The drug ketorol indications for use. We carefully read the instructions for using ketorol tablets. Instructions for use Ketorol
Dosage form"type =" checkbox ">
Dosage form
Film-coated tablets, 10 mg
Composition
One tablet contains
active substance - ketorolac tromethamine 10 mg
Excipients:
microcrystalline cellulose (type 102), pregelatinized corn starch, corn starch, anhydrous colloidal silicon dioxide, magnesium stearate
shell composition: Opadri 03K51148 green (hymethylcellulose (6crs), titanium dioxide E171, triacetin / glycerin, iron (III) oxide yellow E172, dye FD & C No. 1 (diamond blue FCF, aluminum varnish 11-13%)
Description
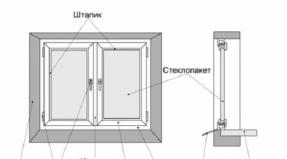
Pills round shape, with a biconvex surface, covered with a film shell of olive green color, engraved with "S" on one side and a smooth surface on the other side, with a diameter of (8.20 ± 0.20) mm and a thickness of (3.50 ± 0.20) mm.
Pharmacotherapeutic group
Anti-inflammatory and antirheumatic drugs. Non-steroidal anti-inflammatory drugs. Acetic acid derivatives. Ketorolac
ATX code М01АВ15
Pharmacological properties"type =" checkbox ">
Pharmacological properties
Pharmacokinetics
Ketorolac tromethamine is a racemic mixture of the enantiometric forms [-] S- and [+] R- with the S form, which has an analgesic effect.
When taken internally, ketorolac is well absorbed from gastrointestinal tract... The maximum concentration in blood plasma (0.7 - 1.1 μg / ml) is achieved 40 minutes after taking a dose of 10 mg on an empty stomach. Food rich in fat reduces Cmax and delays its achievement by 1 hour.
Ketorol® almost completely binds to plasma proteins (> 99%) due to a small volume of distribution (<0.3 л/кг).
The time to reach equilibrium concentration when taken orally is 24 hours when administered 4 times a day. When taken orally 10 mg, it is 0.39 - 0.79 μg / ml.
Almost all the substance circulating in the blood plasma is ketorolac (96%) or its pharmacologically inactive metabolite p-hydroxyketorolac.
Ketorolac is mainly excreted through the kidneys by excretion of ketorolac and its metabolites. In urine, up to 92% of the administered dose of the drug is found, 40% - in the form of metabolites, 60% - in the form of an unchanged substance, 6% of the administered dose - through feces. The drug passes through the placental barrier by 10%. It is found in low concentrations in breast milk. It passes through the blood-brain barrier poorly. The S-enantiomer is excreted twice as fast 2.5 h (SD ± 0.4) than the R-enantiomer - 5 h (SD ± 1.7) and clearance does not depend on the route of drug administration, it follows that the ratio of plasma S / R concentrations decreases with time after each dose. Metabolites have no significant analgesic activity.
In elderly patients (over 65 years of age), the half-life of the terminal phase, compared with that in young people, increases to 7 hours (from 4.3 to 8.6 hours). The total plasma clearance, in comparison with young people, can be reduced to an average of 0.019 l / h / kg.
Renal failure
When renal function is impaired, the elimination of ketorolac slows down, as evidenced by the lengthening of the half-life, which is between 6 and 19 hours (depending on the degree of insufficiency) and leads to a decrease in the total plasma clearance compared to young healthy volunteers.
There is a poor association between creatinine clearance and total clearance of ketorolac tromethamine in the elderly and in the population with renal failure (r = 0.5).
In patients with renal disease, the area under the curve of each enantiomer increased by approximately 100% compared to healthy volunteers. The volume of distribution doubles for the S-enantiomer and increases by 1/5 for the R-enantiomer. An increase in the volume of distribution of ketorolac tromethamine means an increase in the unbound fraction.
The rate of elimination decreases approximately in proportion to the degree of renal impairment, with the exception of patients with severe renal impairment. In such patients, the plasma clearance of ketorolac becomes slightly higher than expected for a given degree of renal damage.
Liver failure
There is no significant difference in the calculation of the half-life, area under the curve.
Pharmacodynamics
Ketorol® is a non-steroidal anti-inflammatory drug (NSAID) with analgesic and anti-inflammatory effects. The main mechanism of action of ketorol, like other NSAIDs, is manifested in its pharmacological effect - inhibition of prostaglandin synthesis. NSAIDs are most active in the periphery.
Ketorol® does not have a sedative or anxiolytic effect. The biological activity of ketorolac tromethamine is associated with form S. The peak analgesic effect of Ketorol occurs after 2-3 hours.
Indications for use
Short-term relief of acute pain syndrome of moderate and severe severity, as well as with the necessary analgesia with opioid analgesics in the postoperative period.
Method of administration and dosage
The potential benefits and risks of using Ketorol should be carefully considered before deciding on its use.
The total duration of treatment with Ketorol injection and Ketorol tablets should not exceed 5 days due to the risk of an increase in the frequency and severity of adverse reactions.
For patients from 18 to 64 years old
Ketorol tablets are taken once 20 mg (2 tablets), followed by 10 mg (1 tablet) after 4-6 hours 4 times a day, no more than 40 mg / day.
For patients ≥ 65 years of age with renal impairment and / or weight< 50 кг:
Ketorol tablets single 10 mg (1 tablet) followed by 10 mg every 4-6 hours four times a day, no more than 40 mg / day.
The minimum effective dose must be used.
Do not shorten the dosing interval from 4 to 6 hours.
Side effects
With an increase in the dose of the drug, the risk of an increase in the frequency and severity of adverse reactions increases. Patients should be warned of serious adverse drug reactions such as ulceration of the gastrointestinal tract mucosa, bleeding and perforation, postoperative bleeding, acute renal failure, anaphylactic and anaphylactoid reactions, liver failure.
In patients taking Ketorol or other non-steroidal anti-inflammatory drugs (NSAIDs), the most common (approximately 1% to 10% of patients) were observed:
From the gastrointestinal tract: abdominal pain *, constipation / diarrhea dyspepsia *, flatulence, gastrointestinal ulcer (stomach / duodenal ulcer), gastrointestinal bleeding / perforation, heartburn, nausea *, stomatitis, vomiting.
From other systems: impaired renal function, anemia, dizziness, drowsiness, edema, an increase in the content of liver enzymes,
headaches *, hypertension, prolonged bleeding time, itching, skin rashes, tinnitus, sweating.
* Incidence greater than 10%
Additionally, the following adverse events were reported:
General reactions: fever, infection, sepsis
Cardiovascular system: heart failure, tachycardia (heart palpitations), pallor, fainting.
Skin reactions: alopecia, photosensitivity, urticaria.
Gastrointestinal tract: anorexia, dry mouth, belching, esophagitis, thirst, gastritis, glossitis, hepatitis, increased appetite, jaundice, rectal bleeding.
Blood and lymphatic system: ecchymosis, eosinophilia, epistaxis, leukopenia, thrombocytopenia.
Metabolic disorders: weight change.
Nervous system: confusion, anxiety, asthenia, depression, euphoria, extrapyramidal symptoms, hallucinations, hyperkinesia, inability to concentrate, insomnia, nervousness, paresthesias, drowsiness, stupor, tremors, dizziness, malaise.
Reproductive system (women): infertility.
Respiratory system: asthma, cough, shortness of breath, pulmonary edema, runny nose.
Tactile organs: changes in taste, visual impairment, hearing loss.
Urogenital tract: cystitis, dysuria, hematuria, increased frequency of urination, interstitial, nephritis, oliguria / polyuria, proteinuria, renal failure, urinary retention.
Rarely observed adverse reactions are:
General reactions: Quincke's edema, death, hypersensitivity reactions such as anaphylaxis, anaphylactoid reactions, laryngeal edema, tongue edema, myalgia
Cardiovascular system: arrhythmia, bradycardia, chest pain, redness, hypotension, myocardial infarction, vasculitis.
Skin reactions: exfoliative dermatitis, erythema multiforme, Lyell's syndrome, bullous reactions including Stevens-Johnson syndrome and toxic epidermal necrolysis.
Gastrointestinal system: acute pancreatitis, liver failure, nonspecific ulcerative stomatitis, exacerbation of inflammatory bowel disease (ulcerative colitis, Crohn's disease).
Blood and lymphatic system: agranulocytosis, aplastic anemia, hemolytic anemia, lymphadenopathy, pancytopenia, postoperative bleeding.
Metabolic disorders: hyperglycemia, hyperkalemia, hyponatremia.
Nervous system: aseptic meningitis, convulsions, coma, psychosis.
Respiratory system: bronchospasm, respiratory depression, pneumonia
Organs of touch: conjunctivitis
Urogenital tract: flank pain with hematuria and / or azotemia, hemolytic uremic syndrome or without it.
