Preparations thrush is afraid of antifungal. Funds from thrush - inexpensive and efficient. Tablets from candidiasis for men
Candidiasis is a fungal disease, predominantly affecting the skin and mucous membranes, less often internal organs. Candidiasis of respiratory, digestive, urogenital systems distinguish. With a sharp weakening of immunity, generalized candidiasis (candidal septis) can develop. Men's urogenital candidiasis is manifested by the inflammation of the penis (redness, swelling, coating with a grayish flare and erosions, itching, burning and pain in the field of penis head). Candidal urethritis and cystitis are possible. Women have defeat outdoor genital organs and vagina. Without timely treatment, candidiasis takes a chronic recurrent course.
Urogenital candidiasis is caused by yeast-like fungi of the genus Candida (Candida), representatives of the normal microflora of the mucous membranes of the genital organs. The development of the candidiasis occurs as a result of intensive reproduction of candidate candidates and violations of the natural balance of the urinary tract. The development of candidias to a considerable degree contributes to the overall decrease in the body's resistance.
Genital candidiasis is not threatening the health and life of the disease, but it is extremely unpleasant with its manifestations, leading to violations in the intimate and psycho-emotional spheres. In addition, the presence of candidiasis can talk about severe concomitant pathology (diabetes mellitus, HIV infection, etc.).
Candidiasis of genital organs or, so-called thrush, affects the mucous membranes of the urogenital tract of men and women, being in essence of sexual infection.
Often, the milk is accompanied by other diseases with sexual transmission: chlamydia, gonorrhea, trichomonosis, etc.
The sharp and subacute current of the candidosis lasts no more than 2 months. During this period, swelling, hyperemia, selection of sex tract and other inflammatory symptoms are pronounced. Chronic forms of candidiasis are characterized by the limitation of current over 2 months. On the mucous membranes, foci of dryness, hyperpigmentation, infiltration, tissue atrophy are developing.
Recently, atypical, erased and resistant to the treatment of the shape of the urinary candidiasis have become often stable.
Tablets Futsis
Fudiis tablets - antifungal preparation of a wide range of action. Fluconazole - the active substance of the drug is a synthetic derivative of a group of thiazolic compounds. Fluconazole, due to the election influence on ...
Tablets Rumikosis

Tablets Rumicosis - antifungal preparation of a wide range of action. Rumicosis contains an active component of itraconazole - the medicinal substance derivative of triazole. Itraconazole inhibits Ergosterol formation, which is ...
Tablets Irununin

Irunun Tablets inhibits (violates) Ergosterol synthesis, which is an important component of the cell membrane of fungi, which causes the antifungal effect of the drug ...
Pimafucin tablets

Pimafucine tablets belong to the pharmacological group of medicines antifungal drugs. They are used with a mushroom intestinal infection caused by fungi genus ...
Tablets Flucostat

Antifungal medicinal pills Flucostate contains an active component of fluconazole - a drug substance, a derivative of triazole. The mechanism of action of tablets Flucostat is based on its ...
Tablets Mikosist

Tablets Mikosist - antifungal drug related to the group of triazoles. Antifungal effect is carried out by violation of ergosterol synthesis, which is necessary for construction ...
Tablets Terezhinan

Tablets Terezhinin complex antibacterial and antifungal drug for therapy of gynecological diseases. Terenidazole is active against anaerobic flora, including Gardnerners, also has ...
Tablets Clion-D

Clion-D tablets are antiprotozoic, antibacterial, antifungal. The mechanism of the action of metronidazole is to biochemical reduction of the 5-nitro-group intracellular transport proteins ...
Tablets Oricanal

The neungal tablets are used to treat various fungal infections. It is a synthetic antifungal agent of a wide range of action. Active substance...
Diflucan tablets

