What is insulin resistance. Its symptoms and treatment. Diet for insulin resistance
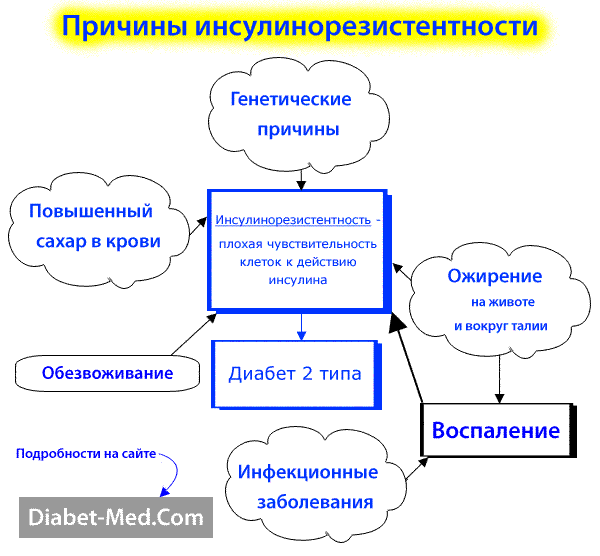
Insulin resistance is an impaired biological response of body tissues to the action of insulin. And it doesn’t matter where insulin comes from, from your own pancreas (endogenous) or from injections (exogenous).
Insulin resistance increases the likelihood of not only type 2 diabetes, but also atherosclerosis, heart attack, and sudden death due to blockage of the vessel by a blood clot.
The action of insulin is to regulate metabolism (not only carbohydrates, but also fats and proteins), as well as mitogenic processes - this is growth, cell reproduction, DNA synthesis, gene transcription.
The modern concept of insulin resistance is not limited to disorders of carbohydrate metabolism and an increased risk of type 2 diabetes. It also includes changes in the metabolism of fats, proteins, gene expression. In particular, insulin resistance leads to problems with the endothelial cells that line the inside of blood vessel walls. Because of this, the lumen of the vessels narrows, and atherosclerosis progresses.
Insulin resistance symptoms and diagnosis
You may suspect insulin resistance if your symptoms and/or tests show that you have. It includes:
- obesity at the waist (abdominal);
- poor blood tests for cholesterol and triglycerides;
- detection of protein in the urine.
Abdominal obesity is the main symptom. In second place is arterial hypertension (high blood pressure). It rarely happens that a person does not yet have obesity and hypertension, but blood tests for cholesterol and fats are already bad.
Diagnosing insulin resistance with tests is problematic. Because the concentration of insulin in the blood plasma can vary greatly, and this is normal. When analyzing insulin in the blood plasma on an empty stomach, the norm is from 3 to 28 mcU / ml. If there is more than normal insulin in the blood on an empty stomach, then the patient has hyperinsulinism.
Elevated insulin levels in the blood occur when the pancreas produces too much insulin to compensate for tissue insulin resistance. This analysis result indicates that the patient has a significant risk of type 2 diabetes mellitus and/or cardiovascular disease.
An accurate laboratory method for determining insulin resistance is called the hyperinsulinemic insulin clamp. It involves continuous intravenous administration of insulin and glucose for 4-6 hours. This is a time-consuming method and therefore rarely used in practice. Limited to fasting blood test for plasma insulin levels
Research has shown that insulin resistance occurs:
- 10% of all people without metabolic disorders;
- in 58% of patients with hypertension (blood pressure above 160/95 mm Hg);
- in 63% of persons with hyperuricemia (serum uric acid is more than 416 µmol/l in men and above 387 µmol/l in women);
- in 84% of people with elevated blood fat levels (triglycerides over 2.85 mmol/l);
- in 88% of individuals with low levels of “good” cholesterol (below 0.9 mmol / l in men and below 1.0 mmol / l in women);
- in 84% of patients with type 2 diabetes;
- in 66% of individuals with impaired glucose tolerance.
When you take a blood test for cholesterol, check not total cholesterol, but separately “good” and “bad”.