Contraindications
Hypersensitivity to ketorolac or other nonsteroidal anti-inflammatory drugs
Complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses, and intolerance to acetylsalicylic acid or other NSAIDs (including a history)
Hives, rhinitis caused by taking NSAIDs (in history)
Intolerance to drugs of the pyrazolone series
Hypovolemia (regardless of the underlying cause)
Confirmed hyperkalemia
Erosive and ulcerative lesions of the gastrointestinal tract in the acute phase, gastrointestinal bleeding, including a history
Inflammatory bowel disease
Hypocoagulation (including hemophilia)
Hematopoietic disorders
Severe renal failure (creatinine clearance less than 30 ml / min)
Severe liver failure or active liver disease
Concomitant use with other non-steroidal anti-inflammatory drugs
Simultaneous reception with probenecid
Simultaneous reception with pentoxifylline
High risk of bleeding (including after surgery
Suspected or confirmed cerebrovascular bleeding, hemorrhagic diathesis,
Persons with hereditary fructose intolerance, deficiency of the enzyme lapp-lactase, glucose-galactose malabsorption
Pregnancy, childbirth and lactation
Children and adolescents under 18 years of age (efficacy and safety have not been established)
As a prophylactic analgesic before any major surgery.
For the treatment of postoperative pain in coronary artery bypass grafting.
Ketorolac is not indicated for the treatment of chronic pain.
Drug interactions
Ketorolac exhibits a strong degree of binding to human plasma proteins (on average by 99.2%), while the binding is independent of concentration.
Ketorolac should not be used with other drugs based on ASA = ASA (acetylsalicylic acid, aspirin) or with other NSAIDs (non-steroidal anti-inflammatory drugs), including selective cyclooxygenase-2 inhibitors, as this may increase the risk of induction of serious adverse events associated with by the action of NSAIDs (see section on contraindications).
Ketorolac inhibits platelet aggregation, reduces the concentration of thromboxane and increases the duration of bleeding. In contrast to the prolonged effects of aspirin, platelet function returns to normal within 24-48 hours after discontinuation of ketorolac.
The use of ketorolac in combination with anticoagulants such as warfarin is contraindicated, since the combined use of NSAIDs and anticoagulants can increase the anticoagulant effect (see section on contraindications).
Although studies do not indicate a significant degree of interaction between ketorolac and warfarin or heparin, with the simultaneous use of ketorolac and therapeutic drugs that affect hemostasis, including therapeutic doses of anticoagulants (warfarin), prophylactic low doses of heparin (2500-5000 units every 12 hours ) and dextrans, an increased risk of bleeding may be associated.
Reportedly, with the use of some drugs that inhibit the synthesis of prostaglandins, inhibition of renal clearance of lithium is observed, leading to an increase in the concentration of lithium in the plasma. During therapy with ketorolac, cases of increased plasma lithium concentrations have been reported.
Probenecid should not be used concomitantly with ketorolac due to the increased plasma concentration of ketorolac and its half-life.
NSAIDs should not be used for eight to twelve days after using mifepristone, as NSAIDs can weaken the effects of mifepristone.
When ketorolac is used concomitantly with oxpentifylline, there is an increased tendency to bleed.
Use Ketorol simultaneously with other drugs with caution:
As with all NSAIDs, caution should be exercised when using the drug together with corticosteroids due to the increased risk of ulceration or bleeding in the gastrointestinal tract (see the Special Instructions section).
There is an increased risk of gastrointestinal bleeding (see Special Instructions) when antiplatelet agents and selective serotonin reuptake inhibitors (SSRIs) are combined with NSAIDs.
According to the literature, some drugs that inhibit the synthesis of prostaglandins reduce the clearance of methotrexate, and thus, possibly, increase its toxicity.
Ketorolac tromethamine does not affect the binding of digoxin to blood proteins. In vitro studies showed that at therapeutic concentrations of salicylate (300 μg / ml), the binding of ketorolac decreased from approximately 99.2% to 97.5%, which is a calculated two-fold increase in the concentration of unbound ketorolac in blood plasma. Therapeutic concentrations of digoxin, warfarin, ibuprofen, naproxen, piroxicam, acetaminophen (paracetamol), phenytoin and tolbutamide do not affect the binding of ketorolac to proteins.
Combined use with diuretics can lead to a decrease in the diuretic effect and an increased risk of developing nephrotoxicity of NSAIDs.
As for all NSAIDs, the drug should be used with caution with the concurrent use of cyclosporine due to the increased risk of nephrotoxicity.
There is a risk of developing nephrotoxicity if NSAIDs are used in conjunction with tacrolimus.
NSAIDs can reduce the effects of diuretics and antihypertensive drugs. With the use of ACE = ACE (angiotensin converting enzyme) inhibitors and / or angiotensin II receptor antagonists in combination with NSAIDs, the risk of developing acute renal failure, which is usually reversible, may be increased in some patients with impaired renal function (for example, in dehydrated patients or elderly patients).
Therefore, the combination of drugs should be done with caution, especially in the elderly. Patients should be properly (as accurately as possible) dosage calculated, while attention should be paid to monitoring renal function at the beginning of concomitant therapy and periodically in the subsequent period.
NSAIDs can exacerbate heart failure, reduce GFR = GFR (glomerular filtration rate) and increase the level of cardiac glycosides in plasma when used together with cardiac glycosides.
Ketorolac has been shown to reduce the need for concomitant opioid analgesia when used to relieve postoperative pain.
Animal data show that NSAIDs may increase the risk of seizures associated with the use of quinolone antibiotics. Patients taking concomitantly NSAIDs and quinolones may have an increased risk of developing seizures.
The use of NSAIDs together with zidovudine increases the risk of hematological toxicity. There is evidence of an increased risk of hemarthrosis (accumulation of blood in the joint cavity) and hematomas in HIV (+) = HIV in patients with hemophilia receiving simultaneous treatment with zidovudine and ibuprofen.
When taken with antiepileptic drugs (phenytoin, carbamazepine), the frequency of attacks increases. When taken simultaneously with psychotropic drugs (fluoxetine, thiothixine, alprazolam), patients experience hallucinations.
With the simultaneous administration of ketorol and non-depolarizing muscle relaxants, patients experience shortness of breath.
special instructions
Since NSAIDs reduce platelet aggregation, it is necessary to prescribe ketorolac with caution to patients with impaired blood coagulation.
Undesirable effects can be minimized by using the lowest effective dose for the shortest period of time according to the control symptoms.
Gastrointestinal ulcers, bleeding and perforation
Gastrointestinal ulcers, bleeding, and perforation have been reported that can be fatal with nonsteroidal anti-inflammatory drug therapy, including ketorolac, and may occur at any time during treatment, with or without warning symptoms or previous serious gastrointestinal problems tract in the anamnesis.
Increased rates of clinically serious gastrointestinal bleeding were observed in patients under 65 years of age who received an average daily dose of more than 90 mg of ketorolac intramuscularly compared with patients who received parenteral opiates.
Elderly people have an increased incidence of side effects due to the use of non-steroidal anti-inflammatory drugs, especially gastrointestinal bleeding and perforation, which can be fatal.
The risk of gastrointestinal bleeding, ulcers or perforation increases with an increase in the dose of non-steroidal anti-inflammatory drugs, including intravenous ketorolac, in patients with a history of ulcers, especially complicated by bleeding or perforation, or in the elderly. The risk of clinically serious gastrointestinal bleeding depends on the dosage. In these patients, treatment should be started with the lowest dose available. For these patients, as well as for patients requiring concomitant use of low-dose aspirin or other drugs that may also increase the risks to the gastrointestinal tract, combination therapy with cytoprotectors (eg, misoprostol or proton pump inhibitors) should be prescribed. This age-related risk group for gastrointestinal bleeding is common to all nonsteroidal anti-inflammatory drugs. Compared with young patients, elderly people have an increased plasma half-life and reduced plasma clearance of ketorolac. A longer interval between doses of the drug is recommended.
Nonsteroidal anti-inflammatory drugs should be used with caution in patients with a history of inflammatory bowel disease (ulcerative colitis, Crohn's disease), as these conditions may worsen. Patients with a history of gastrointestinal toxicity, especially in the elderly, should report all unusual intra-abdominal symptoms (especially gastrointestinal bleeding), especially in the initial stages of treatment. If gastrointestinal bleeding or ulceration occurs in patients taking intravenous ketorolac, treatment should be discontinued.
Precautions are advised in patients concurrently receiving drugs that may increase the risk of ulcers or bleeding, such as oral corticosteroids, certain serotonin reuptake inhibitors, or anti-platelet drugs such as aspirin.
The use of the drug in patients taking anticoagulants such as warfarin is contraindicated.
As with other non-steroidal anti-inflammatory drugs, the percentage of patients and the degree of gastrointestinal complications that arise in them may increase due to an increase in the dose and duration of treatment with ketorolac when administered intravenously. The risk of clinically serious gastrointestinal bleeding depends on the dose of the drug. This is especially true for elderly patients who take an average daily dose of more than 60 mg of ketorolac intravenously. A history of peptic ulcer disease increases the likelihood of serious gastrointestinal complications during the use of ketorolac therapy.
