Transient ischemic attack: causes, signs, diagnosis, therapy, prognosis. What is a transient ischemic attack, symptoms and treatment Transient ischemic attack
Vascular diseases of the brain occupy an important place in cerebral pathology. They account for about 70 percent of all brain pathology. The reason for this is malnutrition, arterial hypertension, concomitant diseases of internal organs. All this leads to the fact that for one reason or another, cerebral blood flow may be disrupted, which leads to the appearance of various cerebral and focal symptoms.
These circulatory disorders are subdivided according to the duration of their onset. If the symptoms of brain damage do not disappear within a day and have a tendency to progress, then in this case, the development of a stroke is judged. If the developed symptoms disappeared within 24 hours, one can safely judge the development of a transient disturbance of blood flow or an ischemic attack.
What is a transient ischemic attack?
Transient ischemic attack - differences from stroke
Transient ischemic attack(or TIA) - refers to temporary disorders of cerebral circulation. As mentioned above, the cause of its development is usually systemic atherosclerosis, diseases of the heart and blood vessels (especially, arterial hypertension), diabetes, hereditary pathology vessels, as well as many other factors. All of them, acting in aggregate or separately, lead to the fact that the amount of blood flowing to the brain decreases. As a result, due to a lack of oxygen, some processes occur in the nervous tissue (the leading among which is anaerobic glycolysis), which lead to disruption of the natural metabolism of neurons and the formation of pathological molecules or substances that provoke damage to the nerve cell and the development of focal or cerebral symptoms.
However, due to their short-term action, neurons are not completely affected and can fully recover for some time. It is in this case that the development of TIA in the patient is judged.

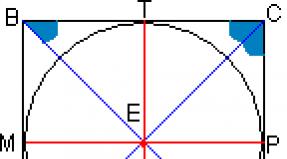
Anatomically, a special vascular “formation” is responsible for the blood supply to the brain - the Wilisian circle, from which all areas of the brain receive blood.
Clinically, the brain receives blood through two main vessels - the carotid and vertebral arteries. The carotid artery, for the most part, feeds the tissue of the hemispheres and cortex with blood. The basin of the vertebral artery (vertebro-basilar) carries blood mainly to the base of the brain and some components of its trunk (in particular, to the cerebellum).
Due to this separation, a transient ischemic attack can develop in any of these pools, leading to the development of a clinic typical for each type of attack.
What are the symptoms of transient ischemic attack?

Most often, the development of TIA is observed in the basin of the carotid artery. As a result, the symptoms can be completely different (depending on the area that the affected vessel innervates).
Most often, a transient ischemic attack in the coronary basin manifests itself in the form of transient speech disorders (with its development in the supply area of the left carotid artery, which feeds the cortex of Broca's center with blood), numbness of a limb or part of the face. For a short period of time, motor activity in the arm and leg of one side of the body may be disrupted (most often it persists in the future, and the process turns into a stroke).
Transient ischemic attack in VBD has a slightly different symptomatology. Symptoms such as dizziness and unsteadiness when walking come first. Patients worried about general weakness all over the body. The attack may be accompanied by a slight trembling sensation in the limbs. With an objective examination, it is possible to determine the presence of symptoms such as nystagmus, ataxia and intention (symptoms of ischemia in the basilar circulation). The feeling of numbness is rare.
Establishing diagnosis

First of all, the diagnosis of TIA consists in identifying cerebral and focal symptoms, as well as their subsequent regression after a while. As already mentioned, if the developed symptoms do not disappear during the day, then we can safely suspect the development of a stroke.
Differential diagnosis can be performed between stroke and TIA on the first day of the onset of the disease using computed tomography. With the development of a stroke in the picture, it is possible to recognize the presence of an ischemic zone (penumbra) in the nervous tissue. If there is a transient ischemic attack, then there may be no changes in the image.
Lumbar puncture, which is used to differentiate ischemic disorders and hemorrhages, with an ischemic attack will not provide reliable data necessary for a diagnosis. A sufficiently informative study is BCA ultrasound, which makes it possible to determine the presence of stenosis in the brachiocephalic arteries.
If there are signs of focal lesions and general cerebral symptoms, treatment should be started immediately.
What drugs are most effective in treating TIA?

As with ischemic stroke, TIA treatment has two main goals:
- Neuroprotection.
- Improving brain metabolism.
- TIA in the vertebrobasilar basin is stopped by taking vinpocetine, pentoxifylline (improve microcirculation).
The sooner the appropriate neuroprotective therapy is prescribed, the higher the likelihood of eliminating the symptoms of ischemia and preventing the development of stroke. Drugs such as choline alfascerate, ceraxon, actovegin are used as neuroprotectors. Quite high results are shown by this therapy in the treatment of ischemic attacks in the coronary artery basin.
A transient ischemic attack, during its development, disrupts the normal consumption of glucose by nerve cells, as a result of which the destruction of nerve cell membranes by products of glucose oxidation develops. In order for such a lesion to be as safe as possible, various solutions are used (in particular, crystalloids are prescribed - acesol, Ringer, trisol). These drugs prevent the development of ischemia in the brain tissue and promote the washing out of glucose oxidation products from it.
Prevention of TIA

