Why is streptococcal infection dangerous and how to treat it? Streptococcus. Symptoms, causes, types, analyzes and treatment of streptococcal infection Means streptococcus
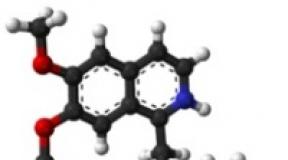
Streptococci Are bacteria that live in the bodies of animals, on the skin, in the respiratory organs and in the intestines of humans. Many of these microorganisms are not dangerous for people, that is, they belong to the saprophytic microflora. However, there are also pathogenic streptococci that cause serious diseases, ranging from angina and streptoderma, ending with meningitis and sepsis. In addition, streptococci play an important etiological role in the development of a number of systemic ailments - rheumatism, glomerulonephritis, endocarditis, etc.
Diseases caused by streptococci
All streptococci are divided into four groups (depending on biochemical, biological and other properties):
- Alpha hemolytic.
- Beta hemolytic (A, B, C).
- Gamma hemolytic.
- Non-hemolytic.
Nonhemolytic streptococci they are harmless to humans - they do not cause any diseases, which cannot be said about their hemolytic relatives.
So, alpha hemolytic streptococci are the cause of the development of infective endocarditis (inflammation of the inner lining of the heart and damage to the heart valves), purulent periodontitis (inflammation of the connective tissue surrounding the tooth root), and when penetrating into the internal organs, abscesses in the internal organs. In addition, microorganisms of this group play a leading role in the occurrence of caries.
- the most pathogenic among all streptococci. It is with them that the development of the following diseases is associated:

Finally, gamma hemolytic streptococci in most cases, they are saprophytic (normal) microflora of the intestines and upper respiratory tract, which, under certain conditions, can cause infections of the urinary system, wounds, as well as septic endocarditis.
How does streptococcus get infected?
Sources of pathogenic streptococci are sick people and healthy carriers. Infection occurs mainly through airborne droplets and contact-household (through common dishes, dirty hands, patient care items, etc.) ways. At the same time, the pathogen enters the body through the respiratory tract, less often through lesions on the skin, as well as the umbilical wound in newborn babies.
After colonization in the primary focus, streptococci begin to actively release enzyme substances, thanks to which microbial cells can penetrate into the blood and lymph. In addition, streptococci in the process of vital activity produce toxins, due to which patients develop severe intoxication syndrome and other signs of the disease.
In addition to the pathways of streptococcus infection described above, autoinfection is also possible.For example, when streptococci enter the blood from abscesses on the skin when they are unsuccessfully squeezed out, from purulent foci in the oral cavity during dental manipulations, as well as from the nasopharynx when removing palatine tonsils or adenoids. In this way, microorganisms spread to the internal organs and cause the development of purulent processes there.
But systemic diseases provoked by streptococci arise not so much because of infection, but because of allergization of the body. The antibodies to streptococci produced by the system are capable of attacking their own tissues in the joints, kidneys, and heart. Therefore, when these microorganisms are present in the human body for a long time or re-enter it, as a result of the hyperimmune reaction, the tissues of these internal organs are damaged.
Symptoms of the most common streptococcal diseases

In childhood, streptococcal infection most often occurs in the form of scarlet fever, and in adults, angina. If you do not start taking antibiotics for these diseases in a timely manner and allow long-term persistence of streptococcus in the body, it is possible to develop rheumatism, endocarditis, arthritis and glomerulonephritis.
Streptococcal angina is manifested by the following symptoms:
- A sharp jump in body temperature to high numbers (39 degrees and above).
- Weakness, chills.
- Joint aches.
- An increase in the palatine tonsils (they seem to swell and become covered at first with small abscesses, and over time - with yellowish purulent deposits).
- Increased cervical lymph nodes.
In addition to the defeat of the tonsils and internal organs (purulent processes in them do not have symptoms characteristic of streptococcal infection), streptococci cause specific diseases of the skin:

Streptococcus in children
For newborns and infants, streptococcal infection is a great danger. They develop skin diseases (impetigo, ecthyma vulgaris), as well as very severe meningitis and sepsis, due to infection with streptococcus from their mother in utero or during childbirth. In order to prevent infection of newborns, all pregnant women are examined for streptococcus in the last trimester, risk factors are assessed (sowing of pathogenic streptococci from urine during pregnancy, the presence of neonatal streptococcal infection in previously born children, etc.) and, if necessary, prophylactic antibiotic therapy is carried out.
