Violation of the rhythm code according to mcb 10. How to control and treat paroxysmal atrial fibrillation (atrial fibrillation)? Extrasystole - causes and treatment of the disease
- Ectopic systoles
- Extrasystoles
- Extrasystolic arrhythmia
- Premature:
- reductions NOS
- compression
- Brugada syndrome
- Long QT syndrome
- Rhythm disturbance:
- coronary sinus
- ectopic
- nodal
In Russia, the International Classification of Diseases of the 10th revision (ICD-10) has been adopted as a single normative document to take into account the incidence, reasons for medical institutions all departments, causes of death.
ICD-10 was introduced into health care practice throughout the Russian Federation in 1999 by order of the Ministry of Health of Russia dated 05/27/97. No. 170
A new revision (ICD-11) is planned by WHO in 2017 2018.
As amended and supplemented by WHO
Processing and translation of changes © mkb-10.com
Ventricular extrasystole encoding according to ICD 10
Extrasystole refers to episodes of premature contraction of the heart due to an impulse that comes from the atria, atrioventricular areas and ventricles. An extraordinary contraction of the heart is usually recorded against the background of a normal sinus rhythm without arrhythmia.
It is important to know that ventricular premature beats in ICD 10 has a code of 149.
The presence of extrasystoles is noted in% of the entire population of the world, which determines the prevalence and a number of varieties of this pathology.
Code 149 v International classification disease is defined as other heart rhythm disturbances, but the following exceptions are also provided:
- rare myocardial contractions (R1 bradycardia);
- extrasystole due to obstetric and gynecological surgical interventions (abortion O00-O007, ectopic pregnancy O008.8);
- disturbances in the work of the cardiovascular vascular system in a newborn (P29.1).
The extrasystole code for ICD 10 determines the plan diagnostic activities and in accordance with the obtained survey data, a set of therapeutic methods used all over the world.
Etiological factor in the presence of extrasystoles according to ICD 10
Worldwide nosological data confirm the prevalence of episodic pathologies in the work of the heart in most of the adult population after 30 years, which is typical in the presence of the following organic pathologies:
- heart disease caused by inflammatory processes (myocarditis, pericarditis, bacterial endocarditis);
- the development and progression of coronary heart disease;
- dystrophic changes in the myocardium;
- oxygen starvation of the myocardium due to the processes of acute or chronic decompensation.
In most cases, episodic interruptions in the work of the heart are not associated with damage to the myocardium itself and are only functional in nature, that is, extrasystoles occur due to severe stress, excessive smoking, coffee and alcohol abuse.
Ventricular extrasystole in the international classification of diseases has the following types of clinical course:
- premature contraction of the myocardium, which occurs after each normal one, is called bigeminy;
- trigeminy is the process of a pathological impulse after several normal contractions of the myocardium;
- quadrigeminia is characterized by the appearance of extrasystoles after three contractions of the myocardium.
In the presence of any type of this pathology, a person feels a sinking heart, and then strong tremors in the chest and dizziness.
Place of ventricular extrasystole in the ICD system - 10
Ventricular premature beats is a type of cardiac arrhythmia. And it is characterized by an extraordinary contraction of the heart muscle.
Ventricular extrasystole, according to the International Classification of Diseases (ICD - 10), has a code of 149.4. and is included in the list of heart rhythm disorders in the heart disease section.
The nature of the disease
Based on the international classification of diseases of the tenth revision, doctors distinguish several types of extrasystoles, the main ones among which are: atrial and ventricular.
With an extraordinary heartbeat, which was caused by an impulse emanating from the ventricular conduction system, ventricular extrasystole is diagnosed. An attack manifests itself as a feeling of an interruption in the heart rhythm, followed by its fading. The disease is accompanied by weakness and dizziness.
According to ECG data, single extrasystoles can periodically occur even in healthy young people (5%). Daily ECG showed positive indicators in 50% of the studied people.
Thus, it can be noted that the disease is common and can affect even healthy people. The functional nature of the disease can be caused by stress.
The use of energy drinks, alcohol, smoking can also provoke extrasystoles in the heart. This type of ailment is harmless and passes quickly.
More serious consequences for the health of the body are pathological ventricular arrhythmia. It develops against the background of serious illnesses.
Classification
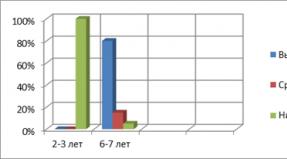
According to the daily monitoring of the electrocardiogram, doctors consider six classes of ventricular extrasystoles.
Extrasystoles belonging to the first class may not manifest themselves in any way. The remaining classes are associated with health risks and the possibility of a dangerous complication: ventricular fibrillation, which can be fatal.
Extrasystoles can vary in frequency, they can be rare, moderate and frequent. On the electrocardiogram, they are diagnosed as single and paired - two impulses in a row. Impulses can occur in both the right and left ventricles.
The origin of extrasystoles can be different: they can come from one source - monotopic, and they can occur in different areas - polytopic.
Disease prognosis
According to prognostic indications, the considered arrhythmias are classified into several types:
- arrhythmias of a benign nature, are not accompanied by heart damage and various kinds of pathologies, their prognosis is positive, and the risk of death is minimal;
- ventricular extrasystoles of a potentially malignant direction occur against the background of heart lesions, the release of blood is reduced by an average of 30%, there is a risk to health;
- ventricular extrasystoles pathological develop against the background of severe heart disease, the risk of death is very high.
In order to start treatment, a diagnosis of the disease is required in order to find out its causes.
Other heart rhythm disorders
Excluded:
- bradycardia:
- NOS (R00.1)
- sinoatrial (R00.1)
- sinus (R00.1)
- vagal (R00.1)
- conditions complicating:
- abortion, ectopic or molar pregnancy (O00-O07, O08.8)
- obstetric surgical procedures and procedures (O75.4)
- neonatal arrhythmia (P29.1)
Ventricular fibrillation and flutter
Premature atrial depolarization
Premature depolarization emanating from the compound
Gradation of ventricular extrasystole according to ryan and laun, microbial code 10
1 - rare, monotopic ventricular arrhythmia - no more than thirty VES per hour;
2 - frequent, monotopic ventricular arrhythmia - more than thirty VES per hour;
3 - polytopic ZhES;
4а - monomorphic paired LES;
4b - polymorphic paired VES;
5 - ventricular tachycardia, three or more VEBs in a row.
2 - infrequent (from one to nine per hour);
3 - moderately frequent (from ten to thirty per hour);
4 - frequent (from thirty-one to sixty per hour);
5 - very frequent (more than sixty per hour).
B - single, polymorphic;
D - unstable VT (less than 30s);
E - stable VT (more than 30 s).
Lack of structural damage to the heart;
No scar or heart hypertrophy;
Normal ejection fraction of the left ventricle (LVEF) - more than 55%;
Slight or moderate frequency of ventricular premature beats;
Absence of paired ventricular extrasystoles and unstable ventricular tachycardia;
Lack of persistent ventricular tachycardia;
Absence of hemodynamic consequences of arrhythmia.
The presence of a scar or heart hypertrophy;
Moderate decrease in LVEF - from 30 to 55%;
Moderate or significant ventricular premature beats;
The presence of paired ventricular extrasystoles or unstable ventricular tachycardia;
Lack of persistent ventricular tachycardia;
Absence of hemodynamic consequences of arrhythmia or their insignificant presence.
The presence of structural damage to the heart;
The presence of a scar or heart hypertrophy;
Significant decrease in LVEF - less than 30%;
Moderate or significant ventricular premature beats;
Paired ventricular extrasystoles or unstable ventricular tachycardia;
Persistent ventricular tachycardia;
Moderate or severe hemodynamic consequences of arrhythmia.
Classification of cardiac arrhythmias in ICD-10
All cardiologists know in which sections you can find heart rhythm disturbances in ICD-10. This pathology is common among people of different ages. With arrhythmias, the heart rate and coordination are impaired. Some conditions are potentially life threatening and can be fatal.
Arrhythmia is a pathological condition in which the regularity of myocardial contractions and heart rate are disturbed. The conductive function of the organ decreases. Often, this pathology remains unnoticed for a person. There are 3 large groups of arrhythmias:
- caused by impaired impulse formation (sick sinus syndrome, extrasystole, atrial and ventricular tachycardia, flutter and flicker);
- associated with the difficulty of conducting the impulse (blockade, syndrome of premature excitation of the ventricles of the heart);
- combined.
They all have their own distinctive features. Common clinical manifestations include a feeling of heart failure, difficulty breathing, fainting, weakness, and dizziness. Often there is an attack of angina pectoris. Discomfort in the chest is possible.
The group of arrhythmias includes ventricular premature beats. It is characterized by premature excitation of the myocardium. The ICD-10 code for this pathology is I49.3. The elderly are at risk. With age, the incidence rate increases. Single extrasystoles are often detected in young people. They pose no danger and are not pathological.
In the development of ventricular extrasystole, the following factors play a leading role:
- angina pectoris;
- acute myocardial infarction;
- cardiosclerosis;
- myocarditis;
- inflammation of the pericardium;
- vagotonia;
- osteochondrosis of the cervical spine;
- hypertonic disease;
- pulmonary heart;
- prolapse mitral valve;
- cardiomyopathy;
- overdose of medicines.
The classification of extrasystoles is known to all cardiologists. Extrasystoles are early, late and interpolated. By frequency, single, paired, group and multiple are distinguished. This disease is manifested by a feeling of palpitations, weakness, dizziness, a sense of fear and anxiety.
Among the diseases characterized by rhythm disturbances, an important place is occupied by atrial fibrillation... Otherwise, it is called atrial fibrillation. This pathology is characterized by chaotic and frequent (up to 600 per minute) contractions. A prolonged attack can cause a stroke. In many diseases, chaotic waves are formed that make it difficult for the heart to function normally.
This becomes the cause of defective contractions. The heart cannot work at this rate for a long time. It is depleted. Up to 1% of the adult population suffers from atrial fibrillation. There are cardiac and non-cardiac causes of this pathology. The first group includes congenital defects, high blood pressure, heart failure, surgery, rheumatism, myocardial infarction.
Arrhythmia can be caused by thyrotoxicosis, low levels of potassium in the blood, drug overdose, and inflammatory diseases. In the ICD-10, this pathology is under the code I48. Symptoms are determined by the form of atrial fibrillation. With tachysystolic arrhythmias, a person is worried about shortness of breath, frequent heartbeats and chest pain. This pathology is the most difficult.
This condition is characterized by seizures. Their frequency and duration are different. Often, the condition of patients worsens. Specific signs include Morgagni-Adams-Stokes attacks, fainting, polyuria (increased urine output). Often worried about excessive sweating. When examining the pulse, its deficit is revealed. This is due to the fact that not all pulse waves reach the periphery.
Icb code 10 arrhythmia
Sinus node automatism disorders
a common part
Under physiological conditions, the cells of the sinus node have the most pronounced automatism in comparison with the rest of the heart cells, providing in a state of wakefulness at rest the heart rate (HR) in the range of 60-100 per 1 min.
Fluctuations in the frequency of the sinus rhythm are caused by reflex changes in the activity of the sympathetic and parasympathetic parts of the autonomic nervous system in accordance with the needs of body tissues, as well as local factors - pH, concentration of K + and Ca 2+. P0 2.
With violations of the automatism of the sinus node, the following syndromes develop:
Sinus tachycardia is an increase in heart rate up to 100 beats / min or more while maintaining the correct sinus rhythm, which occurs when the automatism of the sinus node increases.
Sinus bradycardia is characterized by a decrease in heart rate of less than 60 beats / min while maintaining the correct sinus rhythm, which is due to a decrease in the automatism of the sinus node.
Sinus arrhythmia is a sinus rhythm characterized by periods of its increase and decrease, while fluctuations in the values of the P-P interval exceed 160 ms, or 10%.
Sinus tachycardia and bradycardia can be observed under certain conditions in healthy people, as well as caused by various extra- and intracardiac causes. There are three options sinus tachycardia and bradycardia: physiological, pharmacological and pathological.
Sinus arrhythmia is based on changes in the automatism and conductivity of sinus node cells. There are two forms of sinus arrhythmia - respiratory and non-respiratory. Respiratory sinus arrhythmia is caused by physiological reflex fluctuations in the tone of the autonomic nervous system, which is not associated with breathing usually develops in heart disease.
Diagnosis of all violations of the automatism of the sinus node is based on the identification of ECG signs.
With physiological sinus tachycardia and bradycardia, as with respiratory sinus arrhythmia, treatment is not required. In pathological situations, treatment is aimed primarily at the underlying disease; when these conditions are induced by pharmacological agents, the approach is individual.
- Epidemiology of sinus node automatism disorders
The prevalence of sinus tachycardia is high at any age, both in healthy people and in people with various heart and non-cardiac diseases.
Sinus bradycardia is common in athletes and well-trained people, as well as in the elderly and those with a variety of heart and non-heart conditions.
Respiratory sinus arrhythmia is extremely common in children, adolescents and young adults; nonrespiratory sinus arrhythmia is rare.
One for all sinus node automatism disorders.
I49.8 Other specified cardiac arrhythmias
Atrial fibrillation mcb 10
Atrial fibrillation or atrial fibrillation mcb 10 is the most common type of arrhythmia. For example, in the United States, it affects approximately 2.2 million people. They often experience ailments in the form of fatigue, lack of energy, dizziness, shortness of breath and heart palpitations.
What is the danger of atrial fibrillation mcb 10?
Many people live with atrial fibrillation for a long time and do not feel much discomfort. However, they do not even suspect that the instability of the blood system leads to the formation of a blood clot, which, when it enters the brain, causes a stroke.
In addition, the clot can get into other parts of the body (kidneys, lungs, intestines) and provoke various kinds of deviations.
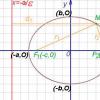
Atrial fibrillation, microbial code 10 (I48) reduces the heart's ability to pump blood by 25%. In addition, it can lead to heart failure and pulse spikes.
How to identify atrial fibrillation?
For diagnostics, specialists use 4 main methods:
- Electrocardiogram.
- Holter monitor.
- A portable monitor that transmits essential and vital data about the patient's condition.
- Echocardiography
These devices help doctors know if you have heart problems, how long they last, and what the cause is.
There is also the so-called persistent form of atrial fibrillation. you need to know what it means.
Atrial fibrillation treatment
Specialists select a treatment option based on the results of the examination, but most often the patient should go through 4 important stages:
- Restore normal heart rate.
- Stabilize and control your heart rate.
- Prevent blood clots.
- Reduce the risk of stroke.
CHAPTER 18 RHYTHM AND HEART CONDUCTIVITY DISORDERS
Supraventricular arrhythmias
Supraventricular extrasystole
SYNONYMS
DEFINITION
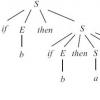
Supraventricular extrasystole is premature in relation to the main rhythm (usually sinus) excitation and contraction of the heart, caused by an electrical impulse that occurs above the level of the branching of the His bundle (i.e. in the atria, AV node, trunk of the His bundle). Recurring supraventricular extrasystoles are called supraventricular extrasystoles.
ICD-10 CODE
EPIDEMIOLOGY
The frequency of detection of supraventricular extrasystole in healthy people during the day ranges from 43 to% and slightly increases with age; frequent supraventricular extrasystole (more than 30 per hour) occurs in only 2-5% of healthy people.
PREVENTION
Prevention is mainly secondary, consists in eliminating non-cardiac causes and treating heart diseases that lead to supraventricular extrasystole.
SCREENING
Active detection of supraventricular extrasystole is carried out in patients with potentially high significance or in the presence of typical complaints using ECG and Holter ECG monitoring during the day.
CLASSIFICATION
There is no predictive classification of supraventricular extrasystole. Supraventricular extrasystole can be classified:
By frequency of occurrence: frequent (more than 30 per hour, i.e. more than 720 per day) and rare (less than 30 per hour);
By the regularity of occurrence: bigeminia (every 2nd impulse is premature), trigeminia (every 3rd), quadrigeminia (every 4th); in general, these forms of supraventricular extrasystole are called allorhythmy;
By the number of extrasystoles arising in a row: paired supraventricular extrasystoles or couplets (two supraventricular extrasystoles in a row), triplets (three supraventricular extrasystoles in a row), while the latter are regarded as episodes of unstable supraventricular tachycardia;
Registration is required to proceed.
What is ventricular premature beats and how dangerous it is
Extrasystole is an untimely contraction of the heart or its chambers separately. In fact, this is one of the types of arrhythmias. Pathology is quite common - from 60 to 70% of people in one way or another are related to it. Moreover, we ourselves provoke the development of extrasystole by abuse of coffee or strong tea, excessive consumption of alcohol, smoking.
