Drawing up diagrams of the composition of inhaled and exhaled air. Laboratory work. Composition of inhaled and exhaled air. Vital capacity of the lungs
Breathing is an essential sign of life. We breathe constantly from the moment of birth until death. We breathe day and night during deep sleep, in health and illness.
In the human and animal bodies, oxygen reserves are limited. Therefore, the body needs a continuous supply of oxygen from the environment. Carbon dioxide must also be constantly and continuously removed from the body, which is always formed during the metabolic process and is a toxic compound in large quantities.
Breathing is a complex continuous process, as a result of which the gas composition of the blood is constantly updated. This is its essence.
Normal functioning of the human body is possible only if it is replenished with energy, which is continuously consumed. The body receives energy through the oxidation of complex organic substances - proteins, fats, carbohydrates. At the same time, hidden chemical energy is released, which is the source of vital activity of body cells, their development and growth. Thus, the importance of breathing is to maintain an optimal level of redox processes in the body.
In the process of breathing, it is customary to distinguish three parts: external, or pulmonary, respiration, gas transport by blood and internal, or tissue, respiration.
External respiration is the exchange of gases between the body and the atmospheric air surrounding it. External respiration can be divided into two stages - the exchange of gases between atmospheric and alveolar air and the gas exchange between the blood of the pulmonary capillaries and the alveolar air. External respiration is carried out due to the activity of the external respiration apparatus.
The external respiration apparatus includes the airways, lungs, pleura, chest skeleton and muscles, and the diaphragm. The main function of the external respiration apparatus is to provide the body with oxygen and relieve it of excess carbon dioxide. The functional state of the external respiration apparatus can be judged by the rhythm, depth, frequency of breathing, the size of the lung volumes, the indicators of oxygen absorption and carbon dioxide release, etc.
Transport of gases is carried out by blood. It is provided by the difference in partial pressure (tension) of gases along their path: oxygen from the lungs to the tissues, carbon dioxide from the cells to the lungs.
Internal or tissue respiration can also be divided into two stages. The first stage is the exchange of gases between blood and tissues. The second is the consumption of oxygen by cells and the release of carbon dioxide by them (cellular respiration).
Composition of inhaled, exhaled and alveolar air
A person breathes atmospheric air, which has the following composition: 20.94% oxygen, 0.03% carbon dioxide, 79.03% nitrogen. Exhaled air contains 16.3% oxygen, 4% carbon dioxide, and 79.7% nitrogen.
The composition of exhaled air is not constant and depends on the intensity of metabolism, as well as on the frequency and depth of breathing. As soon as you hold your breath or make several deep breathing movements, the composition of the exhaled air changes.
Comparison of the composition of inhaled and exhaled air serves as evidence of the existence of external respiration.
Alveolar air differs in composition from atmospheric air, which is quite natural. In the alveoli, gases are exchanged between air and blood, while oxygen diffuses into the blood, and carbon dioxide diffuses out of the blood. As a result, the oxygen content in the alveolar air sharply decreases and the amount of carbon dioxide increases. The percentage of individual gases in the alveolar air: 14.2-14.6% oxygen, 5.2-5.7% carbon dioxide, 79.7-80% nitrogen. Alveolar air differs in composition from exhaled air. This is explained by the fact that the exhaled air contains a mixture of gases from the alveoli and harmful space.
Atmospheric air entering the lungs during inhalation is called inhaled by air; air released through the respiratory tract during exhalation - exhaled. Exhaled air is a mixture of air filling out alveoli, - alveolar air- with air located in the airways (in the nasal cavity, larynx, trachea and bronchi). The composition of inhaled, exhaled and alveolar air under normal conditions in a healthy person is quite constant and is determined by the following figures (Table 3).
These figures may fluctuate somewhat depending on various conditions (state of rest or work, etc.). But under all conditions, alveolar air differs from inhaled air by a significantly lower oxygen content and a higher carbon dioxide content. This occurs as a result of the fact that in the pulmonary alveoli, oxygen enters the blood from the air, and carbon dioxide is released back.
