Chronic obstructive pulmonary disease. Chronic obstructive pulmonary disease (COPD). We are treated at home with the help of folk remedies
Chronic obstructive pulmonary disease (COPD)- symptoms and treatment
What is chronic obstructive pulmonary disease (COPD)? We will analyze the causes of occurrence, diagnosis and methods of treatment in the article of Dr. Nikitin I. L., an ultrasound doctor with an experience of 25 years.
Definition of disease. Causes of the disease
Chronic obstructive pulmonary disease (COPD)- a disease that is gaining momentum, advancing in the ranking of causes of death for people over 45 years old. To date, the disease is in 6th place among the leading causes of death in the world, according to WHO forecasts in 2020, COPD will take the 3rd place.
This disease is insidious in that the main symptoms of the disease, in particular, with smoking, appear only 20 years after the start of smoking. It does not give clinical manifestations for a long time and may be asymptomatic, however, in the absence of treatment, obstruction imperceptibly progresses. respiratory tract, which becomes irreversible and leads to early disability and a reduction in life expectancy in general. Therefore, the topic of COPD seems to be especially relevant today.
It is important to know that COPD is a primary chronic illness where early diagnosis is important initial stages because the disease tends to progress.
If the doctor has diagnosed Chronic Obstructive Pulmonary Disease (COPD), the patient has a number of questions: what does this mean, how dangerous is it, what to change in lifestyle, what is the prognosis for the course of the disease?
So, chronic obstructive pulmonary disease or COPD is a chronic inflammatory disease with damage to the small bronchi (airways), which leads to respiratory failure due to narrowing of the bronchial lumen. Over time, emphysema develops in the lungs. This is the name of a condition in which the elasticity of the lungs decreases, that is, their ability to contract and expand during breathing. At the same time, the lungs are constantly as if in a state of inhalation, there is always a lot of air in them, even during exhalation, which disrupts normal gas exchange and leads to the development of respiratory failure.
Causes of COPD are:
- impact harmful factors environment;
- smoking;
- occupational hazard factors (dust containing cadmium, silicon);
- general environmental pollution (car exhaust gases, SO 2 , NO 2);
- frequent respiratory tract infections;
- heredity;
- deficiency of α 1 -antitrypsin.
If you experience similar symptoms, consult your doctor. Do not self-medicate - it is dangerous for your health!
Symptoms of chronic obstructive pulmonary disease
COPD- a disease of the second half of life, often develops after 40 years. The development of the disease is a gradual long process, often imperceptible to the patient.
Appeared forced to consult a doctor dyspnea And cough- the most common symptoms of the disease (shortness of breath is almost constant; cough is frequent and daily, with sputum in the morning).
The typical COPD patient is a smoker aged 45-50 who complains of frequent shortness of breath when physical activity.
Cough- one of the earliest symptoms of the disease. It is often underestimated by patients. In the initial stages of the disease, the cough is episodic, but later becomes daily.
Sputum also a relatively early symptom of the disease. In the first stages, it is released in small quantities, mainly in the morning. Slimy character. Purulent copious sputum appears during an exacerbation of the disease.
Dyspnea occurs in the later stages of the disease and is noted at first only with significant and intense physical activity, increases with respiratory diseases. In the future, shortness of breath is modified: the feeling of lack of oxygen during normal physical exertion is replaced by severe respiratory failure and intensifies over time. It is shortness of breath that becomes common cause in order to see a doctor.
When can COPD be suspected?
Here are some algorithm questions early diagnosis COPD:
- Do you cough several times a day? Does it bother you?
- Does coughing produce phlegm or mucus (often/daily)?
- Do you get short of breath faster/more often than your peers?
- Are you over 40?
- Do you smoke or have you ever smoked before?
If more than 2 questions are answered positively, spirometry with a bronchodilator test is necessary. When the test indicator FEV 1 / FVC ≤ 70, COPD is suspected.
Pathogenesis of chronic obstructive pulmonary disease
In COPD, both the airways and the tissue of the lung itself, the lung parenchyma, are affected.
The disease begins in the small airways with blockage of their mucus, accompanied by inflammation with the formation of peribronchial fibrosis (densification of the connective tissue) and obliteration (overgrowth of the cavity).
With the formed pathology, the bronchitis component includes:

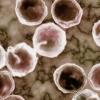
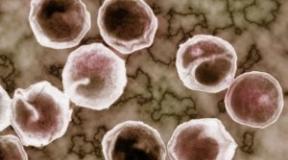
The emphysematous component leads to the destruction of the final sections of the respiratory tract - the alveolar walls and supporting structures with the formation of significantly expanded air spaces. The absence of a tissue framework of the airways leads to their narrowing due to the tendency to dynamically collapse during exhalation, which causes expiratory bronchial collapse.

In addition, the destruction of the alveolar-capillary membrane affects the gas exchange processes in the lungs, reducing their diffuse capacity. As a result, there is a decrease in oxygenation (oxygen saturation of the blood) and alveolar ventilation. Excessive ventilation of underperfused areas occurs, leading to an increase in dead space ventilation and impaired excretion carbon dioxide CO2. The area of the alveolar-capillary surface is reduced, but may be sufficient for gas exchange at rest, when these anomalies may not appear. However, during exercise, when the need for oxygen increases, if there are no additional reserves of gas exchange units, then hypoxemia occurs - a lack of oxygen in the blood.
The hypoxemia that appeared during long-term existence in patients with COPD includes a number of adaptive reactions. Damage to the alveolar-capillary units causes a rise in pressure in the pulmonary artery. Since the right ventricle of the heart under such conditions must develop more pressure to overcome the increased pressure in the pulmonary artery, it hypertrophies and expands (with the development of right ventricular heart failure). In addition, chronic hypoxemia can cause an increase in erythropoiesis, which subsequently increases blood viscosity and exacerbates right ventricular failure.
Classification and stages of development of chronic obstructive pulmonary disease

Complications of chronic obstructive pulmonary disease
Complications of COPD are infections, respiratory failure, and chronic cor pulmonale. Bronchogenic carcinoma (lung cancer) is also more common in patients with COPD, although it is not a direct complication of the disease.