Extrasystoles can also occur due to damage to the myocardium under the influence of a number of pathologies (cardiosclerosis, acute infarction, ischemic disease heart, dystrophy, etc.). In addition to pathologies, excessive (overdose) intake can lead to various types of heart rhythm disturbances (for example, allorhythmias like bigeminy) medicines for example, cardiac glycosides may play a poor role.
In the international classification, extrasystole code according to ICD-10 is referred to the section “Other cardiac arrhythmias” (I49).
What is extrasystole
This suggests that extrasystole can occur not only in persons with pathology of the cardiovascular system. Medical studies and observations indicate that up to 75% of the healthy population feel extrasystoles at certain times. Up to 250 such episodes per day are considered normal.
But if a person has some kind of heart or vascular disease, then here already such rhythm disturbances can cause serious conditions for life.
Classification
In order to deal with extrasystoles and the sources of their occurrence, it is necessary to remember that the physiological pacemaker is the sinus-atrial node.
First of all, all extrasystoles are divided according to the etiological factor:
- Functional - occur in absolutely healthy people due to various factors, which have already been mentioned above. Also, such extrasystoles can occur for no apparent reason.
- Atrial (supraventricular, supraventricular extrasystole) - the foci of excitation do not arise in the conducting system of the heart, but in the atria or the atrioventricular septum, then are transmitted to the sinus node and to the ventricles, i.e., supraventricular extrasystole is characterized by ectopic foci of excitation.
Also, ventricular extrasystoles can be right ventricular and left ventricular.
Extrasystole from grade 2 to grade 5 is characterized by persistent hemodynamic disturbances and can cause ventricular fibrillation and death.
By age factor:
- Congenital extrasystoles are combined with heart defects, impaired structure of the walls of the ventricles.
At the place of occurrence of contractions:
- Monotopic - extraordinary impulses originate from one focus.
- Polytopic - impulses originate from different foci.
By the time of occurrence during diastole:
- Early - those extrasystoles that occur at the beginning of diastole, the ECG is recorded simultaneously with the T wave or no later than 0.05 seconds after the end of the previous cycle of heart contraction.
- Average - determined on the ECG in 0.45 - 0.5 seconds after the T wave.
- Late - such extrasystoles are determined at the end or in the middle of diastole, before the subsequent P wave of the normal contraction of the heart.
By the frequency of occurrence:
- Single.
- Paired - ectopic foci generate extrasystoles in a row.
- Multiple - the development of extrasystoles is recorded more than 5 per minute.
- Volley (group) - arising at once several in a row extrasystoles in the amount of more than two.
By the frequency of education:
- Rare - formed up to 5 per minute.
- Average - extrasystoles are recorded before a minute.
- Frequent - registered from 15 per minute or more.
According to the regularity of the occurrence of extraordinary contractions (allorhythmias):
- Bigeminia - occurs after each normal contraction of the heart muscle.
- Trigimenia - extrasystoles are recorded after every second contraction.
- Quadrigimony - after every third contraction of the heart, extraordinary impulses are formed.
According to the forecast for life:
- Extrasystoles that are not life-threatening develop without the presence of heart disease.
- Potentially dangerous extrasystoles are found against the background of acute myocardial infarction, hypertensive crisis.
- Extrasystoles that are life-threatening are difficult to treat, accompany severe heart disease, and often lead to the development of life-threatening conditions.
Causes of occurrence
The causes of functional extrasystoles:
- Stress.
- Smoking.
- Consumption of alcohol, coffee, strong tea in large volumes.
- Overwork.
- Menses.
- Vegeto-vascular dystonia.
- Infectious and inflammatory diseases, which are accompanied by a high body temperature.
- Neuroses.
- Osteochondrosis of the cervical and thoracic spine.
The causes of organic extrasystoles:
- Cardiac ischemia.
- Infectious diseases of the cardiovascular system (myocarditis).
- Chronic cardiovascular failure.
- Congenital and acquired heart defects.
- Thyrotoxicosis and other diseases of the thyroid gland.
- Pericarditis.
- Cardiomyopathy.
- Pulmonary heart.
- Sarcoidosis
- Amyloidosis.
- Heart surgery.
- Hemochromatosis.
- Pathology of the gastrointestinal tract.
- Oncological diseases.
- Allergic reactions.
- Electrolyte metabolism disorders.
The causes of toxic extrasystoles:
- Poisoning by chemicals.
- Intoxication in infectious diseases and pathology endocrine system.
Pathogenesis
As already mentioned above, extrasystoles are extraordinary and premature contractions of the heart.
Normally, the contraction of the heart muscle occurs when nerve impulse passes from the sinus node, located in the left atrium through the atrioventricular node, located between the atria and ventricles along two nerve bundles in both ventricles.
In this case, there should be no deviations in the path of the pulse. Such a process of pulse passage is strictly limited in time.
This is necessary so that the myocardium has time to rest during the filling period, so that then with sufficient force to carry out the release of a portion of blood into the vessels.
If at any of these stages there are any obstacles or failures, there are foci of excitation not in typical places, then in such cases the heart muscle cannot completely relax, the force of contraction weakens, and it almost completely drops out of the blood circulation cycle.
It is through the vagus nerve from the brain that signals about a slowing down of the heart rate are received, and along the sympathetic nerves - signals about the need to increase it. In the case of the prevalence of the vagus nerve in the sinus node, there is a delay in the transmission of the impulse. The accumulation of energy in other parts of the conducting system tries to generate contractions on its own. This is how the development of extrasystole occurs in healthy people.
In addition, extrasystoles can occur reflexively when the diaphragm is raised, which entails irritation of the vagus nerve. Such phenomena are observed after an abundant meal, diseases of the digestive tract.
The sympathetic effect on the heart muscle leads to its overexcitation. Smoking, insomnia, stress, mental overload can lead to this manifestation. According to this mechanism, extrasystole develops in children.
In the case of an existing pathology of the heart, ectopic (pathological) foci are formed outside the conducting system of the heart with increased automatism. This is the development of extrasystoles in cardiosclerosis, heart defects, myocarditis, ischemic heart disease.
Very often, with a disturbed ratio of potassium, magnesium, sodium and calcium ions in the myocardial cells, a negative effect on the cardiac conduction system occurs, which is transformed into the appearance of extrasystoles.
With the development of extrasystoles, extraordinary impulses spread through the myocardium. This causes early, premature heartbeats in diastole. In this case, the volume of blood ejection decreases, which entails changes in the minute volume of blood circulation. The earlier the extrasystole is formed, the smaller the blood volume will be with extrasystolic ejection. Thus, there is a deterioration in coronary blood flow in cardiac pathology.
Clinical manifestations
Very often, extrasystole is generally invisible to patients and its symptoms are absent. But, most of the patients, on the contrary, characterize their feelings as:
Such sensations of cardiac arrest are due to the fact that these feelings depend on a pause that is generated after an extraordinary contraction. This is followed by a heart beat, which is stronger. This is clinically expressed in a shock sensation.
The most common symptoms in patients with extrasystole are:
- Pain in the region of the heart.
- Weakness.
- Dizziness.
- Cough.
- Sweating.
- Feeling of fullness in the chest.
- Pallor.
- Feeling of lack of air.
- Anxiety.
- Fear of death.
- Panic.
- Loss of pulse wave when probing the pulse, which further increases the fear of patients.
- Paresis.
- Fainting.
- Transient speech disorders.
It should be noted that the tolerance of cardiac failures in persons who suffer from vegetative vascular dystonia is much more difficult, which does not correspond to clinical manifestations. But with patients who have a pathology of the cardiovascular system, the opposite is true - they tolerate arrhythmias more easily, since the heart is already "trained" to various types of failures, and morally such patients are more stable.
Extrasystole in children
In children, disruptions can occur at any age, even in the womb. The reasons for the development of such a pathology in childhood are the same factors as in adults.
A special variety includes genetic processes for which ventricular premature beats and tachycardia are the main manifestations. Such an anomaly lies in the fact that against the background of arrhythmogenic dysplasia of the right ventricle, the myocardium does not develop correctly. The danger of such a pathology lies in the fact that sudden death develops quite often.
This type of heart rhythm disturbance often does not manifest itself clinically and is determined by chance in 70%.
As the child grows up, he presents the same complaints as adults, which can increase during puberty.
Since extrasystoles of vegetative origin are more characteristic for children, such extrasystoles are divided into several types:
- Vago-dependent - more inherent in older children in the form of group, allorhythmic manifestations.
- Combined addicts - typical for younger children and schoolchildren.
- Sympathetic addicts - most often occurs during puberty. A distinctive feature of such extrasystoles is their amplification in upright position, predominance during the daytime and decrease during sleep.
In the case of diagnosing a ventricular extrasystole in a child, it is necessary to observe it, since in many cases treatment is not required, and the extrasystole itself passes by the time puberty is completed. But if the number of extrasystoles per day or more, you must immediately start treatment.
Diagnosis and treatment in children are completely identical to those in adults.
Diagnostics
To do this, it is necessary to conduct daily Holter monitoring, in which all possible extrasystoles that occur both day and night are recorded during the day.
Extrasystole on the ECG will have the following symptoms:
- The early occurrence of the QRST complex or P wave, which indicates a shortening of the pre-extrasystolic coupling interval - with atrial extrasystoles, normal and extrasystolic P waves are taken into account, and with ventricular and atrioventricular - QRS complexes.
- Expansion, deformation, high-amplitude extrasystolic QRS complex with ventricular extrasystole.
- The absence of a P wave in front of a ventricular premature beats.
- Full compensatory pause after ventricular extrasystoles.
Also, for the purpose of diagnosis, the following manipulations are used:
- Bicycle ergometry is an ECG study at the time of physical activity. This method is used to clarify the presence of extrasystoles and signs of ischemia.
- Ultrasound of the heart - allows you to determine the activity of the entire heart muscle and heart valves.
- Transoesophageal examination.
- MRI of the heart and blood vessels.
As a rule, the diagnosis of extrasystole does not take much time, therefore, when carrying out all the necessary procedures, it is necessary to start treatment as early as possible.
Extrasystole. Treatment
You should not self-medicate, since any violation of the heart rhythm in combination with improperly selected medications can not easily harm, and lead to very disastrous consequences.
Currently, the following therapeutic measures are used in the treatment of extrasystole:
- In the case of functional extrasystole, treatment is hardly necessary. However, there is still some risk, so it is recommended that you reduce your cigarette consumption, alcohol and coffee consumption.
Surgical intervention eliminates arrhythmia and significantly improves the prognosis and quality of life of patients.
Complications
- Ventricular fibrillation.
- Atrial fibrillation.
- Paroxysmal tachycardia.
- Atrial fibrillation.
- Cardiogenic shock.
- Sudden cardiac death.
As you can see, extrasystole can lead to dangerous complications, therefore timely diagnosis and treatment will help improve both the patient's condition and the prognosis for future life.
Forecast
The most dangerous are those extrasystoles that have arisen against the background of myocardial infarction, cardiomyopathies and myocarditis. Naturally, in such cases, the prognosis will be the most unfavorable, since changes in the structure of the heart during such processes often lead to the development of atrial or ventricular fibrillation.
If there are no pronounced changes in the structure of the myocardium, then the prognosis in such cases is the most favorable.
Ibs extrasystole mkb 10
Functional extrasystole occurs as a result of a vegetative reaction on the human body to one of the following influences:
- Emotional stress.
- Smoking.
- Coffee abuse.
- Alcohol abuse.
- In patients with neurocirculatory dystonia.
- Also, functional extrasystole can occur in healthy individuals for no apparent reason (the so-called idiopathic extrasystole).
Extrasystole of organic origin, as a rule, occurs as a result of morphological changes in the heart muscle in the form of foci of necrosis, dystrophy, cardiosclerosis or metabolic disorders. These organic changes in the myocardium can be observed in the following diseases:
- Ischemic heart disease, acute myocardial infarction.
- Arterial hypertension.
- Myocarditis.
- Postmyocaditic cardiosclerosis.
- Cardiomyopathies.
- Congestive circulatory failure.
- Pericarditis.
- Heart defects (especially with mitral valve prolapse).
- Chronic cor pulmonale.
- Heart disease in amyloidosis, sarcoidosis, hemochromatosis.
- Surgical interventions on the heart.
- "Athlete's Heart".
Extrasystoles of toxic origin occur in the following pathological conditions:
- Feverish conditions.
- Digitalis intoxication.
- Exposure to antiarrhythmic drugs (proarrhythmic side effect).
- Thyrotoxicosis.
- Reception of aminophylline, inhalation of betamimetics.
Ventricular extrasystoles in more than 2/3 of patients develop on the basis of various forms of ischemic heart disease.
The most common causes of the development of ventricular extrasystoles are the following forms of coronary artery disease:
Ventricular rhythm disturbances (the appearance or increased frequency of ventricular extrasystoles, the first paroxysm of ventricular tachycardia or ventricular fibrillation with the development clinical death) can be the earliest clinical manifestation of acute myocardial infarction and always require the exclusion of this diagnosis. Reperfusion arrhythmias (developed after successful thrombolysis) are practically not amenable to treatment and are relatively benign.
The ventricular extrasystoles emanating from the aneurysm of the left ventricle may resemble an infarction QRS in shape (QR in V1, ST elevation and "coronary" T).
Poor prognostic value is the appearance of paired ventricular extrasystoles during the treadmill test with a heart rate of less than 130 beats / min. Especially poor prognosis with a combination of paired ventricular extrasystoles with ischemic ST changes.
The non-coronary nature of ventricular rhythm disturbances can be confidently talked about only after coronary angiogarfia. In this regard, this study is indicated for the majority of patients over 40 years of age, suffering from ventricular extrasystole.
Among the causes of non-coronary ventricular extrasystoles, in addition to the above, there is a group of genetically determined diseases. In these diseases, ventricular premature beats and ventricular tachycardia are the main clinical manifestations. In terms of the degree of malignancy of ventricular arrhythmias, this group of diseases is close to ischemic heart disease. Given the nature of the genetic defect, these diseases are classified as canalopathies. These include:
- Arrhythmogenic left ventricular dysplasia.
- Long QT syndrome.
- Brugada Syndrome.
- Short QT syndrome.
- WPW syndrome.
- Catecholamine-induced trigger polymorphic ventricular tachycardia.
- Pathogenesis of extrasystoles
The morphological substrate of extrasystole (and some other rhythm disturbances) is the electrical inhomogeneity of the heart muscle of various origins.
The main mechanisms for the development of extrasystole:
- Re-entry of the excitation wave (re-entry) in areas of the myocardium or the cardiac conduction system, which differ in the unequal speed of impulse conduction and the development of unidirectional conduction blockade.
- Increased oscillatory (trigger) activity of the cell membranes of individual sections of the atria, AV junction or ventricles.
- The ectopic impulse from the atria spreads from top to bottom along the cardiac conduction system.
- The ectopic impulse arising in the AV junction propagates in two directions: from top to bottom along the conduction system of the ventricles and from bottom to top (retrograde) along the atria.
Features of the pathogenesis of ventricular extrasystole:
- Single monomorphic ventricular extrasystoles can occur as a result of both the formation of a re-entry of the excitation wave (re-entry) and the functioning of the post-depolarization mechanism.
- Repetitive ectopic activity in the form of several successive ventricular extrasystoles is usually due to the re-entry mechanism.
- The source of ventricular extrasystoles in most cases is the branching of the bundle of His and Purkinje fibers. This leads to a significant violation of the process of propagation of the excitation wave along the right and left ventricles, which leads to a significant increase in the total duration of the extrasystolic ventricular QRS complex.
- With ventricular extrasystole, the repolarization sequence also changes.
Clinic and complications
Extrasystole is not always felt by patients. The tolerance of extrasystole varies significantly in different patients and does not always depend on the number of extrasystoles (there may be a complete absence of complaints even in the presence of stable bi- and trigeminia).
In some cases, at the time of the onset of extrasystole, there is a feeling of interruptions in the work of the heart, "somersaults", "overturning of the heart." If it occurs at night, these sensations make you wake up, accompanied by anxiety.
Less often, the patient complains of attacks of rapid irregular heartbeat, which requires the exclusion of the presence of paroxysmal atrial fibrillation.
Sometimes extrasystole is perceived by patients as a “stop” or “freezing” of the heart, which corresponds to a long compensatory pause following the extrasystole. Often, after such a short period of "stopping" of the heart, patients feel a strong push into the chest, caused by the first after extrasystole increased contraction of the ventricles of sinus origin. The increase in shock ejection in the first post-extrasystolic complex is mainly associated with an increase in diastolic ventricular filling during a long compensatory pause (increased preload).
Supraventricular premature beats are not associated with an increased risk sudden death... In relatively rare cases of falling into the "vulnerable window" of the cardiac cycle and the presence of other conditions for the occurrence of re-entry, it can cause supraventricular tachycardia.
