Diagnosis of ICD 167.8 what. Dyscirculatory encephalopathy - an overview of information. Pathogenesis of discirculatory encephalopathy
Dyscirculatory encephalopathy is an extremely common disease that occurs in almost every person with hypertension.
Deciphering the scary words is quite simple. The word "dyscirculatory" means disorders of blood circulation through the vessels of the brain, while the word "encephalopathy" literally means the suffering of the head. Thus, discirculatory encephalopathy is a term denoting any problems and violations of any functions due to impaired blood circulation through the vessels.
Information for doctors: the code of discirculatory encephalopathy according to ICD 10 is the most often used code I 67.8.
Causes
There are not so many reasons for the development of discirculatory encephalopathy. The main ones are hypertonic disease and atherosclerosis. Less often, discirculatory encephalopathy is spoken of with a tendency to a decrease in pressure.
Constant drops blood pressure, the presence of a mechanical obstruction to blood flow in the form of atherosclerotic plaques creates prerequisites for chronic insufficiency of blood flow to various structures of the brain. Lack of blood flow means insufficient nutrition, untimely elimination of metabolic products of brain cells, which gradually leads to disruption of various functions.
It should be said that frequent pressure drops lead most quickly to encephalopathy, while constantly high or constantly low level pressure will lead to encephalopathy over a longer period of time.
A synonym for discirculatory encephalopathy is chronic insufficiency cerebral circulation, which, in turn, means a long-term formation of persistent disorders of the brain. Thus, the presence of the disease should be discussed only with reliably present vascular diseases for many months and even years. Otherwise, one should look for another reason for the existing violations.
Symptoms
What should you pay attention to in order to suspect the presence of discirculatory encephalopathy? All the symptoms of the disease are quite nonspecific and usually include "everyday" symptoms that can occur in healthy person... That is why patients seek medical care not immediately, only when the severity of the symptoms begins to interfere with a normal life.
According to the classification, in discirculatory encephalopathy, several syndromes should be distinguished that combine the main symptoms. When making a diagnosis, the doctor also takes out the presence of all syndromes, indicating their severity.
- Cephalgic Syndrome. Includes complaints such as headaches (mainly in the occipital and temporal regions), pressing sensations in the eyes, nausea with headache, tinnitus. Also in relation to this syndrome should be attributed to any discomfort associated with the head.
- Vestibulo-coordinating violations. Includes dizziness, throwing when walking, feeling unsteady when changing body position, blurred vision with sudden movements.
- Astheno-neurotic syndrome. Includes mood swings, consistently low mood, tearfulness, feelings of anxiety. With pronounced changes, it should be differentiated from more serious psychiatric diseases.
- Dyssomnic syndrome, including any sleep disorders (including light sleep, "insomnia", etc.).
- Cognitive impairment. They combine memory impairments, decreased concentration, distraction, etc. Dementia of various etiologies (including Alzheimer's disease) should be excluded if the severity of the disorders and the absence of other symptoms.
Dyscirculatory encephalopathy 1, 2 and 3 degrees (description)
Also, in addition to syndromic classification, there is a gradation according to the degree of encephalopathy. So, there are three degrees. Dyscirculatory encephalopathy of 1 degree means the most initial, transient changes in brain function. Dyscirculatory encephalopathy of the 2nd degree indicates persistent disorders, which, however, only affect the quality of life, usually without leading to a gross decrease in working capacity and self-care. Dyscirculatory encephalopathy of grade 3 means persistent gross disorders, often leading to disability and a person.
According to statistics, the diagnosis of grade 2 discirculatory encephalopathy is one of the most common neurological diagnoses.
Author's video
Diagnostics
Only a neurologist can diagnose the disease. To make a diagnosis, it is required that, upon examination, the neurological status of the revitalization of reflexes, the presence of reflexes of oral automatism, pathological reflexes, changes in the performance of coordination tests, signs of a violation of the vestibular apparatus are required. You should also pay attention to the presence of nystagmus, deviation of the tongue away from the midline and some other specific signs that speak of the suffering of the cerebral cortex and a decrease in its inhibitory effect on spinal cord and the reflex sphere.
Only in addition to neurological examination are additional methods research - REG, MRI and others. By rheoencephalography, it is possible to identify violations of vascular tone, asymmetry of blood flow. MR signs of encephalopathy include the presence of calcifications (atherosclerotic plaques), hydrocephalus, and disseminated hypodense vascular inclusions. Usually, MR signs are detected in the presence of grade 2 or 3 discirculatory encephalopathy.
Treatment
Treatment should be comprehensive. The main factor in successful therapy is the normalization of the causes that caused the development of the disease. It is necessary to normalize blood pressure, stabilize lipid metabolism. Treatment standards for discirculatory encephalopathy also include the use of drugs that normalize the metabolism of brain cells and vascular tone... The drugs in this group include Mexidol, Cytoflavin, Gliatilin, Sermion. 
The choice of other medicines depends on the presence and severity of certain syndromes:
- With severe cephalgic syndrome and existing hydrocephalus, they resort to specific diuretics (diacarb, glycerin mixture), venotonics (detralex, phlebodia).
- Vestibulo-coordinating disorders should be eliminated with drugs that normalize blood flow in the vestibular structures (cerebellum, inner ear). The most commonly used are betahistine (betaserc, vestibo, tagista), vinpocetine (cavinton).
- Astheno-neurotic syndrome, as well as sleep disturbances, are eliminated by prescribing light sedatives (glycine, tenoten, etc.). With pronounced manifestations, they resort to prescribing antidepressants. Should also adhere to proper hygiene sleep, normalization of the work-rest regimen, limitation of psycho-emotional stress.
- For cognitive impairment, nootropic drugs are used. The most commonly used drugs are piracetam, including in combination with a vascular component (fezam), as well as more modern drugs such as phenotropil, pantogam. If you have severe concomitant diseases, you should give preference to safe herbal drugs (for example, tanakan).
Treatment with folk remedies for discirculatory encephalopathy usually does not justify itself, although it can lead to a subjective improvement in well-being. This is especially true for patients who are distrustful of the reception drugs... In advanced cases, such patients should be oriented at least to receive constant antihypertensive therapy, and in treatment, parenteral methods of treatment should be used, which, in the opinion of such patients, have a better effect than tablet forms of drugs.
Prophylaxis
There are not so many methods of preventing the disease, but at the same time, standard treatment will not do without prevention. To prevent the development of discirculatory encephalopathy, as well as to reduce its manifestations, the level of blood pressure, the content of cholesterol and its fractions should be constantly monitored. You should also avoid psycho-emotional overload.
With existing discirculatory encephalopathy, you should also regularly (1-2 times a year) undergo a full course of vasoactive, neuroprotective, nootropic therapy in a day or round-the-clock hospital to prevent the progression of the disease. Be healthy!
What if the doctor issued a conclusion after the MRI, and it says that the code of my disease is 167.8. What does this mean and what to think at all? And then it is incomprehensible to cry or rejoice.
Author of the publication
Achievement received on 09/30/2018
Title: Reliable Bearded Man
Achievement received on 7/22/2018
First of all, I would like to draw your attention to the fact that code 167.8 is only a classification according to the ICD. As a rule, next to this figure, they write a clarification of what kind of disease and in what state of development it is now (for example, they can write “deterioration”).
Here's what the ICD is if you don't know:
According to the ICD-10 classification, you definitely do not have these diseases:
- subarchnoid hemorrhage (corresponds to code 160);
- intracerebral hemorrhage (this is paragraph 161);
- other types of large cranial hemorrhage (code 162);
- cerebral infarction;
- stroke;
- blockage or stenosis that or does not cause a heart attack;
I have listed all these ailments because they are related to the brain and are classified near the ICD-10 code 167.8. The problem is that the following definition matches this value:
Other cerebrovascular diseases
This is a very vague term. But at least now you know what diseases of the brain this diagnosis probably does not correspond to.
