Systolic dysfunction. Miocardium diastolic dysfunction systolic heart dysfunction
The diastolic dysfunction of the left ventricle is a violation of natural processes when the blood fills the region of the gastrochie itself, and at this time is in a relaxed state.
Such pathology must be treated as soon as possible and not ignore, as it is considered to be a phenomenon that precedes the development of heart failure with the left ventricular type.
In the future, the patient shows the edema of the lungs and asthma of heart nature.
Causes and symptoms
The dysfunction of the ventricle is a pathology in which normal processes are disturbed when the blood fully fills the part of the heart during its relaxation, which is called diastole. According to statistics, such a problem most often appears in women. The same applies to the elderly.
In normal condition, blood fills the organ stages:
- at first myocardium relaxes;
- then there is a difference in pressure, so there is a passive current of the blood fluid in the ventricle from the atrium;
- the first atrium is reduced, so there will be a fullness.
Different causes lead to the fact that one of the three of these phases is violated. In the future, this will lead to the fact that there is an insufficient blood volume in the ventricle, and this cannot provide a normal emission. As a result, a person gradually develops not enough left-deceased type.
The factors due to which the diastolic dysfunction of the left ventricle is manifested, lead to the fact that relaxation is gradually worsening, the walls of the ventricle become less elastic. As a rule, this is due to the fact that myocardium is compacted. This affects such diseases:
- cardiomyopathy hypertrophic type;
- aortic stenosis (the mouth of the aorta is gradually narrowed);
- hypertensive disease.
In addition, hemodynamic processes may be violated for other reasons:
- Pericarditis connectivity type. Pericardes thickens, and because of this, cardiac cameras are gradually pushed.
- Primary amyloidosis. The amyloid is lowered, which causes atrophy of muscle fibers. Because of this wall, myocardials become not as elastic.
- The pathology of blood coronary vessels, which lead to cardiac ischemia and the development of the stiffness of myocardium due to the fact that scars are formed.
Risk factors are diseases endocrine system, such as diabetes mellitus and obesity.

Signs of the disease may not appear first time, but then they will gradually begin to interfere with the patient normally live. Highlight symptoms:
- Dyspnea. It appears at first only with intense physical exertion, but then it will begin to appear spontaneously, even when the patient is at rest.
- Cough. His intensity is enhanced when a person lies, so it is better to sit down or get up when the next cough attack begins.
- Fatigue. It is difficult for the patient to carry any loads, and even the smallest. He gets up quickly.
- The heartbeat is accelerated.
- Night dance of paroxysmal type.
- Disturbance of the rhythm of the heart. Such a symptom is often manifested. The patient complains of arrogant arrhythmia.
Types and treatment
Patients may have a different type of such a disease. Violations in the left ventricle are developing gradually. Depending on their extent, these forms of illness are distinguished:
- Dysfunction of left ventricle 1 type. In this case, problems with the relaxation of this part of the body are observed. This stage of development of pathology is considered initial. The ventricle is not relaxing enough. The main amount of blood enters the ventricle when the atrium is reduced.
- Second type. It is also called pseudonormal. At this phase in the cavity of the atrium increases the pressure indicator, and completely reflexively. And the ventricle is filled due to the presence of a pressure difference.
- Third type. Still known as restrictive. This stage is considered to be terminal. It is associated with the fact that in the cavity of the atrium pressure increases. The elasticity of the stamps of the ventricle gradually decreases, which is due to strong stiffness.


Before starting treatment, you need to diagnose. It includes procedures such as:
- echocardiography and dopplerography of both cameras;
- ventriaculture radionuclide;
- electrocardiography;
- x-ray examination.
These techniques in the early stages of the development of the disease help prevent the emergence of irreversible changes.
Therapy should be comprehensive.
To adjust the hemodynamic processes, a number of measures are required. First, you need to always control the blood pressure. Secondly, it is necessary to reduce the frequency of heart abbreviations. Thirdly, you always need to maintain aquatic and salt exchange. This will reduce preload. In addition, remodeling of left ventricular hypertrophy is required.
Medical therapy
Medical therapy includes the reception of such drugs:
- Adrenoblocators. Funds help slow down the rhythm of the heart, reduce blood pressure, improve myocardial power at the cellular level.
- Antagonists angiotensin receptors and inhibitors of angiotensin glossy enzyme. These are two different types of drugs, but they have a similar effect. Such means have a beneficial effect on the remodeling of myocardium, increase the elasticity of its tissues, reduce the blood pressure.
- Diuretics. Such means are intended to output the extra reserves of the fluid in the body, which will reduce the shortness of breath.
- Calcium antagonists. When the amount of this compound in myocardiocytes decreases, myocardium can relax normally.
- Nitrates. Are auxiliary means that apply if signs of ischemia appeared.
All these events and drugs will help eliminate the problem with the heart. But such pathology is serious and entails heavy consequences, so it is impossible to ignore the symptoms, but also it is also prohibited from themselves.
tonometra.net
Causes of left ventricular hypertrophy
Persistent arterial hypertension
The most likely cause of the thickening of the muscles of the left ventricle of the heart is arterial hypertension that does not stabilize for many years. When the heart has to swing the blood against a high-pressure gradient, pressure overload occurs, myocardium trains and thickens. Approximately 90% of the left ventricle hypertrophy occurs for this reason.
Cardiomegaly
This is a congenital hereditary or individual feature of the heart. Large heart u big man It may initially have wider cameras and thick walls.
Athletes
The heart of athletes is hypertrophy because of physical exertion at the limit possible. Training muscles are constantly thrown into the total bloodstream additional blood volumes, which heart have to pump as it were additionally. This is hypertrophy due to the overload volume.
Vices of cardiac valves
The vices of the heart valves (purchased or congenital), violate blood flow in a large circulation circle (dummy, valve or linked stenosis of the mouth of the aorta, aortic stenosis with insufficiency, mitral insufficiency, interventricular septum defect) create conditions for volumetric overload.

Coronary artery disease
With ischemic heart disease, hypertrophy of the walls of the left ventricle with diastolic dysfunction (violation of myocardial relaxation) occurs.
Cardiomyopathy
This is a group of diseases in which against the background of sclerotic or dystrophic post-impaired changes, an increase or thickening of the heart departments is noted.
About cardiomyopathy
The basis of pathological processes in myocardial cells are hereditary predisposition (idiopathic cardiopathy) or dystrophy and sclerosis. Myocardits, allergies and toxic damage to the heart cells, endocrine pathologies (excess of catecholamines and somatotropic hormone), immune failures are carried out to the latter.
Varieties of cardiomyopathies leaking from GLB:
Hypertrophic form
It can give diffuse or bounded symmetric or asymmetric thickening of the muscular layer of the left ventricle. In this case, the volume of heart chambers decreases. The disease most often amazes men and is inherited.
Clinical manifestations depend on the severity of the obstruction of the heart chambers. The obstructive version gives the clinic of aortic stenosis: pain in the heart, dizziness, fainting, weakness, pallor, shortness of breath. Arrhythmias can be detected. As disease progressing, signs of heart failure are developing.
The boundaries of the heart are expanding (mainly at the expense of the left departments). There is a shift down the downpour and the deafness of cardiac tones. It is characterized by functional systolic noise listened after the first cardiac tone.
Dialing form
It is manifested by the expansion of the heart chambers and myocardial hypertrophy of all its departments. At the same time, myocardial contractual capabilities fall. Only 10% of all cases of this cardiomyopathy fall on hereditary forms. In other cases, inflammatory and toxic factors are obes. Dilatation cardiopathy is often manifested in young age (in 30-35 years).
The most typical manifestation becomes the left-handhold insufficiency clinic: lips sinusiness, shortness of breath, heart asthma or lung swelling. The right ventricle also suffers, which is expressed in the sinushes of the hands, the increase in the liver, the accumulation of fluid in the abdominal cavity, peripheral eductions, swelling the cervical veins. Heavy rhythm disorders are observed: tachycardia paroxysms, flickering arrhythmia. Patients may die against the background of ventricular fibrillations or asistolia.
Hypertrophy of myocardium left ventricle at the same time diffuse. The expansion of heart cavities prevails over the thickening of myocardium. Read more about symptoms and treatment of cardiomyopathy.
Types of GLG
- Concentric hypertrophy gives a decrease in the cavities of the heart and the thickening of myocardium. This type of hypertrophy is characteristic of arterial hypertension.
- The eccentric version is characterized by the expansion of cavities with simultaneous thickening of the walls. This occurs when the pressure is overloaded, for example, with heart defects.
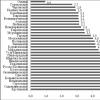
Differences of different types of GLL
Cardiomyopathy |
Hypernizia arterial |
Sports heart |
|
| Age | younger than 35. | older 35. | from 30. |
| Floor | both | both | more than a man |
| Heredity | burdened by hypertension | burdened by cardiomyopathy | not burdened |
| Complaints | dizziness, shortness of breath, fainting, heart pain, rhythm disorders | headache, less often shortness of breath | chilling pain in the heart, bradycardia |
| Type of GLG | asymmetric | uniform | symmetric |
| Myocardial thickness | More than 1.5 cm | less than 1.5 cm | decreases when loading loads |
| LJ Expansion | rarely, more often a decrease | possibly | more than 5.5 cm |
Complications of GLZH.
Moderate left ventricular hypertrophy is usually non-hazardous. This is a compensatory reaction of the body, designed to improve the blood supply to organs and tissues. For a long time, a person may not notice hypertrophy, as it does not appear in any way. As it progresses can develop:
- myocardial ischemia, acute myocardial infarction,
- chronic brain circulation disorders, strokes,
- heavy arrhythmias and sudden heart stop.
Thus, the left ventricular hypertrophy is a heart overload marker and testifies to the potential risks of cardiovascular disasters. Its most unfavorable combinations with ischemic disease Hearts, in elderly and smokers with concomitant diabetes and metabolic syndrome (overweight and lipid exchange disorders).
Diagnosis of GLG
Inspection
It is possible to suspect the left ventricle hypertrophy already with a primary examination of the patient. In case of inspection, the sinusiness of the nasolabial triangle or hands, the increase in breathing, swelling. When performing, there are expansion of the boundaries of the heart. When listening - noises, deafness of the tones, the accent of the second tone. Complaints may be detected for:
- saddy
- heart interruptions
- dizziness
- fainting
- weakness.
ECG
Hypertrophy of the left ventricle on the ECG is noted a characteristic change in the voltage of the teeth R in breast leads to the left.
- In V6, the tooth is greater than in V is asymmetric.
- The ST interval in V6 rises above the isolated, in V4 lowers below.
- In V1, the Tuster T becomes positive, and the tooth S is above the norm in v1,2.
- In V6, the qog is more normal and the prong of S. appears here.
- T negative in v5.6.