Hematological effects
Patients with coagulation disorders should not take Ketorolac. Patients receiving anticoagulation therapy are at risk of bleeding when taking Ketorolac concurrently with these drugs. The simultaneous use of ketorolac and a low prophylactic dose of heparin (2500 - 5000 units every 12 hours), as well as dextran, has not been thoroughly studied, and therefore can also cause a high likelihood of bleeding. Patients who are already on anticoagulants or are receiving low-dose heparin should not use ketorolac. Patients taking other drugs that have a negative effect on hemostasis should be monitored when using Ketorolac. In controlled clinical trials, the incidence of clinically significant postoperative bleeding was less than 1%.
Ketorolac inhibits platelet aggregation and prolongs bleeding time. In patients with normal blood clotting, the coagulation time increased, but within the normal range from two to eleven minutes. In contrast to the long-term effect of aspirin, platelet function returns to normal within 24 to 48 hours after discontinuation of ketorolac.
There are reports of postoperative wound blood loss associated with perioperative use of Ketorolac with intramuscular or intravenous administration. Thus, ketorolac should not be used in patients who have had surgery with a high risk of bleeding. Special care should be taken in situations that do not allow abnormalities in hemostasis, for example, in cosmetic or one-day surgery, during prostate resection or tonsillectomy. When using Ketorolac, signs of wound bleeding and nosebleeds have been reported. Physicians should be alert to the pharmacological similarities between ketorolac and other non-steroidal anti-inflammatory drugs that inhibit cyclooxygenase, as well as the risk of bleeding, especially in the elderly.
Skin reactions
Serious skin reactions, some of them fatal, including exfoliative dermatitis, Stevens-Johnson syndrome and toxic epidermal necrolysis, have been reported very rarely in connection with the use of nonsteroidal anti-inflammatory drugs. Patients at risk for such reactions were identified at the very beginning of therapy: such reactions in most cases occurred in the first month of treatment. Treatment with ketorolac should be discontinued at the first manifestation of a skin rash, mucosal damage or other signs of hypersensitivity to the drug.
Systemic lupus erythematosus and Sharpe syndrome
Patients with systemic lupus erythematosus and Sharp's syndrome are at risk of aseptic meningitis.
Sodium / fluid retention in cardiovascular disease and peripheral edema
Patients with a history of hypertension and / or heart failure should be treated with caution, as fluid retention and swelling have been reported in connection with nonsteroidal anti-inflammatory drug therapy.
Fluid retention, hypertension and peripheral edema have been observed in some patients taking non-steroidal anti-inflammatory drugs, including ketorolac, so this drug should be taken with caution in patients with heart failure, hypertension, or similar pathologies.
Cardiovascular and cerebrovascular effects of the drug
For patients with a history of hypertension and / or mild to moderate congestive heart failure, appropriate monitoring and counseling is necessary, as fluid retention and swelling have been reported due to the use of non-steroidal anti-inflammatory drugs.
Epidemiological data suggest that the use of coxibs or some nonsteroidal anti-inflammatory drugs (especially in high doses) may cause a slight increase in the risk of arterial thrombotic complications (for example, myocardial infarction or stroke). Despite the fact that ketorolac did not reveal the ability to increase the number of thrombotic complications such as myocardial infarction, there is still insufficient data on the basis of which such a risk should be excluded when using ketorolac.
Patients with uncontrolled arterial hypertension, chronic heart failure, established ischemic heart disease, peripheral arterial disease and / or cerebrovascular disorder should take ketorolac only after a thorough examination. A similar decision should be made before starting treatment for patients with a risk factor for cardiovascular disease (eg, hypertension, hyperlipidemia, diabetes mellitus and smoking).
Cardiovascular disorders, renal and liver dysfunctions
Caution should be exercised in patients with pathologies that may cause a decrease in blood volume and / or renal blood flow, in which renal prostaglandins play a supporting role in providing renal perfusion. In such patients, the use of non-steroidal anti-inflammatory drugs can, depending on the dose of the drug, cause a weakening of the renal prostaglandin structure and can provoke overt renal failure. Patients who are depleted in volume due to blood loss or severe dehydration, patients with impaired renal function, heart failure, impaired liver function, the elderly, and patients taking diuretics are at great risk of such a reaction. Renal function should be monitored in these patients. Usually, after the termination of therapy with non-steroidal anti-inflammatory drugs, recovery follows before the start of treatment. Impaired recovery of lost fluid / blood during surgery, causing hypovolemia, can cause renal dysfunction, which in turn can be exacerbated by the use of Ketorolac. Thus, dehydration should be corrected and a specialist's strict observation of serum urea and creatinine, diuresis should be recommended until the patient is normovolemic. For patients on renal dialysis, the clearance of ketorolac was reduced to about half the normal value and the half-life was increased by about 3 times.
Effects on the kidneys
As with other non-steroidal anti-inflammatory drugs, ketorolac should be used with caution in patients with impaired renal function or a history of kidney disease, as it is a potent inhibitor of prostaglandin synthesis. Caution should be exercised, since nephrotoxicity has been identified with the use of ketorolac and other non-steroidal anti-inflammatory drugs in patients with pathologies that cause a decrease in circulating blood volume and / or renal blood flow, in which renal prostaglandins play a supporting role in maintaining renal perfusion.
In such patients, the use of ketorolac or other non-steroidal anti-inflammatory drugs can, depending on the dosage, provoke a reduction in renal prostaglandin formation and can cause overt renal failure or decompensated renal failure. Patients with impaired renal function, hypovolemia, heart failure, liver dysfunction, as well as those taking diuretics and the elderly are at great risk of such a reaction. After stopping the intake of ketorolac or other non-steroidal anti-inflammatory drugs, recovery usually follows to the state before starting the drug.
As well as with other drugs that slow down the synthesis of prostaglandin, it was reported that an increase in serum urea, creatinine and potassium was reported during the use of ketorolac trometamol, which may occur after a single dose of the drug.
Patients with impaired renal function: Since ketorolac trometamol and its metabolites are excreted primarily by the kidneys, patients with moderate to severe impairment of renal function (serum creatinine more than 160 μmol / l) are contraindicated to take Ketorolac. Patients with weaker renal impairment should receive a reduced dose of ketorolac (not exceeding 60 mg / day intramuscularly or intravenously) and their renal status should be under constant medical supervision.
Use for patients with impaired liver function: In patients with hepatic impairment due to cirrhosis, no clinically important changes in ketorolac clearance or terminal half-life were observed.
Boundary increases in one or more hepatic function indicators may appear. These disorders may be variable, may remain unchanged, or may progress with continued therapy. Significant increases (3 times higher than normal) in serum alanine aminotransferase or aspartate aminotransferase were observed in control clinical trials in less than 1% of patients. With developing clinical signs or symptoms associated with hepatic diseases, or with the appearance of systematic manifestations of diseases, Ketorolac should be discontinued.
Anaphylactic (pseudo-anaphylactic) reactions
Anaphylactic (pseudo-anaphylactic) reactions (including, but not limited to, anaphylaxis, bronchospasm, hyperemia, rash, hypotension, laryngeal edema and angioedema) can manifest as in patients with hypersensitivity to aspirin, other nonsteroidal anti-inflammatory drugs and intravenous drugs such as ketone in patients without such a history. Such phenomena can also appear in patients with a history of Quincke's edema, bronchospastic reactivity (eg asthma) or nasal polyps. Pseudo-anaphylactic reactions such as anaphylaxis can be fatal. Thus, ketorolac should not be used for patients with a history of asthma, as well as for patients with pronounced or partial nasal polyp syndrome, Quincke's edema and bronchospasm.
Precautions and Impact on Non-Reproductive Function
The use of Ketorolac, as well as other drugs that slow down the synthesis of cyclooxygenase / prostaglandin, can impair reproductive function, as a result of which the drug is not recommended for women trying to get pregnant. Women who have difficulty conceiving or undergoing a study of reproductive function should cancel the use of Ketorolac.
Fluid retention and swelling
It has been reported about fluid retention, hypertension and edema when using ketorolac, and therefore, the drug should be used with caution in patients with heart failure, hypertension or similar conditions.
Drug abuse and dependence
Ketorolac is not addictive. No symptoms associated with the withdrawal of the drug, and after the sudden cessation of intravenous use of ketorolac, were not observed.
Features of the effect of the drug on the ability to drive a vehicle or potentially dangerous mechanisms
Since patients with the appointment of ketorol develop side effects from the central nervous system (dizziness, drowsiness) and from the sensory organs (hearing loss, ringing in the ears, visual impairment), it is recommended to avoid performing work requiring increased attention and quick reaction.