There are no specific methods for preventing ischemic attacks. All forces should be aimed at restoring the permeability of cerebral vessels, improving blood supply during internal organs, as well as nervous tissue and timely treatment of concomitant diseases that can trigger the development of a stroke.
Particular attention should be paid to competent and timely treatment. arterial hypertension and diabetes mellitus. It is with a combination of these diseases that the risk that a transient ischemic attack will develop is highest.
If TIA has already developed, then after providing medical care to the patient (about 10 days in a hospital), the patient is recommended to be referred to the office of paroxysmal conditions and stroke prediction, where he will be given appropriate instructions and instructions on how to prevent the development of stroke and transient attacks.
In general, adherence to the basic principles of a healthy lifestyle and timely treatment other diseases will prevent the development of ischemic attacks and prevent the development of more formidable complications.
Forecast
The development of a transient disturbance of cerebral blood flow is a dangerous harbinger. If it has shown itself at least once, it is possible that such attacks may be repeated, therefore, it is necessary to take all measures to prevent them.
As for the possible outcomes, it is difficult to predict the patient's condition. It is not known if there will be more ischemic attacks and how they will show themselves. If you follow all the doctor's prescriptions, as well as change your lifestyle, the prognosis for TIA is quite favorable, and the risk of a second attack is minimal.
If you do not carry out preventive treatment and abuse their health, a transient disorder can lead to the development of a more severe pathology - a cerebral infarction, which is much more difficult to cope with.
The most unfavorable prognosis is in those patients who suffer from malignant arterial hypertension and whose history has already had episodes of TIA with a tendency to shorten the period of remission.
TIA, or transistor ischemic attack, is necrosis of brain tissue that occurs as a result of loss of blood supply, but the process is almost always reversible.
Thus, the damaged brain tissue regenerates quite calmly without serious harm to the patient's body. TIA completely regresses within 24 hours.
Depending on which area of the brain was affected, an ischemic attack can have different manifestations. This disease has many different causes, but it is very important to calculate and treat it in a timely manner in order to eliminate the risk.
Therefore, all patients with TIA need urgent hospitalization, followed by rehabilitation and consultation with a doctor.
Violation in detail - concept and features
A transient ischemic attack is a transient disorder in the bloodstream of the brain, in which a small branch that feeds parts of the brain for a while ceases to transmit oxygen along with the blood.
It is very important that with an ischemic attack, as mentioned above, all disorders begin to regress, from which there are no serious consequences in the disruption of life, some time after rehabilitation. Otherwise, it will no longer be an ischemic attack, but.
If you do not carry out the necessary rehabilitation procedures, then the chance of appearance after TIA increases significantly, as in a fifth of patients it develops in just a month from the moment of manifestation, and in half in the first half of the year.
Some neurologists and cardiologists even note that a microstroke makes it possible to "train" the body for a stroke, as it begins to create new vascular branches and completely strengthen the central nervous system. This is confirmed by the fact that if a person who has suffered a stroke, has not previously suffered a TIA, then he will have more serious consequences for the whole body.
Difference from stroke
TIA is still very different from, even if it is a prerequisite for it. The main difference is that with an ischemic attack  the affected nerve tissue is restored, unlike a stroke.
the affected nerve tissue is restored, unlike a stroke.
Even so, during TIA, the human body begins to lose various functionalities, depending on which area of the brain has been damaged.
In a transistor attack, the vessel is blocked only for a short time. At this moment, the neurons to which oxygen is not supplied begin to die off.
To avoid this, the vessels begin to dilate, increasing blood flow to the head. And if an aerobic method of obtaining energy is impossible, neurons proceed to an anaerobic method (glycolysis).
Immediately after the end of the attack, regenerative processes begin to restore dead tissue.

Blood is needed for everyone
The causes of TIA are diseases and conditions of the body in which the blood flow to the brain is blocked. These reasons are:
- atherosclerosis;
- vessels affected by atherosclerosis, very often the carotid artery or vertebral artery;
- hypertension, in which, in the affected areas, the vessels lose their ability to contract;
- heart disease that increases the likelihood of blood clots;
- gradually leaving on the walls of blood vessels in the head, arising due to mechanical damage and;
- inflammatory processes of blood vessels in the brain;
- congenital malformations and anomalies of blood vessels, from which their functions are distorted;
- during childbirth or pregnancy;
- different types of diabetes mellitus;
- bad habits, along with smoking and alcohol, causing vasospasm and leading to TIA;
- overeating and, as a result, obesity.
Features of the clinical picture and diagnosis
The disease begins to develop rapidly, due to which the peak state is reached in literally a few seconds, or less often in a couple of minutes.
Before the attack itself, no visual disturbances or other body functions are observed, no nausea or any strange other conditions of the body appear. TIA has no preliminary symptoms.
According to statistics, men in 60-70 years old have an increased chance of TIA, in the female part of the population it rises in 70-80 years. There is no longer any difference in the development of the disease between the sexes.
The manifestation depends on the area of the brain damage. For example, a transient ischemic attack in the vertebrobasilar basin of the carotid arteries differs from an attack in the spinal artery, and is manifested by the following symptoms:

If a failure in blood circulation occurred in the vertebral artery, then the following symptoms are revealed:
- slight nausea, vomiting is possible;
- and disorientation;
- violations in the area of the vestibular apparatus;
- impaired fine motor skills and general coordination of movements;
- loss of sensation on the side of the body opposite the affected side of the brain.
With a certain form of lesion, one of the eyes is covered with a "veil" for a few seconds, after which it gradually returns to normal.
A prerequisite for this may be high temperatures, or sudden changes blood pressure... The part of the body opposite to the blind side of the face may lose sensitivity and coordination of movements.
Another common symptom is short-term memory loss, from which a person cannot remember what he was doing a couple of hours, or even a day before the attack.
So, if long-term memory is able to be preserved only in part, then short-term memory is lost almost completely. For a patient who wakes up after losing consciousness, repeated and meaningless questions are characteristic.

In order to diagnose TIA, it is enough to identify the following symptoms:
- loss of sensitivity of a certain part of the body, or face;
- loss of fast and fine motor skills of the body, manifested in the inability to take a spoon or run;
- loss of senses is possible, from sight to touch;
- double in the eyes;
- dizzy;
- coordination is disturbed up to loss of consciousness.

After hospitalization, patients are assigned diagnostics nervous system, most often with the help of. The diagnosis is finally made 24 hours after the onset of TIA, referring to the results of an MRI study.
An integrated approach to therapy and rehabilitation
The processes of treatment and rehabilitation of patients after transistor ischemic attack are possible only in special neurological departments.
The medical method of treatment includes the appointment of special drugs, the task of which is to thin the blood and speed up its delivery to the affected areas of the brain. Then the normal heartbeat can be restored by implant or medication.
 It is carried out, and in the case of a stenosis of 50 percent or more of the lumen of the arteries, an operation is performed to stent the arteries, such as: angioplasty or carotid endarterectomy.
It is carried out, and in the case of a stenosis of 50 percent or more of the lumen of the arteries, an operation is performed to stent the arteries, such as: angioplasty or carotid endarterectomy.
After a week after the attack, special massages and exercise therapy are prescribed for rehabilitation.
Also, the patient is recorded to a psychologist for full recovery, and if necessary, then to a speech therapist.
What is dangerous
As a result of TIA, there is a high chance of development, and in order to avoid it, it is necessary to begin the patient's rehabilitation in advance. It is also necessary to consult a doctor so that he prescribes the whole range of therapeutic measures.
It is possible to receive a large number of mechanical injuries as a result of lack of sensitivity during TIA, as well as impaired coordination. In addition, internal damage to the body caused by the symptoms of the disease is also possible.
In order to prevent
According to statistics, the first couple of days after TIA, 15 percent of patients get a stroke, while after three days, the chance doubles. 
The only effective prevention can be only regular examination, and treatment for all pathologies, against which an ischemic attack can develop.
It is also necessary to undergo Doppler sonography of the vessels of the head every year and monitor your cholesterol levels, as well as other fats.
It is necessary to maintain a healthy lifestyle, refrain from fatty and sugary foods, and do not overeat. Undergo a blood clotting test, and be regularly examined by your doctor in order to avoid accidental manifestations.
It is important to avoid severe stressful situations and try not to overwork, it is necessary to maintain healthy sleep.
Transient ischemic attack, or TIA (ICD-10 code - G45) - in medicine is often called a microstroke for very similar to a stroke, but less pronounced, symptoms and consequences.
Nevertheless, this condition is not a stroke, even with the prefix micro. It is a circulatory disorder of the brain that affects the central nervous system, related to neurology.
The condition is dangerous in that its symptoms disappear within 24 hours after the onset of the attack, so it can often be interpreted as frivolous.
But if a patient was diagnosed with TIA, then it must be borne in mind that this pathology has frequent relapses and that it is a harbinger of ischemic stroke.
In most cases, elderly people are susceptible to transient ischemic attacks of the brain. Most often, the manifestation of this pathology is due to problems with pressure and the formation of blood clots and plaques on the walls of blood vessels.
In addition, the reasons may be:
- - the formation of cholesterol plaques on the walls of the vessels of the brain;
- myocardial infarction and other manifestations of heart ischemia;
- heart rhythm disturbances;
- stretching of the cavities of the heart (dilated cardiomyopathy);
- vasculitis;
- diabetes;
- arterial hypertension;
- heart defects;
- hypoplasia or aplasia (underdevelopment) of cerebral vessels;
- osteochondrosis of the cervical spine;
- - inflammation of the arteries and veins.
There are several risk factors, the presence of which in a person can lead to the onset of TIA:
- bad habits (such as alcohol, smoking, drugs, diet and physical inactivity);
- mental disorders (depression);
- cardiac disorders (for example, with heart attacks).
Children and adolescents are practically not susceptible to this disease, but it can still occur in the case of severe heart disease. But most often the pathology occurs in people over fifty years old.
Typical symptoms
The disease is characterized by sudden onset and rapid progression. It is because of the disappearing symptoms and a visible improvement in the condition that patients do not seek medical help and TIA progresses to full-fledged ischemic stroke.
In turn, acute disorders of cerebral circulation (ACVA) lead to disability and, in advanced cases, to death.
The clinical picture of pathology is neurological changes that can change depending on the affected vessels and the severity of the lesion:
In total, there are three degrees of severity of the course of pathology:
- easy - the attack lasts up to 15 minutes;
- medium - an attack lasts from 15 minutes to an hour;
- heavy - duration from an hour to a day.
If the duration of the attack is more than 24 hours, acute cerebrovascular accident and a full-fledged stroke are diagnosed.
Differential diagnosis
Diagnosing this pathology is difficult for several reasons:
- First, the disappearance of symptoms. An attack of TIA lasts a maximum of a day, or it may end in less than 10 minutes.
- Secondly, the manifestations of the attack are similar to the manifestations of other diseases, for example - epilepsy, migraine, multiple sclerosis, stroke, hypertensive cerebral crisis, hypertensive crisis, etc. Therefore, it often remains unspecified.
To clarify the diagnosis, neurologists resort to differential diagnosis.
Its principle is to compile a list of diseases that have similar symptoms, and to search for specific manifestations of any pathology in a patient.
If you suspect a TIA, use:
- collection of anamnesis (pay attention to diseases that manifested themselves in relatives);
- examination in otolaryngology and cardiology (symptoms may resemble diseases of the hearing or heart);
- blood tests (general, biochemical);
- blood clotting analysis (the pathogenesis of TIA is characterized by an increase in blood viscosity);
- instrumental diagnostic methods (ECG, computed tomography, duplex scanning, MRI).
MRI (if this method is not available, then computed tomography) is the most accurate way to differentiate this disease. When TIA decryption should not be detected focal changes, if they appear in the pictures, then the pathology has already passed into the stage of a stroke.