At the ECG, errors are possible in the assessment of hypertrophy. For example, an incorrectly supplied chest electrode will give an incorrect idea of \u200b\u200bthe state of myocardium.
Ultrasound of the heart
With echo-ks (heart ultrasound) hypertrophy already confirmed or refuted on the basis of visualization of heart chambers, partitions and walls. All the volume of cavities and the thickness of myocardium are expressed in numbers that can be compared with the norm. An echo-COP can be diagnosed with left ventricle hypertrophy, clarify its type and assume the cause. The following criteria are used:
- The thickness of the myocardial walls is equal or more than 1 cm for women and 1.1 cm for men.
- The asymmetry coefficient of myocardium (more 1.3) indicates an asymmetrical type of hypertrophy.
- The index of the relative thickness of the walls (norm less than 0.42).
- The ratio of the mass of myocardium to body weight (myocardial index). Normally, it is equal to or exceeds 125 grams per square centimeter, for women - 95 grams.
The increase in the last two indicators indicate concentric hypertrophy. If only the myocardial index exceeds the norm - there is an eccentric GLF.
Other methods
- Doppler Eochocardioscopy - Additional Opportunities Provides Doppler Echocardioscopy, in which you can estimate the coronary blood flow in more detail.
- MRI - also for the visualization of the heart use magnetic resonant tomography, which fully reveals the anatomical features of the heart and allows you to scan it in layers, as if performing cuts in a longitudinally or transverse direction. Thus, sections of damage, dystrophy or myocardial sclerosis are becoming better.
Treatment of left ventricular hypertrophy
Hypertrophy of the left ventricle, the treatment of which is always necessary with the normalization of lifestyle, often reversible. It is important to abandon smoking and other intoxication, reduce weight, conduct correction hormonal imbalance and dyslipidemia, optimize physical exertion. There are two directions in the treatment of left ventricular hypertrophy:
- Preventing the progression of GLZH.
- Attempting myocardial remodeling with return to normal sizes of cavities and thickness of the heart muscle.
- Beta-blockers make it possible to reduce the load and pressure load, reduce the need of myocardium in oxygen, solve some of the problems with rhythm impairment and reduce risks on cardiac catastrophes - Atenolol, metoprolol, betel-zok, supolyol.
- Calcium channel blockers become selection preparations with expressed atherosclerosis. Verapamil, Diltiaze.
- ACE inhibitors - means lowering blood pressure and substantially inhibit the progression of myocardial hypertrophy. Enalapril, lysinopril, dotroid is effective in hyperonia and heart failure.
- Sartans (Kandesartan, Lozartan, Valsartan) very actively reduce the load on the heart and remode the myocardium, reducing the mass of the hypertrophied muscle.
- Antiarrhythmic drugs are prescribed in the presence of complications in the form of heart rhythm disorders. Disaping, County.
zdravotvet.ru.
Diastolic dysfunction: a new diagnosis or a difficult-to-diagnostic disease
Recently, cardiologists and therapists are increasingly exposed to their patients "new" diagnosis - diastolic dysfunction. With a severe form of the disease, diastolic heart failure may occur (CH).
Currently, diastolic dysfunction is found quite often, especially in older women, most of whom will be surprised to find out that they have heart problems.
Neither diastolic dysfunction, nor diastolic heart failure is not really "new" diseases - they always hit the human cardiovascular system. But in recent decades, these two diseases began to be detected. This is due to the extensive use in the diagnosis of heart problems of ultrasound methods (echocardiography).
It is believed that almost half of the patients entering emergency departments with acute heart failure, actually have diastolic CH. But it may be difficult to establish the correct diagnosis, since after stabilizing the state of such a patient, the heart may look completely normal when conducting echocardiography, if a specialist is purposefully looking for signs of diastolic dysfunction. Therefore, inattentive and inconviable doctors often miss this disease.
Characteristics of the disease
The heart cycle is divided into two phases - systole and diastole. During the first ventricle (the main chambers of the heart) are reduced by throwing blood from the heart in artery, and then relax. When relaxation, they are replenished with blood to prepare for the next reduction. This phase of relaxation is called diastole.
However, sometimes due to various diseases of the ventricles become relatively "hard". In this case, they cannot fully relax during the diastole. As a result, the ventricles are not completely filled with blood, and it is stored in other parts of the body (in lungs).
Pathological tightening of the walls of the ventricles and their insufficient filling of them with blood during the diastole is called diastolic dysfunction. When diastolic dysfunction is expressed as it causes stagnation in the lungs (that is, the accumulation of blood in them), it is believed that this is already diastolic heart failure.
Signs of heart failure - video
The reasons
The most frequent cause of diastolic dysfunction is the natural effect of aging on the heart. With increasing age, the heart muscle becomes hard, disrupting the filling of the left ventricle with blood. In addition, there are many diseases that can lead to this pathology.
Diseases provoking diastolic dysfunction - Table
Classification
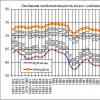
On the basis of these echocardiography, the following degrees of diastolic dysfunction are distinguished:
- I degree (disturbed relaxation) - may be observed in many people, not accompanied by any symptoms of heart failure;
- II degree (pseudonormal filling of the heart) is a diastolic dysfunction of moderate gravity, in which patients often have symptoms of CH, an increase in the left atrium is observed;
- III (reversible restrictive filling of the heart) and IV (irreversible restrictive filling of the heart) - these are heavy forms of diastolic dysfunction, which are accompanied by pronounced symptoms of CH.
Based on the symptoms, you can install the functional class (type) of CH according to the classification of the New York Heart Association (NYHA)
- FC I - no symptoms of CH;
- FC II - symptoms of CH with moderate physical exertion (for example, when lifting per 2nd floor);
- FC III - symptoms of CH with minimal exercise (for example, when lifting per 1st floor);
- FC IV is the symptoms of CH alone.
Symptoms
Symptoms that are concerned about people with diastolic dysfunction, as in patients with any form of heart failure.
With diastolic CN, signs of stagnation in lungs are on the fore.
- dyspnea;
- cough;
- student breathing.
Patients with such a diagnosis often suffer from these symptoms in the form of sudden attacks that appear without any warnings. This diastolic CN differs from other forms of heart failure, in which shortness of breath is usually developing gradually within a few hours or days.
Sudden and hard difficulties of breathing, often occurring during diastolic CN, are called episodes of "Flares of the elder".
Although the distinctive feature of the diastolic CH is precisely the outbreaks of elderly, patients with this disease may also experience less heavy episodes of breathing with more gradual development.
Diagnostics
It is possible to detect the presence of diastolic dysfunction using ultrasonic heart research - echocardiography. This survey method allows you to estimate the characteristics of myocardial relaxation during diastole and the degree of rigidity of the walls of the left ventricle. Echocardiography can also sometimes help detect the cause of diastolic dysfunction. For example, it can be identified with it:
- thickening of the walls of the left ventricle in hypertension and hypertrophic cardiomyopathy;
- aortic stenosis;
- some types of restrictive cardiomyopathy.
Nevertheless, many patients with signs of diastolic dysfunction on echocardiography do not have other pathologies that could explain its availability. Such people cannot determine the specific cause of the disease.
It should be noted that for each of the degrees of diastolic dysfunction, there are specific criteria for conducting echocardiography, therefore, it is possible to determine them only with this study.
Treatment
The best strategy of diastolic dysfunction therapy and diastolic CH is an attempt to detect and treat the cause. Thus, the following problems must be overcome:
- Arterial hypertension. People with diastolic dysfunction often have an increased blood pressure, which is difficult to identify. Moreover, very often such hypertension is treated inadequately. However, patients with diastolic dysfunction are very important to control their blood pressure within the boundaries of the norm.
- Coronary artery disease. People with diastolic dysfunction should be examined for the availability of coronary heart disease. This disease is a frequent cause of diastolic dysfunction.
- Atrial fibrillation. The rapid heartbeat caused by this violation of the rhythm may be the cause of a significant deterioration in the functioning of the heart in people with diastolic dysfunction. Therefore, the control of the rhythm is very important aspect In the treatment of a patient with atrial fibrillation and diastolic dysfunction.
- Sugar diabetes and overweight. Reducing body weight and glucose control help to stop the deterioration of the condition in diastolic dysfunction.
- Passive lifestyle. Many people with diastolic dysfunction are mainly a sedentary lifestyle. The aerobic exercise program can improve the diastolic function of the heart.
In addition to measures aimed at identifying the causes and treatment of diastolic dysfunction, your doctor may prescribe medications that affect its symptoms. For this purpose, diuretics (furosemid) are most often used, which are excess of water and sodium from the body, reducing the severity of stagnation of stagnation in lungs.
Prevention
It is possible to prevent the development of diastolic dysfunction using measures aimed at preventing cardiovascular diseases:
- rational and balanced nutrition with a low content of fats and salts;
- regular exercise;
- control of diabetes and blood pressure;
- maintaining normal weight;
- minimization of stress.
serdcemed.ru.
Structure and structure of the left ventricle
Being one of the chambers of the heart, the left ventricle in relation to other parts of the heart is the post, left and book. Its outer edge is rounded and wears the name of the pulmonary surface. The volume of the left ventricle in the process of life increases from 5,5-10 cm 3 (in infants) up to 130-210 cm 3 (for 18-25 years).
Compared to the right ventricle, the left has a more pronounced oblong-oval form and somewhat longer and muscular.
In the structure of the left ventricle, two departments distinguish:
- The rear department, which is the cavity of the ventricle and with the help of the left venous opening, communicates with the cavity of the corresponding atrium;
- Front department - arterial cone (in the form of an output channel) is reported to the arterial hole with aorta.
Due to myocardium, the wall of the left ventricle in thickness reaches 11-14 mm.
The inner surface of the left ventricular wall is covered with fleshy trabecules (in the form of small protrusions), which form a network, intertwining among themselves. Trabecules are less pronounced than in the right ventricle.
Functions of the left ventricle
Aorta left ventricle hearts begins big circle Circulation, which includes all branches, capillary network, as well as veins of tissues and organs of the whole organism and serves to deliver nutrients and oxygen.
Dysfunction and Treatment of the left ventricle
The systolic dysfunction of the left ventricle is called a decrease in its ability to throw blood into the aorta from its cavity. This is the most common cause of heart failure. Systolic dysfunction, as a rule, causes a drop in the reduction, leading to a decrease in its shock volume.
The diastolic dysfunction of the left ventricle is called the drop in its ability to pump blood from the system into its cavity pulmonary artery (otherwise - provide diastolic filling). Diastolic dysfunction can lead to the development of pulmonary secondary venous and arterial hypertension, which manifest themselves as:
- Cough;
- Dyspnea;
- Paroxysmal night dance.