Gas exchange in the lungs due to the fact that in pulmonary alveoli and venous blood flowing to the lungs, pressure of oxygen and carbon dioxide different: the oxygen pressure in the alveoli is higher than in the blood, and the carbon dioxide pressure, on the contrary, in the blood is higher than in the alveoli. Therefore, in the lungs the transition of oxygen from air to blood takes place, and carbon dioxide from blood to air. This transition of gases is explained by certain physical laws: if the pressure of a gas located in a liquid and in the air surrounding it is different, then the gas passes from the liquid to the air and vice versa until the pressure is balanced.
Table 3
In a mixture of gases, such as air, the pressure of each gas is determined by the percentage content of this gas and is called partial pressure(from the Latin word pars - part). For example, atmospheric air exerts a pressure equal to 760 mmHg. The oxygen content in the air is 20.94%. The partial pressure of atmospheric oxygen will be 20.94% of the total air pressure, i.e. 760 mm, and equal to 159 mm of mercury. It has been established that the partial pressure of oxygen in the alveolar air is 100 - 110 mm, and in the venous blood and capillaries of the lungs - 40 mm. The partial pressure of carbon dioxide is 40 mm in the alveoli, and 47 mm in the blood. The difference in partial pressure between blood and air gases explains gas exchange in the lungs. In this process, the cells of the walls of the pulmonary alveoli and blood capillaries of the lungs, through which gases pass, play an active role.
Transfer of gases by blood
Blood continuously carries oxygen from the lungs to the tissues and carbon dioxide from the tissues to the lungs. The arterial blood flowing from the lungs contains much more oxygen than it should according to the physical laws of dissolution of gases in liquids. This is explained by the fact that most of the oxygen in the blood is not dissolved, but in a chemically bound state. Oxygen coming from the pulmonary alveoli into the blood plasma actively penetrates red blood cells and combines with hemoglobin, forming a fragile chemical compound - oxyhemoglobin. New portions of oxygen flow from the alveoli into the blood plasma, and from it into the red blood cells until almost all of the hemoglobin is converted into oxyhemoglobin. When breathing atomosphere air under normal conditions, 96% of hemoglobin turns into oxyhemoglobin, and as a result, red blood cells contain 60 times more oxygen than blood plasma. This provides the tissues with the amount of oxygen necessary for metabolism.
Gas exchange in tissues occurs according to the same principle as in the lungs. As blood passes through the blood capillaries of various organs, oxygen moves from an area of high partial pressure (blood plasma) to an area of low partial pressure (tissue fluid). From the tissue fluid, oxygen enters the cells and immediately enters into chemical oxidation reactions. As a result, the partial pressure of oxygen inside the cells is always zero. As oxygen leaves the blood plasma, oxyhemoglobin turns into hemoglobin, ensuring a sufficient concentration of oxygen in the plasma. The conversion of oxyhemoglobin into hemoglobin is facilitated by many factors and, in particular, the saturation of the blood with carbon dioxide and an increase in the temperature of the blood in the organs (for example, in the muscles during their contraction).
Carbon dioxide produced in cells during the metabolic process enters the tissue fluid, creating a high partial pressure in it. In the blood flowing through the blood capillaries of various organs, the partial pressure of carbon dioxide is much lower, so carbon dioxide passes from the tissue fluid into the blood. Blood contains significantly more carbon dioxide than is possible due to its dissolution in liquid. This is also determined by the fact that carbon dioxide is not only in a dissolved state in the plasma, but also enters into a chemical combination with the hemoglobin of erythrocytes and with plasma salts. With the participation of a special enzyme, carbon dioxide also relatively easily combines with water in the blood plasma, forming carbonic acid, which again breaks down in the lungs into carbon dioxide and water. This ensures the possibility of removing all carbon dioxide formed in the tissues. Blood that has given up oxygen and is saturated with carbon dioxide is called venous.
Venous blood enters the lungs, where pulmonary respiration occurs.
Mechanism of inhalation and exhalation
The act of breathing consists of rhythmically repeating inhalation and exhalation.