In children after a year, streptococcal infection most often manifests itself in the form of scarlet fever.
The symptoms of this disease are as follows:
- Rash, after its disappearance, the skin is very flaky.
- Angina.
- "Raspberry" language.
- Heat.

This disease, against the background of antibiotic therapy, almost always ends with a full recovery on days 7-10. Subsequently, the ingestion of pathogenic streptococci leads to the development of angina, while repeated cases of scarlet fever are very rare.
 Most diseases caused by streptococci are diagnosed by doctors according to a specific clinical picture (this applies to scarlet fever, tonsillitis, erysipelas, streptoderma). To confirm the diagnosis, an analysis is performed for streptococcus (they take swabs from the surface of the tonsils, inflamed foci on the skin, sow urine, pus, blood, etc.). For a faster diagnosis of streptococcal infection, modern rapid tests have been increasingly used recently.
Most diseases caused by streptococci are diagnosed by doctors according to a specific clinical picture (this applies to scarlet fever, tonsillitis, erysipelas, streptoderma). To confirm the diagnosis, an analysis is performed for streptococcus (they take swabs from the surface of the tonsils, inflamed foci on the skin, sow urine, pus, blood, etc.). For a faster diagnosis of streptococcal infection, modern rapid tests have been increasingly used recently.
Treating streptococcal infection
 The main and mandatory component of anti-streptococcal treatment is .
It allows you to eliminate the infection much faster and prevent the development of complications from the heart, kidneys and other organs. In the case of sore throat and scarlet fever, no topical antiseptic can replace antibiotics. The choice of a specific antibacterial agent for the treatment of these diseases is determined by the sensitivity of the microorganisms. And since all streptococci are sensitive to penicillins, with streptococcal infection, drugs of this group are primarily used, and as an alternative, cephalosporins, macrolides.
The main and mandatory component of anti-streptococcal treatment is .
It allows you to eliminate the infection much faster and prevent the development of complications from the heart, kidneys and other organs. In the case of sore throat and scarlet fever, no topical antiseptic can replace antibiotics. The choice of a specific antibacterial agent for the treatment of these diseases is determined by the sensitivity of the microorganisms. And since all streptococci are sensitive to penicillins, with streptococcal infection, drugs of this group are primarily used, and as an alternative, cephalosporins, macrolides.
In case of skin diseases caused by streptococcus, the appropriateness of systemic antibiotic therapy is determined by the doctor individually. However, erysipelas and prolonged streptoderma with a widespread inflammatory process are always an indication for the appointment of antibiotics.
 Treatment with folk remedies for streptococcal infection can also be used, but only as an auxiliary. In particular, infusions of medicinal herbs (oak bark, chamomile, string) are considered effective. They are recommended for gargling and treating affected skin. In addition, you can cook rosehip decoctions, cranberry fruit drinks and take them inside. These drinks contain a lot
Treatment with folk remedies for streptococcal infection can also be used, but only as an auxiliary. In particular, infusions of medicinal herbs (oak bark, chamomile, string) are considered effective. They are recommended for gargling and treating affected skin. In addition, you can cook rosehip decoctions, cranberry fruit drinks and take them inside. These drinks contain a lot
Streptococcus is one of the types of pathogenic microbes that are normally found in the human body. Under the influence of certain factors, they are able to adopt pathogenic properties.
As a result of a change in their status, microbes lead to the development of serious diseases. The degree of damage to the body depends on the type of bacteria and the protective functions of the immune system.
Non-hemolytic bacteria
Non-hemolytic bacteria are represented by a heterogeneous group. Most of these microorganisms changes the natural color of blood to green... This type of bacteria is found in the mouth. By their pathogenicity, they are among the safest.
Beta hemolytic
The main type of streptococci are beta-hemolytic. They cause diseases of various organs and body systems. They are divided into the following groups of streptococci: A, B, C, D, G, green and peptostreptococci.
