What are leukocytes in the field of view. Increased leukocytes in a smear in a woman - the reasons for the increase, treatment. Why, after the treatment, the leukocytes in the smear remain elevated
Leukocytes are special cells immune system designed to protect the body from infections. When a virus appears, white blood cells begin to multiply actively to defend themselves. Naturally, this increase is immediately displayed in blood tests, and, of course, in a smear. For doctors, the signal for treatment is the presence of more than 15 units of leukocytes in the smear in the field of view. This means that a woman develops an infectious and inflammatory disease. If the number of leukocytes literally goes off scale, then the lady has problems with the genitourinary system. It can be inflammation of the bladder, kidneys, or genitals.
What do leukocytes in a smear say?
Leukocytes can be found in the smear and in the norm. But in this case, there won't be many of them. If the value is outside the normal range, most likely, the lady develops an infectious inflammatory disease - vaginitis, bacterial vaginosis, thrush, colpitis, etc. Moreover, the more leukocytes in the smear, the more acute the course of the disease.
Symptoms that may accompany an increased white blood cell count in a smear are as follows:
- frequent urination which can be quite painful;
- burning sensation in the vagina;
- unpleasant ;
- problems with the menstrual cycle (for example, failure);
- dense, whitish discharge.
Various problems can be the reasons for a gynecological smear. These are vaginal dysbiosis, and various sexually transmitted infections, and Escherichia coli, as well as oncological diseases of the genital organs.
What to do with high white blood cells
First of all, in order to reduce the number of leukocytes in a smear, it is necessary to treat the cause that causes such a pathology. Treatment must be prescribed by an observing gynecologist. Sometimes a urologist is also involved in drawing up a treatment regimen.
In parallel, you can try to reduce the unpleasant sensations that a particular disease causes. For this, sanitation is usually prescribed, which allows you to restore the microflora of the vagina. The course can be carried out both with the help of medicines and herbs - chamomile, nettle, St. John's wort, etc. Naturally, such treatment can only be used with the agreement of a doctor.
You can also make warm baths. The water temperature should be at least 45 degrees, because heat helps fight inflammatory diseases.
Often used to reduce leukocytes in a smear, special suppositories.
A gynecological examination of the vaginal microflora reveals possible inflammatory processes of the genital area. An ideal "clean" vaginal smear contains a single number of leukocytes and rod flora.
The number of leukocytes in a smear is up to 15 considered the norm. Exceeding this value indicates the development of pathological processes or signals a possible sexual infection.
Increased quantity leukocytes are considered together with the bacterial flora of the vagina. Distinguish 2 degrees of negative smear:
- The number of leukocytes is 30 - 40, the flora is predominantly coccal.
- A large number of leukocytes, the absence of lactobacilli, various organisms are present in the microflora, Trichomonas and gonococci can be secreted.
 Myself smear on microflora does not reveal the main reason for the increase in leukocytes and changes in microflora, however, it indicates the presence of inflammatory diseases of the genital organs.
Myself smear on microflora does not reveal the main reason for the increase in leukocytes and changes in microflora, however, it indicates the presence of inflammatory diseases of the genital organs.
For diagnostics possible diseases with negative smears, additional laboratory tests are prescribed - smears for bacterial culture and oncocytology, blood for the presence of hidden infectious diseases... Colposcopy is also shown to determine the state of the endometrium.
Causes
Any inflammatory process in the body is characterized by leukocytosis. An increased number of leukocytes in a smear in a woman signals diseases of the reproductive system, which classified as follows:
- Inflammatory diseases of the lower parts and organs of the small pelvis: cervicitis, colpitis, vulvitis, endocervicitis, endometritis, parametritis
- Viral and infectious: gonorrhea, herpes, trichomoniasis, chlamydia, syphilis, HIV and others.
- Non-specific: candidiasis, ureaplasma, mycoplasma, staphylococcus, etc.
In their course, diseases can occur in a chronic (asymptomatic) and acute stage.
Pelvic inflammatory disease (PID) can be the result of previous abortions, intrauterine contraceptives, chronic diseases (diabetes), hormonal disorders. Chronic stress, smoking, alcohol, sleep disturbance are factors that influence the development of PID. Infection with infectious diseases in 99% of cases occurs through sexual contact.
During pregnancy
 Due to hormonal changes, the level of leukocytes in the vaginal microflora of a pregnant woman may be slightly increased, but not more than 20 leukocytes in a smear. Negative smears during pregnancy also indicate inflammatory processes of the reproductive system and require additional examination.
Due to hormonal changes, the level of leukocytes in the vaginal microflora of a pregnant woman may be slightly increased, but not more than 20 leukocytes in a smear. Negative smears during pregnancy also indicate inflammatory processes of the reproductive system and require additional examination.
Most frequent the reasons for the increase in the level of leukocytes during pregnancy - candidiasis (thrush) and cervicitis, which are caused by: changes in hormonal levels, disruption of the usual way of life, stress and fatigue.