Inhalation is carried out as follows. Under the influence of nerve impulses, the muscles involved in the act of inhalation contract: the diaphragm, external intercostal muscles, etc. During its contraction, the diaphragm lowers (flattens), which leads to an increase in the vertical size of the thoracic cavity. When the external intercostal and some other muscles contract, the ribs rise, and the anteroposterior and transverse dimensions of the thoracic cavity increase. Thus, as a result of muscle contraction, the volume of the chest increases (Fig. 74). Due to the fact that there is no air in the pleural cavity and the pressure in it is negative, simultaneously with the increase in the volume of the chest, the lungs expand. As the lungs expand, the air pressure inside them decreases (it becomes lower than atmospheric pressure) and atmospheric air rushes through the respiratory tract into the lungs. Consequently, when inhaling, the following occurs sequentially: muscle contraction - an increase in the volume of the chest - expansion of the lungs and a decrease in pressure inside the lungs - the flow of air through the airways into the lungs.
Rice. 74. Diagram depicting changes in the chest and diaphragm during breathing
Exhalation occurs after inhalation. The muscles involved in the act of inhalation relax (the diaphragm rises), and the ribs fall as a result of contraction of the internal intercostal and other muscles and due to their heaviness. The volume of the chest decreases (see Fig. 74), the lungs are compressed, the pressure in them increases (becomes higher than atmospheric pressure), and air rushes out through the airways.
Breathing movements are rhythmic. In a calm adult, 16 to 20 respiratory movements occur per minute. In children they are more frequent (in a newborn about 60 per minute). As a rule, physical activity, especially in poorly trained people, is accompanied by increased breathing. In many diseases, increased respiratory movements are also observed. Increased breathing may be accompanied by a decrease in its depth. During sleep, breathing slows down.
There are two types of breathing: abdominal (predominant in men) and thoracic (in women). In the first type, the volume of the chest cavity increases mainly as a result of contraction of the diaphragm (increase in vertical size), in the second - as a result of contraction of other respiratory muscles (increase in the anteroposterior and transverse dimensions of the chest).
Vital capacity of the lungs
To functionally characterize the lungs, they use the determination of their vital capacity. The vital capacity of the lungs refers to the amount of air that a person is able to exhale after a deep breath. On average it is 3500 cm3. The amount of vital capacity of the lungs largely depends on training, age and gender.
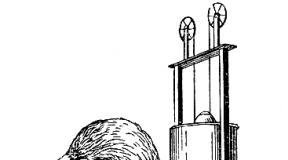
Systematic physical education and sports help increase the vital capacity of the lungs (for some athletes it reaches 6000 - 7000 cm 3). Women have a smaller vital capacity on average than men; in young people it is greater than in older people. To determine the vital capacity of the lungs, a special device is used - a spirometer (Fig. 75).

Fig. 75. Spirometry (the subject exhaled deeply)
During quiet breathing, about 500 cm 3 of air enters the lungs in one breath. This volume is called breathing air. With maximum inhalation after a quiet exhalation, air enters the lungs on average 1500 cm 3 more than with a quiet inhalation. This volume of air is called additional. With maximum exhalation after a normal inhalation, you can remove an average of 1500 cm 3 more air from the lungs than with a normal exhalation. This volume of air is called reserve. All three volumes of air - respiratory, additional and reserve - together make up the vital capacity of the lungs; on average: 500 cm 3 + 1500 cm 3 + 1500 cm 3 = 3500 cm 3 of air.
After exhalation, even the deepest, about 1000 cm 3 of air remains in the lungs. This volume is called residual air.
Due to the presence of residual air, a lung immersed in water does not sink. Before birth, the fetus does not have pulmonary respiration and the lungs do not contain air. A piece of something so light sinks in water. Air enters the lungs after birth with the first breath.
Pneumothorax. When there is a chest injury with damage to the pleura, atmospheric air enters the pleural cavity - pneumothorax. In this case, the pressure in the pleural cavity will be the same as in the lung. The lung, due to its elasticity, collapses and does not participate in breathing. In medical practice, they sometimes resort to artificially introducing air into the pleural cavity (artificial pneumothorax).