Group A
They are provocateurs of negative reactions from the body. They cause the development of angina, scarlet fever, abscesses, infectious skin lesions.
Group B
Group B streptococci were first discovered in cattle. Laboratory and instrumental studies have shown the relationship between the penetration of bacteria into the body and the development of sepsis.
A high probability of such an impact is recorded in newborns. The bacteria are based on capsular polysaccharides characteristic of the bacterial serotype.
Group C and G

Pathogenic microorganisms of groups C and G cause purulent infections in the body (sepsis, purulent arthritis, etc.)
Pathogenic microorganisms of groups C and G belong to the hemolytic type. In their properties, they are similar to the representatives of category A. Penetrating into the body, they provoke soft tissue infections, sepsis, purulent arthritis, inflammation of the lungs and sore throat.
Sepsis is more common in older people.
Group D
Streptococci belonging to D are presented in a separate category. They differ in biochemical properties and the ability to grow in the environment. Enterococci also fall into this category, they prevail mainly in elderly people.
Greening streptococci
Greening streptococci are represented by a specific group of pathogenic microorganisms. They are the main provocateurs of infective endocarditis. Bacteria are normally found on the oral mucosa.
They live on teeth and gums, under the influence of adverse factors take on pathogenic properties... In most cases, this leads to the formation of caries, damage to the liver and intestinal microflora.
Peptostreptococcus streptococci
Peptostreptococci previously belonged to the group of anaerobic microorganisms. Today they are represented by a separate genus. They form the basis of the normal microflora of the intestine, vagina and mouth.
Together with other bacteria, they can cause abscesses, periodontitis, oncology and pneumonia.
These are the main types of streptococci that can harm the body. All of them are united by one beta-hemolytic species.
Streptococcus viridans
This is a special group of microorganisms that are present in the normal microflora of the intestines, mouth and digestive system. In a woman's body, bacteria are found in the genitals and respiratory tract.
If a microbe enters the blood, brain or other organs and systems, nothing good can be expected from this effect.

Timely access to a doctor prevents complications and the spread of pathology
This type of bacterium is called greening or hemolytic. In natural conditions, it is found everywhere. In many cases, it is perfectly safe and harmless.
However, under the influence of some factors, the bacteria can cause serious abnormalities in the body. The most common diseases are abscess, pneumonia, pharyngitis, sepsis, and nephritis.
It is possible to eliminate the pathogenic microorganism by using drugs of the penicillin series. carried out under the guidance of a specialist.
Streptococci represent a large group of dangerous and safe microorganisms. In the human body, they are located on the mucous membranes and form the basis of normal microflora.
Under the influence of certain factors, microbes take on pathogenic properties and become dangerous to the body. In this form, they can cause serious diseases that threaten human life. A timely visit to a doctor prevents the spread of pathology and its complications.
In contact with
Streptococcus is a gram-positive microorganism that causes a group of infectious diseases that affect mainly the skin, respiratory and genitourinary systems. This pathogen is present in any healthy organism and often lives without manifesting itself in any way. But as soon as provoking factors appear, he starts an attack.
Causes and methods of infection
The source of infection of pathogenic streptococci is a sick person or a healthy carrier of these bacteria. Streptococcal infection can be transmitted in several ways:- aerosol or airborne (when coughing, sneezing, talking, kissing - bacteria are released with particles of saliva);
- contact-household (bacteria are transmitted by contact with objects, dishes, linen used by a sick person);
- sexual(transmission of pathogens occurs through sexual intercourse);
- vertical (infection occurs during pregnancy and childbirth from mother to child).
At-risk groups
There is a high risk of contracting streptococcal infection in newborns, pregnant women, burned, wounded and postoperative patients. Their immune system is weakened and unable to resist pathogenic agents.In addition, the likelihood of infection is increased by factors such as:
- unhealthy habits - smoking, alcohol, drugs;
- long-term use of antibiotics;
- visiting beauty salons - manicure, pedicure, piercing, tattooing;
- hypovitaminosis;
- work in polluted and hazardous industries.