By the way, I have come across other diagnoses on some resources, for example, this one:
Other specified cerebral vascular lesions
There is also a reduction in DEP 2, which corresponds to discirculatory encephalopathy. This is a brain disease when the structure of tissues is disturbed. The consequences can be as follows:
- dementia;
- impaired coordination and ability to move normally;
- inhibition of speech;
- a person becomes slow, ordinary things are given to him with difficulty (I do not know what to call it medically).
If I am not mistaken, with a diagnosis of 167.8, they can even get a disability. I would advise you to go to the doctor again, so that he will probably tell you what kind of diagnosis you have, but only in human language, and not with the help of these codes and abbreviations.
According to international classification diseases of the ICD of the 10th revision (figure 10) this code is placed in the class of diseases of the circulatory system in relation to the defeat of the cerebral vessels.
The chain in the classification looks like this:
1 Classes of ICD-10
2 I00-I99 Diseases of the circulatory system
3 I60-I69 Cerebrovascular diseases
4 I67 Other cerebrovascular diseases
5 I67.8 Other specified cerebral vascular lesions
the decoding of the online classifier is as follows:
Explanation of the disease with code I67.8 in the MBK-10 reference book:
Acute cerebrovascular insufficiency NOS Cerebral ischemia (chronic)
You do not need to be afraid, but you need to monitor your health, avoid stress, smoking, low-quality alcohol, overeating, monitor blood pressure, and not bring yourself to shortness of breath. Such a diagnosis is made if the lumen in the vessel is narrowed and, accordingly, cerebral blood flow is reduced, the danger arises from the fact that there is a possibility of closure of the lumen by an atherosclerotic plaque or thrombus, a cerebral circulation disorder will occur, which will be classified as ischemic stroke, or the thinning of the vessel wall will lead to its disruption. integrity and cerebral hemorrhage occurs, such an event is called a hemorrhagic stroke or apoplexy.
The clinical picture with cerebrovascular disease is as follows
there is a decrease in working capacity and increased fatigue, there is a sharp change in mood, alternation of excitement with inhibition, sleep is disturbed or a person gets up in the middle of the night and no longer lies down. After this, symptoms of cognitive impairment may appear - memory loss, thinking slows down, later - persistent headaches, constant tinnitus, impaired gait, speech, sensitivity, vision.
If such symptoms disappear within 48 hours, then they speak of a transient violation of cerebral circulation. If the symptoms persist longer, then it is a stroke.
RCHRH (Republican Center for Healthcare Development of the Ministry of Health of the Republic of Kazakhstan)
Version: Clinical Protocols of the Ministry of Health of the Republic of Kazakhstan - 2014
general information
Short description
The concept of "chronic cerebral ischemia" includes: "discirculatory encephalopathy", "chronic ischemic brain disease", "vascular encephalopathy", "cerebrovascular insufficiency", "atherosclerotic encephalopathy". Of the above names, the term "discirculatory encephalopathy" is most often encountered in modern medicine.
Protocol users: neuropathologist, therapist, general practitioner (family doctor), emergency and emergency medical doctor, psychotherapist, speech therapist, physiotherapist, physiotherapy exercises and sports, psychologist, social worker with higher education, social worker with secondary education, medical assistant.
Classification
Diagnostics
II. METHODS, APPROACHES AND PROCEDURES OF DIAGNOSTICS AND TREATMENT
- determination of glycated glucose.
- Doppler ultrasound of the vessels of the brain and brachiocephalic trunk.
- sensory disturbances (visual, auditory, etc.).
- paroxysmal conditions (with insufficient blood circulation in the basin of the vertebrobasilar system).
- determination of urea, creatinine, electrolytes (sodium, potassium, calcium) - identification of violations electrolyte balance associated with the use of dehydrating therapy.
— X-ray of organs chest (2 projections): changes in the configuration of the heart with valvular defects, expansion of the borders of the heart in the presence of hypertrophic and dilated cardiomyopathy, the presence of pulmonary complications (congestive, aspiration pneumonia, thromboembolism, etc.).
Differential diagnosis
Differential diagnosis:
Undergo treatment in Korea, Israel, Germany, USA

Undergo treatment in Korea, Turkey, Israel, Germany and other countries
Choose a foreign clinic
Free consultation on treatment abroad! Leave a request below
Get advice on medical tourism
Treatment
2) Diet: table number 10 (restriction of salt, liquid).
- glycine, 20 mg / kg body weight (average 1-2 g / day) sublingually for 7-14 days
- tolperisone hydrochloride, 50-150 mg 2 times a day for a long time (under the control of blood pressure).
- Vinpocetine - 5-10 mg tablets 3 times a day / day; 5.10 mg tablets, 2 ml ampoules;
- nicergoline - 10 mg tablets 3 times a day, tablets; ampoules 5 mg, tablets 5, 10 mg;
- bencyclane fumarate - in / in slowly 50-100 mg / day, ampoules; 100 mg 2 times / day for 2-3 months, tablets. Ampoules of 2 ml, tablets of 100 mg.
- tolperisone - 100 mg / day - ampoules, 50 mg tablets - 50-150 mg / day.
Relief of epileptic seizure or status epilepticus is carried out according to the clinical protocol “Epilepsy. Status epilepticus ".
- gabapentin - capsules of 100, 300, 400 mg.
- Tolperisone - 50 mg tablets.
Medical treatment provided at the ambulance stage emergency care:
- Epileptic seizures (see clinical protocol"Epilepsy", "Status epilepticus").
The use of a special system of exercises to restore impaired motor functions and the formation of a compensatory stereotype.
Constant stimulation of motor and mental activity.
- Sanitary educational work aimed at educational, agitation and propaganda activities that form healthy image life.
Nowadays, the diagnosis of grade 2 discirculatory encephalopathy is made, one might say, everywhere. Young and old people on all continents equally suffer from this disease, and it is the Caucasian race that is prone to developing the highest stage of the disease to a greater extent. With prolonged neglect, if not treated, chronic encephalopathy will lead to the risk of ischemic and even hemorrhagic stroke.
What is this disease?
The manifestations of such a disease are associated with several factors, a number of which are considered congenital abnormalities of the blood supply to the brain, and some are acquired due to the action of a combination of factors.
According to statistics, after 70 years, the risk of developing discirculatory encephalopathy in the second or third degree increases by about three times, while the chance of acquiring disability increases by 5-6 times.
Atherosclerotic (resulting from atherosclerosis) or discirculatory encephalopathy in general is considered a diffuse focal disturbance of the blood supply to the brain. As a result, the work of nerve cells is disrupted. Responsible for the functioning of certain body systems. And if a person is not helped in time by providing treatment at the first stage or suppressing symptoms at an early stage of development, the prognosis is disappointing: disability of 1-2 groups.
Causes of encephalopathy
As far as doctors have been able to identify to date, grade 2 discirculatory encephalopathy occurs and develops with insufficient blood supply to the foci of the brain. This can be influenced by the following reasons:
- Atherosclerosis of blood vessels, arteries.
- Arterial hypertension, a sharp spasm of blood vessels due to a jump in blood pressure.
- Venous thrombosis.
- The presence of a high level of cholesterol on the walls of blood vessels - often the reasons lie in unhealthy diet and excess weight.
- The ingress of toxins into the blood - of a bacterial type, as in measles or botulism, illness internal organs, or chemical / organic. For example, improper treatment, alcoholism, poisoning, smoking.
- Osteochondrosis of the cervical spine, pinching the vessel and causing the symptoms of this brain disease.
- Vegetovascular dystonia also significantly affects the appearance of discirculatory encephalopathy.
- Vasculitis is an inflammation of blood vessels.
In addition, one of the most negative factors that can be written down as the causes of the disease already at its first stage is stress.
Frequent psycho-emotional stress, disorders lead to the fact that our brain and blood vessels in it experience excessive shock, wear out prematurely.