Breathing regulation
The mechanism of breathing regulation is very complex. In a schematic presentation it comes down to the following. In the medulla oblongata there is a cluster of nerve cells that regulate breathing - the respiratory center. Its presence was noted by the Russian scientist N.A. Mislavsky in 1885. In the respiratory center, two sections are distinguished: the inhalation section and the exhalation section. The function of both departments is interconnected: when the inhalation department is excited, the exhalation department is inhibited, and, conversely, the excitation of the exhalation department is accompanied by inhibition of the inhalation department. In addition to the respiratory center located in the medulla oblongata, special clusters of nerve cells in the pons and diencephalon are involved in the regulation of breathing. The respiratory center exerts its influence on the respiratory muscles, on which the change in chest volume during inhalation and exhalation depends, not directly, but through the spinal cord. In the spinal cord there are groups of cells, the processes of which (nerve fibers) go as part of the spinal nerves to the respiratory muscles. When the respiratory center (inspiratory department) is excited, nerve impulses are transmitted to the spinal cord, and from there along the nerves to the respiratory muscles, causing them to contract; As a result, the chest expands and inhalation occurs. The cessation of the transmission of impulses from the respiratory center (during inhibition of the inspiratory department) to the spinal cord, and from it to the respiratory muscles is accompanied by relaxation of these muscles; As a result, the chest collapses and exhalation occurs.
In the respiratory center, there is an alternating change in the state of excitation and inhibition (inhalation and exhalation departments), which causes rhythmic alternations of inhalation and exhalation. Changes in the state of the respiratory center depend on nervous and humoral influences. In this case, an important role belongs to the receptors of the lungs and carbon dioxide in the blood. During inhalation, the lungs stretch and due to this, the endings of the vagus nerve embedded in the lung tissue are irritated. Nerve impulses generated in the receptors are transmitted along the vagus nerve to the respiratory center, causing stimulation of the exhalation department and at the same time inhibition of the inhalation department. As a result, the transmission of impulses from the respiratory center to the spinal cord stops and exhalation occurs. When you exhale, the lung tissue collapses, the lung receptors are not irritated, and nerve impulses from the receptors do not enter the respiratory center. As a result, the exhalation section comes into a state of inhibition, at the same time the inhalation section is excited and inhalation occurs. Then everything repeats again. In this way, automatic self-regulation of breathing is carried out: inhalation causes exhalation, and exhalation causes inhalation.
Carbon dioxide is a specific respiratory pathogen. When carbon dioxide accumulates in the blood to a certain concentration, special receptors in the walls of blood vessels are irritated. The impulses generated in the receptors are transmitted along nerve fibers to the respiratory center (inspiratory department) and cause its excitation, which is accompanied by deepening and increased breathing. In addition, carbon dioxide also has a direct effect on the respiratory center: an increase in the concentration of carbon dioxide in the blood washing the respiratory center causes its excitation. A decrease in the concentration of carbon dioxide in the blood is accompanied, on the contrary, by a decrease in the excitability of the respiratory center (inspiratory department).
If, as a result of intense muscular work or for other reasons, an excess amount of carbon dioxide accumulates in the blood, then due to excitation of the respiratory center, breathing becomes rapid - shortness of breath occurs. As a result, carbon dioxide is quickly eliminated from the body and its content in the blood becomes normal. The respiratory rate also becomes normal. The accumulation of carbon dioxide automatically causes its rapid elimination and thereby a decrease in the excitability of the respiratory center (inhalation department).
Along with excess carbon dioxide, excitation of the respiratory center is also caused by a lack of oxygen, as well as some other substances entering the blood, in particular special medicinal substances. It should be noted that the reflex effect on the respiratory center is exerted not only by irritation of the receptors of the walls of blood vessels and the receptors of the lungs themselves, but also by other influences (for example, irritation of the nasal mucosa with ammonia, irritation of the skin with cold water, etc.).