Respiratory failure- the state of the external respiration apparatus, in which either the maintenance of the voltage of O 2 and CO 2 in arterial blood is not ensured at normal level, or it is achieved due to the increased work of the external respiration system. It manifests itself mainly as shortness of breath.
Chronic cor pulmonale- an increase and expansion of the right parts of the heart, which occurs with an increase blood pressure in the pulmonary circulation, which, in turn, developed as a result of pulmonary diseases. The main complaint of patients is also shortness of breath.
Diagnosis of chronic obstructive pulmonary disease
If patients have cough, sputum production, shortness of breath, and risk factors for chronic obstructive pulmonary disease have been identified, then they should all be assumed to have a diagnosis of COPD.
In order to establish a diagnosis, data are taken into account clinical examination(complaints, anamnesis, physical examination).
Physical examination may reveal symptoms characteristic of long-term bronchitis: "watch glasses" and / or "drumsticks" (deformity of the fingers), tachypnea (rapid breathing) and shortness of breath, a change in the shape of the chest (a barrel-shaped form is characteristic of emphysema), small its mobility during breathing, the retraction of the intercostal spaces with the development of respiratory failure, the descent of the boundaries of the lungs, the change in percussion sound to a box sound, weakened vesicular breathing or dry wheezing, which increase with forced expiration (that is, a quick exhalation after a deep breath). Heart sounds can be heard with difficulty. In the later stages, diffuse cyanosis, severe shortness of breath, and peripheral edema may occur. For convenience, the disease is divided into two clinical forms: emphysematous and bronchitis. Although in practical medicine there are more cases mixed form diseases.

The most important step in diagnosing COPD is analysis of respiratory function (RF). It is necessary not only to determine the diagnosis, but also to establish the severity of the disease, draw up an individual treatment plan, determine the effectiveness of therapy, clarify the prognosis of the course of the disease and assess the ability to work. Establishing the percentage of FEV 1 / FVC is most often used in medical practice. A decrease in forced expiratory volume in the first second to the forced vital capacity of the lungs FEV 1 / FVC up to 70% is the initial sign of airflow limitation even with a preserved FEV 1 > 80% of the proper value. A low peak expiratory airflow rate that does not change significantly with bronchodilators also favors COPD. With newly diagnosed complaints and changes in respiratory function, spirometry is repeated throughout the year. Obstruction is defined as chronic if it occurs at least 3 times per year (regardless of treatment), and COPD is diagnosed.
FEV monitoring 1 is an important method for confirming the diagnosis. Spireometric measurement of FEV 1 is carried out repeatedly over several years. The norm of the annual fall in FEV 1 for people of mature age is within 30 ml per year. For patients with COPD, a typical indicator of such a drop is 50 ml per year or more.
Bronchodilator test- primary examination, in which the maximum FEV 1 is determined, the stage and severity of COPD are established, and bronchial asthma is excluded (if the result is positive), the tactics and volume of treatment are selected, the effectiveness of therapy is assessed and the course of the disease is predicted. It is very important to distinguish COPD from bronchial asthma, since these common diseases have the same clinical manifestation- broncho-obstructive syndrome. However, the approach to treating one disease is different from another. Main hallmark in the diagnosis - the reversibility of bronchial obstruction, which is a characteristic feature of bronchial asthma. It has been found that people with a diagnosis of CO BL after taking a bronchodilator, the percentage increase in FEV 1 - less than 12% of the original (or ≤200 ml), and in patients with bronchial asthma, it usually exceeds 15%.
Chest x-rayhas an auxiliary sign chenie, since changes appear only in the later stages of the disease.
ECG can detect changes that are characteristic of cor pulmonale.
echocardiography necessary to detect symptoms of pulmonary hypertension and changes in the right heart.
General blood analysis- it can be used to evaluate hemoglobin and hematocrit (may be increased due to erythrocytosis).
Determining the level of oxygen in the blood(SpO 2) - pulse oximetry, a non-invasive study to clarify the severity of respiratory failure, as a rule, in patients with severe bronchial obstruction. Blood oxygen saturation of less than 88%, determined at rest, indicates severe hypoxemia and the need for oxygen therapy.
Treatment of chronic obstructive pulmonary disease
Treatment for COPD helps:
- reduction of clinical manifestations;
- increasing tolerance to physical activity;
- prevention of disease progression;
- prevention and treatment of complications and exacerbations;
- improving the quality of life;
- reduction in mortality.
The main areas of treatment include:
- weakening the degree of influence of risk factors;
- educational programs;
- medical treatment.
Weakening the degree of influence of risk factors
Smoking cessation is required. This is what is most effective way which reduces the risk of developing COPD.
Occupational hazards should also be controlled and reduced using adequate ventilation and air cleaners.
Educational programs
Educational programs for COPD include:
- basic knowledge about the disease and general approaches to treatment with the encouragement of patients to stop smoking;
- training on how to properly use individual inhalers, spacers, nebulizers;
- the practice of self-control using peak flow meters, the study of emergency self-help measures.
Patient education plays an important role in patient management and influences subsequent prognosis (Evidence A).
The method of peak flowmetry allows the patient to independently control the peak forced expiratory volume on a daily basis - an indicator that closely correlates with the FEV 1 value.
Patients with COPD at each stage are shown physical training programs in order to increase exercise tolerance.
Medical treatment
Pharmacotherapy for COPD depends on the stage of the disease, the severity of symptoms, the severity of bronchial obstruction, the presence of respiratory or right ventricular failure, and concomitant diseases. Drugs that fight COPD are divided into drugs to relieve an attack and to prevent the development of an attack. Preference is given to inhaled forms of drugs.