The active substance of the diflyucan tablets is fluconazole - has a property to effectively suppress synthesis of sterols in mushroom cells. The effectiveness of the dieflucan is proved against yeast and ...
The development of candidias of the genital organs
According to the tests conducted in the field of venererology, the following factors are most often the development of the candidosis of the genital organs:
- reception of antibacterial and row of hormonal drugs;
- pregnancy;
- candidiasis (dysbacteriosis) of the intestine;
- diabetes;
- HIV and other infections that overwhelming the immune system;
- excessive douching;
- wearing synthetic and cramped linen;
- long adverse effects of physical factors (work in warm wet premises, etc.).
Candidian manifestations in women
Gilband Candidiasis is more common among women. About 75% of women at least once in their lives came across the manifestations of the vulvovaginal candidiasis, and in half of them the disease was recurrent.
In women, candidiasis of the urinary tract is characterized by the lesion of the mucous membranes and vagina, less often - the cervix, urethra and bladder.
Candidoid vulvit and vulvoginitis that does not affect urinary paths have the following manifestations:
- abundant, dairy-white and cotton consistency of the discharge from the vagina with an unpleasant odor;
- feeling of irritation, itching or burning or in the field of vulva, amplifying after urination, during sleep or after taking a bath;
- the soreness of sexual interchanges, strengthening the symptoms of irritation and characteristic unpleasant odor after sexual intercourse.
Under candidal vulvite, yeast-like fungi areas of external genital organs are damaged: the clitoris, small and large sexual lips, the anticipation of the vagina. Candidiasis of vulva can flow in typical and atypical clinical forms:
Typical forms of candidiasis, vulva include:
- catarial membrane vulvit of acute and subacute flow;
- catarial chronic vulvit.
Among the atypical forms of candidiasis, the vulva is distinguished
- leukoplakia chronic vulvit;
- corrosion like chronic vulvit;
- asymptomic barginic chronic vulvit;
Also there are often mixed variants of acute fungal infections: candidiasis - bacterial, candidadeous - chlamydial, candidiasis - gonorrheal, candidiasis - trichomonaceous vulvits.
The course of typical forms of candidosis of vulva is characterized by burning and itching, the intensity of which is enhanced before menstruation and decreases or disappears into menstrual and postmenstrual periods.
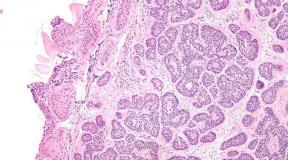
The mucous membranes affected by candidiasis are hyperemic, have a crimson-blue tint. On the mucous, fine-point bubbles are visible, which, when opening, extensive erosion is formed. Small sex lips are covered with layers in the form of white curl films.
In the chronic form of candidiasis, the vulva notes stagnant hyperemia and tissue infiltration, their thickening and increased dryness.
The atypical Candidosis of Vulva is rare and proceeds in chronic form.
From the mucous membranes of vulva, candidiasis can spread to the inguinal femoral folds and the perianal area. Such manifestations are usually observed in chronic candidiasis in patients with micasest, diabetes mellitus, ovarian hypofunction.
For candidal vaginitis, the spread of fungal lesion on the mucous membranes of the vagina and often the vaginal part of the cervix is \u200b\u200boften.
Candidiasis of the vagina proceeds in four basic forms:
- candidial catarrhae-exudative-membrane vaginitis of acute and subacute;
- mixed candidal-bacterial catarrhal-exudative vaginitis of acute and subacute flow;
- candidal catarrhal subacute and chronic vaginitis;
- asymptomic candidal chronic vaginitis.
With the candidiasis of the vagina, the mucous membranes are brightly hyperemic, coated with a sour cream or loose rippled. Walls and vaginal arches, as well as the vaginal part of the cervix erozed. Allocations of abundant, cotton or cream-like consistency, sometimes a foam and even purulent character with an unpleasant smell. Subjectively patients celebrate moderate pain, burning and itching in the vagina.
Candadose endocervicitis is not found independently, but develops only due to vaginal candidiasis.
As a result of the candidiasis of the vagina, the fungal infection in the upward way penetrates through the outer zev in the cervical channel. Often the cause of the development of candidal endocervicitis is the defective ovarian function. In the typical course of the cervical cervical cervical channel, white riveted lumps or white thick mucus are highlighted from the cervical canal. Outside the surface of the cervix is \u200b\u200bcovered with blessed films. The erased form of the cervical cervical shape is characterized by a scant milk-mucous separated.
Comparatively rare manifestations of the urinary candidiasis in women are candidal urethritis and cystitis. Acute candidial urethritis is characterized by constant stupid pains at the bottom of the abdomen and dysuric disorders: hazard, burning, rapid and painful urination. In viewing, there is a swelling and hyperemia of urethra sponges, cotton lumps at the outer opening of the urethra.
Acute cystitis in candidiasis is manifested by pain in urination and frequent false urges.
Chronic candidal urethritis and cystitis outside exacerbations flow with erased symptoms or without it.
Manifestations of candidiasis in men
Greeting candidiasis in men is often manifested in the form of balanitis - inflammation of the head of the penis or post - inflammation of the internal leaflet of the extreme flesh, or in their combination.
Candidial balanopostitis refers to sexually transmitted infections. Its growth is associated with the prevalence of the urinary candidiasis in women due to the use of hormonal contraceptives, antibacterial and counter-syrchrometry.
The clinical picture of candidomic balanopostitis depends on the shape of its flow: membrane, erosive or erytherto-pustular. Subjectively, it is usually noted itching and a burning mind of a penis. The skin in the field of the penis head, theft groove, as well as an inner leaf of the extreme flesh hyperemic, edema and are inflamed, covered with a blessed-gray rode. Extreme flesh infiltration makes it difficult to expose the head. The head of the penis can erose and mock, which makes it easier to attach the secondary purulent infection. With candidal beamopostitis, symptoms of urination disorder are absent.
The chronic flow of candidomic balanopostitis may be complicated by phimosis due to the gradual rupture narrowing of the extreme flesh. Among other complications of candidomic balanopostitis there are lymphadenitis, lymphangitis, silent inflammation of the penis, candygranhelm, warthogs, carcinoma of the penis.
The urethra in Candidiasis in men is amazed less often, and usually candidalosic urethritis occurs in a subacute form. The incubation period is from 2 weeks to 2 months. Candidiasis of the urethra is accompanied by a light itch and a feeling of burning, usually scarce, mucous-watery, less often - abundant and purulent discharge from the urethra. With a urestroscopic study, a whisen flare is noted in the form on the mucous membrane of the urethra. The removal of the beacon is accompanied by the exposure of the edema and sharply hyperemic urethra mucosa.
Complications of candidiasis of urethra often serve prostatitis, cystitis, epididimitis.
Generalized form of Kandidoza