How insulin regulates metabolism
Normally, the insulin molecule binds to its receptor on the surface of cells in muscle, adipose, or liver tissue. This is followed by autophosphorylation of the insulin receptor with the participation of tyrosine kinase and its subsequent connection with the substrate of the insulin receptor 1 or 2 (IRS-1 and 2).
In turn, IRS molecules activate phosphatidylinositol-3-kinase, which stimulates GLUT-4 translocation. It is the carrier of glucose into the cell through the membrane. This mechanism ensures the activation of metabolic (glucose transport, glycogen synthesis) and mitogenic (DNA synthesis) effects of insulin.
Insulin stimulates:
- Uptake of glucose by muscle cells, liver and adipose tissue;
- Synthesis of glycogen in the liver (storage of “fast” glucose in reserve);
- Capture by cells of amino acids;
- DNA synthesis;
- Protein synthesis;
- Synthesis of fatty acids;
- Ion transport.
Insulin suppresses:
- Lipolysis (breakdown of adipose tissue with the release of fatty acids into the blood);
- Gluconeogenesis (transformation of glycogen in the liver and the entry of glucose into the blood);
- Apoptosis (self-destruction of cells).
Note that insulin blocks the breakdown of adipose tissue. That is why, if the level of insulin in the blood is elevated (hyperinsulinism is a frequent occurrence in insulin resistance), then it is very difficult, almost impossible, to lose weight.
Genetic causes of insulin resistance
Insulin resistance is the problem of a huge percentage of all people. It is assumed that it is caused by genes that have become predominant in the course of evolution. In 1962, they hypothesized that it is a survival mechanism during prolonged famine. Because it enhances the accumulation of fat reserves in the body during periods of abundant nutrition.
Scientists subjected mice to starvation for a long time. Those individuals who were found to have genetically mediated insulin resistance survived the longest. Unfortunately, in humans, under modern conditions, the same mechanism “works” for the development of obesity, hypertension and type 2 diabetes.
Studies have shown that patients with type 2 diabetes have genetic defects in signaling after insulin binds to its receptor. These are called post-receptor defects. First of all, the translocation of the glucose transporter GLUT-4 is disrupted.
Patients with type 2 diabetes also found impaired expression of other genes involved in the metabolism of glucose and lipids (fats). These are the genes for glucose-6-phosphate dehydrogenase, glucokinase, lipoprotein lipase, fatty acid synthase, and others.
If a person has a genetic predisposition to develop type 2 diabetes, it may or may not cause diabetes. It depends on the lifestyle. The main risk factors are overnutrition, especially the consumption of refined carbohydrates (sugar and flour), as well as low physical activity.
What is the sensitivity to insulin in different tissues of the body
For the treatment of diseases, insulin sensitivity of muscle and adipose tissue, as well as liver cells, is of the greatest importance. But is the degree of insulin resistance of these tissues the same? In 1999, experiments showed that it was not.
Normally, to suppress by 50% lipolysis (fat breakdown) in adipose tissue, an insulin concentration in the blood of no more than 10 mcU / ml is sufficient. For 50% suppression of the release of glucose into the blood by the liver, about 30 μU / ml of insulin in the blood is already required. And in order for the uptake of glucose by muscle tissue to increase by 50%, an insulin concentration in the blood of 100 μU / ml and above is needed.