The most serious consequence of supraventricular extrasystole is objectively atrial fibrillation, which can develop in patients with supraventricular extrasystole and atrial overload / dilatation. The risk of developing atrial fibrillation can serve as a criterion for the malignancy of supraventricular extrasystole, similar to the risk of sudden death with ventricular extrasystole.
The main complication of ventricular extrasystole, which determines its clinical significance, is sudden death. To assess the risk of sudden death with ventricular extrasystole, a number of special criteria have been developed that determine the required amount of treatment.
Diagnostics
It is possible to suspect the presence of extrasystole when the patient complains about the presence of interruptions in the work of the heart. The main diagnostic method is ECG, however, certain information can be obtained from a physical examination of the patient.
When collecting an anamnesis, it is necessary to clarify the circumstances under which arrhythmia occurs (with emotional or physical stress, at rest, during sleep).
It is important to clarify the duration and frequency of episodes, the presence of signs of hemodynamic disturbances and their nature, the effect of non-drug tests and drug therapy.
Close attention should be paid to the presence in the anamnesis of indications of past diseases that may cause organic defeat heart, as well as their possible undiagnosed manifestations.
During a clinical examination, it is important to make at least an approximate idea of the etiology of extrasystole, since extrasystoles in the absence and presence of organic heart disease require a different approach to treatment.
- Study of the arterial pulse.
In the study of the arterial pulse, prematurely occurring pulse waves of small amplitude correspond to extrasystoles, which indicates insufficient diastolic filling of the ventricles during a short pre-extrasystolic period.
Pulse waves corresponding to the first post-extrasystolic ventricular complex, which occurs after a prolonged compensatory pause, usually have a large amplitude.
In cases of bi- or trigeminia, as well as frequent extrasystole, a pulse deficit is detected; with persistent bigeminy, the pulse can sharply decrease (less than 40 / min), remaining rhythmic and accompanied by symptoms of bradyarrhythmia.
During the extrasystolic contraction, slightly weakened premature I and II (or only one) extrasystolic tones are heard, and after them - loud I and II heart sounds corresponding to the first post-extrasystolic ventricular complex.
Distinctive features of extrasystolic arrhythmia in the presence of organic heart disease and in its absence.
The main electrocardiographic sign of extrasystole is the premature occurrence of the ventricular QRST complex and / or the P wave, that is, a shortening of the adhesion interval.
The adhesion interval is the distance from the preceding extrasystole of the next P – QRST cycle of the main rhythm to the extrasystole.
Compensatory pause is the distance from the extrasystole to the following P – QRST cycle of the main rhythm. Distinguish between incomplete and full compensatory pause:
- Incomplete compensatory pause.
An incomplete compensatory pause is a pause that occurs after an atrial extrasystole or an extrasystole from the AV connection, the duration of which is slightly longer than the usual P – P (R – R) interval of the main rhythm.
Incomplete compensatory pause includes the time required for the ectopic impulse to reach the CA-node and "discharge" it, as well as the time it takes to prepare the next sinus impulse in it.
A full compensatory pause is a pause that occurs after a ventricular extrasystole, and the distance between two sinus complexes P – QRST (pre-extrasystolic and post-extrasystolic) is equal to twice the R – R interval of the main rhythm.
Allorhythmia is the correct alternation of extrasystoles and normal contractions. Depending on the frequency of occurrence of extrasystoles, the following types of allorhythmias are distinguished:
- Bigeminia - after each normal contraction, an extrasystole follows.
- Trigeminia - extrasystoles follow after every two normal contractions.
- Quadrigymenia - extrasystoles follow after every three normal contractions, etc.
- Verse - the occurrence of two extrasystoles in a row.
- Three or more extrasystoles in a row are regarded as a run of supraventricular tachycardia.
The following types of extrasystoles are also distinguished:
- Monotopic extrasystoles are extrasystoles emanating from one ectopic source and, accordingly, having a constant coupling interval and the shape of the ventricular complex.
- Polytopic extrasystoles are extrasystoles emanating from different ectopic foci and differing from each other in the adhesion interval and the shape of the ventricular complex.
- Group (salvo) extrasystole is the presence of three or more extrasystoles in a row on the ECG.
- Premature extraordinary appearance of the P wave and the following QRST complex (the P-P interval is less than the main one).
The constancy of the adhesion interval (from the P wave of the previous normal complex to the P wave of the extrasystole) is a sign of monotopic supraventricular extrasystole. With "early" supraventricular extrasystole, the overlapping of the P wave on the previous T is characteristic, which can complicate the diagnosis.
With extrasystole from the upper atria, the P wave differs little from the norm. With extrasystole from the middle sections, the P wave is deformed, and with extrasystole from the lower sections, it is negative. The need for a more accurate topical diagnosis arises when surgical treatment is necessary, which is preceded by an electrophysiological study.
It should be remembered that sometimes with atrial and atrioventricular extrasystoles, the ventricular QRS complex can acquire a so-called aberrant shape due to the occurrence of a functional blockade of the right bundle branch or its other branches. At the same time, the extrasystolic QRS complex becomes wide (≥0.12 sec), split and deformed, resembling the QRS complex with bundle branch block or ventricular extrasystole.
Blocked atrial extrasystoles are extrasystoles emanating from the atria, which are presented on the ECG only by the P wave, after which there is no extrasystolic ventricular QRST complex.
- Premature extraordinary appearance on the ECG of an unchanged ventricular QRS complex (without the preceding P wave!), Similar in shape to the rest of the QRS complexes of sinus origin. Exceptions are cases of aberration of the QRS complex aberration.
It should be remembered that sometimes with atrial and atrioventricular extrasystoles, the ventricular QRS complex can acquire a so-called aberrant shape due to the occurrence of a functional blockade of the right bundle branch or its other branches. In this case, the extrasystolic QRS complex becomes wide, split and deformed, resembling the QRS complex with blockade of the legs of the bundle of His or ventricular extrasystole.
If the ectopic impulse reaches the ventricles faster than the atria, the negative P wave is located after the extrasystolic P – QRST complex. If the atria and ventricles are excited at the same time, the P wave merges with the QRS complex and is not detected on the ECG.
Stem extrasystoles differ in the occurrence complete blockade retrograde extrasystolic impulse to the atria. Therefore, a narrow extrasystolic QRS complex is recorded on the ECG, after which there is no negative P wave. Instead, a positive P wave is recorded. This is another atrial P wave of sinus origin, which usually falls on the RS – T segment or T wave of the extrasystolic complex.
- Premature appearance on the ECG of an altered ventricular QRS complex, in front of which there is no P wave (except for late ventricular extrasystoles, in front of which there is P. But PQ is shortened compared to sinus cycles).
- Significant expansion (up to 0.12 s and more) and deformation of the extrasystolic QRS complex (in shape it resembles a blockade of the bundle branch, opposite to the side of extrasystoles - the location of the RS – T segment and the T wave of the extrasystole is discordant to the direction of the main tooth of the QRS complex).
- The presence of a complete compensatory pause after a ventricular extrasystole (it complements the extrasystole coupling interval to a satisfactory RR of the main rhythm).
With a ventricular extrasystole, there is usually no "discharge" of the CA node, since the ectopic impulse that occurs in the ventricles, as a rule, cannot retrograde through the AV node and reach the atria and the CA node. In this case, the next sinus impulse freely excites the atria, passes through the AV node, but in most cases cannot cause the next depolarization of the ventricles, since after a ventricular extrasystole they are still in a state of refractoriness.
The usual normal excitation of the ventricles will occur only after the next (second after the ventricular extrasystole) sinus impulse. Therefore, the duration of the compensatory pause with ventricular extrasystole is noticeably longer than the duration of the incomplete compensatory pause. The distance between the normal (sinus origin) ventricular QRS complex preceding the ventricular extrasystole and the first normal sinus QRS complex registered after the extrasystole is equal to twice the R – R interval and indicates a complete compensatory pause.
Occasionally, ventricular extrasystoles can be carried out retrogradely to the atria and, upon reaching the sinus node, discharges it; in these cases, the compensatory pause will be incomplete.
Only sometimes, usually against the background of a relatively rare basic sinus rhythm, a compensatory pause after a ventricular extrasystole may be absent. This is due to the fact that the next (first after extrasystole) sinus impulse reaches the ventricles at the moment when they have already left the state of refractoriness. In this case, the rhythm is not disturbed and the ventricular extrasystoles are called "intercalated".
A compensatory pause may also be absent with ventricular extrasystole against the background of atrial fibrillation.
It should be emphasized that none of the listed ECG signs has 100% sensitivity and specificity.
To assess the prognostic significance of ventricular premature beats, it may be useful to assess the features of ventricular complexes:
- In the presence of organic lesions of the heart, extrasystoles are often low-amplitude, wide, serrated; the ST segment and the T wave can be directed in the same direction as the QRS complex.
- Relatively "favorable" ventricular extrasystoles have an amplitude of more than 2 mV, are not deformed, their duration is about 0.12 seconds, the ST segment and the T wave are directed towards the anti-half-arm QRS.
Of clinical importance is the definition of mono- / polytopicity of the ventricular extrasystole, which is carried out taking into account the constancy of the coupling interval and the shape of the ventricular complex.
Monotopy indicates the presence of a certain arrhythmogenic focus. The location of which can be determined by the shape of the ventricular extrasystole:
- Left ventricular extrasystoles - R dominates in leads V1-V2 and S in V5-V6.
- Extrasystoles from the left ventricular outflow tract: electric axle the heart is located vertically, rS (with their constant ratio) in leads V1-V3 and an abrupt transition to the R-type in leads V4-V6.
- Right ventricular extrasystoles - S dominates in leads V1-V2 and R in leads V5-V6.
- Extrasystoles from the excretory tract of the right ventricle - high R in II III aVF, transition zone in V2-V3.
- Septal extrasystoles - the QRS complex is slightly dilated and resembles WPW syndrome.
- Concordant apical extrasystoles (up both ventricles) - S dominates in leads V1-V6.
- Concordant basal extrasystoles (down both ventricles) - R dominates in leads V1-V6.
With a monomorphic ventricular extrasystole with a non-constant coupling interval, one should think about parasystole - the simultaneous work of the main (sinus, less often atrial fibrillation / flutter) and an additional pacemaker located in the ventricles.
Parasystoles follow each other at different intervals of time, however, the intervals between parasystoles are multiples of the smallest of them. Drain complexes are characteristic, which may be preceded by a P wave.
Holter ECG monitoring is a long-term recording (up to 48 hours) of an ECG. To do this, use a miniature recording device with leads that are attached to the patient's body. When registering indicators, in the course of his daily activity, the patient writes down in a special diary all the symptoms that appear and the nature of the activity. The results are then analyzed.
Holter ECG monitoring is indicated not only in the presence of ventricular extrasystole on the ECG or in history, but also in all patients with organic heart diseases, regardless of the presence of a clinical picture of ventricular arrhythmias and their detection on standard ECGs.
Holter ECG monitoring should be carried out before the start of treatment, and in the future to assess the adequacy of the therapy.
In the presence of extrasystole, Holter monitoring makes it possible to assess the following parameters:
- The frequency of extrasystole.
- The duration of the extrasystole.
- Mono- / polytopicity of ventricular premature beats.
- Dependence of extrasystole on the time of day.
- Dependence of extrasystole on physical activity.
- The connection of extrasystole with changes in the ST segment.
- The connection of extrasystole with the frequency of the rhythm.
Read more: Holter ECG monitoring.
The treadmill test is not used specifically to provoke ventricular arrhythmias (except in cases where the patient himself notes the connection between the occurrence of rhythm disturbances exclusively with exercise). In cases where the patient notes the connection between the occurrence of rhythm disturbances and the load, conditions for resuscitation must be created during the treadmill test.
The connection of the ventricular extrasystole with the load most likely indicates their ischemic etiology.
Idiopathic ventricular premature beats can be suppressed with exercise.
Treatment
Treatment tactics depend on the location and form of extrasystole.
In the absence of clinical manifestations, supraventricular extrasystole does not require treatment.
In case of supraventricular extrasystole that develops against the background of heart disease or non-cardiac disease, therapy of the underlying disease / condition is necessary (treatment of endocrine disorders, correction of electrolyte imbalance, treatment of coronary artery disease or myocarditis, withdrawal of drugs that can cause arrhythmia, refusal of alcohol, smoking, excessive consumption coffee).
- Indications for drug therapy of supraventricular extrasystole
- Subjectively poor tolerance of supraventricular extrasystole.
It is useful to identify situations and times of day in which the sensations of interruption mainly arise, and to time the intake of drugs to this time.
Supraventricular extrasystole in these cases is a harbinger of atrial fibrillation, which is objectively the most serious consequence of supraventricular extrasystole.
The absence of antiarrhythmic treatment (along with etiotropic) increases the risk of fixation of supraventricular extrasystole. Frequent supraventricular extrasystole in such cases is "potentially malignant" in relation to the development of atrial fibrillation.
The choice of an antiarrhythmic is determined by the tropism of its action, side effects and partly by the etiology of supraventricular extrasystole.
It should be remembered that patients with coronary artery disease who have recently had myocardial infarction are not indicated for the administration of class I drugs due to their arrhythmogenic effect on the ventricles.
Treatment is carried out sequentially with the following drugs:
- β-blockers (Anaprilin 30-60 mg / day, atenolol (Atenolol-nikomed, Atenolol) mg / day, bisoprolol (Concor, Bisokard) 5-10 mg / day, metoprolol (Egilok, Vasokardin) mg / day, Nebilet 5- 10 mg / day, Lokrenmg / day - for a long time or until the cause of supraventricular extrasystole is eliminated) or calcium antagonists (Verapamilmg / day, diltiazem (Cardil, Diltiazem-Teva) mg / day, for a long time or until the cause of supraventricular extrasystole is eliminated).
Taking into account the possible side effects, starting treatment with retard drugs should not be due to the need for rapid cancellation in the event of bradycardia and violations of sinoatrial and / or atrioventricular conduction.
Supraventricular extrasystoles, along with paroxysmal supraventricular tachycardias, are rhythm disturbances in which beta-blockers and calcium channel blockers, inactive in other situations, are often ineffective (for example, verapamil (Isoptin, Finoptin)), especially in patients with a tendency to organic heart without serious damage and severe dilatation of the atria.
These groups of drugs are not indicated for patients with vagus-mediated supraventricular extrasystole, which develops against the background of bradycardia, mainly at night. Such patients are shown the appointment of belloid, small doses of Teopek or Corinfar, taking into account their accelerating rhythm of action.
Disopyramide (Ritmilen) mg / day, Quinidine-durulesmg / day, allapininmg / day. ( additional indication to their appointment - a tendency to bradycardia), propafenone (Rithionorm, Propanorm) mg / day., Etatsizinmg / day.
Taking drugs in this group is often accompanied by side effects. Violations of CA- and AV-conduction are possible, as well as an arrhythmogenic effect. In the case of taking quinidine - lengthening of the QT interval, falling contractility and myocardial dystrophy (negative T waves appear in the chest leads). Quinidine should not be prescribed with the simultaneous presence of ventricular premature beats. Caution is also required in the presence of thrombocytopenia.
The appointment of these drugs makes sense in patients with a high prognostic value of supraventricular extrasystole - in the presence of an active inflammatory process in the myocardium, a high frequency of supraventricular extrasystole in patients with organic heart damage, dilatation of the atria, "threatened" by the development of atrial fibrillation.
Class IA or IC drugs should not be used for supraventricular extrasystoles, as in other forms of cardiac arrhythmias, in patients with myocardial infarction, as well as in other types of organic lesions of the heart muscle due to the high risk of proarrhythmic action and the associated deterioration in life prognosis ...
It should be noted that a moderate and no tendency to progression increase in the duration of the PQ interval (up to 0.22-0.24 s), as well as moderate sinus bradycardia (up to 50) are not an indication for discontinuation of therapy, provided that the ECG is monitored regularly.
When treating patients with an undulating course of supraventricular extrasystole, one should strive for a complete cancellation of drugs during periods of remission (excluding cases of severe organic myocardial damage).
Along with the appointment of antiarrhythmics, it is necessary to remember about the treatment of the cause of supraventricular extrasystole, as well as drugs that can improve the subjective tolerance of supraventricular extrasystole: benzodiazepines (Phenazepam 0.5-1 mg, clonazepam 0.5-1 mg), hawthorn tincture, motherwort.
The main principle for choosing therapy for ventricular premature beats is to assess their prognostic significance.
The Lawn-Wolf classification is not exhaustive. Bigger (1984) proposed a prognostic classification that characterizes benign, potentially malignant and malignant ventricular arrhythmias.
The predictive value of ventricular arrhythmias.