Overdose
Symptoms: abdominal pain, nausea, vomiting, peptic ulcer of the stomach and duodenum, erosive gastritis, impaired renal function, metabolic acidosis. Rarely, but possible gastrointestinal bleeding, acute renal failure.
Ketorol is a non-selective non-steroidal anti-inflammatory drug with pronounced analgesic, antipyretic and anti-inflammatory effects.
The active ingredient, ketorolac, causes (mainly in peripheral tissues) an indiscriminate suppression of the activity of cyclooxygenase enzymes of types 1 and 2. As a result, there is a suppression of the formation of prostaglandins, which play an important role in the appearance of pain, inflammation reactions and the mechanism of thermoregulation.
Ketorol does not affect opioid receptors, does not depress the respiratory center, does not have a sedative and antidepressant effect, and does not cause drug dependence. The analgesic effect is comparable in strength to that of morphine and is much more superior to NSAIDs of other groups.
The onset of the analgesic effect of Ketorol injection (intramuscular injection) or oral administration begins after 0.5 and 1 hour, respectively. The maximum analgesic effect is observed after 1-2 hours.
Indications for use
What does Ketorol help from? According to the instructions, the drug is prescribed in the following cases:
- trauma;
- postoperative and postpartum pain;
- toothache;
- muscle pain;
- joint pain;
- pain caused by malignant tumors;
- neuralgia and sciatica;
- sprains and dislocations;
- pain in rheumatism.
The drug is also prescribed as an adjuvant in inflammatory diseases and elevated body temperature.
Instructions for use Ketorol (injections, tablets and gel), dosages
Intramuscular (intramuscular) and intravenous (intravenous) injections Ketorol are used in the minimum effective doses, selected in accordance with the intensity of pain. If necessary, you can simultaneously prescribe narcotic analgesics in reduced doses.
At the age of 65 years, 10-30 mg of the drug is used intramuscularly once or repeated (every 4-6 hours) injections of Ketorol, 10-30 mg. According to the instructions to patients over 65 years old, as well as in case of impaired renal functions, the drug is prescribed intramuscularly once 10-15 mg or 10-15 mg repeatedly every 4-6 hours, depending on the severity of the pain syndrome.
The maximum allowable dose for patients under 65 years of age is 90 mg / day. In case of impaired renal functions or over 65 years of age, the maximum allowable dose is 60 mg / day.
The course of injections is no more than 5 days.
Transition
On the day of transition from intramuscular injections to tablets, the dose of Ketorol for oral administration should not exceed 30 mg. The daily total dose of tablets and solution when switching from intramuscular administration to oral administration should be no more than 90 mg / day for patients 65 years of age or less, for patients with impaired renal functions or over 65 years of age - 60 mg / day.
Pills
Depending on the severity of the pain syndrome, the tablets can be prescribed once or repeatedly.
The standard single dosage of Ketorol tablets according to the instructions for use is 10 mg (1 tablet), again - 10 mg, up to 4 times a day.
Gel instruction
Ketorol gel should be applied to washed and dried skin. A single dose is a strip 1-2 cm long. The gel is distributed on the surface of the most painful area with gentle massaging movements 3-4 times a day.
Reuse of the gel is possible no earlier than after 4 hours.
It is allowed to use Ketorol gel no more than 4 times a day. Do not exceed the recommended dose.
If, after 10 days of treatment, the patient's condition does not improve or the pain and inflammation increase, it is necessary to stop using the drug and seek medical help.
Side effects
The instruction warns of the possibility of developing the following side effects when prescribing Ketorol:
- stomach pain, vomiting, constipation, flatulence, stomatitis, diarrhea, nausea, heartburn;
- low back pain, acute kidney failure, frequent urination, nephritis (inflammation of the kidneys), decreased or increased volume of urine;
- bronchospasm, laryngeal edema, rhinitis;
- headache, drowsiness, dizziness, hyperactivity, depression, ringing in the ears, hearing loss, blurred vision.
- increased blood pressure, fainting, pulmonary edema;
- leukopenia (an increase in leukocytes in the blood), eosinophilia (an increase in the number of eosinophils), anemia (a decrease in the number of red blood cells or hemoglobin);
- rectal, nasal, postoperative bleeding;
- purpura, skin rash, urticaria, Lyell's syndrome (allergic dermatitis as a reaction to drugs), Stevens-Johnson syndrome (the appearance of blisters on the skin and mucous membranes of various organs);
- itching, hives, discoloration of the face, skin rash, swelling of the eyelids, shortness of breath, wheezing, heaviness in the chest;
- weight gain, swelling of feet, fingers, ankles, legs, face, tongue, excessive sweating, fever;
- pain or burning at the injection site.
Contraindications
It is contraindicated to prescribe Ketorol in the following cases:
- bronchial asthma;
- a history of asthma attacks, bronchospasm, frequent obstructive bronchitis;
- individual intolerance to acetylsalicylic acid or drugs from the group of non-steroidal anti-inflammatory drugs;
- chronic diseases of the gastrointestinal tract with the presence of ulcerative and erosive surfaces;
- gastrointestinal bleeding or suspicion of them;
- ulcerative colitis or Crohn's disease in the acute phase;
- hereditary blood diseases, accompanied by a violation of its coagulation function;
- hyperkalemia;
- severe damage to the liver and kidneys, accompanied by disruption of the work of these organs;
- lactase deficiency;
- patients' age up to 16 years;
- pregnancy and lactation;
Prescribe with caution:
- heart failure;
- arterial hypertension;
- cholestasis;
- cardiac ischemia;
- diabetes;
- the age of patients over 60 years old;
- simultaneous administration of anticoagulants or antiplatelet agents.
Overdose
Manifested by abdominal pain, nausea, vomiting, peptic ulcers of the stomach or erosive gastritis, impaired renal function, hyperventilation.
Analogs Ketorol, price in pharmacies
If necessary, you can replace Ketorol with an analogue according to the therapeutic effect - these are drugs:
- Ketanov;
- Ketonal;
- Adolor;
- Ketokam.
When choosing analogues, it is important to understand that the instructions for the use of Ketorol, the price and reviews for drugs of a similar action do not apply. It is important to consult a doctor and not make your own replacement of the drug.
Price in Russian pharmacies: Ketorol 10mg tablets 20pcs. - from 38 to 49 rubles, solution 30 mg / ml 1 ml 10 pcs. - from 105 to 147 rubles, gel for external use 30g - from 200 rubles, according to 717 pharmacies.
Keep out of the reach of children. Store the drug in a dark, dry place at temperatures up to 25 ° C. Shelf life is 3 years. Sale in pharmacies by prescription.
Ketorol or Ketonal - which is better to choose?
Ketonal is a drug, the main one of which is the NSAID ketoprofen (a propionic acid derivative) and has the same indications for use as Ketorol.
With parenteral administration, the analgesic effect appears after 15-30 minutes. With intravenous infusion of Ketorol, the plasma concentration reaches its maximum values after 4 minutes.
The difference between Ketonal and Ketorol is also a shorter half-elimination period - less than 2 hours.
Studies of the effectiveness of drugs for the pain relief of postoperative patients have shown that Ketorol provides a faster, more effective and lasting effect than Ketonal, and also affects the hemostatic system to a lesser extent.
Interaction with other drugs
With the combined use of probenicid and Ketorol, an increase in the concentration of ketorolac in the blood plasma and an increase in its half-life from the body are noted.
With the combined appointment of methotrexate and Ketorol, it should be noted that NSAIDs reduce the clearance of methotrexate and thereby increase its toxicity. Ketorol does not affect the ability of digoxin to bind to blood plasma proteins. With the combined administration of Ketorol and salicylates (when their concentration in the blood plasma is 300 μg / ml), the binding of Ketorol to blood plasma proteins decreases from 99 to 97%.
Warfarin, paracetamol, phenytoin, ibuprofen, naproxen, piroxicam do not affect the binding of ketorolac to blood plasma proteins.
Clinical trials have not revealed important interactions of Ketorol with warfarin or heparin, but the appointment of ketorolac and drugs that affect hemostasis, including anticoagulants (warfarin or heparin in low doses - 2500-5000 units 2 times a day) and dextrins may increase the risk of occurrence bleeding.
The use of Ketorol tablets after a meal rich in fats may be accompanied by a decrease in the maximum concentration in the blood plasma and a slowdown in its achievement by 1 hour.
Antacids do not affect the absorption of ketorolac in the gastrointestinal tract.
special instructions
With a significantly pronounced pain syndrome or the presence of contraindications for oral administration of the drug, Ketorol is prescribed to the patient in the form of a solution for injection.
When using tablets for more than 5 days, the risk of side effects in the patient increases, therefore, in the absence of the expected therapeutic effect, you should consult a doctor again.
Patients with blood clotting disorders during the period of drug treatment should constantly monitor the level of platelets in the blood, especially in postoperative patients.