To stop rare attacks of bronchospasm, inhalations of β-agonists are prescribed. short action: salbutamol, fenoterol.
Preparations for the prevention of seizures:
- formoterol;
- tiotropium bromide;
- combined preparations (berotek, berovent).
If the use of inhalation is not possible or their effectiveness is insufficient, then theophylline may be necessary.
With a bacterial exacerbation of COPD, antibiotics are required. Can be used: amoxicillin 0.5-1 g 3 times a day, azithromycin 500 mg for three days, clarithromycin SR 1000 mg 1 time per day, clarithromycin 500 mg 2 times a day, amoxicillin + clavulanic acid 625 mg 2 times a day, cefuroxime 750 mg twice a day.
Withdrawal COPD symptoms also help glucocorticosteroids, which are also administered by inhalation (beclomethasone dipropionate, fluticasone propionate). If COPD is stable, then the appointment of systemic glucocorticosteroids is not indicated.
Traditional expectorants and mucolytics have little positive effect in patients with COPD.
In severe patients with a partial pressure of oxygen (pO 2) of 55 mm Hg. Art. and less at rest, oxygen therapy is indicated.
Forecast. Prevention
The prognosis of the disease is affected by the stage of COPD and the number of recurrent exacerbations. At the same time, any exacerbation negatively affects the general course of the process, therefore, the earliest possible diagnosis of COPD is highly desirable. Treatment of any exacerbation of COPD should begin as early as possible. It is also important to fully treat the exacerbation, in no case is it permissible to carry it “on the legs”.
Often people decide to go to the doctor for medical care, starting from the II moderate stage. At Stage III the disease begins to have a rather strong effect on the patient, the symptoms become more pronounced (increased shortness of breath and frequent exacerbations). At stage IV, there is a noticeable deterioration in the quality of life, each exacerbation becomes a threat to life. The course of the disease becomes disabling. This stage is accompanied by respiratory failure, the development of cor pulmonale is not excluded.
The prognosis of the disease is affected by patient compliance medical advice adherence to treatment and a healthy lifestyle. Continued smoking contributes to the progression of the disease. Smoking cessation leads to slower progression of the disease and slower decline in FEV 1 . Due to the fact that the disease has a progressive course, many patients are forced to take medicines for life, many require gradually increasing doses and additional funds during exacerbations.
The best ways to prevent COPD are: healthy lifestyle life, including good nutrition, hardening of the body, reasonable physical activity, and the exclusion of exposure to harmful factors. Smoking cessation is an absolute condition for the prevention of exacerbations of COPD. Existing occupational hazards, when diagnosing COPD, are a sufficient reason to change jobs. Preventive measures avoiding hypothermia and limiting contact with those with acute respiratory viral infections are also.
In order to prevent exacerbations, patients with COPD are shown annual influenza vaccination. People with COPD aged 65 years or older and patients with an FEV1< 40% показана вакцинация поливалентной пневмококковой вакциной.
Pulmonary obstruction is a progressive disease of the broncho-pulmonary system, in which the air in the respiratory tract runs incorrectly. This is due to abnormal inflammation of the lung tissue in response to external stimuli.
This is a non-communicable disease, it is not associated with the vital activity of pneumococci. The disease is widespread, according to WHO, 600 million people in the world suffer from pulmonary obstruction. Mortality statistics show that 3 million people die from the disease every year. With the development of megacities, this figure is constantly growing. Scientists believe that in 15-20 years the death rate will double.
The problem of the prevalence and incurability of the disease is the lack of early diagnosis. A person does not attach importance to the first signs of obstruction - cough in the morning and shortness of breath, which appears faster than in peers when performing the same physical activity. Therefore, patients seek medical help at a stage when it is already impossible to stop the pathological destructive process.
Risk factors and mechanism of disease development
Who is at risk of lung obstruction and what are the risk factors for the disease? Smoking comes first. Nicotine several times increases the likelihood of lung obstruction.
Occupational risk factors play an important role in the development of the disease. Professions in which a person is constantly in contact with industrial dust (ore, cement, chemicals):
- miners;
- builders;
- workers in the pulp processing industry;
- railroad workers;
- metallurgists;
- grain and cotton workers.
Atmospheric particles that can serve as a trigger in the development of the disease are exhaust gases, industrial emissions, industrial waste.
Also, hereditary predisposition plays a role in the occurrence of pulmonary obstruction. Internal risk factors include airway tissue hypersensitivity and lung growth.
The lungs produce special enzymes - protease and anti-protease. They regulate the physiological balance of metabolic processes, maintain the tone of the respiratory system. When there is a systematic and prolonged exposure to air pollutants (harmful air particles), this balance is disturbed.
As a result, the skeleton function of the lungs is impaired. This means that the alveoli (lung cells) collapse, lose their anatomical structure. Numerous bullae (formations in the form of vesicles) form in the lungs. Thus, the number of alveoli gradually decreases and the rate of gas exchange in the organ decreases. People begin to feel severe shortness of breath.
The inflammatory process in the lungs is a reaction to pathogenic aerosol particles and progressive airflow limitation.
Stages of development of pulmonary obstruction:
- tissue inflammation;
- pathology of small bronchi;
- destruction of the parenchyma (lung tissues);
- air flow limitation.
Symptoms of lung obstruction
 Obstructive airways disease is characterized by three main symptoms: shortness of breath, cough, sputum production.
Obstructive airways disease is characterized by three main symptoms: shortness of breath, cough, sputum production.
The first symptoms of the disease are associated with respiratory failure.. The person is out of breath. It is difficult for him to climb several floors. Going to the store takes more time, a person constantly stops to catch his breath. It becomes difficult to leave the house.
Development system of progressive dyspnea:
- initial signs of shortness of breath;
- difficulty breathing with moderate physical activity;
- gradual limitation of loads;
- a significant reduction in physical activity;
- shortness of breath when walking slowly;
- refusal of physical activity;
- persistent shortness of breath.
Patients with pulmonary obstruction develop a chronic cough. It is associated with partial obstruction of the bronchi. Cough is constant, daily, or intermittent, with ups and downs. As a rule, the symptom is worse in the morning and may appear during the day. At night, coughing does not bother a person.
Shortness of breath is progressive and persistent (daily) and only gets worse over time. It also increases with physical activity and respiratory diseases.
With obstruction of the lungs in patients, sputum discharge is recorded. Depending on the stage and neglect of the disease, mucus can be scanty, transparent or abundant, purulent.
The disease leads to chronic insufficiency respiration - the inability of the pulmonary system to provide high-quality gas exchange. Saturation (oxygen saturation of arterial blood) does not exceed 88%, at a rate of 95-100%. This is a life threatening condition. In the last stages of the disease, a person may experience apnea at night - suffocation, stopping lung ventilation for more than 10 seconds, on average it lasts half a minute. In extremely severe cases, respiratory arrest lasts 2-3 minutes.
In the daytime, a person feels severe fatigue, drowsiness, instability of the heart.
Lung obstruction leads to early disability and a reduction in life expectancy, a person acquires disability status.
Obstructive changes in the lungs in children
Pulmonary obstruction in children develops due to respiratory diseases, malformations of the pulmonary system, chronic pathologies of the respiratory system. Of no small importance is the hereditary factor. The risk of developing pathology increases in a family where parents constantly smoke.
Obstruction in children is fundamentally different from obstruction in adults. Blockage and destruction of the airways are the result of one of the nosological forms (a certain independent disease):
- Chronical bronchitis. The child has a wet cough, wheezing of various sizes, exacerbations up to 3 times a year. The disease is the result inflammatory process in the lungs. The initial obstruction occurs due to excess mucus and sputum.
- Bronchial asthma. Despite the fact that asthma and chronic pulmonary obstruction are different diseases, they are interconnected in children. Asthmatics are at risk of developing obstruction.
- bronchopulmonary dysplasia. This chronic pathology in babies during the first two years of life. The risk group includes premature and underweight children who have had SARS immediately after birth. In such infants, the bronchioles and alveoli are affected, the functionality of the lungs is impaired. Gradually, respiratory failure and oxygen dependence appear. There are gross changes in the tissue (fibrosis, cysts), the bronchi are deformed.
- Interstitial lung diseases. This is a chronic hypersensitivity of lung tissue to allergenic agents. Develops by inhalation of organic dust. It is expressed by diffuse lesions of the parenchyma and alveoli. Symptoms - cough, wheezing, shortness of breath, impaired ventilation.
- obliterating bronchiolitis. This is a disease of the small bronchi, which is characterized by narrowing or complete blockage of the bronchioles. Such obstruction in a child is predominantly manifested in the first year of life.. Reason: SARS adenovirus infection. Signs - unproductive, severe, recurrent cough, shortness of breath, weak breathing.
Diagnosis of lung obstruction
 When a person contacts a doctor, an anamnesis (subjective data) is collected. Differential symptoms and markers of pulmonary obstruction:
When a person contacts a doctor, an anamnesis (subjective data) is collected. Differential symptoms and markers of pulmonary obstruction:
- chronic weakness, decreased quality of life;
- unstable breathing during sleep, loud snoring;
- weight gain;
- increase in the circumference of the collar zone (neck);
- blood pressure is higher than normal;
- pulmonary hypertension (increased pulmonary vascular resistance).
The mandatory examination includes a general blood test to exclude a tumor, purulent bronchitis, pneumonia, anemia.
A general urine test helps to exclude purulent bronchitis, in which amyloidosis is detected - a violation of protein metabolism.
A general sputum analysis is rarely done, as it is not informative.
Patients undergo peak flowmetry, a functional diagnostic method that evaluates the expiratory rate. This determines the degree of airway obstruction.
All patients undergo spirometry - a functional study of external respiration. Assess the rate and volume of breathing. Diagnosis is carried out on a special device - a spirometer.
During the examination, it is important to exclude bronchial asthma, tuberculosis, obliterating bronchiolitis, bronchiectasis.
Treatment of the disease
 The goals of treating obstructive lung disease are multifaceted and include the following steps:
The goals of treating obstructive lung disease are multifaceted and include the following steps:
- improvement in respiratory function of the lungs;
- constant monitoring of symptoms;
- increased resistance to physical stress;
- prevention and treatment of exacerbations and complications;
- stop the progression of the disease;
- minimization side effects therapy;
- improving the quality of life;
The only way to stop the rapid destruction of the lungs is to completely stop smoking.
In medical practice, developed special programs to combat nicotine addiction in smokers. If a person smokes more than 10 cigarettes a day, then he is shown a drug course of therapy - short up to 3 months, long - up to a year.
Nicotine replacement treatment is contraindicated in such internal pathologies:
- severe arrhythmia, angina pectoris, myocardial infarction;
- circulatory disorders in the brain, stroke;
- ulcers and erosion of the digestive tract.
Patients are prescribed bronchodilator therapy. Basic treatment includes bronchodilators to widen the airways. The drugs are prescribed both intravenously and inhalation. When inhaled, the medicine instantly penetrates the affected lung, has a quick effect, reduces the risk of developing negative consequences and side effects.
During inhalation, you need to breathe calmly, the duration of the procedure is an average of 20 minutes. With deep breaths, there is a risk of developing a strong cough and choking.
 Effective bronchodilators:
Effective bronchodilators:
- methylxanthines - Theophylline, Caffeine;
- anticholinergics - Atrovent, Berodual, Spiriva;
- b2-agonists - Fenoterol, Salbutamol, Formoterol.
In order to improve survival, patients with respiratory failure are prescribed oxygen therapy (at least 15 hours per day).
To thin the mucus, increase its discharge from the walls of the respiratory tract and expand the bronchi, a complex of drugs is prescribed:
- Guaifenesin;
- Bromhexine;
- Salbutamol.
To consolidate the treatment of obstructive pneumonia, rehabilitation measures are needed. Every day, the patient should conduct physical training, increase strength and endurance. Recommended sports are walking 10 to 45 minutes daily, stationary bike, lifting dumbbells. Nutrition plays an important role. It should be rational, high-calorie, contain a lot of protein. An integral part of the rehabilitation of patients is psychotherapy.