A brief description of ventricular extrasystoles can also be presented as follows:
- Benign ventricular extrasystoles - any ventricular extrasystole in patients without heart damage (including myocardial hypertrophy) with a frequency of less than 10 per hour, without fainting and cardiac arrest in history.
- Potentially malignant ventricular extrasystoles - any ventricular extrasystole with a frequency of more than 10 per hour or running ventricular tachycardia in patients with left ventricular dysfunction, without fainting and cardiac arrest in history.
- Malignant ventricular extrasystoles - any ventricular extrasystole with a frequency of more than 10 per hour in patients with severe myocardial pathology (most often with an LV ejection fraction of less than 40%), fainting or cardiac arrest in history; persistent ventricular tachycardia is common.
- Within the groups of potentially malignant and malignant ventricular extrasystoles, the potential risk is also determined by the gradation of ventricular extrasystoles (according to the Laun-Wolf classification).
To improve the accuracy of the prediction, in addition to the fundamental signs, a complex of clinical and instrumental predictors of sudden death is used, each of which, individually, is not decisive:
- Left ventricular ejection fraction. If in IHD the left ventricular ejection fraction decreases to less than 40%, the risk increases by 3 times. With non-coronary ventricular premature beats, the significance of this criterion may decrease).
- The presence of late ventricular potentials is an indicator of areas of slow conduction in the myocardium, detected on a high-resolution ECG. The late potentials of the ventricles reflect the presence of a substrate for ri-entry and, in the presence of ventricular extrasystole, they force us to take its treatment more seriously, although the sensitivity of the method depends on the underlying disease; the ability to control therapy with late ventricular potentials is questionable.
- Increased dispersion of the QT interval.
- Decreased heart rate variability.
- Tactics of therapy for ventricular extrasystole
After assigning a patient to one or another risk category, the question of the choice of treatment can be decided.
As in the treatment of supraventricular extrasystoles, the main method of monitoring the effectiveness of therapy is Holter monitoring: a decrease in the number of ventricular extrasystoles by 75-80% indicates the effectiveness of treatment.
Treatment tactics for patients with different prognostic ventricular extrasystoles:
- In patients with benign ventricular extrasystole, which is subjectively well tolerated by the patient, it is possible to refuse antiarrhythmic therapy.
- Patients with benign ventricular extrasystole, which is subjectively poorly tolerated, as well as patients with potentially malignant arrhythmias of non-ischemic etiology, are preferable to prescribing class I antiarrhythmics.
If they are ineffective - amiodarone or d, l-sotalol. These drugs are prescribed only for non-ischemic etiology of ventricular extrasystole - in postinfarction patients, according to evidence-based studies, the pronounced proarrhythmic effect of flecainide, encainide and etmozine is associated with an increase in the risk of death by 2.5 times! The risk of proarrhythmic action is also increased with active myocarditis.
Of class I antiarrhythmics, the following are effective:
- Propafenone (Propanorm, Ritmonorm) inside pomg / day, or retard forms (propafenone SR 325 and 425 mg, are prescribed twice a day). The therapy is usually well tolerated. Possible combinations with beta-blockers, d, l-sotalol (Sotagexal, Sotalex), verapamil (Isoptin, Finoptin) (under the control of heart rate and AV conduction!), As well as with amiodarone (Cordarone, Amiodarone) at a dose of mg / day.
- Etatsizin inside pomg / day. Therapy begins with the appointment of half doses (0.5 tablets 3-4 times a day) to assess tolerance. Combinations with class III drugs can be arrhythmogenic. The combination with beta-blockers is advisable for myocardial hypertrophy (under the control of heart rate, in a small dose!).
- Etmozin inside pomg / day. Therapy begins with the appointment of smaller doses - 50 mg 4 times a day. Etmozine does not prolong the QT interval and is usually well tolerated.
- Flecainide orally mg / day It is quite effective, slightly reduces myocardial contractility. In some patients, it causes paresthesia.
- Disopyramide orally mg / day It can provoke sinus tachycardia, and therefore combinations with beta-blockers or d, l-sotalol are advisable.
- Allapinin is the drug of choice for bradycardia tendencies. It is prescribed as monotherapy at a dose of 75 mg / day. as monotherapy or 50 mg / day. in combination with beta-blockers or d, l-sotalol (no more than 80 mg / day). This combination is often advisable, since it increases the antiarrhythmic effect, reducing the effect of drugs on heart rate and allows you to prescribe smaller doses with poor tolerance to each drug separately.
- Less commonly used drugs such as Diphenin (with ventricular extrasystole against the background of digitalis intoxication), mexiletine (with intolerance to other antiarrhythmics), aymalin (with WPW syndrome, accompanied by paroxysmal supraventricular tachycardia), Novocainamideren (with rather ineffectiveness or napenarrhythmias) , however, it is extremely inconvenient to use and, with prolonged use, can lead to agranulocytosis).
- It should be noted that in most cases of ventricular premature beats, verapamil and beta-blockers are ineffective. The effectiveness of the first class drugs reaches 70%, however, strict consideration of contraindications is required. The use of quinidine (Kinidin Durules) with ventricular premature beats is undesirable.
It is advisable to quit alcohol, smoking, excessive consumption of coffee.
In patients with benign ventricular extrasystoles, an antiarrhythmic can be prescribed only at the time of day when the manifestations of extrasystole are subjectively felt.
In some cases, you can get by with the use of Valocordin, Corvalol.
In some patients, it is advisable to use psychotropic and / or vegetotropic therapy (Phenazepam, Diazepam, Clonazepam).
d, l-sotalolol (Sotalex, Sotagexal) is used only if amiodarone is intolerant or ineffective. The risk of developing an arrhythmogenic effect (ventricular tachycardia of the "pirouette" type against the background of a higher QT prolongation) significantly increases with the transition to doses above 160 mg / day. and most often appears in the first 3 days.
Amiodarone (Amiodarone, Cordarone) is effective in about 50% of cases. The careful addition of beta-blockers to it, especially in IHD, reduces both arrhythmic and general mortality. Abrupt replacement of beta-blockers with amiodarone is contraindicated! Moreover, the higher the initial heart rate, the higher the effectiveness of the combination.
Only amiodarone simultaneously suppresses ventricular premature beats and improves the prognosis of life in patients who have had myocardial infarction and suffer from other organic lesions of the heart muscle. Treatment is carried out under ECG control - 1 time in 2-3 days. After reaching saturation with amiodarone (an increase in the duration of the Q-T interval, expansion and hardening of the T wave, especially in leads V5 and V6), the drug is prescribed in a maintenance dose (mg 1 r / day for a long time, usually from the 3rd week). The maintenance dose is determined individually. Treatment is carried out under ECG control - once every 4-6 weeks. With an increase in the duration of the Q-T interval by more than 25% of the initial or up to 500 ms, temporary discontinuation of the drug is required and further application it in a reduced dose.
In patients with life-threatening ventricular extrasystoles, the development of thyroid dysfunction is not an indication for the withdrawal of amiodarone. Monitoring of thyroid function with appropriate correction of violations is mandatory.
"Pure" class III antiarrhythmics, as well as class I drugs, are not recommended because of the pronounced proarrhythmic effect. A meta-analysis of 138 randomized placebo-controlled studies on the use of antiarrhythmic therapy in patients with ventricular premature beats after myocardial infarction (total number of patients -) shows that prescribing Class I drugs in this category of patients is always associated with an increased risk of death, especially if these are drugs of class IC. The risk of death is reduced by β-blockers (class II).
Of practical importance is the question of the duration of antiarrhythmic therapy. In patients with malignant ventricular extrasystole, antiarrhythmic therapy should be carried out indefinitely. With less malignant arrhythmias, treatment should be long enough (up to several months), after which an attempt to gradually withdraw the drug is possible.
In some cases - with frequent ventricular extrasystole (dots. Per day) with an arrhythmogenic focus identified during electrophysiological examination and ineffectiveness or in the impossibility of long-term administration of antiarrhythmics in combination with poor tolerance or poor prognosis - radiofrequency ablation is used.
MINISTRY OF HEALTH AND SOCIAL DEVELOPMENT OF THE RUSSIAN FEDERATION
ON THE APPROVAL OF THE STANDARD OF MEDICAL CARE FOR PATIENTS WITH AFILIC ARRHYTHMIA
In accordance with Art. 38 of the Fundamentals of the Legislation of the Russian Federation on the Protection of the Health of Citizens of July 22, 1993 N 5487-1 (Bulletin of the Congress of People's Deputies of the Russian Federation and the Supreme Soviet of the Russian Federation, 1993, N 33, Art. 1318; 2004, N 35, Art. 3607)
I ORDER:
1. To approve the standard of medical care for patients atrial fibrillation(Application).
2. To recommend to the heads of state and municipal medical organizations to use the standard of medical care for patients with atrial fibrillation in the provision of outpatient care in 2007.
3. To recognize as invalid the Order of the Ministry of Health and Social Development of Russia dated November 22, 2004. N 246 "On approval of the standard of medical care for patients atrial fibrillation «.
Deputy Minister V. I. STARODUBOV
Approved by the Order of the Ministry of Health and Social Development of the Russian Federation of October 5, 2006 N 698
STANDARD OF MEDICAL CARE FOR PATIENTS WITH AFILIC ARRHYTHMIA
1. Patient model
Nosological form: atrial fibrillation(atrial fibrillation)
ICD-10 code: I48
Phase: primary diagnosis
glaucoma
Glaucoma is an insidious disease that creeps up unnoticed. Obvious symptoms of glaucoma do not appear immediately, which complicates its effective treatment due to the late treatment of the patient. In this section, we will tell you about the methods of diagnosing glaucoma,
Glaucoma - Type Glaucoma - Causes Glaucoma - Symptoms Glaucoma - Diagnosis Glaucoma - Treatment of Glaucoma - Prevention of Glaucoma - Description Glaucoma is not complex in person, which is due to many factors and specific characteristics of cato injured
The term glaucoma (translated from Greek - the green color of the sea) is found in the works of Hippocrates dated 400 BC. However, modern ideas about glaucoma began to take shape only in the middle of the 9th century. Currently, the term
The famous Russian glaucomatologist professor A.P. Nesterov in his monograph "Glaucoma" rightly notes: ". At present good methods there is no cure for glaucoma. We can only talk about more or less satisfactory methods. TO
There are eye diseases that develop imperceptibly, but ultimately lead to complete loss of vision. Glaucoma is a classic example. Glaucoma is chronic illness eyes, in which intraocular pressure rises. If eye pressure
What is called "glaucoma" today? Glaucoma (from the Greek - the color of sea water, azure) is a serious disease of the organ of vision, named after the greenish color, which acquires a dilated and immobile pupil at the stage of the highest development of painful
Glaukoma (ancient Greek γλαύκωμα - "blue cloudiness of the eye" from γλαυκός - "light blue, blue") - large group eye diseases characterized by a constant or periodic increase intraocular pressure with the subsequent development of typical defects
Glaucoma treatment folk remedies can always be combined with the prescription of the attending physician. Here you will find the most effective traditional methods and treatments for glaucoma from traditional and alternative medicine. Glaucoma is an extensive group of eye diseases, with
Paroxysmal atrial fibrillation mkb 10
MINISTRY OF HEALTH AND SOCIAL DEVELOPMENT OF THE RUSSIAN FEDERATION ORDER 5 October 2006 TREATMENT FROM CALCULATION OF 180 DAYS ——————————— * Anatomical-therapeutic-chemical classification. TREATMENT FROM CALCULATION OF 180 DAYS ———————— ——— * Anatomical-therapeutic-chemical classification. N 698 ON THE APPROVAL OF THE STANDARD OF MEDICAL CARE FOR PATIENTS WITH ATIBLE ARRHYTHMIA In accordance with Art. 38 Fundamentals of the legislation of the Russian Federation on the protection of the health of citizens of July 22, 1993 N 5487-1 Bulletin of the Congress of People's Deputies of the Russian Federation and the Supreme Soviet of the Russian Federation, 1993, N 33, art. 1318; 2004, N 35, Art. 3607 I order 1. To approve the standard of medical care for patients with atrial fibrillation application. Recommend the heads of state and municipal medical organizations to use the standard of medical care for patients with atrial fibrillation in the provision of outpatient care in 2007. To recognize as invalid the order of the Ministry of Health and Social Development of Russia dated November 22, 2004 No.
N 246 "On approval of the standard of medical care for patients with atrial fibrillation." Deputy Minister V.
I. STARODUBOV APPROVED by order of the Ministry of Health and Social Development of the Russian Federation of October 5, 2006 N 698 STANDARD OF MEDICAL CARE FOR PATIENTS WITH ATIBLE ARRHYTHMIA 1. Patient model Category age adults Nosological form atrial fibrillation atrial fibrillation ICD-10 code I48 Phase all primary stages Complications any complications Conditions for providing outpatient care 1.1. Patient model Category age adults Nosological form atrial fibrillation atrial fibrillation ICD-10 code I48 Phase stable permanent form Any stage Complications without complications Conditions for providing outpatient care 2.1. DIAGNOSTICS 2.
** Estimated daily dose. ** Estimated daily dose. *** Equivalent course dose. *** Equivalent course dose. Patient model Category age adults Nosological form atrial fibrillation atrial fibrillation ICD-10 code I48 Phase stable paroxysmal form Any stage Complications without complications Conditions for providing outpatient care 3.1. Example Incorrect ischemic heart disease. Example Incorrect ischemic heart disease. Example Incorrect ischemic heart disease. Example Incorrect ischemic heart disease.
Exertional angina pectoris 2–3 FC. Postinfarction cardiosclerosis. It turns out that these are 3 different diagnoses, and not one. Correctly ischemic heart disease. Correctly ischemic heart disease. Correctly ischemic heart disease. Correctly ischemic heart disease. Exertional angina pectoris 3 FC; postinfarction cardiosclerosis. Ischemic heart disease is a delineated nosological form, represented by a number of possible syndromes. So, angina pectoris can be a manifestation of both atherogenic ischemia and aortic stenosis and, for example, coronaritis.
That is, the abbreviation of ischemic heart disease in the diagnosis requires decoding, since in itself it is not a complete diagnosis. This means that after the abbreviation ischemic heart disease, you cannot put a full stop. A colon is always put, and with a small letter separated by a semicolon, the forms of IHD according to WHO are listed. In addition, it is often possible to find incorrect use of the accepted taxonomy in the disclosure of the diagnosis under discussion.
Each diagnostic formula is self-sufficient and regulated by certain definitions. Well, at least such a hybrid of domestic and foreign approaches as "stable exertional angina" evokes a smile. Acute transmural infarction of the lateral wall of the left ventricle from G. Correctly, depending on the time of writing the epicrisis of coronary artery disease.
Transmural infarction or Q-infarction of the lateral wall of the left ventricle, acute / subacute stage.
Copyright 2015 - All Rights Reserved - http://korol-idea.ru/
- Ectopic systoles
- Extrasystoles
- Extrasystolic arrhythmia
- Premature:
- reductions NOS
- compression
- Brugada syndrome
- Long QT syndrome
- Rhythm disturbance:
- coronary sinus
- ectopic
- nodal
In Russia, the International Classification of Diseases of the 10th revision (ICD-10) has been adopted as a single normative document to take into account the incidence, reasons for the population's visits to medical institutions of all departments, and causes of death.
ICD-10 was introduced into health care practice throughout the Russian Federation in 1999 by order of the Ministry of Health of Russia dated 05/27/97. No. 170
A new revision (ICD-11) is planned by WHO in 2017 2018.
As amended and supplemented by WHO
Processing and translation of changes © mkb-10.com
Gradation of ventricular extrasystole according to ryan and laun, microbial code 10
1 - rare, monotopic ventricular arrhythmia - no more than thirty VES per hour;
2 - frequent, monotopic ventricular arrhythmia - more than thirty VES per hour;
3 - polytopic ZhES;
4а - monomorphic paired LES;
4b - polymorphic paired VES;
5 - ventricular tachycardia, three or more VEBs in a row.
2 - infrequent (from one to nine per hour);
3 - moderately frequent (from ten to thirty per hour);
4 - frequent (from thirty-one to sixty per hour);
5 - very frequent (more than sixty per hour).
B - single, polymorphic;
D - unstable VT (less than 30s);
E - stable VT (more than 30 s).
Lack of structural damage to the heart;
No scar or heart hypertrophy;
Normal ejection fraction of the left ventricle (LVEF) - more than 55%;
Slight or moderate frequency of ventricular premature beats;
Absence of paired ventricular extrasystoles and unstable ventricular tachycardia;
Lack of persistent ventricular tachycardia;
Absence of hemodynamic consequences of arrhythmia.