It is atherosclerosis of all of the above that is the most common factor in the development of discirculatory encephalopathy. Often 2-3 more reasons join it.
Symptoms of encephalopathy
It is difficult to say unequivocally how exactly encephalopathy of the 2nd degree manifests itself, because many symptoms at the initial stage are identical to the manifestations of other brain diseases. Therefore, it is difficult to build a prognosis of the disease.
So, distinguish the following manifestations, more or less requiring treatment:
- Disorders of an emotional and mental nature are characteristic of stage 2, they do not appear earlier.
- Memory problems - in particular, amnesia for recent events.
- Lethargy, apathy, complete lack of interest in a hobby.
- Severe headaches - as focal symptoms.
- Absent-mindedness, sclerosis.
- Inability to perceive large amounts of information.
- Nausea and weakness, dizziness.
It is worth noting that, to a greater extent, symptoms begin to appear towards night, after a long day or after exhausting stress. And if the duration of these symptoms lasts about six months or more, they speak of stage 2 of the development of discirculatory encephalopathy, and after the diagnosis, adequate treatment is prescribed.
Already during treatment on an outpatient or inpatient basis, doctors recommend to issue a disability. Since the brain is severely atrophied, the patient will not be able to return to his previous work.
Encephalopathy treatment
This brain disorder is treated in the same way as similar diseases. Hypertensive, hypertensive, venous encephalopathy, and dyscirculatory require that a complex, mixed with drug treatment... In order to diagnose and confirm the state of the brain, to assess the size of the lesions of encephalopathy, a number of examinations are carried out:
- Positron emission tomography.
- Electroencephalography.
- Magnetic resonance imaging.
- CT scan.
- X-ray of the cervical spine (to exclude osteochondrosis).
- Biochemical analysis blood, etc.
According to the results of the examination, it becomes clear what scale the brain area is and at what stage of the lesion is, therefore, how long the treatment will take and what degree of disability will be assigned (usually at least group II).
In addition to eliminating the pathology of the brain itself, an integrated approach is required to eliminate the symptoms arising from discirculatory encephalopathy. A detailed examination is performed by a neurologist, as well as a cardiologist, a therapist and, if necessary, a psychiatrist.
Treatment includes:
- Restoration of blood circulation in the tissues of the brain. Usually, nootropic drugs are used in combination with blood pressure normalizers - Cavinton, Nootropil, Tanakan, etc.
- Drugs that lower platelets and lower blood viscosity, such as Tiklid or Instenon.
- Tablets and injections that reduce vascular hypertension by the method of potassium antagonists and beta-blockers. For example, Finoptin or Nimopidin.
- Therapy aimed at achieving a lipid-lowering effect.
As well as medicinal methods physiotherapy based on electrophoresis of magnesium sulfate, galvanic collars, hyperbaric oxygenation is widely recommended. In the rarest cases, when it comes to transient ischemic attack or hemorrhage (hemorrhage), as well as severe cerebral edema, surgical intervention is required.
Dyscirculatory encephalopathy is an extremely common disease that occurs in almost every person with hypertension.
Deciphering the scary words is quite simple. The word "dyscirculatory" means disorders of blood circulation through the vessels of the brain, while the word "encephalopathy" literally means the suffering of the head. Thus, discirculatory encephalopathy is a term denoting any problems and violations of any functions due to impaired blood circulation through the vessels.
Information for doctors: the code of discirculatory encephalopathy according to ICD 10 is the most often used code I 67.8.
Causes
There are not so many reasons for the development of discirculatory encephalopathy. The main ones are hypertension and atherosclerosis. Less often, discirculatory encephalopathy is spoken of with a tendency to a decrease in pressure.
Constant drops in blood pressure, the presence of a mechanical barrier to blood flow in the form of atherosclerotic plaques create the prerequisites for chronic insufficiency of blood flow to various structures of the brain. Lack of blood flow means insufficient nutrition, untimely elimination of metabolic products of brain cells, which gradually leads to disruption of various functions.
It should be said that frequent pressure drops lead to encephalopathy most quickly, while a constantly high or constantly low level of pressure will lead to encephalopathy over a longer period of time.
A synonym for discirculatory encephalopathy is chronic cerebral circulatory failure, which, in turn, means a long-term formation of persistent brain disorders. Thus, the presence of the disease should be discussed only with reliably present vascular diseases for many months and even years. Otherwise, one should look for another reason for the existing violations.
Symptoms
What should you pay attention to in order to suspect the presence of discirculatory encephalopathy? All the symptoms of the disease are quite nonspecific and usually include "everyday" symptoms that can occur in a healthy person. That is why patients do not seek medical help immediately, only when the severity of symptoms begins to interfere with a normal life.
According to the classification, in discirculatory encephalopathy, several syndromes should be distinguished that combine the main symptoms. When making a diagnosis, the doctor also takes out the presence of all syndromes, indicating their severity.
- Cephalgic Syndrome. Includes complaints such as headaches (mainly in the occipital and temporal regions), pressing sensations in the eyes, nausea with headache, tinnitus. Also in relation to this syndrome should be attributed to any discomfort associated with the head.
- Vestibulo-coordinating violations. Includes dizziness, throwing when walking, feeling unsteady when changing body position, blurred vision with sudden movements.
- Astheno-neurotic syndrome. Includes mood swings, consistently low mood, tearfulness, feelings of anxiety. With pronounced changes, it should be differentiated from more serious psychiatric diseases.
- Dyssomnic syndrome, including any sleep disorders (including light sleep, "insomnia", etc.).
- Cognitive impairment. They combine memory impairments, decreased concentration, distraction, etc. Dementia of various etiologies (including) should be excluded if the severity of the disorders and the absence of other symptoms.
Dyscirculatory encephalopathy 1, 2 and 3 degrees (description)
Also, in addition to syndromic classification, there is a gradation according to the degree of encephalopathy. So, there are three degrees. Dyscirculatory encephalopathy of 1 degree means the most initial, transient changes in brain function. Dyscirculatory encephalopathy of the 2nd degree indicates persistent disorders, which, however, only affect the quality of life, usually without leading to a gross decrease in working capacity and self-care. Dyscirculatory encephalopathy of grade 3 means persistent gross disorders, often leading to disability and a person.
According to statistics, the diagnosis of grade 2 discirculatory encephalopathy is one of the most common neurological diagnoses.
Author's video
Diagnostics
Only a neurologist can diagnose the disease. To make a diagnosis, it is required that, upon examination, the neurological status of the revitalization of reflexes, the presence, pathological reflexes, changes in performance, signs of a violation of the vestibular apparatus are required. You should also pay attention to the presence of nystagmus, deviations of the tongue away from the midline and some other specific signs that speak of the suffering of the cerebral cortex and a decrease in its inhibitory effect on the spinal cord and the reflex sphere.
Only in addition to neurological examination are additional research methods - and others. By rheoencephalography, it is possible to identify violations of vascular tone, asymmetry of blood flow. MR signs of encephalopathy include the presence of calcifications (atherosclerotic plaques), hydrocephalus, and disseminated hypodense vascular inclusions. Usually, MR signs are detected in the presence of grade 2 or 3 discirculatory encephalopathy.
Treatment
Treatment should be comprehensive. The main factor in successful therapy is the normalization of the causes that caused the development of the disease. It is necessary to normalize blood pressure, stabilize lipid metabolism. Treatment standards for discirculatory encephalopathy also include the use of drugs that normalize brain cell metabolism and vascular tone. The drugs in this group include sermion. 
The choice of other medicines depends on the presence and severity of certain syndromes:
- With severe cephalgic syndrome and existing hydrocephalus, they resort to specific diuretics (diacarb, glycerin mixture), venotonics (detralex, phlebodia).
- Vestibulo-coordinating disorders should be eliminated with drugs that normalize blood flow in the vestibular structures (cerebellum, inner ear). The most commonly used are betahistine (, vestibo, tagista), vinpocetine ().