To reduce the risk of developing a drug ulcer, the patient can be prescribed antacid or enveloping drugs simultaneously with Ketorol tablets, which will reduce the irritating effect of the main substance of the tablet on the mucous membranes of the digestive tract.
During treatment with the drug, patients should be careful when driving vehicles and operating complex devices that require increased concentration of attention.
Quite often, pain can appear unexpectedly, and if it is of an increasing nature, then this often interferes with the normal activity of a person. One of the universal drugs that helps with pain is Ketorol tablets. After taking it, after 20 minutes, relief comes, and the pain gradually disappears completely.
How Ketorol tablets work
Ketorol not only helps relieve pain, but also relieves inflammation and swelling of soft tissues. This drug belongs to the category anti-inflammatory nonsteroidal drugs and has such an effect on the body:
- relieves inflammation foci;
- relieves acute pain;
- has an antipyretic effect.
Anesthesia with Ketorol is quite strong and in this relation resembles the effect of morphine, but the use of these tablets is more effective and safe. The key active ingredient is ketorolac tromethamine, which has a therapeutic effect even in small doses. This drug helps with different types of pain, differing in the type of manifestation and pathogenesis.
Taking Ketorol tablets has an effect due to the complete absorption of active components in the digestive tract. An hour after taking the drug, the maximum concentration occurs. If a person's diet mainly contains fatty foods, then the absorption process slows down. The decomposition and formation of active metabolites occurs in about 3-4 hours.
Depending on the dosage of the drug, after about half an hour, antipyretic and analgesic effects appear. At the same time, Ketorol is taken in order to get rid of symptomatic pains, and to fully treat a number of diseases in which swelling and fever are observed.
Ketorol tablets and their composition
Ketorol tablets are coated with a soluble green film. They have a biconvex shape that improves the swallowing process. The tablets are equipped with a special S-shaped embossing. Packing of the preparation - 10 pieces in a plastic blister with a metal coating. The number of blisters in the package may be different, the cost of the drug depends on this.
The composition of Ketorol is as follows:
The manufacturer can change the composition of the tablets, but the active ingredient will be the same and present in the amount 10 mg per piece.
Ketorol dosage rules
Ketorol tablets are used when the pain is severe, but not life-threatening. To relieve more severe pain, injections are practiced, they are absorbed faster and reduce the soreness of a particular area.
Tablet dosage depends on factors such as:
- age;
- the intensity of pain;
- features of the course of diseases.
For pain relief, the optimal dosage is 10 mg. In case of severe pain, it can be increased to 2 tablets. If Ketorol is prescribed as a course, then the dosage and duration of treatment are determined on an individual basis.
However, the permissible daily dosage of Ketorol is a maximum of 4 tablets... If it is exceeded, then side effects may appear that negatively affect the course of the disease and complicate it.
Indications for the use of Ketorol
Indications for use of these tablets are as follows:

The course of treatment lasts up to 5 days, but often one dose is enough to get rid of the pain. If you need long-term treatment, then a break is taken every 12 days, then the drug is taken again.
Possible contraindications
Ketorol should not be taken in the following cases:
- the presence of hypersensitivity to the components of the drug;
- bronchial asthma;
- individual intolerance to acetylsalicylic acid;
- age under 16;
- pregnancy and breastfeeding;
- active bleeding in the digestive tract;
- chronic inflammation of the intestines and stomach during exacerbation;
- hemorrhagic diathesis;
- heart failure;
- lactose intolerance;
- renal insufficiency;
- stroke;
- stomach ulcer with exacerbation and other symptoms.
Ketorol is used with extreme caution if the patient has a predisposition to cerebrovascular bleeding and edema... It is also prescribed with caution in the presence of diseases such as:
- chronic hypertension;
- ischemic heart disease;
- hepatitis;
- sepsis and pustular skin lesions;
- disorders of the nervous system and somatic diseases;
- diabetes;
- kidney problems.
Doctors do not advise to combine the reception of funds with alcoholic beverages, as this can provoke intoxication. But other non-steroidal drugs should be eliminated or reduced in number.
Side effects
The following categories are most susceptible to the appearance of side effects:
- people 65 and older with chronic liver disease and ulcers;
- those who have an individual intolerance to the components of the product;
- suffering from cancer.
As for the side effects themselves, they are divided into three subcategories:
- frequent;
- medium frequency;
- rare;
- single.
The first group includes heartburn, strong urination, diarrhea, drowsiness, decreased pressure, swelling of soft tissues and extremities, headache.
Increased sweating, stomatitis, pressure surges, skin rashes, flatulence and constipation are less common.
Very rarely observed:

In some cases, fever, rhinitis, laryngeal edema, nosebleeds and more may appear.
Individual intolerance Ketorol can provoke allergies, which manifest themselves in the form of such phenomena as:
- dry mucous membranes;
- breathing problems;
- itchy skin;
- anaphylaxis;
- swelling.
To identify allergies, the use of tablets must be discontinued and take such measures:
- give an antihistamine;
- drink a lot;
- call emergency help.
If an allergy to a certain drug is diagnosed, then the first admission is carried out in stationary conditions, the dose in this case being an eighth of the daily norm. If there are no side effects, it is gradually increased.
Ketorol is most often well tolerated if the patient does not have serious health problems and does not suffer from chronic diseases. Side effects directly depend on the individual characteristics of the patient, his age and lifestyle.
Overdose manifestations and its elimination
If the overdose was severe, then the body succumbs to severe intoxication, which manifests itself in the form of symptoms such as:

In case of an overdose, you need to take the following measures:
- remove the remnants of the pill from the internal organs, when no more than an hour has passed after taking it, by calling the gag reflex;
- we reduce the concentration of toxins using sorbents (activated carbon, Enterosgel, Sorbex, etc.);
- provide the patient with a water-salt balance - you need to drink at least 2 liters in small sips, but infrequently. For best results, make a saline solution based on salt and soda and sugar. The mixture should be drunk for several days until the side effects disappear entirely.
An overdose may occur even with the usual dose of Ketorol when combined with other non-steroidal drugs or together with intramuscular injections... Be sure to read the instructions and observe the dosage.
Ketorol and other drugs at the same time: how they combine
Taking Ketorol tablets cannot be combined with drugs such as:
- Corticotropins;
- Ethanol;
- acetylsalicylic acid;
- calcium-based vitamins.
All this can provoke profuse bleeding in the digestive tract and other complex diseases.
When combined with paracetamol, methotrexate and gold-based preparations Ketorol provokes the development of nephrotoxicity and other serious problems with the excretory system. And if antihypertensive drugs are combined with Ketorol, their effectiveness is reduced. And if the patient has diabetes mellitus, the insulin dose should be adjusted, because Ketorol affects the level of glucose in the blood and its breakdown.
If it is used together with Nefidipin and Verapamil, then their concentration is greatly increased, which helps in the treatment of myalgias and neuralgias.
What else you need to know about Ketorol
 Ketorol is also not recommended for use for anesthesia for minor surgical operations, it is may cause bleeding it is also better not to use it for chronic pain.
Ketorol is also not recommended for use for anesthesia for minor surgical operations, it is may cause bleeding it is also better not to use it for chronic pain.
Treatment with this drug in the presence of problems in the circulatory system should be carried out with constant monitoring of the condition and number of platelets and the rate of their sedimentation. Analyzes are taken before and after taking the pill.
For cancer, Ketorol can be combined with a small amount of opiates. But it cannot be combined with antineoplastic agents, which provokes kidney problems.
Benefits of Ketorol
Key Benefits Ketorol before other drugs are as follows:
- it is used as a safe pain reliever;
- its use does not in any way affect concentration and performance;
- does not have a pronounced sedative effect;
- not capable of causing addiction;
- you can use Ketorol for violations of hepatic function;
- has no anxiolytic effect;
- affordable cost.
And if we talk about the last advantage of Ketorol tablets, then the drug that is sold in a package with two blisters of 20 tablets is inexpensive - only about 50 rubles, and the domestic analogue will cost even less. In different kits, prices will vary slightly.
It can be concluded that Ketorol pain relievers are excellent in helping to cope with pains of a different nature and more serious syndromes. Along with high efficiency, they are safe and inexpensive.
In this article, you can read the instructions for using the medicinal product. Ketorol... Reviews of website visitors - consumers of this medicine, as well as opinions of doctors of specialists on the use of Ketorol in their practice are presented. A big request to more actively add your reviews about the drug: did the medicine help or did not help get rid of the disease, what complications and side effects were observed that may not have been declared by the manufacturer in the annotation. Analogs of Ketorol in the presence of available structural analogs. Use for the treatment of toothache, headache and other types of pain, during menstruation in adults, children, as well as during pregnancy and lactation.
What is this medicine
Ketorol is a drug used most often for pain relief in patients with severe pain syndrome that has arisen for various reasons. It is used quite widely and for various pathologies.
Drug group
International Non-Proprietary Name or INN: Ketorolac
Trade name: Ketorol
Latin name: Ketorolacum
Composition
Active ingredient: ketorolac trometamol - 0.03 g.
