into coronary artery and stains them, so doctors clearly can be clear, which permeability has every segment of the vascular path. If there is a significant narrowing on some plot, it is possible to carry out additional procedures that restore the initial diameter of the vessel.
Forecast
The total mortality rate with acute coronary syndrome is 20-40%, while most patients dies even before they are taken to the hospital (many - from such a deadly arrhythmia as ventricular fibrillation). The fact that a person has a high risk of death, one can say on such signs:
- man for more than 60 years;
- he has decreased blood pressure;
- heartbearance of heartbeat;
- acute heart failure has developed above 1 class by Kilip, that is, there are or only wet wars in the lungs, or the pressure has already increased pulmonary artery, or the emulsion edema developed, or a shock was developed with a falling of blood pressure, a decrease in the amount of separated urine, a violation of consciousness;
- a man suffers from diabetes;
- the heart attack developed on the front wall;
- the man has already transferred myocardial infarction.
Acute coronary syndrome with lifting segment ST (myocardial infarction).
Myocardial infarction is an acute disease caused by the emergence of foci of ischemic necrosis in the heart muscle due to the absolute insufficiency of coronary blood flow caused by the coronary artery thrombosis.
Reason: The gap of the "soft" atherosclerotic plaque launches the cascade of blood coagulation reactions, which leads to acute thrombotic occlusion of the coronary artery. If the restoration of blood perfusion by artery does not occur, the myocardial necrosis develops (starting from subendocardial departments). Depending on the duration of ischemia, the state of coronary vessels and concomitant circumstances (the so-called premorbid background) can occur both reversible damage to cardiomyocytes and their irreversible necrosis.
Classification.
In the acute stage, it is based on the processes of ischemic damage, it is recommended to use the term acute coronary syndrome with lifting ST (as an intermediate diagnosis). When forming infarction changes to the ECG (the appearance of the pathological teeth Q or QS), it is necessary to diagnose the acute myocardial infarction of one or another localization.
Myocardial infarction without pathological teeth Q (in our country is more often indicated as a small-fought myocardial infarction). It is also based on the coronary artery thrombosis, but unlike the large-scale, it is not fully fascinating the clearance of the vessel. Accordingly, this is not accompanied by changes in the QRS complex and the STE segment lifting the ECG. Currently, together with an unstable angina, it is included in the OXC rubric.
Clinic.
1. pain syndrome - intense prudent pain with a duration of more than 15 minutes, not passing after taking nitroglycerin, as a rule, accompanied by
Saddy. The overwhelming majority of patients simultaneously appear signs of activation of the autonomic nervous system (pallor, cold sweat), which is very typical for anginal pain.
2. The syndrome of acute left leave-deceased insufficiency - suffocation (feeling of the lack of air alone). Develops 100% with acute myocardial infarction, in parallel
with pain syndrome. With repeated and recurrent myocardial infarction, it is often leading in the clinic (with weak severity or even the absence of pain syndrome) is an asthmatic version of them.
3. Electrocardiographic syndrome. Even in the early stage of myocardial infarction, the ECG parameters are rarely left normally.
- small-scale myocardial infarction (myocardial infarction without teeth q) - is characterized by the appearance of a coronary teeth of T (negative, pointed
and isobid).
- the large-scale myocardial infarction - is characterized by the appearance of pathological-coast q not less than two leads:
- The transmural myocardial infarction is determined by the appearance of the pathological tooth QS (there is no R):
4. Resorption necrotic syndrome is due to the resorption of necrotic masses and the development of aseptic myocardial inflammation. The most important signs:
Increased body temperature with a duration of up to 10 days, at a body temperature not more than 38 degrees
Leukocytosis to 10-12 LLC from the first days
Acceleration ESP to 5-6 days
The appearance of biochemical signs of inflammation is an increase in the level of fibrinogen, serumcoid, haptoglobin, sialic acids, A2-globulin, Y-globulin, C-reactive protein.
The appearance of biochemical markers of the death of myocardium - aspartate-transferase, lactate dehydrogenase, creatinephosfocinate, glycogenphosphorlase, Mioglobin, myozin, cardiotroponins T, I.
5. Arrhythmic syndrome - with myocardial infarction in 100% of cases, violations of the heart rhythm are recorded (in the overwhelming majority of ventricular cases),
Which in the acute and sharp stage of myocardial infarction often define the prognosis of patients due to the high threat of development on their background of arrhythmic death as a result of ventricular fibrillation.
6. Cardiogenic shock syndrome proceeds in 3 options - pain (reflex shock as a result of intense stubborn pain), arrhythmic - significant
Earnings (more than 180 ice / min) or demolition (less than 40 UD / min) of cardiac abbreviations with the natural development of hemodynamic disorders as a result of falling heart Emission. The third option is the most unfavorable - true cardiogenic shock (it is based on the death of a significant part of myocardium left ventricle).
Clinical options:
1. An anginal is a classic version, the main clinical manifestation is a strong stubble pain, accompanied by a sense of air shortness and pronounced sweating.
2. The asthmatic version is dominated by the syndrome of acute left vehicles. It is often found, especially with the repeated and recurrent myocardial infarction, in patients of elderly and senile age, especially against the background of the previous HSN. Angic pains may not be very intense or not at all, and the attack of cardiac asthma or pulmonary swelling are the first and only clinical symptoms them.
3. Gastralgic - very often causes diagnostic errors. More often observed with a diaphragmal name. It is characterized by pain in the top of the abdomen, dyspeptic phenomena - nausea, vomiting, flatulence, and in some cases, paresis of the gastrointestinal tract. When the abdominal palpation can take place the tension of the abdominal wall. With abdominal shape, it resembles an acute disease of the digestive tract. The incorrect diagnosis is the cause of erroneous therapeutic tactics. There are cases when this sick is washing the stomach and even produce surgical intervention. Therefore, each patient with suspicion of "sharp belly" must be registered ECG.
4. The arrival - debuts by paroxy violations of cardiac rhythm, synicopal states. When arrhythmic form, they may not be absent or may be expressed slightly. If severe rhythm disorders arise against a typical anginal attack or simultaneously with it, they are not talking about atypical shape to them, but its complicated flow, although the conventionality of such division is obvious.
5. The cerebral version characterizes intensive headaches, loss of consciousness, nausea, vomiting, may be accompanied by transient focal symptoms, which makes it possible to largely diagnose diagnostics it is possible only with the timely and dynamic ECG record. This option is most often found in patients with initially driven extracranial and intracranial arteries, often with violations of cerebral circulation in the past.
6. "Asymptomatic" option - very often diagnosed by the presence of scar changes to the ECG.
Diagnostics
EchoCG. The main sign of them is the zone of the disturbed contraction of myocardium.
With this method of research, it is possible to determine the localization of them, which is especially important if there are no diagnostic signs of the disease on the ECG. Ehoche - the main method of diagnosing a number of complications to them: gap interventricular partition, breaking the free wall or formation of an aneurysm of LV, intra-
Sleep thrombosis.
Coronaryography. The detection of acute occlusion of the coronary artery together with clinical symptoms allows you to put an accurate diagnosis.
Treatment
When conducting fibrinolytic therapy in the first hours of the disease, it is possible to save additionally 50-60 lives per 1000 patients and many more to avoid the development of heart failure, other complications of myocardial infarction or reduce their severity. The essence of treatment is the enzymatic destruction of fibrin threads, which constitute the basis of occlusive coronary thrombus, with the restoration of adequate coronary blood circulation.
Indications for fibrinolytic therapy - clinic + Lifting segment ST or acutely arising blockade of the left leg of a beam of Gis. The exceptions are patients with true cardiogenic shock, at which time from the beginning of the disease is not taken into account.
Targets of the treatment of acute thrombolitics:
- Fast recanalization of occlusive coronary artery
- Suggesting of the progress
- limitation of the size of the acute and warning of its distribution
- Saving the LV function due to the maximum preservation of its muscle mass in the lesion zone.
Contraindications to the conduct of thrombolytic therapy:
1) stroke;
2) the absence of consciousness;
3) a large injury transferred over the last 3 weeks; operation;
4) gastrointestinal bleeding over the past month;
4) hemorrhagic diathesis;
5) aortic aortic aneurysm;
6) Arterial hypertension of more than 160 mm Hg. Art.
In our country, for treatment, it is currently the optimal use of the tissue activator of plasminogen - alteplosis (activation). After in / in the administration of the alteplosis, binding to the fibrin, activated and causes the conversion of plasminogen into plasmin, which leads to the dissolution of the fibrin of the thrombus. At the activation, as a result of clinical studies, a much pronounced effectiveness of reconalization of coronary arteries is proved - in comparison with other thrombolitics, in particular streptocinase. The continuation of the use of streptocinase is currently determined only by the relative "low-cost" drug in comparison with the actilization.
Indicators of successful thrombolysis:
1. Resolution of anginal pain;
2. ECG speaker: | ST is 70% of the initial value in the infarction of the rear-line localization and by 50% - in front of them;
3. T level of isfeimers (MF-KFK, TNL, TPT) after 60-90 minutes from the beginning of thrombolysis;
4. Reperfusion arrhythmias (ventricular extrasystole, accelerated idiotric rhythm)
2) direct anticoagulants.
Simultaneously with the introduction of the activation, the use of heparin should be launched for a period of 24 hours or more (with the use of streptocinase heparin contraindicated). Heparin is introduced into / in drip at a speed of 1000 units per hour. The heparin dose should be adjusted depending on the results of the re-determination of the activated partial thromboplasty time (AFTT) - the values \u200b\u200bof this indicator must exceed the initial level of 1.5-2.0 times, but not more (the threat of bleeding). An alternative to this method of treatment is the use of low molecular weight heparins - anoxaparine (cracks) of 1 mg per kg of body weight of the patient, subcutaneously 2 times a day. With the proven equal clinical efficacy - this type of anticoagulant therapy is determined by the ease of use and the absence of a thorough laboratory
Control.
3. The effectiveness of thrombolytic and anticoagulant therapy increases significantly if it is combined with the admission of aspirin in the medical dose of 325 mg.
4. Clopidogrel (smelting, Zilt, Plagryl) is shown to all sore ACS with the lifting of ST segment. The load dose is 300 mg inside, supporting dose - 75 mg per day. Application this drug Shown throughout the period of hospitalization.
5. Statins. Showing from the first day of treatment of acute them.
6. Nitrates (nitroglycerin, smells, perfect) - administered intravenously, improve the perfusion of myocardium, reduce the pre- and postload on the LV, determining
Reducing the need of myocardium in oxygen.