Pathological changes and leav of the left ventricle
To one of the typical lesions of the heart with a hypertension of the left ventricle (otherwise cardiomyopathy) belongs to a hypertension. The development of hypertrophy provoke changes in the left ventricle, which leads to the modification of the partition between the left and right ventricles and the loss of its elasticity.
At the same time, such changes in the left ventricle are not a disease, but are one of the possible symptoms of the development of any type of heart disease.
The cause of the development of left ventricular hypertrophy can be both hypertensive disease and other factors, such as heart defects or significant and frequent loads. The development of changes in the left ventricle is sometimes noted over the years.
Hypertrophy may provoke significant modifications arising in the field of left ventricular walls. Along with the thickening of the wall there is a thickening of a partition located between the ventricles.
Stenzardia is one of the most common signs of left ventricular hypertrophy. As a result of the development of muscle pathology, flickering arrhythmia arises, and also observed:
- Pain in the chest area;
- Increased blood pressure;
- Headaches;
- Pressure instability;
- Sleep disorders;
- Arrhythmia;
- Heart pain;
- Poor well-being and general weakness.
In addition, similar changes in the left ventricle may be symptoms of diseases such as:
- Pulmonary edema;
- Congenital heart disease;
- Myocardial infarction;
- Atherosclerosis;
- Heart failure;
- Acute glomerulonephritis.
Treatment of the left ventricle is most often a medicated nature along with the observance of the diet and the refusal of the existing hazards. In some cases, the operational intervention may be required due to the removal of the heart muscle site, which has undergone hypertrophies.
To small anomalies of the heart, manifested by the presence in the cavity of the ventricles of heavy (additional connective tissue muscular formations) relates false chord of the left ventricle.
Unlike normal chord, false chords of the left ventricle have an atypical mounting to the interventricular septum and the free walls of the ventricles.
Most often, the presence of false chord of the left ventricle does not affect the quality of life, but in the case of their multiplicity, as well as at a disadvantageous location, they can call:
- Serious rhythm disorders;
- Reducing the tolerance of physical exertion;
- Relaxation violations of the left ventricle.
In most cases, the treatment of the left ventricle is not required, but should be regularly observed in the cardiologist and carry out the prevention of infectious endocarditis.
Another frequent pathology is the left ventricular insufficiency of the heart, which is observed with diffuse glomerulonephritis and the aortic vices, as well as against the background of the following diseases:
- Hypertonic disease;
- Atherosclerotic cardiosclerosis;
- Syphilitic aortitis with the lesion of the coronary vessels;
- Myocardial infarction.
Lack of left ventricle can manifest as in acute formand in the form of gradually increasing blood circulation.
The main treatment at the left head of the heart is:
- Strict bed mode;
- Long-term inhalation with oxygen;
- Application of cardiovascular funds - Cordiamine, camphor, stanfantine, cozol, Corgal Golon.
October 24, 2017 no comments
Systolic dysfunction of the left ventricle
The pathogenetic basis of the systolic dysfunction of the left ventricle is to reduce its contractile ability. The reduction of myocardium is the ability of the heart muscle to develop a certain force and the rate of abbreviations, without changing the length of the cardiomofibril. This ability depends mainly on their exhaust properties.
The reduction rate is the maximum rate of increasing the intraventricular pressure into the phase of isometric (isoisolum) reduction - (DP / DT Max), since this indicator is little dependent on changing the inflow of blood, i.e. from the load "at the entrance" and on the pressure in the aorta , i.e. from the load "at the output". This indicator, where: DP is customary to be called an index of isozolumoi myocardial.
To date, the definition of this indicator remains a very relevant problem. Although many ways to determine this index are proposed, the search for new methods of clinical assessment of myocardial reductions mainly to the left ventricle continues. Usually the DP / DT index is determined using cavity catheterization, incl. Heart ventricles in the absence of the possibility of catheterization of the heart calculate the average rate of increase in pressure in the ventricle in the phase of isometric reduction using other methods. For example, taking into account the fact that the finally isometric intragery pressure is almost equal to the diastolic in the aorta, it is possible to do without catheterization, calculating the index by the formula:
dP / DT Wed \u003d DD Aort. / FIS L.ZH,
[Where DD Aort. - diastolic pressure in the aorta; Fisl - the duration of the phase of isometric reduction of the left ventricle.
Considering the proximity of the diastolic pressure values \u200b\u200bin the aorta and the shoulder artery, you can use the value of DD, which is determined in this artery according to the Korotkov method. Finally, it is often in clinical practice that the magnitude of the diastolic pressure is used, and the approximate value of the "developed" pressure into an isometric phase, for which the conditional magnitude of the left-income finite-altar pressure is subtracted from the diastolic pressure, which is taken for 5 mm Hg. Then the formula acquires the following type: DP / DT Wed. \u003d DD - 5 / FIS.
This formula is most convenient for practical use, and the value obtained is close to the true value of the indicator. For the right ventricle, the average rate of increase in pressure in the phase of isometric reduction can be calculated by the formula: DP / DT Wed \u003d DD L.A. / FIS AF., where DD L.A. - diastolic pressure in the pulmonary artery; FIS Pr. Sel. - The duration of the phase of isometric reduction of the right ventricle.
The mechanisms for reducing myocardials can be adequately perceived and evaluated using a graphic image of the "pressure-volume" relationship. Reducing the contractile function of the heart displays the crooked of isolaum systolic pressure to the right and down. This means that each given volume of ventricular filling leads to a smaller increase in intra-palpal pressure compared to the initial (up to a reduction in the reduction) by its lifting with the same heated ventricle.
The fundamental consequence of such a shift is that for this preload and post-loading, the impact volume (UN) is significantly reduced.
At the same time, the heart can use a number of urgent compensatory mechanisms to maintain the WE: an increase in preload, an increase in myocardial intellity and an increase in heart rate. An increase in the preload is one of the ways with which the ventricle may be unnecessary (quickly) to restore the UO. If the curve of isoovolum systolic pressure suddenly moves down and right, i.e. The reduction of the ventricle will decrease, the impact volume (UO) at this postning load will also suddenly decrease. At the same time, a greater amount of blood remains in the ventricle at the end of the systole. If the amount of blood coming into the ventricle remains constant (the filling of the ventricle ends at the point B), i.e., the diastolic volume remains at the same level: ((b-a) approximately equal to (in-a)), then the NE will immediately restore and will be maintained at such a level: the difference C - D is approximately equal to the difference C - D.
With subsequent cuts, the ventricle will operate in the region of a higher finite diastolic pressure. Recall that at the point in (at the end of the diastole) there is a closure of a mitral valve. The increase in the final diastolic pressure in the ventricle may cause an increase in pressure in the left atrium and then in the pulmonary veins to the level leading to the development of interstitial and alveolar edema (pulmonary edema).
Another compensatory heart reaction in acute systolic dysfunction is an increase in the intoment (contractile ability) of myocardium. It is well known that one of the immediate responses of the body on heart failure is the activation of sympathetic nervous system. Stimulation of p-adrenergic gastric receptors leads to an increase in the intracellular concentration of CA ++, which determines the increase in the reduction force (reduction) of cardiomyocytes. This is manifested by a small shift up and left curve isoisolum systolic pressure and helps support the UO.
For systolic dysfunction of the left ventricle, a decrease in cardiac emission is characterized, but since this indicator is derived by the UO and CSS, the increase in heart rate may be a compensatory mechanism for maintaining SV in conditions of reduction of myocardial contractility. The growth of pressure in the right of atrium and the mouths of hollow veins causes reflex tachycardia (Bainbridge Reflex - Reflex from the mouth of the hollow veins on the sinus node). Stimulation of beta-adrenoreceptors in the sinus unit determines the increase in heart rate, which leads to an increase in St.
Causes of systolic dysfunction
The most frequent causes of the development of systolic dysfunction are:
1. Coronary failure.
2. Myocardits:
a) infectious myocardits caused by viruses (cokes in virus, adenovirus), bacteria (Lyme disease - is caused by spirochet Borrelia Burgdorferi, Trypanosoma and Toxoplasma) and the simplest (chagas' desease);
b) noncommunicable myocardits occur when alcoholic intoxication, lead poisoning, metabolic disorders (diabetes), etc.
3. Forms of the pathology of the cardiovascular system, leading to a change in premature loads (valve velocities, long-term arterial hypertension).
4. Nervous muscular disorders (muscle and motonic dystrophy).
5. Collagen vascular diseases.
Systolic dysfunction of right ventricle
The most common cause of the right-loading systolic dysfunction is a post-load caused by increased pressure in the pulmonary artery (the prepillary form of pulmonary hypertension).
The most common variant of the development of such hypertension is due to a decrease in the pump function of the left heart, leading to an increase in pressure in the pulmonary artery system. Increased postload on the right heart can also develop in almost any serious lung disease, including chronic obstructive pulmonary disease, idiopathic pulmonary fibrosis, chronic pulmonary embolism, etc.
All these diseases can lead to pulmonary hypertension and subsequently to the right-hand systolic dysfunction. The form of pathology characterized by hypertrophy and (or) dilatation of the right ventricle under conditions of pulmonary hypertension due to primary lung diseases, WHO expert Committee called " lonantic Heart (Cor Pulmonale). "
With a decrease in the pump function of the right ventricle, an increase in systemic venous pressure occurs, which is accompanied by the transudation of the fluid into the intercellular space, followed by the development of edema in the internal organs (primarily in the liver), the abdominal cavity and lower limbs. First of all, the function of the liver suffers, although there is a deterioration in the function of the stomach and intestines, it is possible to accumulate fluid in the abdominal cavity (ascites).
Initially, a moderate impaired liver function arises, usually with a small hyperbilirubinemia, an increase in the prothrombin time and activity of hepatic enzymes (for example, alkaline phosphatase, ACT, ALT). The damaged liver is unable to inactivate the aldosterone, and the emerging secondary aldosteroneism causes its contribution to the development of edema. Chronic venous stagnation in internal organs can cause anorexia, diarrhea, malabsorption syndrome, constant blood loss through the gastrointestinal and (sometimes) ischemic intestinal infarction.
Read:
In this section, we allocate two reasons that cause the most serious problems concerning the dysfunction of the right ventricle is the infarction of the right ventricle and the pulmonary heart.