Additional substances: octoxynol - 0.00007 g.
Trilon B - 0.001 g.
sodium chloride - 0.00435 g.
ethanol - 0.115 ml.
propane-1,2-diol - 0.4 g.
caustic soda - 0.000725 g.
water for injection - the volume required to increase the contents of the ampoule to 1 ml.
Mechanism of action and properties
Characteristic
Non-steroidal anti-inflammatory drug or NSAID. Ketorolac in structure consists of two isoforms: S (-) and R (+), it can be in three microcrystalline variants, which have good solubility in water. The dissociation constant of Ketorolac acid is 3.5. Molecule mass: 376.41.
Pharmacodynamics (pharmacology)
Ketorol is an NSAID, acting on the body, suppresses pain, inhibits inflammation, and moderately lowers body temperature.
Mechanism of action
5-Benzoyl-2,3-dihydro-1H-pyrrolysine-1-carboxylic acid non-selectively counteracts the activities of cyclooxygenase-1 and cyclooxygenase-2, which catalyze the synthesis of prostaglandins from arachidonic acid.
Prostaglandins are of great importance in the formation of pain, inflammatory reactions and an excessive increase in the patient's body temperature.
Ketorol is a mixture of almost identical isomers S (-) and R (+), differing only in the mirror arrangement. It is the S form that determines the analgesic effect.
Ketorol, in comparison with morphine, shows the same strong analgesic effect, much more than other NSAIDs.
Pharmacokinetics
The effectiveness of the drug and the speed of its action depend on the method of delivery of the active substance into the body.
With the introduction of a solution of the drug intramuscularly or into a vein, the effect occurs within 30 minutes and reaches its maximum after 60-120 minutes. The duration of the action is from 4 to 6 hours. With enteral administration, the action begins after 60 minutes, and the maximum effect occurs only after 120-180 minutes.
The bioavailability of the drug is fast, it is fully manifested. When the contents of one ampoule (1 ampoule - 30 mg) are injected into the muscle, the highest concentration is from 0.00000174 to 0.0000031 g / ml, with the introduction of two ampoules - from 0.00000323 to 0.00000577 g / ml.
The time to reach the highest concentration is from 15 to 73 for 30 mg and from 30 to 60 minutes for 60 mg.
The share of interaction with blood plasma proteins is 99%.
The drug can pass into breast milk. 2 hours after administration, the concentration of the drug in milk becomes maximum (7.3 ng / ml).
About half of the dose of the drug is converted in the liver into chemically inactive compounds: tetrahydroxy-2-oxanoic acids, which are removed by the kidneys, and p-hydroxyketorolac. It is excreted by the kidneys (about 91%) and through the gastrointestinal tract (6%).
The half-life of Ketorol depends on the age of the patient: in the elderly it increases, in the young it decreases accordingly. In patients with renal disorders, the half-life can be from 10 to 13 hours.
Hemodialysis does not affect the metabolism of the drug. The drug can affect the kidneys and liver.
Indications
What heals, what is it for and what is the use of it? The main use of the drug is pain relief, but it also helps to reduce the temperature, reduce the intensity of inflammation.
Why is Ketorol prescribed? Typically for symptomatic therapy.
Solutions are injected for severe to moderate pain:
- With injuries.
- For dental procedures.
- With tumors.
- To relieve pain after surgery.
- For pain in muscles, joints.
- With damage to peripheral nerves.
- With autoimmune diseases, with radiculopathies.
Drops are used for inflammation of the mucous membrane of the eye and after eye surgery.
The gel is applied topically for injuries:
- With bruises.
- Sprains.
- With tendon inflammation.
- Inflammation of the synovial membranes.
- With inflammatory processes in the joint capsules.
- For pain in muscles, joints.
- With the defeat of nerves remote from the center.
- With autoimmune diseases.
- With radiculopathy.
The tablets are used at the same time as the solutions.

Forms of issue
The drug is produced in the form of four dosage forms: a solution for infusion and injection (intramuscularly or intravenously) in a 1 ml ampoule, in the form of tablets, outside of which there is a film shell, in the form of a gel for external use and in the form of eye drops.
What is better solution or tablets? The tablets are easier to use, but the solution is faster and more effective. The gel is applied only externally, for example, for soft tissue bruises.
Instructions for use
When administered parenterally to patients from 16 to 64 years old with a body weight of more than 50 kg, more than 60 mg cannot be injected into the muscle at the same time (it is also necessary to take into account the dose of the drug taken orally). Most often - 30 mg every 6 hours. Intravenous 30 mg is injected, no more than 6 doses in 28 hours.
If the patient weighs less than 50 kg or has renal pathology, then no more than 30 mg is injected into the muscle at a time, usually 15 mg (no more than 8 times in 48 hours), no more than 15 mg is injected into the vein (less than 8 times).
The maximum dose administered per day for patients from 16 to 64 years old and weighing more than 50 kg is 0.09 g (90 mg), for the rest - 0.06 g (60 mg). The duration of use is up to two days.
The drug must be injected slowly into a vein or muscle. The effect begins in 0.5 hours.
The gel must be spread in a thin layer over the disturbing surface.
The tablets must be taken with a sufficient amount of water.
Side effect
- Dysfunction of the gastrointestinal tract: diarrhea, nausea, vomiting, constipation, abdominal pain, peptic ulcer of the stomach or duodenum, bleeding in the stomach cavity, inflammatory liver disease, Gospel disease caused by bile congestion, acute inflammation of the pancreas, enlargement of the liver, perforation of the stomach wall ...
- Renal dysfunction: pain in the lumbar region, blood or high nitrogen in the urine, hemolytic uremic syndrome, pollakiuria, kidney inflammation, renal edema.
- Visual impairment, hearing loss.
- Convulsive contraction of the smooth muscles of the bronchi, inflammation of the mucous layer of the nasal cavity, laryngeal edema.
- Headache, aseptic inflammation of the meninges, fever, weakness of the muscles in the neck or back, muscle spasm, impaired mental activity, increased activity, feelings of melancholy, hallucinations.
- Hypertension, acute pulmonary failure, loss of consciousness.
- Decreased blood hemoglobin levels, increased eosinophil levels, and / or decreased leukocyte counts.
- Bleeding from the nasal cavity, bleeding during operations.
- Urticaria, purpura, inflammatory skin inflammation, effusion erythema, bullous inflammation of the dermis.
- Burning sensation when applied topically, pain along the vein when administered intravenously.
- Anaphylactic reactions, pruritus, shortness of breath, hyperemia, Quincke's edema.
- Increased sweating, weight gain, increased body temperature.
Contraindications
- Intolerance to the drug.
- Information on hypersensitivity reactions when taking NSAIDs in history.
- Inflammatory diseases of the mucous layer of the nasal cavity.
- Bronchial asthma.
- Insufficient circulating blood volume.
- Ulceration of the stomach or duodenum.
- Violations of hemostasis.
- Inflammation of the intestines.
- Hepatic dysfunction.
- Renal dysfunctions.
- Insufficient or excessive levels of potassium in the blood.
- Exacerbation of heart failure.
- Premedication in the preoperative and operational period.
- Simultaneous reception with drugs that affect blood clotting.
- Age under 16.
- Dermatitis.
- Simultaneous use with probenecid and pentoxifylline.
- Pregnancy.
- Lactation.
Application in children
The drug is contraindicated in persons under the age of 16.
Application during pregnancy and lactation
The drug is prohibited during pregnancy and lactation. It can reduce the contractile activity of the uterus, affect the formation of the circulatory system of the fetus. In infants, inhibition of prostaglandins can be detrimental.

Elderly use
In pensioners, the risk of side effects is increased; it is necessary to use the drug with caution.
Driving a car and other mechanisms
Due to the high incidence of adverse reactions, activities that require increased attention are not recommended.
Do I need a prescription
Ketorol is sold by prescription.
Compatibility with other medications
In case of drug interaction with other drugs, Ketorol may have an adverse effect. Simultaneous use with other NSAIDs, ethyl alcohol or alcohol, glucocorticosteroids, anticoagulants, calcium preparations can cause an ulcerogenic effect and bleeding.
It is impossible to prescribe Ketorol with paracetamol for a period of more than 2 days, since when taken simultaneously with paracetamol, toxicity to the kidneys increases, with methotrexate, toxicity to both the kidneys and the liver.
If narcotic analgesics are used together with Ketorol, their dosage can be reduced.
Due to a decrease in prostaglandins in the kidneys, the effectiveness of diuretics and drugs that lower blood pressure decreases.
Antacids have no effect on the absorption of the drug.
When used with hypoglycemic drugs, it increases their effect.
Increases the dose of verapamil and nifedipine in the blood.
Alcohol compatibility
When taken with alcohol, it can cause inflammation of the mucous membrane of the stomach and duodenum. Subsequently, ulcers may form in the gastrointestinal tract, so compatibility with alcohol is dangerous.