Breathing is subordinated to the cerebral cortex, evidence of which is that a person can voluntarily hold his breath (albeit for a very short time) or change its depth and frequency. Evidence of cortical regulation of breathing is also increased breathing during emotional states. Breathing is associated with protective acts: coughing and sneezing. They are carried out reflexively, and the centers of these reflexes are located in the medulla oblongata.
Cough occurs in response to irritation of the mucous membrane of the larynx, pharynx or bronchi (when particles of dust, food, etc. get there). When you cough after a deep breath, air is forcefully pushed out of the respiratory tract and causes the vocal cords to move (a characteristic sound appears). Together with the air, what irritated the respiratory tract is removed.
Sneeze occurs in response to irritation of the nasal mucosa according to the same principle as a cough.
Coughing and sneezing are protective breathing reflexes.
The atmosphere is the air envelope of the earth's surface, consisting of a mixture of gases, having different densities at different altitudes. This circumstance is due to gravity. As you move away from the earth's surface, the density of the air envelope decreases and ultimately equalizes the density of interstellar space.
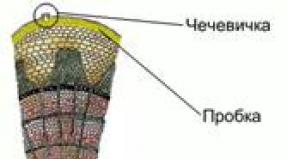
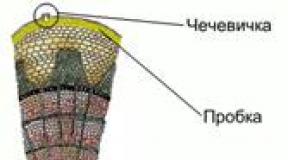
The air shell contains the most nitrogen, followed by oxygen, then carbon dioxide and a number of so-called neutral gases (argon, neon, helium, etc.). There are also always varying amounts of water vapor in the air. Finally, sometimes the outside air contains ozone and hydrogen peroxide, which, however, are temporary impurities of the gas composition of the air. The composition of inhaled (atmospheric) and exhaled air can be judged from Fig. 1.
Rice. 1. The chemical composition of inhaled and exhaled air.
The diagram shows that the composition of exhaled air differs significantly from the composition of inhaled air. If the amount of oxygen in the inhaled air is 20.94%, then approximately 15-16% remains in the exhaled air, therefore, the decrease is about 25%. The quantitative ratios of nitrogen remain approximately the same. Carbon dioxide undergoes the most noticeable changes, the amount of which increases from 0.03-0.04% in inhaled air to 4% in exhaled air, i.e. increases 100 times. The exhaled air also differs in its physical properties: its temperature increases significantly (up to 38°), and the relative humidity approaches 100%. From the above, it is clear that the exhaled air has an unfavorable chemical composition and physical properties, and since the lungs, when working hard, pass from 350-450 to 3800 l/hour of air, it becomes clear why such air (if there is no influx of fresh air) can cause health problems person and have an adverse effect on his health.
Let us dwell in more detail on the physiological and hygienic significance of the individual ingredients of the gas composition of the air mixture.
Oxygen plays the most significant role in the life of the body. Insufficient oxygen supply to tissues causes disturbances in the body's vital functions, which manifest themselves when the oxygen content in the inhaled air decreases to 7-8%. Further reduction leads to more severe consequences, and in case of severe oxygen starvation - to death due to damage to the central nervous system, which is especially in need of a constant supply of oxygen (in particular, as a result of paralysis of the respiratory center).
Oxygen cycles occur in the air all the time. Huge quantities of this gas are spent on the respiration of people and animals, combustion of fuel, oxidation of organic substances, etc. The restoration of this constant consumption of oxygen occurs mainly due to its release by the green chlorophyll parts of plants, which, under the influence of solar radiation, absorb carbon dioxide in the air and in the presence moisture decomposes it to form oxygen. Thanks to this balance, the oxygen concentration in the atmospheric air remains almost unchanged (changes reach only 0.1-0.2%). This explains the fact that practically under normal human living conditions there is no oxygen deficiency. The only exceptions are conditions when the access of oxygen is limited (for example, in deep mines, submarines, etc.), and also when, due to natural conditions, the partial pressure of oxygen in the air is significantly reduced (at mountain altitudes more than 2000 m above level; sea level, when flying at high altitude). However, in these cases, the human body, using compensatory mechanisms (increasing the volume of pulmonary ventilation, increasing the number of red blood cells), is able to adapt to such a decrease in the partial pressure of oxygen, of course, within certain limits.