Harm to the body
Streptococci have the pathogenic property of producing toxins and enzymes that, penetrating the blood and lymph, can cause an inflammatory process in the organs. This pathogen produces the following substances:- erythrogenin - expands small blood vessels, provokes the appearance of a rash (with scarlet fever);
- leukocidin - destroys white blood cells, thereby reducing the immune system;
- streptolysin - has a destructive effect on heart and blood cells;
- necrotoxin - causes tissue necrosis upon contact with them.
- pathology of the endocrine system.
- HIV infection;
- hypothermia;
- ARI,;
- cuts, injuries, burns to the throat, mouth and nasal cavity;
Streptococci that live in hospital walls are considered more dangerous because they are resistant to drugs and difficult to treat.
Classification of streptococci
Pathogenic streptococcus has several types, each of which has a specific area of \u200b\u200bdamage.
- Alpha hemolytic streptococcus - is a less dangerous microbe. Sometimes it causes inflammation in the throat, but more often it is asymptomatic.
- Beta hemolytic streptococcus - a pathogenic agent that affects the skin, respiratory tract, genitourinary system.
- Nonhemolytic or gamma streptococcus - a safe representative that does not destroy blood cells.
Group A causative agent - cause pharyngitis, tonsillitis, sore throat, scarlet fever, and can also give complications such as glomerulonephritis and rheumatism. Form purulent processes in the organs.
Group B streptococci - in many people it does not cause side symptoms, however, with a large number of them in a woman's vagina, vulvovaginitis, endometritis and cystitis can begin. Transmission of the pathogen during pregnancy from mother to child is dangerous for the development of pneumonia, meningitis or sepsis in the child. In men, the presence of this type causes urethritis.
Group C and G streptococci - cause hemolysis of cells, provokes the development of sepsis, purulent arthritis, soft tissue infections.
Group D streptococci - in addition to the actual D pathogens, this also includes enterococci. They cause purulent inflammation of the abdominal cavity.
Streptococcus pneumoniae - is the cause of pneumonia, sinusitis, otitis media, meningitis.
Symptoms
The symptomatology of the disease will depend on the type of pathogen and the place of its localization and reproduction. The incubation period is from several hours to 4-5 days.Strep throat - causes diseases such as tonsillitis, pharyngitis, scarlet fever. Clinically characterized by the following features:
- sore throat and sore throat when swallowing;
- the appearance of plaque on the tongue and tonsils;
- cough;
- chest pain;
- fever;
- rashes on the skin and tongue of a raspberry hue - with scarlet fever.

Streptococcus in the nose - can cause rhinitis, sinusitis, sinusitis, and also cause the development of otitis media. The clinical picture of streptococcus reproduction in the nasal cavity looks like this:
- nasal congestion;
- purulent discharge from the nose;
- headaches, especially when the body bends;
- weakness, poor health.
- redness - there is a clear border between healthy and affected skin areas;
- the presence of bubbles with purulent contents;
- body temperature reaches 38-39 ° C;
- soreness of the skin when touched.
Streptococcus in gynecology - is often the cause of endometritis, vulvovaginitis, endocervicitis, cystitis. The general picture can be manifested by the following signs:
- lower abdominal pain;
- vaginal discharge;
- enlargement of the uterus;
- increased body temperature;
- pain or itching when urinating.
- Stage 1 - the penetration of the pathogen and the development of the inflammatory focus.
- Stage 2 - the spread of pathogenic bacteria throughout the body.
- Stage 3 - the body's immune response.
- Stage 4 - damage to internal organs.
Diagnostic research methods
In order to identify the pathogen itself and its type, as well as to determine its resistance to antibacterial drugs, the following laboratory tests are needed:- bacteriological analysis from palatine tonsils, from lesions on the skin, from the vagina, separated sputum;
- general analysis of blood and urine;
- additional methods of examination - electrocardiogram, x-ray of the lungs, ultrasound of internal organs.
Treatment principles
Drug therapy for streptococcus should be comprehensive, that is, it includes several stages:- Antibacterial therapy - Ampicillin, Augmentin, Amoxicillin, Benzylpenicillin, Cefotaxime, Ceftriaxone, Doxycycline, Claritomycin. The choice of the drug, dosage and course of treatment are decided by the attending physician.