How is the treatment carried out?
This disease is a consequence of the presence of other pathologies in the patient, which in the future can provoke an ischemic stroke. Therefore, after stopping the attack, treatment is to prevent possible complications.
If signs of TIA appear, you need to call emergency care so that the patient is hospitalized. Treatment is carried out in a hospital.
The terms of incapacity for work vary depending on the severity of:
Home treatment is carried out only if the patient does not lose his ability to work, the frequency of attacks is low, and if they increase, the patient will have the possibility of urgent hospitalization (people of age are hospitalized in any case).
Therapy consists in gradually lowering blood pressure and preventing thrombosis. Assign. Rehabilitation also includes diet and daily exercise.
Patients are prescribed the following medications:
- direct anticoagulants - affect blood clotting in thrombosis;
- antihypertensive drugs - lowering blood pressure;
- drugs that improve cerebral blood flow;
- neuroprotectors - prevent damage to neurons.
In addition to drug therapy, balneotherapy is used - treatment with mineral and radon waters. The same method includes rubdowns and a circular shower.
Balneotherapy refers to physiotherapy and, in addition to treatment with waters for pathology, they are used:
- electrophoresis;
- alternating magnetic field;
- microwave therapy
Also, in cases of frequent relapses, so that TIA does not recur again, surgical intervention can be performed - removal of the internal layer of the carotid artery affected by atherosclerosis (endarterectomy).
The only correct first aid measure for this pathology is to call an ambulance. Since TIA is easily confused with other diseases, it is recommended to wait for the arrival of doctors and not to give the patient any medications.
Potential consequences and prognosis
Often, TIA goes away without any consequences, and sometimes neurological symptoms remain, which disappear within a few days. Often, attacks are repeated, and their increased frequency is especially dangerous.
The prognosis depends on the cause, concomitant diseases, but, as a rule, it is unfavorable.
Patients who have undergone an ischemic attack may subsequently develop ischemic stroke.
Key points:
Signs
Symptoms of a transient ischemic attack depend on which vessels are affected and which area of the brain is damaged. If the damage is localized in the carotid basin, that is, if the carotid arteries are damaged, then the person's coordination of movements, speech, vision is impaired (temporary blindness or decreased vision in one eye is possible). Paresis also develops, and predominantly any one area of the body or a group of muscles is affected, for example, paresis of the hand or foot, or fingers. The skin of the face, hands and feet loses sensitivity. In some cases, the sensitivity decreases in half of the body.
With ischemia in the vertebrobasilar basin (in the vertebral basin and the basilar artery), a person develops dizziness. headache in the back of the head. Speech, memory, coordination of movements are impaired, dysphagia develops. Double vision, darkens, vision falls, hearing deteriorates. Possibly numbness around the mouth or paresis of half of the face.
Description
Unfortunately, a transient ischemic attack is not recognized in time in 60% of cases. This is due to the fact that many often underestimate the severity of the symptoms and do not go to the doctor. In addition, this condition often occurs in a dream, and since it has no consequences, patients do not even know about it. That is why it is impossible to accurately establish the incidence of the disease. Doctors suggest that transient ischemic attacks occur in 12-35% of people over 50 years old.
The cause of a transient ischemic attack is a restriction of blood supply to any part of the brain due to blockage of a vessel supplying blood to the brain. This can be due to a blood clot or an atherosclerotic plaque. In very rare cases, a transient ischemic attack can be caused by hemorrhage. However, in this condition, blood circulation is restored rather quickly.
Thromboembolism can occur when:
- artificial heart valve;
- mitral stenosis with atrial fibrillation;
- sick sinus syndrome;
- infective endocarditis;
- acute period of myocardial infarction;
- atrial fibrillation;
- dilated cardiomyopathy;
- myxoma of the atrium (a benign tumor in the upper left or right side of the heart that has grown into this organ);
- thrombus of the left ventricle or left atrium.
However, the development of this condition is also possible with non-closure of the foramen ovale, non-bacterial thrombotic endocarditis, congestive heart failure, calcification mitral valve, mitral valve prolapse, coagulopathies, angiopathies, especially with abnormalities in the development of the carotid and vertebral arteries.
Risk factors for transient ischemic attack:
Although the prognosis for TIA is good, it is a dangerous harbinger of stroke. There is evidence that within a month after TIA, stroke develops in 4-8% of patients, during the first year - in 12%, during the next five years - in 29%.
Diagnostics
With a transient ischemic attack, you need to consult a cardiologist, angiologist and ophthalmologist. You may also need testing by a medical psychologist.
It is also necessary to pass the general and biochemical analysis blood, general analysis urine. blood on a coagulogram.
Treatment
Treatment usually takes place in a hospital. The patient is allowed to go home only if he has the opportunity, in the event of a second attack, to be immediately hospitalized in a hospital. Those who have undergone a transient ischemic attack are prescribed antiplatelet (blood thinning) drugs, vasodilator drugs, drugs to lower blood cholesterol levels. If necessary, antihypertensive drugs are also prescribed.
With an increase in the frequency and duration of transient ischemic attacks, they can resort to surgical treatment- remove fat, constricting the artery and its damaged area, or do angioplasty.
Balneotherapy - coniferous, radon, salt, gives a good effect in treatment. Pearl baths, circular shower, wet wipes.
Physiotherapy is often prescribed - electrophoresis, alternating magnetic field, microwave therapy.
Prophylaxis
Prevention is aimed at eliminating risk factors. That is, you need to go in for sports, eat right. limit the use of salty and fatty foods, monitor weight. do not abuse alcohol. quit smoking.
It is also necessary, if necessary, to take drugs that improve the rheological properties of the blood ("thinning" the blood).
Transient ischemic attack - a harbinger of stroke
TIA (transient ischemic attack) refers to ischemic stroke. TIA symptoms last no more than 1 hour. If the clinical signs of an attack do not go away within a day, then doctors diagnose a stroke. TIA (and in the people, just a microstroke) seems to be a signal for a person that a catastrophe is brewing in the brain, so this condition must be taken very seriously.
TIA reasons
TIA is caused by oxygen deficiency in one of the brain regions. Ischemia (oxygen starvation) develops, and if you do not take action, then a stroke may occur. If ischemia occurs in the part of the brain responsible for speech, then the person will have speech disturbances, if the "visual" area, then there will be disturbances in the function of vision. If ischemia occurs in the vestibular region of the brain, then the patient complains of severe dizziness and nausea.
Clinical manifestations
Depending on the focus of ischemia, the clinical manifestations will be different. Most often, the patient is worried about severe dizziness, nausea, vomiting, double vision, severe pain in the back of the head, fear of light, impaired coordination. Focal symptoms include paresis of one or two limbs, decreased sensitivity and numbness in the limbs, impaired speech function, and its slowdown. The so-called “scissors” symptom is present, when the right (left) part of the brain hemisphere is affected, and paresis occurs in the opposite limb. On the first day of TIA, stroke occurs in about 10% of patients, and after 3 months, in another 20%. About 30% of patients, within 5 years after TIA, suffer a cerebral stroke, its severity depends on the frequency of ischemic attack.
Diagnostics
Most often, it is very difficult to establish a diagnosis of TIA, since before the arrival of the doctor, its symptoms disappear abruptly. However, one cannot refuse hospitalization, since if the cause of the attack was a blockage of one of the vessels, then a stroke will develop within a few hours or days. In the hospital, the victim will be diagnosed and urgently taken measures. It would be best to arrive at the hospital within 3 hours after the first TIA.