For infarction of right ventricle Systemic venous hypertension, ECG changes (segment rise ST, wave Q. Above the zone of the right sections of the heart - V 4 P) and changes in the corresponding enzymes. According to JJ. Marini and A.R. Wheeler (1997), with the right ventricle infarction, usually requires massive intravenous injection of fluid. Work on the "pushing" of blood both in the artery of a large circle (straight) and into pulmonary artery (indirect method through the interaction of both ventricles) performs the left ventricle. At the same time, the dilatation and load of the liquid of the right ventricle complicate blood flow on both paths due to the constraint of the ventricles within the heart rate, stretching the involvement in the reduction of circulatory muscle fibers and the displacement of the interventricular partition. For several days, compensation mechanisms are formed. In the primary right-minded deficiency, therapeutic measures are not significantly different from those at left-deuded deficiency. The exception is the secondary right-hand deficiencies
an occasion that occurred, for example, with excessive fluid infusion. Main benchmarks are JLL and CVD. The use of non-invasive hemodynamic monitoring is also important because it allows in dynamics to evaluate such indicators as CB, OPS and DNLG. When increasing the pressure of the junction, DNLG and CVD, it is necessary to reduce the rate of infusion therapy or complete cessation of infusion to the normalization of the FLO. In these cases, Dobutamine is most indicated, the dose of which is determined by the effect that it causes (from 5 to 15 μg / kg / min) [Marino P. 1998].
With a reduced CVD and ZLL, in-fusium therapy may have a normalizing effect on hemodynamics. Dobutamine can be used with myocardial infarction and pulmonary artery embolism. From the use of vasodilators should be refracted, since they reduce the venous influx to the right heart, which can lead to a further fall of CB. If it is possible to maintain CB during the first critical days, then the prognosis for patients who lack other cardiovascular diseases is usually favorable. The outcome depends not only on the size of the heart attack, but also on the presence or absence of resistance of pulmonary vessels.
Lonantic Heart - · Pathological condition, developing in parenchymal, vascular diseases of the lungs, leading to a decrease in functioning pulmonary capillaries and pulmonary hypertension. As a result, hypertrophy, dilatation or deficiency of right ventricle are developing. The concept of "pulmonary heart" does not include secondary changes in the right ventricle, developed under the conditions of hypertension of the pulmonary veins or the lack of left ventricle.
The main reasons for pulmonary hypertension include a reduction in the number of pulmonary capillaries, the emergence of alveolar hypoxia and acidosis. In all these cases, a significant increase in pressure in the pulmonary artery system is possible. Normally, the right ventricle with its myocardium cannot provide adequate emissions if the pressure in the pulmonary artery is more than 35 mm Hg. Compensatory mechanisms are gradually included: hypertrophy of the walls of the right ventricle develops, which creates pressure comparable to those in the system circulation. Smooth muscle fibers of pulmonary arteries are also hypertrophy, strengthening the answer to alveolar hypoxemia.
Acute pulmonary heart Developed over a short period of time, and compensatory reactions may be absent. The most common cause of a sharp pulmonary heart is a massive tel. An extensive lung infarction can also be the cause of a sharp pulmonary heart.
Chronic pulmonary heart develops at chronic diseases Lightways of any etiology (COZL, etc.), causing obliteration of pulmonary capillaries. Basic signs - shortness of breath and chronic arterial hypoxemia. This disease can always go to the phase of acute decompensation.
Diagnostics. The main benchmarks in the diagnosis of referee are indicators of FLA, pressure in the right of atrium (p of PP), in the pulmonary artery (PA) and the calculation of pulmonary vascular resistance. They help to distinguish terrible failure from the left elder.
Fisical data of the pulmonary heart - hypoperfusion, gallop rhythm, loud second tone, pulsating hepatomegaly and venous stagnation in a large circulation circle. Unfortunately, many scientific research is not always possible. The physical research data can be confirmed by identifying-- and resistance of pulmonary vessels (SLS) and determining CB, DZL, OPS, as well as an indicator of oxygen saturation in mixed venous blood. It is very important to use non-invasive techniques, as it allows us to estimate such indicators as CB, OPS and DNLG.
Treatment of acute pulmonary heart. Key points of therapy - the creation of adequate filling of the right ventricle, the correction of hypoxemia and acidosis, the establishment of a normal heart Rhythm and treatment of the main disease.
Adequate venous influx - One of the important conditions for the functioning of the right ventricle. A sharply reduced venous influx and an uncontrolled increase of it can be causes of cardiac decompensation. In this regard, the monitoring of R PP is becoming a special meaning. DNLG, CB and R LA -I, when to create an adequate CB, the maximum expansion of the right ventricle and the use of the phenomenon of the interaction of two ventricles, the purpose of powerful diuretics can lead to undesirable results. The measurement of the FED should be carried out with special care, since the purpose of any inotropic agents and changes in infusion therapy can give an unpredictable effect.
Oxigenotherapy. The adequate level of PAO 2 and SAO 2 is of great importance. This immediately reduces the resistance of pulmonary vessels. Despite the fact that many patients with Hose level Paco 2 is increased, it is important to remember that under conditions of hypoxemia, acidosis enhances the effect of the latter on the resistance of pulmonary vessels, while hypercarbium itself in the absence of hypoxemia has a less pronounced effect on the resistance of the pulmonary vessels. It is important to normalize the pH of the blood, allowing the possibility of moderate hyperkapin.
Inotropic and diuretic therapy. The effect of Digitalis preparations, inetropic drugs and diuretics in the treatment of acute pulmonary heart is different. These drugs should be prescribed with caution. Soft diuretics help remove stagnant phenomena in lower limbs, intestines and portal system. Diuretics can help reduce the stretching of the right ventricular chamber and, consequently, tension of myocardial fibers, reducing the preload and improvement of perfusion. But it is necessary to remember that a significant decrease in the ZLL, as well as the PA in patients with stagnant heart failure, can lead to a decrease in CB.
DiGitalis preparations can give an effect in the treatment of chronic pulmonary heart, contribute to the normalization of the heart rhythm during atrial fibrillation, since in this case they do not have a cardiodepressive action.
Dopamine and Dobutamine can improve the function of the left ventricle due to the support of perfusion pressure in the myocardium of the right ventricle, as well as to promote the interaction of two ventricles during ventricular dilatation. In addition, since the ventricles have a single interventricular partition and circulatory muscle fibers, improving the reduction of left ventricle has a positive effect on the right ventricle (again due to the interaction of ventricles). However, arrhythmia caused by the action of these drugs may disrupt the atrioventricular coordination, on which the filling and efficiency of the right ventricle depends.
So, in the treatment of heart failure, it is necessary to take into account the physiological features of the functions of the right and left ventricles. Due to the different power of the muscles of the left and right ventricles and the different resistance of systemic and pulmonary vessels, there are significant differences in the functions of both ventricles to pre-and post-load. The right ventricle under normal conditions is more sensitive to changes and post-load changes than the left. In heart failure, both ventricles, according to JJ. Marini and A.R. Wheeler, become insensitive to preload, but sensitive to post-load.
The increase in post-loading of the right ventricle depends on hypoxemia and acidosis (observed in patients with COP), the state of capillary vascular bed, reduce the functioning pulmonary vessels, hypertrophy of smooth muscle vessels and pulmonary hypertension. Most often, the causes of the acute pulmonary heart are TEL, infarction pneumonia, changes in hemodynamics under RDSV. The resistance of the left ventricle emission is determined mainly by the vascular tone of the arteriole and can be associated with a narrowing or dysfunction of the aortic valve.
A number of factors can lead to loss of ventricular elasticity and to incomparable relaxing in the diastole phase. At the same time, even the normal systolic function of the left ventricle against the background of stagnant heart failure is not a guarantee from the development of acute pulmonary edema. Diastolic dysfunction is usually the first symptom of heart failure arising against the background of arterial hypertension, myocardial ischemia and other factors. In the orort diastolic dysfunction - a frequent form of heart failure.
The recognition of diastolic and systolic dysfunction is important due to significant differences in their treatment. Its first signs can be growing congestive phenomena in the lungs without changing the systolic function of the left ventricle. Usually in these patients, inotropic drugs do not contribute to the improvement of the diastolic function. In the treatment of heart failure caused by a sharp pulmonary heart, the mainstream is maintained by the adequate pressure of filling the right ventricle, the elimination of hypoxemia and acidosis, which helps to reduce the pulmonary vascular resistance and post-loading of the right ventricle.
Options for acute heart failure. Treatment of the dysfunction of the right ventricle.
Clinical options of acute heart failure. with a stagnant type of hemodynamics (PJ or LV insufficiency); its hypokinetic type; With small emissions syndrome - CSh (arrhythmic and true). In the acute phase, it is often observed by the dysfunction of the LV severity of which correlates with the vastness of the heart damage. A number of patients with a small one can only have a local violation of the movement of the walls of the ventricles, but the total function of the LV can be normal due to hyperkinesia of unaffected myocardial segments.
Small dysfunction of right ventricle It is often noted with the lower or lower-beetles of the LV wall. The essential violation of the PJ function appears only in 10% of patients with these localizes. Extensive necrosis of the PJ occurs rarely, as it has a smaller need for oxygen and the pressure of the wall, perfumed during the entire period of the heart (diastole and systole), often due to peripheral coronary arteries. The degree of lesion of the PJ depends on the site of occlusion of the right coronary artery (severe PJ insufficiency arises only in the case of closing its proximal branch), the state of the peripheral blood circulation and the value of blood flow in small heart veins. The healing tactic with the Impage includes:
Maintaining preloads on the right ventricle (saline intravenous);
Conducting ex with symptomatic av-blockade;
Inotropic support (dopamine introduction);
Reduction of post-load on the hypertrophic left ventricle;
Introduction of arterial vasodilators (sodium nitroprusside), IAPF;
Conducting reperfusion.
Clinical symptomatics of acute heart failure. Dyspnea, the appearance of the 3rd cardiac tone, the presence of wet wheezes in the lungs (first in the lower departments).
Diagnosis of acute heart failure.
Acute heart failure is diagnosed (And the mechanisms of its development are clarified) according to radiography of the heart (signs of stagnation in the lungs) and EhCG (evaluation of the function of LV, detection of mitral regurgitation, DMWP, etc.).
Approximately degree of acute heart failure (OLZHN) with it is estimated on T. Kilip et al.
1st grade (Frequency - 33%; mortality - 6%) - no symptoms of the OSN (there are no manifestations of LV insufficiency, venous and pulmonary stagnation - there are no wheezes in the lungs and 3rd tones of the heart). Hemodynamic monitoring and treatment is not required;
2nd class (frequency - 38%; mortality - 17%) - moderate land (moderate LV insufficiency (double-sided wet no bells in the lower departments, but not more than 50% of the surface of the lungs, rhythm of gallop, tachycardia) and symptoms of lack of failure - venous stagnation and an increase in the size of the liver. Hemodynamics and treatment monitoring are required - reduction of preloads with diuretics;
3rd class (Frequency - 10%; Mortality - 38%) - Strong Osn (Ol - Warms in the lungs more than 50% of their surface). Hemodynamics and treatment monitoring are required - reducing the preload of diuretics or vasodilators;
4th grade (Frequency - 19%; mortality - more than 80%) - True CSH. Hemodynamics and treatment monitoring are required - a combination of analgesics, infusions and vazopressors.