- Immunostimulants - Immudon, Lizobact, Immunal, ascorbic acid.
- Probiotics to restore bowel function after taking antibiotics - Linex, Bifidobacterin, Enterojermina.
- Symptomatic treatment - Pharmazolin (for nasal congestion), ibuprofen (at high temperatures).
- Vitamin complexes.
The patient must comply with bed rest, eat easily digestible food and drink plenty of fluids.

Folk remedies
The use of folk methods can only have an effect in combination with medications. In the treatment of streptococcal infection, the following agents have proven their beneficial effect:- Gargling with herbal infusions - propolis.
- Apricots. Eat mashed potatoes from this fruit 3 times a day; lesions on the skin can also be lubricated with pulp.
- ... Take 50 g of fruit in 500 ml of water and boil the mixture for 5 minutes. Let it brew a little and consume 150-200 ml 2 times a day.
- Onions and garlic are natural remedies against infection. It is better to consume them raw 1-2 times a day.
- Chlorophyllipt. Can be used as a spray, oil and alcohol solution. Well relieves inflammation from the tonsils.
- Hop. Pour 10 g of cones with 500 ml of boiled water and cool. Take 100 ml on an empty stomach 3 times a day.
Treatment with traditional medicine should be carried out strictly after consulting a doctor.
Features of the clinical picture and methods of treatment of infection in newborns and children
Streptococcal infections for newborns and young children pose a serious danger. Infection of the fetus occurs through the amniotic fluid, birth canal or breast milk. The manifestation of this infection is observed already in the first hours after birth.If the mother infects the baby during pregnancy, the baby may be born with meningitis or sepsis. Immediately after birth, you can notice skin rashes on the body, fever, bleeding from the mouth, hemorrhages under the skin.
The tactics of treatment are selected by the doctor, but accordingly, first of all, it is necessary to start antibiotic therapy.
Features of the course and treatment of streptococcal infection in pregnant women
Streptococcus can be present in the vaginal environment in women asymptomatically, but during pregnancy the body weakens, immunity falls, and the pathogen already manifests itself from the pathological side. It causes cystitis, endometritis, cervicitis, colpitis, postpartum sepsis, glomerulonephritis, and that can lead to infection of the fetus.Streptococci are chain-shaped bacteria that live in the microflora of the human body. Very often they coexist with an infection such as Staphylococcus aureus. With a favorable environment for bacteria, an inflammatory or infectious process may develop. Since these organisms do not form spores, they quickly die under the influence of sunlight and special preparations.
Streptococcus Viridans (Viridans) make up about 30-60% of the total number of bacteria in the human body. They enter the body along with the food consumed. Most often, bacteria are localized in the digestive tract, mouth, genitals, respiratory tract mucosa and on the skin.
Transmission path
The development of the pathological process is possible only if there is a favorable environment for this. Infection with staphylococci and streptococci is possible in the following ways:
- autoinfection;
- infection from the outside.
In the first case, infection is possible due to the following circumstances:
- self-removal of boils;
- dental operations;
- infectious diseases in the oral cavity;
- chronic;
- removal of tonsils.
The infection is transmitted in the following ways:
- domestic;
- sexual;
- airborne;
- food;
- placental (from an infected mother to a child).
The greatest danger is a person whose infection is located in the respiratory tract. This is possible with angina or scarlet fever.
Streptococcus can provoke the development of such diseases:
- erysipelas;
- bronchitis;
- abscess of soft tissues.
According to statistics, the disease is diagnosed in 15% of pregnant women. Fetal infection with the development of an underlying disease is diagnosed in 0.3%. Most often, streptococcal infection provokes the development of pneumonia and tonsillitis.
Streptococcal pneumonia
When an infection enters the respiratory tract, pneumonia develops. But it should be noted that such pathological processes are possible only if the person's immunity is too weakened.
The infection leads to the fact that inflammation begins in the alveoli, which quickly captures adjacent tissues. This leads to the formation of exudate in the lungs. Ultimately, this leads to disruption of gas exchange and pneumonia.