Patients with COPD of the 3rd degree are entitled to disability, but its assignment is considered by the medical and social expert commission on an individual basis. The disability group is determined on the basis of an assessment of the patient's condition and the frequency of exacerbations of the disease. Only then will the ITU make its decision.
The third degree of the disease
In total, there are 4 stages of COPD (chronic obstructive pulmonary disease). Stage 3 is a severe form of the disease, which has its own distinctive features:
- shortness of breath appears not only after physical activity, but also at rest;
- breathing is difficult, there is a feeling of chest tightness;
- cough that worries even in a dream, discharge of purulent sputum;
- regular exacerbations of bronchitis and tracheitis;
- there is an increase in temperature for no apparent reason and during the time when the disease worsens;
- there is a sharp decline in strength during the day;
- weak functioning of the immune system.
Earlier stages have less pronounced symptoms, for example, stage 2 COPD is characterized by shortness of breath on exertion, cough in the morning with sputum, and minor changes in general condition.
This chronic disease significantly shortens the life span. If the doctor puts stage 3, then the patient still has to live up to 10 years. Often the disease has complications that further reduce life expectancy:
- the transition of COPD to stage 4;
- oncological formations in the lungs;
- pneumonia;
- increased pressure in pulmonary artery(hypertension);
- palpitations;
- thrombosis.
With these diseases, patients diagnosed with COPD are 30% more likely than healthy people. Properly selected therapy reduces the risks and alleviates the symptoms of the disease. The doctor prescribes mucolytic drugs that can increase the lumen in the bronchi. If bronchial inflammation is recorded, glucocorticoid drugs are prescribed - these are hormones of the adrenal cortex.
Treatment of a patient with stage 3 COPD is carried out in a hospital:
- symptoms worsen and treatment does not help;
- immediate and advanced diagnostics are required;
- accompany serious illness(obstructive bronchitis, diabetes, liver and kidney disease, heart problems).
This stage of the disease is serious, the patient may qualify for disability.
Conditions for applying for a disability
Patients undergo a medical and social expert commission, which decides on the assignment of disability and its degree.
A number of indications that serve as a referral to the expert commission:
- regular exacerbations of the disease;
- body resistance to long-term treatment and rehabilitation therapy;
- the occurrence of incurable consequences (disturbance of cardiac activity, changes in the shape and size of the heart muscle, malignant tumors).
With these indications, they go to the polyclinic at the place of residence, to the authority social protection population or to the pension fund. There you need to get a certificate confirming the disease, which serves as a referral to an expert commission.
To apply for a disability, you need to collect a number of documents:
- sick leave;
- original and copy of the passport;
- a copy of the work book certified by a notary;
- referral to the commission;
- personal characteristic issued at the place of work or study;
- originals and copies of extracts from the hospital, a map from the clinic;
- an application filled in by the medical and social expert commission.
As soon as the documents for obtaining a disability degree are collected, you need to make an appointment at the bureau of the medical and social expert commission. Admission is made at the place of permanent or temporary registration. An examination is scheduled within 30 days. If the patient is not able to appear in person, then by law the commission cannot refuse to conduct an examination. In this case, you can submit documents without appearing for examination. The decision will be made in absentia.
After a successful passage, the patient is recognized as a disabled person and a certificate, a rehabilitation plan and a closed sick leave are issued. If the commission refused to award the degree, then its decision is appealed at the federal level of the ITU or through the courts.
Degrees of Disability and Benefits
Patients with COPD can be assigned one of three degrees of disability, it all depends on the course of the disease.
Disability of the third group is assigned to patients with mild and moderate course of the disease, the result of which is the limitation of the ability to work, self-sufficiency, movement and service.
Benefits for disabled people of the 3rd group:
- purchase of prescription drugs with a 50% discount;
- sanatorium treatment under special conditions;
- 50% discount on utility bills;
- monthly compensation.
Disability of the 2nd group is assigned in case of severe or moderate course of COPD. The disease limits the possibility of labor activity, self-service and self-sufficiency, full movement is impossible. The patient can work at home if certain conditions are created.
Benefits for disabled people of the second group:
- monthly compensation;
- 50% discount on notary services, purchase of medicines by doctor's prescriptions, utilities;
- no property taxes.
Disability of the 1st group is assigned to patients in whom COPD is actively progressing, completely limiting labor activity and wholly or partly restricting self-care, self-sufficiency and mobility.
Benefits for the disabled of the third troupe:
- monthly compensation;
- free travel on public transport;
- the possibility of a voucher to a health resort according to the profile of the disease;
- prosthetics of teeth at the expense of the state;
- the absence of a number of property taxes;
- 50% discount on notary services, purchase of prescription drugs, utilities.
Video about the features of COPD:
In patients diagnosed with COPD, properly selected therapy reduces the risk of developing the disease.
Chronic obstructive pulmonary disease (COPD) is a progressive disease of the bronchi and lungs associated with an increased inflammatory response of these organs to the action of harmful factors (dust and gases). It is accompanied by a violation of lung ventilation due to deterioration of bronchial patency.
Physicians also include emphysema in the concept of COPD. Chronic bronchitis is diagnosed by symptoms: the presence of a cough with sputum for at least 3 months (not necessarily consecutive) in the last 2 years. Emphysema is a morphological concept. This is an expansion of the airways behind the final sections of the bronchi, associated with the destruction of the walls of the respiratory vesicles, alveoli. In patients with COPD, these two conditions are often combined, which determines the characteristics of the symptoms and treatment of the disease.
The prevalence of the disease and its socio-economic significance
COPD is recognized as a worldwide medical problem. In some countries, such as Chile, it affects one in five adults. In the world, the average prevalence of the disease among people over 40 years of age is about 10%, with men getting sick more often than women.
In Russia, morbidity data largely depend on the region, but in general they are close to world indicators. The prevalence of the disease increases with age. In addition, it is almost twice as high among people living in rural areas. So, in Russia, every second person living in a village suffers from COPD.
In the world, this disease is the fourth leading cause of death. Mortality in COPD is growing very rapidly, especially among women. Factors that increase the risk of dying from this disease are increased weight, severe bronchospasm, low endurance, severe shortness of breath, frequent exacerbations of the disease, and pulmonary hypertension.
The costs of treating the disease are also high. Most of them are for inpatient treatment of exacerbations. COPD therapy is more expensive for the state than treatment. The frequent disability of such patients, both temporary and permanent (disability), is also important.
Causes and mechanism of development
The main cause of COPD is smoking, active and passive. Tobacco smoke damages the bronchi and lung tissue itself, causing inflammation. Only 10% of cases of the disease are associated with the influence of occupational hazards, constant air pollution. Genetic factors may also be involved in the development of the disease, causing a deficiency of certain lung-protecting substances.
Predisposing factors for the development of the disease in the future are low body weight at birth, as well as frequent respiratory diseases suffered in childhood.
At the onset of the disease, the mucociliary transport of sputum is disturbed, which ceases to be removed from the respiratory tract in time. Mucus stagnates in the lumen of the bronchi, creating conditions for the reproduction of pathogenic microorganisms. The body reacts defensive reaction- inflammation that becomes chronic. The walls of the bronchi are impregnated with immunocompetent cells.
Immune cells secrete a variety of inflammatory mediators that damage the lungs and set off a vicious cycle of disease. Oxidation and the formation of free oxygen radicals that damage the walls of lung cells increase. As a result, they are destroyed.
Violation of bronchial patency is associated with reversible and irreversible mechanisms. Reversible include spasm of the muscles of the bronchi, swelling of the mucosa, an increase in mucus secretion. Irreversible are caused by chronic inflammation and are accompanied by the development of connective tissue in the walls of the bronchi, the formation of emphysema (bloating of the lungs, in which they lose their ability to ventilate normally).
The development of emphysema is accompanied by a decrease in blood vessels, through the walls of which gas exchange occurs. As a result, pressure in the pulmonary vasculature rises - pulmonary hypertension occurs. High blood pressure creates an overload for the right ventricle, pumping blood into the lungs. Develops with the formation of cor pulmonale.
Symptoms
 Patients with COPD experience cough and shortness of breath.
Patients with COPD experience cough and shortness of breath. COPD develops gradually and flows for a long time without external manifestations. The first symptoms of the disease are a cough with light sputum or, especially in the morning, and frequent colds.
The cough is aggravated in the cold season. Shortness of breath increases gradually, appearing first with exertion, then with normal activity, and then at rest. It occurs about 10 years later than cough.
Periodic exacerbations occur, lasting several days. They are accompanied by increased coughing, shortness of breath, the appearance of wheezing, pressing pain in the chest. Reduced exercise tolerance.
The amount of sputum increases or decreases sharply, its color, viscosity changes, it becomes purulent. The frequency of exacerbations is directly related to life expectancy. Exacerbations of the disease are more common in women and more severely reduce their quality of life.
Sometimes you can meet the division of patients according to the predominant feature. If inflammation of the bronchi is important in the clinic, such patients are dominated by cough, lack of oxygen in the blood, causing a blue tint of the hands, lips, and then the entire skin (cyanosis). Rapidly developing heart failure with the formation of edema.
If emphysema, manifested by severe shortness of breath, is of greater importance, then cyanosis and cough are usually absent or they appear in the later stages of the disease. These patients are characterized by progressive weight loss.
In some cases, there is a combination of COPD and bronchial asthma. In this case, the clinical picture acquires the features of both these diseases.
 Differences between COPD and bronchial asthma
Differences between COPD and bronchial asthma In COPD, a variety of extrapulmonary symptoms associated with a chronic inflammatory process are recorded:
- weight loss;
- neuropsychiatric disorders, sleep disturbance.
Diagnostics
The diagnosis of COPD is based on the following principles:
- confirmation of the fact of smoking, active or passive;
- objective research (examination);
- instrumental confirmation.
The problem is that many smokers deny that they have a disease, considering coughing or shortness of breath as a consequence of a bad habit. Often they seek help already in advanced cases, when they become disabled. It is no longer possible to cure the disease or slow its progression at this time.
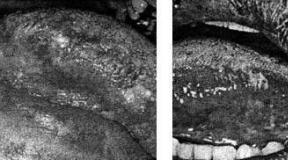
On the early stages disease external examination does not reveal changes. In the future, exhalation is determined through closed lips, a barrel-shaped chest, participation in breathing of additional muscles, retraction of the abdomen and lower intercostal spaces during inspiration.
On auscultation, dry whistling rales are determined, on percussion - a boxed sound.
From laboratory methods a general blood test is required. It may show signs of inflammation, anemia, or blood clots.
Cytological examination of sputum allows to exclude a malignant neoplasm, as well as to assess inflammation. To select antibiotics, sputum culture (microbiological examination) or analysis of bronchial contents, which are obtained during bronchoscopy, can be used.
A chest X-ray is performed, which allows you to exclude other diseases (pneumonia, lung cancer). For the same purpose, bronchoscopy is prescribed. For rate pulmonary hypertension using electrocardiography and
The main method for diagnosing COPD and assessing the effectiveness of treatment is spirometry. It is carried out at rest, and then after inhalation of bronchodilators, such as salbutamol. Such a study helps to identify bronchial obstruction (decrease in airway patency) and its reversibility, that is, the ability of the bronchi to return to normal after using medications. Irreversible bronchial obstruction is often observed in COPD.
With an already confirmed diagnosis of COPD, peak flowmetry with the determination of peak expiratory flow can be used to monitor the course of the disease.
Treatment