Condition of right ventricle and interventricular interaction in patients with chronic heart failure
O.I. Zharinov, Salam Said, R.R. Komorowsky
Institute of Cardiology. N.D. Strazhestko AMN of Ukraine, Kiev, Kiev Medical Academy of Postgraduate Education. P.L. Shouting MZ of Ukraine,
Keywords: Heart failure, right ventricle, stomach interaction.
Right Ventricular Status and Ventricular Interaction in the Patients with Chronic Heart Failure
O.J. Zharinov, Salam Saaid, R.R. Komorovsky.
The Article Reviews The Contemporary Understanding of the Functional Status of Right Ventricle (RV) in the Patients with Chronic Heart Failure (CHF). Methodological DiffiCulties of the Investigation of RV, The Principal Parameters of the Systolic and Diastolic RV Function and The Peculiar FEATURES OF TRANSTRICUSPIDAL FLOW IN CHF ARE PRESENTED. The causes of the involvement of RV in different myocardial pathology, accompanied by left ventricular dysfunction, the principal ways of the formation of RV dysfunction in CHF caused by IHD, postinfarction cardiosclerosis, arterial hypertension and dilated cardiomyopathy, are discussed. IT SHOWN THAT THE STUDY OF THE MAIN FACTORS OF THE EVALUATION OF THE GRAVITY OF THE PATIENTS OF THE EVALUATION OF THE CHARACTERIS OF THE PATIENTS OF THE CHF, THE CHARACTERISTICS OF THE ROLE OF THE RV IN THE MECHANISMS OF CHF PROGRESS IS PRESENTED . AT The Same Time RV Status SHOLD BE EVALUATED THROUGH INTERDEPENDENCE AND INTERACTION OF LEFT AND RIGHT VENTRICLES - THE COMON INFLUENCE OF CONTRACTILITY, Pre- and Afterloading of Both Ventricles During Systole and Diastole. The Main Factor Mediating Ventricular Interaction Is Interventricular Septum.
The formation and comprehensive development of the problems of myocardial dysfunction have recently revised the ways of forming chronic heart failure (CHHN), to propose new criteria for the diagnosis of early disturbances of relaxation and filling of the ventricles of the heart, to develop ways of differentiated CHF treatment, depending on the nature of the dysfunction of the heart muscle. In most studies, diagnostic and therapeutic recommendations, the term "myocardial dysfunction" is identified with the concept of left ventricle dysfunction (LV) described when various diseases and heart lesions. Information on the state of the right ventricle (PZH) in the development of CXN is significantly less. Meanwhile, judged on the state of the PJ, based on the indicators of the LV function, it seems unlawful due to the differences in their configuration and operation mechanisms. With many heart diseases, both ventricular function is disturbed. Not only the rul-like type of CHF, formed without substantial involvement in the pathological process of LV, but also the PJ dysfunction, which appears in parallel or secondary to the LV dysfunction through an increase in pressure in a small circle of blood circulation and interventricular interaction is possible.
Methodical aspects of assessing the structure and functions of the PJ
The study of the contractile ability and geometry of the PJ has a number of restrictions on the well-known difficulties of its visualization. Although such modern research methods are like angiography, radionuclide ventriculography, nuclear magnetic resonance and heart catheterization with hemodynamic measurements make it possible to assess the structure and pumping function of the PJ, due to invasiveness or high cost, they cannot routinely be used in the cardiology clinic.
The publicly available method of non-invasive assessment of the function of the right-hand heart departments is echocardiography. This method also has a number of technical limitations. First, the informativeness of the study is largely determined by the quality of the device and the sensor. This problem can be largely solved by using more perfect and sensitive equipment. Secondly, the elderly patients often observed emphysema of the lungs adjacent to the heart, which limits the ultrasound window and access to research. With the narrowing of the intercostal interval, the study is possible only with a strictly sagital direction of the beam, since the slightest slope of the sensor is accompanied by the rib fabric location field. Thirdly, PJ, unlike LV, has a more complex cavity configuration. The PZ cavity consists of an input and output departments, as well as the main chamber, curved in the shape of a crescent. The spatial model of the PJ is a pyramid with a triangular base. It is difficult to describe with conventional mathematical approaches that cannot take into account the transverse expansion of the PJ and its endowing path.
Normally, during a parasolinary study along a long axis (or on a short axis at the level of chore papillary muscles), the size of the PJ does not exceed 2.6 cm. From this access, the LV dominance is clearly traced, and if the size of the PZ is equal to or exceeds the size of the LV, it can be concluded about Dilatation of PJ. When studying from the apical four-chamber position in the norm, the top is fully occupied by LV, and if the PJ at least partially occupies the top, it seems to be dilated.
Explore the thickness of the PZ walls is difficult. The main obstacle are Trabecules and a moderator beam (intermushkin trabecula) of PJ, which make a significant error in measurement; In the presence of hypertrophy, the PJ measurements are simplified. Normally, the thickness of the front wall of the PJ does not exceed 0.5 cm
Due to the complex configuration of the PJ, several different approaches to the definition of its volume are proposed. The most reliable is the analysis of orthogonal sections from the top access based on the use of the Simpson method, which makes it possible to determine the volume of incorrect geometric figures with the lowest error. It should be borne in mind that the volume of PJ calculated by this method, by an average of 10-12% less than the actual, since the resulting sections do not cover the Output tract of the PJ.
In echocardiographic examination, such indicators of the PJ function determine: the finite-diastolic (CSO) and the finite-systolic (CSR) volume and the emission fraction (FV). According to various studies, in the norm of FV PZ is 55%, but not less than 48.8 ± 1.48%. So, in healthy faces of FV LH slightly exceeds FV PJ. It is assumed that the difference between FV LV and FV PJ characterizes the equity participation of each of the ventricles in the functioning of the heart as a single pump. Considering that the volume of the PJ cavity, as well as LV, is largely determined by the anthropometric characteristics of the patient, it is advisable to analyze the indices of the CDO and the CSR - their attitude to the surface of the body surface. Determine the ratios of diastolic and systolic volumes of PJ and LV (KDOPZ / KDOLZH / KSOP / KSOL). Healthy faces of KDO PJ 1.5 times more than QDO Lie.
The parameters of the diastolic function of the PJ are defined similarly and are similar to the corresponding parameters of the diastolic function of LV. Normally, there is almost a linear relationship between the relations of E / A, defined at the level of mitral and tricked valves: the greater the peak velocities e and and the waves of the transmitral flow, the more and for the transit-propelled stream. However, since the area of \u200b\u200bthe trickspeople is greater than mitral, the maximum streaming speeds E and A in the right hearts of the heart are somewhat less than in the left. At the same time, the flow area does not differ, since the volume of blood passing per unit of time through the tricuspid and mitral valve is the same.
Several otherwise, compared to similar parameters of the diastolic filling of the LV, only the duration of the period of isolauming relaxation of PZ (IVRTPZ) is calculated between the closure of the pulmonary artery valve (LA) and the opening of the tricuspid valve. This indicator is calculated as the difference between the vertices of the synchronously registered R to the ECG, respectively, until the end of the systolic flow in the pulmonary artery and the opening of the tricudal valve.
An independent effect on the formation of the indicators of the transcentuate stream has age, heart rate and breathing. However, if changes in the filling process of the LV and PZH when aging and increasing the frequency of the rhythm of the heart occur the same type, with respiration there are specific changes in transmittral and transcentrous streams. The respiratory act causes only minor fluctuations (less than 10%) filling LV and moderate changes (up to 30%) of the filling of PJ. In the inhalation phase, the amplitude of the transstrate flow increases, and the transmitral - decreases, whereas during the exhalation there are reverse changes. This is due to oscillations of intragenic and intrapericardial pressure: in the inhalation phase, the pressure in the chest cavity is reduced, and in the abdominal - increases; Accordingly, the return of blood in the heart and filling of the PJ increases. The interventricular partition (MZHP) is shifted to the left, which in turn reduces the volume, fuel and filling of LV. Obviously, this phenomenon should be considered as a manifestation of the interaction of ventricles.
FEATURES OF TRANSPITSPIDE FLOW FOR HSN
In patients with HSN, with all types of diastolic dysfunction, LV usually observe similar changes in the dopplerhocardiographic indices of the PJ filling. However, the correlation relationships of the parameters of the transit-propelled and transmittral flow, which are quite clearly traced in healthy individuals, are significantly more weak with HSN. In this regard, the indicators of the filling of the PJ can acquire an independent diagnostic value. Thus, the presence of signs of the diastolic dysfunction of the PJ with normal indicators of the diastolic filling of LV, as a rule, indicates pseudonalization of the latter. This is proved by evaluating the blood flow in pulmonary veins from a perverse approach, when pronounced reverse blood flows are found during the atrial systole and the predominance of diastolic peak speed over the systolic. In another study, there was no close relationship between the parameters of the diastolic function of the PJ and the indicators of the systolic function of the LV, its size or wall thickness.
One of the most important to assess the severity of the CHHN transmittral flow parameters is known, is a period of slowing the first peak (DT), reflecting the pressure of the junction in pulmonary capillaries and to a certain extent - the severity of pulmonary hypertension (LH). At the same time, the early diastolic content of LV can impermatably affect the increase in the pressure in the PJ through the dyskinesia of the MZhP. Probably, the degree of shortening the DT of the transcispical flow is associated with the severity of LH and the overload pressure of the PJ.
Ways of forming dysfunction pzh
The most common causes of dysfunction of the ventricles of the heart are IBS and arterial hypertension (AG), less often - cardiomyopathy. The defeat of the PJ extremely rarely occurs at intact LV. Moreover, the primary disorders that lead to the occurrence of PJ dysfunction are most often formed in LV, left atrium (LP) or pulmonary veins. At the same time, independently of the triggering factor, the Hypertension of the PJ and the increase in the PZh is plays a leading importance in the formation of pump failure.
In patients with IBS, the leading mechanism for the defeat of the PJ is disturbances of the coronary blood circulation and an increase in post-loads against the background of LV dysfunction and the increase in pressure in LA. The radionuclide method found that in patients with IBS, the contractile function of the PJ primarily correlates with FV LV, and not with the degree of stenosis of the right coronary artery.
Many patients with acute myocardial infarction (im) arise global and regional PJ Dysfunction, the degree of which is largely depends on the localization and prevalence of LV defeat. PJ dysfunction of various severity is observed approximately 40-50% of cases of LV lower localization. In these patients, there is no direct connection between the fractions of the height of the ventricles of the heart, however, there is a concomitant violation of the mobility of the free wall of the PJ. Probably, with LV lower localization, the PZ dysfunction is caused by the accompanying infarction of the free wall of the PJ. In turn, the ischemic dysfunction of the myocardium PJ has mechanically adverse effects on the function of both ventricles, since it leads to a decrease in the preload of the LV and a reduction in cardiac output.