Streptococcal pneumonia symptoms:
- fever;
- coughing for no apparent reason;
- dyspnea.
The most severely streptococcal pneumonia is tolerated by children under 3 years of age and the elderly. Especially if the person has a weakened immune system.
Possible consequences of streptococcal pneumonia:
- lung abscess;
- pneumosclerosis.
But if you start treating pneumonia caused by this infection, then complications can be avoided.
The main reasons for the development of streptococcal sore throat include the following factors:
- primary infection with a child's body;
- previously transferred infectious or viral diseases;
- long-term antibiotic treatment, chemotherapy;
- weakened immunity.
Children are more susceptible to strep throat due to the fact that their immune systems are much weaker than in adults.
Symptoms of the development of the disease in children:
- irritability, moodiness;
- sore throat;
- refusal to eat, significant deterioration in appetite;
- unstable body temperature;
- discharge from the nose, yellow, greenish;
- nausea and vomiting.
Such symptoms in children indicate strong or. Therefore, some parents simply do not seek medical help in a timely manner, which greatly aggravates the situation.
Due to the fact that such an infection quite often grows along with Staphylococcus aureus, the development of other, background diseases is possible. Also, do not forget that angina can cause more complex and dangerous diseases in children.
With streptococcal sore throat, children may experience a dry cough and headache. In general, the clinical picture depends on the characteristics of the child's development and general health. In more rare clinical cases, the manifestation of streptococcal infection in children may be accompanied by a rash in the nose, on the skin around the nose. As a rule, such infections are accompanied by Staphylococcus aureus.
Possible complications:
- meningitis;
- otitis;
- pneumonia or chronic bronchitis;
- abscess.
Such complications in children can be avoided by promptly seeking medical attention.
Symptoms
There are no uniform symptoms for this infection. The clinical picture depends on what kind of disease is provoked by streptococcus. The most common symptoms of this infectious disease are:
- unstable body temperature;
- intoxication of the body;
- rashes on the skin;
- enlarged lymph nodes;
- sore throat, for no apparent reason;
- low blood pressure;
- tissue necrosis.
In addition to the above symptoms, the patient may often be disturbed by discomfort in the kidney area. In this case, the general list of symptoms can be supplemented with the following signs:
- trouble urinating;
- discomfort in the area of \u200b\u200bthe affected organ;
- when analyzing urine, an increased level of hemoglobin and creatinine is observed.
The most sure sign of the development of streptococcal infection can be considered the following symptoms:
- redness of the affected area;
- the formation of pus;
- painful sensations when pressed.
Due to the fact that toxins can enter the bloodstream, a person may be in a state of shock.
When the first symptoms appear, you should immediately consult a doctor. Self-medication can only aggravate the situation and give rise to the development of another background ailment.
Streptococcus groups
In official medicine, it is customary to distinguish between the following groups of this infection:
- greening or alpha hemolytic;
- beta-hemolytic (group A streptococci);
- non-hemolytic.
Group A streptococci (pyogenic streptococcus) cause various ailments in humans. The frequency of these diseases depends on the season. So, for children, the greatest danger is streptococci in the throat. In winter, streptococci in the throat can cause the development of tonsillitis, pharyngitis,.

Infection during pregnancy
According to statistics, streptococcal infection is diagnosed in 20% of women during pregnancy. The etiological factors include the following:
- non-observance of intimate hygiene;
- wearing synthetic, tight underwear;
- the use of non-sterile items for personal hygiene;
- unprotected sex.
It should be noted that this infection is present almost constantly in the vagina. But during pregnancy, the woman's body is weakened, which gives rise to the development of this infectious organism. Often, streptococcus can be activated simultaneously with Staphylococcus aureus.
Possible complications during pregnancy:
- severe allergic diseases;
- purulent otitis media;
- diseases of the cardiovascular system;
- sepsis;
- diseases of the genitourinary system.
As for the newborn, the following complications may develop:
- sepsis;
- meningitis;
- pneumonia;
- neurological disorders.
If during pregnancy streptococcus is diagnosed along with Staphylococcus aureus, then the development of allergic diseases in the baby is possible.