- Astheno-neurotic syndrome, as well as sleep disturbances, are eliminated by prescribing light sedatives (glycine, tenoten, etc.). With pronounced manifestations, they resort to prescribing antidepressants. You should also adhere to proper sleep hygiene, normalization of the work-rest regimen, and limitation of psycho-emotional stress.
- For cognitive impairment, nootropic drugs are used. The most commonly used drugs are piracetam, including in combination with a vascular component (fezam), as well as more modern drugs such as phenotropil, pantogam. If you have severe concomitant diseases, you should give preference to safe herbal drugs (for example, tanakan).
Treatment with folk remedies for discirculatory encephalopathy usually does not justify itself, although it can lead to a subjective improvement in well-being. This is especially true for patients who are suspicious of taking medications. In advanced cases, such patients should be oriented at least to receive constant antihypertensive therapy, and in treatment, parenteral methods of treatment should be used, which, in the opinion of such patients, have a better effect than tablet forms of drugs.
Prophylaxis
There are not so many methods of preventing the disease, but at the same time, standard treatment will not do without prevention. To prevent the development of discirculatory encephalopathy, as well as to reduce its manifestations, the level of blood pressure, the content of cholesterol and its fractions should be constantly monitored. You should also avoid psycho-emotional overload.
With existing discirculatory encephalopathy, you should also regularly (1-2 times a year) undergo a full course of vasoactive, neuroprotective, nootropic therapy in a day or round-the-clock hospital to prevent the progression of the disease. Be healthy!
Catad_tema Chronic cerebral ischemia - articles
Modern approach to the diagnosis and treatment of chronic cerebral ischemia
Published in the journal:"RUSSIAN MEDICAL JOURNAL" Neurology; TOM 18; No. 6; 2010; pp. 1-7.
Dr. med. S.P. Markin
Voronezh State medical Academy them. N.N. Burdenko
In recent years, an aging population has been observed in the world, primarily due to a decrease in the birth rate. In the figurative expression of V. Konyakhin, “young people come and go, but old people remain”. So, in 2000 there were about 400 million people over the age of 65 all over the world. However, this age group is expected to increase to 800 million by 2025.
External changes nervous system occupy a leading place among this contingent of people. In this case, the most common are lesions of the vessels of the brain, leading to its ischemia, i.e. the development of discirculatory encephalopathy (DE).
DE is a syndrome of progressive multifocal or diffuse brain damage, manifested by clinical neurological, neuropsychological and / or mental disorders, caused by chronic cerebral vascular insufficiency and / or repeated episodes of acute cerebrovascular accidents.
V modern classification ICD-10 lacks the term "discirculatory encephalopathy". Instead of the previous diagnosis, it is recommended to use the following disease codes:
167.2 Cerebral atherosclerosis
167.3 Progressive vascular leukoencephalopathy
167.4 Hypertensive encephalopathy
167.8 Other specified vascular lesions of the brain.
However, the term "discirculatory encephalopathy" is traditionally used among neurologists in our country. DE is a heterogeneous condition that can have different etiology... The greatest etiological significance in the development of DE are:
- atherosclerosis (atherosclerotic DE);
- arterial hypertension(hypertensive DE);
- their combination (mixed DE).
In atherosclerotic DE, damage to large main and intracranial vessels (stenosis) prevails. Moreover, in initial stages diseases, stenosing changes in one (less often two) major vessels are revealed, while in the advanced stages of the process, most (or all) of the major arteries of the head are often changed. A decrease in blood flow occurs with hemodynamically significant stenosis (narrowing of 70-75% of the arterial lumen area) and then increases in proportion to the degree of narrowing. At the same time, the state of the intracranial vessels (development of the collateral circulation network) plays an important role in the mechanisms of compensation of cerebral circulation.
In hypertensive DE, the main pathological processes are observed in the smaller branches of the cerebral vascular system (perforating arteries) in the form of lipohyalinosis and fibrinoid necrosis.
The main pathogenetic mechanisms of DE development:
- chronic ischemia;
- "incomplete stroke";
- completed stroke.
The main morphological changes in DE:
- focal changes brain (postischemic cysts due to lacunar stroke);
- diffuse changes in white matter (leukoaraiosis);
- cerebral atrophy (cerebral cortex and hippocampus).
The defeat of small cerebral arteries (40-80 microns in diameter) is one of the main causes of lacunar stroke (up to 15 mm in diameter). Depending on the location and size, lacunar infarctions can manifest themselves as characteristic neurological syndromes or be asymptomatic (in functionally "mute" zones - the shell, white matter of the cerebral hemispheres). With the multiple nature of deep lacunae, a lacunar state is formed (Fig. 1)
Rice. 1. Multiple lacunar foci in the basin of the right middle cerebral artery, according to MRI of the brain
Leukoaraiosis is visualized as bilateral focal or diffuse areas of reduced density in the white matter on computed tomography and T1-weighted images on magnetic resonance imaging, or as areas of increased density on T2-weighted images on magnetic resonance imaging (Fig. 2).
Rice. 2. Severe leukoaraiosis
The widespread involvement of small arteries causes several main types of changes:
- diffuse bilateral white matter lesion (leukoencephalopathy) - leukoencephalopathic (Binswanger's) variant of DE;
- multiple lacunar infarctions - a lacunar variant of DE.
In the clinical picture of DE, a number of basic syndromes are distinguished:
- vestibular-atactic (dizziness, staggering, unsteadiness when walking);
- pyramidal (revitalization of tendon reflexes with expansion of reflexogenic zones, anisoreflexia, sometimes clonuses of the feet);
- amiostatic (trembling of the head, fingers, hypomimia, muscle rigidity, slow motion);
- pseudobulbar (blurred speech, "violent" laughter and crying, choking when swallowing);
- psychopathological (depression, impaired cognitive functions).
Dizziness
- the most common complaint of patients with DE (occurs in 30% of cases). Dizziness in the elderly is caused by the following reasons and their combinations:
- age-related changes in the sensory system;
- a decrease in the compensatory capabilities of the central mechanisms of balance;
- cerebrovascular insufficiency with predominantly lesion of the vertebrobasilar system.
In this case, the leading role is played by the defeat of the vestibular nuclei of the trunk or vestibulo-cerebellar connections. The so-called peripheral component, due to atherosclerotic lesions of the vessels of the inner ear, is of certain importance.
Movement disorders in old age (up to 40% of cases) are caused by damage to the frontal lobes and their connections with subcortical formations.
Major movement disorders in the elderly:
- "frontal gait disorder" (frontal dysbasia);
- "frontal imbalance" (frontal astasia);
- "subcortical imbalance" (subcortical astasia);
- violation of the initiation of walking;
- "careful" (or uncertain) walking.
Movement disorders are often accompanied by falls. According to a number of researchers, falls at least once a year are observed in 30% of people aged 65 and over, while in about half of cases this happens more than once a year. The likelihood of falls increases in the presence of impaired cognitive functions, depression, as well as patients taking antidepressants, benzodiazepine tranquilizers, antihypertensive drugs.
The prevalence of depression among patients with DE (according to the Compass study) is more than 50% (with a third of patients having severe depressive disorders).
Peculiarities clinical picture depression in the elderly:
- the predominance of somatic symptoms of depression over mental;
- severe disturbance of vital functions, especially sleep;
- mask mental symptoms depression can be anxiety, irritability, "grumpiness", which are often viewed by others as features of old age;
- the cognitive symptoms of depression are often assessed in terms of senile forgetfulness;
- significant fluctuations in symptoms;
- incomplete compliance with the criteria for a depressive episode (individual symptoms of depression);
- a close relationship between exacerbations of somatic illness and depression;
- the presence of general symptoms of depression and somatic illness.