Atmospheric air, which a person inhales while outdoors (or in well-ventilated rooms), contains 20.94% oxygen, 0.03% carbon dioxide, 79.03% nitrogen. In enclosed spaces filled with people, the percentage of carbon dioxide in the air may be slightly higher.
Exhaled air contains on average 16.3% oxygen, 4% carbon dioxide, 79.7% nitrogen (these figures are based on dry air, i.e. minus water vapor, which is always saturated in exhaled air).
Composition of exhaled air very fickle; it depends on the intensity of the body's metabolism and the volume of pulmonary ventilation. It is worth making several deep breathing movements or, on the contrary, holding your breath so that the composition of the exhaled air changes.
Nitrogen does not participate in gas exchange, but the percentage of nitrogen in visible air is several tenths of a percent higher than in inhaled air. The fact is that the volume of exhaled air is slightly less than the volume of inhaled air, and therefore the same amount of nitrogen, distributed in a smaller volume, gives a higher percentage. The smaller volume of exhaled air compared to the volume of inhaled air is explained by the fact that slightly less carbon dioxide is released than oxygen is absorbed (part of the absorbed oxygen is used in the body to circulate compounds that are excreted from the body in urine and sweat).
Alveolar air differs from exhaled breath by a larger percentage of non-acid and a smaller percentage of oxygen. On average, the composition of alveolar air is as follows: oxygen 14.2-14.0%, carbon dioxide 5.5-5.7%, nitrogen about 80%.
Definition alveolar air composition important for understanding the mechanism of gas exchange in the lungs. Holden proposed a simple method for determining the composition of alveolar air. After a normal inhalation, the subject exhales as deeply as possible through a tube 1-1.2 m long and 25 mm in diameter. The first portions of exhaled air leaving through the tube contain air from the harmful space; the last portions remaining in the tube contain alveolar air. For analysis, air is taken into the gas receiver from the part of the tube that is closest to the mouth.
The composition of alveolar air differs somewhat depending on whether the air sample is taken for analysis at the height of inhalation or exhalation. If you exhale quickly, briefly, and incompletely at the end of a normal inhalation, the air sample will reflect the composition of the alveolar air after the lungs have been filled with respiratory air, i.e., during inhalation. If you exhale deeply after a normal exhalation, the sample will reflect the composition of the alveolar air during exhalation. It is clear that in the first case the percentage of carbon dioxide will be slightly less, and the percentage of oxygen will be slightly higher than in the second. This can be seen from the results of Holden's experiments, who found that the percentage of carbon dioxide in the alveolar air at the end of inspiration averages 5.54, and at the end of exhalation - 5.72.
Thus, there is a relatively small difference in the content of carbon dioxide in the alveolar air during inhalation and exhalation: only 0.2-0.3%. This is largely explained by the fact that during normal breathing, as mentioned above, only 1/7 of the volume of air in the pulmonary alveoli is renewed. The relative constancy of the composition of alveolar air is of great physiological importance, as will be clarified below.
| Parameter name | Meaning |
| Article topic: | Composition of inhaled and exhaled air |
| Rubric (thematic category) | Sport |
Physiology of breathing
The vital activity of a living organism is associated with its absorption of O 2 and the release of CO 2. For this reason, the concept of respiration includes all processes associated with the delivery of O 2 from the external environment into cells and the release of CO 2 from the cell into the environment.
The physiology of respiration refers to the following processes: external respiration, gas exchange in the lungs, gas transport in the blood, tissue and cellular respiration.
External respiration is carried out by the human respiratory apparatus. It includes the chest with the muscles that move it and the lungs with the airways. The main respiratory muscles are the diaphragm and intercostal muscles - internal and external.