Clinical indications in which the appointment of nitrates is necessary:
- an anginal attack
- Signs of SN
- uncontrollable ag.
Contraindications for nitrates:
GARDEN< 90 мм рт. ст. или его снижение более чем на 30 мм рт. ст. от исходного
Heart rate<50 уд/мин
CSS\u003e 100 Ud / min
They are right ventricle
7. Beta-adrenoblays - reducing the need of myocardium in oxygen, improve perfusion in the ischemia zone, having an antiarrhythmic, antifibrillary effect, ensure a decrease in mortality not only to remote, but also in early time from the beginning of myocardial infarction. It is recommended to use high-selective
Preparations that do not have their own sympathomimetic effects. Preference is given to Metoprolol, Bisoprolol and Betaxolol.
8. Calcium antagonists in the early deadlines of myocardial infarction are not recommended.
9. ACE inhibitors.
Treatment of acute coronary syndrome without persistent lifting segment ST on ECG
Developed by the Committee of Experts of the All-Russian Scientific Society of Cardiologists
Moscow 2006.
All-Russian Scientific Society of Cardiologists
Moscow, 2006.
© All-Russian Scientific Society Cardiologists Playback In any form and reprint data of materials are possible only with the resolution of the INC

Deep-valued colleagues!
These recommendations are drawn up taking into account new data that appeared from the moment of publishing the first version in 2001. They can be considered a single standard for the treatment of patients with acute coronary syndrome without lifting ST segment based on the most advanced ideas about the pathogenesis, diagnosis and treatment of this group of diseases and, be sure to, taking into account the specific conditions of Russian health care.
The proposed methods of treatment based on a clear stratification of risk factors were confirmed by the results of internationally conducted international, multicenter studies and proved their effectiveness in thousands of treated patients.
The All-Russian Scientific Society of Cardiologists hopes that Russian recommendations for the treatment of acute coronary syndrome without lifting ST segment will lead to action for each cardiologist.
President of Inect, Academician R.G. Oganov
1. Introduction............................................... .................................................. .................... |
|
1.1. Some definitions..................................................................................................... |
|
1.1.1. The ratio of the concepts of NA and ISBP ST. NA with elevated levels p ................... |
|
2. Diagnosis ................................................. .................................................. ..................... |
|
2.1. Clinical symptoms ................................................ .............................................. |
|
2.2. Physical examination ................................................ .............................................. |
|
2.3. ECG................................................. .................................................. ............................. |
|
2.4. Biochemical markers of myocardial damage .............................................. .................. |
|
2.5. Risk assessment................................................ .................................................. ................. |
|
2.5.1. FR ..................................................... .................................................. ......................... |
|
2.5.1.1. Clinical data ............................................ .................................................. ...... |
|
2.5.1.2. ECG................................................. .................................................. ......................... |
|
2.5.1.3. Myocardial damage markers - page ............................................... ........................ |
|
2.5.1.4. Echokg ................................................. .................................................. ...................... |
|
2.5.1.5. Load tests before discharge .............................................. .......................... |
|
2.5.1.6. Kag ................................................. .................................................. ........................ |
|
3. Meetings of treatment .............................................. .................................................. ......... |
|
3.1. Anti-Hiscertic drugs ................................................ .......................................... |
|
3.1.1.Bab ............................................. .................................................. ........................... |
|
3.1.2. Nitrates ............................................... .................................................. .................. |
|
3.1.3. AK ................................................... .................................................. ........................ |
|
3.2. Antitrombotic drugs. Antithrombins ................................................. ............. |
|
3.2.1. Heparins (NFG and NMG) ........................................ .................................................. ... |
|
3.2.1.1. Long introduction of NMG in patients with signs of increased risk of complications11 |
|
3.2.2. Bright inhibitors of thrombin ........................................... ......................................... |
|
3.2.3. Treatment of hemorrhagic complications associated with antithrombins therapy ........... |
|
3.3. Antitrombotic drugs. Antitroscittarians ...................................... |
|
3.3.1. Aspirin (acetyl salicylic acid) ............................................ ......................... |
|
3.3.1.1. Dose Aspirin ................................................ .................................................. ........ |
|
3.3.1.2. Resistance to aspirin ............................................... ..................................... |
|
3.3.2. Receptor antagonists: Tienopyridines ............................................ ......... |
|
3.3.3. Blockers GP IIB / IIIa platelet receptors ........................................................... ........... |
|
3.3.3.1. Antagonists of GP IIB / IIIA platelets and NMG .......................................... ............ |
|
3.4. Indirect anticoagulants at ox ................................................ ............................... |
|
3.5. Fibrinolytic (thrombolytic) treatment ........................................................... ............... |
|
3.6. Coronary revascularization ................................................ ........................................ |
|
3.6.1. Kag ................................................. .................................................. ....................... |
|
3.6.2. CHV. Stents ................................................... .................................................. ....... |
|
3.6.2.1. ATT after PCB ............................................... .................................................. ........ |
|
3.6.2.2. ChKV and NMG ............................................... .................................................. ............. |
|
3.6.3. Ksh ............................................................. .................................................. ...................... |
|
3.6.4. Indications for ChCV and surgical interventions ............................................ ..... |
|
3.6.5. Comparison of the effectiveness of invasive and drug treatment techniques ........... |
|
4. Strategy for the treatment of patients with OX ........................................... .................................. |
|
4.1. Primary assessment of the patient ............................................... ............................................. |
|
4.2. Patients with signs of acute occlusion of large ka ....................................................... ............ |
|
4.3. Patients with suspected oxep st ............................................ ................................ |
|
4.3.1. The use of heparin ................................................ ................................................ |
|
4.3.1.1. NFG ................................................. .................................................. ....................... |
|
4.3.1.2. NMG ................................................. .................................................. ...................... |
|
4.3.2. Patients with high direct risk of death or development |
|
the results of the initial observation (8-12 hours) ........................................... ..................... |
|
4.3.3. Patients with low risk of death or development in the near future ..................... |
|
4.4. Maintaining patients after stabilizing the state ............................................. ................ |
|
5. For example, the sequence of actions when conducting patients with OXBP ST ................. |
|
5.1. First contact with the doctor (district, cardiologist polyclinics) .................................... |
|
5.2. A ambulance doctor ............................................... .................................................. ..... |
|
5.3. Reception of the hospital ............................................... .............................................. |
|
5.3.1. Hospitals without cardiology bits or having opportunities for emergency |
|
treating patients in the receiving rest ............................................... ......................................... |
|
5.3.2. Hospitals with cardiology bits .............................................. .............................. |
|
5.4. Bit (with its absence, the department in which treatment is carried out) ......................... |
|
5.4.1. Institutions with surgical service or the possibility of fulfillment of the CCV ................. |
|
5.5. Cardiology department After transferring from the bit .............................................. ......... |
|
Application................................................. .................................................. ............... |
|
Literature................................................. .................................................. ................ |
|
Composition of the Committee of Experts Ink on Preparation of Recommendations ...................................... |
|
List of abbreviations and symbols used in recommendations |
ACC / AAS - American Cardiology College / American
kaya Heart Association |
||
aorto-coronary shunting. |
||
antithrombotic therapy |
||
adenosine trifosphate |
||
activated partial thromboplastiny |
||
β -adrenoblays |
||
balloon angioplasty |
||
block of intensive therapy |
||
Blnpg - blockade of the left leg of the beam of His |
||
top boundary of the norm for the method used |
||
intravenously, - |
||
GLG - |
hypertrophy lzh. |
|
GMG-KOA - Hydroxy MethylGlutaryl Coenzyme A |
||
GP IIB / IIIA receptors - |
glycoprotein IIB / IIIA receptor |
|
torah platelets. |
||
GP IIB / IIIA platelets - Glycitoproten IIB / IIIA platelets
GTG - Hypertriglyceridemia Dad - diastolic hell
IAPF - inhibitors of angiotensin-converting farm
left ventricle |
||
MV (Muscle Brain) faction KFK |
||
international Normalized Attitude |
||
They are without teeth q |
||
low molecular weight heparin (s) |
||
unstable angina |
||
neficcated heparin |
||
n / k - |
subcutaneously, - |
|
acute |
||
acute coronary syndrome (s) |
||
OXBP ST - |
acute coronary syndrome without lifts |
|
sT SEGE ON ECG |
||
SKSP ST - OKS with the lifting of ST segment on the ECG |
||
common cholesterol |
||
systolic hell |
||
heart failure |
||
stable angina |
||
heart troponins |
||
thrombotic therapy |
||
triponins |
||
emission fraction |
||
functional class |
||
risk factors |
||
low density lipoprotein cholesterol |
||
high density lipoprotein cholesterol |
||
percutaneous coronary intervention (bap ka |
||
and / or installation wall, atherctomy, others |
||
methods to eliminate stenosis, devices for |
||
which are usually entered through |
||
peripheral vessel) |
||
heart rate |
||
electrocardiogram |
||
echocardiography |
||
SAO2 - |
saturation arterial blood Oxygen |
|
TXA2 - |
thromboxan A2. |
|
1. Introduction
For CBS as chronic diseaseCharacterized periods of stable flow and exacerbations. The exacerbation period of the CBS is denoted as OKS. This term combines such clinical states, as it, including not q-im, small-scale, micro, etc.) and ns. Ns and they are different clinical manifestations of a single pathophysiological process - thrombosis various degrees Industion over an atherosclerotic plaque or erosion of endothelium ka, and subsequent distal thromboembolism.
The term OX was introduced into clinical practiceWhen it turned out that the question of the use of some active treatment methods, in particular TLT, should be solved before the final diagnosis of the presence or absence of large-scale them.
With the first contact of the doctor with the patient with suspected ACS for clinical and ECG signs, it can be attributed to one of its two main forms.
SKSP ST. These are patients with the presence of pain or other unpleasant sensations (discomfort) in the chest and resistant lifts of the ST or "new" segment, which first arose, or presumably first emerged BLNPG on the ECG. Resistant lifts of ST segment reflect the presence of acute complete occlusion. The purpose of treatment in this situation is the rapid and persistent restoration of the lumen of the vessel. To do this, in the absence of contraindications, thrombolytic agents or direct angioplasty are used - CHV.
OKSBP ST. Patients with the presence of pain in the chest and changes to the ECG, indicating acute myocardial ischemia, but BP ST. These patients may determine persistent or transient depressed ST, inversion, smoothness or pseudonormalization of the teeth T; ECG during admission may be normal. The strategy of conducting such patients is to eliminate ischemia and symptoms, observing repeated (serial) registration of ECG and the definition of markers of myocardial necrosis: Page and MV KFK. In the treatment of such patients, thrombolytic agents are not effective and not used. Therapeutic tactics depends on the degree of risk (the severity of the state) of the patient.