Unlike patients with the bottom, the strong correlation between the severity of PJ and LV dysfunction after the transmural of the front localization indicates the relationship of the PJ dysfunction in these patients with disorders of the pumping function and the diastolic filling of the LV. Consequently, the PJ Dysfunction may reflect the filling pressure of the LV and post-loading of the PJ in patients with extensive front.
With the AG, a small circle of blood circulation is damaged by the same humoral factors that lead to an increase in systemic blood pressure. The disorder of the diastolic function of the LV, typical for systemic AG, is often associated with the diastolic dysfunction of the PJ, also exposed with pressure overload. However, the most important factors, independently defining the formation of diastolic dysfunction of the PJ with the system AG, according to our data, are the thickening of the wall of the LV and hypertrophy of the MZP.
When comparing the diastolic function of the PJ in patients with HSN, pulmonary hypertension, against the background of the preserved contractile ability of LV and healthy persons, it was found that CHF is often accompanied by violations of the diastolic function of the PJ. At the same time, the mechanisms for the occurrence of these disorders are not fully refined. Although the increase in pressure in LA, determined in the majority of patients with severe CHD, leads to the diastolic dysfunction of the PJ, its formation may be due not only to the LG itself, but also by interventricular interaction.
PJ Dysfunction and HSN Progression
The PJ dysfunction can play an independent and significant role in the progression of hemodynamic disorders in patients with lesions of LV and left ventricular failure.
The physiological role of the PJ primarily consists in ensuring blood flow through the lungs. The emptying of the PJ allows to maintain normal pressure in the system of the main veins, which prevents their overflow by blood, exclamation and prevents the occurrence of stagnation in a large circle circle. In patients with LV dysfunction, the increase in pressure in the LD leads to an increase in pressure on the paths of the inflow to it - in the pulmonary veins and capillaries. The condition for maintaining a normal pressure gradient between LP and LA in 20 mm Hg. Art. Necessary to ensure blood current through the lungs is an increase in preload by increasing the tone of the veins, the return of blood to the heart and formation of venous LH. When progressing hsn, pressure in pulmonary capillaries can achieve critical level With the heating of liquid into the cavity of the alveoli and the occurrence of edema of the lungs. However, the inclusion of baroreceptors due to the increase in pressure in the LP through the reflex of KITEEV leads to arterioleary LH, which allows to unload a small circle of blood circulation to a certain extent.
So, an increase in the preload of the LV is first conjugate with the overload of the PJ volume; Then the increase in pressure in La creates an additional pressure load. Development under these conditions Hypertrophy of PJ, and then its dilatation, lead to contractual dysfunction of myocardium, accompanied by pressure growth in pulmonary capillaries, increase pressure in the right of atrium and central venous pressure. The end result is to reduce the diastolic filling of the LV and the reduction of cardiac output. Even with common pathological changes in PJ, compensation can be maintained for a certain period of time by increasing the reduction of its free wall and MZP. The exhaustion of compensatory mechanisms supporting the PJ function leads to the emergence of symptoms of worldwide failure. The situation is exacerbated by the stretching of the ring of the right atrioventricular hole with the occurrence of relative deficiency of the tricuspid valve, and in the future - dilatation of the right atrium and in many cases - flickering arrhythmia. The appearance of deficiency of the tricuspid valve is conjugate with a more pronounced insufficiency of blood circulation in a large circle and correlates with the expansion of the right heart departments.
In the study of the functional state of the heart chambers in patients with post-infarction cardiosclerosis, regardless of the severity of the CHF, there are differences of the pumping function of the ventricles. In contrast to healthy persons in which FV LH is higher than the FV PZ, in patients with the CXN I functional class (FC) of FV LV decreases, while FV PZ is maintained within the normal range and in many cases exceeds FV LV. For patients with HSN II and III FC, it is characterized by the excess of FV PJ compared to such LV, however, on the background of reducing the pump function of both ventricles. In the group of patients with CXH IV FC, the values \u200b\u200bof the FV of both ventricles are aligned with a generally significant reduction in the contractile ability of myocardium.
Given the essential importance of the right-hand heart departments in the mechanisms of compensation and progression of the CHF, the study of systolic and diastolic function of the PJ is important for assessing the prediction of patients and determining therapeutic tactics. In a number of studies, it is shown that with a stagnation of CXN, the PZh function is more connected with the tolerance of physical exertion than the LV function, and the FV PJ has an independent value for survival. PJ dysfunction begins to be determined in patients with HSN II FC. It is with a decrease in FV PJ below 40% associated the transition of patients in IV FC; Therefore, low FV PZ is a bad prognostic sign. On the other hand, in patients with low FV LV and sharply reduced physical load tolerance, the preserved PJ function (which indicated its shortening\u003e 1.25 cm) was a reliable predictor of the best survival. This indicator had a sensitivity of 90%, the specificity of 80% and the predictive accuracy of 83% for the separation of survivors during the observation period from unbearable. When conducting studies of the function of both ventricles in patients with IDAs with dilatation of LV in front of the aorto-coronary shunting, it was found that FV PZ is more accurate than the FV LV, the induration of the survival of this category of patients.
The diastolic function of the PJ can be a significant factor in the determination of symptoms and forecast. However, it is unclear whether the disorders of the PJ filling with the result of its defeat actually or are formed against the background of the restrictive type of filling of the left sections of the heart. According to our data, in patients with agricultural diastolic function, the PJ occur in parallel with changes in the diastolic filling of LV, however are formed later.
In many patients with HSN, during the DopplerHocardiographic study, restrictive filling of LV (E / A\u003e 2) is recorded and the type of impaired relaxation or a tendency to pseudonormalizing the filling of PJ (E / A less than 1 or more than 2). The use of an angiotensin-converting enzyme inhibitors in the acute test leads to multidirectional changes in flows in the left and right hearts of the heart: a decrease in the degree of restriction of filling LV (decrease in the E / A transmittral flow) and a decrease in the disorders of the Relaxation of the PJ (an increase in the E / A of the transstickspedral flow). The discovered phenomenon is not associated with a decrease in pressure in LA or pressure gradients on the tricuspid valve, and apparently reflects the direct interaction of the ventricles during the early phase of diastole.
These data indicate the close interdependence of the ventricles of the heart, which is probably enhanced with CHF. Therefore, in the overwhelming majority of patients with CHSN on the background of IBS, AG and cardiomyopathy, the PJ state should be considered due to the function of LV, through the prism of the interaction of the left and right hearts.
Interaction and interdependence of ventricles
The true nature of the relationship between PJ and LV, even with those pathological conditions, which selectively influence the large circle of blood circulation, is not yet clear enough. In some patients, pronounced LH leads to clinical manifestations Reasonless deficiency, while other patients with LH dominate signs of left ventricular insufficiency. Not clear whether these features are due clinical picture Differences of the structure and geometry of the heart chambers, metabolic disorders, or they are associated with the influence of interventricular interaction, as well as peripheral factors on the manifestation of dysfunction of the heart muscle.
Anatomically combined blood supply system, fibrous muscular apparatus, a common partition, pericardium and intragenium pressure, heart ventricles are subject to close mechanical and functional interaction, which allows you to consider the heart as a mechanical single or sycitium. The interventricular interaction is expressed in the mutual influence of the reduction, the post- and preload of both ventricles, their interdependence during the phases of systole and diastologists, both in the norm and during myocardial lesions.
The interaction of the ventricles in each of the phases of the cardiac cycle has significant physiological and pathophysiological significance. For example, the systolic function of LV significantly affects the reduction of the PJ. The experiment shows that about 20-40% of systolic pressure in the PJ and the volume of emissions from the PJ are a consequence of the reduction of LV. This dependence of the PJ from LV allows you to explain the response of the PJ for overloading the volume and pressure of myocardial LV. The main factor through which the interaction of ventricles is mediated, is MZP. One of the possible factors for the implementation of interventricular interaction is the deformation of the ventricles, which is formed depending on the ratio of forces in the field of MZHP, the elastic properties of the myocardial wall and the severity of its structural changes, in particular hypertrophy and dilatation.
The interaction of the ventricles of the heart becomes especially distinct with sudden changes in the position of the body, due to the phases of breathing and fluctuations in the preload. When conducting in healthy volunteers, the Valzalviva samples during the phase of the flooring volumes of LV and PZ were progressively decreased, and the PJ is to a greater extent than LV. After the start of the relaxation phase, the KLO PJ suddenly increased sharply, while the BLA continued to decrease. Obviously, the transient overload of the PJ and the associated displacement of the MZHP led to a change in the geometry of the LV and a decrease in its volume, which in turn caused a decrease in systemic blood pressure.
A sudden reduction in the contractile ability of the PJ is usually leading to a significant decrease in cardiac output due to a sharp decrease in pressure in the LD and the preload of LV. This condition can be corrected by increasing the volume of circulating blood, but hypervolemia is always associated with the volumetric overload of the PJ and the increase in central venous pressure. Although the strengthening of the contractile activity of LV allows to somehow support the release of blood from the LV, without an adequate increase in the PJ emission, the pressure in the LP has a tendency to further decrease.
The assumption that the abbreviation of the LV wall is the most important factor in maintaining the systolic function of the PJ, can explain the response of the PJ to the LV Ischemia. On the other hand, in the insulated heart of the heart, Ischemia of the free wall of the PJ slightly influenced the systolic pressure in the LV. The acute decrease in the preload of the PJ during samples with nitroglycerin contributes to an increase in the resistance of the LV and the finite-diastolic voltage, and changes in the reduction of the free side wall of the LV and its volume with coronary occlusion can directly affect the pressure in the PJ. Finally, Izhemia MZP influenced the function and right, and left ventricles.
With a sudden decrease in the post-loading of the LV, the duration of the emission of the PJ is reduced, which in turn is reliably connected with the length of the LV systole. Probably, the duration of the emission of the PJ is conjugate with the reduction of LV through the systolic interaction of the ventricles. But the transformation of hemodynamic disorders in the LVE on the PJ occurs in the aggregate effects of biochemical factors, pericardium, interventricular septum and changes in the La system. Overloading PZ pressure first causes a number of its structural changes and appropriate adaptation of the state of hemodynamics. And yet quite rapidly developing expressed manifestations of destroying failure with characteristic of it clinical signs. Increased postning in the development of LH aggravates the Dysfunction of the PJ, while the correction of lesions of the left heap departments with a decrease in the degree of pulmonary venous and arterial hypertension reduces the deficiency of the PJ.
A direct consequence of severe LH is a long-term chronic progressive decrease in the PJ voltage, which in turn, to the insufficiency of the tricuspid valve. According to the DopplerHocardiographic study, tricuspid regurgitation remains sufficiently long. On the other hand, with a pronounced LG, the relaxation of the left sections of the heart in the phase of isoovolumical relaxation is disorganized, which causes a violation of the filling of LV. The described effects are likely to be mediated via MZhP, and such an asynchronism of the ventricles of the heart presents another possible way of forming interventricular interaction.