Analogs of the drug Ketorol
Structural analogues for the active substance:
- Adolor;
- Akular LS;
- Dolak;
- Dolomin;
- Ketalgin;
- Ketanov;
- Ketolac;
- Ketorolac;
- Ketofril;
- Toradol;
- Torolac.
In the absence of analogues of the drug for the active substance, you can follow the links below to the diseases for which the corresponding drug helps, and see the available analogues for the therapeutic effect.
Composition
Each ampoule contains ketorolac tromethamine 30 mg, as well as excipients: ethyl alcohol 95% 0.125 ml, sodium chloride 4.35 mg, disodium EDTA 1.0 mg, octoxynol 0.07 mg, sodium hydroxide 0.725 mg, propylene glycol 400 mg, water for injection up to 1 ml
Pharmacotherapeutic group
Non-steroidal anti-inflammatory and antirheumatic drugs. ATX code: M01 AB15.
Description
Clear, colorless or pale yellow liquid, in yellow ampoules, 1 ml, USP 1 type.
Pharmacological properties
Pharmacodynamics: ketorolac, being a non-steroidal anti-inflammatory drug, has an analgesic, antipyretic and anti-inflammatory effect. The mechanism of action at the biochemical level is inhibition of the cyclooxygenase enzyme mainly in peripheral tissues, which results in inhibition of the biosynthesis of prostaglandins - modulators of pain sensitivity, thermoregulation and inflammation. Ketorolac is a racemic mixture of [-] S and [-] P enantiomers, with the analgesic effect due to the [-] S form. The drug does not affect opioid receptors, does not depress respiration, does not suppress intestinal motility, does not have sedative and anxiolytic effects, does not cause drug dependence, does not affect the progression of the disease. Ketorolac inhibits platelet aggregation and increases bleeding time. The functional state of platelets is restored within 24-48 hours after discontinuation of the drug.
Pharmacokinetics: the bioavailability of ketorolac after oral administration ranges from 80% to 100%. The maximum plasma concentration is reached within 30-60 minutes. The pharmacokinetics of ketorolac in terms of the appointment of average therapeutic doses is a linear function. The equilibrium concentration of the drug in plasma is 50% higher than that determined after a single dose. More than 99% of the drug binds to blood plasma proteins, as a result, the apparent volume of distribution is less than 0.3 l / kg.
Ketorolac is metabolized mainly with the formation of conjugated forms of glucuronic acid, which are excreted through the kidneys. Metabolites have no analgesic activity. The half-life of the drug is 5 hours on average.
Indications for use
Short-term relief of moderate and severe acute pain in the postoperative period. Treatment should be started only in a hospital setting, the maximum duration of treatment is 2 days.
Method of administration and dosage
Ketorol is intended for intramuscular injection; the drug should not be used for epidural or spinal administration. The solution is injected slowly intramuscularly (deep into the muscle). The onset of the analgesic effect is about 30 minutes with its maximum severity within 1-2 hours, the average duration of analgesia is 4-6 hours.
The introduction of the drug several times a day for more than 2 days is not recommended, since in most cases patients do not need more prolonged analgesic therapy, or they can be switched to oral ketorolac. In this case, the duration of parenteral and oral administration of ketorolac should not exceed 5 days in total.
To achieve the maximum analgesic effect in the early postoperative period, it is possible to use ketorolac and narcotic analgesics together, the daily dose of the latter in this case is reduced. Ketorolac does not affect opioid addiction and does not increase the associated respiratory depression or sedation.
The selection and adjustment of the dose should be made in accordance with the intensity of the pain and the response to the administration of the drug. To minimize side effects, it is recommended to use the minimum effective dose for the shortest possible course of treatment.
Adults; the usual recommended starting dose of Ketorol is 10 mg, followed by 10-30 mg every 4-6 hours. In the early postoperative period, it is permissible to administer the drug every 2 hours, if necessary. The maximum daily dose is 90 mg / day. in patients weighing less than 50 kg - no more than 60 mg / day.
Elderly patients (over 65): it is recommended to use the drug in the lowest effective dose, the total dose should not exceed 60 mg / day. Due to the higher risk of side effects in this group of patients, the minimum possible duration of treatment is recommended, regular monitoring of the patient's condition to exclude gastrointestinal bleeding. Children: the safety and efficacy of ketorolac in children has not been confirmed, the drug is not recommended for use in children under 16 years of age.
Patients with impaired renal function: the use of ketorolac is contraindicated in patients with severe and moderate renal impairment. In the case of mild renal dysfunctions, it is permissible to use Ketorol at a dose of no more than 60 mg / day.
If a joint parenteral and oral administration of Ketorol is necessary, the total daily dose should not exceed 90 mg (60 mg in persons over 65 years of age, weighing less than 50 kg or impaired renal function), while the dose of the drug taken orally should not exceed 40 mg / days The prompt transfer of the patient to the oral form of the drug only is recommended.
Side effect
From the gastrointestinal tract: anorexia, abdominal discomfort, stomach fullness, nausea, dyspepsia, gastrointestinal pain, epigastric pain, diarrhea, flatulence, belching, vomiting, constipation, erosive and ulcerative changes, bleeding and perforation of the gastrointestinal tract (sometimes fatal) , vomiting of blood, blood in the stool, gastritis, peptic ulcer, pancreatitis, ulcerative stomatitis, esophargitis, exacerbation of Crohn's disease and colitis.
From the liver and biliary tract: liver dysfunction, liver failure, jaundice, hepatitis, hepatomegaly, increased activity of hepatic transaminases.
From the nervous system: headache, dizziness, fainting, fatigue, weakness, irritability, dry mouth, increased thirst, mood changes, anxiety, impaired concentration, euphoria, nervousness, confusion, paresthesias, unusual dreams, depression, drowsiness, disturbance sleep, insomnia, hallucinations, agitation, hyperkinesia, convulsions, pathological thoughts, aseptic meningitis, stiff neck muscles, anxiety, vertigo, disorientation, thought disorder.
From the senses: violation of taste, blurred vision, optic neuritis, tinnitus, hearing loss and hearing loss.
From the side of the musculoskeletal system: myalgia.
From the sideurinarysystems: pain at the site of renal projection, dysuria, frequent urination, oliguria, hematuria, proteinuria, increased serum urea and creatinine levels, hyponatremia, hyperkalemia, urinary retention, renal failure, interstitial nephritis, papillary necrosis, nephrotic syndrome, hemolytic uremic syndrome.
On the part of the cardiovascular system: pallor, hyperemia, chest pain, palpitations, bradycardia, heart failure, arterial hypertension, edema. Data from clinical and epidemiological studies indicate that the use of some NSAIDs, especially in high doses and for a long time, may be associated with an increased risk of arterial thromboembolic complications (myocardial infarction or stroke).
From the side blood: purpura, leukopenia, eosinophilia, neutropenia, agranulocytosis, aplastic anemia, hemolytic anemia, thrombocytopenia, a decrease in the rate of blood clotting, the occurrence of hemorrhages under the skin, hematomas, nosebleeds, prolonged bleeding time, increased bleeding of postoperative wounds.
From the respiratory system: shortness of breath, tachypnea, bronchospasm, complication of asthma, pulmonary edema.
On the part of the reproductive system: infertility (in women).
On the part of the skin: itching, urticaria, photosensitivity, Lyell's syndrome, exfoliative dermatitis, toxic epidermal necrolysis, erythema multiforme, Stevens-Johnson syndrome, skin rashes, including maculopapular and weeping, discoloration of the face.
Allergic reactions: anaphylactic and anaphylactoid reactions, urticaria, bronchospasm, laryngeal edema, angioedema, eyelid edema, periorbital edema, exfoliative dermatitis, bullous dermatosis.
From the side of the body as a whole: general malaise, swelling, fever, excessive sweating, weight gain; pain, swelling and hyperemia at the injection site. To prevent possible side effects, one should strive to use the minimum effective dose of the drug, strictly observe the established dosages and modes of administration, take into account the patient's condition (age, concomitant diseases, liver and kidney function, the state of water and electrolyte metabolism and the hemostatic system), as well as possible drug interactions with combination therapy.
Contraindications
Bronchial asthma, Complete or partial nasal polyp syndrome, bronchospasm, history of angioedema. Peptic ulcer of the stomach and duodenum during an exacerbation, as well as a history of ulcers or gastrointestinal bleeding, the presence or suspicion of gastrointestinal bleeding. History of blood clotting disorders, conditions with a high risk of bleeding, hemorrhagic diathesis, coagulopathy, hemorrhagic stroke, intracranial bleeding, simultaneous use with anticoagulants (including warfarin, low doses of heparin). Surgical interventions with a high risk of bleeding or the risk of incomplete stopping it. Moderate and severe renal failure (plasma creatinine more than 50 mg / l), risk of renal failure, hypovolemia, dehydration. Pregnancy, labor and lactation. Hypersensitivity to ketorolac, aspirin, other NSAIDs or any component of the drug. Concomitant use of other NSAIDs (risk of summation of side effects) Age up to 16 years Congestive heart failure The drug is not used for pain relief before and during surgery. Ketorolac is not used for epidural and intrathecal administrations. Severe liver failure. Combined use with lithium preparations, pentoxifylline probenecid. Epidural or intrathecal administration of the drug is contraindicated.