1.1. Some definitions OX - any group of clinical recognition
cove or symptoms, allowing to suspect a sharp OIM or NA, includes OIM, IMT ST, ICPP ST, to them, diagnosed on changes in enzymes, on biomarkers, in late ECG signs, and NA. The term appeared in connection with the need to choose therapeutic tactics to the final diagnosis of the listed states. It is used to designate patients with the first contact with them and implies the need to treat as patients with them or ns.
The ISBP ST is a sharp process of ischemia myocardium sufficient gravity and duration to cause myocardial necrosis. In the initial ECG there are no lifts of ST. In the majority of patients who have a disease begins as ISBP ST, the q teeth do not appear and in the end is diagnosed with noq-im. IMBP ST differs from the NA presence (raising levels) of myocardial necrosis markers, which are missing at NA.
NA is a sharp process of myocardial ischemia, the severity and the duration of which is not enough to develop myocardial necrosis. Usually there are no lifts in ECG. There is no emission in the bloodstream biomarkers of myocardial necrosis in quantities sufficient to diagnose them.
1.1.1. The ratio of the concepts of NA and ISBP ST. NA with elevated levels page
The concept of ISBP ST appeared in connection with the wide implementation of the definition of the definition into the clinical practice. Patients with OXBP ST with a high level of page have the worst forecast (higher risk) and require more active treatment and observation. The term ISBP ST is used for the "marking" of the patient for a short time, until it becomes definitely, whether he has not developed a large-scale or the process limited himself to the emergence of non-them. The allocation of ISBP ST without determining the pion on the basis of less sensitive necrosis markers, in particular MV KFK, possibly, leads to the identification of only a part of patients with the foci of necrosis in myocardium and, therefore, high risk.
Thus, for quick distinction inside the OKSBP ST, the ISBP ST and NS requires defined levels.

The NA and the ISBP of the ST standings are very close, having a common pathogenesis and a similar clinical picture may differ only in severity (severity) of symptoms. In Russia, various, both quantitative and qualitative methods for defining pages are used in medical institutions. Accordingly, depending on the sensitivity of the method of determining the necrosis markers, the same state can be estimated differently: ns or ISBP ST. Until now, the attitude to the diagnosis is not formulated on the basis of an increase in the content of the content of any severity. On the other hand, positive analysis On Tr (Increased levels with a quantitative determination) significantly affects the choice of the method and treatment site and should be somehow reflected in the diagnosis. Therefore, it is permissible to use the formulation of "NS with an increased level page" (T or I) as an equivalent term ISBP ST. This formulation is provided for by the classification of HAMM CW and BraUnwald E - NA class IIIB, TP positive (Table 1).
2. Diagnosis
2.1. Clinical symptoms
Patients with suspected development of OKSBP ST, the treatment of which is considered in these Recommendations, when applying for
medical help can be attributed to the following clinical groups:
patients after a protracted\u003e 15 min. An attack of anginal pain alone. Such a state usually serves as a basis for challenging ambulance or emergency appeal to the medical institution in some other way. It corresponds to the III classification of the HAMM CW and Braunwald E classification (Table 1). Patients relating to this group make up the main object of these recommendations;
patients with first arising in the preceding28-30 days heavy angina;
patients who have occurred destabilization of the previously existing SS with the advent of the characteristics inherent in at least III PK angularity according to the classification of the Canadian Cardiology Association (Appendix), and / or Pain Pain Attachments (progressive angina, angina drive).
OX can manifest themselves atypically, especially in young (25-40 years) and the elderly (\u003e 75 years) patients, patients with dias and women. Atypical manifestations of NA include pain that arises predominantly alone, the pain in the epigastrics, acutely appeared disorders of the digestion, cigarette In the chest, pain with signs inherent in the defeat of the pleura, or increasing shortness of breath. In these
Table 1
Classification of HAMM CW, Braunwald E.
I is the first appearance of severe angina, progressive angina; Without angina rest
II - Roast angina in the preceding month, but not in the next 48 hours; (Stenokardia rest, undercaping)
III - rest angina in the preceding 48 hours; (Stenokardia rest, acute)
Note: * Circulation 2000; 102: 118.
cases of proper diagnosis contribute to the instructions on a more or less long existence of the CBS.
2.2. Physical examination
The objectives of the survey are: the exclusion of non-memory causes of pain, diseases of the heart of non-haemic origin (pericarditis, damage to valves), as well as emergency reasons that potentially contribute to the strengthening of ischemia (anemia); Detection of heart reasons for amplifying (or causing) myocardial ischemia (CH, AG).
ECG OKOY - the main method of evaluating patients with OX. ECG registration should be registered in the presence of symptoms and compare with the ECG, removed after their disappearance. It is desirable to compare the registered ECG with the "old", obtained to the present exacerbation, especially if there is a GLB or preceding them. Teeth Q, pointing to the scars after them, are highly specific to pronounced coronary atherosclerosis, but do not indicate instability at the moment.
ECG signs of unstable KBS - shifts of ST segment and progress T. T. The likelihood of the presence of NAs is particularly high when combining the corresponding clinical picture with the depression of the ST\u003e 1 mm segment depression in two or more adjacent leads, as well as inverted T\u003e 1 mm inversion inversion R; The last sign is less specific. Deep symmetric inversions of the Tusque T in the front breasts often indicate a pronounced proximal stenosis of the anterior downward branch of the LKA; Non-specific shifts of the ST segment and changing the teeth, according to amplitude ≤1 mm, less informative.
Fully normal ECG in patients with symptoms, forcing the suspect of OX, does not exclude its presence. However, if a normal ECG is registered during severe pain, it should be stubbornly to look for other possible reasons Complaints of the patient.
The lifting of the ST segment indicates a transmural myocardial ischemia due to occlusion. The resistant rise of the ST segment is characteristic of developing them. Progress
the lifting rise of the ST segment may be with the walls of the printela (vasospadic angina).
2.4. Biochemical myocardial damage markers
When STSBP ST Page T and I as a myocardial necrosis markers due to their greater specificity and reliability, preferably traditionally defined KFK and its MV fraction. The elevated level of page T or I reflects the necrosis of myocardial cells. If there are other signs of myocardial ischemia - the progressive pain, changes in the ST segment. This increase should be called them.
The definition of the page allows you to detect myocardial damage to about a third of the patients without increasing MV KFK. To confirm or eliminate myocardium damage, re-fences blood and measurements are required within 6-12 hours after admission and after any episode of severe peppercake pain.
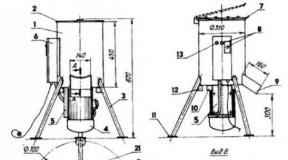
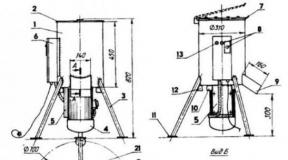
Changing the content of various markers of myocardial necrosis in time in relation to painful attack is shown in Figure 1. Mioglobin is a relatively early marker, while the increase in MV KFK and the page appears later. Page may remain elevated within 1-2 weeks, which makes it difficult to diagnose re-necrosis in patients with a recent (Table 6 in the annex).
2.5. Risk assessment
W. patients with a diagnosis of OKSBP ST In each particular case, the choice of the medical strategy depends on the risk of developing them or death.
The risk of death and occurrence is increasing with age. With an increased risk of coronary complications, male gears and such preceding manifestations of the CBS are connected, as a heavy and long-lasting angina or previously transferred to them. Signs of increased risk are violations of the function of LV, stagnant CH, as well as the AG and SD. Most well-known FR CBS are also signs of a bad forecast for ACS.

* Vertical axis - the content of the marker in the blood in relation to the level sufficient for the diagnosis of the OIM (diagnostic level for it) adopted per unit.
Fig. 1 biochemical markers of myocardial necrosis and changes in their blood content after painful attack.
2.5.1.1. Clinical data
Prognostically important are the time passed after the last episode of ischemia, the presence of a rest angina and an answer to drug treatment. These features, along with the concentration, are taken into account in the Hamm CW and Braunwald E. classification (Table 1).
ECG data are decisive to diagnose OX and forecast estimation. In patients with depression of the ST segment, the risk of subsequent complications are higher than in patients who have the only change in the inversion of the T. T. In turn, the latter have a greater risk of complications compared with patients with normal ECG.
Burely ("dumb") episodes of myocardial ischemia cannot be determined using the usual ECG. Therefore, it is advisable to Holter monitoring ECG, although its ability is limited to registering only
two-three assignments and resulting in no less than a few hours after recording *.
2.5.1.3. Myocardial damage markers - page
In patients with high levels, short-term and remote predictions are less favorable compared to patients without such an increase. The risk of new coronary events correlates with a degree of increase in TR. Risk Risk associated with high levels The page does not depend on other FRs, including the ECG changes alone or with long monitoring. The identification of patients with increased contents is important to select the treatment method.
2.5.1.4. Ehoche
EchoCG allows you to estimate the status of the systolic function of LV, which has an important prognostic value. During myocardium ischemia, local can be detected
* A promising methodology is the continuous monitoring of the ECG in 12 leads with a constant analysis of the results using a computer. Continuous monitoring of the ST segment is useful and to assess the effect of treatment for ischemia

hypocinezia or the axinesia of the walls of the LV, and after the disappearance of ischemia - the restoration of normal contractility. To assess the forecast and the choice of tactics of patients, it is important to diagnose such states as the stenosis of the aorta mouth or hypertrophic cardiomyopathy.
2.5.1.5. Load tests before discharge
Stress test, made after stabilizing the state of the patient and before discharge, is useful to confirm the diagnosis of the CBS and to assess the risk of complications. A significant part of the patients cannot perform load tests, and this in itself is associated with a bad forecast. Adding visualization methods to detect myocardial ischemia, such as ECCG, provides further increase in the sensitivity and specificity of the forecast. However, large, long, prognostic studies using stress-echoca in patients after the episode of OKSBP ST are missing.
This research method provides information on the presence of stenzing changes and their severity. Patients with multi-sowned lesions and patients with stenosis of the draft barrel have a higher risk of serious complications. KAG Evaluation of the degree and localization of the stenosis, which caused deterioration, and other stenosis is necessary if it is planned to be CCV. The greatest risk is associated with the presence of filling defects pointing to intra-block thrombus.