Neurological disorders are provoked by streptococcus agalactia. It is noteworthy that this subtype of infection can be diagnosed only during pregnancy. In addition to disorders in the nervous system, streptococcus agalactia can cause premature birth and even fetal death. As a rule, the infection is diagnosed at 32–33 weeks of pregnancy.
It should be noted that Staphylococcus aureus causes practically the same diseases as streptococcal infection. The main difference is only in the manifestation of the clinical picture and the rate of development of the disease. Since the immune system is weakened during pregnancy, the risk of developing any disease increases significantly.
To avoid this, during pregnancy, you should be especially careful about your health and follow the rules of personal hygiene. Thus, the development of diseases caused by streptococcus and Staphylococcus aureus during pregnancy can be prevented ..
Streptococcus in a vaginal smear may indicate:
- urethritis.
Streptococcus in a smear of the pharynx or pharynx indicates a sore throat, pharyngitis, laryngitis.
As for streptococcus in the nasal mucosa, the following diseases are possible:
If it is impossible to make an accurate diagnosis using the above methods, then differential diagnosis is carried out.
Treatment
The main course of treatment for streptococcus consists of taking antibiotics. Since strong medications will affect the body for a long time, treatment includes taking medications to restore microflora:
- linex;
- acipol;
- bifiform;
- cetrin;
- zodak.
Treat the infection only under the supervision of a doctor. If the body is in the stage of severe intoxication, bed rest should be observed. Excessive physical activity can lead to serious complications.
Please note that it is impossible in any case to remove plaque from the throat on your own with streptococcal sore throat. This only leads to a worsening of the disease. It is also not recommended to treat such diseases with folk remedies without a doctor's recommendation.
You can use folk remedies for treatment only after consulting a doctor. As a rule, gargle with a decoction of chamomile and sage is prescribed.
Prevention and prognosis
The main preventive measures are aimed at observing the rules of personal hygiene and strengthening the immune system. If treatment is started in a timely manner, complications can be avoided.
Streptococci got their name from the Greek words "chain" and "bead", because under a microscope they look like balls or ovoids and resemble beads strung on a string.
Streptococcus is a conditionally pathogenic microorganism, is a gram-positive bacterium and is present in the human body. For the time being, the microbe behaves "approximately", but as soon as the immune system is weakened, streptococcus is activated and becomes a source of various diseases.
Views
About 40 species of streptococci are known. Depending on the presence of certain polysaccharides in their composition, these microbes were divided into groups from A to V.
The pathogenic streptococci, the most dangerous for humans, are those that are in group A. In turn, group A streptococci are divided into 3 subgroups, taking into account their ability to destroy red blood cells:
- alpha green streptococci;
- beta-hemolytic streptococci;
- gamma streptococci.
Streptococci of group A of the beta-hemolytic subgroup are called pyogenic streptococci (Streptococcus pyogenes). They are responsible for the development of many diseases:
- scarlet fever, tonsillitis;
- pharyngitis, bronchitis, pneumonia.
- abscess, sepsis;
- osteomyelitis;
- lesions of the genitourinary system.
Causes
The source of infection is a sick person or a carrier of streptococcus (much less often). Infection occurs in several ways:
- contact and household (penetration of a microbe through damaged skin during close contact with a sick person or through infected household items: dishes, toys, bedding, etc.);
- airborne droplets (with particles of mucus and saliva when coughing, sneezing, screaming);
- vertical (infection of the fetus during pregnancy and childbirth);
- sexual (unprotected sexual intercourse, non-observance of personal hygiene rules).
In addition, the risk of infection with streptococcus increases sharply with the weakening of the body's defenses (hypothermia, chronic diseases, HIV infection, etc.).
Diagnostics
Differential diagnosis of streptococcal infection should be carried out to distinguish
- streptococcal sore throat from diphtheria and infectious mononucleosis,
- scarlet fever from rubella and measles,
- erysipelas from dermatitis and eczema.
The diagnosis of diseases caused by streptococcus is established on the basis of a characteristic clinical picture.
Also, to clarify the nature and severity of the infection and in order to exclude complications, the following are prescribed:
- general blood and urine tests;
- electrocardiography;
- radiography of the lungs;
- Ultrasound of internal organs;
- other additional methods of examination.