According to a number of epidemiological studies, from 25 to 48% of people over 65 years of age experience a variety of sleep disorders. At the same time, sleep disorders are most often manifested in the form of insomnia: presomnic disorders - 70%, intrasomnic disorders - 60.3% and postsomnic disorders - 32.1% of cases.
The main manifestations of sleep disorders in the elderly:
- persistent complaints of insomnia;
- constant difficulty falling asleep;
- superficial and intermittent sleep;
- the presence of vivid, multiple dreams, often painful content;
- early awakenings;
- a feeling of anxious anxiety on awakening;
- difficulty or inability to fall asleep again;
- lack of feeling of rest from sleep.
Cognitive impairment in depression
due to redistribution of attention, low self-esteem and mediator disorders. Cognitive dysfunctions in depression are characterized by:
- acute / subacute onset of the disease;
- rapid progression of symptoms;
- indications of previous mental pathology;
- persistent complaints about a decrease in intellectual abilities;
- lack of effort when performing tests ("don't know");
- variability of test execution;
- Attracting attention improves test performance;
- memory of recent and distant events suffers equally.
However, in depression, the subjective assessment of cognitive abilities and the degree of social maladjustment, as a rule, do not correspond to the objective data of cognitive tests. A decrease in the severity of emotional disturbances leads to a regression of cognitive disorders associated with depression. Nevertheless, as a result of numerous studies of the hippocampus area in patients with large depressive disorder Evidence has accumulated that atrophy occurs with depression. Recently there have even been reports of hippocampal atrophy after the first depressive episode [J.P. Olier, France, 2007]. In addition, according to the Chicago experts from the Rush Alzheimers Disease Center, prolonged depression can lead to the development of Alzheimer's disease. So, with each new sign of depression, the likelihood of developing Alzheimer's disease increases by 20%.
Moderate cognitive impairment
(MCI) with DE (according to the study "Prometheus") occurs in 56% of cases. The relationship between moderate cognitive disorders detected in a patient and DE may be evidenced by:
- the predominance of regulatory cognitive impairments associated with dysfunction of the frontal lobes (impaired planning, organization and control of activities, decreased speech activity, moderate secondary memory impairment with relatively intact recognition);
- a combination of cognitive impairments with affective disorders (apathy, depression, irritability), as well as focal neurological symptoms, including those indicative of suffering in the deep parts of the brain (dysarthria, impaired walking and postural stability, extrapyramidal signs, neurogenic urination disorders).
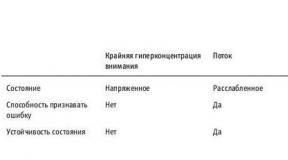
Table 1 shows the comparative characteristics of the "Alzheimer's type" MCR and DE with MCR.
Table 1. Distinctive characteristics of Alzheimer's type MCR and DE with MCR
| Signs | UKR Alzheimer's type | DE with UKR |
| Vascular risk factors (arterial hypertension, diabetes, obesity, etc.) | ± | ++ |
| Signs of cerebrovascular disease (History of TIA or stroke, carotid stenosis, etc.) | ± | ++ |
| Flow | Progressive (periods of plateau are possible) | Variable |
| Neuropsychological research | Memory impairment (hippocampal dysfunction) predominates | Disturbances in attention and regulatory functions (frontal dysfunction) predominate |
| Affective disorders | ± | + |
| Movement disorders (gait disorders, pseudobulbar syndrome, extrapyramidal or pyramidal signs) | ± | ++ |
| Neurogenic urinary disorders | - | + |
|
MRI data
hippocampal atrophy multiple lesions / leukoaraiosis | + ± | ± ++ |
MCI in patients with diffuse white matter lesions appear when their volume exceeds 10% of the volume of the white matter of the hemispheres. However, within 5 years, 70-80% of patients with moderate cognitive impairment "move" to the group of patients with dementia. At the same time, the presence of “silent” heart attacks, especially multiple ones, is associated with a general deterioration in cognitive performance and more than doubles the risk of developing dementia in the next few years.
DE is the leading cause of vascular dementia. Thus, in the structure of vascular dementia, 67% is dementia due to disease of small vessels (subcortical dementia, lacunar status, senile dementia of the Binswanger type). With this type of dementia, cognitive impairment can progress continuously with episodes sharp deterioration due to strokes. At the stage of dementia, patients are partially or completely dependent on others. The decline in the quality of life of patients with dementia can be traced most clearly by analyzing the works of famous artists suffering from dementia. Figure 3 shows the early work of the American artist William de Kooning (1904-1997), who was a master of abstract art. In the 80s he was diagnosed with dementia, which was reflected in the works under the general title Untitled. Figure 4 shows paintings by an artist in the dementia stage.

Rice. 3. Early works of de Kooning ("Women")

Rice. 4. Recent works of de Kooning ("Untitled")
The main clinical manifestations of vascular dementia (according to T. Erkinjuntti (1997) with amended)
The course of the disease:
- relatively sudden onset (days, weeks) of cognitive impairment;
- frequent stepwise progression (some improvement after an episode of deterioration) and fluctuating course (i.e. differences in the condition of patients on different days) of cognitive impairment;
- in some cases (20-40%), a more imperceptible and progressive course.
Neurological / psychiatric symptoms
- the symptomatology revealed in the neurological status indicates a focal lesion of the brain in the initial stages of the disease (mild movement defect, impaired coordination, etc.);
- bulbar symptoms (including dysarthria and dysphagia);
- walking disorders (hemiparetic, etc.);
- instability and frequent, unprovoked falls;
- increased urination and urinary incontinence;
- slowing down of psychomotor functions, impaired executive functions;
- emotional lability (violent crying, etc.);
- preservation of personality and intuition in mild and moderately severe cases;
- affective disorders (depression, anxiety, affective lability).
Accompanying illnesses
A history of cardiovascular disease (not in all cases): arterial hypertension, ischemic disease hearts.
Depending on the severity of the main symptoms, there are 3 degrees of DE severity:
1st degree
- the presence of focal disseminated neurological symptoms, which are insufficient in their severity for the diagnosis of the outlined neurological syndrome (mild cognitive impairments of a neurodynamic nature are detected);
2nd degree
- the presence of a sufficiently pronounced neurological syndrome (clinically obvious cognitive impairment, usually of a moderate degree);
3rd degree
- a combination of several neurological and neuropsychological syndromes that indicate multifocal brain damage (cognitive impairment reaches the degree of dementia).
As DE progresses, the number of patients 'complaints decreases significantly, which is due to a decrease in patients' criticism of their condition. Mainly complaints of unsteadiness when walking, noise and heaviness in the head, sleep disturbances persist. At the same time, the severity of social maladjustment increases. Figure 5 shows a fragment of a record of complaints of patient B., 59 years old, suffering from DE of grade 3.

Rice. 5. Complaint of patient B., 59 years old, with DE of grade 3
The severity of social maladjustment:
1st stage
- the patient is able to serve himself in normal conditions, difficulties arise only with increased stress (emotional or physical);
2nd stage
- some help is required under normal conditions;
3rd stage
- due to a neurological and / or cognitive defect, the patient is unable to perform even simple functions, constant help is required.
Currently, there are 3 options for the rate of progression of DE:
- fast pace - stage change in less than 2 years;
- average rate - change of stages within 2-5 years;
- slow pace - change of stages in more than 5 years
Diagnostic criteria for DE:
- objectively detectable neuropsychological and / or neurological symptoms;
- signs of cerebrovascular disease, including risk factors and / or instrumentally confirmed signs of damage to cerebral vessels (for example, ultrasound data) and / or brain matter (CT / MRI data);
- the presence of a causal relationship between vascular brain damage and the clinical picture;
- the absence of signs of other diseases that can explain the clinical picture.
O.S. Levin (2006) developed diagnostic criteria based on CT and MRI data of various stages of discirculatory encephalopathy (Table 2).