The presence of a scar or heart hypertrophy;
Moderate decrease in LVEF - from 30 to 55%;
Moderate or significant ventricular premature beats;
The presence of paired ventricular extrasystoles or unstable ventricular tachycardia;
Lack of persistent ventricular tachycardia;
Absence of hemodynamic consequences of arrhythmia or their insignificant presence.
The presence of structural damage to the heart;
The presence of a scar or heart hypertrophy;
Significant decrease in LVEF - less than 30%;
Moderate or significant ventricular premature beats;
Paired ventricular extrasystoles or unstable ventricular tachycardia;
Persistent ventricular tachycardia;
Moderate or severe hemodynamic consequences of arrhythmia.
Ventricular extrasystole encoding according to ICD 10
Extrasystole refers to episodes of premature contraction of the heart due to an impulse that comes from the atria, atrioventricular areas and ventricles. An extraordinary contraction of the heart is usually recorded against the background of a normal sinus rhythm without arrhythmia.
It is important to know that ventricular premature beats in ICD 10 has a code of 149.
The presence of extrasystoles is noted in% of the entire population of the world, which determines the prevalence and a number of varieties of this pathology.
Code 149 in the International Classification of Diseases is defined as other heart rhythm disorders, but the following exceptions are also provided:
- rare myocardial contractions (R1 bradycardia);
- extrasystole due to obstetric and gynecological surgical interventions (abortion O00-O007, ectopic pregnancy O008.8);
- disturbances in the work of the cardiovascular system in a newborn (P29.1).
The extrasystole code according to ICD 10 determines the plan of diagnostic measures and, in accordance with the obtained examination data, a complex of therapeutic methods used all over the world.
Etiological factor in the presence of extrasystoles according to ICD 10
Worldwide nosological data confirm the prevalence of episodic pathologies in the work of the heart in most of the adult population after 30 years, which is typical in the presence of the following organic pathologies:
- heart disease caused by inflammatory processes (myocarditis, pericarditis, bacterial endocarditis);
- the development and progression of coronary heart disease;
- dystrophic changes in the myocardium;
- oxygen starvation of the myocardium due to the processes of acute or chronic decompensation.
In most cases, episodic interruptions in the work of the heart are not associated with damage to the myocardium itself and are only functional in nature, that is, extrasystoles occur due to severe stress, excessive smoking, coffee and alcohol abuse.
Ventricular extrasystole in the international classification of diseases has the following types of clinical course:
- premature contraction of the myocardium, which occurs after each normal one, is called bigeminy;
- trigeminy is the process of a pathological impulse after several normal contractions of the myocardium;
- quadrigeminia is characterized by the appearance of extrasystoles after three contractions of the myocardium.
In the presence of any type of this pathology, a person feels a sinking heart, and then strong tremors in the chest and dizziness.
Icb code 10 arrhythmia
Sinus node automatism disorders
a common part
Under physiological conditions, the cells of the sinus node have the most pronounced automatism in comparison with the rest of the heart cells, providing in a state of wakefulness at rest the heart rate (HR) in the range of 60-100 per 1 min.
Fluctuations in the frequency of the sinus rhythm are caused by reflex changes in the activity of the sympathetic and parasympathetic parts of the autonomic nervous system in accordance with the needs of body tissues, as well as local factors - pH, concentration of K + and Ca 2+. P0 2.
With violations of the automatism of the sinus node, the following syndromes develop:
Sinus tachycardia is an increase in heart rate up to 100 beats / min or more while maintaining the correct sinus rhythm, which occurs when the automatism of the sinus node increases.
Sinus bradycardia is characterized by a decrease in heart rate of less than 60 beats / min while maintaining the correct sinus rhythm, which is due to a decrease in the automatism of the sinus node.
Sinus arrhythmia is a sinus rhythm characterized by periods of its increase and decrease, while fluctuations in the values of the P-P interval exceed 160 ms, or 10%.
Sinus tachycardia and bradycardia can be observed under certain conditions in healthy people, as well as caused by various extra- and intracardiac causes. There are three types of sinus tachycardia and bradycardia: physiological, pharmacological and pathological.
Sinus arrhythmia is based on changes in the automatism and conductivity of sinus node cells. There are two forms of sinus arrhythmia - respiratory and non-respiratory. Respiratory sinus arrhythmia is caused by physiological reflex fluctuations in the tone of the autonomic nervous system, which is not associated with breathing usually develops in heart disease.
Diagnosis of all violations of the automatism of the sinus node is based on the identification of ECG signs.
With physiological sinus tachycardia and bradycardia, as with respiratory sinus arrhythmia, treatment is not required. In pathological situations, treatment is aimed primarily at the underlying disease; when these conditions are induced by pharmacological agents, the approach is individual.
- Epidemiology of sinus node automatism disorders
The prevalence of sinus tachycardia is high at any age, both in healthy people and in people with various heart and non-cardiac diseases.
Sinus bradycardia is common in athletes and well-trained people, as well as in the elderly and those with a variety of heart and non-heart conditions.
Respiratory sinus arrhythmia is extremely common in children, adolescents and young adults; nonrespiratory sinus arrhythmia is rare.
One for all sinus node automatism disorders.
I49.8 Other specified cardiac arrhythmias
Atrial fibrillation mcb 10
Atrial fibrillation or atrial fibrillation mcb 10 is the most common type of arrhythmia. For example, in the United States, it affects approximately 2.2 million people. They often experience ailments in the form of fatigue, lack of energy, dizziness, shortness of breath and heart palpitations.
What is the danger of atrial fibrillation mcb 10?
Many people live with atrial fibrillation for a long time and do not feel much discomfort. However, they do not even suspect that the instability of the blood system leads to the formation of a blood clot, which, when it enters the brain, causes a stroke.
In addition, the clot can get into other parts of the body (kidneys, lungs, intestines) and provoke various kinds of deviations.
Atrial fibrillation, microbial code 10 (I48) reduces the heart's ability to pump blood by 25%. In addition, it can lead to heart failure and pulse spikes.
How to identify atrial fibrillation?
For diagnostics, specialists use 4 main methods:
- Electrocardiogram.
- Holter monitor.
- A portable monitor that transmits essential and vital data about the patient's condition.
- Echocardiography
These devices help doctors know if you have heart problems, how long they last, and what the cause is.
There is also the so-called persistent form of atrial fibrillation. you need to know what it means.
Atrial fibrillation treatment
Specialists select a treatment option based on the results of the examination, but most often the patient should go through 4 important stages:
- Restore normal heart rate.
- Stabilize and control your heart rate.
- Prevent blood clots.
- Reduce the risk of stroke.
CHAPTER 18 RHYTHM AND HEART CONDUCTIVITY DISORDERS
Supraventricular arrhythmias
Supraventricular extrasystole
SYNONYMS
DEFINITION
Supraventricular extrasystole is premature in relation to the main rhythm (usually sinus) excitation and contraction of the heart, caused by an electrical impulse that occurs above the level of the branching of the His bundle (i.e. in the atria, AV node, trunk of the His bundle). Recurring supraventricular extrasystoles are called supraventricular extrasystoles.
ICD-10 CODE
EPIDEMIOLOGY
The frequency of detection of supraventricular extrasystole in healthy people during the day ranges from 43 to% and slightly increases with age; frequent supraventricular extrasystole (more than 30 per hour) occurs in only 2-5% of healthy people.
PREVENTION
Prevention is mainly secondary, consists in eliminating non-cardiac causes and treating heart diseases that lead to supraventricular extrasystole.
SCREENING
Active detection of supraventricular extrasystole is carried out in patients with potentially high significance or in the presence of typical complaints using ECG and Holter ECG monitoring during the day.
CLASSIFICATION
There is no predictive classification of supraventricular extrasystole. Supraventricular extrasystole can be classified:
By frequency of occurrence: frequent (more than 30 per hour, i.e. more than 720 per day) and rare (less than 30 per hour);
By the regularity of occurrence: bigeminia (every 2nd impulse is premature), trigeminia (every 3rd), quadrigeminia (every 4th); in general, these forms of supraventricular extrasystole are called allorhythmy;
By the number of extrasystoles arising in a row: paired supraventricular extrasystoles or couplets (two supraventricular extrasystoles in a row), triplets (three supraventricular extrasystoles in a row), while the latter are regarded as episodes of unstable supraventricular tachycardia;
Registration is required to proceed.
Place of ventricular extrasystole in the ICD system - 10
Ventricular premature beats is a type of cardiac arrhythmia. And it is characterized by an extraordinary contraction of the heart muscle.
Ventricular extrasystole, according to the International Classification of Diseases (ICD - 10), has a code of 149.4. and is included in the list of heart rhythm disorders in the heart disease section.
The nature of the disease
Based on the international classification of diseases of the tenth revision, doctors distinguish several types of extrasystoles, the main ones among which are: atrial and ventricular.
With an extraordinary heartbeat, which was caused by an impulse emanating from the ventricular conduction system, ventricular extrasystole is diagnosed. An attack manifests itself as a feeling of an interruption in the heart rhythm, followed by its fading. The disease is accompanied by weakness and dizziness.
According to ECG data, single extrasystoles can periodically occur even in healthy young people (5%). Daily ECG showed positive indicators in 50% of the studied people.
Thus, it can be noted that the disease is common and can affect even healthy people. The functional nature of the disease can be caused by stress.
The use of energy drinks, alcohol, smoking can also provoke extrasystoles in the heart. This type of ailment is harmless and passes quickly.
More serious consequences for the health of the body are pathological ventricular arrhythmia. It develops against the background of serious illnesses.
Classification
According to the daily monitoring of the electrocardiogram, doctors consider six classes of ventricular extrasystoles.
Extrasystoles belonging to the first class may not manifest themselves in any way. The remaining classes are associated with health risks and the possibility of a dangerous complication: ventricular fibrillation, which can be fatal.
Extrasystoles can vary in frequency, they can be rare, moderate and frequent. On the electrocardiogram, they are diagnosed as single and paired - two impulses in a row. Impulses can occur in both the right and left ventricles.
The origin of extrasystoles can be different: they can come from one source - monotopic, and they can occur in different areas - polytopic.
Disease prognosis
According to prognostic indications, the considered arrhythmias are classified into several types:
- arrhythmias of a benign nature, are not accompanied by heart damage and various kinds of pathologies, their prognosis is positive, and the risk of death is minimal;
- ventricular extrasystoles of a potentially malignant direction occur against the background of heart lesions, the release of blood is reduced by an average of 30%, there is a risk to health;
- ventricular extrasystoles of a pathological nature develop against the background of severe heart disease, the risk of death is very high.
In order to start treatment, a diagnosis of the disease is required in order to find out its causes.
Ventricular premature beats: symptoms and treatment
Ventricular premature beats - the main symptoms:
- Headache
- Weakness
- Dizziness
- Dyspnea
- Fainting
- Lack of air
- Increased fatigue
- Irritability
- Sinking heart
- Heartache
- Abnormal heart rhythm
- Increased sweating
- Pallor of the skin
- Interruptions in the work of the heart
- Panic attacks
- Capriciousness
- Fear of death
- Feeling overwhelmed
Ventricular extrasystole is one of the forms of heart rhythm disturbance, which is characterized by the occurrence of extraordinary or premature ventricular contractions. Both adults and children can suffer from this disease.
To date, a large number of predisposing factors leading to the development of such a pathological process are known, which is why it is customary to divide them into several large groups. The reason may be the course of other ailments, drug overdose or toxic effects on the body.
The symptomatology of the disease is nonspecific and is typical for almost all cardiac ailments. In the clinical picture, there are sensations in the violation of the heart, a feeling of lack of air and shortness of breath, as well as dizziness and pain in the sternum.
Diagnostics is based on the implementation of a physical examination of the patient and a wide range of specific instrumental examinations. Laboratory research is of an auxiliary nature.
Treatment of ventricular extrasystole in the overwhelming majority of situations is conservative, however, if such techniques are ineffective, surgical intervention is indicated.
The international classification of diseases of the tenth revision defines a separate code for such a pathology. Thus, the ICD-10 code is I49.3.
Etiology
Ventricular extrasystole in children and adults is considered one of the most common types of arrhythmias. Among all types of ailment, this form is diagnosed most often, namely in 62% of situations.
The causes of occurrence are so diverse that they are divided into several groups, which also determine the options for the course of the disease.
Cardiological disorders leading to organic extrasystole are represented by:
The functional type of ventricular extrasystole is due to:
- long-term addiction to bad habits, in particular, to smoking cigarettes;
- chronic stress or severe nervous strain;
- drinking a lot of strong coffee;
- neurocirculatory dystonia;
- osteochondrosis of the cervical spine;
- vagotonia.
In addition, the development of this type of arrhythmia is influenced by:
- hormonal imbalance;
- overdose of drugs, in particular diuretics, cardiac glycosides, beta-adrenostimulants, antidepressants and antiarrhythmic substances;
- the course of the VSD is the main reason for the origin of ventricular extrasystole in children;
- chronic oxygen starvation;
- electrolyte disturbances.
It is also worth noting that in about 5% of cases, a similar disease is diagnosed in a perfectly healthy person.
In addition, experts from the field of cardiology note the course of such a form of the disease as idiopathic ventricular extrasystole. In such situations, arrhythmia in a child or an adult develops for no apparent reason, that is, the etiological factor is established only during diagnosis.
Classification
In addition to the fact that the type of pathology will differ in predisposing factors, there are several more classifications of the disease.
Based on the time of formation, the disease happens:
- early - occurs when the atria, which are the upper parts of the heart;
- interpolated - develops at the border of the time interval between the contraction of the atria and ventricles;
- late - observed with a contraction of the ventricles, protruding the lower parts of the heart. Less commonly, it forms in diastole - this is the stage of complete relaxation of the heart.
Based on the number of sources of excitability, there are:
- monotopic extrasystole - while there is one pathological focus, leading to additional cardiac impulses;
- polytopic extrasystole - in such cases, several ectopic sources are found.
Classification of ventricular premature beats by frequency:
- single - characterized by the appearance of 5 extraordinary heartbeats per minute;
- multiple - there are more than 5 extrasystoles per minute;
- steam room - this form differs in that 2 extrasystoles are formed in a row in the interval between normal heartbeats;
- group - these are several extrasystoles going one after another between normal contractions.
According to its orderliness, pathology is divided into:
- disordered - there is no pattern between normal contractions and extrasystoles;
- ordered. In turn, it exists in the form of bigeminy - it is an alternation of normal and extraordinary contractions, trigeminia - an alternation of two normal contractions and extrasystoles, quadrigeminia - 3 normal contractions and extrasystoles alternate.
According to the nature of the course and prognoses, extrasystole in women, men and children can be:
- benign course - differs in that the presence of organic damage to the heart and malfunctioning of the myocardium is not observed. This means that the risk of developing sudden death is minimized;
- potentially malignant course - ventricular extrasystoles are observed due to organic damage to the heart, and the ejection fraction decreases by 30%, while the likelihood of sudden cardiac death increases in comparison with the previous form;
- malignant course - severe organic damage to the heart is formed, which is a dangerously high chance of sudden cardiac death.
A separate type is intercalary ventricular extrasystole - in such cases, the formation of a compensatory pause does not occur.
Symptoms
A rare arrhythmia in a healthy person is completely asymptomatic, but in some cases there is a sensation of heart sinking, "interruptions" in functioning, or a kind of "jolt". Such clinical manifestations are the result of increased post-extrasystolic contraction.
The main symptoms of ventricular premature beats are:
- severe dizziness;
- pallor of the skin;
- pain in the heart;
- increased fatigue and irritability;
- periodic headache;
- weakness and weakness;
- feeling short of breath;
- fainting conditions;
- shortness of breath;
- unreasonable panic and fear of dying;
- violation of heart rate;
- increased sweating;
- capriciousness - such a sign is characteristic of children.
It is worth noting that the course of ventricular extrasystole against the background of organic heart disease can go unnoticed for a long period of time.
Diagnostics
The basis of diagnostic measures is formed by instrumental procedures, which are necessarily supplemented by laboratory studies. Nevertheless, the first stage of diagnosis will be the independent implementation of the following manipulations by the cardiologist:
- the study of the history of the disease - will indicate the main pathological etiological factor;
- collection and analysis of a life history - this can help in finding the causes of idiopathic ventricular premature beats;
- a thorough examination of the patient, namely palpation and percussion of the chest, determining the heart rate by listening to a person with a phonendoscope, as well as probing the pulse;
- a detailed survey of the patient - to draw up a complete symptomatic picture and determine a rare or frequent ventricular extrasystole.
Laboratory research is limited to the behavior of only general clinical analysis and blood biochemistry.
Instrumental diagnosis of extrasystole of the heart implies the implementation of:
- ECG and EchoCG;
- daily monitoring of electrocardiography;
- stress tests, in particular bicycle ergometry;
- chest x-ray and MRI;
- rhythmocardiography;
- polycardiography;
- sphygmography;
- CHPECG and CT.