In particularly unfavorable cases, the pathological process can capture many bodies with the development of the generalized form of candidiasis. The risk factors in the development of candidosis generalization are the presence, the use of glucocorticoids and antibiotics, artificial nutrition, chemotherapy, drug addiction, surgical operations and the postoperative period, etc. The generalized candidiasis proceeds with severe fever, reactions from the central nervous system, disorders of the gastrointestinal tract, Changes in peripheral blood indicators (leukocytosis, neutrophilee with a shift to the left), homoeostasis disorders.
Diagnosis of genital candidiasis
In the event of symptoms of candidias, men usually turn to an urologist, and women come to consult a gynecologist. The diagnosis of urinary candidiasis is carried out on the basis of complaints and inspection of the mucous membranes of the genital organs. The diagram diagnosis is confirmed by the study of the discharge vagina or penis by the method of light microscopy, bakpospose, and the dedication of the sensitivity of the selected varieties of Candida to antifungal drugs.
Consultation of venereologist is necessary for the behavior of the differential diagnosis of candidiasis with trichomoniasis, gonorrhea, gardnerellosis, other urogenital infections and exclusion of accompanying STIs.
Under the candidiasis of the genital organs it is necessary to eliminate the presence of chronic diseases of the body, to assess the state of immunity.
Diagnosis of candidiasis does not require the use of high-precision laboratory techniques, such as FIF or PCR, detecting even single pathogens. The criterion for the diagnosis of the diagnosis of urogenital organs is the identification of the fact of intensive reproduction of fungal pathogens.
Candidose treatment of genital organs
For the treatment of urinary candidiasis, events are carried out both local and general. The choice of the therapy method is determined by the severity of the flow of the candidiasis. The light shapes of the candidiasis of the genital organs are usually treated with the use of local drugs, while heavy forms suggest additional use of overall preparations.
Local Candidian therapy is carried out by vaginal candles and tablets, ointments containing antifungal drugs: Nystatin (Polizinaks, Terezhin), Clotrimazole (Candibane, Caurent, Antifungal, Kanizon), Pimafucin (Natamicin), Mikonazole (Ginezol 7, Clion-D 100, Gino Daktarine), ketoconazole (nipped).
Common preparations for the treatment of candidiasis are accepted inside. For this purpose, fluconazole is prescribed (diphlacan, diphulason, flukostat, microsist), itraconazole (neungal).
The side effects of the majority of these drugs for the treatment of candidiasis are the suppression of normal microflora of the genital organs, especially the lactobacilli, in the normal place to exclude the growth of pathogenic microorganisms. To restore the normal balance of the microflora of the genital organs, after the course of antifungal therapy of the candidiasis, eubiotics are prescribed, including lactobacilli (lactobacterin), or the injection of salicotrichovaka - a drug containing inactivated lactobacillic versions.
Since candidiasis strikes not only the genital organs, but also the intestine, in its treatment, the vitamins of the group B, the synthesis of which is broken under the intestinal dysbiosis are applied. Also justified when candidiasis, the appointment of polyvitamins ("Vitrum", Duovo "Multitabs", etc.).
The simultaneous treatment of the urinary candidide is carried out by all patient's partners.
Among the conditions provoking pathogenic are developed - immune failure, pregnancy, long-term intake of antibiotics and other drugs, mechanical injuries.
Most often, the culprit of the candidiasis is the candida albicans fungus, and although some physicians do not consider it deadly for a person to get rid of it. At least for the reason that candidiasis turns everyday life into a nightmare: it worries unbearable itching and peeling, there are edema of mucous membranes, purulent inflammation, etc.
Autoinfection (because the source of infection - its own microflora) can last for years, then exacerbated, then athighted, gradually penetrating everything deeper into the tissue. Sometimes such a tightened process leads to the defeat of vital systems of the human body. So, for example, vaginal candidiasis can cause infertility. The very sad version is a fungal sepsis.
The following forms of candidiasis distinguish:
- Candidiasis of skin folds;
- Paronichia and onyhia Candidal origin;
- Candadose Haleitis;
- Candidiasis of intestine and stomach;
Any of these diagnoses are postponed after diagnostics (taking scraping from mucous or skin). If you still doubt whether to go to the doctor, we offer a dozen most popular questions on the topic: "Candidiasis: treatment." They are most often asked to dermatologists during the reception.
Question 1. Why are some chick candidiasis, and others are not?
Candida mushrooms are in the body of every person, but, as it was rightly noticed, only individual categories are ill. First of all, these, which from the intestines disappear bifidobacteria and lactobacillia and there is dysbacteriosis. In the intestine, yeast mushrooms begin to actively multiply and conquer new territories of the body. In addition, the risk of developing candidiasis in those who have accepted antibiotics for a long time are great.
Question 2. How to treat Candidiasis of the oral cavity?
 Candidiasis of the oral cavity occurs most often in two categories: in children of breasts, as well as in individuals using dentures. It begins with the swelling of the gum, redness of the mucous cheeks and language. Then there are white curls, which gradually capture the increasing area and form different shapes of the film. Temperatures, inflammation of lymph nodes in this form of the candidiasis does not happen. The kids in the thrush refuse to eat, become restless, and adults mark increased dryness in the mouth and burning, which is enhanced during food intake. If the disease flows into a chronic form, then the defeat of voice ligaments, candidal rhinitis, candidiasis of the pharynx, etc. occurs.
Candidiasis of the oral cavity occurs most often in two categories: in children of breasts, as well as in individuals using dentures. It begins with the swelling of the gum, redness of the mucous cheeks and language. Then there are white curls, which gradually capture the increasing area and form different shapes of the film. Temperatures, inflammation of lymph nodes in this form of the candidiasis does not happen. The kids in the thrush refuse to eat, become restless, and adults mark increased dryness in the mouth and burning, which is enhanced during food intake. If the disease flows into a chronic form, then the defeat of voice ligaments, candidal rhinitis, candidiasis of the pharynx, etc. occurs.
Treatment of the Candidosis of the oral cavity takes 2-4 weeks. Duration depends on how the drug is a mycologist considers it necessary to use.
In advanced cases, when erosion and ulcers are formed under the touch, they will have to take stronger systemic preparations (pills). These include ketoconazole, fluconazole, itraconazole.
Question 3. How to treat bowlist candidiasis?
The main symptoms of the intestinal candidiasis are pain at the bottom of the abdomen, a feeling of constant gravity in the stomach, bloating, a liquid chair with mucous splashes. In addition, in the chair you can see white curls. Additional signs of candidiasis are considered rash on face, various dermatitis, rashes on the back and other parts of the body.
The treatment of the bowel candidia depends on which form of the disease is diagnosed. Thus, with non-invasive candidiasis (light shape), resorbative antimitics of Levuary, nystatin, neutamicin are prescribed; With invasive form (it is rarely, other organs are affected with it) it is necessary to take fluconazole, ketoconazole, intrancezol. However, systemic antifungal drugs often cause side effects and do not always reach the level of the ileum, where numerous colonies of fungi live.