Drug treatment
For the treatment of inflammatory diseases of the genital organs are used following methods:
- Douching the vagina with antiseptic agents: miramistin, chlorhexidine, potassium permanganate;
- Antibacterial vaginal suppositories: "Genferon", "Hexicon", "Terzhinan", "Viferon";
- With candidiasis, the drugs "Fluconazole", "Flucostat" are taken orally.
 Treating infectious diseases requires intravenous administration antibacterial drugs: Ornidazole, Tsiprinol, Metronidazole. Local douching of the vagina with antiseptics is jointly prescribed. Upon completion of treatment, a course of restorative therapy is carried out, aimed at the population of the vagina with beneficial bacteria, with the help of eubiotics: "Bifidumbacterin", "Lactobacterin", Vagilak "and others.
Treating infectious diseases requires intravenous administration antibacterial drugs: Ornidazole, Tsiprinol, Metronidazole. Local douching of the vagina with antiseptics is jointly prescribed. Upon completion of treatment, a course of restorative therapy is carried out, aimed at the population of the vagina with beneficial bacteria, with the help of eubiotics: "Bifidumbacterin", "Lactobacterin", Vagilak "and others.
Important: all medications should be taken strictly as directed by your doctor. Self-medication with antibiotics has many side effects.
Treatment with folk remedies
- A tablespoon of chamomile flowers, calendula, stinging nettle (optional) is poured with a glass of water, brought to a boil, removed from heat and insisted for half an hour. Before using, the decoctions should be strained through a sieve or cheesecloth.
- Pour 6 cloves of chopped garlic with 1.5 liters of hot water, leave to infuse overnight, strain before use.
- Pour 2 cloves of minced garlic with 2 cups of hot water, add 1.5 tablespoons apple cider vinegar, mix and strain.
- For thrush: mix 1 dose of dry bifidumbacterin with a teaspoon of warm water, add 1 teaspoon of petroleum jelly. Soak a tampon with the resulting ointment and insert into the vagina for 10 hours. Treatment course: 7 - 10 days.
An increase in the level of leukocytes is a signal of the presence of inflammatory, infectious diseases, and many of them may be asymptomatic. The identification of the cause and its elimination should be carried out immediately. Otherwise, the woman is putting her health at great risk.
The consequences of inflammatory diseases:
- Infertility;
- Ectopic pregnancy;
- Complications during pregnancy;
- Endometriosis;
- Oncology;
- Violation menstrual cycle;
- Adhesions leading to infertility;
- Myoma of the uterus.
For the prevention and timely detection of diseases of the reproductive system, a woman should undergo a gynecological examination every 6 months.
In antenatal clinics, such a phenomenon is often observed as the concealment of important information about the state of health of patients from themselves. Why doesn't the doctor explain how serious the problem is, what are the causes, how many treatment options are there? Why should a patient blindly believe in the recommendations of a gynecologist? If a specialist does not provide information, then it makes sense to figure out what and how it works, why failures occur in the system, how to deal with them.
Important! It has been proven that the better the patient is aware of their problems, the faster the treatment goes. This is due not only to physical changes, but also to the inner attitude to fight the disease.
One of the indicators of a woman's health is the presence in the bloodstream of white blood cells - leukocytes. They are responsible for the general immunity of the body, which makes it possible to accurately determine the presence infectious agents... The activity of bacteria and viruses undermines the defenses, releasing the products of their vital activity. In this case, the reduced immunity suffers even more.
In gynecology, the number of leukocytes is determined by analyzing a smear from the cervical canal. If they are normal, then there is nothing to worry about. But it often happens that a woman does not feel any changes in her health, and her leukocytes rise.
In the photo - leukocytesWhite blood cells are the general name for a group of cells that track and consume bacteria. This process is called phagocytosis. In this case, the white cells die. Accumulations of pus in a certain area of the body are dead leukocytes.
There are several types of white blood cells:
- neutrophils;
- basophils;
- eosinophils;
- lymphocytes;
- monocytes.
They differ in size, shape of the nucleus and functions that they perform in the body.
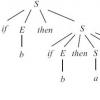
The algorithm of action of a leukocyte is as follows: when an infection enters the body, leukocytes detect it and absorb it. When bacteria are digested, substances are released that form a focus of inflammation. In this case, redness occurs, the temperature rises, and swelling or swelling appears.
If the cells are able to destroy all the infection, then the person recovers on his own. If the leukocytes are weak, there are few of them, or they are inactive due to low immunity, then an abscess appears.
An abscess is a local inflammatory response of the body to foreign microorganisms. The body delimits the sore spot with a capsule. The main manifestation of an abscess is the formation of a purulent cavity.