3. Methods of treatment
3.1. Anti-acemic drugs
These drugs reduce the consumption of oxygen by myocardium, reducing the heart rate, blood pressure, suppressing the reduction of LV or cause vasodilation.
cases that some particular women are more effective. Therapy can be started from metoprolol, propranolol or atenolol. In cases where, in the opinion of the doctor, a very rapid cessation of women is needed, it is advisable to use esmolol.
From the most shortly active drugs should begin treatment in the presence of concomitant diseases, such as pathology of lungs or dysfunction of LV. Parenteral introduction of women requires careful monitoring of blood pressure, desirable continuous monitoring of the ECG. The purpose of the subsequent reception of Bab Per OS should be the achievement of CSS 50-60 UD / min. You should not use women in patients with pronounced violations of AV conduction (AB blockade I with PQ\u003e 0.24 sec, II or III degrees) without a working artificial rhythm driver, bronchial asthma in history, severe acute LV dysfunction with signs of CH *.
Special caution should be observed in patients with chronic obstructive diseases of the lungs, starting treatment with a relatively short-acting, cardioslelective women, for example, metoprolol in reduced doses.
3.1.2. Nitrate
It should be borne in mind that the use of nitrates at NA is based on pathophysiological prerequisites and clinical experience. Data of controlled studies, which would prove optimal dosages and the duration of use, are absent.
In patients with persistent episodes of ischemia myocardium (and / or coronary pain), it is advisable to assign nitrates in / c. The dose should be gradually increased ("Title") before the disappearance of symptoms or appearance side Effects: Headache, hypotension. It should be remembered that long use Nitrates can cause addictory.
As the symptoms are achieved over the symptoms, the introduction of nitrates should be replaced with non-parastral forms, while observing some neglected interval.
* On the use of women after eliminating acute myocardial ischemia in patients with chronic CH, see the relevant recommendations of the INC.
10 Annex to the magazine "Cardiovascular therapy and prevention"
Acute coronary syndrome with a lifting segment St.SSPST) is characterized by typical pain in the chest, during which the ecg register persistent (more than 20 minutes) the rise of the segment St.(Or reaping the full blockade of the left leg of the Gis beam). Resistant segment St.the ECG reflects the occurrence of extensive transmural ischemia myocardium of the left ventricle, due to the total thrombotic occlusion of a large epicardially located coronary artery. As a rule, in the future in these zones of ischemia, extensive (often transmural) myocardial necrosis is developing, i.e. SSPST transforms in them with a segment lifting St.(IMPST). On ECG, this is manifested by the appearance of pathological teeth Q, or QS,those. Formed by him with a tooth Q. Previously, they wore a large-scale clogging (tooth Q.on ECG) or transmural (teeth QS.on ECG) The main goal of the treatment of patients with OSPST is the speedy, the most complete and persistent restoration of blood flow on the occlusion coronary artery. For this purpose, either thrombolytic drugs are used, or CCV (balloon angioplasty and stenting coronary arteries).
Myocardial infarction with the lift of the ST segment
Regardless of what they are talking about (IMPST, IMBPST, with a teeth Q,They are without teeth Q)under this term, from the point of view of pathomorphology, the disease is understood by the disease characterized by the occurrence of cardiomyocyte necrosis, which has developed due to ischemia myocardium, due to absolute or relative failure of coronary blood flow. It should be noted that necrosis of cardiomyocytes arising from inflammation (myocarditis), toxic effects on myocardium, sepsis, infiltrative diseases of myocardium, kidney or heart failure, injury, electric cardioversion, arrhythmia catheter ablation, etc., is not it.
In men, the impsta meets more often than women, especially in young age groups. In the group of patients aged 21 to 50 years, this relation is equal to 5 \\ 1, from 51 to 60 years - 2 \\ 1. In later age periods, this difference disappears due to the increase in the number of infarction in women.
Recently, the incidence of impst persons of young age has significantly increased (men under 40).
Classification
There are several classifications to them built on various principles. There is a classification, which is based on the mechanism of development to them, there is a clinical version of the beginning and the flow of them, there is a classification built on the extensions of myocardial lesions, there is a classification built on the pathological changes in myocardium, depending on the time interval, which has passed since the beginning of the disease, is Classification that takes into account the presence and lack of complications during them, etc.
In 2007, the international community adopted new criteria for diagnosing them, in which biochemical markers of myocardial necrosis are in the first place.
The diagnosis is based on the following clinical and laboratory-and-conventional diagnostic criteria:
The increase (followed by a decrease) of the blood plasma concentration of biochemical markers of myocardial necrosis (preference has cardiac troponins) to a level exceeding the value of the 99th percentage of the upper boundary of them normal values In healthy individuals in combination with one of the following signs Myocardial Ischemia:
Clinical signs of myocardial ischemia;
ECG signs of newly emerging myocardial ischemia (lifting or depression segment ST,the appearance of the blockade of the left feet of the Gis beam);
The occurrence of the pathological teeth Q on the ECG;
Identifying with the help of visualization methods of a newly arising loss of viable myocardium or newly emerged disorders of the local reduction in the myocardium of the ventricular heart.
In 2007, a new one was accepted clinical classification themmixing five types.
Type 1. Spontaneouscondected by it by ischemia due to erosion, cracks or gap of an atherosclerotic plaque of the coronary artery or the dissection of the coronary artery wall.
Type 2. Secondaryconditioned by ithemia as a result of either the increased need of myocardium in oxygen, or as a result of the reduction of its delivery due to spasms, coronary artery embolism, anemia, arrhythmias, hypertension or hypotension.
Type 3. Sudden, unexpected heart death,including cardiac arrest, often in combination or with clinical symptoms, characteristic of myocardial ischemia, or with changes in ECG in the form of an allegedly newly emerging segment lift St.or newly emerging blockade of the left leg of the Gis beam, or in the presence of signs of fresh blood cloth in the coronary artery according to angiography or autopsy, in cases where death came earlier than it was possible to take blood samples, or during the period of time preceding the level of biochemical markers Myocardial necrosis in blood plasma.
Type 4A. They associated with the implementation of the CCV.It is diagnosed in cases where after performing the Patients in patients with the initially normal level of heart troponins or MV-KFK in the blood plasma, more than threefold excess of the 99th percentage of the upper boundary of their normal values \u200b\u200bis observed.
Type 4b. They associated with the trombosis of the stentconfirmed by angiography or autopsy.
Type 5. They associated with the performance of coronary shunt operations.It is diagnosed in cases when after performing the coronary shunting operation in patients with the initially normal level of cardiac troponins or MV-KFK in the blood plasma, more than five times the excess of the 99th percentage of the upper boundary of their normal values \u200b\u200bin combination with one of the following Signs: newly appeared on ECG by pathological teeth Q.either the full blockade of the leg beam leg; with angiographically proven, newly emerged occlusion of a coronary shunt, or a native coronary artery; either with identified methods with signs of newly emerging loss of viable myocardium.
Depending on the nature of the ECG changes, they all can be divided into it with a tooth Q.and on them without teeth Q.Despite the fact that a clear relationship between myocardial necrosis sizes (prevalence, depth) and its ECG manifestations are not, usually with deep teeth. Q.and especially with teeth QS.necrosis is transmural, capturing on a certain area all the thickness of the myocardial of the left ventricle. With it without education on the ECG pathological teeth Q.or QS.myocardial necrosis usually has a smaller size. In connection with this with the teeth Q.and QS.the ECG was called before, respectively, "large-scale" and "transmural"; They are without teeth Q.they were called "small-scale" or "subendocardial".
Depending on the localization, they are divided into front, top, side, septal (partition), lower (diaphragmal) and basal. In case of extensive necrosis, combinations of these localizations are possible (front-barrect it, the Lower Software, etc.).
These localizations belong to the left ventricle, as most often suffering from it. The infarction of the right ventricle develops significantly less frequently, usually with occlusion of the right coronary artery, which usually its blood supply.
Depending on the pathological changes that occur in a damaged myocardium at various time periods that have passed since the onset of the disease, allocate certain stages that it takes place in their development:
It is the first 6 hours of development to them, when some part of viable myocardial persists, and therapeutic measures aimed at restoring blood flow in an occlusive coronary artery are most effective, since they give a chance to save part of this preserved myocardium;
Acute it is them in the time interval from 6 hours to 7 days from the beginning of the clinical picture of the disease;
Saluing (shaking) them - it is in a period of 7 to 28 days of the disease;
Healing them (post-infarction cardiosclerosis, old im) is them, starting with 29 days of the disease.
Depending on the clinical flow, the primary, repeated and recurrent it is isolated.
Primary im.- This is the first time developed by him.
Under repeated themunderstand the emergence of new foci of myocardial necrosis in terms, exceeding 29 days from the beginning of the previous heart attack. Repeat it can occur both in the infarction-bound coronary artery basin and in the basins of other coronary arteries.
Recurrent- This is an option of a disease in which new areas of necrosis occur in the first 4 weeks after the development of the previously prior to them, i.e. Before the end of the main scarring processes. In the diagnosis of recurring them, in addition to the clinical picture (an angin attack of more than 20 minutes) and ECG changes (re-lifting segment St.\u003e 1 mm either 0.1 mV, not less than 2 adjacent leads), is of great importance to the re-determination in the blood plasma level of cardiac troponins with an interval of 3-6 hours. For re-necrosis of myocardium, it is characterized by an increase in the level of cardiac troponins in the second analysis\u003e 20 % compared with the previous one.
Etiology
The main reason for them is the atherotrombosis in the coronary pool, i.e. Formation of thrombus at the site of gap, erosion or cracks, the so-called "unstable" atherosclerotic plaque. The "unstable" atherosclerotic plaque is far from always happen by hemodynamically significant, narrowing clearance of the coronary artery by 50% or more. Approximately 2/3 cases of blood clots in coronary arteries are formed on "unstable" atherosclerotic plaques, which narrow the clearance of the arteries only slightly or moderately. The "unstable" atherosclerotic plaque is characterized by a large lipid core and a thin fibrous coat with cellular elements of inflammation. Those or other signs of atherosclerosis of the coronary arteries are found in patients who died from them in 90-95% of cases.
Less often, the causes of them are spasms, embolism of coronary arteries, their thrombosis with inflammatory lesions (Trombalgitis, rheumatic coronet, etc.), anemia, hypertension or hypotension, compression of the mouth of the coronary arteries of aging aortic aneurysm, etc.