In addition, it is necessary to consult a therapist, pediatrician (if the patient is a child) and obstetrician-gynecologist (in cases where extrasystole is formed during pregnancy).
Treatment
In situations where the development of a similar disease has occurred without the course of cardiac pathologies or VSD, specific therapy for patients is not provided. To relieve symptoms, it is enough to observe clinical guidelines attending physician, including:
- normalization of the daily routine - people are shown to rest more;
- adherence to a correct and balanced diet;
- avoidance of stressful situations;
- performing breathing exercises;
- spending a lot of time outdoors.
In other cases, first of all, it is necessary to cure the underlying disease, which makes the therapy individual. However, there are several general aspects, namely the treatment of ventricular extrasystole with the help of such medications:
- antiarrhythmic substances;
- omega-3 preparations;
- antihypertensive drugs;
- anticholinergics;
- tranquilizers;
- beta-blockers;
- phytopreparations - in cases of the course of the disease in a pregnant woman;
- antihistamines;
- vitamins and restorative medicines;
- drugs aimed at eliminating the clinical manifestations of such heart disease.
Surgical intervention in the course of ventricular or ventricular extrasystole is carried out only according to indications, among which is the ineffectiveness of conservative methods of treatment or the malignant nature of the pathology. In such cases, they resort to performing:
- radiofrequency catheter ablation of ectopic foci;
- open intervention, implying excision of damaged areas of the heart.
There are no other ways how to treat such a disease, in particular folk remedies.
Possible complications
Ventricular extrasystole is fraught with the development of:
- sudden onset of cardiac death;
- heart failure;
- changes in the structure of the ventricles;
- aggravation of the course of the underlying ailment;
- ventricular fibrillation.
Prevention and prognosis
You can avoid the occurrence of extraordinary ventricular contractions by observing the following preventive recommendations:
- complete rejection of addictions;
- limiting the consumption of strong coffee;
- avoiding physical and emotional overwork;
- rationalization of the mode of work and rest, namely, full-fledged long sleep;
- application drugs only under the supervision of the attending physician;
- complete and vitamin-enriched nutrition;
- early diagnosis and elimination of pathologies leading to ventricular extrasystole;
- regular full preventive examination by clinicians.
The outcome of the disease depends on the variant of its course. For example, functional extrasystole has a favorable prognosis, and pathology that develops against the background of organic lesions of the heart has a high risk of sudden cardiac death and other complications. Nevertheless, the mortality rate is quite low.
If you think that you have ventricular extrasystole and symptoms characteristic of this disease, then a cardiologist can help you.
We also suggest using our online disease diagnosis service, which, based on the entered symptoms, selects probable diseases.
Extrasystolic arrhythmia mkb 10
What is the danger of ventricular extrasystole and its treatment
- Causes
- B.Lown classification - M.Wolf
- Diagnostics
- Extrasystole in pregnant women
- Treatment
- Surgical treatments
- Modern forecasting
In the group of arrhythmias of the extrasystolic type, ventricular extrasystole occupies one of the most important places in terms of importance for prognosis and treatment. An extraordinary contraction of the heart muscle occurs on a signal from the ectopic (additional) focus of excitation.
According to the International Classification of Diseases (ICD-10), this pathology is coded I 49.4.
The prevalence of extrasystoles among sick and healthy people was established with long-term Holter monitoring of the heart rhythm. Extrasystoles from the ventricles are detected in 40–75% of cases of examined adults.
Where is the source of extrasystoles located
Ventricular extrasystoles occur in the wall of the left or right ventricle, more often directly in the fibers of the conducting system. If extrasystole occurs at the end of the ventricular relaxation phase, then it coincides in time with the next atrial contraction. The atrium is not completely emptied, a backward wave goes through the vena cava.
Usually, ventricular extrasystoles cause contraction only of the ventricles themselves and do not transmit impulses in the opposite direction to the atria. "Supraventricular" is called extrasystoles from ectopic foci located above the level of the ventricles, in the atria, atrioventricular node. They can be combined with ventricular. There are no pancreatic extrasystoles.
The correct rhythm from the sinus node is maintained and disturbed only by compensatory pauses after extraordinary beats.
Causes
The reasons for ventricular premature beats appear with heart disease:
- inflammatory nature (myocarditis, endocarditis, intoxication);
- myocardial ischemia (foci of cardiosclerosis, acute infarction);
- metabolic-dystrophic changes in the muscle and the conducting system (violation of the ratio of potassium-sodium electrolytes in myocytes and intercellular space);
- a sharp depletion of the energy supply of cells caused by malnutrition, lack of oxygen in acute and chronic heart failure, decompensated defects.
Ventricular extrasystoles can occur in people with a healthy cardiovascular system due to:
- irritation of the vagus nerve (with overeating, insomnia, mental work);
- increased tone of the sympathetic nerve (smoking, physical work, stress, hard work).
Types of ventricular extrasystoles
The classification of ventricular extrasystole takes into account the frequency of pathological impulses, the localization of ectopic foci.
Extrasystoles from the ventricles, as well as from other foci, can be single (one nanormal contractions) or group (3-5 ectopic contractions between normal).
The constant repetition of extraordinary single contractions for each normal one is called bigeminy, for two - trigeminy. Extrasystolic arrhythmia of the type of bigeminy or trigeminia refers to allorhythmias (irregular, but persistent rhythm disturbance).
Depending on the number of identified foci, extrasystoles are distinguished:
- monotopic (from one focus);
- polytopic (more than one).
By location in the ventricles, the most frequent are left ventricular extraordinary contractions. Right ventricular extrasystole is less common, possibly due to the anatomical features of the vascular bed, rare ischemic lesions of the right heart.
B.Lown classification - M.Wolf
Not all specialists use the existing classification of ventricular extrasystole according to Lown and Wolf. She offers five degrees of extrasystole in myocardial infarction according to the risk of the risk of developing fibrillation:
- degree 1 - monomorphic extraordinary contractions are recorded (no more than 30 per hour of observation);
- degree 2 - more frequent, from one focus (over 30 per hour);
- degree 3 - polytopic extrasystole;
- degree 4 - subdivided depending on the ECG pattern of the rhythm ("a" - paired and "b" - salvo);
- degree 5 - the most dangerous in the prognostic sense type "R to T" is registered, which means that the extrasystole "climbed" on the previous normal contraction and is capable of disrupting the rhythm.
In addition, a "zero" degree is allocated for patients without extrasystoles.
M. Ryan's suggestions for gradation (classes) supplemented the B.Lown - M.Wolf classification for patients without myocardial infarction.
In them, “gradation 1”, “gradation 2” and “gradation 3” completely coincide with the Launian interpretation.
- "Gradation 4" - is considered in the form of paired extrasystoles in monomorphic and polymorphic variants;
- Ventricular tachycardia is included in "grade 5".
How extrasystole is felt by patients
Symptoms of ventricular premature beats do not differ from any extraordinary contractions of the heart. Patients complain of a feeling of "sinking" of the heart, stopping, and then a strong impulse in the form of a blow. At the same time, some feel:
Rarely, extrasystole is accompanied by a coughing movement.
A more colorful description consists in "turning" the heart, "pushing into the chest."
Diagnostics
The use of electrocardiography (ECG) in diagnostics is of great importance, since the technique is not difficult to master, the equipment is used for removal at home, on an ambulance.
Taking an ECG takes 3-4 minutes (together with the application of electrodes). On the current record during this time it is not always possible to "catch" extrasystoles, to give them a characteristic.
Exercise tests are used to examine healthy individuals, an ECG is done twice: first at rest, then after twenty squats. For some professions with high overloads, it is important to identify possible violations.
Ultrasound of the heart and blood vessels allows you to exclude various cardiac causes.
It is important for the doctor to establish the cause of the arrhythmia, therefore, the following are prescribed:
- general blood analysis;
- C-reactive protein;
- globulin level;
- blood for thyroid-stimulating hormones;
- electrolytes (potassium);
- heart enzymes (creatine phosphokinase, lactate dehydrogenase).
Idiopathic (unclear in origin) extrasystole remains if the patient does not have any diseases and provoking factors during the examination.
Features of extrasystole in children
Arrhythmia is detected in newborn babies at the first listening. Extrasystoles from the ventricles can have congenital roots (various malformations).
Acquired ventricular premature beats in childhood and adolescence are associated with rheumatic heart disease (after angina), infections complicated by myocarditis.
Extrasystole in older children is accompanied by disorders in the endocrine system, occurs when:
- overdose of drugs;
- in the form of a reflex from a distended gallbladder with its dyskinesia;
- flu intoxication, scarlet fever, measles;
- food poisoning;
- nervous and physical overload.
In 70% of cases, ventricular extrasystole is detected in a child by chance during a routine examination.
Growing up children catch heart rhythm interruptions and extraordinary tremors, complain about stitching pains to the left of the sternum. In adolescents, there is a combination with vegetative dystonia.
Depending on the predominance of vagal or sympathetic nervous regulation, extrasystoles are observed:
Diagnosis in childhood goes through the same stages as in adults. In treatment, more attention is paid to the daily regimen, a balanced diet, and light sedatives.
Extrasystole in pregnant women
Pregnancy in a healthy woman can cause rare ventricular premature beats. This is more typical for the second trimester, due to an imbalance of electrolytes in the blood, a high standing of the diaphragm.
The presence of diseases of the stomach, esophagus, gallbladder in a woman causes reflex extrasystole.
For any complaints of a pregnant woman about a feeling of interruptions in rhythm, it is necessary to conduct an examination. After all, the pregnancy process significantly increases the load on the heart and contributes to the manifestation of the latent symptoms of myocarditis.
Treatment
Treatment of ventricular premature beats includes all the requirements of a healthy diet and regimen.
- quit smoking, drinking alcohol, strong coffee;
- be sure to eat foods containing potassium in the diet (jacket potatoes, raisins, dried apricots, apples);
- you should refrain from lifting weights, strength training;
- if sleep suffers, mild sedatives should be taken.
Drug therapy is connected:
- with poor tolerance of arrhythmia by the patient;
- increased frequency of idiopathic (unclear) group extrasystole;
- high risk of developing fibrillation.
In the arsenal of the doctor there are antiarrhythmic drugs of various strengths and directions. The purpose must be consistent with the root cause.
The drugs are very carefully used in case of a previous heart attack, the presence of ischemia and symptoms of heart failure, various blockages of the conducting system.
Against the background of treatment, the effectiveness is judged by repeated Holter monitoring: a decrease in the number of extrasystoles by 70 - 90% is considered a positive result.
Surgical treatments
Lack of effect from conservative therapy and the presence of a risk of fibrillation is an indication for radiofrequency ablation (RF). The procedure is carried out in a cardiac surgery hospital under sterile conditions in the operating unit. Under local anesthesia, a catheter with a source of radio frequency radiation is inserted into the patient's subclavian vein. Cauterization of the ectopic focus with radio waves is performed.
With a good "hit" in the cause of the impulses, the procedure provides an efficiency in the range of 70 - 90%.
Using folk remedies
Folk remedies are used for extrasystoles of a functional nature. If there are organic changes in the heart, you should consult your doctor. Some methods may be contraindicated.
Several popular recipes
At home, it is convenient and easy to brew medicinal herbs and plants in a thermos.
- In this way, decoctions are prepared from valerian root, calendula, cornflower. It should be brewed at the rate of 1 tablespoon of dry plant materials for 2 cups of water. Keep in a thermos for at least three hours. Can be brewed overnight. After straining, drink ¼ glass 15 minutes before meals.
- Horsetail is brewed in the proportion of a tablespoon to 3 glasses of water. Drink a spoonful up to six times a day. Helps with heart failure.
- You can buy alcoholic hawthorn tincture at the pharmacy. Drink 10 drops three times a day. To cook it yourself, you need 10 g of dry fruit for every 100 ml of vodka. Insist for at least 10 days.
- Honey recipe: mix equal volumes of squeezed radish juice and honey. Take a tablespoon three times a day.
All decoctions are stored in the refrigerator.
Modern forecasting
Over the 40 years of its existence, the above classifications have helped to train doctors, to enter the necessary information into programs of automatic ECG decoding... This is important for quickly obtaining a research result in the absence of a specialist nearby, in the case of remote (in rural areas) examination of a patient.
To predict dangerous situations, it is important for a doctor to know:
- if a person has ventricular extrasystoles, but there is no confirmed heart disease, their frequency and localization does not matter for the prognosis;
- the risk to life is increased for patients with heart defects, organic changes in hypertension, myocardial ischemia only in case of contraction of the strength of the heart muscle (increasing heart failure);
- The risk for patients after myocardial infarction should be considered high if there are more than 10 ventricular extrasystoles per hour of observation and a reduced blood ejection volume (widespread heart attack, heart failure) is detected.
The patient needs to see a doctor and be examined for any unclear heart rhythm interruptions.
Classification of cardiac arrhythmias in ICD-10
All cardiologists know in which sections you can find heart rhythm disturbances in ICD-10. This pathology is common among people of different ages. With arrhythmias, the heart rate and coordination are impaired. Some conditions are potentially life threatening and can be fatal.
Arrhythmia is a pathological condition in which the regularity of myocardial contractions and heart rate are disturbed. The conductive function of the organ decreases. Often, this pathology remains unnoticed for a person. There are 3 large groups of arrhythmias:
- caused by impaired impulse formation (sick sinus syndrome, extrasystole, atrial and ventricular tachycardia, flutter and flicker);
- associated with the difficulty of conducting the impulse (blockade, syndrome of premature excitation of the ventricles of the heart);
- combined.
They all have their own distinctive features. Common clinical manifestations include a feeling of heart failure, difficulty breathing, fainting, weakness, and dizziness. Often there is an attack of angina pectoris. Discomfort in the chest is possible.
The group of arrhythmias includes ventricular premature beats. It is characterized by premature excitation of the myocardium. The ICD-10 code for this pathology is I49.3. The elderly are at risk. With age, the incidence rate increases. Single extrasystoles are often detected in young people. They pose no danger and are not pathological.
In the development of ventricular extrasystole, the following factors play a leading role:
- angina pectoris;
- acute myocardial infarction;
- cardiosclerosis;
- myocarditis;
- inflammation of the pericardium;
- vagotonia;
- osteochondrosis of the cervical spine;
- hypertonic disease;
- pulmonary heart;
- mitral valve prolapse;
- cardiomyopathy;
- overdose of medicines.
The classification of extrasystoles is known to all cardiologists. Extrasystoles are early, late and interpolated. By frequency, single, paired, group and multiple are distinguished. This disease is manifested by a feeling of palpitations, weakness, dizziness, a sense of fear and anxiety.
Atrial fibrillation occupies an important place among diseases characterized by rhythm disturbances. Otherwise, it is called atrial fibrillation. This pathology is characterized by chaotic and frequent (up to 600 per minute) contractions. A prolonged attack can cause a stroke. In many diseases, chaotic waves are formed that make it difficult for the heart to function normally.
This becomes the cause of defective contractions. The heart cannot work at this rate for a long time. It is depleted. Up to 1% of the adult population suffers from atrial fibrillation. There are cardiac and non-cardiac causes of this pathology. The first group includes congenital defects, high blood pressure, heart failure, surgery, rheumatism, myocardial infarction.
Arrhythmia can be caused by thyrotoxicosis, low levels of potassium in the blood, drug overdose, and inflammatory diseases. In the ICD-10, this pathology is under the code I48. Symptoms are determined by the form of atrial fibrillation. With tachysystolic arrhythmias, a person is worried about shortness of breath, frequent heartbeats and chest pain. This pathology is the most difficult.
This condition is characterized by seizures. Their frequency and duration are different. Often, the condition of patients worsens. Specific signs include Morgagni-Adams-Stokes attacks, fainting, polyuria (increased urine output). Often worried about excessive sweating. When examining the pulse, its deficit is revealed. This is due to the fact that not all pulse waves reach the periphery.
Extrasystole - causes and treatment of the disease
Extrasystole of the heart is a type of heart rhythm disorder based on an abnormal contraction of the whole heart or its individual parts. Contractions are extraordinary under the influence of any impulse or excitation of the myocardium. This is the most common type of arrhythmia affecting both adults and children, and it is extremely difficult to get rid of it. Drug treatment and treatment with folk remedies are practiced. Gastric extrasystole is registered in ICD 10 (code 149.3).
Ventricular extrasystole is a fairly common disease. It affects quite healthy people.
Causes of extrasystole
- overwork;
- binge eating;
- the presence of bad habits (alcohol, drugs and smoking);
- drinking large amounts of caffeine;
- stressful situations;
- heart disease;
- toxic poisoning;
- osteochondrosis;
- diseases internal organs(stomach).