It is better for the human body when inflammation occurs in the presence of an infection. It remains to find out what kind of bacteria provokes the process and prescribe treatment. Lack of reaction means a non-working immune system and serious disturbances in the body. Most often, a reduced number of white cells is found in the analyzes.
It takes a long time. This means that there is not enough strength to fight the infection and help is required in the form drugs that suppress infection and stimulate the immune system. Great importance It has proper nutrition and the use of vitamins - natural (vegetables, fruits) and complex pharmaceuticals.
The property of leukocytes to penetrate the walls of blood vessels and back into the bloodstream gives reason to think that the presence of a focus of inflammation in any part of the body can lead to an increase in the total number of leukocytes in the body. However, they may also appear in a smear from the cervix.

The main indicator of the presence of infection is an increase in the number of neutrophilic leukocytes. Their function is to fight bacteria that most often affect the genitourinary system. Normally, the number of neutrophils is up to 75% of the total number of leukocytes. If this indicator is increased, then there is inflammation. During a gynecological examination, the vaginal mucosa may be hyperemic, there is discharge from the cervical canal.
A smear test for pathogenic flora is carried out in parallel with a blood test. To determine the treatment, it is also necessary to examine the woman's partner. The detected infections in a woman are in most cases present in the man's urethra.
The number of neutrophils increases if:
- there are acute infectious processes;
- intoxication of the body;
- purulent processes;
- malignant tumors;
- great blood loss.
Together with the tests for leukocytes, a number of diagnostic measures are required:
The main place in diagnostics is occupied by analyzes.
Genitourinary tract infections
Bad smear tests from the cervix indicate the ingress and reproduction of infection in the genital tract. Particularly dangerous are:
This is not the entire list. Complicate the flow female diseases infections in the bladder, urethra, kidneys, intestines. The reason for the increase in leukocytes in the smear may be outside the scope of the gynecologist's study.

Elevated leukocytes with erosion of the cervix, they say that infection is multiplying in the damaged epithelium. With erosion, the stratified epithelium is replaced by a single layer, which facilitates the penetration of microbes into the mucous membrane. Normally, there should be no more than 20 white blood cells in the cervix. This is the upper limit after which the doctor diagnoses inflammation and prescribes an analysis for a specific infection. 35 leukocytes is already a sluggish inflammation or its initial stage.
White blood cells in a smear from the cervix can increase during pregnancy. This is due to a general decrease in immunity. Therefore, microbes, fungi that were in the body before pregnancy are activated during this period. The number of neutrophils in the cervix increases with thrush, which is very common in women in later stages. Sometimes their number reaches 60 units.
It is an additional factor that attracts immune cells to the genital area. Leukocytes protect the damaged mucous membrane of the cervix from the effects of microbes.
70 - 80 leukocytes in a smear indicates that there are infections in the kidneys and urinary tract... You should be examined with an ultrasound scan and urine tests. If at the same time the temperature rises and urination is painful, then it is necessary to treat not only erosion, but also the kidneys.
100 - 150 leukocytes in a smear with erosion is a severe form of infection with the formation. The process is very dangerous, because the infection enters the bloodstream through the damaged epithelium. The choice of drug in this case is an antibiotic. In parallel with treatment, the level of leukocytes should be monitored, so the doctor prescribes repeated smears. In the acute stage of the disease, the inguinal lymph nodes may be enlarged.
During pregnancy, it often happens that uterine leukocytosis rises to critical levels - 200 units. At the same time, no microbes are detected, and discharge is quite common. Sometimes the tone of the uterus rises. This is due to the reaction of the woman's body to a foreign protein. This is especially pronounced with the difference between the Rh factor of the mother and the fetus. According to reviews - usually everything goes away by itself after childbirth. Hormone levels also affect the number of white blood cells.
Leukocytes are lowered during erosion - causes
- endocrine disorders;
- lack of nutrients;
- with oncology;
- disorders in the work of the bone marrow.
A decrease in the number of neutrophils is a dangerous phenomenon that requires additional blood tests. If there are also few leukocytes in the blood, then a complete examination is worthwhile.
Erosion of the uterus in this case can become the gateway for any infection, therefore, it is necessary to follow the rules of personal hygiene, to streamline sex life, since with a large number of sexual partners, the risk of germs getting in increases.
How to lower the white blood cell count in a smear?
Reducing the number of white blood cells is required when there is an established infection - bacterial, viral or fungal. Antibiotics are usually the drugs of choice against bacteria. After the course of treatment, a second analysis is carried out. After 2 - 3 weeks, another one.
Antiviral therapy consists in the use of agents that strengthen the immune system. Candidiasis is treated with antifungal medications.
Care should be taken with medications during pregnancy, because during this period increased content white blood cells may not be related to infection.
Video from free courses presented on the site: Leukocytes smear
Video: What did they find in my smears
Video: white blood cell count in smears
By the level of leukocytes, which is easily determined by specialists under a microscope, they judge the existing inflammatory process. With regard to gynecology, white blood cells are determined and counted in the following studies - smears on:
- flora (microscopy);
- cytology;
- degree of purity.