Pathogenesis
In the pathogenesis, the leading role is owned by ischemia, i.e. Termination of blood flow to the portion of the heart muscle. However, it should be noted that the death of the styled cardiomyocytes does not occur instantly, this is a process stretched over time. In many respects, the duration of this process depends on the presence and severity of collateral blood circulation, permanent or intermittent nature of thrombotic occlusion, sensitivity of cardiomyocytes to ischemia and their individual need for oxygen and energy substrates. Typically, cardiomyocytes are beginning to die no earlier than 20-30 minutes after the development of ischemia. After 60 minutes, approximately 20% of myocardial dies, after 3 hours, about 40-50% of myocardials, after 6 hours, about 60-80% of myocardium, after 12 hours, all myocardia dies, which was in the zone of the occlusive coronary artery. That is why the key factor affecting the effectiveness of the treatment of patients with OSPST is the time factor, and the introduction of thrombolytic drugs or the implementation of primary PCV is advisable only in the first 12 hours of the disease.
Myocardial necrosis is manifested by resorption-necrotic syndrome (laboratory test data, an increase in body temperature).
Disorders of electrophysiological and metabolic processes in myocardium caused severe heart rhythm disorders, often ending with ventricular fibrillation.
Myocardial necrosis leads to a violation of the contractile ability of the myocardial of the left ventricle and launches its remodeling processes. The formation of a focus of necrosis in myocardium is accompanied by a change in size, shape and thickness of the left ventricular wall, and the preserved myocardium is experiencing an increased load and exposed to hypertrophy. The pumping function of myocardial left ventricle undergoing remodeling processes deteriorates, which contributes to the development of chronic heart failure. The maximum pronounced version of the remodeling of the left ventricle is manifested in the form of the formations of its chronic aneurysm after the transferred extensive.
If the ischemia and necrosis are simultaneously exposed to a large amount of myocardial left ventricle (\u003e 50% of its mass), which happens with proximal occlusion of the front interventricular artery or occlusion of the left coronary artery and occlusion, an acute left-mellucker deficiency is developing - pulmonary edema and (or) cardiogenic shock. The reduction of coronary blood flow occurs during cardiogenic shock even more contributes to a decrease in the pump function of the heart, blood pressure and exacerbates the cardiogenic shock. Further progression of arterial hypotension leads to a sharp decrease in the blood supply to vital organs, which causes a disruption of microcirculation, tissue hypoxia, acidosis, polyorgan deficiency and ends with the death of the patient.
Clinical picture
Often, the IMTST develops suddenly, without any harbingers. However, approximately 15-20% of patients before developing the IMPST, there is a period of unstable angina (see above the appropriate section of the textbook).
The clinical picture of the IMTST is determined by the option of its start, the nature of the course and the development of certain complications.
A classic (typical) or an angin version of the beginning of the IMTST is observed in about 70-80% of cases. The clinical picture is characterized by typical intense anginal pain syndrome with the localization of sternum pain (less often in the heart area), often irradiating to the left hand, shoulder, shovel, lower jaw, etc. Pains in character are usually a pressing, compressive, burning character. Unlike angina, the pain is long, more than 20 minutes, does not stop nitroglycerin, is accompanied by cold later, fear of death.
In addition to the typical form of the beginning of the disease, a number of other, atypical options for the start of the IMTST are distinguished:
Astmatic - the beginning of the disease is manifested by breath, choking, attacks of pulmonary edema; there is no pain syndrome or expressed not sharply (this option is usually developing when they repeated by elderly patients against the background of the previously existing chronic heart failure);
Abdominal (gastralgic) - abdominal pain, more often in the opposite region, dyspeptic disorders, more often occurs at the lower (diaphragmal);
Arrhythmic - the disease is manifested by impaired rhythm or conductivity, more often in the form of an atrocarditricular blockade of IIIII degree or ventricular tachycardia, while painful syndrome is missing or weakly expressed;
Cerebral (cerebrovascular) - manifests itself by neurological disorders: dizziness, fainting, symptoms resembling a clinical picture of a stroke. More often occurs in elderly patients who have defeats intra- and extracranial arteries who have previously overlooking the violation of the cerebral circulation;
Asymptomatic (nonsense) - symptoms of general ailment, unmotivated weakness, adamis; Especially often occurs in the elderly, in patients with diabetes, which previously suffered a violation of cerebral circulation; Often the diagnosis is raised retrospectively, after random registration of the ECG.
Complications
During the period of developing pulp by more than 90% of patients, various ventricular rhythm disorders arise (usually ventricular extrasystolia), including heavy (ventricular tachycardia, ventricular fibrillation), which can lead to death (sudden heart death).
In the period of acute impste, complications may arise, most of which can also cause the death of patients:
Rhythm and conductivity disorders (HPTs, ventricular fibrillation, atrial and ventricular blocks, flickering and TP and other less formidable violations);
Outragia left-delicate deficiency - cardiac asthma, pulmonary swelling, shock (reflex, cardiogenic or arrhythmic);
Acute heart aneurysm;
Epistenocardic pericarditis;
Myocardial breaks both internal and external (including the perforation of the interventricular partition and the separation of the papillary muscles);
Thromboembolic complications (in a large and small circulation circle);
Parameas of the stomach and intestines, erosive gastritis with gastric bleeding, pancreatitis.
The period of the healing (scorching) impost proceeds more favorably, but also in its course complications are possible:
Thromboendocarditis with thromboembolic syndrome (more often - embolism of small blood circulation vessels);
Pneumonia;
Post-infarction syndrome - Dressler syndrome, front breast wall syndrome, shoulder syndrome - usually develops on the 2nd-6th week after it is characterized by pericarditis, pleurrites, pneumonite; Sometimes the synovial joints of the joints are involved in the inflammatory process (at the same time all the symptoms are rare, more often there is a combination of pericarditis with pleurite or pneumonite; sometimes each of these symptoms can occur in isolated, making it difficult to diagnose post-infarction syndrome);
Mental changes (more often negros-like symptoms);
Chronic left ventricular heart failure;
The beginning of the formation of chronic heart aneurysm;
Rightly failure is rarely developed; If it is presented, it is necessary to think about the thromboembolism of the branches of the pulmonary artery, the breaking of the interventricular partition and is extremely rare - about the infarction of the right ventricle.
In the period of healing pulp, the remodeling of the left ventricle continues, the formation of chronic aneurysm can go, the development of symptoms of chronic heart failure. New heart rhythm (MA) may also occur. In general, for this period, the development of severe complications is uncharacteristic.
On the first stage of diagnostic searchbased on the clinical picture, the nature of its development, taking into account the preceding anamnesis, age and sex of the patient, you can:
Suspect the development of them;
Suggest the assumptions about the clinical version of the disease;
Get information about certain complications.
In the presence of a long attack of unbearable pains behind the sternum and in the heart area with the characteristic irradiation, non-nitroglycerin, should, first of all, assume the development of them, especially in men older than 40 years. It should be remembered that such symptoms can sometimes be due to other reasons (neuritis, pleurite, myiosit, etc.).
The acute attack of the suffocation, especially in the elderly, primarily suggests an asthmatic version of them and requires mandatory ECG registration. However, an acute left-rude deficiency may be a manifestation of other disease (aortic or mitral heart disease, GB). Cardiac asthma and pulmonary edema with the appropriate clinical picture they may be complicated, but not an option to start.
The presence of sudden pain in the epigastric area, especially in patients with chronic IBS, makes it possible to suspect the abdominal (gastralgic) version of them and requires ECG registration. Such a clinical picture may be a manifestation of other diseases (exacerbation of ulcerative disease, gastritis, as well as cholecystitis, acute pancreatitis, food poisoning), especially in the presence of symptoms of gastric dyspepsia.
Complaints of the patient on the attacks of heartbeats or a sharp resinuation of the rhythm, the appearance of arrhythmia, fainting may indicate the beginning of them or its complications. In addition, the rhythm violations may appear and out of connection with them and be the manifestation of NCD, myocarditic cardiosclerosis, chronic IBS, etc.
The intense pain syndrome with atypical localization is less likely to remind them, but does not exclude it, and therefore the further examination of the patient is necessary.
Suddenly unmotivated development of cardiogenous shock, when the patient hesitated, badly, his consciousness is confused, it should also cause a suspicion of a suspicion for him.
All information obtained at the first stage of diagnostic search should be assessed taking into account the data of the physical and laboratory and instrumental examination. Sometimes at this stage of diagnostic search you can not get any information that allows you to diagnose them.
On the the second stage of diagnostic searchyou can get information:
Indirectly indicating the development of them (direct signs do not exist);
Allowing to identify complications.
With an appropriate history, symptoms such as an increase in body temperature, tachycardia, arterial hypotension, especially developed against the background of previous hypertension, the deafness of the heart tones and briefly listen to the fridge friction noise, allow them to speak in favor of the diagnosis. However, these symptoms themselves are nonpathogenic for them and may occur under a number of diseases (rheumatism, myocarditis, pericarditis, etc.).
Physical research helps to identify the symptoms of possible complications.
For cardiogenic shock is characteristic: cold skin of the gray-pale color, covered with sticky, then (violation of peripheral circulation); oliganuria (reducing urica); threaded pulse; reduction of pulse pressure (less than 20-30 mm Hg); Reducing systolic blood pressure (below 80 mm Hg).
Symptoms of acute left ventricular failure can be observed: shortness of breath, orthopneus, wet unvniable fine-grained wheezes in the lungs.
Increased liver, peripheral swelling - symptoms of blood circulation deficiency in a large circle.
In a physical examination, it seems possible to detect brandycardia, extrasystole, Ma, PT.
The diagnostic significance of all these complications is small, as they meet with other diseases. Only in combination with the history and data of the third stage of the diagnostic search, they are significant when diagnosing them.
The detection of acute aneurysm acquires a large diagnostic value (pathological pulsation in the precipitial area in the fourth intercostride to the left of the sternum), the breaking of the interventricular partition (intensive systolic noise in the lower third of the sternum with the symptoms of rapidly increasing blood circulation failure in the small and large circle), breaking or separating the nobby muscle (blowing systolic noise at the top of the heart, sometimes defined palpatorially, in combination with increasing stagnation in a small circle of blood circulation).
Third stage of diagnostic searchallows:
Put the final diagnosis to them;
Clarify its localization and prevalence (degree of myocardial damage);
Confirm or identify violations of rhythm and conductivity;
Identify new complications (the aneurysm of the heart, the focal kidney damage during thromboembolism).
Put the final diagnosisit is possible on the basis of a combination of signs of resorption-necrotic syndrome and ECG data.
Resorption-necrotic syndrome is detected by the results of generally increasing blood and biochemical blood studies: leukocytosis with a leukocytic formula shift to the left and aezinophyllium (not always) from the first hours of the disease; Increase in SE from the 3-5th day.