In the hospital, the patient will undergo ECG, magnetic resonance imaging, angiography of blood vessels, ultrasound with Doppler. Treatment should be carried out only in a hospital, no later than 2 days after the initial manifestations of TIA. Regardless of when the attack was and how it manifested itself, people over 45 years old, or those who have had at least one TIA attack in the last 5 years, are subject to compulsory hospitalization.
According to statistics, TIA is considered very dangerous factor risk of ischemic stroke. Neurologists say people who have had TIA are at greater risk of developing a stroke. Within 30 days, the danger reaches 4-8%, during the year it increases to 12-13%, and after another 5 years it reaches 24-29%. According to studies, the risk of stroke in people who have undergone an attack increased 13-16 times during the first year and about 7 times over the next 5 years. These indicators do not show all the difference in the forecast of individual groups. Patients who underwent TIA of the cerebral hemispheres, and at the same time stenosis of the internal carotid artery was more than 70%, have a risk of more than 40% of stroke, within 2 years.
It is very important to diagnose TIA correctly and quickly. As mentioned above, the risk of stroke exceeds the threshold of more than 5% during the first month. The early development of ischemic stroke is significantly increased in those people who have had a recent TIA, or an attack that has been repeated several times in the last 5 years. The doctor needs to clarify with the patient how the TIA proceeded, what clinical manifestations contributed to it, whether there were speech impairments or decreased sensitivity in the limbs, whether it was manifested by numbness of the fingers. One of the important clinical signs associated with the presence of atherosclerosis of the carotid artery is short-term blindness of the ipsilateral eye (from lat.amauros fugax).
It is believed that stenosis of the carotid artery is the very first sign of the development of cerebral ischemia, which is manifested by an ischemic attack. A neurologist must necessarily carry out auscultation of the vessels of the neck in people over 40 years old. If the carotid arteries are affected by atherosclerosis, a systolic murmur is heard in 70% of cases, which is already a sign of vascular damage. More than a quarter of a century ago, Academician Pokrovsky identified 4 degrees of vascular lesion and clinical manifestations cerebral ischemia. This classification differed from others in that it had the first group of cerebrovascular insufficiency - asymptomatic. This group included patients who did not have any clinical manifestations of cerebral vascular insufficiency. However, these patients had vascular lesions in the form of systolic murmur on auscultation of the neck vessels and in the difference in arterial systolic pressure between the two arms.
Transient ischemic attack: causes, signs, diagnosis, therapy, prognosis
Transient ischemic attack (TIA) used to be called dynamic or transient cerebral disorder circulation... which, in general, quite well expressed its essence. Neurologists know that if TIA does not go away within 24 hours, then the patient should be given another diagnosis - ischemic stroke .
People without medical education, referring to search engines or in some other way trying to find reliable sources describing this type of cerebral hemodynamic disorder, may call TIA a transit or transistor ischemic attack. Well, they can be understood, diagnoses are sometimes so tricky and incomprehensible that you break your tongue. But if we talk about the names of TIA, then, in addition to the above, it is also called cerebral or transient ischemic attack .
In its manifestations, TIA is very similar to ischemic stroke, but that is why it is an attack in order to attack only for a certain short time. after which there is no trace of general cerebral and focal symptoms. Such a favorable course of a transient ischemic attack is due to the fact that it is accompanied by microscopic damage to nerve tissue... who subsequently do not affect on human life.
difference between TIA and ischemic stroke
Causes of transient ischemia
Factors that have caused impaired blood flow in some part of the brain, mainly microemboli... become the causes of a transient ischemic attack:
- Progressive atherosclerotic process (vasoconstriction, disintegrating atheromatous plaques and cholesterol crystals can be carried with the bloodstream into vessels of smaller diameter, contribute to their thrombosis, resulting in ischemia and microscopic foci of tissue necrosis);
- Thromboembolism resulting from many heart diseases (arrhythmias, valvular defects, myocardial infarction, endocarditis, congestive heart failure, coarctation of the aorta, antrioventricular block and even atrial myxoma);
- Arising suddenly arterial hypotension. inherent in Takayasu's disease;
- Burger's disease (obliterating endarteritis);
- Osteochondrosis of the cervical spine with compression and angiospasm, which results in vertebrobasilar insufficiency (ischemia in the basin of the main and vertebral arteries);
- Coagulopathy, angiopathy and blood loss. Microemboli in the form of aggregates of erythrocytes and platelet conglomerates, moving with the blood flow, they can stop in a small arterial vessel, which they could not overcome, since they turned out to be larger in size. As a result - blockage of the vessel and ischemia;
- Migraine.
In addition, the onset of cerebral ischemic attack is well promoted by the eternal prerequisites (or satellites?) Of any vascular pathology: arterial hypertension. diabetes mellitus, cholesterolemia. bad habits in the form of drunkenness and smoking, obesity and physical inactivity.
Signs of TIA
The neurological symptoms of an ischemic attack of the brain, as a rule, depend on the site of the circulatory disorder (the basin of the basilar and vertebral arteries or the carotid basin). The identified local neurological symptoms help to understand in which particular arterial basin the disorder occurred.
For transient ischemic attack in the area vertebro —basilar basin are characterized by such signs as:
If TIA has affected pool of carotid arteries... then the manifestations will be expressed by a disorder of sensitivity, speech disorders, numbness with impaired mobility of the arm or leg (monoparesis) or one side of the body (hemiparesis). In addition, apathy, deafness, drowsiness can complement the clinical picture.
Sometimes patients have severe headache with the appearance meningeal symptoms... Such a depressing picture can change as quickly as it began, which does not give any reason to calm down, since TIA can attack the patient's arterial vessels in the very near future. More than 10% of patients develop ischemic stroke in the first month and in almost 20% within a year after a transient ischemic attack.
Obviously, the TIA clinic is unpredictable, and focal neurological symptoms can disappear even before the patient is taken to the hospital, therefore, anamnestic and objective data are very important for a doctor.
Diagnostic measures
Of course, it is very difficult for an outpatient with TIA to undergo all the examinations stipulated by the protocol, besides, the risk of a second attack remains, so only those who have the opportunity to be taken to the hospital immediately in case of neurological symptoms appear at home. However, persons over 45 years of age are deprived of this right and are hospitalized without fail.
Diagnosis of transient ischemic attacks is rather difficult, since the symptoms disappear, and the causes that caused the cerebrovascular accident continue to remain. They need to be clarified, since the likelihood of ischemic stroke in such patients remains high, therefore, patients who have undergone a transient ischemic attack need in-depth examination according to a scheme that includes:
- Palpation and auscultatory examination of arterial vessels of the neck and extremities with blood pressure measurement on both hands (angiological examination);
- Detailed blood test (general);
- A set of biochemical tests with the obligatory calculation of the lipid spectrum and atherogenic coefficient;
- Study of the hemostasis system (coagulogram);
- Electroencephalogram (EEG);
- REG of head vessels;
- Doppler ultrasound of the cervical and cerebral arteries;
- Magnetic resonance angiography;
- CT scan.