Analysis for the composition of microflora
A urogenital smear for microflora is taken from three points: the vagina, cervix and urethra. If an inflammatory process is detected, then it is called colpitis(if the vagina is affected), cervicitis(if leukocytosis is fixed in the cervical canal) and urethritis(there is a problem in the urethra).
In addition to leukocytes, doctors are interested in the amount of epithelium and mucus. This additionally speaks of health or pathology.
So, normally, there should be how many leukocytes in a smear in women.
As you can see, 0 is also indicated in the table, which means that the absence of leukocytes is also an acceptable option. Not below the norm.
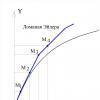
Analysis for the degree of purity
A smear for the degree of purity is similar to that of microscopy. And often in the results you will see a numerical indication of the "purity" of the genital tract. If single leukocytes are found - 1-3-5 in sight, one speaks of the first degree. In addition, a lot of useful microflora is found in the woman's vagina - lactic acid sticks.
With the second degree, there are still not too many leukocytes, perhaps a little more than the norm, for example, 10-15 , but in the vagina, in addition to Dederlein's sticks, opportunistic microorganisms are determined - Klebsiella, Candida mushrooms, Gardnerella, etc.
In the third degree, there are many opportunistic bacteria in the vagina. Leukocytes are found in clusters, in large numbers. Their approximate level 25-30 or even 40-50.
With the fourth degree in a smear from 60 white blood cells. Sometimes they completely cover the entire field of view, that is, their number reaches above 100... Highly high leukocytes are diagnosed against the background of other signs of the inflammatory process - coccobacillary flora and the almost complete absence of lactobacilli.
Analysis for atypical cervical cells (oncocytology)
In a cytological smear, information on the number of leukocytes is important if a woman has atypical cells of the cervix or is suspected of having them. The fact is that cervicitis, which is characterized by leukocytosis, causes reactive processes in cells, similar to those that occur in precancerous diseases.
If the leukocytes are high, first you need to be treated, and then, when their level becomes small, after 2-3 months, repeat the analysis. Recall how many white blood cells in the cervical canal is up to 30 units.
Causes of increased white blood cells in a smear in women, symptoms and treatment
The culprit is the inflammatory process. And it is provoked by various bacteria, fungi and viruses.
Genitourinary infection. Chronic or acute cystitis
In girls, it often occurs simultaneously with vulvovaginitis, that is, the mucous membrane of the labia and vagina turns red and becomes edematous. Cystitis is a very common disease in women due to their anatomical features- a short distance separating the vagina, rectum from the urethra and a very short and wide urethra, in which case the infection easily gets into bladder.
Hypothermia or the so-called cold plays a negative role and leads to the rapid progression of inflammation.
At the same time, the following pathogens are diagnosed in the inoculation or in the smear by the PCR method:
- Chlamydia trachomatis (chlamydia);
- Mycoplasma genitalium (genital mycoplasma);
- Ureaplasma urealyticum (ureaplasma);
- Mycoplasma hominis (mycoplasma hominis);
- E. coli (Escherichia coli);
- Staphylococcus saprophyticus (saprophytic staphylococcus);
- Enterococcus faecalis (fecal enterococcus);
- Klebsiella (klebsiella);
- Proteus mirabilis (proteus myribilis).
Thrush (vaginal candidiasis)
The causative agent is yeast-like fungi of the genus Candida. Yeast is not sexually transmitted. This is a conditionally pathogenic microorganism that is present in the vaginal microflora of almost every woman, but it causes the disease only when the number of lactobacilli decreases, if its number increases.
Contribute to the development of candidiasis:
- diabetes;
- pregnancy;
- taking antibiotics;
- HIV infection.
Signs of the disease:
- itching and burning in the labia;
- a white, cheesy or creamy discharge that gets worse before menses;
- pain during sex;
- painful urination if the urethra is also affected by fungi.
Diagnosis of candidiasis is carried out using bacterial sowing. Microscopy does not always show clear signs of the disease.
Treatment tactics depend on whether the disease is chronic, how often it recurs, and how bright and painful the symptoms are.
Are used the following drugs for local treatment (intravaginally):
- clotrimazole tablets (100 mg once a day for 7 days, or 200 mg once a day for 3 days);
- clotrimazole cream (if the labia is affected) for 1-2 weeks;
- natamycin (100 mg for 6 days);
- butoconazole 2% cream, single dose;
- itraconazole (200 mg for 10 days).
For oral administration (oral):
- fluconazole (150 mg once);
- itraconazole (200 mg for 3 days).
During pregnancy, drugs are prescribed for local use with the active ingredients clotrimazole (from the second trimester of pregnancy) and natamycin (from the first trimester).