The only way to reduce the risk of the disease or slow its development is to stop smoking. Do not smoke in front of children!
Attention should also be paid to the cleanliness of the surrounding air, respiratory protection when working in hazardous conditions.
Drug treatment is based on the use of drugs that expand the bronchi - bronchodilators. They are mainly used. Combinations are the most effective.
The doctor may prescribe the following groups of drugs, depending on the severity of the disease:
- Short-acting M-cholinergic blockers (ipratropium bromide);
- M-anticholinergics long-acting(tiotropium bromide);
- long-acting beta-agonists (salmeterol, formoterol);
- short-acting beta-agonists (salbutamol, fenoterol);
- long-acting theophyllines (teotard).
In moderate and severe inhalations can be carried out with. In addition, spacers are often useful in older people.
Additionally, when severe course diseases, inhaled glucocorticosteroids (budesonide, fluticasone) are prescribed, usually in combination with long-acting beta-agonists.
(sputum thinners) are indicated only for some patients in the presence of thick, difficult to expectorate mucus. For long-term use and prevention of exacerbations, only acetylcysteine is recommended. Antibiotics are prescribed only during an exacerbation of the disease.
COPD (chronic obstructive pulmonary disease) is a disease that develops as a result of an inflammatory response to the action of certain environmental stimuli, with damage to the distal bronchi and the development of emphysema, and which is manifested by a progressive decrease in the airflow rate in the lungs, an increase, as well as damage to other organs.
COPD ranks second among chronic non-communicable diseases and fourth among causes of death, and this figure is steadily increasing. Due to the fact that this disease is inevitably progressive, it occupies one of the first places among the causes of disability, as it leads to a violation of the main function of our body - the respiratory function.
COPD is a truly global problem. In 1998, an initiative group of scientists created the Global Initiative for Chronic Obstructive Lung Disease (GOLD). The main tasks of GOLD are the wide dissemination of information about this disease, the systematization of experience, the explanation of the causes and the corresponding preventive measures. The main idea that doctors want to convey to humanity: COPD can be prevented and treated this postulate is even included in the modern working definition of COPD.
Causes of COPD
COPD develops with a combination of predisposing factors and provoking environmental agents.