Bacteriological studies are shown:
- sputum cultures;
- taking swabs from the tonsils, affected areas of the skin.
Streptococcus treatment
Streptococcus is treated by the doctor whose profile corresponds to the form of the disease. For example, a dermatologist treats erysipelas, abscesses, phlegmon and osteomyelitis - a surgeon, cystitis is supervised by a urologist, and so on.
Etiotropic therapy (elimination of the cause of the disease) consists in the appointment of penicillin antibiotics:
- ampicillin;
- oxacillin;
- benzylpencillin;
- amoxicillin;
- bicillin-5;
- other.
These are the only antibiotics to which streptococci are unable to acquire resistance.
Depending on the severity and form of the disease, antibiotics are prescribed orally or intramuscularly 4 times a day, the duration of the course is 5-10 days.
In case of allergy to penicillins, antibiotics from the macrolide group (erythromycin, oleandomycin) are prescribed.
For the purpose of detoxification, an abundant drink of up to three liters per day is indicated. In parallel, ascorbic acid is prescribed to strengthen the walls of blood vessels. Symptomatic drugs to lower the temperature (paracetamol, aspirin) are taken for no more than three days.
With streptococcal infection in the oropharynx, rinses of the mouth and throat with a solution of furacillin are prescribed (with a hygienic, but not with a therapeutic purpose).
Consequences and forecast
The consequences of streptococcal infection are due to the absorption of endotoxin, which is released when bacteria die. This provokes allergic reactions and leads to the development of such severe and chronic diseases as glomerulonephritis, rheumatism and collagenosis.
The development of streptococcal infection depends on the form and severity of the disease. With damage to internal organs, the prognosis for life is relatively favorable.
Symptoms of streptococcal infections
Common forms:
The disease begins abruptly, with a rise in temperature to high numbers and severe intoxication (weakness, lack of appetite, nausea, headache, sore throat when swallowing). After a few hours (after about 6-12 hours) a rash appears. First, it becomes noticeable on the hands, feet and upper body, then spreads throughout the body (on days 2-3 of the illness). The rash disappears in the second week.
Acute tonsillitis is said to be when the tonsils become inflamed. Streptococcus, having penetrated into the tonsils, causes an inflammatory process in them, the nature of which can be different (catarrhal, follicular, lacunar, necrotic tonsillitis).
If the barrier function of the tissues that surround the tonsils is reduced, then they are also involved in the inflammatory process, resulting in paratonsillitis (paratonsillar abscess - acute inflammation in the soft tissues of the tonsils).
The incubation period ranges from several hours to 2-5 days. The disease begins acutely and suddenly. There is a chill, severe weakness, headache, the inability to swallow is felt, there is a feeling of aching in the joints.
With a severe course of angina, the chill continues for several days. The headaches are dull and last for 2-3 days. The feeling of aches in the joints, pulling pain in the lower back persists for 1-2 days. Sore throat is mild at first, then intensifies and reaches a peak on the second day.
Angina differs from scarlet fever in the absence of a rash.
When examining the tonsils, their significant increase and the presence of a yellow-white purulent plaque or whitish vesicles (follicles) are noted.
Erysipelas is acute and, as a rule, severe. There is a significant increase in temperature (39-40 ° C), severe headache, severe weakness, chills, muscle pain. Against the background of intoxication, consciousness becomes confused, the patient begins to delirium.
A characteristic sign of erysipelas is local inflammation of skin areas. The site of inflammation rises above the level of healthy skin, is distinguished by its bright red color, fever and clear boundaries. In the case of a severe course of the disease, bubbles and hemorrhages appear on the affected area.
Inflammation of the bone marrow that invades all layers of the bone is called osteomyelitis. Purulent inflammation develops, as a result of which the bone marrow necrotizes, and an abscess arises at this place, which tends to break out.
People with sharply reduced body defenses may develop sepsis. From the primary focus, streptococcus enters the bloodstream and spreads throughout the body (septicemia). At the same time, new foci of infection are formed in different places - abscesses in the lungs, liver, kidneys, brain, etc. (septicopyemia).