Vaginal candidiasis is not sexually transmitted, but there are conditions that favor the growth of fungi that should be avoided:
- uncontrolled intake of antibiotics and hormonal drugs;
- wearing thick synthetic underwear;
- endocrine, gastrointestinal, gynecological diseases;
- frequent use of sanitary napkins;
douching; - one sexual partner (there is "addiction" to his microflora).
Complications of thrush include:
- inflammatory diseases of the pelvic organs;
urethrocystitis; - during pregnancy - infection of the fetus, its intrauterine death, premature birth;
- postpartum candidal endometritis.
Allergic vulvitis or vulvovaginitis
The reason is sanitary pads, tampons, intimate hygiene products. The labia become swollen, itchy. Passes by itself. The main thing is not to use an allergen.
Trichomoniasis (Trichomonas vaginitis)
The causative agent of the disease is Trichomonas vaginalis (Trichomonas vaginalis). Sexually transmitted, very rarely by household (through bed linen, towels, etc.). It is detected in a general smear or bacterial culture and is one of the most common causes of leukocytosis in a smear.
From infection to the appearance of the first symptoms, it takes 7 to 28 days:
- yellow, gray foamy vaginal discharge;
- redness of the genital mucosa;
- soreness during intercourse;
- pain when urinating;
- pain in the lower abdomen.
Trichomoniasis is dangerous for pregnant women, as it causes them to premature rupture of the amniotic fluid and give birth prematurely.
It is the cause of paraurethritis, salpingitis.
- metronidazole - 2 g orally once or 500 mg orally 2 times a day for one week;
- tinidazole - 500 mg 2 times a day for 5 days or 2 g once;
- Ornidazole - 500 mg 2 times a day for 5 days or 1.5 g once.
In case of a complicated and recurrent course of the disease, corrections are made to the indicated treatment regimens - higher doses of drugs and a longer intake are recommended. Antimicrobial drugs are also prescribed intravaginally: metronidazole in the form of tablets of 500 mg one at a time for 6 days or a vaginal cream of the same name for 5 days.
During pregnancy, treatment is carried out with the same drugs, but not earlier than the second trimester of pregnancy (13-14 weeks).
Latent sexually transmitted infections (ureaplasmosis, mycoplasmosis, chlamydia)
There are three infectious pathogens, due to which there may be an inflammatory type of smear with an increase in white blood cells, but they are not detected in a regular smear on flora. Only by a special PCR method. These are chlamydia, ureaplasmosis and mycoplasmosis. They are provoked by the following microorganisms: Chlamydia trachomatis, Mycoplasma genitalium, Mycoplasma hominis, Ureaplasma urealyticum, Ureaplasma parvum.
In more than half of cases, latent infections are asymptomatic. If the signs of the disease appear, they are as follows:
- mucopurulent discharge;
- pain during sexual intercourse;
- itching and burning;
- pain when urinating;
- aching pain in the uterus.
Chlamydia also causes intermenstrual bleeding and cervical erosion.
If the infection spreads higher, into the uterus, fallopian tubes, ovaries, then she is diagnosed with sapingoophoritis and endometritis.
Possible treatment regimens (one of the drugs is prescribed orally):
- doxycycline monohydrate - 100 mg 2 times a day for a week;
- azithromycin - 1.0 g, taken once;
- josamycin - 500 mg 3 times a day for a week;
- ofloxacin - 400 mg 2 times a day for a week.
In some cases, longer therapy is required - 2-3 weeks. Pregnant women are treated with the same antibacterial agents.
If microorganisms M. Hominis and / or Ureaplasma spp. Are detected, while high leukocytes are the symptoms of the disease, then the doctor should look for more obvious pathogens: Trichomonas, gonococcus, genital mycoplasma.
Treatment is not carried out in the absence of symptoms of the disease, that is, accidental detection of ureaplasma in an amount of even more than 10 to the 4th degree. Exceptions are expectant mothers. If they have a history of frozen, non-developing pregnancies, premature discharge of amniotic fluid, intrauterine infection of the fetus - they need to be treated.
Violation of the microflora of the vagina or nonspecific vaginitis
In addition to cocci (staphylococci, streptococci, etc.), other conditionally pathogenic representatives of the flora are also the culprits of nonspecific vaginitis: Escherichia (intestinal microorganisms), fungi, Trichomonas.
Symptoms:
- itching and burning;
- pain during intercourse and slight spotting;
- swelling of the vaginal mucosa;
- serous-purulent discharge.
Diagnostics. Microscopy reveals strongly overestimated leukocytes, many gram-positive and gram-negative microorganisms, desquamated epithelium.
Bacterial sowing is carried out to accurately diagnose pathogens and determine their sensitivity to antibiotics.
Stage 1 - antibiotics and antibacterial agents locally:
- Terzhinan;
- Polygynax;
- Neo-penotran;
- Nifuratel;
- Ginalgin;
- Betadine;
- Metronidazole;
- Clindamycin;
- Ornidazole.
