Pancreatitis - diet
When the pancreas becomes inflamed, it stops throwing digestive juice into the duodenum. Without this secretion, food is not broken down into simple substances and is not absorbed. The most common cause of pancreatitis is an addiction to fatty foods flavored with alcohol. That is why diet in its treatment is the main remedy.
Diet rules for pancreatitis
For many people, the disease quickly becomes chronic. If acute pancreatitis is diagnosed, the 5p diet reduces the risk of this prospect and protects against the development of diabetes. Table 5a is prescribed when pancreatitis is complicated by inflammation of the bile ducts, and table 1 – by stomach diseases. The diet for chronic pancreatic disease during exacerbations is more strict.
The basic rules of diet for pancreatitis are prescribed to the patient:
- maintain the norm of fats – 80 g, carbohydrates – 350 g;
- give up smoked foods and fried foods;
- prepare food according to dietary recipes;
- eat every 3 hours;
- eat warm dishes pureed;
- eat food in small portions;
- eat slowly, chewing food for a long time;
- don't wash down your food.
What can you eat if you have pancreatitis?
Despite all the prohibitions and restrictions, the menu can be very diverse. What can you eat if you have pancreatitis? The diet includes:
- salads, vinaigrettes, purees (boiled carrots, beets, potatoes, zucchini, cauliflower, young beans);
- celery (in remission);
- vegetable soups, borscht;
- meat dishes from boiled lean chicken, beef, fish;
- vegetable oils;
- any low-fat dairy products (including cream, yogurt), cottage cheese, cheeses;
- oatmeal, buckwheat, pumpkin porridge with milk;
- chicken egg whites;
- compotes (fresh fruits, berries, dried fruits);
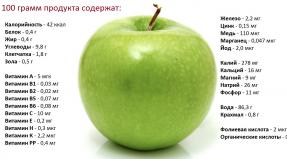
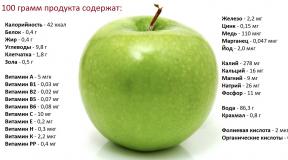
- apples of non-acidic varieties, rich in iron;
- slightly stale bread.
What not to eat if you have pancreatitis
The inflamed organ is in dire need of a break, a gentle mode of operation. What should you not eat if you have pancreatitis? Completely prohibited:
- alcohol;
- fatty, rich first courses;
- pork, lard, lamb, goose, duck, offal;
- smoked meats, sausages;
- fatty fish;
- any canned food, marinades;
- fried main courses (including scrambled eggs);
- hard-boiled eggs;
- fast food;
- hot sauces, seasonings;
- raw onion, garlic, radish, radish, bell pepper;
- legumes;
- mushrooms;
- sorrel, spinach;
- bananas, grapes, pomegranate, figs, dates, cranberries;
- sweet desserts;
- cocoa, coffee, soda;
- fresh bread, pastries, baked goods.
Diet for chronic pancreatitis
It is very important that the sick body receives about 130 g of proteins daily, which are needed for optimal metabolism. Moreover, approximately 90 g should consist of animal products (boiled or steamed according to recipes), and only 40 g of vegetable products. Consumption of lean products protects the patient from the risk of fatty liver.
Animal fats in the diet for pancreatitis should be 80%. It is better to add butter to prepared dishes. Do not forget about recipes for dishes with laxative products (prunes, dried apricots). It is better to use milk in soups, porridges, sauces, and jelly. Fresh kefir is much healthier. Diet for mild chronic pancreatitis can be varied with low-fat cheeses and steamed omelettes. The body should not receive more than 350 g of carbohydrates daily.
A diet during exacerbation of chronic pancreatitis should give a respite to the exhausted pancreas. For the first 2 days of a severe attack of illness, you can only drink warm infusion of rose hips, tea, Borjomi. On the third day, a patient with pancreatitis is allowed to give liquid puree soups, water porridge, and milk jelly. After the pain disappears, the diet is carefully expanded, adding denser, unprocessed dishes.

Diet for acute pancreatitis
For the first 2 days of illness, complete abstinence from food is also indicated - you can only drink water, tea, rosehip infusion (4-5 glasses each). For the next 2 days, nutrition is administered through droppers. Then the diet for inflammation of the pancreas in the acute phase is formed on the basis of exclusively low-calorie foods. They are given in very small quantities so as not to cause harm.
The diet for acute pancreatitis during the second and subsequent weeks becomes more varied. The menu includes:
- soups, liquid porridges and jelly, juices, green tea;
- lean chicken (especially steamed cutlets) instead of red meat, other protein products;
- antioxidant-rich vegetables and fruits.
How long does the diet last for pancreatitis?
The timing of compliance with dietary rules for both adults and children depends on the type of illness. Treatment of the disease in its acute form must be carried out only inpatiently, and exacerbation of the chronic stage - on an outpatient basis. How long does the diet last for pancreatitis of the pancreas in the acute stage? The course of treatment takes approximately 2-3 weeks. The diet after discharge should be followed for at least six months.
A correct, gentle attitude towards the pancreas prevents future exacerbations of the disease and protects the patient from the onset of diabetes. If the inflammation has become chronic, then the person must follow the dietary menu for pancreatitis all his life. Even after the disease has entered the stage of stable remission, one should not delude oneself into the hope of a complete recovery.