Predisposing factors
- hereditary predisposition. It has already been proven that congenital deficiency of certain enzymes predisposes to the development of COPD. This explains the family history of this disease, as well as the fact that not all smokers, even with long experience, get sick.
- Gender and age. Men over the age of 40 suffer more from COPD, but this can be explained both by the aging of the body and the duration of smoking. Data are given that now the incidence rate among men and women is almost equal. The reason for this may be the spread of smoking among women, as well as increased sensitivity female body to passive smoking.
- Any negative impact that affect the development of the respiratory organs of the child in the prenatal period and early childhood increase the risk of future COPD. In itself, physical underdevelopment is also accompanied by a decrease in lung volume.
- Infections. Frequent respiratory infections in childhood, as well as increased susceptibility to them at an older age.
- Bronchial hyperreactivity. Although bronchial hyperreactivity is the main mechanism of development, this factor is also considered a risk factor for COPD.
Provoking factors

COPD pathogenesis
Exposure to tobacco smoke and other irritants in susceptible individuals leads to chronic inflammation in the walls of the bronchi. The key is the defeat of their distal departments (that is, those located closer to the lung parenchyma and alveoli).
As a result of inflammation, there is a violation of the normal secretion and discharge of mucus, blockage of small bronchi, infection easily joins, inflammation spreads to the submucosal and muscle layers, muscle cells die and are replaced connective tissue(the process of bronchial remodeling). At the same time, the destruction of the parenchyma of the lung tissue, the bridges between the alveoli occurs - emphysema develops, that is, hyperairiness of the lung tissue. The lungs seem to swell with air, their elasticity decreases.

Small bronchi on exhalation do not expand well - the air hardly comes out of the emphysematous tissue. Normal gas exchange is disturbed, as the volume of inhalation also decreases. As a result, the main symptom of all patients with COPD- shortness of breath, especially aggravated by movement, walking.
Respiratory failure results in chronic hypoxia. The whole body suffers from this. Prolonged hypoxia leads to a narrowing of the lumen of the pulmonary vessels - occurs, which leads to the expansion of the right heart ( cor pulmonale) and the addition of heart failure.
Why is COPD singled out as a separate nosology?

The awareness of this term is so low that most of the patients who already suffer from this disease do not know that they have COPD. Even if such a diagnosis is made in medical records, in the everyday life of both patients and doctors, the previously familiar and "emphysema" still prevail.
The main components in the development of COPD are indeed chronic inflammation and emphysema. So why, then, is COPD singled out as a separate diagnosis?
In the name of this nosology, we see the main pathological process - chronic obstruction, that is, narrowing of the airway lumen. But the process of obstruction is also present in other diseases.
The difference between COPD and bronchial asthma is that COPD obstruction almost or completely irreversible. This is confirmed by spirometric measurements using bronchodilators. At bronchial asthma after the use of bronchodilators, there is an improvement in FEV1 and PSV by more than 15%. This obstruction is treated as reversible. With COPD, these numbers change slightly.
Chronic bronchitis may precede or accompany COPD, but it is an independent disease with well-defined criteria (prolonged cough and), and the term itself implies damage only to the bronchi. With COPD, all structural elements of the lungs are affected - bronchi, alveoli, blood vessels, pleura. Not always chronic bronchitis is accompanied by obstructive disorders. On the other hand, increased sputum production is not always observed in COPD. That is, in other words, maybe Chronical bronchitis without COPD, and COPD doesn't quite fit the definition of bronchitis.