Stage 2 - microflora restoration:
- Vagilak;
- Bifidumbacterin;
- Lactobacterin;
- Biovestin.
Gonorrhea
The causative agent of the disease is gonococcus (Neisseria gonorrhoea - gram-negative diplococci). Common cause female and male infertility.
Symptoms:
- difficulty urinating;
- itching in the vagina;
- purulent discharge from the cervix.
If the disease does not affect the urethra and the bladder, then it can be detected only with the help of an analysis - a smear for flora or bacterial culture, since there are no vaginal signs of the disease in women. Leukocytes in a smear for gn are increased and microorganisms, causative agents of the disease, are present.
If the disease rises higher and affects the reproductive organs, then the following symptoms are possible:
- temperature up to 39 degrees and above;
- nausea, vomiting - intoxication;
- menstrual irregularities.
They provoke an ascending infection:
- abortion;
- diagnostic and therapeutic curettage;
- probing of the uterine cavity;
- cervical biopsy;
- intrauterine device.
Usually, the inflammatory process aggravates after menstruation, childbirth.
Gonorrhea is dangerous with the following complications:
- adhesion process in the small pelvis;
- infertility;
- ectopic pregnancy;
- miscarriages and premature birth;
- pelvic pain;
- endometritis.
Treatment is quick and simple, with one of the following drugs:
- Ceftriaxone (500 mg) once intramuscularly;
- Cefixime (400 mg) orally once;
- Spectinomycin (2 g) intramuscularly once.
The same drugs are used to treat pregnant women, and at any time.
True erosion
This is a wound on the cervix. It can appear as a result of intercourse, examination by a gynecologist, taking tests, inaccurate insertion of a suppository (suppository) into the vagina, etc. It heals on its own within 10 days.
It is diagnosed by examination with a gynecological mirror or by. Sometimes suppositories "Depantol", sea buckthorn, methyluracil, douching with calendula are prescribed for its treatment. Different folk remedies and healing products
But, as medical practice shows, within 10 days it goes away on its own - even with treatment, even without.
Herpes simplex virus
If there are no infections, the pathogen is not visible in the smear, hidden infections are not detected, viruses should be looked for by the culture method (analysis for HSV-1,2). This must be done even if the woman has been treated antibacterial drug or an antibiotic broad action, but her leukocytes have only become higher or have not decreased. Antibiotics do not work on viruses.
Also, leukocytosis in the smear is determined with HIV infection.
Oncology - cervical cancer (CC)
Directly malignant tumor rarely provokes an increase in the level of leukocytes. Therefore, we put this reason in the very last place.
With bacterial vaginosis, the white blood cell count is normal. For this reason, it is not on the list above. Signs of vaginal dysbiosis are the presence of key cells in the smear and a decrease in the number of lactobacilli, against the background of the appearance of opportunistic flora (gardnerella, klebsiella, leptotrix, etc.). By the way, very frequent illness during menopause, when the protective function of the vaginal mucosa and cervix becomes weaker due to a lack of estrogen.
The growth of leukocytes depending on the phase of the menstrual cycle and during pregnancy
There are always more leukocytes in the cervical canal than in the vagina. Moreover, this amount grows in the middle of the cycle (when ovulation) and before menstruation. Often, doctors take a smear incorrectly - there is too much material or rub it too thoroughly on a piece of glass, which leads to the destruction of epithelial cells. But it is the ratio of leukocytes to that is the most important sign of inflammation or its absence. Normally, this is about 10 polymorphonuclear leukocytes (PMN, and there are other types) per epithelial cell.
In some women, for some unknown reason, the white blood cells remain high for some time. And this is in the clear absence of inflammation and other good analyzes. Trying to reduce the number of white blood cells or get rid of them altogether should not be. It is not the result of the analysis that is treated, but the disease, if any.
Even more leukocytes become during pregnancy. Physiological process. And if nothing else bothers you, you can be observed. However, doctors are reinsured and often prescribe a local antiseptic for a "bad" smear - Hexicon candles ( active substance- chlorhexidine). They can be used in any trimester of pregnancy. And at the end of it, before childbirth, the vagina is sanitized in this way.
During pregnancy, a cervical plug forms from leukocytes and mucus. It is she who protects the uterus from infection.
Questions from our readers on the topic
Do white blood cells interfere with getting pregnant? If a woman does not have gynecological disease, which would prevent her from conceiving, for example, endometritis, then there will be no infertility for this reason. However, it is imperative to get tested for infections and treat them. After all, it is they who are most often to blame for leukocytosis.
Will they be admitted to IVF with pathology by microscopy? If the problem is only in the number of white blood cells, it may make sense to retake the smear a little later, at another phase of the menstrual cycle. Perhaps there is a medical error during the collection of material or laboratory. But if the result is confirmed, while there are no other problems, the doctor may prescribe an antiseptic with a small course. This is not dangerous.