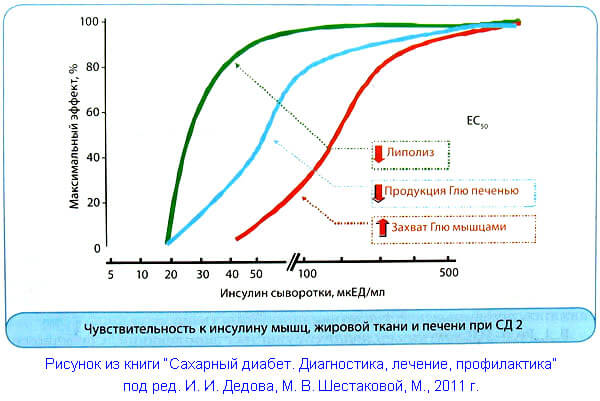
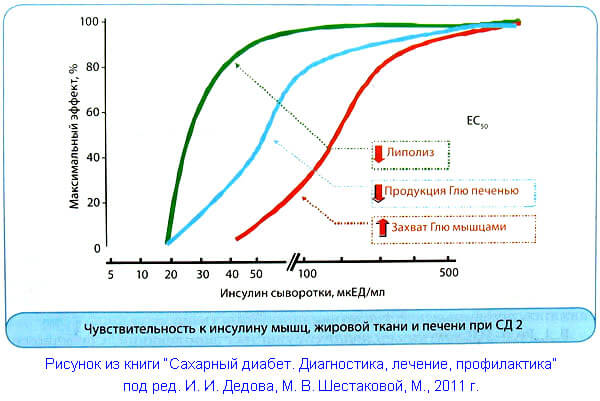
We remind you that lipolysis is the breakdown of adipose tissue. The action of insulin suppresses it, as well as the production of glucose by the liver. And the uptake of glucose by the muscles under the action of insulin, on the contrary, increases. Please note that in type 2 diabetes, the indicated values of the required concentration of insulin in the blood are shifted to the right, i.e., in the direction of increasing insulin resistance. This process begins long before diabetes manifests itself.
The sensitivity of body tissues to insulin decreases due to genetic predisposition, and most importantly, due to an unhealthy lifestyle. In the end, after many years, the pancreas ceases to cope with the increased load. Then they diagnose “real” type 2 diabetes. The patient is greatly benefited if the treatment of the metabolic syndrome is started as early as possible.
What is the difference between insulin resistance and metabolic syndrome?
You should be aware that insulin resistance occurs in people with other health problems that are not included in the concept of “metabolic syndrome”. This:
- polycystic ovaries in women;
- chronic renal failure;
- infectious diseases;
- glucocorticoid therapy.
Insulin resistance sometimes develops during pregnancy and disappears after childbirth. It also usually increases with age. And it depends on the lifestyle of an older person whether it will cause type 2 diabetes and / or cardiovascular problems. In the article "" you will find a lot of useful information.
Cause of type 2 diabetes
In type 2 diabetes mellitus, insulin resistance of muscle, liver, and adipose tissue cells is of greatest clinical importance. Due to the loss of sensitivity to insulin, less glucose enters and “burns out” in muscle cells. In the liver, for the same reason, the process of breakdown of glycogen to glucose (glycogenolysis), as well as the synthesis of glucose from amino acids and other “raw materials” (gluconeogenesis), is activated.
Insulin resistance of adipose tissue is manifested in the fact that the anti-lipolytic effect of insulin weakens. At first, this is compensated by increased production of insulin by the pancreas. In the later stages of the disease, more fat is broken down into glycerol and free fatty acids. But during this period, losing weight is no longer a particular joy.
Glycerol and free fatty acids enter the liver, where they form very low density lipoproteins. These are harmful particles that are deposited on the walls of blood vessels, and atherosclerosis progresses. Also from the liver, an excess amount of glucose enters the bloodstream, which appears as a result of glycogenolysis and gluconeogenesis.
The symptoms of metabolic syndrome in humans long precede the development of diabetes mellitus. Because insulin resistance for many years is compensated by excess production of insulin by pancreatic beta cells. In this situation, there is an increased concentration of insulin in the blood - hyperinsulinemia.
Hyperinsulinemia with normal blood glucose levels is a marker of insulin resistance and a precursor to the development of type 2 diabetes. Over time, the beta cells of the pancreas can no longer cope with the load, which is several times higher than normal. They produce less and less insulin, the patient's blood sugar rises and diabetes develops.