All people who have undergone TIA at least once should undergo such an examination, due to the fact that focal and / or cerebral symptoms characterizing a transient ischemic attack and arising suddenly, usually do not linger for a long time and do not give consequences. Yes, and an attack can happen only once or twice in a lifetime, so patients often do not attach much importance to such a short-term health disorder at all and do not run to the clinic for advice. As a rule, only inpatients are examined, therefore it is difficult to talk about the prevalence of cerebral ischemic attack.
Differential diagnosis
The difficulty in diagnosing a transient ischemic attack also lies in the fact that many diseases, with neurological disorders, are very similar to TIA, for example:
- Migraine with aura gives a similar symptomatology in the form of speech or visual disturbances and hemiparesis;
- Epilepsy... an attack of which can end in a disorder of sensitivity and motor activity, and even tends to sleep;
- Transient global amnesia... characterized by short-term memory disorders;
- Diabetes can "afford" any symptomatology, where TIA is no exception;
- The initial manifestations of multiple sclerosis are well mimicked for transient ischemic attack. which confuse doctors with such TIA-like signs of neurological pathology;
- Meniere's disease... proceeding with nausea, vomiting and dizziness, very similar to TIA.
Does transient ischemic attack require treatment?
Many experts are of the opinion that TIA itself does not require treatment, unless the patient is in a hospital bed. However, given that transient ischemia is caused by cause-diseases, it is still necessary to treat them so that an ischemic attack or, God forbid, an ischemic stroke does not occur.
Fighting bad cholesterol with it high rates, carried out by the appointment of statins, so that cholesterol crystals do not run through the bloodstream;
An increased sympathetic tone is reduced by the use of adrenergic blockers (alpha and beta), well, and its unacceptable decrease is successfully stimulated by the appointment of tinctures such as pantocrine, ginseng, caffeine and lure. Preparations containing calcium and vitamin C are recommended.
With the intensive work of the parasympathetic department, drugs with belladonna, vitamin B6 and antihistamines are used, but the weakness of the parasympathetic tone is leveled by potassium-containing drugs and small doses of insulin.