Is the IUD put on a third or fourth degree of purity smear? No, as this will lead to the spread of microbes into the uterus and endometritis, adnexitis, salpingo-oophoritis.
Is hysteroscopy done for a non-ideal smear? If a routine procedure is scheduled, then it may have to be postponed.
Can leukocytes be elevated due to endometriosis? Yes, it can be.
If after a miscarriage a bad smear - what to do? Get tested for hidden infections and the herpes virus. Remember that the infection interferes with carrying the baby, leading to early termination.
When preparing the material, we used clinical guidelines Ministry of Health of Russia.
In gynecological practice, such a diagnostic method as a smear is used very widely and is often used. This is one of the main standard procedures to help assess the state of the reproductive system in women.
Of course, absolutely all pathologies cannot be detected using this diagnostic method, but at least it will be possible to suspect many of them on the basis of smear results. That is why the analysis is paramount: it allows you to determine the course of further diagnostics, to select deeper and more informative research methods.
What do you look for when decoding an analysis?
The analysis of the smear allows you to assess the indicators: leukocytes, squamous epithelial cells, key cells, mucus in the biomaterial, as well as the content of normal, pathogenic and opportunistic flora. The last category includes yeast of the genus Candida. From pathogenic microorganisms using a smear on the flora, Trichomonas and gonococci can be detected.
A very important diagnostic indicator is the content of leukocytes. These cells of the immune system protect the body from foreign agents, be it microorganisms or destroyed or altered own structural elements.
It is leukocytes or white blood cells that rush to the pathological focus of inflammation in the body, wherever it is. And if the pathology develops in the organs of the reproductive system, these cells will go there.
In women, leukocytes in a smear on the flora are always present, and their norm is a rather arbitrary concept. The fact is that in different parts of the genitourinary system, their permissible value differs. Most of the white blood cells in the cervical region; their lowest content is normally observed in the urethra.
However, for the diagnosis of inflammatory processes, it is important to assess not so much the number of leukocytes as their morphology. This is due to the fact that white blood cells, which have fulfilled their function of "cleaning" the body from pathogens, are destroyed. These white blood cells are called neutrophils.
- Accordingly, the more of them in the smear, the stronger the inflammatory reaction.
In addition, it is important to take into account the fact that the concentration of white blood cells during the menstrual cycle changes under the influence of sex hormones, so if the leukocytes in the smear are slightly increased, this is not necessarily a sign of serious pathology.
In any case, the content of these cells should be assessed only in conjunction with other diagnostic criteria: the composition of normal flora and opportunistic microorganisms, the presence or absence of pathogenic bacteria, the number of epithelial and key cells.
Fast page navigation

As noted above, diagnostic material for conducting a smear on the flora is collected from three points - the cervix, urethra and vagina.
And in each smear obtained, similar indicators are assessed, but the norms of some of them differ depending on the area of localization. Below is a table explaining what is the norm for the content of leukocytes, normal and pathogenic flora, cellular elements and mucus in a smear in women.
| Diagnostic criterion | Normal indicators | ||
| Vagina (V) | Cervix (C) | Urethra (U) | |
| Leukocytes (Le) | 0-10 | 0-30 | 0-5 |
| Slime | moderately | — | |
| Epithelial cells | 5-10 | ||
| Key cells | — | — | — |
| Microflora | Gram-positive bacilli (bifido and lactobacilli) ++++ |
— | — |
| Yeast (Candida) | — | — | — |
| Trichomonas (Trich) | — | — | — |
| Gonococcus (Gn) | — | — | — |
A smear that fully corresponds to the parameters of the norm is a rather rare phenomenon. However, minor deviations from the norm are allowed when it comes to the vagina. The urethra and cervix, if there are no pathologies, should be sterile - no microflora should be there. With regard to the vagina, the situation is ambiguous.
Depending on the content of various microorganisms, 4 degrees of purity are distinguished.
The ideal smear, which does not contain leukocytes and pathogenic flora, corresponds to the first. However, most women cannot boast of such results. Often in the vaginal discharge, individual leukocytes are found within the normal range (up to 10 pcs.), An insignificant content of epithelial cells and opportunistic bacteria. This picture is not characterized as pathological, and the smear belongs to the second degree of purity.
If gram-variable coccal flora, gram-negative bacilli or yeast cells are found in the vaginal discharge against the background of a decrease in the concentration of lactobacilli and bifidobacteria (Doderlein sticks), this is a reason for further diagnosis. Such a smear is classified as the third degree of purity. Leukocytes in it exceed the norm, and also contains a lot of mucus.
In a smear of the fourth degree of purity, Doderlein sticks (normal flora) are very little or not at all, leukocytes cover the entire field of view, the content of mucus and epithelial cells is increased. In addition, pathogenic microorganisms are found in large numbers. This condition requires prompt treatment.