In the overload of PJ by pressure and / or volume, the direction of the MZHP movement may vary: it moves to the Sisteole towards the PJ, and not LV. The formation of this phenomenon, primarily depends on the severity of LH. At lower levels of pressure in LA, the normal focus of the MZP movement is usually preserved, while its paradoxical movement is formed with pronounced LH. In these patients, there are simultaneously significant hypertrophy and dilatation of the PJ, which indicates a significant overload of the PJ. As the PJ expansion with impaired MZP movement, the LV dimensions are progressively reduced, obviously due to the compression of its huge PJ, which occupies most of the intrapericardial space.
The interaction of the ventricles of the heart is especially pronounced in patients with dilatation cardiomyopathy. Obviously, this is due to an increase in the contribution of LV to ensuring systolic pressure in the PJ. This phenomenon is consistent with the reduced elasticity of the MZP, which leads to an increased pairing between the ventricles. On the other hand, the PG dilatation changes the peak filling rate of LV.
A significant role in the implementation of the systolic and diastolic interaction of the ventricles of the heart is played by pericardium, largely determining pressure and volume in the heart chambers. During a sharp increase in the size of the heart, which leads to the stretching of the pericardium, the elastic properties of pericardia limit the further dilatation of the heart and the ability of ventricles to increase the impact volume. On the other hand, an increase in the volume of the PJ can change the diastolic extension of the LV. The interdependence of the ventricles is enhanced as a direct consequence of the elastic properties of pericardia. The appearance of pericardial restriction, which is characterized by an unchanged shock volume against the background of an increase in pressure in the right of atrium and the pressure of the junction in the pulmonary capillaries during the load, does not depend on the degree of reducing the maximum consumption of oxygen or the severity of the CHF. On the contrary, with an elastic pericarde, the shock volume is ensured due to a pronounced increase in the pressure of the jam in pulmonary capillaries at a relatively low pressure in the right atrium.
Thus, the PJ dysfunction plays a significant role in the mechanisms of the progression of the CHF. Its formation must be viewed through the prism of the assessment of the interdependence and interaction of the left and right ventricles of the heart. The definition of the functional state of the PJ is an important factor in the gravity of the clinical course and the forecast of patients with CXN.
LITERATURE
- Working classification of heart failure of the Ukrainian scientific society of cardiologists (1996). Ukr. Cardiol. Journal 1996; 5-6: 125-128.
- European Study Group on Diastolic Heart Failure. How to Diagnose Diastolic Heart Failure. Europ. Heart J. 1998; 19: 990-1003.
- The Task Force of the Working Group on Heart Failure of the European Society of Cardiology. THE TREATMENT OF HEART FAILURE. Europ. Heart J. 1997; 18: 736-753.
- Effects of ENALAPRIL ON MORTALITY IN SEVERE HEART FAILURE: Results of the Cooperative North Scandinavian Elapril Survival Study (CONSENSUS). The Consensus Trial Study Group. NEW ENGL. J. Med. 1987; 316: 1429-1435.
- Effects of ENALAPRIL ON SURVIVAL IN PATIENTS WITH REDUCED LEFT VENTRICULAR EJECTION AND CONGESTIVE HEART FAILURE. The Solvd Investigators. NEW ENGL. J. Med. 1991; 325: 293-302.
- Mareev V.Yu. New achievements in optimizing the treatment of chronic heart failure. Cardiology 1997; 12: 4-9.
- Feigenbaum H. echocardiography. 4-th Edition. Philadelphia: Lea-Febirger, 1987. 580 p.
- Oldershow P. Bishop A. The DiffiCulties of Assessing Right Ventricular Function. Brit. Heart J. 1995; 74: 99-100.
- Schiller N. Osipov MA Clinical echocardiography. M. 1993. - 347 p.
- Gavrisyuk V.K. Jachnik A.I. Chronic pulmonary heart. K. 1997. - 96 p.
- Mamedova F.A. Modern approach To the study of cardiohymeodynamics of the right ventricle for diseases of myocardium. Cardiology 1987; 12: 112-114.
- Bobrov V.A. Yabluchansky N.I. Guide for clinical echocardiography. Kharkov, 1995. - 235 p.
- Azizov V.A. Jamilov R.R. The relationship between the functional state of the heart cameras and the degree of heart failure in patients with post-infarction cardiosclerosis. Cardiology 1998; 5: 45-48.
- Kubota S. Kubota S. IWASE T. ET AL. Right Ventricular Function in Patients with Dilated Cardiomyopathy: Assessment using Krypton-81 M Blood Pool Scintigraphy. J. Cardiol. 1993; 23 (2): 157-164.
- ZoghBi W.A. Habib G.B. Quinones M.A. Doppler Assessment of Right Ventricular Filling in a Normal Population. COMPARISON WITH LEFT VENTRICULAR FILLING DYNAMICS. Circulation 1990; 82: 1316-1324.
- Bobrov V.A. Chubovny V.N. Ivanov Yu.A. Pavlyuk V.I. Transstoracal echocardiography: research methodology and clinical interpretation. K. 1998. - 83 p.
- COHEN V.I. PietrolUngo J.F. Thomas J.d. et al. A Practical Guide. Assessment of Ventricular Diastolic Filling using Doppler Echocardiography. J.mer. Coll. Cardiology. 1996; 27: 1753-1760.
- YU C.M. Sanderson J.E. Chan S. et al. Right Ventricular Diastolic Dysfunction in Heart Failure. Circulation 1996; 8: 1509-1514.
- YU C.M. Sanderson J.E. Right and Left Ventricular Diastolic Function in Patients with And Without Heart Failure: Effect of Age, Sex, Heart Rate, and Respiration on Doppler-Derived Measurements. Amer. Heart J. 1997; 3: 426-434.
- Hubalewska-Hola A. STACHURA-DEREN M. Dubiel J. et al. Evaluation of Right Ventricular Function in Patients with Hypertrophic Cardiomyopathy. Przegl. Lek. 1996; 2: 67-72.
- Nagaya N. Satoh T. Uematsu M. et al. Shortening Of Doppler-Dersive Deceleration Time Of Early Diastolic Transmitral Flow in The Presense of Pulmonary Hypertension Through Ventricular Interaction. Amer. J. Cardiol. 1997; 79 (11): 1502-1506.
- SETARO J.F. Cleman M.W. Remetz M.S. The Right Ventricle in Disorders Causing Pulmonary Venous Hypertension. Cardiol. CLIN. 1992; 10 (1): 165-183.
- Berger H. Johnstone D. Sands Y. et al. Response of Right Ventricular Ejection Fraction to Upright Bicycle Exercise in Coronary Arttery Disease. Circulation 1979; 60: 1292-300.
- Lopez-Sendon J. Lopez de Sa E. Delcan J.L. ISChemia Right Ventricular Dysfunction. Cardiovasc. Drugs Ther. 1994; 8 (2): 393-406.
- Goldstein J.A. Right Heart Ischemia: Pathophysiology, Natural History, and Clinical Management. Prog. Cardiovasc. DIS. 1998; 40 (4): 325-41.
- Caplin J. The DiffiCulties in Assessing Right Ventricular Function. Heart 1996; 3: 322.
- Baker B.J. Franciosa J.A. Effect of the Left Ventricle on the right ventircle. Cardiovasc. CLIN. 1987; 17 (2): 145-55.
- MySlinski W. Mosiewicz J. Ryczak W. et al. Right Ventricular Function in Systemic Hypertension. J. Hum. Hypertens. 1998; 12 (3): 149-155.
- Zharinov O.I. Anchine HD Salam Said. Geometric remodeling and diastolic filling of heart ventricles in patients with essential hypertension. Ukr. Cardiol. Journal 1999; 3: 25-29.
- Furey S.A. Harrison A. Levy M.N. The Essential Function of the Right Ventricle. Amer. Heart J. 1984; 107: 404-410.
- Schuler G. Hoffman M. Schwarz F. et al. Effect of ThromBolytic Therapy On Right Ventricular Function in Acute Inferior Wall Myocardial Infarction. Amer. J. Cardiol. 1984; 54: 951-957.
- Amosova E.N. Clinical cardiology. In 2 volumes. Tom I. K. "Healthy'y", "Bookplus", 1998. - 710 p.
- Knyoshov G.V. Beared Ya.A. Acquired heart defects. K. 1997. - 279 p.
- Small L.T. Gorb Yu.G. Rachinsky I.D. Chronic blood circulation failure. K. "Healthy'y", 1994. - 623 p.
- Weber K.T. Janicki J.S. Campbell C.H. et al. Pathophysiology of Acute and Chronic Cardiac Failure. Amer. J. Cardiol. 1987; 5: 3-9.
- Jamilov R.R. Azizov V.A. The functional state of the right heart departments in patients with post-infarction cardiosclerosis according to contrast echocardiography. Cardiology 1998; 7: 24-28.
- Ostrumov E.N. Cormer A.E. Yermolenko A.E. and others. The fraction of the emission of the right ventricle as an indicator of the effectiveness of myocardial revascularization in patients with coronary heart disease with stagnation of circulatory failure. Cardiology 1996; 4: 57-61.
- Polak J.F. Holman B.L. Wynne J. et al. Right Ventricular Ejection Fractions: An Indicator of Increased Mortality in Patients with Congestive Heart Failure Associated with Coronary ARTERY DISEASE. J.mer. Coll. Cardiol. 1983; 2: 217.
- Karatasakis G.T. Karagounis L.A. Kalyvas P.A. et al. Prognostic significance of echocardiography of echocardiographically estimated Right Ventricular Shortening in Advanced Heart Failure. Amer. J. Cardiol. 1998; 82 (3): 329-34.
- Henein M.Y. O'Sullivan C.A. Coats A.J. et al. Angiotensin-Converting Enzyme (ACE) Inhibitors Revert Abnormal Right Ventricular Filling in Patients with Restrictive Left Ventricular Disease. J.mer. Coll. Cardiol. 1998; 32 (5): 1187-1193.
- Li k.s. Santamore W.P. Contribution of Each Wall to Biventricular Function. Cardiovasc. RES. 1993; 27 (5): 792-800.
- Santamore W.P. Dell'italia L.J. VENTRICULAR INTERDEPENDENCE: Significant Left Ventricular Contributions to Right Ventricular Systolic Function. Prog. Cardiovasc. DIS. 1998; 40 (4): 289-308.
- Aebischer N. Malhotra R. Connors L. et al. Ventricular Interdependence During Valsalva Maneuver As Seen by Two-Dimensional Echocardiography: New Insights About An Old Method. J. am. SOC. Echocardiogr. 1995; 8 (4): 536-42.