Application features
Prescribing to patients with impaired function liver: appointed with caution. While taking ketorolac, the level of liver enzymes may increase. In the presence of functional abnormalities in the liver while taking ketorolac, a more severe pathology may develop. If signs of liver pathology are detected, treatment should be discontinued.
Patients with renal failure or a history of kidney disease: Ketorolac is prescribed with caution.
Appointment elderly patients: since patients in this age group develop adverse reactions more often, the minimum effective dose should be used (daily therapeutic dose of not more than 60 mg for patients over 65 years of age).
Pregnancy and lactation
Efficacy and safety have not been established. Drugs that affect the synthesis of prostaglandins, including ketorolac, can cause a decrease in fertility, and therefore are not recommended for use by women planning pregnancy. The safety of the drug in pregnant women has not been studied. When studied on rats and rabbits in toxic doses, no teratogenic effect was revealed. In rats, an extension of gestational age and a delay in labor were noted. Due to the known negative effect of drugs of the NSAID group on the cardiovascular system of the fetus (risk of clogging of the ductus arteriosus), ketorolac is contraindicated in pregnant women. The use of ketorolac during labor is not recommended due to the increased risk of bleeding in the mother and baby. Ketorolac penetrates into milk, and therefore is not recommended for use during lactation.
Influence on the indicators of laboratory tests: an increase in bleeding time is possible in the study of clotting indicators.
Impact on the ability to drive transportand other mechanisms
Since a significant part of patients, when prescribing ketorolac, develop side effects from the central nervous system (drowsiness, dizziness, headache), it is recommended to avoid performing work that requires increased attention and a quick reaction.
Warnings and Precautions
Ketorolac is capable of causing severe adverse reactions from the digestive tract at any stage of drug therapy, after or without precursor symptoms; such adverse reactions can be fatal. The risk of serious gastrointestinal bleeding is dose dependent, but side effects can occur even with short therapy. In addition to having a history of peptic ulcer disease, provoking factors are the simultaneous use of oral corticosteroids, anticoagulants, long-term therapy with non-steroidal anti-inflammatory drugs, smoking, drinking alcoholic beverages, old age. If you suspect the development of adverse reactions from the gastrointestinal tract, ketorolac should be canceled.
NSAIDs should be used with caution in patients with Crohn's disease and a history of ulcerative colitis due to the possibility of worsening the course of the disease.
Ketorolac inhibits platelet aggregation and lengthens bleeding time, platelet function returns to normal within 24-48 hours after drug withdrawal. In patients receiving anticoagulant therapy, the use of ketorolac may increase the risk of bleeding. Patients who are already taking anticoagulants or requiring low-dose heparin should not receive ketorolac. In patients taking other drugs that affect hemostasis, ketorolac should be used with caution. In patients who underwent surgery with a high risk of bleeding or incomplete hemostasis, ketorolac should not be used.
Like other NSAIDs, ketorolac inhibits the synthesis of prostaglandins and can have toxic effects on the kidneys, so it should be used with caution in patients with impaired renal function or with a history of kidney disease. The risk group includes patients with impaired renal function, hypovolemia, heart failure, impaired liver function, patients who use diuretics, and elderly patients.
Fluid retention, sodium chloride, hypertension, oliguria and peripheral edema have been observed in some patients taking NSAIDs, including ketorolac, so it should be used with caution in patients with hypertension, heart failure, before administration of the drug, violations of the water-electrolyte balance should be corrected.
Clinical studies and epidemiological data indicate that the use of some NSAIDs, especially in high doses and for a long time, may be associated with an increased risk of arterial thrombotic complications such as myocardial infarction or stroke. This risk cannot be excluded for ketorolac. To minimize the potential risk of developing side cardiovascular complications in patients using NSAIDs, the minimum effective dose should be used for the shortest possible period of time. Ketorolac should be prescribed to patients with uncontrolled hypertension, congestive heart failure, established coronary heart disease, peripheral arterial and / or cerebrovascular disease only after a careful assessment of all the advantages and disadvantages of such treatment.
Ketorolac should be used with caution in patients with impaired liver function or a history of liver disease. Significant increases (more than three times higher than normal) in serum ALT and ACT were observed in controlled clinical trials in less than 1% of patients. In addition, isolated cases of severe hepatic reactions have been reported, including jaundice, fulminant hepatitis, liver necrosis and liver failure, in some cases leading to death. If signs of liver dysfunction appear, ketorolac should be canceled.
The use of the drug in patients with systemic lupus erythematosus or connective tissue diseases may be associated with an increased risk of developing aseptic meningitis.
Serious skin reactions have been reported such as exfoliative dermatitis, Stevens-Johnson syndrome, and toxic epidermal necrolysis. The risk of these reactions is highest at the beginning of treatment.
The development of serious anaphylactic and anaphylactoid reactions, such as bronchospasm, laryngeal edema, angioedema, anaphylactic shock, has been reported. Ketorolac should not be used in patients with bronchial asthma, nasal polyp syndrome, bronchospasm, a history of angioedema. If a rash or other manifestations of hypersensitivity occurs, treatment with the drug should be discontinued.
This medicinal product contains a small amount of ethanol (ethyl alcohol), i.e. less than 100 mg in 1 ml sodium content in the drug is less than 1 mmol (23 mg) in 1 ml.
Interaction with other medicinal products
Ketorolac slightly reduces the degree of binding to warfarin proteins.
In research in vitro shows the effect of therapeutic doses of salicylates on the degree of binding of ketorolac to plasma proteins downward from 99.2% to 97.5%. When combined with furosemide, its diuretic effect may be weakened by about 20%.
Probenecid reduces plasma clearance and the volume of distribution of ketorolac increases its concentration in blood plasma and increases its half-life. Against the background of the use of ketorolac, it is possible to reduce the clearance of methotrexate and lithium and increase the toxicity of these substances.
Possible interaction between ketorolac and non-depolarizing muscle relaxants, leading to the development of apnea, was noted.
It is possible that the simultaneous use with ACE inhibitors may increase the risk of renal dysfunction.
Rare cases of the development of seizures are described when ketorolac is combined with anticonvulsants (phenytoin, carbamazepine).
Hallucinations may occur while taking ketorolac and psychostimulating drugs (fluoxetine, thiothixene, alprazolam).
The simultaneous use of ketorolac and NSAIDs, including selective cyclooxygenase-2 inhibitors, should be avoided due to the increased risk of serious adverse reactions. Ketorolac inhibits platelet aggregation, reduces thromboxane concentration and prolongs bleeding time. Platelet function returns to normal within 24-48 hours after stopping ketorolac. Although studies do not indicate a significant interaction between ketorolac and anticoagulants, the simultaneous use of ketorolac and therapeutic doses of warfarin, prophylactic doses of heparin (2500-5000 units over 12 hours) and dextrans may be associated with an increased risk of bleeding.
NSAIDs should not be used within 8-12 days of mifepristone administration due to the potential reduction in the effect of mifepristone.
The simultaneous use of ketorolac with pentoxifylline increases the risk of bleeding.
As with other NSAIDs, caution should be exercised when co-administered with corticosteroids due to the increased risk of gastrointestinal symptoms or bleeding.
Ketorolac has been shown to reduce the need for opioid analgesics when used to relieve postoperative pain.
Patients who are concomitantly taking quinolines may have an increased risk of seizures.
The simultaneous use of NSAIDs with zidovudine leads to an increased risk of hematological toxicity.
There is an increased risk of nephrotoxicity when NSAIDs are used together with tacrolimus or cyclosporine.
NSAIDs can worsen the course of heart failure, reduce the glomerular filtration rate and increase plasma levels of cardiac glycosides when used together.
Incompatibility
Ketorolac solution for injection should not be mixed in small containers (for example, in one syringe) with morphine sulfate, meperidine hydrochloride, promethazine hydrochloride or hydroxyzine hydrochloride, as this can precipitate ketorolac.
Overdose
An overdose of ketorolac with a single or repeated use is usually manifested by pain in the abdomen, the occurrence of peptic ulcers of the stomach or erosive gastritis, impaired renal function, hyperventilation, metabolic acidosis, these symptoms are cured after stopping the drug. In these cases, gastric lavage, the introduction of adsorbents (activated carbon) and symptomatic therapy are recommended. Ketorolac is not sufficiently excreted by dialysis.
Manufactured
"Dr. Reddy's Laboratories Ltd"
Village Khol, Nalagarh Road, Buddy, Solan District, Himachal Pradesh, 173205, India.