Table 2. Neuroimaging changes in DE
| Stages types of changes | 1st stage | 2nd stage | 3rd stage |
| Leukoaraiosis | |||
| type of | Periventricular and / or punctate subcortical | Spotted, partially confluent subcortical | Fusing subcortical |
| width | Less than 10 mm | More than 10 mm | More than 20 mm |
| Lacunas | |||
| number | 2-5 | 3-5 | More than 5 |
| Territorial heart attacks | |||
| number | 0-1 | 2-3 | More than 3 |
| square | No more than 1/8 hemispheres | No more than 1/4 hemispheres | at least 1/4 hemispheres |
| (diameter) | (up to 10 mm) | (up to 25 mm) | (> 25 mm) |
| Brain atrophy | ± | +/++ | ++/+++ |
DE treatment principles:
1) action on vascular factors (correction of blood pressure, prevention of stroke);
2) restoration of cerebral blood flow, improvement of cerebral metabolism;
3) improvement and stabilization of cognitive functions;
4) correction of others clinical manifestations diseases.
One of the most promising approaches in DE therapy is prescribing combination drugs with polymodal action (antihypoxic, metabolic (nootropic) and vasodilator). Recently, the drug has been widely used for these purposes. Omaron containing 400 mg of piracetam and 25 mg of cinnarizine.
The mechanism of action of piracetam is diverse. One theory that explains the many effects of piracetam is membranous. According to her, the effects of piracetam may be the result of the restoration of membrane fluidity (and it decreases with age):
- specific interaction with the cell membrane;
- restoration of membrane structure;
- restoration of the liquid properties of cell membranes;
- normalization of the function of the cell membrane.
It is customary to distinguish two main areas of action of piracetam: neuronal and vascular. The neuronal effect is realized due to the improvement of metabolic processes due to the optimization of oxygen consumption and glucose utilization. Piracetam has been shown to interact with the transmitter system to exert a modulating effect. Improving the neuronal effect facilitates cognitive processes. In a number of studies with double-blind control, it was found that the use of piracetam significantly increases higher mental functions not only under conditions of so-called physiological aging, but also in patients with psychoorganic syndrome with senile involution. In addition, in recent years, works have appeared confirming the effectiveness of piracetam on early stage Alzheimer's disease.
The vascular effect of piracetam is manifested due to its effect on microcirculation and blood cells: a decrease in platelet aggregation, an increase in erythrocyte deformability. As a result, piracetam exhibits an antithrombotic effect and significantly improves the rheological properties of blood, which, in turn, is the basis for the normalization of impaired cerebral circulation.
However, cerebrovascular pathology is accompanied not only by metabolic disorders, but also by disorders of cerebral hemodynamics, as a result of which another group of drugs is widely used in neurological practice - vasoactive agents, in particular cinnarizine. Cinnarizine is a selective blocker of slow calcium channels, inhibits the entry of calcium ions into cells and reduces their content in the plasmolemma depot, reduces the tone of smooth muscles of arterioles, reduces their response to biogenic vasoconstrictor substances, increases the elasticity of erythrocyte membranes, their ability to deform, and reduces blood viscosity.
When piracetam is combined with cinnarizine, the action of both drugs is potentiated. Thus, the time to reach the maximum concentration of cinnarizine in the blood plasma is 1-4 hours, while that of piracetam is 2-6 hours. As a result, the vascular effect precedes the nootropic one, which improves the delivery of piracetam to the ischemic zone of the brain. In addition, the use of lobster neutralizes the side effects of each of the components: piracetam (irritability, internal tension, sleep disturbances, increased excitability) and cinnarizine (weakness, depression, drowsiness). Omaron is prescribed 1 tablet 3 times a day for 2-3 months.
In a multicenter (5 clinical centers Russian Federation) an open, randomized study that included 90 stroke patients (1 month to 1 year old) compared the efficacy and tolerability of lobster (1 tablet 3 times a day) in combination with basic therapy (antihypertensive drugs, antiplatelet agents and statins) when using within 2 months. compared with basic therapy.
The results of the study showed that in the Omaron therapy group, a significant improvement in all cognitive functions was noted after a month of treatment. The improvement was most significant after two months of treatment. In the control group, the dynamics was much less pronounced. So, as an example, the results of the tests of memorizing 5 words and drawing a clock are presented below (Fig. 6, 7).

Rice. 6. Dynamics of indicators of the test of memorization of 5 words

Rice. 7. Dynamics of the clock drawing test indicators (points)
In addition, in the lobster treatment group, a significant decrease in the severity of depressive and anxiety disorders(fig. 8).

Rice. 8. Dynamics of indicators of the scale of depression and anxiety
The study established good tolerance of lobster, lack of side effects when combined with other medicines, which are used to prevent recurrent stroke, as well as the lack of influence of lobster on the indicators of systemic hemodynamics.
Literature
1. Damulin I.V. Dyscirculatory encephalopathy: pathogenesis, clinical picture, treatment. Guidelines- Moscow - 2005 - 43 p.
2. Damulin I.V. Actual aspects of neurogeriatrics in the practice of a therapist. Methodical recommendations for general practitioners - Moscow - 2004 - 23 p.
3. Kamchatnov P.R. Chronic disorders of cerebral circulation - Moscow - 2008 -39 p.
4. Levin O.S. Pathogenetic therapy cognitive impairment - Moscow - 2008 - 12 p.
5. Levin O.S. Dyscirculatory encephalopathy: modern ideas about the mechanisms of development and treatment - Moscow - 2006 - 24 p.
6. Markin S.P. Cognitive impairment in medical practice. Methodological manual - Moscow - 2007 - 42 p.
7. Parfenov V.A. et al. Open randomized multicenter study of the efficacy and safety of the drug Omaron in patients with stroke and moderate cognitive impairment - Moscow - 2008 - 15 p.
Dr. med. S.P. Markin
Voronezh State Medical Academy named after V.I. N.N. Burdenko
In recent years, an aging population has been observed in the world, primarily due to a decrease in the birth rate. In the figurative expression of V. Konyakhin, “young people come and go, but old people remain”. So, in 2000 there were about 400 million people over the age of 65 all over the world. However, this age group is expected to increase to 800 million by 2025.
Changes in the nervous system occupy a leading place among this contingent of people. In this case, the most common are lesions of the vessels of the brain, leading to its ischemia, i.e. the development of discirculatory encephalopathy (DE).
DE is a syndrome of progressive multifocal or diffuse brain damage, manifested by clinical neurological, neuropsychological and / or mental disorders, caused by chronic cerebral vascular insufficiency and / or repeated episodes of acute cerebrovascular accidents.
In the modern classification of ICD-10, the term "discirculatory encephalopathy" is absent. Instead of the previous diagnosis, it is recommended to use the following disease codes:
167.4 Hypertensive encephalopathy
167.8 Other specified vascular lesions of the brain.
However, the term "discirculatory encephalopathy" is traditionally used among neurologists in our country. DE is a heterogeneous condition that can have a different etiology. The greatest etiological significance in the development of DE are:
- atherosclerosis (atherosclerotic DE);
- arterial hypertension (hypertensive DE);
- their combination (mixed DE).
In atherosclerotic DE, damage to large main and intracranial vessels (stenosis) prevails. At the same time, in the initial stages of the disease, stenosing changes in one (less often two) major vessels are detected, while in the advanced stages of the process, most (or all) of the major arteries of the head are often changed. A decrease in blood flow occurs with hemodynamically significant stenosis (narrowing of 70-75% of the arterial lumen area) and then increases in proportion to the degree of narrowing. At the same time, the state of the intracranial vessels (development of the collateral circulation network) plays an important role in the mechanisms of compensation of cerebral circulation.
In hypertensive DE, the main pathological processes are observed in the smaller branches of the cerebral vascular system (perforating arteries) in the form of lipohyalinosis and fibrinoid necrosis.
The main pathogenetic mechanisms of DE development:
- chronic ischemia;
- "incomplete stroke";
- completed stroke.