It is believed that in order to improve the functioning of the autonomic nervous system, it is advisable to act on both of its parts, using the preparations of grandaxin and ergotamine.
Arterial hypertension, which greatly contributes to the onset of an ischemic attack, needs long-term treatment, which includes the use of beta-blockers, calcium antagonists and angiotensin-converting enzyme (ACE) inhibitors. The leading role belongs to medicines improving venous blood flow and metabolic processes occurring in the brain tissue. The well-known cavinton (vinpocetine) or xanthinol nicotinate (theonikol) is very successfully used to treat hypertension, and, consequently, to reduce the risk of cerebral ischemia.
With hypotension of cerebral vessels (REG conclusion), venotonic drugs (venoruton, troxevasin, anavenol) are used.
Treatment of disorders plays an important role in the prevention of TIA. hemostasis... which is being corrected antiplatelet agents and anticoagulants .
Useful for the treatment or prevention of cerebral ischemia and drugs that improve memory: piracetam, which also has antiplatelet properties, actovegin, glycine.
Various mental disorders (neuroses, depression) are fought with tranquilizers, and a protective effect is achieved with the use of antioxidants and vitamins.
Prevention and prognosis
The consequences of an ischemic attack are a recurrence of TIA and ischemic stroke, therefore, prevention should be aimed at preventing a transient ischemic attack so as not to aggravate the situation with a stroke.
In addition to the drugs prescribed by the attending physician, the patient himself must remember that his health is in his hands and take all measures to prevent cerebral ischemia, even if transient.
Everyone now knows what role belongs in this plan. healthy way life, proper nutrition and physical education. Less cholesterol (some people like to fry 10 eggs with pieces of lard), more physical activity (it's good to do swimming), giving up bad habits (everyone knows that they shorten life), use of funds traditional medicine(various herbal seagulls with the addition of honey and lemon). These funds will definitely help, how many people have experienced themselves, because TIA has a favorable prognosis, but it is not so favorable in ischemic stroke. And this should be remembered.
Everyone knows about such a disease as stroke. Much less people is aware of the ischemic attack of the brain, which is also dangerous.
Etiology and pathogenesis
Acute circulatory disturbance in the brain is not always diagnosed, since it proceeds very quickly, and its symptoms disappear within an hour after the onset of the attack. Ischemic attack is called transient (TIA), which means "passing imperceptibly, transient." This is where its danger lies.
TIA is caused by damage to a segment of the brain due to a decrease or complete cessation of blood flow due to partial blockage of blood vessels.
Since this condition lasts no more than 1 hour, brain tissue is not damaged as deeply as in a stroke.