High fungicidal potential has antifungal antibiotic pimafucine. In clinical practice, there were no fungi, which could resist or get used to this drug. Pimafucin begins to act only in the lumen of the intestine and is not absorbed in the gastrointestinal tract. The advantage of the drug can also be considered the possibility of its use during pregnancy and breastfeeding.
Question 4. How to treat Candidiasis of skin and nails?
Candidias of the skin occurs often in large folds of the skin: inguinal, inter-fodder, under the milk glands, under the mouse. Sometimes small bubbles with purulent content, cracks, peeling appear in interdantal folds. Plots of inflammation can occupy huge areas, and in case of autopsy, leave behind red-burgundy erosion. Externally, clidiasis of the skin resembles an extensive burn.
If the fungi of the genus Candida is striking the near-gas roller, he opens first, and then begins to peel. At first, it starts to suffer the nail plate: it is thinning or thickened, begins to crumble. Usually inflammation takes place in itself, otherwise treatment is required.
With damage to the skin and folds, antibiotics of the polyenk row in the form of cream, solution or ointment are prescribed. It:
- Zalain;
- Kanizon;
- Candid.
They are applied 1-2 times a day until the symptoms are completely disappeared, and then another 7-10 days to avoid re-infection. If local drugs could not help, then we need to receive systemic antimicotics: fluconazole, Oronghal. Their dose depends on body weight and age.
When candidiasis of near-heating rollers and nails can also be used by systemic drugs: fluconazole 2-3 months 150 μg, neungal by pulse therapy. You can treat the nail fungus on the feet of the candid (the drug is produced in various forms). It is applied by a thin layer on a plot of inflammation, which is washed in advance with soap having a neutral pH.
Question 5. How to treat candidias in the throat?
If the temperature rose, it became painful to swallow, the appetite worsened, and a grayish-white flare appeared in the sky, almonds and handles, then a grayish-white challenge appeared, then perhaps the candida's mushrooms were struck. Treatment of fungus Candida in the throat is carried out according to other types of candidiasis. So, for rinsing uses Lugol, hexetidine, manganese, chlorhexidine, copper sulfate, propolis. It is possible to lubricate the throat with a cotton wand, moistened in a solution of borax in glycerin, a solution of methylene blue and diamond green. Due to the fact that these tools often cause irritation, it is worth considering the possibility of receiving imidazole antibiotics of local applications: nestatin chewable tablets, amphotericin, ketoconazole, fluconazole.
In severe cases, it is necessary 3-4 times a day to take pills of fungicine, Nistatin, micostatine inside without chewing. The course lasts a maximum of 10 days. Fluconazole and drugs based on it are well established: Diflucan, Fusis, Mikosist. The duration of treatment and the dosage determines the doctor.
There is also fungal angina (usually in children)
Question 6. What is the most effective treatment of candidiasis?
 Treatment is recognized effective only if the disease can be defeated. That's just antifungal systemic and local drugs, it does not always succeed. First, there may be reduced individual sensitivity to the components of the drug. Secondly, mushrooms can develop immunity to medicine. So a few decades ago, Nystatin was a good account, only yeast mushrooms have formed stability to it. Amphotericin and Lev Rooms are trying not to prescribe due to their high toxicity.
Treatment is recognized effective only if the disease can be defeated. That's just antifungal systemic and local drugs, it does not always succeed. First, there may be reduced individual sensitivity to the components of the drug. Secondly, mushrooms can develop immunity to medicine. So a few decades ago, Nystatin was a good account, only yeast mushrooms have formed stability to it. Amphotericin and Lev Rooms are trying not to prescribe due to their high toxicity.
In modern medicine, preference is given to funds based on fluconazole. This is a diefucan, microsist, flukostat, diphlasone. They are well absorbed into the gastrointestinal tract, absorbed by the body by 90%, have a long action and, important for women, do not affect the hormonal background.
Another good drug is pimafucin candles. It does not have almost no contraindications (his reception is allowed to pregnant and children), does not harm the body, well, the most important thing is to be surelessly: the fungi was not detected, which would show resistance to pymofucin.
At the initial stages of the candidiasis are both local antifungal agents: they act purely at the localization site of the fungus, practically not absorbed into the bloodstream and do not affect the allocation organs (kidney and liver).
Question 7. The drug "Candid": in what cases can it be used?
Candid is a synthetic antifungal drug, which is used with various fungal lesions of mucous membranes and leather. In pharmacies, you can purchase candida in the form of a solution, powder, cream. The cream does not penetrate the systemic bloodstream, and therefore the side effects are practically absent. All who have been identified by surface candidiasis can use. Pregnant women are no exception. Similarly, Candid in the form of powder is also used.
Treatment of nail fungus Candide solution in rare cases causes redness of the skin, and therefore can also be assigned to all categories of patients, with the exception of persons with increased sensitivity to Clotrimazole - the main active substance of the drug. The solution can be used (with caution) to apply when candidiasis of mucous membranes in newborns: the sterile bandage is wound on the finger, immersed in the candidium solution.
Vaginal candidiasis is treated candidium gel, but it cannot be applied in the first trimester of pregnancy (in the second and third - only under the control of the doctor), during menstruation. Ointment and solution are not suitable for persons who have impaired skin integrity.
Question 8. Is it possible to cure candidiasis recipes of traditional medicine?
Treatment of fungus Candida recipes of traditional medicine plays an auxiliary role, because the main components are grass, and they have antimicrobial, anti-inflammatory, drying, disinfectant properties. At the same time, phytotherapy does not eliminate the cause of fungal infection, but only slows down the development of the disease and in some cases helps to avoid relapse. It is better to consult with a doctor and complement the medication treatment of phytotherapy.
Therapy of such a disease as candidiasis involves the use of funds such as local and systemic effects. Each method of treatment has a number of their advantages. Antifungal drugs from candidiasis for intakes eliminate the fungus quickly and throughout the body, and local destination - help restore the normal microflora of the genitals, and affect the mucous membrane only in a particular place.
In modern medical practice there are several substances destroying mycelium fungus, and a huge variety of drugs in which they are contained. Antifungal drugs for the treatment of thrush differs at the rate of absorption in the body and dosages. But at the same time, all of them peculiar to prevent the growth and reproduction of the yeast-like fungus of the genus Candida.
For effective treatment, it is most often necessary to combine. Before using any medicines, it is important to consult with a specialist, self-medication can harm your health.
For women