The main morphological changes in DE:
- focal changes in the brain (postischemic cysts due to lacunar stroke);
- diffuse changes in white matter (leukoaraiosis);
- cerebral atrophy (cerebral cortex and hippocampus).
The defeat of small cerebral arteries (40-80 microns in diameter) is one of the main causes of lacunar stroke (up to 15 mm in diameter). Depending on the location and size, lacunar infarctions can manifest themselves as characteristic neurological syndromes or be asymptomatic (in functionally "mute" zones - the shell, white matter of the cerebral hemispheres). With the multiple nature of deep lacunae, a lacunar state is formed (Fig. 1)
Rice. 1. Multiple lacunar foci in the basin of the right middle cerebral artery, according to MRI of the brain
Leukoaraiosis is visualized as bilateral focal or diffuse areas of reduced density in the white matter on computed tomography and T1-weighted images on magnetic resonance imaging, or as areas of increased density on T2-weighted images on magnetic resonance imaging (Fig. 2).
Rice. 2. Severe leukoaraiosis
The widespread involvement of small arteries causes several main types of changes:
- diffuse bilateral white matter lesion (leukoencephalopathy) - leukoencephalopathic (Binswanger's) variant of DE;
- multiple lacunar infarctions - a lacunar variant of DE.
In the clinical picture of DE, a number of basic syndromes are distinguished:
- vestibular-atactic (dizziness, staggering, unsteadiness when walking);
- pyramidal (revitalization of tendon reflexes with expansion of reflexogenic zones, anisoreflexia, sometimes clonuses of the feet);
- amiostatic (trembling of the head, fingers, hypomimia, muscle rigidity, slow motion);
- pseudobulbar (blurred speech, "violent" laughter and crying, choking when swallowing);
- psychopathological (depression, impaired cognitive functions).
Dizziness - the most common complaint of patients with DE (occurs in 30% of cases). Dizziness in the elderly is caused by the following reasons and their combinations:
- age-related changes in the sensory system;
- a decrease in the compensatory capabilities of the central mechanisms of balance;
- cerebrovascular insufficiency with predominantly lesion of the vertebrobasilar system.
In this case, the leading role is played by the defeat of the vestibular nuclei of the trunk or vestibulo-cerebellar connections. The so-called peripheral component, due to atherosclerotic lesions of the vessels of the inner ear, is of certain importance.
Movement disorders in old age (up to 40% of cases) are caused by damage to the frontal lobes and their connections with subcortical formations.
Major movement disorders in the elderly:
- "frontal gait disorder" (frontal dysbasia);
- "frontal imbalance" (frontal astasia);
- "subcortical imbalance" (subcortical astasia);
- violation of the initiation of walking;
- "careful" (or uncertain) walking.
Movement disorders are often accompanied by falls. According to a number of researchers, falls at least once a year are observed in 30% of people aged 65 and over, while in about half of cases this happens more than once a year. The likelihood of falls increases in the presence of impaired cognitive functions, depression, as well as patients taking antidepressants, benzodiazepine tranquilizers, antihypertensive drugs.
The prevalence of depression among patients with DE (according to the Compass study) is more than 50% (with a third of patients having severe depressive disorders).
Features of the clinical picture of depression in the elderly:
- the predominance of somatic symptoms of depression over mental;
- severe disturbance of vital functions, especially sleep;
- the mask of mental symptoms of depression can be anxiety, irritability, "grumpiness", which are often considered by others as features of old age;
- the cognitive symptoms of depression are often assessed in terms of senile forgetfulness;
- significant fluctuations in symptoms;
- incomplete compliance with the criteria for a depressive episode (individual symptoms of depression);
- a close relationship between exacerbations of somatic illness and depression;
- the presence of general symptoms of depression and somatic illness.
According to a number of epidemiological studies, from 25 to 48% of people over 65 years of age experience a variety of sleep disorders. In this case, sleep disorders are most often manifested in the form of insomnia: presomnic disorders - 70%, intrasomnic disorders - 60.3% and postsomnic disorders - 32.1% of cases.
The main manifestations of sleep disorders in the elderly:
- persistent complaints of insomnia;
- constant difficulty falling asleep;
- superficial and intermittent sleep;
- the presence of vivid, multiple dreams, often painful content;
- early awakenings;
- a feeling of anxious anxiety on awakening;
- difficulty or inability to fall asleep again;
- lack of feeling of rest from sleep.
Cognitive impairment in depression due to redistribution of attention, low self-esteem and mediator disorders. Cognitive dysfunctions in depression are characterized by:
- acute / subacute onset of the disease;
- rapid progression of symptoms;
- indications of previous mental pathology;
- persistent complaints about a decrease in intellectual abilities;
- lack of effort when performing tests ("don't know");
- variability of test execution;
- Attracting attention improves test performance;
- memory of recent and distant events suffers equally.
However, in depression, the subjective assessment of cognitive abilities and the degree of social maladjustment, as a rule, do not correspond to the objective data of cognitive tests. A decrease in the severity of emotional disturbances leads to a regression of cognitive disorders associated with depression. Nevertheless, numerous studies of the hippocampus in patients with major depressive disorder have accumulated evidence that atrophy occurs with depression. Recently there have even been reports of hippocampal atrophy after the first depressive episode [J.P. Olier, France, 2007]. In addition, according to the Chicago experts from the Rush Alzheimers Disease Center, prolonged depression can lead to the development of Alzheimer's disease. So, with each new sign of depression, the likelihood of developing Alzheimer's disease increases by 20%.
Moderate cognitive impairment (MCI) with DE (according to the study "Prometheus") occurs in 56% of cases. The relationship between moderate cognitive disorders detected in a patient and DE may be evidenced by:
- the predominance of regulatory cognitive impairments associated with dysfunction of the frontal lobes (impaired planning, organization and control of activities, decreased speech activity, moderate secondary memory impairment with relatively intact recognition);
- a combination of cognitive impairments with affective disorders (apathy, depression, irritability), as well as focal neurological symptoms, including those indicative of suffering in the deep parts of the brain (dysarthria, impaired walking and postural stability, extrapyramidal signs, neurogenic urination disorders).
Table 1 shows the comparative characteristics of the "Alzheimer's type" MCR and DE with MCR.
Table 1. Distinctive characteristics of Alzheimer's type MCR and DE with MCR
Signs
UKR Alzheimer's type
CEREBRAL ATHEROSCLEROSIS
Cerebral atherosclerosis
Prevalence: Typically diagnosed between the ages of 50-60.
Prognosis for cerebral atherosclerosis: The rate of formation of neurological disorders can be different. There are "unfavorable" variants of the course of cerebral atherosclerosis: rapidly progressing, slowly progressing with seizures and transient disorders of cerebral circulation, and most often with atherosclerosis of the cerebral vessels, a slowly progressive course.
The course is slowly progressive. The effect of a number of factors can accelerate and aggravate the course of cerebral atherosclerosis: trauma, infection, intoxication, decompensation of cardiac activity, emotional and intellectual overload, incoming cerebral circulation disorders. There are three stages of cerebral atherosclerosis: I - moderately expressed; II - pronounced, III - pronounced. With a rapidly developing variant of the course, pronounced cerebral atherosclerosis develops within about 5 years. Relative stabilization of the condition is possible against the background of persisting neurological symptoms, but progression with repeated crises and transient ischemic attacks Oh. An increase in clinical manifestations with increasing age of patients is characteristic, which reflects the addition of cardiovascular and other pathologies of internal organs. There is a rapid rate of progression of the disease in patients with arterial hypertension with an unfavorable course.
Cerebral atherosclerosis of the first stage (1 degree) -
Moderately pronounced stage. It is expressed by the development of "neurasthenic" syndrome and the predominance of subjective manifestations. This stage is characterized by complaints of memory impairment, decreased performance, headaches and heaviness in the head, dizziness, sleep disorders, general weakness, rapid fatigability, inattention. Often, these symptoms of overwork are accompanied by complaints of: pain in the heart, palpitations, shortness of breath, pain in the joints and spine, etc.