Gastric extrasystole is a consequence of various myocardial lesions (coronary artery disease, cardiosclerosis, myocardial infarction, chronic insufficiency blood circulation, heart defects). Its development is possible with febrile conditions and with VSD. And it is also a side effect of certain medications (Euphelin, Caffeine, glucocorticosteroids and some antidepressants) and can be observed with improper treatment with folk remedies.
The reason for the development of extrasystole in people actively involved in sports is myocardial dystrophy associated with intense physical exertion. In some cases, this disease is closely related to a change in the amount of sodium, potassium, magnesium and calcium ions in the myocardium itself, which adversely affects its work and does not allow getting rid of seizures.
Often gastric extrasystole can occur during or immediately after a meal, especially in patients with VSD. This is due to the peculiarities of the heart during such periods: the heart rate decreases, therefore, extraordinary contractions occur (before or after the next). It is not necessary to treat such extrasystoles, since they are functional in nature. In order to get rid of extraordinary contractions of the heart after eating, you cannot take a horizontal position immediately after taking food. Better to sit in a comfortable chair and relax.
Classification
Depending on the place of origin of the impulse and its cause, the following types of extrasystole are distinguished:
- ventricular premature beats;
- atrioventricular premature beats;
- supraventricular extrasystole (supraventricular extrasystole);
- atrial premature beats;
- atrioventricular extrasystole;
- stem and sinus extrasystoles.
A combination of several types of impulse is possible (for example, supraventricular extrasystole is combined with stem, gastric extrasystole occurs along with sinus), which is characterized as parasystole.
Gastric extrasystole is the most common type of disturbance in the work of the cardiac system, characterized by the appearance of an additional contraction (extrasystole) of the heart muscle before its normal contraction. Extrasystole can be single or double. If three or more extrasystoles appear in a row, then we are already talking about tachycardia (ICD code - 10: 147.x).
Supraventricular extrasystole differs from the ventricular localization of the source of arrhythmia. Supraventricular extrasystole (supraventricular extrasystole) is characterized by the occurrence of premature impulses in the upper parts of the heart (atria or in the septum between the atria and ventricles).
There is also the concept of bigeminy, when an extrasystole occurs after a normal contraction of the heart muscle. It is believed that the development of bigeminy is provoked by disorders in the work of the autonomic nervous system, that is, the VSD can become the trigger for the development of bigeminy.
Also, there are 5 degrees of extrasystole, which are due to a certain number of impulses per hour:
- the first degree is characterized by no more than 30 impulses per hour;
- for the second - more than 30;
- the third degree is represented by polymorphic extrasystoles.
- the fourth degree is when 2 or more types of impulse arise in turn;
- the fifth degree is characterized by the presence of 3 or more extrasystoles one after another.
In most cases, the symptoms of this disease are invisible to the patient. The surest signs are sensations of a sharp blow to the heart, cardiac arrest, chest fading. Supraventricular extrasystole can manifest itself as an VSD or neurosis and is accompanied by a feeling of fear, profuse sweating, anxiety, lack of air.
Diagnostics and treatment
Before treating any extrasystole, it is important to correctly establish its appearance. The most revealing method is electrocardiography (ECG), especially with ventricular impulses. An ECG allows you to identify the presence of extrasystole and its location. However, the resting ECG does not always reveal the disease. Diagnosis becomes more difficult in patients with VSD.
If this method has not shown the proper results, ECG monitoring is used, during which the patient is put on a special device that monitors the work of the heart during the day and records the progress of the study. This ECG diagnosis allows you to identify the disease, even in the absence of complaints from the patient. A special portable device attached to the patient's body records the ECG readings for 24 or 48 hours. In parallel, the patient's actions are recorded at the time of the ECG diagnosis. Then the data of daily activity and ECG are compared, which allows you to identify the disease and treat it correctly.
In some literature, the norms for the occurrence of extrasystoles are indicated: for a healthy person, the norm is ventricular and ventricular extrasystoles per day, identified on the ECG. If, after ECG studies, no deviations were found, the specialist may prescribe special additional studies with exercise (treadmill test)
In order to properly treat this disease, it is necessary to take into account the type and degree of extrasystole, as well as its location. Single impulses do not require specific treatment, they do not pose any threat to human health and life, only if they are caused by a serious heart disease.
Treatment features
To cure a disease caused by neurological disorders, sedatives (relanium) are prescribed and herbal preparations(valerian, motherwort, mint).
If the patient has a history of serious heart disease, the extrasystole is supraventricular in nature, and the frequency of impulses per day exceeds 200, individually selected drug therapy is required. To treat extrasystaly in such cases, drugs such as Propanorm, Cordaron, Lidocaine, Diltiazem, Panangin, as well as beta-blockers (Atenolol, Metoprolol) are used. Sometimes such means can get rid of the manifestations of VSD.
A drug such as Propafenone, which is an antiarrhythmic drug, is currently the most effective and allows you to treat even an advanced stage of the disease. It is quite well tolerated and absolutely safe for health. That is why it was ranked as a first-line drug.
A rather effective method to cure extrasystole forever is to cauterize its focus. This is a fairly simple surgical intervention that has practically no consequences, but it cannot be performed in children, there is an age limit.
If gastric extrasystole is present in the later stages, then it is recommended to treat it with the method of radiofrequency ablation. This is a method of surgical intervention, with the help of which the focus of arrhythmia is destroyed under the influence of physical factors... The procedure is easily tolerated for the patient, the risk of complications is minimized. In most cases, gastric extrasystole is irreversible.
Treatment of children
In most cases, there is no need to treat the disease in children. Many experts say that in children, the disease goes away without treatment. If desired, you can stop severe attacks with safe folk remedies. However, it is recommended to undergo an examination to determine the degree of neglect of the disease.
Extrasystole in children can be congenital or acquired (after nervous shocks). The presence of mitral valve prolapse and the occurrence of impulses in children are closely related. As a rule, ventricular extrasystole (or gastric extrasystole) does not need special treatment, but it is necessary to undergo an examination at least once a year. At risk are children suffering from VSD.
It is important to restrict children from provoking factors that contribute to the development of this disease (healthy lifestyle and sleep, absence of stressful situations). For children, it is recommended to eat foods enriched with elements such as potassium and magnesium, for example, dried fruits.
In the treatment of extrasystole and VSD in children, drugs such as Noofen, Aminalon, Phenibut, Mildronat, Panangin, Asparkam and others are used. Treatment with folk remedies is effective.
Fight with folk remedies
You can get rid of severe attacks with folk remedies. At home, you can use the same means as in the treatment of VSD: soothing infusions and decoctions of herbs.
- Valerian. If the attack is classified according to the emotional type, then a pharmacy infusion of valerian root will help get rid of anxiety. It is enough to take 10 - 15 drops of the infusion one time, preferably after a meal.
- Cornflower infusion will save during an attack. It is recommended to drink the infusion 10 minutes before meals, 3 times a day (only on the day when the attack occurs).
- Infusion of calendula flowers will help get rid of frequent attacks.
Treatment by such folk methods should only be practiced after consulting a doctor. If you use them incorrectly, then you can simply not get rid of the disease, as well as aggravate it.
Prophylaxis
To get rid of the risk of developing extrasystole, timely examination and treatment of heart diseases is necessary. Compliance with a diet high in potassium and magnesium salts prevents the development of an exacerbation. It is also necessary to give up bad habits (smoking, alcohol, coffee). In some cases, treatment with folk remedies is effective.
Effects
If the impulses are single and not burdened with anamnesis, then the consequences for the body can be avoided. When the patient already has heart disease, in the past there was a myocardial infarction, frequent extrasystoles can cause tachycardia, atrial fibrillation and atrial and ventricular fibrillation.
The most dangerous is considered gastric extrasystole, since ventricular impulses can lead to a sudden death, through the development of their flicker. Gastric extrasystole needs careful treatment, since it is very difficult to get rid of it.
Heart rhythm disorder - ICD code 10
Atrial fibrillation (MA) is a disease that has its own code in the International Classification of Diseases (ICD-10 code - І48), although there its name sounds like atrial fibrillation (AF). What is the essence of this disease? The heartbeat of a person is called atrial fibrillation if it is of a chaotic nature. So, atrial muscle fibers, contracting and being excited irregularly, along with the same chaotic contractions and excitations of the myocardium, provoke cardiac arrhythmias. Let's take a closer look at this process.
Ordinary (correct) heart impulses, which set the heart rate, form the sinus node - special cells in the heart wall that generate impulses of an electrical nature. These impulses are carried by specialized fibers that make up the cardiac conduction system. Such a system, in turn, consists of many cells connected to the muscle fibers of the heart. Thus, the generated electrical impulse is transmitted to the heart muscle and causes the heart to contract.
If malfunctions occur in any part of this structure, then the functioning of the entire cardiovascular system of the body suffers - the well-adjusted work of the heart is interrupted, the wrong sequence of contractions of the ventricles, atria, etc.
 Normal condition and atrial fibrillation
Normal condition and atrial fibrillation MA reasons
The main reasons that can cause MA in humans can be combined into several groups:
- the presence of rheumatic heart defects;
- coronary artery disease and neoplastic heart disease;
- the appearance of cardiomyopathies, microcardiodystrophy;
- combinations of various etiological indicators.
But it is also necessary to know that there are factors that contribute to the development of AF and maintain atrial fibrillation. These include:
- chronic arterial hypertension;
- being overweight;
- chronic renal failure;
- the presence of HIV in the blood.
The older a person is, the higher their risk of a possible occurrence of this disease, and since MA almost doubles the possibility of death, it is simply necessary to understand all the possible risks in order to know how to protect yourself.
 The risk of disease increases with older age
The risk of disease increases with older age MA classification
Atrial fibrillation according to ICD-10 code І48 is subdivided into:
- first discovered;
- paroxysmal (lasts up to 7 days, can be stopped on its own);
- persistent (lasts more than 7 days and cannot be stopped on its own);
- constant.
By its form, the arrhythmia code according to ICD-10 І48 can be subdivided into:
- tachysystolic (ventricles are activated more than 90 times per minute);
- normosystolic (ventricular contraction rate from 60 to 90 times per minute);
- bradystolic (ventricular activation occurs less than 60 times per minute).
In addition to these, there are several special forms of cardiac arrhythmias code I48 according to ICD-10, including atrial fibrillation with Parkinson-White syndrome, AF with a weak sinus-atrial node, atrial fibrillation with complete AV block.
 Reciprocal tachycardia in SVC syndrome
Reciprocal tachycardia in SVC syndrome Paroxysm of MA
Paroxysm of atrial fibrillation is not a violation of the heart rhythm, it is in this case absolutely normal, but this is an increase in heart rate - it can rise to 240. Paroxysmal arrhythmia can suddenly make itself felt with a sharp attack, which can also suddenly end. The symptoms of this disease are manifested:
- chest pain;
- general weakness;
- fainting and lack of air;
- blue lips;
- general pallor of the skin.
Paroxysm of atrial fibrillation, or rather, its attack, can last for several minutes or several days. The end of the attack is accompanied by profuse diuresis, excessive sweating, increased intestinal peristalsis.
In the presence of this type of MA, constant medical supervision is very important, since there is a risk of a heart attack.
Sinus MA
Sinus arrhythmia manifests itself as a violation of the rhythm of the heart. At this moment, the contractions of the heart become irregular, that is, the beats occur at different intervals of time, but their coordination remains. Sinus arrhythmia is characterized by the following symptoms:
- a feeling of irregular heartbeats;
- weakness, dizziness;
- shortness of breath, feeling short of breath.
 Shortness of breath occurs with sinus arrhythmia
Shortness of breath occurs with sinus arrhythmia It is important to know that sinus arrhythmia, along with common causes of MA manifestation, can be triggered by some other reasons, including:
- physical activity, including sports;
- the state of sleep, food intake;
- the presence of vascular dystonia;
- respiratory diseases;
- malfunctions of the endocrine system of the body;
- long-term or uncontrolled use of certain types of medications;
- bad habits;
- changes in the ratio of potassium, sodium and magnesium salts.
Treatment tactics
Cardiac arrhythmias ICD-10 recommends treating with the two most well-known strategies - restoring and maintaining a normal heart rate or decreasing MA intensity while maintaining its presence. The algorithm of medical treatment tactics is as follows:
- assess the state of the circulatory system and circulation;
- conduct electrical impulse therapy (EIT) only if there are urgent indicators;
- use pharmacological cardioversion if there are no urgent indications or necessary conditions for EIT;
- preliminary to carry out pharmacological control of the heart rate when using cardioversion or the presence of a permanent form of atrial fibrillation;
- in case of MA duration more than 2 days, prescribe indirect anticoagulants for 3-4 weeks before and after cardioversion;
- prevent recurrence of AF.
 Treatment with pills
Treatment with pills It is important to understand that any medications are not absolutely harmless to the body, therefore, if there is an opportunity to refuse their use, doctors often do so. In particular, intermittent treatment of AF is permissible in patients who have rather rare attacks - no more than once a year.
It is also important that the treatment of heart rhythm abnormalities cannot be effective without eliminating the main cause of such abnormalities. Therefore, it is very important to eliminate provoking factors or, for example, in case of heart defect, to surgically eliminate this defect.
Contraindications
As with any therapy, treatment for MA has its own contraindications. In this case, the following conditions are contraindications:
- if atrial fibrillation lasts more than a year, cardioversion is contraindicated, since it gives too unstable effect compared to the risks of its use;
- if the patient has atriomegaly and cardiomegaly (mitral valve, dilated cardiomyopathy), cardioversion should be performed only in case of medical indications;
- with bradystolic AF, one should carefully approach the choice of treatment, since after the elimination of atrial fibrillation, AV block or weakness in the sinus-atrial node is often found;
- blood clots in the atria are also a contraindication for the treatment of AF.
And a little about secrets ...
Have you ever tried to get rid of varicose veins on your own? Judging by the fact that you are reading this article, the victory was not on your side. And of course you know firsthand what it is:
- over and over again to observe the next portion spider veins on foot
- wake up in the morning with the thought of what to wear to cover the swollen veins
- suffer every night from heaviness, schedule, swelling or buzzing in the legs
- a constantly bubbling cocktail of hope for success, anxious expectation and disappointment from a new unsuccessful treatment
Education: North-Western State Medical University named after V.I. I.I. Mechnikov, city ...
Atrial fibrillation is one of the forms of rhythm disturbances caused by the occurrence of a pathological focus of pulse circulation in the sinus node or in the atrial tissue, characterized by the occurrence of irregular, rapid and chaotic contraction of the atrial myocardium, and manifested by the sensation of a frequent and irregular heartbeat.
Forms of atrial fibrillation; paroxysmal, constant
In the general concept of atrial fibrillation, atrial fibrillation (flickering) and atrial flutter are distinguished. In the first type, the atrial contractions are "small-wave", with a pulse of about 500 per minute, providing a rapid contraction of the ventricles. In the second type of atrial contraction of about 300-400 per minute, "large-wave", but also forcing the ventricles to contract more often. In both the first and the second type, ventricular contractions can reach more than 200 per minute, but with atrial flutter, the rhythm can be regular - this is the so-called rhythmic, or correct form of atrial flutter.
In addition, atrial fibrillation and atrial flutter can occur simultaneously in one patient for a certain period of time, for example, with paroxysm of atrial fibrillation - atrial flutter. Often during atrial flutter, the ventricular rate can remain within normal limits, and then a more accurate analysis of the cardiogram is required for a correct diagnosis.

In addition to such a division of atrial fibrillation, according to the principle of the course of this disease, the following forms are distinguished:
- Paroxysmal, characterized by the occurrence of interruptions in the work of the heart and recorded by ECG during the first 24-48 hours (up to seven days), which can be stopped independently or with the help of medications,
- Persistent, characterized by rhythm disturbances such as atrial fibrillation or atrial flutter for more than seven days, but capable of spontaneous or medication restoration of the rhythm,
- Long-term persistent, existing for more than one year, but capable of restoring rhythm with the introduction of drugs or electrocardioversion (restoration of sinus rhythm using a defibrillator),
- Constant - a form characterized by the inability to restore sinus rhythm, which has existed for years.
Depending on the frequency of ventricular contractions, there are brady-, normo- and tachysystolic variants of atrial fibrillation. Accordingly, in the first case, the ventricular rate is less than 55-60 per minute, in the second - 60-90 per minute and in the third - 90 or more per minute.
Statistical data
According to studies conducted in Russia and abroad, atrial fibrillation occurs in 5% of the population over the age of 60 and in 10% of the population over 80. At the same time, women suffer from atrial fibrillation 1.5 times more often than men. The danger of arrhythmia is that in patients with paroxysmal or permanent forms, strokes and other thromboembolic complications occur 5 times more often.