- Ludbrook P.A. Byre J.d. MCKNIGHT R.C. Influence of Right Ventricular Hemodynamics On Left Ventricular Pressure Volume Relass in Man. Circulation 1979; 59: 21-31.
- Santamore W.P. Lynch P.R. Heckman J.L. et al. Left Ventricular Effects on Right Ventricular Developed Pressure. J. Appl. Physiol. 1976; 117: 211-221.
- Yamaguchi S. Li K.S. Harasawa H. et al. The Left Ventric Affects The Duration of Right Ventricular Ejection. Cardiovasc. RES. 1993; 27 (2): 211-215.
- Stojnic B.B. Brecker S.J. Xiao H.B. et al. Left Ventricular Filling Characteristics in Pulmonary Hypertension: A New Mode of Ventricular Interaction. Brit. Heart J. 1992; 68 (1): 16-20.
- Zhao Shufan, Chazov I.E. RESTVANOVA EN et al. The condition of the right and left ventricles of the heart in patients with primary pulmonary hypertension with various characteristics of the interventricular partition movement (echocardiographic study). Cardiology 1994; 12: 48-52.
- Agata Y. Hiraishi S. Misawa H. et al. Two-Dimensional Echocardiographic Determinants of Interventricular Septal Configurations in Right or Left Ventricular Overload. Amer. Heart J. 1994; 110: 819-825.
- Farrar D.J. Woodard J.C. Chow E. Pacing-Induced Dilated Cardiomyopathy Increases Left-to-Right Ventricular Systolic Interaction. Circulation 1993; 88 (2): 720-725.
- Konstam M.A. Kronenberg M.W. UDelson J.E. et al. Effect of Acute Agiotensin Converting Enzyme Inhibition On Left Ventricular Filling in Patients with Congestive Heart Failure. Relation to Right Ventricular Volumes. Circulation 1990; 81 (2): III-115-122.
- Janicki J.S. Influence of the Pericardium and Ventricular Interdependence on Left Ventricular Diastolic and Systolic Function in Patients with Heart Failure. Circulation 1990; 81 (2): III-15-20.
Type 1 - What is this disease, and how should it be treated? The answer to the asked question we will give in the materials of the submitted article. In addition, you will learn about why such a pathological condition arises, and for what obvious features it can be identified.
general information
Before answering the question of why diastolic dysfunction of the left ventricular 1 type occurs, it should be found out what is a given organ.
The left ventricle is called one of the 4th person. It is in him that he originates which provides a continuous blood flow in the body.
What is the disease?
The diastolic dysfunction of the submitted part of the heart is called a significant decrease in its ability to distinguish the blood into its cavity from the pulmonary artery. In other words, such a pathological state leads to the impossibility of ensuring normal blood circulation.
Thus, the diastolic dysfunction of the type of type 1 is a severe heart disease, which is characterized by the insufficient ability of the said part of the organ to relax during the diastole period. It should be especially noted that it can occupy about 0.4 seconds. This time is quite enough in order to fully restore the tone, as well as the energy fullness of the heart muscle.

What is dangerous for the disease?
The diastolic dysfunction of the type of type 1 type is caused by a drop in the expulsion fraction, which further leads to a noticeable decrease in the shock volume. To prevent blood stagnation in the lungs and compensate for dilatation, the increase in ventricle begins. If such a protective reaction of the body does not follow, the obvious threat of pulmonary hypertension appears (repeated), and also significantly increases the load on another ventricle (right), which subsequently leads to a decrease in its volume. As a result, venous hyperemia may occur in it. If there is an acute dysfunction, then easily develops swelling of the lungs.
Probable causes of occurrence
Why can diastolic dysfunction of left ventricular 1 type can develop? The reasons for this phenomenon lies in the following:
- hypertensive pathologies;
- hypertrophic cardiomyopathy;
- infiltrative (periodic) heart lesions (i.e., infarction, IBS, chronic hypertension (arterial), as well as hypertrophy of individual heart segments that are outside the dilatation zone and thinning).
Signs of deviation
This state very often leads to the development of secondary pulmonary arterial and venous hypertension. This pathological condition may manifest itself in the following:

- permanent cough (often parole);
- night dnae (paroxysmal);
- dyspnea.
What other features are 1 type? Symptoms of such deviations can not exhibit any time. However, with the development of the disease, patients begin to observe such signs as:
- regular pain in the heart, which carry an attacking character (both under ischemic disease);
- swelling of the lower extremities;
- shortness of breath (may even be observed at rest);
- spastic phenomena;
- feeling shortness of air.
With such signs, it is necessary to apply for consultation to the attending physician. After all, the earlier this pathological state will be revealed, the easier it is to take control. If the presented disease is detected too late, its treatment will last a very long time, with a large quantity medicinal preparations and all necessary procedures.
How to cure?
Currently, a single scheme of therapy, which would be recognized by the majority of specialists, does not exist. This is partly due to the fact that this disease is satisfied poorly to diagnose. As mentioned above, such a deviation takes place very long asymptomatic, as a result of which the patient appeals for medical help too late.
So what should I do if you have discovered the diastolic dysfunction of the left ventricle 1 type? Treatment of such a disease comes down to eliminating the reasons that provoke negative trends. Thus, patients need:
- cure existing ischemia;
- do the normalization of heart rhythm;
- drop blood pressure.
Among other things, when discovering such a pathological condition, the patient is prescribed drugs group of ACE blockers. Most often, the choice of specialists falls on "Lisonopril". It is prescribed in the form of tablets of 20-40 milligrams per day (in two receptions).

Not bad results in the treatment of this deviation can be achieved and by using calcium blockers. Thus, both drug groups reduce blood pressure, significantly reduce the needs of cardiac tissues in oxygen, and also stop and reduced by the way, due to the reception of these drugs, the operation of the heart diastole is improved, which further leads to the normalization of hemodynamics.
The best results of the treatment of such a disease were noted with a combination of potassium-saving diuretics with cardiac drugs. In case of acute need, other hypotensive medicines can also be used.
For a clear and coordinated work of the heart, the harmonious work of the entire cardiovascular system is necessary. The diastolic dysfunction of myocardium refers to very serious pathologies, which causes chronic CH. The heart is a complex system, and each of its layer is responsible for an important function, which makes it possible to maintain the viability of a person. The diastole of the ventricles is responsible for compressing and relaxing the heart muscle. The walls of the heart are first relaxed, taking blood, then pushing it in the necessary direction.
Low diastolic dysfunction 1 type: What is it? The diastolic dysfunction of the myocardium of the left ventricle is caused by the impossibility of mothic threads to take the required amount of blood. As a result, the left atrial strengthens the production. This contributes to the fact that the atrium is overloaded and increases in volume. Such pathology sometimes causes simple in lungs and arteries, and this, in turn, makes it difficult for blood circulation throughout the body.
The study of disorders of diastolic work of the heart is an urgent task.
It is worth knowing! The deterioration of pathological deviations can lead to the development of chronic heart failure.
The disease is divided into several types:
The causes of the occurrence of illness
Statistics notes that the key factor in the formation of the disease is the malfunction of the myocardial function correctly take and push blood. Due to the limited elasticity of muscle mass, some diseases can be formed:, IHD, heart attack.
The disease can manifest itself both in adults and in newborns. In infants, the strengthening of blood supply to lungs causes a number of complications:
- an increase in heart offices in size;
- atrium overload;
- the possibility of the heart muscle is disturbed;
- tachycardia develops.
The child does not always require special treatment, because the condition does not apply to pathological.
Basic symptoms of the disease
Myocardium diastolic dysfunction does not consider an independent disease. As a rule, it is in itself a sign already developing disease. This pathology leads to heart failure and manifests itself with the following symptoms:
- edema legs;
- high fatigue;
- the appearance of shortness of breath even with a small exercise. If manifests itself in a state of rest, the disease passed on a serious form;
- rhythm of heart;
- the skin is pale, especially it concerns the parts of the body removed from the heart.
Cough can also be attributed to one of the symptoms of CH. Most often, it appears at night, pointing to the resulting stagnation in the lungs.
Diagnostics of diastolic heart failure
Diagnosing a disease at an early stage will avoid irreversible changes.
To determine the diagnosis, as a rule, you need three conditions:
- manifestation of symptoms and signs of CH;
- the systolic function of the LV is normal or slightly lowered;
- in the instrumental methods of diagnostics, disorders of the LV operation are detected, increasing its rigidity.

Diagnostics in the early stages makes it possible to prevent irreversible changes in the heart
The main instrumental methods of diagnosis include:
- two-dimensional echocardiography with dopplerography is one of the most effective methods for determining the diagnosis;
- radionuclide Ventriaculography will determine the failure of myocardial reduction functions;
- Ehoche reveals;
- the chest x-ray will determine the pulmonary hypertension.
Methods of treating disease
The main problem for the effective treatment of the disease remains the restoration of a full-fledged contractility. Miocardium diastolic dysfunction includes drug and operational therapy. Therefore, treatment has several main directions:
- stabilization of normal heart rhythm to prevent the development of arrhythmia;
- treatment of ischemic disease;
- stabilization of blood pressure.
With the aim of comprehensive treatment Attributes the following groups of drugs:
| Adrenoblocators | aimed at normalization of heart rhythm, decay of blood pressure, improve the food procedure of myocardium cells |
| Inhibitors or sartans | work, improve its elasticity, reduce the load. Significantly improve the results of analyzes of patients with permanent heart failure |
| Diuretics | explore excess liquid, reducing asthmatic manifestations, and also allow control of blood pressure. The medical preparation is prescribed in small quantities, because it leads to a decrease in shock volume |
| Calcium antagonists | assign myocardial relaxation, reduce blood pressure |
| Nitrate | only additional drugs that can be appointed with myocardial ischemia |
The treatment process takes place in the hospital, where medical personnel observes for the patient's condition.
A patient with dysfunction of the ventricle must be observed a diet. To do this, limit the consumption of salt, monitor the drinking liquid - this will reduce the load on blood system. It is necessary to eat rationally, adhering to the regime, it is necessary to separate food for 4-6 times. It is enough to abandon fat, fried and acute.

Treatment is aimed at the correction of hemodynamic disorders
It is also important to adjust your lifestyle: get rid of bad habits, do not overstrain, get enough sleep. Pay attention to physical activity. Loads must be rational, comply with the capabilities of the body. It is necessary to carry out more time in the fresh air. If the disease is complicated, it is worth excluding the load or consult with the doctor.
Read also ...
- The work of "Alice in Wonderland" in a brief retelling
- That transformation. "Transformation. Attitude towards the hero from the sister
- Tragedy Shakespeare "King Lear": the plot and the history of the creation
- Gargantua and Pantagruel (Gargantua et Pantagruel) Francois Rabl Gargantua and Pantagruel Brief