Ginsen
Antifungal drug against thrush related to the derivative of Nistatan. Therapeutic effect is manifested due to the part of the drug miconazole. It is he who destroys the membrane fabric of fungi, thereby preventing the growth and reproduction of pathogenic microflora. The medicinal product has two forms of release: and.
For the treatment of thrush in women. They must be used in the dosage 1 time per day. Before administration, it is recommended to accept hygienic. The duration of therapy is one week. With a recurrent thrush, local treatment can be combined with taking tablets, to enhance the effect.
Diflucan
Anti-gribery from a group of triazoles. The active substance is fluconazole, which has the ability to inject the exchange processes inside the fungal cell. The drug is made to combat diseases caused by yeast-like fungi genus Candida.
Fluconazole is considered one of the most effective substances of the Candidian therapy, finds its use in gynecological practice. Therapeutic dose of the drug - 150 mg once. However, it is most often necessary to combine it with antifungal intravaginal suppositories.
Torzhin
Vaginal pills. Active substances: Terenidazole and neomycin. It is an extremely effective drug against candidiasis due to the fact that a fungicidal agent is also affected by pathogenic microorganisms.
For men

Nystatin
Antibiotic from a group of polyentes, showing its activity against the fungi of the genus Candida. The main mechanism of its action is associated with a decrease in the protective function of the cell membrane fungus, which leads to its death. It has a bacteriostatic and bactericidal action. Men can use the drug in the form and.
The course of treatment with pills lasts at least 10 days. They must be taken twice a day, drinking half the glass of water. Used overnight after the isolation. During treatment, alcohol should be eliminated from the diet and refrain from intimate life.
Clotrimazole ointment
Antifungal agent for outdoor use, slowing down the growth of pathogenic microorganisms. A small concentration of its concentration stops the processes of reproduction of fungi, and large causes irreparable harm to pathogenic cells, destroys their membranes and leads to death. The active action of ointments is manifested in respect of all kinds of fungi, especially the genus Candida.
It is necessary to apply after receiving the bath, massaging movements up to 3 times a day. The duration of therapy is individual and depends on. On average, it takes up to two weeks, but after the disappearance of all signs of the disease, ointment is used once a day for 1-2 weeks in order to prevent recurrence.
Iratenazole.
Synthetic antifungal agent having a wide range of action. A system of system action, which, in accordance with the instructions for use in the forces, to destroy fungal bacteria from the inside and prevent the appearance of relapses.
When candidiasis, men in men should take 200 mg twice a day strictly after meals (in order not to disturb the performance of the gastrointestinal tract). The duration of therapy should be adjusted by the doctor and is selected individually.
For kids