In patients with heart defects, atrial fibrillation occurs in more than 60% of all cases, and in people with coronary heart disease - in almost 10% of cases.
What happens with atrial fibrillation?
Pathogenetic changes in this rhythm disturbance are due to the following processes. In normal myocardial tissue, the electrical impulse moves unidirectionally - from the sinus node towards the atrioventricular junction. In the presence of any blocks on the path of the impulse (inflammation, necrosis, etc.), the impulse cannot bypass this obstacle and is forced to move in the opposite direction, again causing excitation of the myocardial sections that have just contracted. Thus, a pathological focus of constant circulation of impulses is created.
Constant stimulation of certain areas of atrial tissue leads to the fact that these areas spread excitation to the remaining atrial myocardium, and its fibers contract separately, chaotically and irregularly, but often.
In the future, the impulses are conducted through the atrioventricular junction, but due to its relatively small "throughput" capacity, only part of the impulses reaches the ventricles, which begin to contract with different frequencies and also irregularly.
Video: Atrial Fibrillation - Medical Animation
What causes atrial fibrillation?
In the vast majority of cases, atrial fibrillation occurs as a result of organic damage to the myocardium. Diseases of this type include, first of all, heart defects. As a result of stenosis or valve failure, over time, the patient develops cardiomyopathy - a change in the structure and morphology of the myocardium. Cardiomyopathy leads to the fact that some of the normal muscle fibers in the heart are replaced by hypertrophied (thickened) fibers, which lose their ability to conduct impulses normally. Areas of hypertrophied tissue are pathological foci of impulses in the atria when it comes to stenosis and / or insufficiency of the mitral and tricuspid valves.
The next disease, which ranks second in the incidence of atrial fibrillation, is ischemic heart disease, including acute and postponed myocardial infarction. The path of development of arrhythmia is similar to defects, only areas of normal muscle tissue are replaced not by hypertrophied, but by necrotic fibers.
Also a significant cause of arrhythmia is cardiosclerosis - the proliferation of connective (scar) tissue instead of ordinary muscle cells. Cardiosclerosis can form within a few months or years after heart attacks or myocarditis (inflammatory changes in the heart tissue of a viral or bacterial nature). Atrial fibrillation often occurs in the acute period of myocardial infarction or in acute myocarditis.
In some patients, atrial fibrillation occurs in the absence of organic damage to the heart due to diseases of the endocrine system. The most common cause in this case is thyroid disease, accompanied by an increased release of thyroid hormones into the blood. This condition is called hyperthyroidism and occurs with nodular or autoimmune goiter. In addition, the constant stimulating effect of thyroid hormones on the heart leads to the formation of dyshormonal cardiomyopathy, which in itself can lead to impaired conduction in the atria.
In addition to the main reasons, risk factors can be identified that increase the likelihood of developing atrial fibrillation in a particular patient. These include age over 50, female sex, obesity, hypertension, endocrine pathology, including diabetes mellitus, a history of heart disease.
The factors that provoke the onset of paroxysm of atrial fibrillation in persons with a history of arrhythmia include conditions that cause changes in the autonomic regulation of cardiac activity.
For example, with the predominant influence of the vagus nerve (vagal, parasympathetic effects), an attack of arrhythmia can begin after a heavy meal, when turning the body, at night or during daytime rest, etc. sympathetic nerves on the heart, the onset or worsening of the course of arrhythmia occurs as a result of stress, fright, strong emotions or physical exertion - that is, all those conditions that are accompanied by increased secretion of adrenaline and norepinephrine into the blood.
Atrial fibrillation symptoms
Symptoms of atrial fibrillation may vary from patient to patient. Moreover, clinical manifestations are largely determined by the form and variant of atrial fibrillation.

For example, the clinic of paroxysmal atrial fibrillation is striking and characteristic. The patient, against the background of complete health or minor precursors (shortness of breath when walking, painful sensations in the heart region), experiences sudden unpleasant symptoms - a sharp feeling of rapid heartbeat, a feeling of shortness of breath, an attack of suffocation, a feeling of a coma in the chest and throat, inability to breathe in or out. At the same time, according to the description of the patients themselves, the heart flutters like a "hare's tail", ready to jump out of the chest, etc. In addition to this most characteristic symptom, some patients develop vegetative manifestations - excessive sweating, a feeling of internal trembling throughout the body, redness or pale skin, nausea, feeling lightheaded. This symptom complex in simple language is called "breakdown" of the rhythm.
But the ominous signs that should alert relatives and the doctor examining the patient are a sharp jump blood pressure upward (more than 150 mm Hg) or, conversely, a significant decrease in pressure (less than 90 mm Hg), since against the background high pressure the risk of stroke is high, and low blood pressure is a sign of acute heart failure or arrhythmogenic shock.
The clinical manifestations are brighter, the higher the heart rate. Although there are exceptions when a patient tolerates a frequency of 120-150 per minute more than satisfactory, and, on the contrary, a patient with a bradystolic variant experiences heart interruptions and dizziness more pronounced than with normo- and tachysystole.
With an uncompensated constant form of atrial fibrillation or atrial flutter, the heart rate is usually 80-120 per minute. Patients get used to this rhythm, and practically do not feel interruptions in the work of the heart, only with physical exertion. But here, due to the development of chronic heart failure, complaints of shortness of breath during physical exertion come to the fore, and often with minimal household activity and at rest.
Diagnostics
The algorithm for diagnosing atrial fibrillation consists of the following points:
- Examination and questioning of the patient. So, even in the process of collecting complaints and anamnesis, it is possible to establish that the patient has any rhythm disturbance. Counting the pulse per minute and determining its irregularity can prompt the doctor to think about atrial fibrillation.
- ECG diagnostics is a simple, accessible and informative method for confirming atrial fibrillation. The cardiogram is performed already when the ambulance team is called or during the initial treatment of the patient with interruptions to the clinic.

The criteria for atrial fibrillation are:
- After ECG the indications for hospitalization in a hospital are determined (see below). In case of hospitalization, further examination is carried out in the department of cardiology, therapy or arrhythmology, in case of refusal of hospitalization, the patient is sent for further examination to the polyclinic at the place of residence.
- From additional methods Diagnostics most often prescribed and informative is daily monitoring of ECG and blood pressure. This method allows you to register even short runs of arrhythmias that are not "caught" on a standard cardiogram, and also helps to assess the quality of the treatment.
- Ultrasound of the heart, or echo-CS (echo-cardioscopy). Is the "gold standard" in the imaging diagnosis of heart disease, as it allows you to detect
significant violations of myocardial contractility, its structural disorders and to evaluate the left ventricular ejection fraction, which is a decisive criterion for evaluating the effectiveness of therapy for heart failure with a constant form of atrial fibrillation. - A transesophageal electrophysiological study (PEEPI) is a method based on artificial stimulation of the myocardium and on provoking flicker, which can be immediately recorded on an ECG. It is carried out in order to register arrhythmias, which clinically disturb the patient with subjective sensations, and was not registered on the ECG (including with the help of Holter monitoring).
- Chest X-ray is used to examine patients with a paroxysmal form (suspected pulmonary embolism) and with a permanent form (to assess venous congestion in the lungs due to chronic heart failure).
- General and biochemical analyzes blood, study of the level of thyroid hormones in the blood, ultrasound of the thyroid gland - helps in differential diagnosis cardiomyopathies.
In principle, for the diagnosis of atrial fibrillation, characteristic complaints (interruptions in the heart, chest pain, dyspnea), anamnesis (acute or long-lasting), and an ECG with signs of atrial fibrillation or flutter are sufficient. However, it is necessary to find out the cause of such rhythm disturbance only in the process of a thorough examination of the patient.
Atrial fibrillation treatment tactics
Therapy for paroxysmal and persistent forms of atrial fibrillation is different. The purpose of assistance in the first form is to provide emergency care and to conduct rhythm-restoring therapy. In the second form, the priority is the appointment of rhythm-reducing therapy with the constant use of medications. The persistent form can be subject to both rhythm-restoring therapy and, in case of an unsuccessful implementation of the latter, the transfer of the persistent form to a permanent one using rhythm-reducing drugs.

Treatment of paroxysmal atrial fibrillation
The relief of a paroxysm of flickering or flutter is carried out already at the prehospital stage - by an ambulance or in a polyclinic.
Of the main drugs for an attack of arrhythmia, the following are used intravenously:
- The polarizing mixture is a solution of potassium chloride 4% + glucose 5% 400 ml + insulin 5 ED. In patients with diabetes mellitus, physical is used instead of a glucose-insulin mixture. solution (sodium chloride 0.9%) 200 or 400 ml.
- Panangin or asparkam solution 10 ml intravenously.
- A solution of novocainamide 10% 5 or 10 ml in saline. In case of a tendency to hypotension (low pressure), it should be administered simultaneously with Mesatone to prevent drug hypotension, collapse and loss of consciousness.
- Cordaron at a dosage of 5 mg / kg of body weight is injected in a 5% glucose solution intravenously slowly or by drip. Should be used in isolation from other antiarrhythmic drugs.
- Strofantin 0.025% 1 ml in 10 ml saline solution intravenously slowly or in 200 ml saline solution intravenously drip. It can be used only in the absence of glycosidic intoxication (chronic overdose with drugs of digoxin, korglikon, strophanthin, etc.).
After the administration of the drugs, after 20-30 minutes, the patient has an ECG taken and, in the absence of sinus rhythm, he must be taken to the admission department of the hospital to resolve the issue of hospitalization. The restoration of the rhythm at the level of the admission department is not carried out, the patient is hospitalized in the department, where the started treatment continues.
Indications for hospitalization:
- First identified paroxysmal arrhythmia,
- Prolonged paroxysm (from three to seven days), since the likelihood of thromboembolic complications is high,
- Paroxysm uncropped at the prehospital stage,
- Paroxysm with developing complications (acute heart failure, pulmonary edema, pulmonary embolism, heart attack or stroke),
- Decompensation of heart failure with a constant form of flicker.
Treatment of persistent atrial fibrillation
In the case of persistent flicker, the physician should seek to restore sinus rhythm with medication and / or cardioversion. This is due to the fact that with a restored sinus rhythm, the risk of developing thromboembolic complications is much lower than with a permanent form, and chronic heart failure progresses less. When successful recovery sinus rhythm, the patient must constantly take antiarrhythmic drugs, such as amiodarone, cordarone or propafenone (propanorm, rhythmonorm).
Thus, the tactics for a persistent form is as follows - the patient is observed in an outpatient clinic with atrial fibrillation more than seven days old, for example, after discharge from the hospital with unsuccessful relief of paroxysm and with ineffectiveness of the pills taken by the patient. If the doctor decides to try to restore sinus rhythm, he again sends the patient to the hospital for planned hospitalization for the purpose of medication to restore the rhythm or for cardioversion. If the patient has contraindications (past heart attacks and strokes, blood clots in the heart cavity according to the results of echocardioscopy, untreated hyperthyroidism, severe chronic heart failure, arrhythmia more than two years ago), the persistent form is transferred to a permanent form with the administration of other groups of drugs.
Treatment of a permanent form of atrial fibrillation
With this form, the patient is prescribed pills that slow down the heart rate. The main ones here are the group of beta-blockers and cardiac glycosides, for example, Concor 5 mg x 1 time per day, Coronal 5 mg x 1 time per day, egilok 25 mg x 2 times a day, Betaloc ZOK 25-50 mg x 1 time per day and others. From cardiac glycosides used digoxin 0.025 mg 1/2 tablet x 2 times a day - 5 days, a break - 2 days (Sat, Sun).
It is imperative to prescribe anticoagulants and antiplatelet agents, for example, cardiomagnyl 100 mg at lunchtime, or clopidogrel 75 mg at lunchtime, or warfarin 2.5-5 mg x 1 time per day (it is mandatory under the control of INR - the parameter of the blood coagulation system, usually 2.0-2.5 is recommended). These drugs prevent increased blood clots and reduce the risk of heart attacks and strokes.
Chronic heart failure should be treated with diuretics (indapamide 1.5 mg in the morning, veroshpiron 25 mg in the morning) and ACE inhibitors (prestarium 5 mg in the morning, enalapril 5 mg x 2 times a day, lisinopril 5 mg in the morning), which have an organoprotective effect on blood vessels and the heart.
When is cardioversion indicated?
Cardioversion is the restoration of the original heart rhythm in a patient with atrial fibrillation using medication (see above) or an electric current passed through the chest and affecting the electrical activity of the heart.

Electrical cardioversion is performed on an emergency or routine basis using a defibrillator. This type of assistance should be provided only in the intensive care unit with the use of anesthesia.
Indication for emergency cardioversion is a paroxysm of atrial fibrillation not more than two days old with the development of arrhythmogenic shock.
The indication for elective cardioversion is a paroxysm more than two days old, not stopped by medication, in the absence of blood clots in the atrial cavity, confirmed by transesophageal ultrasound of the heart. If a thrombus is found in the heart, the patient takes warfarin on an outpatient basis for a month, during which, in most cases, the thrombus dissolves, and then, after repeated ultrasound of the heart, in the absence of a thrombus, is sent back to the hospital to decide on cardioversion.
Thus, planned cardioversion is carried out mainly when the doctor strives to restore the sinus rhythm with a persistent form of atrial fibrillation.
Technically, cardioversion is performed by placing defibrillator electrodes on the anterior chest wall after the patient is anesthetized using intravenous drugs... After that, the defibrillator delivers a shock, which affects the heart rate. The success rate is very high and accounts for over 90% of successful restoration of sinus rhythm. However, cardioversion is not suitable for all patient populations, and in many cases (eg, in the elderly), MA will rapidly reappear.
Thromboembolic complications after cardioversion account for about 5% among patients who did not take anticoagulants and antiplatelet agents, as well as about 1% among patients who receive such drugs from the onset of arrhythmia.
When is surgical treatment indicated?
Surgical treatment for atrial fibrillation can serve several purposes. So, for example, with heart defects as the main cause of arrhythmia, surgical correction of the defect as an independent operation prevents further recurrence of atrial fibrillation in a greater percentage of cases.
For other heart diseases, radiofrequency or laser ablation of the heart is justified in the following cases:
- Ineffectiveness of antiarrhythmic therapy with frequent paroxysms of atrial fibrillation,
- A persistent form of flicker with rapid progression of heart failure
- Intolerance to antiarrhythmic drugs.
Radiofrequency ablation consists in the action of an electrode with a radio sensor at the end of the atria involved in the pathological circulation of the impulse. The electrode is inserted into the patient under general anesthesia through femoral artery under the control of X-ray television. The operation is safe and low-traumatic, takes a short period of time and is not a source of unpleasant sensations for the patient. RFA can be performed according to quotas from the Ministry of Health of the Russian Federation or at the patient's own money.
Is treatment with folk remedies acceptable?
Some patients may ignore the advice of their doctor and begin to heal themselves using traditional medicine. As an independent therapy, the intake of herbs and decoctions, of course, is not recommended. But as an auxiliary method, in addition to the main drug therapy, the patient can take decoctions of soothing plants, which have a beneficial effect on the nervous and cardiovascular system. For example, decoctions and infusions of valerian, hawthorn, clover, chamomile, mint and lemon balm are often used. In any case, the patient should inform the treating doctor about the intake of such herbs.
Are complications of atrial fibrillation possible?
The most common complications are pulmonary embolism (PE), acute heart attack and acute stroke, as well as arrhythmogenic shock and acute heart failure (pulmonary edema).
The most significant complication is stroke. Ischemic stroke, caused by a shot of a blood clot into the vessels of the brain (for example, when paroxysm stops), occurs in 5% of patients in the first five years after the onset of atrial fibrillation.

Prevention of thromboembolic complications (stroke and PE) is the constant intake of anticoagulants and antiplatelet agents. However, there are some nuances here. So, for example, with an increased risk of bleeding, the patient is likely to have a hemorrhage in the brain with the development of a hemorrhagic stroke. The risk of developing such a condition is more than 1% in patients in the first year from the start of anticoagulant therapy. Prevention of increased bleeding is regular monitoring of INR (at least once a month) with timely correction of the dose of the anticoagulant.
Video: how a stroke occurs due to atrial fibrillation
Forecast
The prognosis for life with atrial fibrillation is determined primarily by the causes of the disease. So, for example, in survivors of acute myocardial infarction and with significant cardiosclerosis, the short-term prognosis for life can be favorable, and for health and in the medium term, unfavorable, since in a short period of time the patient develops chronic heart failure, which worsens the quality of life and shortens it. duration.
However, with the regular use of prescribed medications, the prognosis for life and health will undoubtedly improve. And patients with a permanent form of MA registered at a young age, with proper compensation, live with it for up to 20-40 years.