When you inhale, the muscle fibers of the diaphragm contract, it flattens and moves down. In this case, the chest increases in the vertical direction. Contraction of the external costal muscles lifts the ribs and moves them to the sides and the sternum forward. In this case, the chest expands in the transverse and anteroposterior directions. As the chest cavity expands, the lungs also passively expand due to atmospheric pressure acting through the airways on the inner surface of the lungs. When the lungs expand, the air in them is distributed in a larger volume and the pressure in the lung cavity becomes lower than atmospheric (by 3-4 mmHg). The pressure difference is the reason why atmospheric air begins to enter the lungs - inhalation occurs.
Exhalation occurs as a result of relaxation of the respiratory muscles. When their contraction stops, the chest lowers and returns to its original position. The relaxed diaphragm rises up and takes the shape of a dome. Stretched lungs decrease in volume. All together leads to an increase in intrapulmonary pressure. Air leaves the lungs to the outside - exhalation occurs.
Gas exchange or ventilation of the lungs is the volume of air passing through the lungs in one minute - the minute volume of respiration. At rest it is 5-8 l/min, and increases with muscular work.
A person inhales atmospheric air, which contains 20.94% oxygen, 78.03% nitrogen, and 0.03% carbon dioxide. Exhaled air contains less oxygen (16.3%) and 4% carbon dioxide. Due to the difference in the partial pressure of O 2 in the inhaled and exhaled air, oxygen from the air enters the alveoli of the lungs. The partial pressure of CO 2 in the capillaries of venous blood is 47 mm Hg, and the partial pressure of CO 2 in the alveoli is 40. Due to the difference in partial pressure, CO 2 leaves the venous blood into the air. Nitrogen does not participate in gas exchange. The conditions of gas exchange in the lungs are so favorable that, despite the fact that the time of passage of blood through the capillaries of the lungs is about 1 second, the tension of gases in the alveolar blood flowing from the lungs is the same as it would be after prolonged contact.
If ventilation of the lungs is insufficient and the CO 2 content in the alveoli increases, then the level of CO 2 in the blood also increases, which immediately leads to increased breathing - shortness of breath.
Transfer of gases by blood.
Gases dissolve very poorly in liquid: 100 ml of blood can physically dissolve about 2% oxygen and 3-4% carbon dioxide. But red blood cells contain hemoglobin, which is capable of chemically binding O 2 and CO 2. The combination of hemoglobin with oxygen is usually called oxyhemoglobin Hb+O 2 ®HbO 2, which is found in arterial blood. Oxyhemoglobin is not a strong compound; if we consider that human blood contains about 15% hemoglobin, then 100 ml of blood can bring up to 21 ml of O 2. This is the so-called oxygen capacity of the blood. Oxyhemoglobin with arterial blood is sent to tissues and cells, where O2 is consumed as a result of continuously ongoing oxidative processes. Hemoglobin picks up carbon dioxide released from the tissues and a fragile compound HbCO 2 - carbhemoglobin is formed. About 10% of the released carbon dioxide enters into such a compound. The rest combines with water and turns into carbonic acid. This reaction is accelerated thousands of times by a special enzyme, carbonic anhydrase, found in red blood cells. Next, carbonic acid in tissue capillaries reacts with sodium and potassium ions, forming bicarbonates (NaHCO 3, KHCO 3). All these compounds are transported to the lungs.
Hemoglobin combines especially easily with carbon monoxide CO 2 (carbon monoxide) to form carboxyhemoglobin, which is incapable of carrying oxygen. Its chemical affinity for hemoglobin is almost 300 times higher than for O 2. So, with a CO concentration in the air equal to 0.1%, about 80% of the hemoglobin in the blood is associated not with oxygen, but with carbon monoxide. As a result, symptoms of oxygen starvation occur in the human body (vomiting, headache, loss of consciousness). Mild carbon monoxide poisoning is a reversible process: CO is gradually split off from hemoglobin and eliminated by breathing fresh air. In severe cases, the death of the body occurs.
Composition of inhaled and exhaled air - concept and types. Classification and features of the category “Composition of inhaled and exhaled air” 2017, 2018.