The second necessary criterion for the diagnosis of stage 1 atherosclerotic encephalopathy is the detection by a neurologist during examination of disseminated organic symptoms of damage to the nervous system, many of which are variable in nature.
Neuropsychological studies confirm the presence of asthenia, a decrease in short-term memory, attention. Psychological testing reveals a decrease in attention and memorization, a decrease in the volume of perceived information. The criticism is saved. At this stage, as a rule, with a properly selected treatment, it is possible to reduce the severity or eliminate individual symptoms. Social maladjustment is minimally expressed, the patient's difficulties arise only from emotional or physical overload.
Cerebral atherosclerosis of the second stage (2 degrees) -
Pronounced stage. It is expressed by the fact that along with internal unpleasant sensations, objective signs appear. Working capacity progressively decreases, fatigue, sleep and memory disorders increase. Patients stop noticing their defects and often overestimate their real capabilities.
In the neurological status, clear symptoms characteristic of organic defeat certain structures of the brain (for example, symptoms of parkinsonism).
Cerebral atherosclerosis of the third stage (3 degrees) -
A pronounced stage. There may be no complaints or the paucity of complaints attracts attention. During a neurological examination, there is an increase in the severity of previously existing symptoms. Patients showed a sharp decrease in intelligence, weakness, flattening of emotions. Headache, dizziness, noise in the head, sleep disorders are constant.
Symptoms are certain clinical syndromes: motor pathway insufficiency - pyramidal syndrome; unsteadiness and instability - atactic syndrome; pseudobulbar, vascular parkinsonism, psychosis, vascular dementia.
Cerebral atherosclerosis 3 degrees

Modern methods of treating cerebral atherosclerosis
Cerebral Atherosclerosis Treatment Standards
Protocols for the treatment of cerebral atherosclerosis
Modern methods of treatment of discirculatory encephalopathy
Treatment standards for discirculatory encephalopathy
165 Blockage and stenosis of precerebral arteries, not leading to cerebral infarction
166 Blockage and stenosis of cerebral arteries, not leading to cerebral infarction
I67.4 Hypertensive encephalopathy
167.2 Cerebral atherosclerosis
167.3 Progressive vascular leukoencephalopathy
I67.8 Cerebral ischemia (chronic)
169 Consequences of cerebrovascular diseases
170 Atherosclerosis
167 Other cerebrovascular diseases.
Definition: Atherosclerosis is characterized by deposits of lipids in the form of plaques in the intima of large and medium-sized arteries; accompanied by fibrosis and calcification. The term cerebral reflects the localization of the process.
Cerebral atherosclerosis develops as a result of occlusive, stenosing lesions of extra- and / or intracranial arteries, i.e. arteries supplying the brain. Violation of cerebral circulation is caused by the same changes in the vessels that lead to myocardial infarction or intermittent claudication.
As a working classification chronic forms of disorders of cerebral circulation can be used classification of E.V. Schmidt (1985).
According to this classification, the term DE reflects the entire spectrum of manifestations of chronic cerebrovascular disorders - from minimally expressed disorders to the degree vascular dementia, i.e. includes all pre-dementia forms of angioneurological disorders.
Dyscirculatory encephalopathy (DE) is a slowly progressive violation of the blood supply to the brain, leading to gradually increasing structural changes in the brain and dysfunction. The main pathogenetic mechanisms of DE include lesions of extra - and intracranial cerebral vessels.
Classification: encephalopathy:
Stage I - diffuse focal neurological symptoms.
Stage II is characterized by a progressive deterioration of mnestic functions, a decrease in working capacity, a personality change occurs, and focal symptoms are more distinct.
stage iii is characterized by diffuse changes brain tissue, which lead to the development of focal syndromes, depending on the predominant damage to any area of the brain, the aggravation of mnestic and mental disorders up to dementia.
Risk factors:
1. Smoking
2. High level cholesterol
3. High triglyceride levels
4. Hyperhomocysteinemia
List of additional diagnostic measures:
1. Consultation with an ophthalmologist (fundus)
2. Consultation with a cardiologist
3. Electrocardiography
4. Computed tomography.
Treatment tactics:
1. Correction of risk factors (RF) of atherogenesis processes;
2. Improved perfusion;
3. Neuroprotective therapy.
Correction of RF consists in controlling blood pressure levels, lowering cholesterol levels, and quitting smoking in patients.
Treatment of arterial hypertension is carried out with the use of low doses of diuretics, beta blockers, APF inhibitors or calcium channel blockers A.
Hypercholesterolemia is an important risk factor for cerebrovascular disease.
Treatment of dyslipoproteinemia begins with the correction of lipid metabolism disorders using diet. Lifestyle changes are necessary: increasing physical activity, quitting smoking, losing weight, etc.
The initial dose of lovastatin is 20 mg at bedtime. The dose can be increased to 80 mg / day (prescribed 1 or 2 times).
Pravastatin: 20-40 mg / day.
Simvastin: the initial dose is 10-20 mg, can be increased to 80 mg / day.
Fluvastatin: 20-40 mg (up to 80 mg).
Patients with concomitant cardiovascular diseases (coronary heart disease, stroke) are advised to take statins when their total cholesterol level is less than 6.0 mmol / L.
Treatment of the sick chronic ischemia the brain should be comprehensive and include activities aimed at correcting the main vascular disease, prevention of recurrent cerebral dyshemias, restoration of quantitative and qualitative parameters of cerebral blood flow and normalization of impaired brain functions, impact on existing risk factors for cerebrovascular diseases.
- it is necessary to use antiplatelet agents in relation to patients with a high risk of cardiovascular complications;
- in the absence of contraindications, low doses of acetylsalicylic acid (75 mg / day) are recommended for the primary prevention of cardiovascular complications in patients with hypertension over 50 years of age who have a 10-year risk> 20% (high or very high), and blood pressure controlled at a level less than 150/90 mm Hg.
A) there are no contraindications to taking acetylsalicylic acid;
B) BP is controlled at a level of less than 150/90 mm Hg, and there is also one item from the following list: cardiovascular complications, target organ damage, 10-year risk of cardiovascular complications 20%.
For the prevention of acute disorders of cerebral circulation (onmc), transient ischemic attacks (thia), acetylsalicylic acid 75 mg is used daily.
In case of intolerance to acetylsalicylic acid, as well as in the presence of thia, onmc, clopidogrel 75 mg daily is prescribed.
Neuroprotective therapy: pyritinol, 1 tab. 3 times a day, the course of treatment is 1 month, vinpocetine 5, 10 mg, 1 tablet 2-3 times a day.
Ginkgo biloba is taken at 40-80 mg - 3 times a day with meals. The course of treatment is 1-3 months. The drug improves microcirculation, cerebral circulation, stimulates cellular metabolism, has an antiaggregatory effect.
With progressive DE it is recommended - deproteinized hemoderivat from calf blood (dragees from 200 to 600 mg or 40 mg intramuscularly); complex of etamivan hexobendin + dihydrochloride + etofillin appoint 1-2 tab. 3 times / day or 1 tab. forte 3 times / day (maximum 5 tab.) for 6 weeks. Parenterally prescribed in a single dose of 2 ml intramuscularly or intravenously drip in 200 ml of 5% glucose solution. The frequency of administration is 1-2 times / day. The course of treatment is 7-10 days.
List of essential medicines:
1. Pravastatin 20 mg, table.
2. Simvastin 20 mg, tab.
3. Lovastatin 10 mg, 20 mg, 40 mg, tab.
4. Fluvastatin 20 mg, table.
5. Acetylsalicylic acid 100 mg, table.
6. Pyritinol.
7. Vinpocetine 5, 10 mg, tab.
8. Ginkgo biloba, standardized extract 40 mg.