Currently, the most informative diagnostic method is the definition of the blood plasma of cardiac troponins T or I. If myocardine necrosis occurs, the level of cardiac troponins increases to diagnostically significant level Not earlier than after 6 hours, therefore, for diagnosis, it is recommended to 2 times the definition of cardiac troponins: when the patient is admitted to the hospital and again after 6-9 hours. A diagnostically significant increase in the level of cardiac troponins in blood plasma is considered to be the level exceeding the 99th percentile The values \u200b\u200bof this indicator in healthy persons determined by the laboratory method in which the ratio of the variation of definitions does not exceed 10%. The values \u200b\u200bof the 99th percenter of normal values \u200b\u200bfor various laboratory methods can be found on the website of the International Federation of Clinical Chemistry. The elevated level of heart troponins is preserved in the blood plasma to 7-14 days after it occurs.
If the use of cardiac troponins is not possible as markers of myocardium necrosis, it is permissible to use MB-KFK for this purpose, although its sensitivity is somewhat lower than the sensitivity of cardiac troponins. As in the case of heart troponins, the diagnostically significant level in the blood plasma MB-KFK reaches 6-9 hours after the occurrence of myocardial necrosis, but it retains the increased value of only about 2-3 days. Similar to cardiac troponins, the levels of Blood MB-KFK in plasma plasma are diagnorated, exceeding the 99th percentage of the values \u200b\u200bof this indicator in healthy faces.
Another biochemical marker of myocardial necrosis used to diagnose a heart attack is Mioglobin. Its advantage is a rapid increase in blood plasma concentration, which reaches a diagnostic value after 2 hours after an angin attack occurs. However, Mioglobin has a significant drawback - with high sensitivity it has low specificity.
Previously used in the diagnosis of the blood plasma of the level of aminotransferase (AST, Alt), lactate dehydrogenase (LDH) and its isoenzymes (LDH-1 and LDH-2) and its isoenzymes (LDH-1 and LDH-2) have been lost and practically not applied.
ECG is one of the main methods of Diagnostic IMTS, which allows you to diagnose them, clarify its localization, depth and extensity of the lesion, the flow phase; confirm or identify violations of rhythm and conductivity; To express the assumption of the development of the aneurysm of the heart.
In patients with OSPST and in patients with impsta during the period developing and in the initial period of acute them (the first 6-12 hours of the disease) marked the rise of the segment St.in the so-called "direct" leads (in these leads, the pathological tooth q) and the reciprocal decline will be formed St.in leads, with changes in the complex QRS.and the formation of pathological teeth Q.it will not be yet. Diagnostically meaningful consider the rise of the segment St.at point j in 2 consecutive leads and more\u003e 0.2 mm (0.2 mV) for men and\u003e \u003d 0.15 mm (0.15 mV) for women in leads V 2 -V 3 and\u003e 0.1 mm (0.1 mV) in other leads.
In the period acute in the "direct" leads, the ECG sharply decreases the amplitude of the teeth R.and a pathological tooth is formed, an amplitude is equal to at least 1/3 of the teeth R,and in duration - equal to 0.04 C and more (previously called "large-scale" them). Either tooth R.fully disappears and the pathological complex is formed QS.(previously called transmural; Fig. 2-18).
The subsequent evolution of the ECG at the IPST is reduced to the return of the segment St.to the isoelectric line and the formation in the "direct" leads of the negative ("coronary") teeth
For the front wall of the left ventricle, including the region of the top, the interventricular partition and the side wall, are characterized by the ECG changes in leads I, II, AVL and V 2 v 6; For a heart attack in the top of the left ventricle - in leads V 3 -V 4; With lesions of the area of \u200b\u200bthe interventricular partition, changes are detected in leads V 1 -V 3; With a side wall infarction - in leads I, AVL and V 5, V 6; For infarction of the lower wall, changes are characterized - in leads II, III and AVF.
Fig. 2-18.The acute period of myocardial infarction (3-day) in a patient with the IMTST (the same patient, as in Fig. 2-15): ECG signs of the formation of myocardial infarction with teeth Q.front, top, septal and lateral regions of the left ventricle: the appearance of pathological teeth Q.and QS.in leads I, AVL, V 2-6; segment St.decreased compared with fig. 2-18, but not yet dropped to the isolated. The beginning of the formation of negative "coronary" teeth T.leads i, avl, v 2-6
ECG in 12 standard leads is not informative in the case of the preceding blockade of the left leg of the beam of Gis and with the infarction of the right ventricle.
The ECG may identify a wide variety of rhythm disturbances. According to the ECG, it is possible to find out for the first time on impairment of atrial and ventricular conductivity and conduction on the legs of the beam of Gis, to determine the nature of the blockade.
A sign that suggests aneurysm, is the so-called "frozen" ECG - preservation of the lifting of the segment St.in combination with the complex QS.in the "direct" leads, while the "coronary" teeth of T.
Ultrasound examination of the heart is an important additional research method in patients with infarction. Uzi allows you to identify areas of violation of the local reduction in the myocardial of the left ventricle (hypokinesia, axinesia) corresponding to the area of \u200b\u200bdamage, as well as the state of the nobble muscles and the interventricular partition, which can also be affected by it. The importance of the ultrasound of the heart in the assessment of the global reduction of the left ventricle (the magnitude of the left ventricle emission fraction), in the assessment of its shape, sizes, in recognizing such complications, as the formation of blood clots in the cavities of the heart, myocardial breaks, the occurrence of pericarditis occurs.
The radoscopy of the chest organs is recommended to be carried out in all patients with suspicion of them or with an already established diagnosis of heart attack. For this, moving x-ray installations are usually used. Radiography of the chest organs allows you to clarify the state of the lungs, hearts. It is especially great to its importance in the diagnosis of initial signs of stagnation in a small circle of blood circulation, which are not yet clinically.
In the overwhelming majority of cases, this third stage of the diagnostic search ends and a deployed clinical diagnosis is formulated. Sometimes they resort to special diagnostic methods.
Visualization with the help of radioactive isotopes. This method is used if diagnosis is difficult to them with the help of ECG, and the study of the activity of serum enzymes is impossible or uninformative.
The pyrophosphate labeled with technetiz (99mtc-mibi), begins to accumulate in the necrosis area 12 hours from the beginning of the disease, and the focus of "glow" is determined up to 2 weeks, and with extensive lesions - 2-3 months.
Radioactive waves are less commonly (T1201), which accumulates in well-blooded myocardial sites and does not enter the necrosis area.
Selective coronary survey in the acute period, they apply if it is planned to perform primary angioplasty and stenting coronary arteries.
Diagnostic Criteria of Myocardial Infarction
Increase and (or) subsequent reduction in the level of biochemical markers of myocardial necrode in the blood (preferably cardiac troponins), if their concentration is at least in one blood sample exceeds the upper limit of the norm adopted in this laboratory, and there is at least one of the following myocardial ischemia certificates:
Clinical picture of myocardial ischemia;
ECG changes indicating the appearance of myocardial ischemia (the occurrence of segment displacements ST-T,blocks of the left leg feet of Gis);
The appearance of pathological teeth Q.on ECG;
The appearance of signs of loss of viable myocardium or violations of a local contractility using techniques that allow visualize the heart.
The wording of the deployed clinical diagnosis to themmust reflect:
The nature of the flow (primary, recurrent, repeated);
Necrosis depth (with a teeth Q,or without teeth Q);
Localization of them;
Date of appearance;
Complications (if they were): Rhythm and conductivity disorders, acute heart failure, etc.;
Background diseases - atherosclerosis of the coronary arteries (if coronoagoangiography was performed, it is the severity, prevalence and localization), GB (if available) and its stage, diabetes mellitus, etc.
Treatment
The provision of assistance to patients with impsta is made up of a system of organizational and medical measures.
Organizational activities include:
Early diagnosis of emergency medical care doctors, regional doctors, therapists and general practitioners of the regional Polyclinic of OSPST on the basis of the criteria shown earlier (see OKSPST);
As an early hospitalization of the victim of the patient with the SSPST in the block of intensive cardiology of the emergency cardiology;
As early as possible, the initiations aimed at restoring the coronary blood flow: the implementation of primary PCIs for 90 minutes from the moment of entering the patient to the hospital, which has such possibilities, or the introduction of thrombolytic drugs on chipboard either no later than 30 minutes from the moment the patient's entry into the hospital, which does not have the possibilities of performing primary PCV;
Staying patient during the acute pulp period in the intensive cardiology unit;
Regenerative treatment system (rehabilitation).
Therapeutic measures are carried out taking into account the stage of the IMTS, the severity and nature of complications.
In the initial period of the IMTST, the main medical measures are aimed at pain relief, the speedy full and persistent restoration of coronary blood flow in the heart attack-bound artery and the treatment of complications, if they occur.
Cutting pain syndrome.Anesthesia is one of the most important tasks of the initial period of treatment of patients with impst. With the ineffectiveness of 1-2 multiple reception of 0.4 mg of nitroglycerin in the form of tablets or spray, use intravenous administration of narcotic analgesics, among which 1% morphine solution (morphine hydrochloride) is most effective. Typically, 1.0 ml of the drug divorced in 20.0 ml of isotonic sodium chloride solution is introduced intravenously (slowly!). Instead of morphine, other narcotic analgesics can be used: 1.0 ml of 1% trimeperidine solution (Promedol *), 1-2 ml of 0.005% fentanyl solution, as in combination with tranquilizers or neuroleptics (2 ml of 0.25% Droperidol solution), So without them.
Oxigenotherapythrough the facial mask or nasal catheters are shown in patients having shortness of breath or clinical signs of acute heart failure (pulmonary edema, cardiogenic shock).
Restoration of coronary blood flow and myocardial perfusion.The speedy reduction of blood flow in the occlusion coronary artery (reperfusion) serves as the cornerstone in the treatment of patients with impst, the solution of which affects both hospital mortality and the nearest and remote forecast. It is desirable that, in addition to as fast as possible, the restoration of coronary blood flow was full and resistant. The key point that affects both the effectiveness of any reperfusion intervention and its remote results is the time factor: the loss of every 30 minutes increases the risk of death in the hospital by about 1%.
There are two possibilities for recovering coronary blood flow: thrombolytic therapy,those. Reperfusion with thrombolytic preparations (streptocinase, plasminogen fabric activators), and Chkv,those. Reperfusion with the use of mechanical destruction of thrombotic masses, occlusive coronary artery (balloon angioplasty and stenting coronary arteries).