Candid
Specialized agent for the treatment of milk of the mouth in children. The composition contains clotrimazole, which has a bactericidal and bacteriostatic effect on fungi. The drug candidy is produced in the form of a solution, cream and gel. For the therapy of the mucous membranes of the oral cavity in children use a solution. Details of treatment are prescribed by a specialist depending on the situation, but most often the treatment scheme is approximately as follows:
- The procedure is carried out strictly after feeding the child;
- There are several drops of solution on cotton wand (or tampon);
- The affected areas of mucous membranes are abundantly lubricated by the drug;
- The frequency of use should not exceed 4 times a day.
After a few days, significant improvements in the state of the child will be noticeable, but the treatment should be continued for at least a week.
Pimafucin
Common medicine for the treatment of fungal lesions caused by the fungi of the genus Candida. The main component is an antibiotic from a group of macrolides with a wide range of action. The mechanism of action is based on the binding of sterol groups in the cell membrane of bacteria, which leads to a violation of the exchange processes and the death of pathogenic microorganisms. The advantage of the drug is the possibility of its use during pregnancy and children.
It is better to combine with overall preparations, comprehensive therapy will exclude the likelihood of relapses.
For the treatment of thrush in children, the cream is applied to the affected areas up to 4 times a day strictly after feeding the baby. The duration of therapy is appointed by a doctor, most often is 10-14 days.
Kanizon
A medicinal remedy with antifungal, anti-inflammatory and antibacterial effect. The main active substance is Clotrimazole. The drug belongs to the group of combined medicines. The properties of the caison are associated with its ability to slow down the biosynthesis of substances necessary for the vital activity of fungi, thereby causing their death.
When candidial defeat of the ointment ointment, the ointment should be applied to the affected areas within 7-14 days. The duration of the course of treatment is determined by the doctor, assessing the severity of the course of the disease.
Ketoconazole has a fungistatic effect. And with a local application, a high concentration of the drug.
For the treatment of thrush, one candle of ketoconazole is introduced into the vagina before bedtime. Depending on the severity of treatment, you can continue from 3 to 10 days.
With complicated or chronic disease, the ketoconazole tablets are taken inside, 0.2 g twice a day or 0.4 g 1 time per day during food intake. Course of treatment on average 7 days.
The analogues of ketoconazole are dermazole and.