Causes leading to cerebral ischemia include:

All factors provoke a narrowing of the lumen of the arteries and blood vessels up to the complete blockage of the lumen.
Symptomatic picture
There are two forms of TIA, depending on the location of the focus with impaired circulation. If a failure occurred in the carotid arteries, then they speak of a carotid attack. When the blood supply is stopped due to damage to the vascular basin formed by the vertebral arteries, vertebrobasilar (VBD) ischemia is diagnosed.
With an ischemic attack of the brain, the symptoms are due to these types.
Common symptoms of the disease include:

The disease begins suddenly, and its symptoms grow with lightning speed to a maximum within a few seconds or minutes and persist for another 10 minutes, after which the patient's condition returns to normal.

Features of the disease
Failures of cerebral circulation can be repeated several times in a row for weeks and months, or occur once or twice in a lifetime. If the attack proceeds in easy form, then the clinical picture is blurred, and the patient does not go to the doctor. With more severe symptoms, the consequences of TIA are serious: from ten to forty percent of attacks lead to a stroke. The risk is especially high in the first week after an attack of cerebral ischemia.

A lethal outcome is likely within the first year after undergoing TIA in 10% of patients and five years in 40%.
In fact, an ischemic attack is a harbinger of a stroke.
In men from 60 to 70 years old and in women 75-85 years old, the disease is most likely against the background of cardiovascular pathologies and metabolic disorders.

Diagnostic measures
To make a diagnosis, the doctor asks the patient in detail about the symptoms. After collecting an anamnesis, a blood test is performed to determine:
- creatinine, sodium and potassium;
- glucose;
- plasma coagulation factors;
- cholesterol.
Other physiological fluids are also being investigated.
To exclude pathologies of the heart and lungs, an ECG and X-ray are performed.
If the doctor has doubts about the diagnosis, selectively prescribe:

TIA symptoms are similar to those with short-term neurological disorders, and it is the doctor's job to differentiate them. Such pathologies include:


After careful study clinical picture further examination is recommended to the patient.
Determining the cause of TIA
People who have had a cerebral ischemic attack are at risk of stroke. Therefore, procedures are carried out to determine the cause of the attack.:

CT and MRI do not always reveal ischemic foci, but in 25% of cases it is possible to determine a cerebral infarction.
Treatment of the disease
Only 40% of patients go to the clinic after an attack. A neurologist works with them.
Upon completion of the complex diagnostic activities treatment is prescribed to stop ischemia and restore normal blood circulation.
Drug treatment
To restore blood flow, ticlopidine, dipyridamole, and aspirin are prescribed. If the attack was caused by a blockage of the vessel, then apply indirect anticoagulants: warfarin sodium, ethyl biscumacetate, phenindione.
To thin the blood, saline solutions, a ten percent glucose solution, and dextran are injected drip. If the cause of TIA was a sharp rise in blood pressure against a background of hypertension, the doctor prescribes drugs to normalize it: atenolol, captopril, nifedipine, diuretics. To improve cerebral circulation, take vinpocetine, cinnarizine.

When attacked, neurons die due to metabolic disturbances. To stop cell death, the use of metabolites and cerebroprotectors is required. They include:

To relieve the main symptoms, take diclofenac (with severe headache); mannitol (with incipient cerebral edema).
Physiotherapy procedures
Along with the reception drugs, the neurologist recommends the consultation of a physiotherapist who may prescribe:


Depending on the concomitant diseases, the patient is prescribed one procedure or several.
Preventive measures
To prevent a recurrence or reduce the likelihood of its occurrence in people who have not yet experienced cerebral ischemia, it is necessary to change the lifestyle:

At elevated level cholesterol in the blood, as prescribed by a doctor, should take long-term drugs that reduce the amount of lipids (pravastatin, atorvastatin).

If a pathology of the vessels supplying the brain is detected, surgical intervention is indicated:
- endarterectomy - removal of plaque on the inner wall of the carotid artery;
- micro-shunting;
- arterial stenting.
Preventing TIAs can help prevent stroke.
0