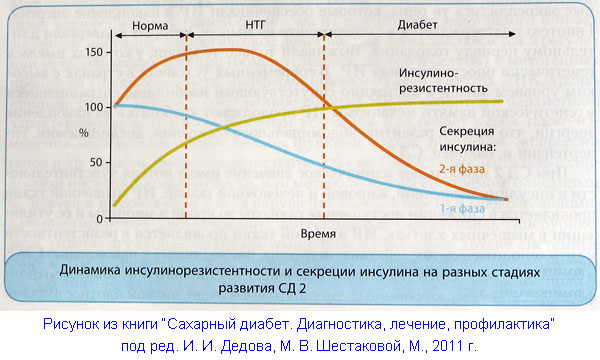
First of all, the 1st phase of insulin secretion suffers, i.e., the rapid release of insulin into the blood in response to a food load. And basal (background) secretion of insulin remains excessive. When blood sugar levels rise, this further increases insulin resistance in tissues and inhibits the function of beta cells to secrete insulin. This mechanism for the development of diabetes is called “glucose toxicity”.
Risk of cardiovascular disease
It is known that in patients with type 2 diabetes, cardiovascular mortality increases by 3-4 times, compared with people without metabolic disorders. Now more and more scientists and practitioners are convinced that Insulin resistance, and with it hyperinsulinemia, is a serious risk factor for heart attack and stroke. Moreover, this risk does not depend on whether the patient has developed diabetes or not.
Since the 1980s, studies have shown that insulin has a direct atherogenic effect on the walls of blood vessels. This means that atherosclerotic plaques and narrowing of the lumen of the vessels progress under the action of insulin in the blood that flows through them.
Insulin causes proliferation and migration of smooth muscle cells, lipid synthesis in them, fibroblast proliferation, activation of the blood coagulation system, and a decrease in fibrinolysis activity. Thus, hyperinsulinemia (increased concentration of insulin in the blood due to insulin resistance) is an important cause of atherosclerosis. This happens long before the onset of type 2 diabetes in a patient.
Studies show a clear direct relationship between excess insulin and risk factors for cardiovascular disease. Insulin resistance leads to:
- increased abdominal obesity;
- the blood cholesterol profile worsens, and plaques from “bad” cholesterol form on the walls of blood vessels;
- increases the likelihood of blood clots in the vessels;
- the wall of the carotid artery becomes thicker (the lumen of the artery narrows).
This stable relationship has been proven both in patients with type 2 diabetes mellitus and in individuals without it.
An effective way to treat insulin resistance in the early stages of type 2 diabetes, and even better before it develops, is in the diet. To be precise, this is not a method of treatment, but only control, restoring balance in case of impaired metabolism. A low-carbohydrate diet for insulin resistance should be followed for life.
After 3-4 days of switching to a new diet, most people notice an improvement in their well-being. After 6-8 weeks, tests show that “good” cholesterol in the blood rises and “bad” cholesterol falls. The level of triglycerides in the blood drops to normal. Moreover, this happens after 3-4 days, and cholesterol tests improve later. Thus, the risk of atherosclerosis is reduced several times.
Recipes for a low-carbohydrate diet against insulin resistance get
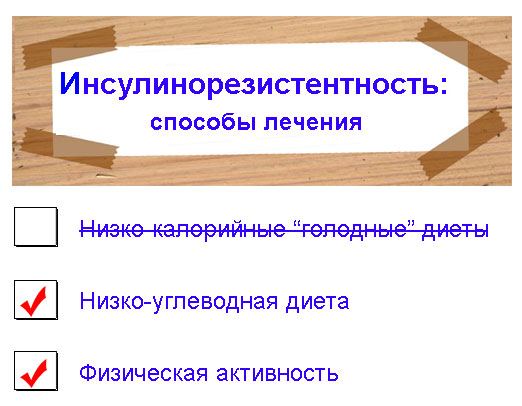
Currently, there is no real treatment for insulin resistance. Specialists in the field of genetics and biology are working on this. You will be able to control this problem well by following a low-carbohydrate diet. First of all, you need to stop eating refined carbohydrates, i.e. sugar, sweets and white flour products.
Medicine gives good results. Use it in addition to your diet, not in place of it, and check with your doctor before taking the pills. Every day we follow the news in the treatment of insulin resistance. Modern genetics and microbiology work wonders. And there is hope that in the coming years they will be able to finally solve this problem. If you want to be the first to know, subscribe to our newsletter, it's free.