An attempt to restore coronary blood flow using one or another method should be undertaken in all patients with impst in the first 12 hours of diseases (in the absence of contraindications). Reperfusion interventions are justified and after 12 hours from the beginning of the disease, if there are clinical and ECG signs of continuing myocardial ischemia. In stable patients, in the absence of clinical and ECG signs of continuing ischemia, myocardials, carrying out thrombolytic therapy, nor PCV later than 12 hours from the beginning of the disease is not shown.
Currently, the method of choosing the restoration of coronary blood flow in patients with impsta in the first 12 hours of the disease is the primary PCV (Fig. 2-19).

Fig. 2-19.Choosing a reperfusion strategy for the treatment of patients with myocardial infarction with a segment lifting St.in the first 12 hours of disease
Under primary chkvunderstand the balloon angioplasty with stenting (either without it) of the infarctional coronary artery, made in the first 12 hours from the beginning of the clinical picture of the IPST without the prior to the use of thrombolytic or other drugs capable of dissolving blood clots.
Ideally, in the first 12 hours of diseases, the patient with the IMST should be delivered to the hospital, which has the possibilities of performing primary PCV 24 hours a day for 7 days per week, provided that the intended time loss between the first patient's contact with the doctor and the moment of inflating the balloon catheter in the coronary The arteries (that is, the moment of recovery of coronary blood flow) will not exceed 2 hours. in patients with extensive pulp, diagnosed in the first 2 hours from the beginning of the disease, time loss should not exceed 90 min.
However, in real life, not all patients with IMTST are possible to perform primary PCW, since, on the one hand, for various reasons, significantly less than 50% of patients are hospitalized in the first 12 hours, and in the first 6 hours most favorable for treatment, less 20% of patients with impst. On the other hand, not all major hospitals have the ability to perform emergency PCV 24 hours a day 7 days a week.
In this regard, all over the world, including Russian Federation, the main way to restore coronary blood flow in patients with impsta is still remaining thrombolytic therapy.The advantages of thrombolytic therapy include simplicity of its conduct, relatively low cost, the possibility of its holding both in the prehospital stage (substantial, not less than 30 minutes (!) Reduction of time before the start of reperfusion therapy) and in any hospital. Its disadvantages should include insufficient effectiveness (50-80% depending on the type of thrombolytic drug and the time spent on the beginning of the disease), the development of early (5-10% of patients) and later (30% of patients) repeated occlusion of coronary arteries, the possibility of heavy Hemorrhagic complications, including hemorrhagic stroke (in 0.4-0.7% of patients).
In the absence of contraindications, the conducting of thrombolytic therapy should be carried out in the first 12 hours from the beginning of the clinical picture of the IPST in patients who cannot be performed in the above intervals of time for any reason.
It is fundamentally important that the system of systemic thrombizis is appropriate only in the first 12 hours from the beginning of the clinical picture of the IMT.
In a later date, the system thrombolysis is not shown, since its effectiveness is extremely low, and it does not have a significant impact on the indicators of hospital and remote mortality.
Currently, the most widely used thrombolytic drugs are streptocinase (the world's most commonly used in the world) and plasminogen fabric activators, which include Alteplias (T-PA), RETEPLAZ (RT-PA) and TENECTELES (NT-PA), and PUROLOZA ).
The advantage of plasminogen fabric activators, since they are fibrinsecific thrombolytic drugs.
In the presence of trained personnel, it is recommended to begin thrombolytic therapy at the prehtipal stage in the ambulance brigade, which allows you to significantly (at least 30-60 minutes) reduce the time loss associated with the conduct of reperfusion interventions.
Indications for conducting systemic thrombolysis:
The presence of a typical clinical picture of acute coronary syndrome in combination with ECG changes in the form of a segment lifting St.\u003e 1.0 mm in 2 adjacent standard leads from the limbs or lifting segment ST\u003e 2.0 mm in two adjacent breasts and more;
For the first time, the full blockade of the left leg of the Gis beam in combination with a typical clinical picture.
TO absolute contraindications
Hemorrhagic stroke or a stroke of an unknown nature of any limitation in history;
Ischemic stroke for the last 6 months;
The presence of vascular brain pathology (arteriovenous malformation);
The presence of a malignant tumor of the brain or metastases;
Recent injury, including the cranial-brain, extensive operation, during the last 3 weeks;
Gastrointestinal bleeding over the last 1 month;
Famous diseases accompanied by bleeding;
Suspicion of the bundle of the aorta wall;
Puncture of unconditional compression of bodies (liver puncture, lumbal puncture), including vessels (subclavian vein).
TO relative contraindicationsthe system of systemic thrombolysis includes:
Transit ischemic Attack over the last 6 months;
Therapy indirect anticoagulants;
Pregnancy and 1st week after childbirth;
Resuscitation activities accompanied by a chest injury;
Uncontrollable ag (systolic blood pressure\u003e 180 mm Hg);
Ulcerative ulcer of the stomach and duodenal intestine in the aggravation phase;
Far liver diseases;
Streptokinase is administered intravenously in a dose of 1.5 units dissolved in 100 ml of 0.9% sodium solution chloride or 5% glucose * for 30-60 minutes. Previously, to reduce the likelihood of allergic reactions, it is advisable to introduce intravenously 60-90 mg of prednisolone.
Althelza is administered intravenously in the total dose of 100 mg as follows: Initially, 15 mg of the preparation is injected intravenously in the form of a bolus, then an intravenous drip administration of alteplosis is started at the rate of 0.75 mg / kg of body weight, in the next 60 min, intravenous drip continues The introduction of the drug at the rate of 0.5 mg / kg body weight.
Tenctenselaza is administered intravenously in the form of one-time bolus injection in a dose, calculated depending on the weight of the patient: with a weight of 60-70 kg - 35 mg of the drug is injected, with a weight of 70-80 mg - 40 mg of teneptlazes is introduced, with weight 80-90 kg - introduced 45 mg of the drug, with weight more than 90 kg - 50 mg.
PRUUROKINASA (PURLAZ), the domestic drug is introduced intravenously (pre-preparation is dissolved in 100-200 ml of distilled * water or isotonic sodium chloride solution) according to the "Bolus + infusion" scheme. Bolus is 2,000,000 me; Subsequent infusion of 4 000 000 IU for 30-60 minutes.
Compared with streptokinase (three-generation thrombolytic), alteplia and retiene (three-generation thrombolytics), which require intravenous drip administration for a certain time, the ease of use of tetakteplosis (three-generation thrombolytic) is the possibility of its bolus intravenous administration . It is extremely convenient when conducting a dog-bind thrombolysis in a brigade of ambulance.
Indirectly the effectiveness of thrombolytic therapy is assessed by the degree of decline in the interval S-T.(Compared with the severity of the initial lift) 90 min after the start of the injection of the thrombolytic preparation. If interval S-T.it has decreased by 50% or more compared to the initial level, it is believed that thrombolysis turned out to be effective. Another indirect confirmation of the effectiveness of thrombolytic therapy is the emergence of the so-called reperfusion arrhythmias (frequent ventricular extrasystolia, jogging of slow ventricular tachycardia, ventricular fibrillation extremely rarely occurs). However, it should be noted that the thrombolytic therapy is not always formally effective in indirect signs leads to the restoration of coronary blood flow (according to coronaryogiography). The reperfusion efficacy of streptocinase is about 50%, alteplosis, relazes * 9 and tenextelase - 75-85%.
With the ineffectiveness of thrombolytic therapy, the question of the transfer of a patient with the IMTST to a hospital, which has the ability to conduct a PCB (in order for it for 12 hours from the beginning of the disease, it was fulfilled by the so-called "saving" CCV).
In the case of effective systemic thrombizisis patients over the next 24 hours, but not earlier than 3 hours from the beginning of the injection of the thrombolytic drug, it is advisable to carry out coronaryogiography and testimony - the implementation of the CCV.
In order to strengthen the thrombolytic effect and prevention of re-thrombosis of the coronary artery (with effective thrombolesis), antithrombocyte drugs (acetylsalicylic acid and clopidogrel) and antithrombinic drugs are used (NFG,NMG, ha-factor inhibitors).
Given the extremely important role of platelets in the pathogenesis of OSPST, the suppression of adhesion, activation and platelet aggregation serves as one of the key points in the treatment of this category of patients. Acetylsalicylic acid, blocking cyclooxygenase-1 platelets, disrupts the synthesis of thrombooxane A2 in them and, thus, irreversibly suppresses a platelet aggregation induced by collagen, ADP and thrombin.
Acetylsalicylic acid (aspirin)as an antiarrhegnant, the patient is prescribed as early as possible (still at the prehospital stage). The first loading dose of 250 mg of the patient is asked to delay; Then, at a dose of 100 mg, the patient takes aspirin * inside (preferably in intestinal form) once a day for a long time. The appointment of aspirin * simultaneously with the conduct of thrombolytic therapy is accompanied by a decrease in 35-day mortality by 23%.
Tienopyridines (clopidogrel).Even more effective is the addition of a combination of aspirin * and clopidogrel to thrombolytic therapy (both using a loading dose of clopidogrel 300-600 mg, and without it). Such two-component antitrombocyte therapy leads to a reliable decline on the 30th day of the disease of the frequency of serious cardiovascular complications by 20%.
Antithrombin preparations (anticoagulants).The feasibility of using anticoagulants (NFG, NMG, ha-factor inhibitors) is related to the need to maintain the patency and prevention of the repeated thrombosis of the infarction-bound coronary artery after successful systemic thrombolysis; Prevention of the formation of cloth thromboms in the left ventricle and subsequent systemic arterial embolism, as well as the prevention of possible vein thrombosis of the lower extremities and thromboembolism of the lung artery branches.
The choice of anticoagulant depends on whether systemic thrombolysis was conducted or not, and if it was carried out, then what drug was used.
If the systemic thrombolysis was carried out using streptocinase, the selection drug among anticoagulants serves a sodium Fondaparinux (Arikstra *) inhibitor, the first dose of 2.5 mg is introduced intravenously in the form of a bolus, in the future it is subcutaneously subcutaneously once a day in a dose 2, 5 mg for 7-8 days. In addition to Fondaparinux, NMG ENOKSAPARIN Sodium can be used, which is initially administered in the form of an intravenous bolus at a dose of 30 mg, following it, with an interval of 15 minutes, the first subcutaneous injection At the rate of 1 mg / kg body weight. In the future, the sodium ENOCAPARIN is introduced subcutaneously 2 times a day at a dose of 1 mg / kg body weight over the maximum of 8 days.