Causes of increased white blood cells in a smear
If leukocytes are increased in a woman's smear, the reasons for this are associated with inflammatory processes... The greater the concentration of these cells, the more pronounced the process. However, this indicator should be assessed in conjunction with other diagnostic aspects.
For example, an increase in mucus content is noted with the development of infections. So the body seeks to "cleanse" of pathogens. An increase in the number of epithelial cells, as well as leukocytes, warns of inflammation.
According to some laboratories, the content of these elements up to 10 in the field of view is allowed, but this indicator varies depending on the phase of the menstrual cycle and should not be interpreted without looking at other diagnostic signs.
Key epithelial cells are called epithelial cells dotted with gardnerella bacteria. This is the so-called "bacterial sand". If such cells are detected in a smear, the likelihood of developing bacterial vaginosis (gardnerellosis) is high.
The detection of a large number of candida in a smear against the background of suppression of the normal flora is a sign of thrush. This is due to the fact that with a decrease in the concentration of Doderlein's sticks, which produce lactic acid, the pH of the vagina rises.
This condition leads to the active growth of conditionally pathogenic flora, including Candida. In an acidic environment, these microorganisms cannot multiply, and thus bifidobacteria and lactobacilli inhibit the process of colonization of the vagina.
Gonococci and Trichomonas are pathogenic microorganisms. They should not be in the smear under any circumstances. The detection of these bacteria signals the development of gonorrhea or trichomoniasis.

Conception launches a cascade of processes in a woman's body, and for all of them to proceed smoothly, the balanced work of the endocrine organs that produce hormones is important. Changing their balance causes powerful restructuring in the work of organs and systems.
So, sex hormones - progesterone and estrogens - stimulate the work of squamous epithelial cells. They begin to actively synthesize glycogen, which supports the reproduction of normal flora. By breaking down this compound, Doderlein's sticks produce large amounts of lactic acid, an acidifying medium, and thus provide protection against infections.
However, against the background physiological decline immunity during pregnancy, this measure is often not enough. When the balance of hormones changes, many expectant mothers begin to suffer from thrush or other pathologies caused by opportunistic microorganisms.
Against this background, an increased content of leukocytes is noted in the smear. Often, the concentration of such cells in the vagina in pregnant women exceeds the norm - up to 10 pcs. in one field of view.
- If their content is no more than 15-20, and the expectant mother does not experience any signs of pathology, and the rest of the smear indicators are normal, you should not worry.
It is important to note that the concentration of leukocytes in the urethra and cervix should not change. The rates of these indicators are the same as for non-pregnant women. Elevated leukocytes in the urethra are a sign of inflammation. This condition requires diagnosis and treatment.
During pregnancy, the leukocyte count should be monitored especially carefully, since it warns of the manifestation of pathologies chronic course... It is better for the expectant mother to undergo an examination once again.
Proper preparation for the smear test
Like most diagnostic research in medicine, a flora smear requires preparation. When going to a gynecologist, a woman should remember that the result of the analysis will be reliable only if the following recommendations are followed:
- observe sexual rest before the delivery of the biomaterial for at least 2 days;
- refuse to use lubricants, vaginal suppositories, creams on the eve of the study;
- do not wash off using gels and other means for intimate hygiene;
- refrain from taking the test after a course of antibiotics (at least 10 days);
- do not urinate less than 2 hours before visiting a gynecologist;
- do not get tested during menstruation.
Intimacy, any means topical application, antibiotics distort data on the real state of the microbial biocenosis of the genitourinary system in women.
In the process of urination, diagnostically significant objects of study are washed off: cellular elements, microorganisms, which also changes the overall picture. Menstruation makes it difficult to obtain material for diagnosis - it will be "contaminated" with a large number of red blood cells.
Indications for taking a smear
A smear in women involves taking a biomaterial not only from the vaginal mucosa. Samples for analysis are also taken from the urethra, cervix.
After the onset of sexual activity, every woman should undergo this diagnostic procedure regularly: at least 1 time per year. In addition to preventive examinations, a smear must be taken during pregnancy. If there are no alarming symptoms, the expectant mother will have to go through this procedure twice: at the very beginning of pregnancy when registering and in the third trimester, after 30 weeks.
However, a significant reason for passing a smear is the appearance in any woman, both pregnant, and there is no following symptomatology:
- discoloration and consistency of discharge;
- the appearance of discomfort when urinating;
- itching in the groin area;
- unpleasant odor of discharge;
- burning sensation in the vagina;
- pain in the abdomen at rest or with intimacy.
In addition, it should be remembered that prolonged antibiotic treatment can affect the vaginal microflora in a negative way: cause the death of beneficial bacteria, which will be replaced by opportunistic inhabitants. Against this background, candidiasis, bacterial vaginosis often develop and they can be diagnosed with a smear on the flora. That is why it is advisable to take such an analysis after completing the course of antibiotic therapy.