This article is often read:
Flucostat
The main active substance is fluconazole, which refers to the derivative of the triazole. It oppresses the synthesis of sterols in the cells sensitive to the drug of mushrooms from the genus Candida or Kryptokokok.
The drug is quickly absorbed, and its half-life is up to 30 hours.. For the treatment of thrush, it is most often used once in the dosage of 150 mg. To reduce often recurrences of the disease at more than 3 episodes per year, 1 capsule (150 mg) of flukostat occasionally per month. The duration of therapy can be from 6 to 12 months, depending on the severity of the disease. In some cases, the reception frequency can be increased.
Diflucan
 Fluconazole enters the diplucan. This derivative of triazole is oppressing ergosterol synthesis in mushroom cell membranes. The drug is used for the treatment of thrush, including in the chronic form of the disease.
Fluconazole enters the diplucan. This derivative of triazole is oppressing ergosterol synthesis in mushroom cell membranes. The drug is used for the treatment of thrush, including in the chronic form of the disease.
In order to get rid of the disease, a single reception of diphlucan in a dose of 150 mg. With severely form of the disease, the drug is accepted in the 1st, 3rd, 7th day and an additional one capsule on the first day of menstruation.
In the chronic form of the disease, the diefucan takes 150 mg times per month. The number of techniques can be increased if necessary. It is not recommended to take the drug during pregnancy and during lactation.
Livaroll.
The active substance is ketoconazole. It refers to the means from the group of imidazoles and has a pronounced antifungal action. The drug is used to treat acute and chronic form of candidiasis in women, as well as diseases caused by mixed infections.
In order to get rid of thrush candle placed in the vagina once a day before bed. Treatment lasts from 3 to 10 days, depending on the form of the disease and on the frequency of its relapses.
Pregnant women can use the drug in the second and third trimester, as appointing a doctor.
Irunun
The active substance is an etraconazole (antifungal agent from a group of triazoles). It negatively affects the cell membranes of mushrooms, causing their death. The drug has a wide range of action and effectively copes with yeast mushrooms and mold mushrooms, as well as dermatophitis.
For the treatment of thrush, 100 mg of the drug is prescribed twice a day for one day. You can also apply 100 mg 1 time per day for 3 days.
In order to get rid of the disease, you can use vaginal tablets. They are introduced into the vagina 1 time per day before bedtime. Treatment continues from 7 to 14 days, depending on the severity of infection.
Clotrimazole
Clotrimazole is one of the most famous drugs from the candidiasis in women. It belongs to the derivative of imidazole and has a fungistatic action. The drug violates the biosynthesis of ergosterol in the membrane of fungus, thereby destroying it.
 Clotrimazole do not take inside. It is produced in the form of cream or vaginal tablets of 0.1 g.
Clotrimazole do not take inside. It is produced in the form of cream or vaginal tablets of 0.1 g.
For the treatment of thrush Clotrimazole 1 tablet introduced into the vagina overnight.
The effect of the use of the drug becomes noticeable for 3 days, but treatment must be continued, since the premature cessation may cause the disease to go into a chronic form.
Clotrimazole's analogues are -, Kaporno.
Lymbassin
The existing substance of Lymbosin is Fenticonazole. It has both a fungicidal, so a fungistatic action.
It oppresses the production of ergosterner, which is part of the mushroom cell membranes, disturbing the ability of the fungus cells to play.
We produce a drug in the form of capsules of 600 and 1000 mg or cream. It only acts locally, so capsules are not used inside, but introduced into the vagina.
For the treatment of thrush can be enough 1 capsuleswhich is put before bedtime. If necessary, after 3 days, another Capsule of Lymbosin is introduced.
In most cases, the thrush in women is complicated by other diseases, so in order to get rid of it, it is necessary to consult a doctor and pass tests.
Treatment of chronic thrush
In order to get rid of chronic thrush, first of all it is necessary to restore the work of the immune system. To do this, you need to conduct a healthy lifestyle, to eat right and turn to the doctor in time, in order to prevent the emergence of other chronic diseases.
 In chronic thrush, fluconazole is used (Diflucan, diphluzol, microsist).
In chronic thrush, fluconazole is used (Diflucan, diphluzol, microsist).
This drug takes 150 mg in the 1st, 3rd and 5th day of exacerbation of the disease, as well as on the first day of the start of menstruation. With frequent recurrences of the disease, 150 mg of fluconazoles are prescribed once a month over 4 - 12 months.
In chronic thrush, intraconazole can be appointed, which must be taken by 200 mg 2 times a day for 3 days.
Additionally, prescribe preparations in the form of candles: pimafucine, Zalayan, Polizinaks, Nystatin.
The best remedy for the thrush in women will help choose a doctor!
Treatment of chronic thrush during pregnancy and feeding drugs
The causes of the thrush include changes in hormonal background and weakening immunity that accompany pregnancy and lactation.
One of the most efficient and safe means is candles. The active ingredient means is an antibiotic of a Natamicin polyenic series, which disrupts the integrity of the mushroom cell membranes.
Under the local application, the drug is not absorbed through the skin and mucous membranes, so it does not penetrate the systemic bloodstream and does not fall into breast milk. They are introduced deep into the vagina before bedtime. Apply 1 candle per day for 3 to 9 days, depending on the severity of the disease.
In the second and third trimester of pregnancy, you can use Candles Terezhinin, Livarol or Clotrimazole.
Before applying drugs from thrush during pregnancy or feeding, you need to consult a doctor.
Now you know what to treat the thrush in women and what popular drugs for this take.