Chronic obstructive pulmonary disease
Thus, COPD is now a separate diagnosis, has its own criteria, and in no way replaces other diagnoses.
Diagnostic Criteria for COPD
You can suspect COPD in the presence of a combination of all or several signs, if they occur in people over 40 years of age:

A reliable confirmation of COPD is the spirometric indicator of the ratio of forced expiratory volume in 1 s to the forced vital capacity of the lungs (FEV1 / FVC), carried out 10-15 minutes after the use of bronchodilators (beta-sympathomimetics, salbutamol, berotek or 35-40 minutes after short-acting anticholinergics -ipratropium bromide). The value of this indicator<0,7 подтверждает ограничение скорости воздушного потока и в сочетании с подтвержденными факторами риска является достоверным критерием диагноза ХОБЛ.
Other spirometry measures, such as peak expiratory flow rate, as well as FEV1 measurement without a bronchodilator test, can be used as a screening examination, but do not confirm the diagnosis of COPD.
Other methods prescribed for COPD, in addition to the usual clinical minimum, include lung x-ray, pulse oximetry (determination of blood oxygen saturation), blood gases (hypoxemia, hypercapnia), bronchoscopy, chest CT, sputum examination.
COPD classification
There are several classifications of COPD according to stages, severity, clinical options.
Classification by stages takes into account the severity of symptoms and spirometry data:
- Stage 0. Risk group. Impact of adverse factors (smoking). No complaints, lung function is not impaired.
- Stage 1. Mild COPD.
- Stage 2. Moderate course of COPD.
- Stage 3. Severe course.
- Stage 4. Extremely severe course.

The latest GOLD report (2011) proposed to exclude the classification by stages, it remains severity classification based on FEV1:
In patients with FEV1/FVC<0,70:
- GOLD 1: Mild FEV1 ≥80% predicted
- GOLD 2: Moderate 50% ≤ FEV1< 80%.
- GOLD 3: Severe 30% ≤ FEV1< 50%.
- GOLD 4: Extremely severe FEV1<30%.
It should be noted that the severity of symptoms does not always correlate with the degree of bronchial obstruction. Patients with mild obstruction may be bothered by fairly severe dyspnea, and, conversely, patients with GOLD 3 and GOLD 4 may feel quite satisfactory for a long time. To assess the severity of dyspnea in patients, special questionnaires are used, the severity of symptoms is determined in points. It is also necessary to focus on the frequency of exacerbations and the risk of complications in assessing the course of the disease.
Therefore, this report proposes, based on the analysis of subjective symptoms, spirometry data and the risk of exacerbations, to divide patients into clinical groups - A, B, C, D.

Practitioners also distinguish clinical forms of COPD:
- Emphysematous variant of COPD. Of the complaints in such patients, shortness of breath predominates. Cough is observed less often, sputum may not be. Hypoxemia, pulmonary hypertension come late. Such patients, as a rule, have a low body weight, the color of the skin is pink-gray. They are called "pink puffers".
- bronchitis variant. Such patients complain mainly of cough with phlegm, shortness of breath is less disturbing, they develop cor pulmonale quite quickly with a corresponding picture of heart failure - cyanosis, edema. Such patients are called "blue puffers".
The division into emphysematous and bronchitis variants is rather conditional, mixed forms are more often observed.
During the course of the disease, a phase of a stable course and an exacerbation phase are distinguished.
Exacerbation of COPD
An exacerbation of COPD is an acutely developing condition when the symptoms of the disease go beyond its usual course. There is an increase in shortness of breath, cough and deterioration of the general condition of the patient. Conventional therapy, which he used previously, does not stop these symptoms to the usual state, a change in dose or treatment regimen is required. Usually, hospitalization is required for an exacerbation of COPD.
Diagnosis of exacerbations is based solely on complaints, anamnesis, clinical manifestations, and can also be confirmed by additional studies (spirometry, complete blood count, microscopy and bacteriological examination of sputum, pulse oximetry).
The causes of exacerbation are most often respiratory viral and bacterial infections, less often - other factors (exposure to harmful factors in the surrounding air). A common event in a patient with COPD is an event that significantly reduces lung function, and return to baseline may take a long time, or stabilization will occur at a more severe stage of the disease.
The more frequent exacerbations occur, the worse the prognosis of the disease and the higher the risk of complications.
Complications of COPD
Due to the fact that patients with COPD exist in a state of constant hypoxia, they often develop the following complications:

COPD treatment
Basic principles of therapeutic and preventive measures for COPD:
- To give up smoking. At first glance, a simple, but the most difficult to implement moment.
- Pharmacotherapy. Early initiation of basic drug treatment can significantly improve the patient's quality of life, reduce the risk of exacerbations and increase life expectancy.
- The drug therapy regimen should be selected individually, taking into account the severity of the course, the patient's adherence to long-term treatment, the availability and cost of drugs for each individual patient.
- Influenza and pneumococcal vaccinations should be offered to patients with COPD.
- The positive effect of physical rehabilitation (training) has been proven. This method is under development, while there are no effective therapeutic programs. The easiest way that can be offered to the patient is daily walking for 20 minutes.
- In the case of a severe course of the disease with severe respiratory failure, long-term oxygen inhalation as a means of palliative care improves the patient's condition and prolongs life.

To give up smoking
Tobacco cessation has been proven to have a significant impact on the course and prognosis of COPD. Despite the fact that the chronic inflammatory process is considered irreversible, smoking cessation slows down its progression, especially in the early stages of the disease.
Tobacco addiction is a serious problem that requires a lot of time and effort not only for the patient himself, but also for doctors and relatives. A special long-term study was conducted with a group of smokers, which offered various activities aimed at combating this addiction (conversations, persuasion, practical advice, psychological support, visual agitation). With such an investment of attention and time, it was possible to achieve smoking cessation in 25% of patients. Moreover, the longer and more often the conversations are held, the more likely they are to be effective.
 Anti-tobacco programs are becoming national targets. There is a need not only to promote a healthy lifestyle, but also to legislate punishment for smoking in public places. This will help limit the harm from at least passive smoking. Tobacco smoke is especially harmful for pregnant women (both active and passive smoking) and children.
Anti-tobacco programs are becoming national targets. There is a need not only to promote a healthy lifestyle, but also to legislate punishment for smoking in public places. This will help limit the harm from at least passive smoking. Tobacco smoke is especially harmful for pregnant women (both active and passive smoking) and children.
For some patients, tobacco addiction is akin to drug addiction, and in this case, interviews will not be enough.
In addition to agitation, there are also medical ways to combat smoking. These are nicotine replacement tablets, sprays, chewing gums, skin patches. The effectiveness of some antidepressants (bupropion, nortriptyline) in the formation of long-term smoking cessation has also been proven.
Pharmacotherapy for COPD
Drug therapy for COPD is aimed at managing symptoms, preventing exacerbations, and slowing the progression of chronic inflammation. It is impossible to completely stop or cure the destructive processes in the lungs with currently existing drugs.
The main drugs used to treat COPD are:

Bronchodilators
Bronchodilators, used to treat COPD, relax the smooth muscles of the bronchi, thereby expanding their lumen and facilitating the passage of air on exhalation. All bronchodilators have been shown to increase exercise tolerance.
Bronchodilators include:
- Short-acting beta stimulants ( salbutamol, fenoterol).
- Long acting beta stimulants ( salmoterol, formoterol).
- Short acting anticholinergics ipratropium bromide - atrovent).
- Long acting anticholinergics ( tiotropium bromide - spiriva).
- Xanthines ( eufillin, theophylline).
Almost all existing bronchodilators are used in inhaled form, which is more preferable than oral administration. There are different types of inhalers (metered dose aerosol, powder inhalers, breath-activated inhalers, liquid nebulizer forms). In severely ill patients, as well as in patients with intellectual disabilities, it is better to carry out inhalation through a nebulizer.
This group of drugs is the main one in the treatment of COPD; it is used at all stages of the disease as monotherapy or (more often) in combination with other drugs. For permanent therapy, the use of long-acting bronchodilators is preferable. If it is necessary to prescribe short-acting bronchodilators, combinations are preferred fenoterol and ipratropium bromide (berodual).
Xanthines (eufillin, theophylline) are used in the form of tablets and injections, have many side effects, and are not recommended for long-term treatment.

Glucocorticosteroid hormones (GCS)
GCS are a powerful anti-inflammatory agent. They are used in patients with a severe and extremely severe degree, and are also prescribed in short courses for exacerbations in the moderate stage.
The best form of application is inhaled corticosteroids ( beclomethasone, fluticasone, budesonide). The use of such forms of corticosteroids minimizes the risk of systemic side effects of this group of drugs, which inevitably occur when taken orally.
GCS monotherapy is not recommended for patients with COPD, more often they are prescribed in combination with long-acting beta-agonists. The main combination drugs: formoterol + budesonide (symbicort), salmoterol + fluticasone (seretide).
In severe cases, as well as during an exacerbation, systemic corticosteroids can be prescribed - prednisolone, dexamethasone, kenalog. Long-term therapy with these drugs is fraught with the development of severe side effects (erosive and ulcerative lesions of the gastrointestinal tract, Itsenko-Cushing's syndrome, steroid diabetes, osteoporosis, and others).
Bronchodilators and corticosteroids (and more often a combination of them) are the main most affordable drugs that are prescribed for COPD. The doctor selects the treatment regimen, doses and combinations individually for each patient. In the choice of treatment, not only recommended GOLD schemes for different clinical groups are important, but also the social status of the patient, the cost of drugs and its availability for a particular patient, the ability to learn, and motivation.
Other drugs used in COPD
 Mucolytics(sputum thinning agents) are prescribed in the presence of viscous, difficult to expectorate sputum.
Mucolytics(sputum thinning agents) are prescribed in the presence of viscous, difficult to expectorate sputum.
Phosphodiesterase-4 inhibitor roflumilast (Daxas) is a relatively new drug. It has a prolonged anti-inflammatory effect, is a kind of alternative to GCS. It is used in tablets of 500 mg 1 time per day in patients with severe and extremely severe COPD. Its high efficiency has been proven, but its use is limited due to the high cost of the drug, as well as a rather high percentage of side effects (nausea, vomiting, diarrhea, headache).
There are studies that the drug fenspiride (Erespal) has an anti-inflammatory effect similar to corticosteroids, and can also be recommended for such patients.
Of the physiotherapeutic methods of treatment, the method of intrapulmonary percussion ventilation of the lungs is gaining popularity: a special device generates small volumes of air that are supplied to the lungs with quick shocks. From such a pneumomassage, the collapsed bronchi are straightened and the ventilation of the lungs is improved.
Treatment of exacerbation of COPD
The goal of exacerbation treatment is to manage the current exacerbation as much as possible and prevent future exacerbations. Depending on the severity, exacerbations can be treated on an outpatient basis or in a hospital.

Basic principles of treatment of exacerbations:
- It is necessary to correctly assess the severity of the patient's condition, exclude complications that can be disguised as exacerbations of COPD, and promptly send for hospitalization in life-threatening situations.
- With an exacerbation of the disease, the use of short-acting bronchodilators is preferable to long-acting ones. Doses and frequency of administration, as a rule, increase compared to usual. It is advisable to use spacers or nebulizers, especially in critically ill patients.
- With insufficient effect of bronchodilators, intravenous administration of aminophylline is added.
- If monotherapy was previously used, a combination of beta-stimulants with anticholinergics (also short-acting) is used.
- In the presence of symptoms of bacterial inflammation (the first sign of which is the appearance of purulent sputum), broad-spectrum antibiotics are prescribed.
- Connection of intravenous or oral administration of glucocorticosteroids. An alternative to the systemic use of corticosteroids is the inhalation of pulmicort through a nebulizer 2 mg twice a day after berodual inhalations.
- Dosed oxygen therapy in the treatment of patients in a hospital through nasal catheters or a Venturi mask. The oxygen content in the inhaled mixture is 24-28%.
- Other activities - maintaining water balance, anticoagulants, treatment of concomitant diseases.
Caring for patients with severe COPD
As already mentioned, COPD is a disease that is steadily progressing and inevitably leads to the development of respiratory failure. The speed of this process depends on many things: the patient's refusal to smoke, adherence to treatment, the patient's financial capabilities, his memory abilities, and the availability of medical care. Starting with a moderate degree of COPD, patients are referred to MSEC to receive a disability group.

With an extremely severe degree of respiratory failure, the patient cannot even perform normal household activities, sometimes he cannot even take a few steps. These patients require constant care. Inhalations for seriously ill patients are carried out only with the help of a nebulizer. Significantly facilitates the condition of many hours of low-flow oxygen therapy (more than 15 hours a day).
For these purposes, special portable oxygen concentrators have been developed. They do not require filling with pure oxygen, but concentrate oxygen directly from the air. Oxygen therapy increases the life expectancy of such patients.
COPD prevention
COPD is a preventable disease. It is important that the level of COPD prevention depends very little on physicians. The main measures should be taken either by the person himself (quitting smoking) or by the state (anti-smoking laws, improving the environment, promoting and stimulating a healthy lifestyle). It has been proven that COPD prevention is economically beneficial by reducing the incidence and reducing the disability of the working population.
Video: COPD in the program “Live healthy”
Video: what is COPD and how to detect it in time