NFH can be applied as anticoagulant therapy, which is less convenient than ENOCAPARIN and Sodium Fondaparinux. The route of administration of the NFH is fundamentally important: it should be prescribed exclusively (!) In the form of a constant intravenous infusion through the dosing devices under the control of AFTV. The purpose of such therapy is to achieve the value of the AUTV 1.5-2 times greater in relation to the initial value. For this, initially NFG is administered intravenously in the form of a bolus 60 units / kg (no more than 4000 units), followed by intravenous infusion at a dose of 12 units per hour, but not exceeding 1000 UR / h under regular (after 3, 6, 12 And 24 hours after the start of the infusion) by the control of the AMTV and the corresponding dose correction of the NFG.
If systemic thrombolesis was performed using a plasminogen tissue activator, either an eoxaparine or an enexacional heparin can be used as anticoagulant therapy.
Nitrates.Organic nitrates - drugs that reduce myocardial ischemia. However, there is no convincing data in favor of the use of nitrates with uncomplicated flow of impost, so their routine use in such cases is not shown. Intravenous administration of nitrates can be used during the first 1-2 day of the IMTST in clinical signs of continuous myocardial ischemia, with high hypertension, with heart failure. The initial dose of the drug is 5-10 μg / min, if necessary, it increases by 10-15 μg / min, until the required effect is reached or systolic blood pressure will not reach the level of 100 mm Hg.
Application beta-adrenoblocatorsat an early stage of treatment of patients with impst (by reducing the needs of myocardium in oxygen), it helps to reduce myocardial ischemia, restricting the necrosis zone and the likelihood of life-degrading rhythm disorders, including ventricular fibrillation. In the "stable" patients who do not have impaired hemodynamics (arterial hypotension, acute left ventricular failure), violations of the conductivity of the heart, bronchial asthma, In the first hours of the IPST, the intravenous introduction of beta-adrenoblastors is possible, followed by a transition to a supporting intake. However, in most patients, after stabilizing their condition, preferably the prescription of beta-adrenoblockers (metoprolol, bisoprolol, carvedilol, propranolol) inside. At the same time, the beta-adrenobloclars first are prescribed in a small dose, followed by its increase under the control of blood pressure, heart rate and the state of hemodynamics.
APF inhibitorsit should be appointed from the first day of the IMTST if there are no contraindications. Captive, enalapril, ramipril, perindopril, zofensoid, transdolapril, etc. can be used, taking into account the instability of hemodynamics in the first day of the IMTST, the possibility of simultaneous use of beta-adrenobloclars and nitrates, the initial doses of ACE inhibitors should be small, followed by their increase under the control of blood pressure, the level of potassium and creatinine blood plasma to the maximum transferred doses or before reaching their target values. If the patient does not tolerate ACE inhibitors, angiotensin II receptor blockers (Valsartan, Losartan, Telmisartan, etc.) can be used. The inhibitors of ACE in patients with IMTST, in which in the early phase of the disease, there was a decrease in the ejection fraction or were signs of heart failure.
The final decision on the treatment of acute coronary syndrome of a particular patient should be taken by the attending physician. The adoption of this decision should be based on the knowledge of all topical materials on this topic; This knowledge and should help the doctor's practitioner choose the best possible approaches to the treatment of each patient.
The initial and leading symptom that gives the basis for the diagnosis and decision-making on therapeutic tactics is the pain in the chest.
It should be noted that the diagnosis of various forms of coronary heart disease (IBS) is based on a large number of subjective data, and when evaluating the pain in the chest, it is necessary to remember the nature of pain, their typical, provoking factors and other points.
Further classification of patients is based on the results of electrocardiography (ECG).
- 1. Patients with acute coronary syndrome (OX) with lifting s-T segment (SSPST) are patients with typical acute pain in the chest in combination with persistent (more than 20 minutes) the S-T segment climb.
- 2. Patients with acute patient in the chest, but without a resistant increase in the S-T segment (OXBPST). These patients meet various ECG changes: a resistant or transient depression of the S-T segment, inversion or a flat tooth ton, pseudonormalization of the Tusque T, as well as the absence of changes to the ECG at the time of the study.
Depending on the repeated measurements of troponins, all patients with OXBPST are qualified as patients with Myocardial infarction without lifting S- T (imbps) or with unstable angina.
There are several clinical options for OXBPST flow:
- long (more than 20 minutes) Angic pain in peace,
- for the first time, the attack of angina region (angina region de novo),
- progressive angina
- early post-infarction angina.
The first clinical option is found almost 80% of patients. However, one clinical picture does not allow reliably to distinguish the OX with the lift S-T and without it. In physical examination, we usually do not find deviations from the norm or any specific clinical signs, With the exception of the symptoms of transient mitral regurgitation, talking about the involvement in the ischemic zone of one of the papillary muscles.
The displacement of the S-T segment and the changes of the TC are ECG indicators of instability of the IBS. The depression of the S-T segment is more than 1 mm in two or more adjacent leads indicates the severity of ischemia, and when the segment is depressed by 2 and more mm, the risk of mortality increases 6 times. Inversion of Tissue T in breastless leads usually talks about significant stenosis proximal department front interventricular branch or led coronary artery trunk.
The biochemical markers of myocardial necrosis (troponins) increase with myocardial infarction (im) after 3-4 hours. Their level can remain elevated to two weeks after it. In case of imbps, a minor increase in troponin can only be observed within 48-72 hours.
The treatment of myocardial infarction without lifting ST segment (imbps)
The treatment of imbps includes five directions:
- Anti -cehetic means
- Anticoagulants
- DeaGreganta
- Coronary revascularization
- Long-term therapy
Preparations of the first group provide their own anti-hype Either by reducing the needs of myocardium in oxygen (by reducing the heart rate, blood pressure, preload or reduction of myocardial reductions), or by increasing the coronary blood flow (through the stimulation of coronary vasodilating). These drugs include The following groups of drugs:
- nitrate
- beta blockers
- calcium antagonists
Nitrate Showing to all patients with OXBPST, their intravenous administration is recommended for patients with recurrent angina and / or with signs of left ventricular failure.
Beta blockers, in the absence of contraindications, are also prescribed to all patients, especially with tachycardia and arterial hypertension.
Calcium antagonists Assigned to patients already accepting nitrates and beta-blockers, to reduce the symptoms of angina. It is advisable for their purpose as well as vasospadic angina and in the presence of contraindications to beta blockers. It is not recommended to use nifidipin and other dihydropyridines without a combination with beta blockers.
Anticoagulant therapy
- - indirect coagulation inhibitors (unfractionated heparin - NFG, low molecular weight heparin - NMG, Fondaparinux),
- - Direct coagulation inhibitors (Apiksaban, Rivroxabahn),
- - Direct thrombin inhibitors (Bivalirudin, Dabigatran).
Fondaparinux (at a dose of 2.5 mg subcutaneously) is recommended as a drug with the most favorable profile of security efficiency; During the percutaneous coronary intervention (NFG), NFG (85 IU / kg) should be added. In the absence of FondaParinux, Econxaparine is recommended (1 mg / kg twice a day). If Fondaparinux and Enoxaparina are not available, the NFH is shown or other NMGs in specific recommended doses. Bivalirudine is shown to patients only with planned invasive intervention. Anticoagulant therapy can be discontinued 24 hours after the invasive procedure. In the conservative tactics of treatment, anticoagulants are prescribed to extract from the hospital.
Disaggregative therapy
Disaggregative therapy It should be started as early as possible after the diagnosis of OKSBPST diagnosis in order to reduce the risk of both acute ischemic complications and recurrent atherotromability. Platelets can be inhibited by three grades of drugs: cyclooxygenase-1 inhibitors (aspirin), P2YI2 receptor inhibitors (clopidogrel, prasugrell, ticagrelor) and glycoprotein inhibitors IIB / IIIA (Eptifibad, Tyrofiban, Abciximab).
Aspirin should be prescribed to all patients in the initial loading dose of 150-300 mg and maintaining a dose of 75-100 mg for long-term therapy, regardless of invasive or conservative treatment tactics. The P2YI2 inhibitor should be added to aspirin as quickly as possible, the reception continues at least 12 months. Recommended dose of Ticagrelor-180 mg Load, 90 mg twice a day or prasuagrel- 60 mg Load dose, 10 mg daily. In the absence of these drugs, clopidogrel-300-600 mg loading dose is used, 75 mg supporting. When carrying out a planned operational treatment, the cancellation of P2yi2 inhibitors is required by no less than 5-7 days before the operation.
Adding to the treatment of inhibitors of glycoprotein IIB / IIIA patients already receiving double antitrombocytic therapy is recommended at high RISK PCV (elevated troponin, discovered trombo) or patients received to angiography only aspirin.
Revascularization at OKSBPST It is carried out to relieve anginal pain, elimination of myocardial ischemia and preventing them and death and death. Indications for its implementation depend on the volume and severity of the lesion and are determined by the data of coronaryogeniography, the condition of the patient and the concomitant pathology.
Urgent invasive tactic
The urgent invasive tactic (less than 2 hours) is used in very high risk patients:
- refractory angina;
- returning angina (with changes or without S-T segment, teeth T), despite intensive drug treatment;
- clinical manifestations of heart failure;
- life-degraded arrhythmias (ventricular fibrillation, ventricular tachycardia).
Early invasive tactics (within 24 hours) is used in patients with a primary positive response to antianginal therapy, but having a primary high-risk criterion: an increase or decrease in troponin or dynamic oscillation of the S-T segment or T. T.
In patients without recurrence symptoms, but having a diabetes in history, recently transferred to PCV, preceding aorto-coronary shunting, reduction of the left ventricular emission fraction, renal failure or early post-infarction angina, invasive tactics are carried out within 72 hours.
Patients who do not have the above risk factors are treated conservatively. Before discarding from the hospital, you need to perform a stress test for further treatment planning.
Long-term treatment
Long-term treatment is of paramount importanceSince the ischemic complications continue to occur with a high frequency after the acute phase of the CHA. Intensive impact on risk factors and lifestyle change is necessary for all patients with OXBPST. The first, where to start - this is a refusal of smoking. A long-term (lifelong) reception of beta-blockers to all patients with a reduced left ventricular emission fraction is recommended (FV Lzh<40%).
Inhibitors of angiotensin-converting enzyme (ACE) are prescribed to patients with heart failure, diabetes, arterial hypertension, chronic kidney diseases, as well as to all other patients * for the prevention of recurrences of ischemic events. Angiotensin receptor blockers should be prescribed with the intolerance of ACE inhibitors. Stantian therapy It is recommended to begin in the early duration of the disease with the target level of low density lipids less than 1.8 mmol / l.
Attention! The information on the site is not a medical diagnosis, or leadership to action and It is intended only for familiarization.