Nowadays, fungal diseases of various types and distribution of diseases of the mucous membranes, skin, respiratory tract, nails are very common. Antifungal preparations are used to treat fungal infections.
Vaginal candidiasis (thrush) is also cured by antifungal medicines, which today are presented in a wide range. The thrush is acute and chronic forms. From the diagnosis of this disease, its severity of the flow and manifestations depends on the treatment of those or other drugs.
If the thrush in the initial stage, then it can be cured in a matter of days, and if the form is running or chronic, then the process of recovery is long, conjugate with multiple studies and recurrence (repetition) of the disease.
Treatment by much more efficient if the human body receives the required amount of minerals, vitamins. Often, the intestinal microflora is impaired, which entails bowel bacteriosis, and it turns out in parallel in the body several fungal lesions that must be treated in the complex.
Spectrum of action of antifungal drugs

The lack of antifungal drugs is that when applied in gynecology, vaginosis can develop - allocations with fish odor. Preparations in capsules and tablets have a toxic effect on the kidneys and the liver.
Important!
It is necessary to know that when taking antifungal drugs, multiple side effects occur from the digestive tract and from the nervous system.
Side effects:
- Nausea, pain in the abdomen, diarrhea.
- Violation of the liver function, change in taste and meteorism.
- Headache, cramps, dizziness.
- Allergic reactions.
I especially want to say about the preparations, which contains the substance of itraconazole. This substance causes serious side effects especially often. That is why the use of oral antifungal drugs in gynecology should be appointed exclusively a gynecologist and only with the serious development of the thrush, the chronic form, when local therapy does not help.
Many drugs cannot be used during pregnancy and during breastfeeding period of the child, with renal and liver failure and hypersensitivity to individual drugs. We will get acquainted with some of the most famous antifungal drugs.
Ten most effective antifungal drugs

- Diflucan. This is the most popular drug. Its capsules contain fluconazole, overwhelming the growth of fungi. It is enough to drink 1 capsule (150mg). Contraindications: lactation period, pregnancy, kidney and liver disease.
- Pimafucin. A popular and efficient drug that is allowed during pregnancy and lactation. Produced in the form of tablets, creams and candles. It is well tolerated, non-toxic. Allergic reactions are absent. The substance is natamycin, has a wide spectrum of antifungal action.
- Clotrimazole. This antifungal agent is produced in the form of vaginal tablets and cream. For outdoor use there are ointments, powders, cream and solution. Contraindications: Cannot be used in the first trimester during pregnancy, and during lactation - with caution.
- Livaroll.. Effective and safe antiharyal action preparation. It has an active substance - ketoconazole. The drug can be used during pregnancy, except for the first trimester. Available in the form of vaginal type suppositories. The course of treatment is 5 days, and 10 days in the chronic form of the disease.
- Hexicon. This agent is produced in the form of a gel and a solution for external use, as well as in the form of vaginal suppositories. The composition of the drug includes chlorhexidynibigyluconate as an active substance. Excellent result of the treatment of thrush in pregnant women. It is also used to have a reservation during childbirth. It can be used to treat children.
- Microsist. Property of antifungal action with fluconazole as an active substance. Not recommended during pregnancy and feeding babies, and for children who under 6 months.
- Epigen-sex. This is a spray with antiviral, anti-inflammatory, anti-loving immunostimulating effect. As an active substance - glycyrrhizinic acid. Can be used during pregnancy and lactation.
- Torzhin. Antibacterial and antifungal drug. Vaginal tablets can be used during pregnancy (except for the first trimester) and during lactation. This means does not apply during menstruation.
- Mikomax. This is an antifungal drug with an active substance Fluconazole. Produced in the form of capsules, syrup and mortar. Contraindications: It is impossible to use during pregnancy during lactation. Sometimes used to treat children.
- Polizinaks. Antibacterial antifungal drug. Produced in the form of intravaginal and vaginal capsules with emulsion. Not recommended during pregnancy and lactation.
Remember that all drugs from the thrush have different side effects and contraindications, so the destination is producing only a doctor in each individual case.
Anti-gear drugs of the new generation

Antimicotics IV generation. New generation of drugs. Some of them are already registered, and some are in the test stage.
New drugs include:
- Liposomal forms of Nistatin and Amphotericin V.
- New triazoles, this is: Posakonazole, vorikonazole, Echinochandines, Rauconazole.
Polyena. At the implementation stage there are lipid forms of antibiotics of polyenov forms:
- Liposomal form of amphotericin V.
- Liposomal form of nystatin.
- Polyen. Amphotericin derivatives are represented by new drugs: ambiz - liposomal, amphotericin B, abelcetes - lipid complex amphotericin B, amphocyl-colloid dispersion of amphotericin V.
Triazoles. New triazoles - generation IV antimicotics. Already fits the use of voriconazole. This is the newest class of antifungal drugs that affect the cell of the pathogen.
Echinocandines. These drugs block the biosynthesis of one of the components of the fungal cell. Preparations with good tolerability and with minimal side effects. Echinocandines are an improved preparation for the treatment of thrush and mycoses for the nearest period. One of the representatives of Echikandinov - Kaspofungin, which is used in practice.
All listed antifungal spectrum preparations described in this article are given to familiarize themselves, and not applications. Self-health is dangerous to health.